In the past year, several reports have highlighted emerging global threats from neurological infections and have brought up a new appreciation for the particular sensitivity of the CNS to damage from dysregulated inflammatory responses.
Between Aug 2, 2014, and April 14, 2015, the US Centers for Disease Control and Prevention received reports of 118 children (median age 7 years) with acute flaccid paralysis.1 This disease was associated with an infection with enterovirus D68 (EV-D68). Neurological symptoms progressed rapidly, with maximum illness severity occurring by 2–4 days after infection. MRI showed non-enhancing lesions of the grey matter in the spinal cord and affecting multiple levels, including the brainstem in some patients.2
Ebola infections in west Africa have been a major news story in the past year. As of October, 2015, nearly 18000 cases have been reported, with about 6500 deaths, with the infection spreading rapidly because the virus is present in all body fluids, including sweat and mucous membrane secretions. It is now becoming apparent that many patients might have died from neurological complications such as meningoencephalitis, which was not recognised easily at the peak of the epidemic because of multi-organ involvement. Survivors of the infection also have persistent neurological symptoms but the full range of neurological sequelae is only now being characterised in ongoing studies in Liberia. Importantly, a case of recurrent meningoencephalitis of a nurse in the UK nearly 9 months after the initial infection in Africa suggests that the brain might act as a reservoir for the virus, which could reside for prolonged periods despite recovery from the acute infection.3
At present, cryptococcal meningitis is the largest single cause of neurological infectious death worldwide, with up to 500 000 fatalities per year and mortality rates of 25–50% despite treatment. Three studies of HIV-infected individuals have highlighted the exquisite sensitivity of the CNS to host-damaging immune reconstitutions after antiretroviral therapy. Studies by Jarvis and colleagues4 and Meya and colleagues5 characterised the fine balance between an effective CNS response needed for fungal clearance and an excessive damaging response, with a prominent role for activated pro-inflammatory macrophages. In a third study, Scriven and colleagues6 characterised neuroinflammatory changes in patients from the Cryptococcal Optimal ART Timing (COAT) trial, which was halted last year following the surprising finding that antiretroviral therapy early in the course of cryptococcal meningitis (at 1–2 weeks after diagnosis) resulted in a worse outcome than if given later (at 5 weeks after diagnosis), by contrast with the clinical experience in patients with non-neurological infections such as pneumocystis pneumonia where early ART therapy is preferred. These studies showed the role that CSF cellular infiltrates and macrophage activation have in excess mortality, even in the absence of overt CNS immune reconstitution syndrome. An additional study of cryptococcal meningitis in previously healthy individuals without HIV infection described a new post-infectious inflammatory response syndrome.7 This natural history study showed that, unlike the disease in HIV-infected patients with T-cell defects, the disease in this population was associated with increased markers of T-cell activation, accompanied by axonal damage. All these studies showed the important role of intrathecal immunological characterisations to clarify and resolve controversies in CNS infections and to guide the selection of immune-modulating therapeutics.
The burden of tuberculous meningitis is a major problem in developing countries, where the risk of death in children with tuberculous meningitis can be almost 20% and neurological sequelae occur in more than 50% of patients. A study by Visser and colleagues8 contributed important insights into immune-mediated host damage that could guide treatment. The study suggested a role for intrathecal inflammation in the pathology of childhood tuberculous meningitis, with increased proinflammatory cytokines and a disease-specific pattern of biomarkers, including cathlicidin antimicrobial peptides, found in lysosomes of macrophages and neutrophils.8 These data provide physiological confirmation that could support recent efforts to use adjunct steroids to control inflammation and to manipulate cathlicidin antimicrobial peptides in patients by improving cathlicidin-boosting vitamin D levels.
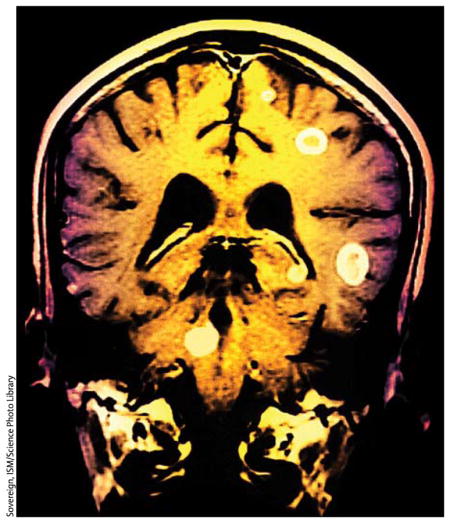
Cerebral malaria is one of the most devastating complications of a disease that kills more than half a million people every year and is refractory to adjuvant therapies such as corticosteroids. In a recent study, Seydel and colleagues9 analysed MRI data from 168 children with cerebral malaria and found evidence for brain swelling in 21 of the 25 children who died, whereas only 27% of the survivors had similar MRI findings.9 This finding supports previous data indicating differences in adult and childhood cerebral malaria and distinguishes it from most other forms of vasogenic cerebral oedema, that are often responsive to steroid treatment.
During a 2-year period (2011–13), three breeders of variegated squirrels in Germany developed signs and symptoms of a viral encephalitis, with fever, cognitive dysfunction, ataxia, myoclonus, ocular paresis, or a combination of these symptoms, progressing to coma and death 2–4 months after presentation. CSF showed a moderate pleocytosis, which was lymphocytic in the only patient from whom a differential count was obtained. MRI scans indicated the presence and progressive worsening of oedematous lesions in the cerebral cortex and basal ganglia or, in one patient, mainly meningeal enhancement with dilated ventricles. Through the use of next-generation sequencing and real-time reverse-transcriptase quantitative PCR, investigators detected a new bornavirus in a contact squirrel and in brain specimens from the three patients.10 The squirrels had been imported from Latin America, which suggests that this infection could be much more widespread than initially thought and might often go undiagnosed.10
A recent study also showed that an endogenous retrovirus called HERV-K that was incorporated into the human genome nearly 2–5 million years ago can get activated in the brain of patients with amyotrophic lateral sclerosis. Although this virus has an important role in early embryogenesis, it is silenced in mature cells. Reactivation in neurons is toxic, and transgenic animals expressing the envelope protein of the virus have classic symptoms and pathology similar to those in amyotrophic lateral sclerosis.11 These findings have raised hope that targeting this virus could provide a novel and viable therapeutic approach to amyotrophic lateral sclerosis—a disease for which very few treatment options are currently available.
Acknowledgments
Our work is supported by intramural funding of the National Institute of Allergy and Infectious Diseases, National Institutes of Health. We declare no competing interests.
References
- 1.Centers for Disease Control and Prevention. Acute flaccid paralysis with anterior myelitis—California, June 2012–June 2014. Morb Mortal Wkly Rep. 2014;63:903–06. [PMC free article] [PubMed] [Google Scholar]
- 2.Messacar K, Schreiner TL, Maloney JA, et al. A cluster of acute flaccid paralysis and cranial nerve dysfunction temporally associated with an outbreak of enterovirus D68 in children in Colorado, USA. Lancet. 2015;385:1662–71. doi: 10.1016/S0140-6736(14)62457-0. [DOI] [PubMed] [Google Scholar]
- 3.The New York Times. [accessed Nov 19, 2015];New clues into Ebola as ill nurse improves. 2015 Oct 21; http://www.nytimes.com/2015/10/22/world/europe/new-clues-into-ebola-as-ill-nurse-improves.html?_r=0.
- 4.Jarvis JN, Meintjes G, Bicanic T, et al. Cerebrospinal fluid cytokine profiles predict risk of early mortality and immune reconstitution inflammatory syndrome in HIV-associated cryptococcal meningitis. PLoS Pathog. 2015;11:e1004754. doi: 10.1371/journal.ppat.1004754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meya DB, Okurut S, Zziwa G, et al. Cellular immune activation in cerebrospinal fluid from ugandans with cryptococcal meningitis and immune reconstitution inflammatory syndrome. J Infect Dis. 2015;211:1597–606. doi: 10.1093/infdis/jiu664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scriven JE, Rhein J, Hullsiek KH, et al. Early ART after cryptococcal meningitis is associated with cerebrospinal fluid pleocytosis and macrophage activation in a multisite randomized trial. J Infect Dis. 2015;212:769–78. doi: 10.1093/infdis/jiv067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Panackal AA, Wuest SC, Lin YC, et al. Paradoxical immune responses in non-HIV cryptococcal meningitis. PLoS Pathog. 2015;11:e1004884. doi: 10.1371/journal.ppat.1004884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Visser DH, Solomons RS, Ronacher K, et al. Host immune response to tuberculous meningitis. Clin Infect Dis. 2015;60:177–87. doi: 10.1093/cid/ciu781. [DOI] [PubMed] [Google Scholar]
- 9.Seydel KB, Kampondeni SD, Valim C, et al. Brain swelling and death in children with cerebral malaria. N Engl J Med. 2015;372:1126–37. doi: 10.1056/NEJMoa1400116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoffmann B, Tappe D, Hoper D, et al. A variegated squirrel bornavirus associated with fatal human encephalitis. N Engl J Med. 2015;373:154–62. doi: 10.1056/NEJMoa1415627. [DOI] [PubMed] [Google Scholar]
- 11.Li W, Lee MH, Henderson L, et al. Human endogenous retrovirus-K contributes to motor neuron disease. Sci Transl Med. 2015;7:307ra153. doi: 10.1126/scitranslmed.aac8201. [DOI] [PMC free article] [PubMed] [Google Scholar]


