Abstract
Importance
Limited evidence exists on salary differences between male and female academic physicians, largely due to difficulty obtaining data on salary and factors influencing salary. Existing studies have been limited by reliance on survey-based approaches to measuring sex differences in earnings, lack of contemporary data, small sample sizes, or limited geographic representation.
Objective
To analyze sex differences in earnings among U.S. academic physicians.
Design, setting, and participants
Freedom of Information laws mandate release of salary information of public university employees in several states. In 12 states with salary information published online, we extracted salary data on 10,241 academic physicians at 24 public medical schools. We linked this data to a unique physician database with detailed information on sex, age, years of experience, faculty rank, specialty, scientific authorship, NIH funding, clinical trial participation, and Medicare reimbursements (proxy for clinical revenue). We estimated sex differences in salary adjusting for these factors.
Exposure
Physician sex
Main outcome measures
Annual salary
Results
Female physicians had lower unadjusted salaries than male physicians ($206,641 vs. $257,957; difference $51,315; 95% CI $46,330–$56,301). Sex differences persisted after multivariable adjustment ($227,782 vs. $247,661; difference $19,878; 95% CI $15,261–$24,495). Sex differences in salary varied across specialties, institutions, and faculty ranks. Female full and associate professors had comparable adjusted salaries to those of male associate and assistant professors, respectively.
Conclusions and relevance
Among physicians with faculty appointments at 24 U.S. public medical schools, significant sex differences in salary exist even after accounting for age, experience, specialty, faculty rank, and measures of research productivity and clinical revenue.
INTRODUCTION
The number of women in medicine has grown rapidly since 1970. Women now comprise half of all U.S. medical school graduates and hold 38% of faculty positions in U.S. medical schools.1,2 Nonetheless, significant sex differences in job achievement and compensation exist in medicine. Within U.S. medical schools, several studies have documented sex differences in faculty rank.3–11 A recent analysis of sex differences in faculty rank in 2014, which used a comprehensive cross-sectional database of 91,073 U.S. physicians, found substantial sex differences in faculty rank after adjustment for physician age, years since residency completion, specialty, scientific authorship, National Institutes of Health (NIH) research funding, and clinical trial participation.12
Less attention has been paid to differences in earnings between male and female physicians, largely due to limited availability of earnings data and matching information on factors that may affect earnings, such as specialty, years of experience, clinical practice characteristics, and within academic medicine, measures of research productivity. Still, among physicians overall, several surveys have found that women earn substantially less than men after adjustment for specialty choice, hours worked, years of experience, and family structure.13–16 Within academic medicine, several studies have found that women earn less than men after adjustment for factors such as age, race, marital status, years of experience, specialty, reported work hours, research productivity and faculty rank.17–22 However, these studies have been limited by several factors, including: reliance on survey-based approaches to measuring sex differences in physician earnings, lack of contemporary data, small sample sizes, and limited geographic representation.
We undertook an analysis of sex differences in academic physician salary that was designed to mitigate many of the limitations of previous studies on this topic. Specifically, we assembled a database of salary information of academic physicians employed in 24 public medical schools in 12 states, relying on the fact that several states have Freedom of Information laws which mandate the release of government financial records that frequently include salary information on employees of public universities. We combined these data with information on clinical and research productivity of physicians to analyze sex differences in earnings.
METHODS
Salary data
Many states have Freedom of Information laws, which mandate the release of government records. These records frequently include public employee salary data, detailing the full name, title, institution, and salary of all public employees in that state. We extracted salary information of all employees in 24 state medical schools in 12 states that had public employee data available online as of November 1, 2015 (schools: Universities of California at Davis, Irvine, Los Angeles, San Diego, and San Francisco; the Universities of Florida and South Florida; Southern Illinois University and University of Illinois; University of Kansas; University of Maryland; University of Michigan; East Carolina University and University of North Carolina; Ohio State University; University of Tennessee; Universities of Texas at Houston, San Antonio, Medical Branch, and Southwestern, Texas Tech University, and MD Anderson Cancer Center; University of Washington; and University of Wisconsin). Year of salary ranged from 2011 to 2013; for instance, published salaries of UT Southwestern employees were from 2012, while salaries of University of California employees were from 2013.
We merged this individual-level salary data with a comprehensive database of U.S. physicians obtained from Doximity, a company that provides online networking services for U.S. physicians. The purpose of the match was to identify physician faculty in each state employee salary database using a list of physician names and institutional affiliations from the Doximity database. The database draws on several sources to identify physicians, including the National Plan and Provider Enumeration System (NPPES) National Provider Identifier (NPI) Registry, self-registered members, and collaborating hospitals and medical schools that provide information to the company. Additional details of this database are described below.
Individuals in the two datasets were matched iteratively, through various combinations of first and last name, middle initial, and university affiliation. University affiliation and associated faculty rank of physicians in the Doximity database were obtained from the Association of American Medical Colleges faculty roster database. Because it is possible that a physician in a medical school may share the same first and last name as a non-physician employee in that university, we excluded all non-unique names in the salary datasets.
We assessed the validity with which we were able to identify public medical school physician faculty in state employee databases in two ways. First, we sought to confirm that individuals who we identified in the salary data as being physician faculty were in fact physician faculty. For a random sample of 240 physicians (10 per school), we verified through online searches that each physician was, in fact, affiliated with that medical school. Second, we sought to determine whether unmatched physicians (that is, physicians who were listed as faculty members at a given medical school in the Doximity database, but were not matched to state employee salary records) failed to match for “correct” reasons. To accomplish this, we manually confirmed that each unmatched physician who was listed by the AAMC as a professor at a given medical school was not in the payroll data at all. Most of these physicians held titular positions at various medical schools, but earned a majority, if not the entirety, of their salary through an affiliated private hospital, and as such were not listed in the public employee payroll data.
Physician characteristics
In addition to university affiliation and faculty rank, the Doximity database included information on physician age, sex, specialty, and year of residency completion, obtained through partnerships with the American Board of Medical Specialties, state licensing boards, and collaborating hospitals and medical schools. The database also included information on the number of authored scientific publications indexed in PubMed (first, last, and total publications), number of NIH grants for which the physician was a principal investigator, obtained from the NIH RePORT database, and the number of registered clinical trials for which the physician was a principal or sub-investigator, obtained from ClinicalTrials.gov. Details of the database and validation of the accuracy of its data have been published elsewhere.12
In addition to these characteristics, we obtained information on the total amount a physician was reimbursed by Medicare in 2013, as reported in publicly available data published by the Centers for Medicare and Medicaid Services. This figure was used as a proxy for clinical revenue and full- versus part-time effort, which may influence a physician’s salary.
Statistical analysis
We estimated a physician-level multivariable linear regression model of annual salary as a function of physician sex, age, years since residency completion, faculty rank (assistant, associate, or full professor), specialty, NIH funding (yes/no indicator for whether a physician was ever a principal investigator on an NIH grant), clinical trial participation (yes/no indicator), publication count (first or last authored, and total), whether the medical school the physician graduated from ranked among the top twenty in U.S. News and World Report research rankings of medical schools in 2013 (yes/no indicator), and the total amount the physician billed to Medicare in 2013. Our model included medical school-level fixed effects, thereby identifying the sex difference in physician salary on the basis of comparisons of physicians within the same institution rather than across institutions.
We reported the absolute adjusted difference in salary between male and female physicians overall, as well as in several pre-specified subgroups (by specialty and faculty rank; for each of the 24 medical schools in our database; and for the three Census regions in which schools were located, Midwest, South, and West).
Sensitivity analysis
We conducted several sensitivity analyses. First, to address the potential impact of data inaccuracies in our measures of research productivity, we re-estimated the earnings model among registered physician members who themselves provide information in their own Doximity profiles. Second, although we used Medicare reimbursements as a proxy for clinical revenue and effort, it is possible that physicians on different faculty tracks (e.g., clinical vs research) or with varying work hours (e.g., full vs part time) may be compensated differently, which could confound sex differences in faculty rank.23 We therefore analyzed sex differences in earnings among faculty with NIH funding, who we assumed were more likely to be full-time researchers. Moreover, to further address this issue, we re-estimated our earnings model excluding the bottom 25% of earners in each specialty and institution to limit the sample to those physicians more likely be in full time rather than part time positions Third, we assessed the sensitivity of adjusted sex differences in earnings to models which included years since residency as a categorical variable (rather than continuous, to allow for non-linear effects of experience on earnings) and which included counts of NIH grants and clinical trials as opposed to binary indicators for each.
Data were approved for study by the human subjects review committee at Harvard Medical School. Stata software, version 13 (StataCorp) was used for analyses.
RESULTS
Characteristics of study population
Our sample consisted of 10,241 physician faculty in 24 public medical schools (comprising 11.0% of 93,480 physicians with academic appointments in the U.S.). Of these, 6,692 (65.4%) were men, a proportion comparable to that seen among physician faculty in remaining U.S. medical schools (55,754/83,239; 66.9% men). In unadjusted analyses, women had lower salaries than men ($206,641 vs. $257,957; absolute difference $51,315; 95% CI $46,330–$56,301) (Table 1). Women were less likely than men to be full professors (20.2% (717/3,594) vs 38.0% (2,543/6692), p<0.001), were younger (mean age 46.4 vs 51.1 years, p<0.001), completed residency more recently (14.6 vs 19.4 years, p<0.001), and were disproportionately in internal medicine, obstetrics and gynecology, and pediatrics. Women had fewer total and first/last author publications (mean total, 13.5 vs 26.1; mean first/last author, 8.6 vs 17.1; p<0.001 for both), were less likely to have had NIH funding (11.6% (412/3,594) vs 16.1% (1,076/6,692, p<0.001), and were less likely to have conducted a clinical trial (8.1% (287/3,594) vs 11.6% (773/6,692), p<0.001). Women were also less likely to have received payments from Medicare and among physicians receiving payments the mean amount received was lower for women ($38,409 vs $52,320, p<0.001). Women were equally likely to have graduated from a medical school ranked in the top 20 in terms of research according to U.S. News and World Report (24.9% (821/3,594) vs 26.4% (1,667/6,692), p=0.11).
TABLE 1.
Characteristics of the study population
| All faculty (N = 10,241) |
Male faculty (N = 6,692) |
Female faculty (N=3,549) |
p-value for male-female comparison | |
|---|---|---|---|---|
| Mean Salary, $ (SD) | 240,173 (124,877) | 257,957 (137,202) | 206,641 (88,238) | <0.001 |
| Salary Category, No. (%) | ||||
| < $100,000 | 421 (4.1%) | 277 (4.1%) | 144 (4.1%) | <0.001 |
| $100,000–$149,999 | 1,562 (15.3%) | 799 (11.9%) | 763 (21.5%) | |
| $150,000–$199,999 | 2,567 (25.1%) | 1,448 (21.6%) | 1,119 (31.5%) | |
| $200,000–$249,999 | 2,091 (20.4%) | 1,403 (21.0%) | 688 (19.4%) | |
| $250,000–$299,999 | 1,326 (12.9%) | 951 (14.2%) | 375 (10.6%) | |
| >= $300,000 | 2,274 (22.2%) | 1,814 (27.1%) | 460 (13.0%) | |
| Faculty Rank, No. (%) | ||||
| Assistant Professor | 4,479 (43.7%) | 2,516 (37.6%) | 1,963 (55.3%) | <0.001 |
| Associate Professor | 2,502 (24.4%) | 1,633 (24.4%) | 869 (24.5%) | 0.925 |
| Full Professor | 3,260 (31.8%) | 2,543 (38.0%) | 717 (20.2%) | <0.001 |
| Age, mean years (sd) | 49.49 (10.5) | 51.10 (10.8) | 46.43 (9.2) | <0.001 |
| Age, No. (%) | ||||
| <40 years | 1,999 (20.4%) | 1,065 (16.5%) | 934 (27.8%) | <0.001 |
| 40–44 years | 1,733 (17.7%) | 1,037 (16.1%) | 696 (20.7%) | |
| 45–49 years | 1,559 (15.9%) | 1,007 (15.6%) | 552 (16.4%) | |
| 50–54 years | 1,358 (13.8%) | 897 (13.9%) | 461 (13.7%) | |
| 55–59 years | 1,291 (13.2%) | 916 (14.2%) | 375 (11.1%) | |
| 60–64 years | 955 (9.7%) | 718 (11.1%) | 237 (7.0%) | |
| >= 65 years | 913 (9.3%) | 803 (12.5%) | 110 (3.3%) | |
| Years since residency, mean (sd) | 17.7 (10.9) | 19.4 (11.4) | 14.6 (9.0) | <0.001 |
| Specialty, No. (%) | ||||
| Anesthesiology | 654 (6.4%) | 444 (6.6%) | 210 (5.9%) | 0.158 |
| Cardiology | 369 (3.6%) | 294 (4.4%) | 75 (2.1%) | <0.001 |
| Emergency Medicine | 361 (3.5%) | 261 (3.9%) | 100 (2.8%) | 0.005 |
| Family Medicine | 519 (5.1%) | 277 (4.1%) | 242 (6.8%) | <0.001 |
| Gastroenterology | 228 (2.2%) | 175 (2.6%) | 53 (1.5%) | <0.001 |
| Hematology/Oncology | 419 (4.1%) | 288 (4.3%) | 131 (3.7%) | 0.137 |
| Infectious Disease | 237 (2.3%) | 143 (2.1%) | 94 (2.7%) | 0.101 |
| Internal Medicine | 927 (9.1%) | 527 (7.9%) | 400 (11.3%) | <0.001 |
| Neurology | 449 (4.4%) | 307 (4.6%) | 142 (4.0%) | 0.168 |
| Obstetrics & Gynecology | 418 (4.1%) | 178 (2.7%) | 240 (6.8%) | <0.001 |
| Orthopedic Surgery | 233 (2.3%) | 199 (3.0%) | 34 (1.0%) | <0.001 |
| Other | 1,331 (13.0%) | 868 (13.0%) | 463 (13.1%) | 0.914 |
| Pathology | 440 (4.3%) | 284 (4.2%) | 156 (4.4%) | 0.719 |
| Pediatrics | 1,285 (12.6%) | 661 (9.9%) | 624 (17.6%) | <0.001 |
| Psychiatry | 455 (4.4%) | 294 (4.4%) | 161 (4.5%) | 0.738 |
| Radiology | 573 (5.6%) | 402 (6.0%) | 171 (4.8%) | 0.013 |
| Surgery | 590 (5.8%) | 454 (6.8%) | 136 (3.8%) | <0.001 |
| Surgery subspecialty | 744 (7.3%) | 629 (9.4%) | 115 (3.2%) | <0.001 |
| Publications (total), mean no. (sd) | 21.7 | 26.1 | 13.5 | <0.001 |
| Publications (first or last author), mean no. (sd) | 14.2 | 17.1 | 8.6 | <0.001 |
| NIH Grants | ||||
| At least one grant, No. (%) | 1,488 (14.5%) | 1,076 (16.1%) | 412 (11.6%) | <0.001 |
| Mean, given at least one | 6.09 | 6.70 | 4.48 | <0.001 |
| Clinical Trials | ||||
| At least one trial, No. (%) | 1,060 (10.4%) | 773 (11.6%) | 287 (8.1%) | <0.001 |
| Mean, given at least one | 2.2 | 2.2 | 2.1 | 0.502 |
| Medicare Payments | ||||
| Any payment | 7,366 (71.9%) | 5,017 (75.0%) | 2,349 (66.2%) | <0.001 |
| Mean, given any payment ($) | 47,884 | 52,320 | 38,409 | <0.001 |
| Graduated from a top-20 U.S. medical school | 2,488 (25.9%) | 1,667 (26.4%) | 821 (24.9%) | 0.111 |
| Census Region | ||||
| Midwest | 1,858 (18.1%) | 1,235 (18.5%) | 623 (17.6%) | 0.260 |
| South | 4,552 (44.4%) | 2,986 (44.6%) | 1,566 (44.1%) | 0.631 |
| West | 3,831 (37.4%) | 2,471 (36.9%) | 1,360 (38.3%) | 0.165 |
Notes: Top-20 medical school defined according to U.S. News and World Report 2013 medical school research rankings. Schools were located in three of four Census regions (Midwest, South, and West; none in Northeast). P-values reflect 2-sided t-tests and chi-square comparisons where appropriate. P-value for age reflects comparison of age distributions.
The salary distribution of women was skewed leftward compared to men, with a substantially higher proportion of women receiving lower salaries compared to men (Figure 1). For example, a majority of women (56.4%; 2,026/3,594) earned under $200,000 annually, compared to 37.7% (2,524/6,692) of men. Similarly, 3.2% of women earned above $400,000 annually compared to 11.6% of men.
FIGURE 1.
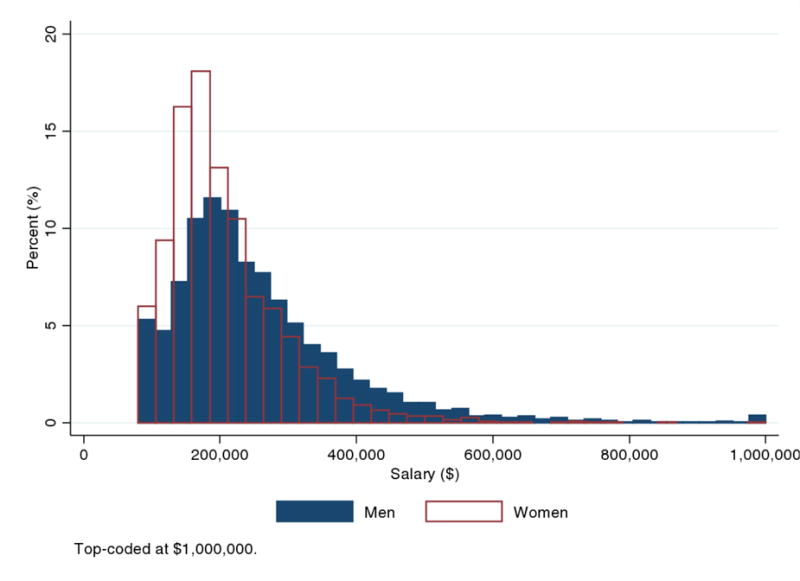
Salary distribution by sex
Multivariable analysis
Adjusting for faculty rank, age, years since residency, specialty, NIH funding, clinical trial participation, publication count (total as well as first/last-authored articles), total Medicare payments, and graduation from a medical school ranked among the top 20 by U.S. News and World Report explained only a portion of the observed salary difference between male and female physicians (adjusted salaries: $227,782 for women vs. $247,661 for men; absolute difference: $19,878; 95% CI: $15,261–$24,495) (Table 2). Approximately 40% of the unadjusted sex difference in salary remained after adjustment ($19,878/$51,315).
TABLE 2.
Multivariable analysis of factors associated with physician salary
| Unadjusted Salary ($) | Adjusted Salary ($) | |||
|---|---|---|---|---|
| Sex | Mean (sd) | Mean | 95% CI | p-value |
| Male | 257,957 (137,203) | 247,661 | (245,065, 250,258) | [Reference] |
| Female | 206,641 (88,239) | 227,783 | (224,117, 231,448) | <0.001 |
| Rank | ||||
| Assistant | 207,913 (93,111) | 217,179 | (212,963, 221,395) | [Reference] |
| Associate | 239,303 (118,221) | 240,422 | (236,001, 244,843) | <0.001 |
| Full | 285,166 (151,344) | 274,614 | (269,414, 279,814) | <0.001 |
| Age, years | ||||
| <40 years | 207,147 (95,621) | 241,430 | (233,753, 249,107) | [Reference] |
| 40–44 years | 225,572 (108,927) | 245,500 | (239,193, 251,807) | 0.263 |
| 45–49 years | 246,958 (127,610) | 250,330 | (244,743, 255,918) | 0.042 |
| 50–54 years | 261,280 (138,644) | 249,234 | (243,453, 255,016) | 0.139 |
| 55–59 years | 259,157 (126,502) | 238,158 | (231,298, 245,018) | 0.602 |
| 60–64 years | 263,973 (137,492) | 236,456 | (227,199, 245,713) | 0.513 |
| >= 65 years | 258,165 (151,665) | 210,663 | (198,095, 223,231) | 0.001 |
| Specialty | ||||
| Anesthesiology | 271,883 (96,541) | 286,337 | (277,879, 294,796) | [Reference] |
| Cardiology | 276,151 (128,230) | 254,188 | (243,251, 265,124) | <0.001 |
| Emergency Medicine | 229,182 (63,082) | 235,975 | (224,995, 246,955) | <0.001 |
| Family Medicine | 171,270 (56,815) | 191,341 | (181,807, 200,876) | <0.001 |
| Gastroenterology | 265,024 (129,705) | 258,690 | (244,709, 272,670) | 0.001 |
| Hematology/Oncology | 265,921 (148,804) | 244,404 | (233,968, 254,840) | <0.001 |
| Infectious Disease | 181,743 (68,994) | 190,184 | (176,325, 204,044) | <0.001 |
| Internal Medicine | 198,687 (73,413) | 202,332 | (195,421, 209,243) | <0.001 |
| Neurology | 197,991 (96,739) | 192,674 | (182,812, 202,537) | <0.001 |
| Obstetrics & Gynecology | 259,635 (121,156) | 273,507 | (263,536, 283,477) | 0.054 |
| Orthopedic Surgery | 355,704 (162,508) | 358,093 | (344,354, 371,831) | <0.001 |
| Other | 225,200 (115,126) | 214,406 | (208,521, 220,290) | <0.001 |
| Pathology | 214,248 (96,759) | 212,111 | (202,052, 222,170) | <0.001 |
| Pediatrics | 191,576 (78,601) | 210,939 | (205,041, 216,837) | <0.001 |
| Psychiatry | 198,777 (73,897) | 206,568 | (196,799, 216,337) | <0.001 |
| Radiology | 290,402 (107,125) | 282,368 | (273,058, 291,678) | 0.535 |
| Surgery | 310,895 (171,207) | 302,666 | (294,060, 311,272) | 0.008 |
| Surgery subspecialty | 330,992 (191,272) | 318,760 | (311,030, 326,491) | <0.001 |
| NIH Grant | ||||
| None | 238,853 (123,028) | 243,071 | (240,763, 245,378) | [Reference] |
| At Least 1 | 247,944 (135,029) | 227,667 | (221,160, 234,175) | <0.001 |
| Clinical Trial | ||||
| None | 235,461 (121,243) | 239,356 | (237,159, 241,554) | [Reference] |
| At Least 1 | 280,994 (146,639) | 253,501 | (246,631, 260,371) | <0.001 |
| Years since residency (ref. increment, 1 yr) | 1764.5 | 559 | (18.2,1,100.0) | 0.043 |
| Publications, total (ref. increment, 1 pub.) | 784.7 | 409 | (298.7,518.3) | <0.001 |
| Publications, first or last author (ref. increment, 1 pub.) | 683.2 | −79 | (−196.6,38.9) | 0.189 |
| Medicare payment (ref. increment, 1 dollar) | 0.3 | 0.3 | (0.3,0.3) | <0.001 |
| Graduated from a top-20 U.S. medical school | ||||
| No | 237,264 (121,460) | 239,799 | (237,338, 242,260) | [Reference] |
| Yes | 252,643 (135,563) | 243,768 | (239,465, 248,072) | 0.129 |
Notes: Estimates are from a multivariable linear regression of salary as a function of age, years of experience, sex, NIH funding, publication count (total as well first or last authored publications), clinical trial participation, Medicare payments, and medical school fixed effects. Medicare payments reflect the amount a physician was reimbursed by Medicare in 2013, as reported in publicly available data published by the Centers for Medicare and Medicaid Services. This figure was used as a proxy for clinical revenue and full- versus part-time effort, which may influence a physician’s salary.
Average adjusted salary was higher among full professors ($274,614) than associate ($240,421) and assistant professors ($217,178), p<0.001 for both comparisons). While salary rose with age in unadjusted analysis, this relationship disappeared after multivariable adjustment (and income was lower among those above age 65 years compared to all other groups, p<0.001). Among specialties, adjusted salaries were highest in orthopedic surgery ($358,092; 95% CI $344,354–$371,830), surgical subspecialties ($318,760; 95% CI $311,029–$326,491), and general surgery ($302,665; 95% CI $294,059–$311,271), and lowest in infectious disease, family medicine, and neurology (average income < $200,000). Years of experience, total publications, clinical trial participation, and Medicare payments were positively associated with salary.
Sex differences in salary according to specialty and faculty rank
There was substantial heterogeneity across specialties in the size of sex differences in salary (Table 3). In all specialties but radiology, the estimated adjusted salary among men exceeded women, although this difference was statistically significantly in 9 of 18 specialties. Surgical specialties demonstrated the largest absolute adjusted sex differences in salary ($329,097 vs $285,369, absolute difference $43,728, 95% CI $22,272–$65,184), orthopedic surgery ($368,070 vs $327,117, absolute difference $40,942, 95% CI $2,277–$79,628), hematology/oncology ($256,959 vs $219,166, absolute difference $37,792, 95% CI $16,030–$59,556), obstetrics/gynecology ($289,777 vs $253,387, absolute difference $36,390, 95% CI $16,375–$56,406), and cardiology ($263,690 vs $229,940, absolute difference $33,749, 95% CI $6,479–$61,020).
TABLE 3.
Sex differences in salary by specialty
| Unadjusted Salary ($) | Adjusted Salary ($) | |||||
|---|---|---|---|---|---|---|
| Specialty | Males | Females | Difference | Males | Females | Difference (95% CI) |
| Anesthesiology (N=654) | 278,931 | 256,981 | 21,950 | 291,617 | 276,684 | 14,933 (−2,822, 32,688) |
| Cardiology (N=369) | 284,378 | 243,904 | 40,474 | 263,690 | 229,940 | 33,749 (6,479, 61,020) |
| Emergency Medicine (N=361) | 234,997 | 214,007 | 20,990 | 239,257 | 232,534 | 6,723 (−17,907, 31,353) |
| Family Medicine (N=519) | 179,080 | 162,330 | 16,750 | 191,879 | 185,635 | 6,244 (−12,529, 25,017) |
| Gastroenterology (N=228) | 273,915 | 235,666 | 38,249 | 263,838 | 251,130 | 12,709 (−20,499, 45,916) |
| Hematology/Oncology (N=419) | 282,705 | 229,021 | 53,684 | 256,959 | 219,166 | 37,793 (16,030, 59,556) |
| Infectious Disease (N=237) | 192,077 | 166,023 | 26,054 | 196,449 | 177,886 | 18,563 (−9,889, 47,016) |
| Internal Medicine (N=927) | 210,062 | 183,700 | 26,362 | 207,497 | 191,338 | 16,159 (2,256, 30,061) |
| Neurology (N=449) | 210,705 | 170,504 | 40,201 | 202,832 | 172,351 | 30,482 (9,371, 51,592) |
| Obstetrics & Gynecology (N=418) | 290,183 | 236,978 | 53,205 | 289,777 | 253,387 | 36,390 (16,375, 56,406) |
| Orthopedic Surgery (N=233) | 363,847 | 308,045 | 55,802 | 368,070 | 327,117 | 40,953 (2,277, 79,628) |
| Other (N=1331) | 237,452 | 202,230 | 35,222 | 217,786 | 207,800 | 9,985 (−2,262, 22,233) |
| Pathology (N=440) | 223,214 | 197,924 | 25,290 | 216,592 | 203,614 | 12,977 (−7,812, 33,767) |
| Pediatrics (N=1285) | 210,366 | 171,671 | 38,695 | 220,009 | 195,457 | 24,553 (13,058, 36,047) |
| Psychiatry (N=455) | 211,892 | 174,826 | 37,066 | 211,709 | 196,909 | 14,799 (−5,709, 35,308) |
| Radiology (N=573) | 290,660 | 289,797 | 863 | 282,749 | 285,127 | −2,378 (−22,631, 17,875) |
| Surgery (N=590) | 323,149 | 269,990 | 53,159 | 312,411 | 280,030 | 32,381 (12,253, 52,509) |
| Surgery Subspecialty (N=744) | 342,810 | 266,353 | 76,457 | 329,097 | 285,369 | 43,728 (22,272, 65,184) |
Notes: Specialty-specific sex differences in salary were estimated using a multivariable linear regression of salary as a function of age, years of experience, sex (interacted with specialty), NIH funding, publication count (total as well first or last authored publications), clinical trial participation, Medicare payments, and medical school fixed effects.
Sex differences in salary were present at all faculty ranks and were largest among full professors (male-female difference among assistant professors $13,240, 95% CI 6,884–19,596; associate, $20,329, 95% CI $11,381–$29,276; full, $33,620, 95% CI $24,439–$42,801; eFigure 1). Of note, adjusted salaries of female associate professors ($226,884; 95% CI $219,504–$234,264) were comparable to those of male assistant professors ($221,046; 95% CI $216,098–$225,995). Moreover, adjusted salaries of female full professors ($250,971; 95% CI $242,307–$259,635) were comparable to those of male associate professors ($247,212; 95% CI $241,850–$252,575).
Sex differences in salary by medical school and Census region
Adjusted salaries of male physicians were significantly higher than salaries of female physicians in 9/24 (37.5%) schools, although point estimates were higher in 17/24 (70.1%) schools (Figure 2). The two schools with the largest male-female earnings gap had absolute adjusted sex differences in salary of $54,174 (95% CI $38,901–$69,446) and $59,338 (95% CI $29,572–$89,104). In contrast, female physicians had significantly higher adjusted salaries than male physicians at 2 schools. Female physicians had lower adjusted salaries than male physicians in all three Census regions in which schools were located, with the largest sex differences observed in schools in the West (e.g., adjusted sex difference $33,042 in the West vs $16,044 in the South and $4,541 in the Midwest; p<0.001 for difference between West vs South and for West vs Midwest) (eTable 1).
FIGURE 2. Sex differences in salary according to medical school.
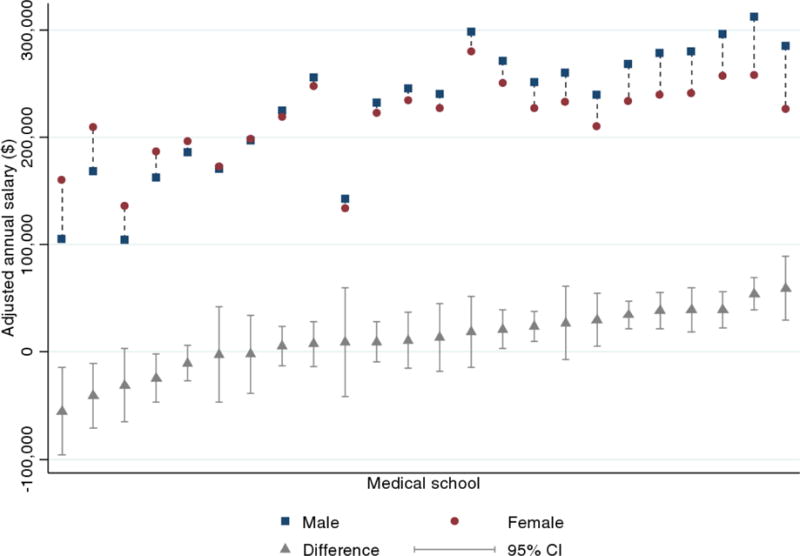
Notes: School-specific sex differences in salary were estimated using a multivariable linear regression of salary as a function of age, years of experience, sex (interacted with school), NIH funding, publication count (total as well first or last authored publications), clinical trial participation, and Medicare payments.
Additional analyses
Adjusted sex differences in salary were present among physicians self-registered with Doximity ($255,825 vs $233,843; difference $21,982; 95% CI $15,073–$28,890); among physicians with NIH funding ($268,165 vs $245,666; difference $22,499; 95% CI $9,465–$35,533); among physicians in the upper three-quartiles of earnings within each school and institution, an analysis conducted to increase the likelihood that our sample included physicians who were full time effort; and in analyses of earnings models that included years since residency as a categorical variable or models that included counts of NIH grants and clinical trials as opposed to binary indicators for each (eTable 1).
DISCUSSION
We analyzed sex differences in salary between male and female academic physicians at 24 U.S. public medical schools using contemporary administrative salary data of state employees made publicly available online by state governments. After adjusting these analyses for physician age, years of experience, specialty, faculty rank, several measures of research productivity, and payments by Medicare—information obtained from a comprehensive database of U.S. physicians—we found that annual salaries of female academic physicians were approximately 8% (or nearly $20,000) lower than male physicians. This difference represents approximately 40% of the unadjusted difference in salary between men and women. The magnitude of sex differences in adjusted salary varied across specialties and institutions. Sex differences in salary were present at all faculty ranks. In fact, female full and associate professors had comparable adjusted salaries to those of male associate and assistant professors, respectively. By relying on administrative salary data and a rich set of physician characteristics, we were able to analyze a substantially larger population of academic physicians than has previously been possible with survey data, making this the largest study of sex differences in earnings among academic physicians to date.
Several studies have documented persistent sex differences in faculty rank at U.S. medical schools,3–11 including a recent analysis using the same physician databased utilized for this analysis.12 However, fewer studies have investigated sex differences in salary among academic physicians.17–22 Two relatively recent national surveys found that female academic physician researchers earn less than males after adjustment for demographics, experience, specialty, work hours, research productivity and faculty rank, but these studies were survey-based, smaller in size than the current study, and focused on investigators with specific forms of early career investigator funding by the NIH.17,18
Our study has several implications. First, sizeable differences in salary between male and female physicians in public medical schools persist after accounting for a rich set of factors that influence salary. A number of explanations have been put forth to explain sex differences in salary and academic advancement more generally.6,7,24–29 One set of explanations focuses on factors that may lead to lower research and clinical productivity among women, which would result in unadjusted income differences. Such factors include differential household responsibilities,30–32 childrearing, greater difficulty finding effective mentors,24–26,33 inequitable allocation of institutional research funding and work space,15,17,18,34 and different preferences on work-life balance35,36 although evidence on the latter is mixed.37,38 Another set of explanations focuses on factors that may explain sex differences in salary even among men and women who are similarly productive in research and clinical work. Such factors include several of those above, as well as women physicians being less likely to receive recognition for achievements,24–26,33 overt discrimination, and the possibility that women physicians may place less emphasis on salary negotiations compared to male counterparts in both initial and subsequent salary negotiations.39
Although a number of strategies have been proposed to address the issue of sex differences in academic physicians salary,40 a second implication of our study is that publicly available administrative salary data potentially allow for public transparency to facilitate efforts to understand, and even close, the male-female physician salary gap. Specifically, publicly available salary information may compel institutions or specific departments within institutions to serially assess progress towards reducing sex differences in salary. Relatedly, our linkage of administrative salary data to a broad range of clinical and research productivity measures of individual physicians that can be updated frequently and in automated manner implies that sex differences in salary may be continually evaluated by departments and institutions.
A third implication of our study is that we found that sex differences in salary varied considerably across specialties and institutions. Specialties such as orthopedic surgery, surgical subspecialties, obstetrics and gynecology, and cardiology had the largest absolute sex differences in salary, whereas radiology, family medicine, and emergency medicine had sex differences in salary that were small in magnitude and not statistically significant. In another study, which used the same database of physician characteristics as the present study, radiology had among the smallest sex differences in full professorship of all specialties,12 which suggests the potential importance of studying specific specialties to understand practices associated with improved male-female equity in academic medicine. Similarly, the variation in sex differences in salary across institutions underscores both the importance of institutional accountability and the potential role for inter-institutional initiatives to learn about practices that promote or undermine sex equity in physician compensation. Finally, because our findings were among physicians who are state employees of public medical schools, interest in reducing sex differences in salary should lie not only at the school-level but at the state-level as well.
A potential concern with our study was that we lacked information on faculty track or part-time status, which could confound sex differences in salary if women are more likely to enter lower paying tracks or work part-time. Nonetheless, we adjusted for total Medicare payments, which should correlate with clinical volume after adjusting for clinical specialty and institution-specific fixed effects (which would adjust for inter-institutional variations in insurance case-mix and reimbursement patterns). Sex differences in clinical revenue are arguably as important to account for as information on full- or part-time effort, given that physicians with similar effort may differ in clinical revenue due to differences in billing practices, volume, and procedural mix. Importantly, however, our use of Medicare reimbursements as a proxy for clinical revenue and effort would not apply well to fields such as pediatrics or obstetrics.
In addition to the specific issue of sex differences in part-time status, it is possible that women and men may differ in their likelihood of being in research versus clinical tracks. To address the issue that women may be less likely to enter research tracks, which correlate with more rapid promotion and possibly higher salary,12,23 we demonstrated persistent sex differences in salary among faculty who were NIH-funded investigators and therefore more likely to be on research tracks and unlikely to be part-time. Finally, although part-time status is frequently endorsed as a reason why female academic physicians have lower earnings and slower academic advancement than male physicians, part-time status arguably mediates much of its effect through decreased research productivity and clinical volume. Once these factors are accounted for, however, it remains unclear how large an independent residual effect part-time status should have on sex differences in earnings. Nonetheless, we cannot exclude the possibility of part-time status as an unmeasured confounder.
Our study had several additional limitations. First, it is possible that reported incomes in some schools or states may exclude other payments to physicians (e.g., incentive payments, grant income, clinical income from non-state sources, etc.) and therefore not reflect the full salary physicians receive. The extent to which this issue varies across schools and departments within schools is unknown. However, to reduce our estimated sex differences in earnings, these payments would have to be higher among women than men, which seems unlikely. Moreover, Medicare reimbursements, which we argue are a proxy for clinical revenue, were approximately $14,000 higher among men than women, suggesting that any incentive payments to physicians that are correlated with clinical revenue are unlikely to be higher among women than men. Therefore, our estimated sex differences in income are likely lower bounds of true salary differences. Second, we examined only public medical schools due to availability of salary data. It is possible that observed sex differences in salary may not generalize to private institutions. Nonetheless, the schools we considered had wide geographic representation and the proportion of male physician faculty at these schools was similar to that of all remaining U.S. medical schools. Third, while we took several steps to validate the accuracy of our physician-salary matches, matching errors may occasionally have occurred. However, to influence our findings, these errors would need to be correlated with physician sex, which is unlikely given that the proportion of male physician faculty in our sample mirrored the proportion of male physician faculty in U.S. medical schools overall. Fourth, our database of physician characteristics was externally developed, and data on publications, NIH funding, and clinical trial investigation was gathered through links to other databases. While we previously audited a randomly selected subset of the database to verify its accuracy,12 we cannot exclude the possibility that it contains errors. Nonetheless, to meaningfully impact the outcomes of this analysis, any errors in the primary dataset would have to correlate with physician sex. Moreover, our sensitivity analyses confirmed persistent sex differences in salary among registered Doximity members, who presumably verified their profile information. Fifth, our database lacked information on physician race and ethnicity which may influence earnings as well. Sixth, we lacked data on sub-specialty training (e.g., interventional cardiology and electrophysiology within the field of cardiology), which may confound our analysis. Notably, however, our adjustment for Medicare reimbursements would arguably capture differences in income stemming from procedural case-mix differences across specialties. Seventh, we lacked data on other graduate degrees which may influence salary (e.g., PhDs), although we would expect much of this effect to be mediated through our research productivity measures. Finally, despite extensive efforts to control for potential confounders, our results, like those of all observational studies, could be influenced by unmeasured variables (e.g., sex differences in administrative or leadership positions, teaching, committee service, etc.).
Conclusions
Among academic physicians in 24 U.S. public medical schools, annual salaries of female physicians were substantially lower than male physicians after adjustment for a rich set of factors that influence salary. Nearly 40% of the unadjusted difference in average salaries between men and women remained unexplained after adjustment for these potential confounders. Our use of publicly available state employee salary data highlights the importance of physician salary transparency to efforts to reduce the male-female earnings gap.
Supplementary Material
Acknowledgments
The authors report funding from the Office of the Director, National Institutes of Health (Dr. Jena, NIH Early Independence Award, Grant 1DP5OD017897-01). The funder had no involvement in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. Dr. Jena had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Conflicts of interest: The authors have no conflicts of interest to report.
References
- 1.AAMC. U.S. Medical School Applicants and Students 1982–1983 to 2011–2012. 2012 ( https://www.aamc.org/download/153708/data/).
- 2.Lautenberger DM, Dandar VM, Raezer CL, Sloane RA. The State of Women in Academic Medicine: The Pipeline and Pathways to Leadership. Association of American Medical Colleges; 2014. [Google Scholar]
- 3.Women in U.S. Academic Medicine and Science: Statistics and Benchmarking Report 2011–2012. 2012 (Accessed at https://www.aamc.org/download/415556/data/2011-2012wimsstatsreport.pdf.)
- 4.Nickerson KG, Bennett NM, Estes D, Shea S. The status of women at one academic medical center. Breaking through the glass ceiling. Jama. 1990;264:1813–7. [PubMed] [Google Scholar]
- 5.Kaplan SH, Sullivan LM, Dukes KA, Phillips CF, Kelch RP, Schaller JG. Sex differences in academic advancement. Results of a national study of pediatricians. N Engl J Med. 1996;335:1282–9. doi: 10.1056/NEJM199610243351706. [DOI] [PubMed] [Google Scholar]
- 6.Nonnemaker L. Women physicians in academic medicine: new insights from cohort studies. N Engl J Med. 2000;342:399–405. doi: 10.1056/NEJM200002103420606. [DOI] [PubMed] [Google Scholar]
- 7.Tesch BJ, Wood HM, Helwig AL, Nattinger AB. Promotion of women physicians in academic medicine. Glass ceiling or sticky floor? Jama. 1995;273:1022–5. [PubMed] [Google Scholar]
- 8.Wallis LA, Gilder H, Thaler H. Advancement of men and women in medical academia. A pilot study. Jama. 1981;246:2350–3. [PubMed] [Google Scholar]
- 9.Carr PL, Friedman RH, Moskowitz MA, Kazis LE. Comparing the status of women and men in academic medicine. Ann Intern Med. 1993;119:908–13. doi: 10.7326/0003-4819-119-9-199311010-00008. [DOI] [PubMed] [Google Scholar]
- 10.Eloy JA, Svider PF, Cherla DV, et al. Gender disparities in research productivity among 9952 academic physicians. Laryngoscope. 2013;123:1865–75. doi: 10.1002/lary.24039. [DOI] [PubMed] [Google Scholar]
- 11.Reed DA, Enders F, Lindor R, McClees M, Lindor KD. Gender differences in academic productivity and leadership appointments of physicians throughout academic careers. Acad Med. 2011;86:43–7. doi: 10.1097/ACM.0b013e3181ff9ff2. [DOI] [PubMed] [Google Scholar]
- 12.Jena AB, Khullar D, Ho O, Olenski AR, Blumenthal DM. Sex Differences in Academic Rank in US Medical Schools in 2014. Jama. 2015;314:1149–58. doi: 10.1001/jama.2015.10680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baker LC. Differences in earnings between male and female physicians. N Engl J Med. 1996;334:960–4. doi: 10.1056/NEJM199604113341506. [DOI] [PubMed] [Google Scholar]
- 14.Lo Sasso AT, Richards MR, Chou CF, Gerber SE. The $16,819 pay gap for newly trained physicians: the unexplained trend of men earning more than women. Health Aff (Millwood) 2011;30:193–201. doi: 10.1377/hlthaff.2010.0597. [DOI] [PubMed] [Google Scholar]
- 15.Seabury SA, Chandra A, Jena AB. Trends in the earnings of male and female health care professionals in the United States, 1987 to 2010. JAMA Intern Med. 2013;173:1748–50. doi: 10.1001/jamainternmed.2013.8519. [DOI] [PubMed] [Google Scholar]
- 16.Hoff TJ. Doing the same and earning less: male and female physicians in a new medical specialty. Inquiry. 2004;41:301–15. [PubMed] [Google Scholar]
- 17.Jagsi R, Griffith KA, Stewart A, Sambuco D, DeCastro R, Ubel PA. Gender differences in the salaries of physician researchers. Jama. 2012;307:2410–7. doi: 10.1001/jama.2012.6183. [DOI] [PubMed] [Google Scholar]
- 18.Jagsi R, Griffith KA, Stewart A, Sambuco D, DeCastro R, Ubel PA. Gender differences in salary in a recent cohort of early-career physician-researchers. Acad Med. 2013;88:1689–99. doi: 10.1097/ACM.0b013e3182a71519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ash AS, Carr PL, Goldstein R, Friedman RH. Compensation and advancement of women in academic medicine: is there equity? Ann Intern Med. 2004;141:205–12. doi: 10.7326/0003-4819-141-3-200408030-00009. [DOI] [PubMed] [Google Scholar]
- 20.Weeks WB, Wallace TA, Wallace AE. How do race and sex affect the earnings of primary care physicians? Health Aff (Millwood) 2009;28:557–66. doi: 10.1377/hlthaff.28.2.557. [DOI] [PubMed] [Google Scholar]
- 21.Ness RB, Ukoli F, Hunt S, et al. Salary equity among male and female internists in Pennsylvania. Ann Intern Med. 2000;133:104–10. doi: 10.7326/0003-4819-133-2-200007180-00009. [DOI] [PubMed] [Google Scholar]
- 22.DesRoches CM, Zinner DE, Rao SR, Iezzoni LI, Campbell EG. Activities, productivity, and compensation of men and women in the life sciences. Acad Med. 2010;85:631–9. doi: 10.1097/ACM.0b013e3181d2b095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thomas PA, Diener-West M, Canto MI, Martin DR, Post WS, Streiff MB. Results of an academic promotion and career path survey of faculty at the Johns Hopkins University School of Medicine. Acad Med. 2004;79:258–64. doi: 10.1097/00001888-200403000-00013. [DOI] [PubMed] [Google Scholar]
- 24.Hamel MB, Ingelfinger JR, Phimister E, Solomon CG. Women in academic medicine–progress and challenges. N Engl J Med. 2006;355:310–2. doi: 10.1056/NEJMe068143. [DOI] [PubMed] [Google Scholar]
- 25.Kaplan SH, Sullivan LM, Dukes KA, Phillips CF, Kelch RP, Schaller JG. Sex differences in academic advancement. Results of a national study of pediatricians. The New England journal of medicine. 1996;335:1282–9. doi: 10.1056/NEJM199610243351706. [DOI] [PubMed] [Google Scholar]
- 26.Fried LP, Francomano CA, MacDonald SM, et al. Career development for women in academic medicine: Multiple interventions in a department of medicine. Jama. 1996;276:898–905. [PubMed] [Google Scholar]
- 27.Carr PL, Ash AS, Friedman RH, et al. Relation of family responsibilities and gender to the productivity and career satisfaction of medical faculty. Annals of internal medicine. 1998;129:532–8. doi: 10.7326/0003-4819-129-7-199810010-00004. [DOI] [PubMed] [Google Scholar]
- 28.Nattinger AB. Promoting the career development of women in academic medicine. Arch Intern Med. 2007;167:323–4. doi: 10.1001/archinte.167.4.323. [DOI] [PubMed] [Google Scholar]
- 29.Holliday EB, Jagsi R, Wilson LD, Choi M, Thomas CR, Jr, Fuller CD. Gender differences in publication productivity, academic position, career duration, and funding among U.S. academic radiation oncology faculty. Acad Med. 2014;89:767–73. doi: 10.1097/ACM.0000000000000229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carr P, Friedman RH, Moskowitz MA, Kazis LE, Weed HG. Research, academic rank, and compensation of women and men faculty in academic general internal medicine. J Gen Intern Med. 1992;7:418–23. doi: 10.1007/BF02599159. [DOI] [PubMed] [Google Scholar]
- 31.Carr PL, Ash AS, Friedman RH, et al. Relation of family responsibilities and gender to the productivity and career satisfaction of medical faculty. Ann Intern Med. 1998;129:532–8. doi: 10.7326/0003-4819-129-7-199810010-00004. [DOI] [PubMed] [Google Scholar]
- 32.Jolly S, Griffith KA, DeCastro R, Stewart A, Ubel P, Jagsi R. Gender differences in time spent on parenting and domestic responsibilities by high-achieving young physician-researchers. Ann Intern Med. 2014;160:344–53. doi: 10.7326/M13-0974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yedidia MJ, Bickel J. Why aren’t there more women leaders in academic medicine? the views of clinical department chairs. Acad Med. 2001;76:453–65. doi: 10.1097/00001888-200105000-00017. [DOI] [PubMed] [Google Scholar]
- 34.Holliday E, Griffith KA, De Castro R, Stewart A, Ubel P, Jagsi R. Gender Differences in Resources and Negotiation Among Highly Motivated Physician-Scientists. J Gen Intern Med. 2014 doi: 10.1007/s11606-014-2988-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dorsey ER, Jarjoura D, Rutecki GW. Influence of controllable lifestyle on recent trends in specialty choice by US medical students. Jama. 2003;290:1173–8. doi: 10.1001/jama.290.9.1173. [DOI] [PubMed] [Google Scholar]
- 36.Bland KI, Isaacs G. Contemporary trends in student selection of medical specialties: the potential impact on general surgery. Archives of surgery. 2002;137:259–67. doi: 10.1001/archsurg.137.3.259. [DOI] [PubMed] [Google Scholar]
- 37.Dorsey ER, Jarjoura D, Rutecki GW. The influence of controllable lifestyle and sex on the specialty choices of graduating U.S. medical students, 1996–2003. Acad Med. 2005;80:791–6. doi: 10.1097/00001888-200509000-00002. [DOI] [PubMed] [Google Scholar]
- 38.Lambert EM, Holmboe ES. The relationship between specialty choice and gender of U.S. medical students, 1990–2003. Acad Med. 2005;80:797–802. doi: 10.1097/00001888-200509000-00003. [DOI] [PubMed] [Google Scholar]
- 39.Sarfaty S, Kolb D, Barnett R, et al. Negotiation in academic medicine: a necessary career skill. Journal of women’s health. 2007;16:235–44. doi: 10.1089/jwh.2006.0037. [DOI] [PubMed] [Google Scholar]
- 40.Byington CL, Lee V. Addressing Disparities in Academic Medicine: Moving Forward. Jama. 2015;314:1139–41. doi: 10.1001/jama.2015.10664. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


