Abstract
IMPORTANCE
Studies have found differences in practice patterns between male and female physicians, with female physicians more likely to adhere to clinical guidelines and evidence-based practice. However, whether patient outcomes differ between male and female physicians is largely unknown.
OBJECTIVE
To determine whether mortality and readmission rates differ between patients treated by male or female physicians.
DESIGN, SETTING, AND PARTICIPANTS
We analyzed a 20% random sample of Medicare fee-for-service beneficiaries 65 years or older hospitalized with a medical condition and treated by general internists from January 1, 2011, to December 31, 2014. We examined the association between physician sex and 30-day mortality and readmission rates, adjusted for patient and physician characteristics and hospital fixed effects (effectively comparing female and male physicians within the same hospital). As a sensitivity analysis, we examined only physicians focusing on hospital care (hospitalists), among whom patients are plausibly quasi-randomized to physicians based on the physician’s specific work schedules. We also investigated whether differences in patient outcomes varied by specific condition or by underlying severity of illness.
MAIN OUTCOMES AND MEASURES
Patients’ 30-day mortality and readmission rates.
RESULTS
A total of 1 583 028 hospitalizations were used for analyses of 30-day mortality (mean [SD] patient age, 80.2 [8.5] years; 621 412 men and 961 616 women) and 1 540 797 were used for analyses of readmission (mean [SD] patient age, 80.1 [8.5] years; 602 115 men and 938 682 women). Patients treated by female physicians had lower 30-day mortality (adjusted mortality, 11.07% vs 11.49%; adjusted risk difference, −0.43%; 95% CI, −0.57% to −0.28%; P < .001; number needed to treat to prevent 1 death, 233) and lower 30-day readmissions (adjusted readmissions, 15.02% vs 15.57%; adjusted risk difference, −0.55%; 95% CI, −0.71% to −0.39%; P < .001; number needed to treat to prevent 1 readmission, 182) than patients cared for by male physicians, after accounting for potential confounders. Our findings were unaffected when restricting analyses to patients treated by hospitalists. Differences persisted across 8 common medical conditions and across patients’ severity of illness.
CONCLUSIONS AND RELEVANCE
Elderly hospitalized patients treated by female internists have lower mortality and readmissions compared with those cared for by male internists. These findings suggest that the differences in practice patterns between male and female physicians, as suggested in previous studies, may have important clinical implications for patient outcomes.
There is evidence that men and women may practice medicine differently. Literature has shown that female physicians may be more likely to adhere to clinical guidelines,1–3 provide preventive care more often,4–11 use more patient-centered communication,12–15 perform as well or better on standardized examinations,16 and provide more psychosocial counseling to their patients than do their male peers.14 Although studies suggest differences in practice patterns and process measures of quality between male and female physicians, these studies have not examined patient outcomes, what we arguably care about the most. In fact, whether patient outcomes differ between male and female physicians is largely unknown.
Female physicians now account for approximately one-third of the US physician workforce17 and comprise half of all US medical school graduates.18 Despite evidence suggesting that female physicians may provide higher-quality care,1–4,7,8,10,12–16 some have argued that career interruptions for childrearing, higher rates of part-time employment, and greater tradeoffs between home and work responsibilities19 may compromise the quality of care provided by female physicians and justify higher salaries among male physicians.20–22 Therefore, empirical evidence on whether patient outcomes differ between male and female physicians is warranted.
In this context, using a national sample of Medicare beneficiaries hospitalized with medical conditions, we sought to investigate 3 key questions. First, are there important differences in clinical outcomes for hospitalized patients cared for by female internists compared with those treated by male internists? Second, does the influence of physician sex on patient outcomes differ across a variety of conditions for which patients are commonly hospitalized? Finally, do these differences in outcomes vary with the underlying severity of a patient’s illness?
Methods
This study was approved by the Harvard Medical School Institutional Review Board and patient consent was not required.
Data Source
We analyzed a 20% sample of the Medicare Inpatient and Carrier Files to identify Medicare fee-for-service beneficiaries 65 years or older who were hospitalized in acute care hospitals from January 1, 2011, through December 31, 2014. Our study population was restricted to patients who were hospitalized owing to medical conditions as defined by the presence of a medical diagnosis-related group (Medicare Severity Diagnosis Related Group). To allow for sufficient follow-up, patients admitted in December 2014 were excluded from the analyses of 30-day mortality. Patients discharged in December 2014 and patients who were out of the hospital for fewer than 30 days at the time of admission were excluded from the analyses of 30-day readmission. Patients who were transferred between acute care hospitals had their hospital stays combined into a single episode of care, with the patient outcome attributed to the first hospitalization.23,24 We restricted our sample to non-elective hospitalizations. We also excluded patients who left against medical advice.
We assigned each hospitalization to a physician based on the National Provider Identifier in the Carrier File that accounted for the largest amount of Medicare Part B spending during that hospitalization.25 Part B spending comprises professional and other fees determined by the physician. On average, these physicians were responsible for 51.1% of total Part B spending for a given hospitalization. We restricted our analyses to hospitalizations for which the physicians with the highest amount of Part B spending were general internists to avoid comparing physicians across different specialties. Physician data, including physician age, were obtained by linking the Medicare data with a comprehensive database of US physicians assembled by a company that provides online networking services for US physicians (Doximity; https://www.doximity.com/) through data partnerships, including the American Board of Medical Specialties, state licensing boards, and collaborating hospitals and medical schools.26,27
Adjustment Variables
We accounted for patient characteristics, physician characteristics, and hospital fixed effects. Patient characteristics included patient age in 5-year increments (the oldest group was categorized as ≥95 years), sex, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, and other), primary diagnosis (Medicare Severity Diagnosis Related Group), 27 coexisting conditions (determined using the Elixhauser comorbidity index28), median annual household income estimated from residential zip codes (in deciles), an indicator variable for Medicaid coverage, and indicator variables for year. Physician characteristics included physician age in 5-year increments (the oldest group was categorized as ≥70 years), indicator variables for the medical schools from which the physicians graduated, and type of medical training (ie, allopathic vs osteopathic29 training).
Statistical Analysis
We first examined the association between physician sex and 30-day mortality (whether patients died within 30 days of the admission date) and 30-day readmissions (whether patients were readmitted within 30 days of the discharge date) by using 3 regression models. Model 1 compared patient outcomes (mortality and readmissions) between male and female physicians, adjusting for patient characteristics. Model 2 adjusted for all variables in model 1 plus hospital fixed effects (ie, hospital indicators), effectively comparing male and female physicians within the same hospital.30 Model 3 adjusted for all variables in model 2 plus physician characteristics, to evaluate if the differences in patient outcomes between male and female physicians could be explained by other physician characteristics that are correlated with physician sex. We used a multivariable linear probability model30,31 (ie, fitting ordinary least-squares to binary outcomes) as our primary model for computational efficiency and because there were problems with complete or quasi-complete separation in logistic regression models. To account for potential correlation between patient outcomes within the same physician, SEs were clustered at the physician level. After fitting regression models, we calculated adjusted patient outcomes using the marginal standardization form of predictive margins.32
Next, we assessed whether differences in patient outcomes between male and female physicians differed according to the primary condition for which a patient was admitted. We evaluated the 8 most common medical conditions treated by general internists, according to the Medicare data: sepsis, pneumonia, congestive heart failure, chronic obstructive pulmonary disease, urinary tract infection, acute renal failure, arrhythmia, and gastrointestinal bleeding. A list of International Classification of Diseases, 9th Revision, codes is available in eTable 1 in the Supplement.33
Finally, we assessed whether differences in outcomes between male and female physicians varied according to illness severity. We used a logistic regression model with 30-day mortality as an outcome, and the patient-level adjustment variables listed above as explanatory variables to determine each patient’s likelihood of death. Within each quintile of expected mortality, we then examined patient outcomes between male and female physicians, adjusting for patient and physician characteristics and hospital fixed effects.
Analysis of Potential Mechanisms
We explored potential mechanisms for observed differences between male and female physicians, including differences in length of stay, use of care, patient volume (number of hospitalized Medicare patients each physician treated annually), and discharge location of patients (home, skilled nursing facility, rehabilitation facility, hospice, or other). Use of care was measured by total Part B spending per hospitalization. Length of stay and use of care were used as continuous variables with quadratic and cubic terms, and patient volume was categorized into deciles. In addition, to address the possibility that physicians’ age may not fully account for the differences in clinical experience between female and male physicians, we further adjusted for physicians’ years in practice as measured by years since completion of residency. We did not include this variable in our main models because of collinearity with physicians’ age and because data were missing for 27 447 physicians (47.4%).
Sensitivity Analyses
We conducted several sensitivity analyses. First, to address the possibility that female physicians may treat healthier patients, we restricted the study population to hospitalized patients treated by physicians who specialize in the care of hospitalized patients (hospitalists). Hospitalists typically work in shifts; therefore, within the same hospital, patients treated by hospitalists are plausibly quasi-randomized to a given physician based on when patients become sick and based on hospitalists’ work schedule.34 We defined hospitalists using a validated approach: general internists who filed at least 90% of their total evaluation and management billings in an inpatient setting.35 Second, to evaluate whether our findings were sensitive to how we attributed patients to physicians, we tested the following 2 alternative attribution methods: attributing patients to physicians who had the largest number of evaluation and management claims and attributing patients to physicians who billed the first evaluation and management claim for a given hospitalization.25,36,37 Third, within some hospitals, male internists may be more likely to work in intensive care units and have severely ill patients. To address this issue, we reanalyzed our data after excluding hospitals with a medical intensive care unit. Fourth, to test whether our findings were sensitive to follow-up periods for measuring patient outcomes, we used 60-day mortality and readmissions instead of 30-day patient outcomes. Fifth, we modeled physician and patient age as continuous rather than categorical variables with quadratic and cubic terms to allow for nonlinear associations. Finally, we used logistic regression models instead of linear probability models.
Data preparation was conducted using SAS, version 9.4 (SAS Institute), and analyses were performed using Stata, version 13 (StataCorp). Additional details are provided in the eAppendix in the Supplement.
Results
Characteristics of Female and Male Physicians
During the study periods, 58 344 general internists treated at least 1 Medicare beneficiary who was hospitalized with a medical condition (Table 1). Among those, 18 751 physicians (32.1%) were female. Female physicians were younger (mean [SD] age, 42.8 [9.4] vs 47.8 [11.4] years), were more likely to have undergone osteopathic training (1577 [8.4%] vs 2770 [7.0%]), and treated fewer patients (131.9 vs 180.5 hospitalizations per year) compared with male physicians. Patient characteristics were similar between those treated by female physicians vs those treated by male physicians, with 1 modest exception: female physicians treated slightly higher proportions of female patients than male physicians did (258 091 [62.1%] vs 722 038 [60.2%]). We also found that female physicians were more likely to work in large (7460 [41.9%] vs 13 628 [35.7%]), nonprofit (13 947 [78.2%] vs 28 850 [75.6%]), major teaching hospitals (5168 [29.0%] vs 8061 [21.1%]) located in the Northeast region (4746 [26.8%] vs 8574 [22.7%]) compared with male physicians (eTable 2 in the Supplement).
Table 1.
Physician and Patient Characteristics, by Physician Sexa
| Characteristic | Female Physicians (n = 18 751) | Male Physicians (n = 39 593) |
|---|---|---|
| Physicians | ||
| Age, mean (SD), y | 42.8 (9.4) | 47.8 (11.4) |
| Years of experience since completion of residency, mean (SD), y | 11.6 (8.7) | 16.4 (10.9) |
| Credentials, No. (%) | ||
| MD (allopathic) | 17 174 (91.6) | 36 823 (93.0) |
| DO (osteopathic) | 1577 (8.4) | 2770 (7.0) |
| Annual hospitalizations per physician, No.b | 131.9 | 180.5 |
| Patients | ||
| No. of patients | 415 559 | 1 200 296 |
| Age, mean (SD), y | 80.8 (8.5) | 80.6 (8.5) |
| Female, No. (%) | 258 091 (62.1) | 722 038 (60.2) |
| Race/ethnicity, No. (%) | ||
| White | 336 879 (81.1) | 973 507 (81.1) |
| Black | 45 949 (11.1) | 126 593 (10.6) |
| Hispanic | 19 605 (4.7) | 65 186 (5.4) |
| Other | 13 126 (3.2) | 35 010 (2.9) |
| Annual household income, mean (SD), $ | 59 570 (23 839) | 55 841 (22 007) |
| Medicaid coverage, No. (%) | 96 275 (23.2) | 294 940 (24.6) |
| Coexisting conditions, No. (%) | ||
| Congestive heart failure | 82 693 (19.9) | 241 113 (20.1) |
| Chronic obstructive pulmonary disease | 101 966 (24.5) | 315 736 (26.3) |
| Diabetes | 131 640 (31.7) | 388 833 (32.4) |
| Renal failure | 91 745 (22.1) | 261 492 (21.8) |
| Neurologic disorders | 65 085 (15.7) | 192 980 (16.1) |
| Cancer | 30 469 (7.3) | 83 704 (7.0) |
| Mental illness | 65 286 (15.7) | 182 815 (15.2) |
P < .001 for all comparisons.
Estimated assuming that the proportion of Medicare beneficiaries with Medicare Advantage plans is 30%, and Medicare beneficiaries comprise 40% of all hospitalizations in the United States.
Physician Sex and Patient Mortality
The final sample for the analyses of 30-day mortality rates included 1 583 028 hospitalizations treated by 57 896 physicians. Overall 30-day mortality for the entire sample was 179 162 (11.32%). Patients cared for by female physicians had lower 30-day mortality than did patients treated by male physicians (10.82%vs11.49%; risk difference [RD], −0.67%; 95% CI, −0.80% to −0.54%; P < .001; number needed to treat [NNT] to prevent 1 death, 149) after accounting for patient characteristics (Table2). The difference in mortality persisted after adjustment for hospital fixed effects (female physicians, 10.91% vs male physicians, 11.46%; adjusted RD, −0.55%; 95% CI, −0.67% to −0.42%; P < .001; NNT, 182). Further adjusting for physician characteristics had a limited effect on these results (female physicians, 11.07% vs male physicians, 11.49%; adjusted RD, −0.43%; 95% CI −0.57% to −0.28%; P < .001; NNT, 233).
Table 2.
Association Between Physician Sex and 30-Day Patient Mortality and Readmissions
| Characteristic | No. of Hospitalizations (No. of Physicians) | Patient Outcomes, % (95% CI) | Adjusted Risk Difference, % (95% CI)a | P Value | |
|---|---|---|---|---|---|
| Female Physicians | Male Physicians | ||||
| 30-d Mortality rate | |||||
| Model 1: risk-adjusted 30-d mortality rateb | 1 583 028 (57 896) | 10.82 (10.71 to 10.93) | 11.49 (11.42 to 11.56) | −0.67 (−0.80 to −0.54) | <.001 |
| Model 2: Model 1 + hospital fixed effects | 1 583 024 (57 896) | 10.91 (10.81 to 11.01) | 11.46 (11.40 to 11.52) | −0.55 (−0.67 to −0.42) | <.001 |
| Model 3: Model 2 + physician characteristics | 1 283 621 (46 201) | 11.07 (10.95 to 11.19) | 11.49 (11.43 to 11.56) | −0.43 (−0.57 to −0.28) | <.001 |
| 30-d Readmission rate | |||||
| Model 1: risk-adjusted 30-d readmission rateb | 1 540 797 (57 876) | 15.01 (14.89 to 15.14) | 15.57 (15.49 to 15.65) | −0.55 (−0.71 to −0.41) | <.001 |
| Model 2: Model 1 + hospital fixed effects | 1 540 797 (57 876) | 15.00 (14.89 to 15.13) | 15.57 (15.50 to 15.64) | −0.56 (−0.70 to −0.42) | <.001 |
| Model 3: Model 2 + physician characteristics | 1 249 210 (46 205) | 15.02 (14.88 to 15.15) | 15.57 (15.49 to 15.64) | −0.55 (−0.71 to −0.39) | <.001 |
Adjusted risk differences between female and male phyisicans. SEs were clustered at the physician level.
Risk adjustment using patients’ age, sex, race, primary diagnosis, coexisting conditions (Elixhauser comorbidity index), median household income, Medicaid status, and year indicators.
Physician Sex and Patient Readmissions
The analyses of 30-day readmission rates included 1 540 797 hospitalizations treated by 57 876 physicians. The overall 30-day readmission rate for this sample was 237 644 (15.42%). Patients of female physicians had significantly lower readmission rates than those with male physicians, after accounting for patient characteristics (15.01% vs 15.57%; RD, −0.55%; 95% CI, −0.71% to −0.41%; P < .001; NNT to prevent 1 readmission, 182) (Table 2). Adjusting for hospital fixed effects (female physicians, 15.00% vs male physicians, 15.57%; adjusted RD, −0.56%; 95% CI, −0.70% to −0.42%; P < .001; NNT, 179) and further accounting for physician characteristics (female physicians, 15.02% vs male physicians, 15.57%; adjusted RD, −0.55%; 95% CI, −0.71% to −0.39%; P < .001; NNT, 182) had little effect on these results.
Physician Sex and Patient Outcomes by Primary Diagnoses
Patients of female physicians had lower mortality and readmission rates across all medical conditions we examined, although the magnitude of the difference varied by condition and was not always statistically significant. Patients of female physicians had lower mortality for sepsis (23.05% vs 25.09%), pneumonia (10.11% vs 11.03%), acute renal failure (12.54% vs 13.30%), and arrhythmia (5.08% vs 6.02%) vs patients of male physicians; however, we did not observe a statistically significant difference in mortality for congestive heart failure (11.69% vs 11.95%), urinary tract infection (5.79% vs 6.11%), and gastrointestinal bleeding (9.70% vs 10.27%) (Table 3). Patients’ readmission rates were significantly lower for female physicians than male physicians for most of the conditions (Table 4).
Table 3.
Association Between Physician Sex and 30-Day Patient Mortality by Condition
| Condition | No. of Hospitalizations (No. of Physicians) | Adjusted 30-Day Mortality Rate, % (95% CI)a | Adjusted Risk Difference, % (95% CI)b | P Value | |
|---|---|---|---|---|---|
| Female Physicians | Male Physicians | ||||
| Sepsis | 118 623 (28 972) | 23.05 (22.51 to 23.58) | 25.09 (24.79 to 25.39) | −2.05 (−2.68 to −1.41) | <.001 |
| Pneumonia | 98 665 (28 564) | 10.11 (9.71 to 10.50) | 11.03 (10.81 to 11.24) | −0.92 (−1.39 to −0.45) | <.001 |
| Congestive heart failure | 92 956 (27 677) | 11.69 (11.25 to 12.13) | 11.95 (11.71 to 12.18) | −0.26 (−0.78 to 0.26) | .33 |
| Chronic obstructive pulmonary disease | 70 971 (24 019) | 5.05 (4.70 to 5.40) | 5.42 (5.24 to 5.60) | −0.37 (−0.79 to 0.04) | .08 |
| Urinary tract infection | 68 542 (24 363) | 5.79 (5.43 to 6.14) | 6.11 (5.91 to 6.31) | −0.32 (−0.75 to 0.11) | .14 |
| Acute renal failure | 54 039 (22 060) | 12.54 (11.98 to 13.10) | 13.30 (12.99 to 13.61) | −0.76 (−1.44 to −0.09) | .03 |
| Arrhythmia | 42 411 (19 947) | 5.08 (4.63 to 5.53) | 6.02 (5.77 to 6.27) | −0.94 (−1.48 to −0.39) | .001 |
| Gastrointestinal bleeding | 24 031 (14 536) | 9.70 (8.87 to 10.53) | 10.27 (9.85 to 10.69) | −0.57 (−1.6 to 0.42) | .26 |
Risk-adjusted mortality rates with additional adjustment for physician characteristic and with hospital fixed effects (model 3). Standard errors were clustered at the physician level.
Adjusted risk differences between female and male phyisicans.
Table 4.
Association Between Physician Sex and 30-Day Patient Readmissions by Condition
| Condition | No. of Hospitalizations (No. of Physicians) | Adjusted 30-Day Readmission Rate, % (95% CI)a | Adjusted Risk Difference, % (95% CI)b | P Value | |
|---|---|---|---|---|---|
| Female Physicians | Male Physicians | ||||
| Sepsis | 104 446 (27 714) | 15.51 (15.05 to 15.98) | 16.15 (15.90 to 16.40) | −0.64 (−1.19 to −0.09) | .02 |
| Pneumonia | 95 822 (28 249) | 14.01 (13.53 to 14.49) | 15.15 (14.90 to 15.40) | −1.14 (−1.70 to −0.58) | <.001 |
| Congestive heart failure | 90 365 (27 375) | 19.91 (19.36 to 20.47) | 21.02 (20.72 to 21.32) | −1.10 (−1.76 to −0.45) | .001 |
| Chronic obstructive pulmonary disease | 70 769 (24 019) | 18.12 (17.48 to 18.76) | 18.99 (18.67 to 19.31) | −0.87 (−1.62 to −0.12) | .02 |
| Urinary tract infection | 68 533 (24 393) | 14.11 (13.57 to 14.66) | 14.91 (14.60 to 15.21) | −0.79 (−1.45 to −0.14) | .02 |
| Acute renal failure | 52 969 (21 809) | 16.61 (15.96 to 17.27) | 17.14 (16.78 to 17.51) | −0.53 (−1.32 to 0.26) | .19 |
| Arrhythmia | 42 338 (19 950) | 14.38 (13.67 to 15.08) | 14.41 (14.04 to 14.79) | −0.04 (−0.88 to 0.81) | .93 |
| Gastrointestinal bleeding | 23 709 (14 439) | 14.68 (13.67 to 15.69) | 16.24 (15.71 to 16.77) | −1.55 (−2.77 to −0.34) | .01 |
Risk-adjusted readmission rates with additional adjustment for physician characteristic and with hospital fixed effects (model 3). Standard errors were clustered at the physician level.
Adjusted risk differences between female and male phyisicans.
Physician Sex and Patient Outcomes by Severity of Illness
The association between physician sex and patient outcomes was consistent across patients’ severity of illness (Figure, A and B). With regard to mortality, patients of female physicians had significantly lower mortality rates than did patients of male physicians in all subgroups except for patients in the second lowest quintile of expected mortality (eTable 3 in the Supplement). The interaction between physician sex and expected mortality of patients was statistically significant.
Figure. Association Between Physician Sex and Patient Outcomes by Expected Mortality Rates.
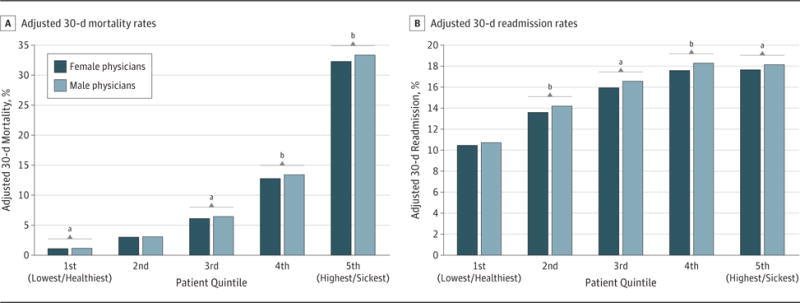
A, Adjusted 30-day mortality rates. B, Adjusted 30-day readmission rates. Risk-adjusted mortality rates were calculated with additional adjustment for physician characteristics and with hospital fixed effects (model 3). Standard errors were clustered at the physician level.
aP < .05.
bP < .001.
Readmission rates of patients were lower for female physicians than for male physicians for all subgroups except for the least sick patients. The interaction between physician sex and patient illness severity was not statistically significant.
Analysis of Potential Mechanisms
We found that additional adjustment for length of stay, use of care, discharge location, patient volume, or physicians’ years of practice did not affect our findings (eTable 4 in the Supplement).
Sensitivity Analyses
We found similar patterns when we restricted our sample to patients treated by hospitalists (24 429 of 57 896 general internists [42.2%] were defined as hospitalists). Patients receiving care by female hospitalists had lower mortality and readmission rates compared with patients receiving care by male hospitalists (eTable 5 in the Supplement). Our findings were not qualitatively affected by attributing physicians according to evaluation and management claims (eTable 6 and eTable 7 in the Supplement), excluding hospitals with a medical intensive care unit (eTable 8 in the Supplement), using 60-day patient outcomes (eTable 9 in the Supplement), or modeling age as a continuous variable (eTable 10 in the Supplement). Our findings were also unaffected by estimating multivariable logistic regression models instead of linear probability models (eTable 11 in the Supplement). Patients treated by female physicians had 0.95 times the odds of death (95% CI, 0.93–0.97; P < .001) and 0.96 time the odds of readmission (95% CI, 0.95–0.97; P < .001) compared with patients cared for by male physicians.
Discussion
We found that elderly patients receiving inpatient care from female internists had 30-day lower mortality and readmission rates compared with patients cared for by male internists. This association was consistent across a variety of conditions and across patients’ severity of illness. Taken together with previous evidence1–15 suggesting that male and female physicians may practice differently, our findings indicate that potential differences in practice patterns between male and female physicians may have important clinical implications for patient outcomes.
Our findings that female internists appear to have better outcomes for inpatient care than their male peers are consistent with results from prior studies of process measures of quality. There is evidence in the primary care setting suggesting that, compared with male physicians, female physicians are more likely to practice evidence-based medicine,3 perform as well or better on standardized examinations,16 and provide more patient-centered care.12–15 Patients of female primary care physicians also experience fewer emergency department visits compared with patients of male primary care physicians.38 Data from other industries suggest that men may be less deliberate in their approach to solving complex problems.39–41 If these findings also apply to how male and female physicians approach clinical problems and decisions, these patterns of behavior may provide a plausible mechanism linking physician sex with patient outcomes.
Although the difference in patient mortality between male and female physicians was modest, an observed effect size of a 0.43-percentage point difference or a relative risk reduction of 4% in mortality is arguably a clinically meaningful difference. For context, there has been widespread recognition that patient outcomes have improved substantially during the past decade; all-cause mortality declined from 5.0% in 2003 to 4.5% in 2013 among Medicare beneficiaries.42 This reduction in mortality is recognized as the result of large national investments in innovation, new treatments, and quality improvement that allow us to treat patients better. The difference in mortality rates between patients of male and female physicians in our study was of a comparable magnitude. Furthermore, given that there are more than 10 million Medicare hospitalizations due to medical conditions in the United States annually and assuming that the association between sex and mortality is causal, we estimate that approximately 32 000 fewer patients would die if male physicians could achieve the same outcomes as female physicians every year.43 The effect would be even larger if the associations between physician sex and patient outcomes also hold for non-Medicare populations.
An important issue in interpreting our findings is whether they can be explained by differences in unmeasured severity of illness of patients treated by male vs female physicians. The inpatient setting, compared with the outpatient setting, offers a unique advantage when studying patient outcomes between male and female physicians: within a given hospital, there is plausibly less selection of the physician by the patient or of the patient by the physician. Although some patients choose their primary care physician, and sex of the physician may be a factor in making their decision, patients hospitalized urgently or emergently are less likely to select their physicians. We found that nearly all observable characteristics typically associated with illness severity were well balanced between female and male physicians. Even for hospitalist physicians, among whom patients are plausibly more likely to be randomly assigned, we found that patient characteristics were balanced between male and female physicians and that patients of female physicians continued to have lower patient mortality and readmission rates.
We are aware of only 1 other study examining the association between physician sex and patient mortality. Jerant and colleagues44 analyzed a small cohort of relatively healthy outpatients (who are, in general, healthier than hospitalized patients) and found no associations between physician sex and patient mortality. However, several analyses investigating differences in processes of care between male and female physicians have yielded results that align with our findings. For instance, Kim et al1 and Berthold et al2 both found that female physicians outperform male physicians on process measures for patients with diabetes.
Limitations
First, as is the case for any observational study, we could not fully account for unmeasured differences in the risk of death and readmissions between patients of male and female physicians. Although we addressed this issue in several ways, including the use of a natural experimental design exploiting the quasi-randomized assignment of patients to hospitalists, it is still possible that unmeasured confounding (eg, residual differences in socioeconomic status of patients that are not explained by patient race/ethnicity, Medicaid eligibility, and household income level) could explain the observed differences in patient outcomes. However, the residual confounding would have to be of substantial magnitude to explain the differences we found. Second, we were unable to identify exactly why female physicians have better outcomes than male physicians. Given that physician sex by itself does not determine patient outcomes, sex should serve as a marker of differences in practice patterns between male and female physicians that meaningfully affect patient outcomes. Further studies using clinical data would be helpful in understanding which practice patterns of physicians are driving the differences in patient outcomes. Third, we used self-reported data to identify physician sex, which requires respondents to categorize themselves as either male or female; therefore, we could not capture respondents who were transgender. It is possible that transgender physicians chose to either leave this question blank or select 1 of the 2 available categories, which may lead to a low degree of misclassification. Any misclassification in self-reported sex would likely bias our estimates toward the null. Finally, our analysis was limited to Medicare patients hospitalized with medical conditions treated by general internists. Thus, our findings may not be generalizable to surgical conditions, to patients treated by physicians of other specialties, or to outpatient care.
Conclusions
Using a national sample of hospitalized Medicare beneficiaries, we found that patients who receive care from female general internists have lower 30-day mortality and readmission rates than do patients cared for by male internists. These findings suggest that the differences in practice patterns between male and female physicians, as suggested in previous studies, may have important clinical implications for patient outcomes. Understanding exactly why these differences in care quality and practice patterns exist may provide valuable insights into improving quality of care for all patients, irrespective of who provides their care.
Supplementary Material
Key Points.
Question
Do patient outcomes differ between those treated by male and female physicians?
Findings
In this cross-sectional study, we examined nationally representative data of hospitalized Medicare beneficiaries and found that patients treated by female physicians had significantly lower mortality rates (adjusted mortality rate, 11.07% vs 11.49%) and readmission rates (adjusted readmission rate, 15.02% vs 15.57%) compared with those cared for by male physicians within the same hospital.
Meaning
Differences in practice patterns between male and female physicians, as suggested in previous studies, may have important clinical implications for patient outcomes.
Acknowledgments
Dr Tsugawa reported being supported in part by St Luke’s International University. Dr Jena reported receiving consulting fees unrelated to this work from Pfizer Inc, Hill Rom Services Inc, Bristol Myers Squibb, Novartis Pharmaceuticals, Vertex Pharmaceuticals, and Precision Health Economics, a company providing consulting services to the life sciences industry.
Funding/Support: Dr Jena was supported by the Early Independence Award, grant 1DP5OD017897-01, from the National Institutes of Health.
Role of the Funder/Sponsor: The funding source had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Author Contributions: Dr Tsugawa had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Tsugawa, Jena, Jha. Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Tsugawa, Jena, Jha.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Tsugawa, Orav.
Administrative, technical, or material support: Jha.
Study supervision: Jena, Jha.
Conflict of Interest Disclosures: No other disclosures were reported.
References
- 1.Kim C, McEwen LN, Gerzoff RB, et al. Is physician gender associated with the quality of diabetes care? Diabetes Care. 2005;28(7):1594–1598. doi: 10.2337/diacare.28.7.1594. [DOI] [PubMed] [Google Scholar]
- 2.Berthold HK, Gouni-Berthold I, Bestehorn KP, Böhm M, Krone W. Physician gender is associated with the quality of type 2 diabetes care. J Intern Med. 2008;264(4):340–350. doi: 10.1111/j.1365-2796.2008.01967.x. [DOI] [PubMed] [Google Scholar]
- 3.Baumhäkel M, Müller U, Böhm M. Influence of gender of physicians and patients on guideline-recommended treatment of chronic heart failure in a cross-sectional study. Eur J Heart Fail. 2009;11(3):299–303. doi: 10.1093/eurjhf/hfn041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andersen MR, Urban N. Physician gender and screening: do patient differences account for differences in mammography use? Women Health. 1997;26(1):29–39. doi: 10.1300/J013v26n01_03. [DOI] [PubMed] [Google Scholar]
- 5.Frank E, Dresner Y, Shani M, Vinker S. The association between physicians’ and patients’ preventive health practices. CMAJ. 2013;185(8):649–653. doi: 10.1503/cmaj.121028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Frank E, Harvey LK. Prevention advice rates of women and men physicians. Arch Fam Med. 1996;5(4):215–219. doi: 10.1001/archfami.5.4.215. [DOI] [PubMed] [Google Scholar]
- 7.Franks P, Bertakis KD. Physician gender, patient gender, and primary care. J Womens Health (Larchmt) 2003;12(1):73–80. doi: 10.1089/154099903321154167. [DOI] [PubMed] [Google Scholar]
- 8.Franks P, Clancy CM. Physician gender bias in clinical decisionmaking: screening for cancer in primary care. Med Care. 1993;31(3):213–218. doi: 10.1097/00005650-199303000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Kruger J, Shaw L, Kahende J, Frank E. Health care providers’ advice to quit smoking, National Health Interview Survey, 2000, 2005, and 2010. Prev Chronic Dis. 2012;9:E130. doi: 10.5888/pcd9.110340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lurie N, Slater J, McGovern P, Ekstrum J, Quam L, Margolis K. Preventive care for women: does the sex of the physician matter? N Engl J Med. 1993;329(7):478–482. doi: 10.1056/NEJM199308123290707. [DOI] [PubMed] [Google Scholar]
- 11.Smith AW, Borowski LA, Liu B, et al. US primary care physicians’ diet-, physical activity-, and weight-related care of adult patients. Am J Prev Med. 2011;41(1):33–42. doi: 10.1016/j.amepre.2011.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bertakis KD, Helms LJ, Callahan EJ, Azari R, Robbins JA. The influence of gender on physician practice style. Med Care. 1995;33(4):407–416. doi: 10.1097/00005650-199504000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Krupat E, Rosenkranz SL, Yeager CM, Barnard K, Putnam SM, Inui TS. The practice orientations of physicians and patients: the effect of doctor-patient congruence on satisfaction. Patient Educ Couns. 2000;39(1):49–59. doi: 10.1016/s0738-3991(99)00090-7. [DOI] [PubMed] [Google Scholar]
- 14.Roter DL, Hall JA, Aoki Y. Physician gender effects in medical communication: a meta-analytic review. JAMA. 2002;288(6):756–764. doi: 10.1001/jama.288.6.756. [DOI] [PubMed] [Google Scholar]
- 15.Roter DL, Hall JA. Physician gender and patient-centered communication: a critical review of empirical research. Annu Rev Public Health. 2004;25:497–519. doi: 10.1146/annurev.publhealth.25.101802.123134. [DOI] [PubMed] [Google Scholar]
- 16.Ferguson E, James D, Madeley L. Factors associated with success in medical school: systematic review of the literature. BMJ. 2002;324(7343):952–957. doi: 10.1136/bmj.324.7343.952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kaiser Family Foundation. Distribution of Physicians by Gender. Menlo Park, CA: Kaiser Family Foundation; 2016. [Google Scholar]
- 18.Association of American Medical Colleges. US Medical School Applicants and Students 1982–1983 to 2011–2012. https://www.aamc.org/download/153708/data/charts1982to2012.pdf. Accessed November 10, 2016.
- 19.Jolly S, Griffith KA, DeCastro R, Stewart A, Ubel P, Jagsi R. Gender differences in time spent on parenting and domestic responsibilities by high-achieving young physician-researchers. Ann Intern Med. 2014;160(5):344–353. doi: 10.7326/M13-0974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Seabury SA, Chandra A, Jena AB. Trends in the earnings of male and female health care professionals in the United States, 1987 to 2010. JAMA Intern Med. 2013;173(18):1748–1750. doi: 10.1001/jamainternmed.2013.8519. [DOI] [PubMed] [Google Scholar]
- 21.Nonnemaker L. Women physicians in academic medicine: new insights from cohort studies. N Engl J Med. 2000;342(6):399–405. doi: 10.1056/NEJM200002103420606. [DOI] [PubMed] [Google Scholar]
- 22.Jagsi R, Griffith KA, Stewart A, Sambuco D, DeCastro R, Ubel PA. Gender differences in the salaries of physician researchers. JAMA. 2012;307(22):2410–2417. doi: 10.1001/jama.2012.6183. [DOI] [PubMed] [Google Scholar]
- 23.Ross JS, Normand SL, Wang Y, et al. Hospital volume and 30-day mortality for three common medical conditions. N Engl J Med. 2010;362(12):1110–1118. doi: 10.1056/NEJMsa0907130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Drye EE, Normand SL, Wang Y, et al. Comparison of hospital risk-standardized mortality rates calculated by using in-hospital and 30-day models: an observational study with implications for hospital profiling. Ann Intern Med. 2012;156(1, pt 1):19–26. doi: 10.1059/0003-4819-156-1-201201030-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McWilliams JM, Landon BE, Chernew ME, Zaslavsky AM. Changes in patients’ experiences in Medicare Accountable Care Organizations. N Engl J Med. 2014;371(18):1715–1724. doi: 10.1056/NEJMsa1406552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jena AB, Olenski AR, Blumenthal DM. Sex differences in physician salary in US public medical schools. JAMA Intern Med. 2016;176(9):1294–1304. doi: 10.1001/jamainternmed.2016.3284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jena AB, Khullar D, Ho O, Olenski AR, Blumenthal DM. Sex differences in academic rank in US medical schools in 2014. JAMA. 2015;314(11):1149–1158. doi: 10.1001/jama.2015.10680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 29.Carey TS, Motyka TM, Garrett JM, Keller RB. Do osteopathic physicians differ in patient interaction from allopathic physicians? an empirically derived approach. J Am Osteopath Assoc. 2003;103(7):313–318. [PubMed] [Google Scholar]
- 30.Wooldridge JM. Econometric Analysis of Cross Section and Panel Data. Cambridge, MA: MIT Press; 2010. [Google Scholar]
- 31.Hellevik O. Linear vs logistic regression when the dependent variable is a dichotomy. Qual Quant. 2009;43(1):59–74. doi: 10.1007/s11135-007-9077-3. [DOI] [Google Scholar]
- 32.Williams R. Using the margins command to estimate and interpret adjusted predictions and marginal effects. Stata J. 2012;12(2):308–331. [Google Scholar]
- 33.Agency for Healthcare Research and Quality. Clinical Classifications Software (CCS) for ICD-9-CM. https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Updated October 7, 2016. Accessed November 7, 2016.
- 34.Hinami K, Whelan CT, Miller JA, Wolosin RJ, Wetterneck TB, Society of Hospital Medicine Career Satisfaction Task Force Job characteristics, satisfaction, and burnout across hospitalist practice models. J Hosp Med. 2012;7(5):402–410. doi: 10.1002/jhm.1907. [DOI] [PubMed] [Google Scholar]
- 35.Kuo YF, Sharma G, Freeman JL, Goodwin JS. Growth in the care of older patients by hospitalists in the United States. N Engl J Med. 2009;360(11):1102–1112. doi: 10.1056/NEJMsa0802381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McWilliams JM, Hatfield LA, Chernew ME, Landon BE, Schwartz AL. Early performance of accountable care organizations in Medicare. N Engl J Med. 2016;374(24):2357–2366. doi: 10.1056/NEJMsa1600142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Adams JL, Mehrotra A, Thomas JW, McGlynn EA. Physician cost profiling—reliability and risk of misclassification. N Engl J Med. 2010;362(11):1014–1021. doi: 10.1056/NEJMsa0906323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dahrouge S, Seale E, Hogg W, et al. A comprehensive assessment of family physician gender and quality of care: a cross-sectional analysis in Ontario, Canada. Med Care. 2016;54(3):277–286. doi: 10.1097/MLR.0000000000000480. [DOI] [PubMed] [Google Scholar]
- 39.Powell M, Ansic D. Gender differences in risk behaviour in financial decision-making: an experimental analysis. J Econ Psychol. 1997;18(6):605–628. doi: 10.1016/S0167-4870(97)00026-3. [DOI] [Google Scholar]
- 40.Barber BM, Odean T. Boys will be boys: gender, overconfidence, and common stock investment. Q J Econ. 2001;116(1):261–292. doi: 10.1162/003355301556400. [DOI] [Google Scholar]
- 41.Charness G, Gneezy U. Strong evidence for gender differences in risk taking. J Econ Behav Organ. 2012;83(1):50–58. doi: 10.1016/j.jebo.2011.06.007. [DOI] [Google Scholar]
- 42.Krumholz HM, Nuti SV, Downing NS, Normand SL, Wang Y. Mortality, hospitalizations, and expenditures for the Medicare population aged 65 years or older, 1999–2013. JAMA. 2015;314(4):355–365. doi: 10.1001/jama.2015.8035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Weiss AJ, Elixhauser A. HCUP Statistical Brief #180. Rockville, MD: Agency for Healthcare Research and Quality; Oct, 2014. Overview of hospital stays in the United States, 2012. [PubMed] [Google Scholar]
- 44.Jerant A, Bertakis KD, Fenton JJ, Franks P. Gender of physician as the usual source of care and patient health care utilization and mortality. J Am Board Fam Med. 2013;26(2):138–148. doi: 10.3122/jabfm.2013.02.120198. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


