Introduction
Key Teaching Points.
-
•
We experienced the case of an elderly woman with ventricular fibrillation and a bronchogenic cyst located in the atrioventricular septal region that was identified by echocardiography, cardiac magnetic resonance imaging, and contrast-enhanced computed tomography.
-
•
After ruling out congenital and acquired long QT syndrome, we believe that the ventricular fibrillation was attributable to prolonged QT accompanying bradycardia associated with AV block from compression of the AV node area by the cyst.
-
•
The possible presence of cardiac tumors located in the septal region should be assessed by imaging in patients with marked first- and second-degree atrioventricular block.
Bronchogenic cysts are one of the types of primary cardiac tumors that can occur. They arise in the interatrial septum, especially near the atrioventricular node,1 which may cause atrioventricular block owing to its location. The incidence of these cardiac tumors is very low.2, 3, 4 Previous case reports regarding bronchogenic cysts of the interatrial septum have shown association of bronchogenic cysts with atrioventricular block, but not with the life-threatening ventricular arrhythmias. We report a case with bronchogenic cyst in the atrioventricular nodal region presenting as ventricular fibrillation.
Case report
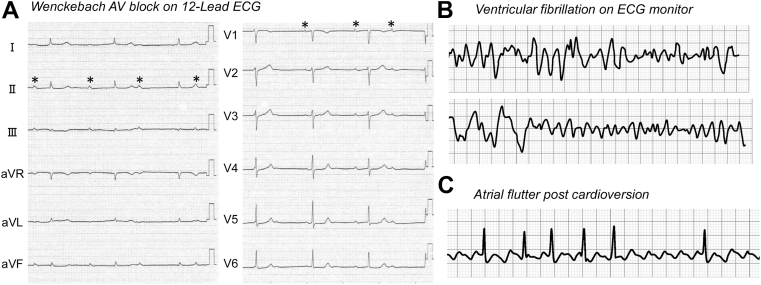
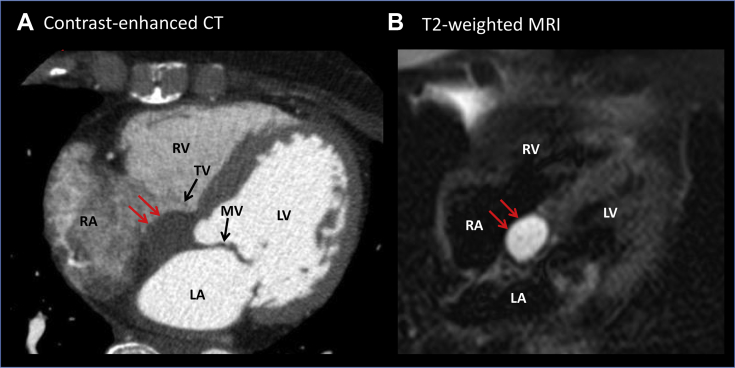
A 77-year-old woman experienced syncope while walking. She was sent to the emergency department at a local hospital. Twelve-lead electrocardiogram on her arrival showed Wenckebach atrioventricular block and QT-interval prolongation (Figure 1A, QT interval 0.55 seconds) in the absence of electrolyte abnormality. Neither did she have any previous history of QT-interval prolongation to suggest congenital long QT syndrome. After admission, she collapsed with a seizure owing to ventricular fibrillation documented on electrocardiogram monitor (Figure 1B). Atrial flutter was observed after the cardioversion (Figure 1C). An intracardiac mass with 2 cm diameter was identified in the atrioventricular septum by echocardiography, which was further evaluated by cardiac contrast-enhanced computed tomography (Figure 2A). Cardiac magnetic resonance imaging (MRI) performed after she was transferred to our hospital identified a 3-cm-diameter mass in the atrioventricular septal region on T2-weighted images (Figure 2B). Neither fat deposition nor late gadolinium enhancement was identified in the tumor on cardiac MRI images, which led to the diagnosis of a probable cystic tumor. The tumor was successfully resected surgically, but resulted in complete atrioventricular block. During the surgery, the tumor appeared to be compressing the atrioventricular septal region including the atrioventricular node. Electrophysiological testing for the induction of malignant ventricular arrhythmias was performed 3 weeks after the surgery. However, no sustained ventricular tachyarrhythmias were induced even with delivery of triple extrastimuli from the right ventricular apex and outflow tract during isoproterenol infusion. Based on this result, the patient was only given a dual-chamber pacemaker. During the 6 months of follow-up after discharge, the patient has been free of further cardiac events and symptoms.
Figure 1.
A: The previous 12-lead electrocardiogram (ECG) showed Wenckebach second-degree atrioventricular block (* indicates P wave) and QT-interval prolongation. B: Ventricular fibrillation was recorded on ECG monitoring after admission to the hospital. C: Atrial flutter was observed after the cardioversion of ventricular fibrillation.
Figure 2.
Contrast-enhanced computed tomography (CT) (A) and T2-weighted cardiac magnetic resonance imaging (MRI) (B) showed a 3-cm mass (red arrows) in the atrioventricular septal region, which was identified as a cystic tumor. LA = left atrium; LV = left ventricle; MV = mitral valve; RA = right atrium; RV = right ventricle; TV = tricuspid valve.
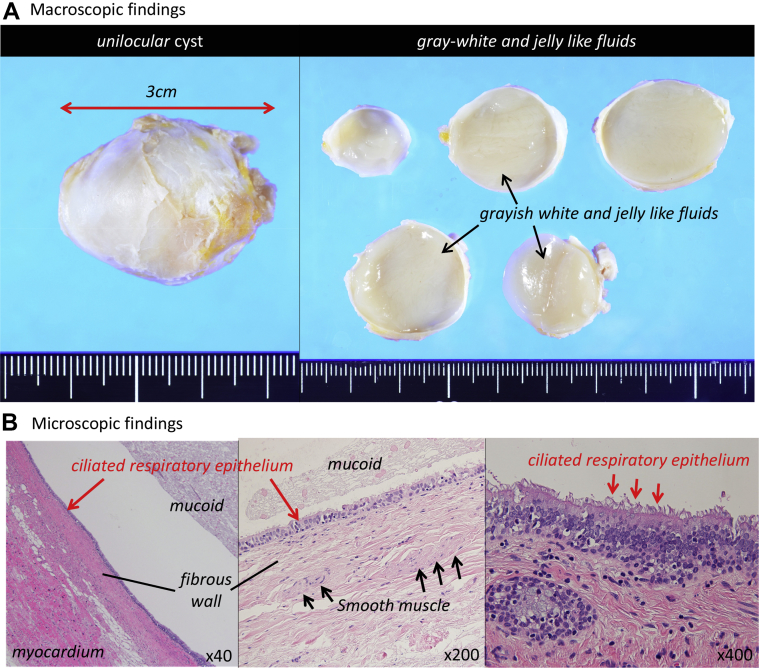
Pathology
The resected unilocular cyst contained a grayish white jelly-like fluid (Figure 3A). Histology showed ciliated respiratory epithelium on the inner wall of the cyst (Figure 3B). Smooth muscle cell was also observed within the wall. These histologic findings strongly suggest diagnosis of a bronchogenic cyst.
Figure 3.
A: The resected cyst was unilocular (left), and contained a grayish white gel, as the sections show (right). B: Histology showed smooth muscle cell within the fibrous tissue wall of the cyst. The ciliated respiratory epithelium was also observed on the inner wall.
Discussion
Most such cardiac tumors are benign, although some have caused sudden death owing to hemodynamic and conduction system disturbances. There have been 120 cases of sudden death reported to be associated with primary intracardiac tumors.5, 6 Bronchogenic cysts are known as a rare tumor located in the atrioventricular septal region that may cause heart block.7 In fact, there are a few case reports of bronchogenic cyst presenting with heart block. The association of bronchogenic cyst with life-threatening ventricular arrhythmia remains unclear.
This is the first report that has demonstrated the association of bronchogenic cyst with malignant ventricular arrhythmias leading to sudden cardiac death. We hypothesize that ventricular fibrillation in this case occurred as a consequence of QT prolongation owing to bradycardia from unstable heart block, although compression of the atrioventricular septum is another possible cause.
The incidence of ventricular fibrillation may have been secondarily affected by compression of the atrioventricular septal region, including the atrioventricular node, owing to the tumor growth because no infiltration of the tumor into the surrounding tissue was observed on histology. In general, bronchogenic cysts may increase in size over time without causing symptoms owing to mucoid production from ciliated epithelial cells.9 However, our case shows that enlarged bronchogenic cysts may also affect the surrounding tissue. Atrial flutter was recurrently observed in this patient after cardioversion. Compression by the tumor may have facilitated atrial flutter by creating an area of conduction delay in the lower region of the right atrioventricular septum. No observations were made during the surgery that might otherwise explain the atrial flutter. Cardiac MRI is useful for the assessment of cardiac tumors.8 In this case, cardiac MRI clearly showed an oval tumor in the atrioventricular septal region with T2 high intensity and T1 low intensity and no late gadolinium enhancement, which helped diagnosis of the tumor as a bronchogenic cyst. The presence of structural heart disease, including cardiac tumors located in the septal region, should be assessed by echocardiography and cardiac MRI in patients with marked first- and second-degree atrioventricular block. The early diagnosis of such rare cardiac tumors may provide us with significant information regarding the risk of heart block progression or sudden cardiac death owing to life-threatening ventricular arrhythmias.
References
- 1.Law K.B., Feng T., Nair V., Cusimano R.J., Butany J. Cystic tumor of the atrioventricular node: rare antemortem diagnosis. Cardiovasc Pathol. 2012;21:120–127. doi: 10.1016/j.carpath.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 2.Borges A.C., Knebel F., Lembcke A., Panda A., Komoda T., Heimann N.E., Meyer R., Baumann G., Hetzer R. Bronchogenic cyst of the interatrial septum presenting as atrioventricular block. Ann Thorac Surg. 2009;87:1920–1923. doi: 10.1016/j.athoracsur.2008.10.051. [DOI] [PubMed] [Google Scholar]
- 3.Jiang H., Wang H., Wu H., Li X. Bronchogenic cyst of the interatrial septum. J Cardiothorac Surg. 2013;8:171. doi: 10.1186/1749-8090-8-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reynen K. Frequency of primary tumors of the heart. Am J Cardiol. 1996;77(1):107. doi: 10.1016/s0002-9149(97)89149-7. [DOI] [PubMed] [Google Scholar]
- 5.Ford S.E. Congenital cystic tumors of the atrio-ventricular node: successful demonstration by an abbreviated dissection of the conduction system. Cardiovasc Pathol. 1999;8:233–237. doi: 10.1016/s1054-8807(99)00013-7. [DOI] [PubMed] [Google Scholar]
- 6.Cina S.J., Smialek J.E., Burke A.P., Virmani R., Hutchinson G.M. Primary cardiac tumors causing sudden death: a review of the literature. Am J Forensic Med Pathol. 1996;17:271–281. doi: 10.1097/00000433-199612000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Travers H. Congenital polycystic tumor of the atrioventricular node: possible familial occurrence and critical review of reported cases with special emphasis on histogenesis. Hum Pathol. 1982;13(1):25–35. doi: 10.1016/s0046-8177(82)80135-4. [DOI] [PubMed] [Google Scholar]
- 8.Motwani M., Kidambi A., Herzog B.A., Uddin A., Grrenwood J.P., Plein S. MR imaging of cardiac tumors and masses: a review of methods and clinical applications. Radiology. 2013;268:26–43. doi: 10.1148/radiol.13121239. [DOI] [PubMed] [Google Scholar]
- 9.Naidich D.P., Srichai M.B., Krinsky G.A. Lippincott Williams & Wilkins; Philadelphia, PA: 2007. Computed Tomography and Magnetic Resonance of the Thorax. [Google Scholar]