Abstract
Aims and Objectives:
Dentures in the oral cavity may act as a reservoir of microorganisms, which may be related to systemic infections. The aim of this study was to investigate the nonoral pathogenic bacteria in the oral cavity of patients with removable dentures in Shiraz, Southern Iran.
Materials and Methods:
The bacterial flora of saliva samples from 50 men and 50 women with removable dentures and 100 age- and sex-matched controls with normal dentate were compared using culture, Gram staining, and API20E Kit methods. All data were analyzed using SPSS software.
Results:
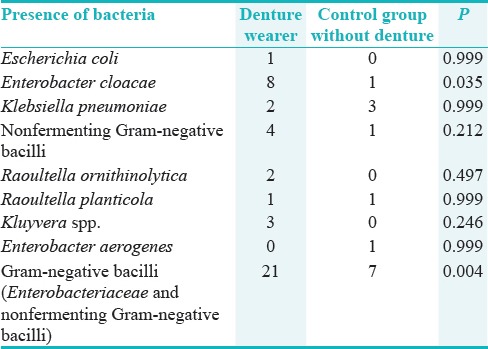
Except for Enterobacter cloacae isolate (P = 0.03), there was no significant difference between both groups for the presence of Escherichia coli, Klebsiella pneumoniae, nonfermenting Gram-negative bacilli, Raoultella ornithinolytica, Raoultella planticola, Kluyvera spp., and Enterobacter aerogenes. No significant correlation was noticed between age and presence of bacteria in the oral cavity. The Gram-negative rod bacteria were more in males, but the difference was not significant. When a total of Gram-negative rods were considered, there was a significant difference between case and control groups (P = 0.004).
Conclusions:
Based on our findings that nonoral pathogenic bacteria are detected from the saliva of the denture wearers, general and oral health measures in patients with removable dentures should be adopted to decrease the risk of cross infection.
KEYWORDS: Dental prosthesis, Gram-negative bacilli, nonoral pathogenic bacteria, oral cavity, saliva
INTRODUCTION
The normal microbial population included bacteria and fungi in the human oral cavity is very diverse.[1] Among all microbial strains, anaerobic Gram-negative bacteria and Streptococci (as Gram-positive bacteria) are the main types of human mouth's normal flora. Any alterations in this normal population affect the oral health because these microorganisms have pivotal roles in inhibiting of colonization of pathogenic microbiota.[1,2]
Complete or partial dentures are used by adults and elderly peoples in response to different factors that affect tooth extraction.[3,4] Dentures were shown to serve as a reservoir for oral bacteria and halitosis development that can be a concern for denture wearers.[5,6] Use of removable dental prosthesis induces some changes in the oral microbial population. In certain cases, this situation leads to dental prosthetic- or denture-associated stomatitis.[7]
Nonoral flora can cause diseases in patients who used contaminated denture or in technicians due to occupational hazards.[8] In two reports, colonization of denture materials with Candida albicans was identified as etiological cause of denture-associated stomatitis (sore mouth), which affects 24%–75% of denture wearers.[9,10,11]
Hence, new developments related to denture materials have been undertaken to decrease bacterial and yeast colonization to reduce denture stomatitis with appropriate denture hygiene.[12,13] Increased life span and dynamic development of prosthetic treatment resulted into an increase in the number of people using removable dentures for a long period that can be a potential pathogen factor for oral mucosa being in contact with this material. Prosthetic stomatopathy was reported in 20%–70% of patients with removable dentures.[14] Removable dentures have been proposed as a reservoir for pathogens to cause systemic infections.[15,16] Therefore, this study was conducted to determine the nonoral pathogenic bacteria in the oral cavity of patients with removable dentures.
MATERIALS AND METHODS
ETHICAL STATEMENT
The protocol of this study was approved by the Local Ethical Committee of Shiraz University of Medical Sciences (8819-1), and all participants signed informed consent before entering the study. All subjects were informed about the study. The demographic details in relation to age, sex, oral hygiene practice, and medical history of each participant were recorded.
REAGENTS
Eosin methylene blue (EMB), thioglycollate broth, blood agar, barium chloride, sulfuric acid, crystal violate, safranin, lugol solution, acetone, ethanol, oxidase, and catalase reagents were purchased from Merck (Germany). API20E kit was obtained from Biomerieux (France). All other chemicals were analytic grade and of commercially available.
PARTICIPANTS
In a cross-sectional study from January 2014 to October 2015, 100 saliva samples were provided from 50 men and 50 women with removable dentures (case group). They were wearing their present dentures at least for 1 year and all were admitted to the Department of Prosthodontics, Dental School, Shiraz University of Medical Sciences, Shiraz, Iran. The sampling method was convenience sampling. The exclusion criteria were systemic conditions that could affect the bacterial flora and any use of antibiotics before the study. Among them, 90 were without any systemic disease, and seven suffered from hypertension. Their systemic diseases were under control and they used related drugs routinely. A control group consisted of 100 age- and sex-matched participants having their own dentition (wearing no dentures) and all were admitted to other departments of dental school for routine checkups, scaling, or filling.
SALIVA SAMPLING AND MICROBIAL CULTURE
The unstimulated whole saliva was collected between 10 am and 12 pm and at least 60 min after the last intake of drink or food. The subjects were instructed to spit unstimulated saliva into sterile Falcon tubes containing 3 ml thioglycollate broth. Each sample was centrifuged at 12,500 rpm for 10 min and the supernatant was discarded. The precipitate was suspended in 1 ml of phosphate-buffered saline to obtain a concentrated sample suspension. One loop full of concentrated suspension was inoculated onto EMB and MacConkey agar culture media using a standard streak plate method. All culture plates were incubated at 37°C for 24 h, and the growth of bacteria was observed as pink- and white-colored colonies. The suspected colonies were subjected to Gram stain for identification of Gram-negative rod bacteria. Once identified, the colonies were further subjected to biochemical reactions by API20E Kit (Biomerieux).
STATISTICAL ANALYSIS
All data were analyzed using SPSS software (SPSS Ltd., Hong Kong). The Chi-square test was used to correlate the positive and negative cases with dentures. Two-independent sample t-test was used to compare the groups regarding gender and age. Statistically, significant difference was considered when P < 0.05.
RESULTS
The frequency of detected bacteria in relation to age in different groups is presented in Table 1. Except for Enterobacter cloacae isolate (P = 0.03), there was no significant difference between both groups for the presence of other bacteria. For Gram-negative rods, a significant difference was visible between case and control groups (P = 0.004). E. cloacae and Gram-negative bacilli (Enterobacteriaceae and nonfermenting) were significantly more visible in case group than the control group. There was no significant correlation between age and presence of bacteria in the oral cavity (P = 0.07). The Gram-negative rods were prevalent more in men than women but with no significant correlation between gender and presence of the nonoral pathogens (P = 0.08).
Table 1.
Presence of nonoral pathogens in saliva of removable denture wearer and nondenture wearing control groups
DISCUSSION
In the present study, the difference for microbial population in saliva samples between participants with removable dentures and the control group was compared revealing a variety of pathogens in removable dentures including Escherichia coli, Klebsiella pneumoniae, and Enterobacter aerogenes. E. cloacae and Gram-negative bacilli (Enterobacteriaceae and nonfermenting) were significantly more in case group than the control group. Potentially pathogenic bacteria, including Gram-negative bacilli of Acinetobacter, Pseudomonas, Moraxella Micrococcus, and Alcaligenes species were reported as sources of contamination in commercial dental laboratories.[17,18]
The number of studies on denture plaque is lower than those performed on dental plaque with controversies on similarity of microbial flora. It was shown that Bifidobacteria were seen in denture plaque at the same level to those of carious lesions and Bifidobacterium dentium cannot be sustained in an edentulous mouth.[19] The presence of Treponema denticola and Fusobacterium nucleatum in edentulous area and the oral hygiene status of the mucosal or denture surfaces were demonstrated to affect the colonization by the bacteria.[20]
A typical biofilm with morphology of columnar microcolonies surrounded by maxillary epithelial cells was previously reported during imaging.[21] Changes in the mouth condition in response to a denture can lead to lack of saliva accessibility and tongue-related mechanical cleaning.[22,23] In addition, dentures were shown to harbor a mixed species of bacterial biofilm.[24,25]
Dentures can play significant roles in harboring of pathogens that cause inhalation pneumonia.[26] Some unusual microorganisms such as Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae, Haemophilus parainfluenzae, E. coli, K. pneumoniae, Proteus mirabilis, E. cloacae, and Pseudomonas aeruginosa were shown to be isolated from dentures.[27]
An increase in pneumonia was reported in individuals working in dental laboratories and exposed to lathe aerosol.[17] Manipulation of Mycoplasma pneumoniae contaminated prostheses caused infection in 10 subjects working in dental prosthetic laboratories,[28] while all of these studies denote to the public importance of removable dentures.
The microbial strains which detected in implants and adjacent teeth at 10 years after implantation were periodontitis-related strains in 6.2%–78.4% of the implants. A significantly higher count was noted for Tannerella forsythia, Parvimonas micra, F. nucleatum/necrophorum, and Campylobacter rectus in implants than the other teeth. In comparison to whom with removable maxillary prosthesis, it was demonstrated that C. albicans was the most frequently isolated yeast species in both groups.[29]
K. pneumoniae was found as the dominant bacterial species in cases wearing removable maxillary prosthesis with and without denture stomatitis lesions.[30] It was shown that the normal microbial population of oral cavity changed with increase in age due to immune system alteration and further colonization with nonoral bacterial species such as Staphylococci and Enterobacteriaceae.[31,32]
In our study, E. coli was isolated just from one patient, and other Gram-negative rods were visible in remained denture wearing patients. Unusual oral cavity microorganisms have been previously isolated from dentures and were reported by other researchers.[33,34,35,36,37] Umeda et al. reported Helicobacter pylori in the oral cavity of a patient with periodontal pockets that existed even after extirpation of the bacterium from the stomach.[38]
The tongue surface was also evaluated by some researchers. It was shown that 43% of the individuals had the microorganisms on the tongue dorsum, which was more prevalent in the age range of 40–50 years and who had not consumed cigarette. However, they could not find any correlations between detected species and the presence of dentures, indicating that tongue can act as an initial reservoir of the microorganisms. In the present study, different nonoral pathogens were noted in 21 cases and 7 controls. It seems that finding the source of these species in other parts of the body and indication of those site as a reservoir for denture infection must be addressed in future studies.[11,35,39]
In the present study, there was no statistically significant difference for age and gender between patients and the control group. Similar results have been reported before by Agwu et al. in HIV-positive patients.[3] Our findings are in line with the above-mentioned study and indicated that wearing of removable dentures can be considered as a risk factor for colonization of different species of microbiota and with public health importance.
CONCLUSIONS
Based on the findings in the present study that nonoral pathogenic bacteria are detected from the saliva of the denture wearers, considering the possibility that the oral cavity may act as a potential origin of pathogenic species that may cause infection in other body sites, general and oral health measures in patients with removable dentures should be adopted to decrease the risk of cross-infection.
FINANCIAL SUPPORT AND SPONSORSHIP
We thank the Vice Chancellor of Shiraz University of Medical Sciences for the financial support of this research (Grant no. 98-01-21-8819-1).
CONFLICTS OF INTEREST
There are no conflicts of interest.
ACKNOWLEDGMENT
We thank the Vice Chancellor of Shiraz University of Medical Sciences for the financial support of this research (Grant no. 98-01-21-8819-1).
REFERENCES
- 1.Samaranayake L, Matsubara VH. Normal oral flora and the oral ecosystem. Dent Clin North Am. 2017;61:199–215. doi: 10.1016/j.cden.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 2.Aas JA, Paster BJ, Stokes LN, Olsen I, Dewhirst FE. Defining the normal bacterial flora of the oral cavity. J Clin Microbiol. 2005;43:5721–32. doi: 10.1128/JCM.43.11.5721-5732.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agwu E, Ihongbe JC, Ezeonwumelu JO, Lodhi MM. Baseline burden and antimicrobial susceptibility of pathogenic bacteria recovered from oral lesions of patients with HIV/AIDS in South-Western Uganda. Oral Sci Int. 2015;12:59–66. [Google Scholar]
- 4.Khorshidi H, Moaddeli MR, Golkari A, Heidari H, Raoofi S. The prevalence of pathologic tooth migration with respect to the severity of periodontitis. J Int Soc Prev Community Dent. 2016;6(Suppl 2):S122–5. doi: 10.4103/2231-0762.189738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu T, He X, Lu H, Bradshaw DJ, Axe A, Loewy Z, et al. Development of in vitro denture biofilm models for halitosis related bacteria and their application in testing the efficacy of antimicrobial agents. Open Dent J. 2015;9:125–31. doi: 10.2174/1874210601509010125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Geest S, Laleman I, Teughels W, Dekeyser C, Quirynen M. Periodontal diseases as a source of halitosis: A review of the evidence and treatment approaches for dentists and dental hygienists. Periodontol 2000. 2016;71:213–27. doi: 10.1111/prd.12111. [DOI] [PubMed] [Google Scholar]
- 7.Pinke KH, Freitas P, Viera NA, Honório HM, Porto VC, Lara VS. Decreased production of proinflammatory cytokines by monocytes from individuals presenting Candida-associated denture stomatitis. Cytokine. 2016;77:145–51. doi: 10.1016/j.cyto.2015.10.017. [DOI] [PubMed] [Google Scholar]
- 8.Agostinho AM, Miyoshi PR, Gnoatto N, Paranhos Hde F, Figueiredo LC, Salvador SL. Cross-contamination in the dental laboratory through the polishing procedure of complete dentures. Braz Dent J. 2004;15:138–43. doi: 10.1590/s0103-64402004000200010. [DOI] [PubMed] [Google Scholar]
- 9.Webb BC, Thomas CJ, Willcox MD, Harty DW, Knox KW. Candida-associated denture stomatitis. Aetiology and management: A review. Part 2 Oral diseases caused by Candida species. Aust Dent J. 1998;43:160–6. doi: 10.1111/j.1834-7819.1998.tb00157.x. [DOI] [PubMed] [Google Scholar]
- 10.Barbeau J, Séguin J, Goulet JP, de Koninck L, Avon SL, Lalonde B, et al. Reassessing the presence of Candida albicans in denture-related stomatitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:51–9. doi: 10.1067/moe.2003.44. [DOI] [PubMed] [Google Scholar]
- 11.Moosazadeh M, Akbari M, Tabrizi R, Ghorbani A, Golkari A, Banakar M. Denture stomatitis and Candida albicans in Iranian population: A systematic review and meta-analysis. J Dent (Shiraz) 2016;17(3 Suppl):283–92. [PMC free article] [PubMed] [Google Scholar]
- 12.Gendreau L, Loewy ZG. Epidemiology and etiology of denture stomatitis. J Prosthodont. 2011;20:251–60. doi: 10.1111/j.1532-849X.2011.00698.x. [DOI] [PubMed] [Google Scholar]
- 13.Yarborough A, Cooper L, Duqum I, Mendonça G, McGraw K, Stoner L. Evidence regarding the treatment of denture stomatitis. J Prosthodont. 2016;25:288–301. doi: 10.1111/jopr.12454. [DOI] [PubMed] [Google Scholar]
- 14.Sobolewska E, Fraczak B, Czarnomysy-Furowicz D, Ey-Chmielewska H, Karakulska J. Bacteria adhesion to the surface of various prosthetics materials. Ann Acad Med Stetin. 2007;53:68–71. [PubMed] [Google Scholar]
- 15.Le Bars P, Kouadio AA, N'goran JK, Badran Z, Soueidan A. Relationship between removable prosthesis and some systemics disorders. J Indian Prosthodont Soc. 2015;15:292–9. doi: 10.4103/0972-4052.171828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Przybylowska D, Mierzwinska-Nastalska E, Swoboda-Kopec E, Rubinsztajn R, Chazan R. Potential respiratory pathogens colonisation of the denture plaque of patients with chronic obstructive pulmonary disease. Gerodontology. 2016;33:322–7. doi: 10.1111/ger.12156. [DOI] [PubMed] [Google Scholar]
- 17.Williams HN, Falkler WA, Jr, Hasler JF, Libonati JP. The recovery and significance of nonoral opportunistic pathogenic bacteria in dental laboratory pumice. J Prosthet Dent. 1985;54:725–30. doi: 10.1016/0022-3913(85)90260-4. [DOI] [PubMed] [Google Scholar]
- 18.Nair VV, Karibasappa GN, Dodamani A, Prashanth VK. Microbial contamination of removable dental prosthesis at different interval of usage: An in vitro study. J Indian Prosthodont Soc. 2016;16:346–51. doi: 10.4103/0972-4052.176536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mantzourani M, Gilbert SC, Fenlon M, Beighton D. Non-oral bifidobacteria and the aciduric microbiota of the denture plaque biofilm. Mol Oral Microbiol. 2010;25:190–9. doi: 10.1111/j.2041-1014.2009.00565.x. [DOI] [PubMed] [Google Scholar]
- 20.Yasui M, Ryu M, Sakurai K, Ishihara K. Colonisation of the oral cavity by periodontopathic bacteria in complete denture wearers. Gerodontology. 2012;29:e494–502. doi: 10.1111/j.1741-2358.2011.00506.x. [DOI] [PubMed] [Google Scholar]
- 21.Verran J. Malodour in denture wearers: An ill-defined problem. Oral Dis. 2005;11(Suppl 1):24–8. doi: 10.1111/j.1601-0825.2005.01083.x. [DOI] [PubMed] [Google Scholar]
- 22.Kobayashi K, Ryu M, Izumi S, Ueda T, Sakurai K. Effect of oral cleaning using mouthwash and a mouth moisturizing gel on bacterial number and moisture level of the tongue surface of older adults requiring nursing care. Geriatr Gerontol Int. 2017;17:116–21. doi: 10.1111/ggi.12684. [DOI] [PubMed] [Google Scholar]
- 23.Ghapanchi J, Kamali F, Moattari A, Poorshahidi S, Shahin E, Rezazadeh F, et al. In vitro comparison of cytotoxic and antibacterial effects of 16 commercial toothpastes. J Int Oral Health. 2015;7:39–43. [PMC free article] [PubMed] [Google Scholar]
- 24.Koopmans AS, Kippuw N, de Graaff J. Bacterial involvement in denture-induced stomatitis. J Dent Res. 1988;67:1246–50. doi: 10.1177/00220345880670091901. [DOI] [PubMed] [Google Scholar]
- 25.Shi B, Wu T, McLean J, Edlund A, Young Y, He X, et al. The denture-associated oral microbiome in health and stomatitis. mSphere. 2016;1:pii: E00215-16. doi: 10.1128/mSphere.00215-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Daniluk T, Fiedoruk K, Sciepuk M, Zaremba ML, Rozkiewicz D, Cylwik-Rokicka D, et al. Aerobic bacteria in the oral cavity of patients with removable dentures. Adv Med Sci. 2006;51(Suppl 1):86–90. [PubMed] [Google Scholar]
- 27.Goldberg S, Cardash H, Browning H, 3rd, Sahly H, Rosenberg M. Isolation of Enterobacteriaceae from the mouth and potential association with malodor. J Dent Res. 1997;76:1770–5. doi: 10.1177/00220345970760110801. [DOI] [PubMed] [Google Scholar]
- 28.Sande MA, Gadot F, Wenzel RP. Point source epidemic of Mycoplasma pneumoniae infection in a prosthodontics laboratory. Am Rev Respir Dis. 1975;112:213–7. doi: 10.1164/arrd.1975.112.2.213. [DOI] [PubMed] [Google Scholar]
- 29.Eick S, Ramseier CA, Rothenberger K, Brägger U, Buser D, Salvi GE. Microbiota at teeth and implants in partially edentulous patients. A 10-year retrospective study. Clin Oral Implants Res. 2016;27:218–25. doi: 10.1111/clr.12588. [DOI] [PubMed] [Google Scholar]
- 30.Pereira CA, Toledo BC, Santos CT, Pereira Costa AC, Back-Brito GN, Kaminagakura E, et al. Opportunistic microorganisms in individuals with lesions of denture stomatitis. Diagn Microbiol Infect Dis. 2013;76:419–24. doi: 10.1016/j.diagmicrobio.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 31.Percival RS, Challacombe SJ, Marsh PD. Age-related microbiological changes in the salivary and plaque microflora of healthy adults. J Med Microbiol. 1991;35:5–11. doi: 10.1099/00222615-35-1-5. [DOI] [PubMed] [Google Scholar]
- 32.Fure S. Five-year incidence of caries, salivary and microbial conditions in 60-, 70- and 80-year-old Swedish individuals. Caries Res. 1998;32:166–74. doi: 10.1159/000016449. [DOI] [PubMed] [Google Scholar]
- 33.Sumi Y, Miura H, Michiwaki Y, Nagaosa S, Nagaya M. Colonization of dental plaque by respiratory pathogens in dependent elderly. Arch Gerontol Geriatr. 2007;44:119–24. doi: 10.1016/j.archger.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 34.Lamfon H, Al-Karaawi Z, McCullough M, Porter SR, Pratten J. Composition of in vitro denture plaque biofilms and susceptibility to antifungals. FEMS Microbiol Lett. 2005;242:345–51. doi: 10.1016/j.femsle.2004.11.032. [DOI] [PubMed] [Google Scholar]
- 35.O'Donnell LE, Smith K, Williams C, Nile CJ, Lappin DF, Bradshaw D, et al. Dentures are a reservoir for respiratory pathogens. J Prosthodont. 2016;25:99–104. doi: 10.1111/jopr.12342. [DOI] [PubMed] [Google Scholar]
- 36.Sedghizadeh PP, Mahabady S, Allen CM. Opportunistic oral infections. Dent Clin North Am. 2017;61:389–400. doi: 10.1016/j.cden.2016.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Silva SS, Ribeiro MO, Gomes FI, Chaves HV, Silva AA, Zanin IC, et al. Occurrence and antimicrobial susceptibility of enteric rods and pseudomonads isolated from the dental prostheses biofilm. J Appl Oral Sci. 2016;24:462–71. doi: 10.1590/1678-775720160032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Umeda M, Komatsubara H, Minamikawa T, Furudoi S, Shibuya Y, Yokoo S, et al. A questionnaire on requests for disclosure of diagnosis, self-choice of treatment, and second opinion of patients with oral cancer in Japan. J Palliat Care. 2003;19:206–8. [PubMed] [Google Scholar]
- 39.Conti S, dos Santos SS, Koga-Ito CY, Jorge AO. Enterobacteriaceae and pseudomonadaceae on the dorsum of the human tongue. J Appl Oral Sci. 2009;17:375–80. doi: 10.1590/S1678-77572009000500005. [DOI] [PMC free article] [PubMed] [Google Scholar]


