Abstract
This paper compares black-white health disparities among prisoners to disparities in the noninstitutionalized community to provide a more complete portrait of the nation’s heath. We use data from the 2004 Survey of Inmates in State and Federal Correctional Facilities and the 2002 and 2004 National Health and Nutrition Examination Survey for incarcerated and noninstitutionalized adult (aged 18–65) men and women, respectively. Health disparities between black and white male prisoners based on self-reported prevalence are similar to disparities in the general population for hypertension and diabetes but significantly reduced for kidney problems and stroke. Health disparities between black and white female prisoners are similar to disparities in the general population for obesity but significantly reduced for hypertension, diabetes, heart problems, kidney problems, and stroke. Our study reveals that prisoners report far worse health profiles than non-prisoners but there is differential health selection into prison for whites and blacks, and population health estimates for adult black men in particular underreport the true health burden for U.S. adults. Our findings highlight the importance of incorporating prison populations in demographic and public health analyses.
Keywords: Health disparities, Population health, Prison, NHANES
Highlights
-
•
Inmates have poorer health overall than the noninstitutionalized population, but more so for white women demonstrating a differential health selection into prison.
-
•
Health problems increase when inmates are included in national health statistics, especially for black men.
-
•
U.S. health statistics may underestimate the health of the nation with potential consequences for understanding racial health disparities.
-
•
Properly characterizing population health and health disparities requires the inclusion of incarcerated adults in mainstream epidemiologic studies.
1. Introduction
A large body of population health research examines adult health disparities, especially black-white differences in mortality and morbidity (Adler and Rehkopf, 2008, Frisbie et al., 2004, Geruso, 2012, Pampel et al., 2010, Williams and Jackson, 2005, Williams and Mohammed, 2009). Yet, incarceration is an often ignored and poorly understood factor in health disparities research (Moore & Elkavich, 2008) in part because incarcerated persons are excluded from national health surveys (Ahalt, Binswanger, Steinman, Tulsky, & Williams, 2011) and clinical research (Wang & Wildeman, 2011), former inmates are often not identified in national health surveys (Ahalt et al., 2011), and research among prisoners is difficult due to a long history of medical abuses (Gostin, 2007). Inmates report a higher prevalence of infectious diseases and chronic conditions compared to the noninstitutionalized population (Baillargeon et al., 2000, Hammett et al., 2002, Solomon et al., 2004, Wilper et al., 2009). This is largely due to the selection of prisoners from the most vulnerable segments of the U.S. population (Clear, 2007, Greenfeld and Snell, 1999, Kirk, 2008, Richie, 2001, Fazel and Danesh, 2002, James and Glaze, 2006, Steadman et al., 2009), although there is evidence to suggest a potential causal relationship (Massoglia, 2008a, Porter, 2014, Schnittker and John, 2007). Thus, incarceration is a pressing public health concern affecting not only incarcerated persons, but also their families and communities (Brinkley-Rubenstein, 2013, Dumont et al., 2012, Massoglia and Pridemore, 2015, Schnittker et al., 2015, Turney, 2017). There are also potential macro-level consequences for U.S. society (Wildeman, 2016).
We argue that due to mass incarceration, at any given time large portions of the population are “missing” from the noninstitutionalized community and, therefore, from national health surveillance systems. The consequences are that current estimates of population health and health disparities may be biased, and that we cannot fully understand the consequences of mass incarceration on racial health disparities (Wildeman & Wang, 2017). In other words, excluding information about residents of institutional—and non-institutional—group quarters can bias population estimates (Stapleton, Honeycutt, & Schechter, 2011). But more importantly, the failure to report estimates from institutionalized individuals limits our ability to fully describe the complexity of health disparities in the United States (Ahalt et al., 2011, Wang and Wildeman, 2011).
1.1. Prisons and disparities
The effect of incarceration on racial/ethnic health disparities has been theorized (Asad and Clair, 2017, Binswanger et al., 2011), but there have been limited empirical examinations. In a recent review article, five studies were identified that directly assessed this question—all generally supporting the hypothesis that mass incarceration explains some of the racial/ethnic health disparities documented in the United States (Wildeman & Muller, 2012). For example, Wang & Green (2010) used a population-based survey of non-institutionalized adults in New York City and propensity score matching to examine the association between incarceration and chronic diseases. They found that individuals with a history of incarceration had a higher prevalence of asthma and that the increased rates of incarceration among blacks partially contributed to racial disparities in asthma prevalence.
Theoretically, comparing disparities among incarcerated and non-institutionalized populations may provide valuable insights into the relevance for five common explanations for health disparities: (1) stress and discrimination, (2) health lifestyles, (3) health care access and utilization, (4) childhood poverty, and (5) neighborhood and work environments (Adler and Rehkopf, 2008, Williams and Jackson, 2005, Williams and Mohammed, 2009). Correctional institutions are multiracial, unsegregated settings that create more similar environments for black and white prisoners which render the above explanations less-applicable. For example, prisoners have similar physical housing environments, the same limited food choices, access to the same types and duration of physical activity, and access to legally-mandated healthcare regardless of racial identification. Prisons have been described as total institutions – “places of residence and work where a large number of like-situated individuals, cut off from the wider society for an appreciable period of time, together lead an enclosed, formally administered round of life” (Goffman, 1961, p. xii). Thus, prisons provide an important context because they “level the playing field” with respect to nutrition, exercise, health care access, and stress exposure, although evidence suggests that racial/ethnic disparities in utilization of care may exist even in this “equal access” system (Nowotny, 2015). We are not suggesting that there is no stress exposure within prisons. Indeed, prisoners are exposed to multiple chronic and acute stressors (see Massoglia, 2008a). Rather, our point is that black and white prisoners are likely exposed to the same levels of stress because of the structure of prison life and, as a result, the effects of imprisonment are likely to be the same across racial groups (Massoglia, 2008b, Roettger and Swisher, 2011).
Given the growth of the incarcerated population and the overrepresentation of black adults within prisons, describing disparities within prisons and comparing them to the noninstitutionalized population will also shed light on the consequences of excluding 2.4 million individuals from population health research (Wagner & Sakala, 2014). Understanding the health of current and former inmates has been identified as one element of a comprehensive strategy to improve the health of urban communities by reducing population health disparities (Binswanger et al. 2011). Yet, knowledge about who is removed from and returned to the community, and how these selective forces are different for black and white communities is critically lacking in health disparities research (Wildeman & Wang, 2017).
Estimates of lifetime incarceration predict that 1 in 12 Americans will be incarcerated at some point in their lives (Bonzcar, 2003). For blacks, estimates are higher, at 1 in 3. And at any given time, 1 in 9 black men aged 20 to 34 are in prison (Western, 2006) with a 28% cumulative risk for incarceration for black men by the age of 34 and a 68% cumulative risk for those with less than a high school education (Pettit, 2012). Importantly, surveys that draw their samples from households exclude inmates by definition. Therefore, these “point in time” incarceration estimates provide insight on who is excluded (Pettit, 2012). These estimates “only partially represent the total number of people at risk for undersampling in conventional surveys [because] former inmates may be particularly likely to be excluded from social surveys that sample from households because they have high rates of residential mobility, instability, and homelessness” (Pettit, 2012, p. 16). Due to high rates of incarceration, black men are also more likely to drop out of prospective longitudinal surveys. For example, black men who experience incarceration spend 13.4 percent of their working lives in prison (Patterson & Wildeman, 2015). The high percentages of current and lifetime risk for incarceration make it likely that excluding prisoners and recently released prisoners from health surveillance systems will bias population estimates, especially for black men. Western (2006) demonstrates this by adjusting national statistics for imprisonment. He finds that black-white inequalities in joblessness, education, and wages are larger. Thus, the gap in economic progress among blacks is less optimistic than official statistics suggest. We speculate that this is also the case with health disparities. In other words, “the loss of black men from medical research due to incarceration may produce biased, underpowered estimates in studies of health disparities” (Wang & Wildeman, 2011, p. 1708).
Some recent research on mortality and morbidity indicates that the association between race/ethnicity and health may operate differently within prisons than in the general community (see Massoglia & Pridemore, 2015). For example, there are significant black-white gaps in life expectancy in the United States for the noninstitutionalized population (Harper et al., 2007, Hummer, 1996, Hummer et al., 1999, Warner and Hayward, 2006) but there is increasing evidence that prison has a protective effect on mortality for black men. Mumola (2007) found that the mortality rate for black male prisoners (aged 15–64) was 19 percent lower than for black men in the noninstitutionalized population. A study of prisoners in North Carolina found 48 percent fewer deaths than expected among black prisoners (Rosen, Wohl, & Schoenbach, 2011). Patterson (2010) found that the mortality rate for white male prisoners was higher than the rate for white males in the noninstitutionalized population, whereas the mortality rate for black male prisoners was lower than the rate for black males in the noninstitutionalized population. The lower death rate for black male prisoners was largely, but not entirely accounted for by protections from external causes of death. It is important to note, however, that any mortality benefit may be outweighed by long-term consequences. For example, Patterson (2013) used mortality data from New York State and found a dose-response effect. Each additional year of incarceration produced a 16 percent increase in the odds of death and a 2-year decrease in life expectancy.
When examining morbidity using pooled national data, Binswanger, Krueger & Steiner (2009) found that hypertension is higher among incarcerated whites compared to noninstitutionalized whites while no differences were found among incarcerated blacks and Hispanics compared to their noninstitutionalized counterparts. Similarly, Houle (2011) found that the exclusion of inmates from national obesity estimates leads to an overestimation in obesity prevalence particularly for disadvantaged white and black men.
Collectively, the results of previous research highlight the differential selection among racial and ethnic minorities into the prison system. This research supports the hypothesis that racial health disparities in morbidity and mortality among prisoners are muted. In fact, the health of black prisoners may be more likely to reflect the health of the noninstitutionalized black population whereas white prisoners may be drawn from some of the unhealthiest whites in the population. As such, noninstitutionalized disparities may be smaller, nonexistent, or reversed among prisoners. To date, no existing work has explicitly compared estimates of health disparities among incarcerated adults with comparable estimates from the general population of adults in the United States.
1.2. Study aims
The objective of this paper is to determine the patterns of black-white health disparities within prisons, and how they differ from noninstitutionalized community settings. If there is no health bias in the selection of individuals into prison, then the race disparities documented for the noninstitutionalized population will be comparable to the disparities in the prison setting so that black prisoners have worse health than white prisoners. But given what we know about the racialized and gendered selection of adults into prison, we expect health disparities to be either neutralized or significantly reduced. Specifically, disparities will be smaller within prisons due to the selection of the least healthy whites into prison but very little health selection among black prisoners. Due to the social processes associated with incarceration (Beckett et al., 2006, Bridges and Steen, 1998, Steffensmeier et al., 1998, Wakefield and Uggen, 2010; Wildeman & Muller, 2012), younger adults, males, and racial and ethnic minorities are overrepresented within prisons. Therefore, we expect that whites will represent a highly select group of individuals and they will have worse health than their noninstitutionalized counterparts.
2. Materials and methods
2.1. Data
We examine comparable indicators of physical health using two large and nationally representative cross-sectional samples of adults within and outside of prisons (Binswanger et al., 2009, Wilper et al., 2009). First, the 2004 Bureau of Justice Statistics (BJS) Survey of Inmates in State and Federal Correctional Facilities (SPI) provides a nationally-representative sample of persons incarcerated in prisons similar to previous studies (United States Department of Justice Bureau of Justice Statistics, 2007). The sample design for state inmates employed a stratified, two-stage selection: 301 prisons were randomly selected for inclusion in the study and 287 prisons participated. Prisoners were then randomly selected for participation. A total of 14,499 prisoners participated, for an overall response rate of 89.1%. The sampling design for federal inmates includes a universe of 131 male prisons and 17 female prisons. In total, 32 male and 8 female facilities were selected for inclusion. Nondrug offenders were oversampled to ensure large enough numbers to be analyzed. The final sample size was 3686. The survey asks respondents about their incarceration history, offense characteristics, family and background characteristics, drug and alcohol use and abuse, prison activities, and self-reported health, mental health, and treatment history.
Second, the National Health and Nutrition Examination Survey (NHANES), which is designed to assess the health and nutritional status of U.S. adults and children, provides a nationally-representative sample of the noninstitutionalized population (National Center for Health Statistics NCHS, 2002, 2004). We pooled two waves from 2001–2002 and 2003–2004 (time periods roughly comparable to the data collection period for the SPI) to create a similar sample size to the SPI. The 2001–2002 total sample size is 11,039, with a response rate of 84%; the 2003–2004 total sample size is 10,122, with a response rate of 79%. The interview includes demographic, socioeconomic, dietary, and self-reported health as well as the results of medical and laboratory examinations. The final pooled sample of respondents aged 18 to 65 who identified as non-Hispanic white or black is 18,266, including 12,237 incarcerated and 6029 noninstitutionalized adults.
2.2. Measures
Age is measured as a continuous variable ranging from 18 to 65. Three age categories are also assessed: 18–33, 34–49, and 50–65. Dichotomous variables include sex (0 female, 1 male), race (0 non-Hispanic white, 1 non-Hispanic black), and inmate status. Education is included as a control given its strong association with health (Link and Phelan, 1995, Phelan et al., 2010) and racial health disparities (e.g., Hayward, Miles, Crimmins, & Yang, 2000). Categories include less than high school, high school/GED, and more than high school. GED attainment is coded for degree obtained inside or outside of the correctional facility. Incarcerated adults are younger and are overrepresented by men and blacks. The prison sample has a mean age of 35.6 with 89% males compared to a mean age of 40.4 and 49% males in the noninstitutionalized sample. The incarcerated sample is 46% white and 54% black compared to 85% and 15%, respectively, in the noninstitutionalized sample. The prisoners in the study also have lower levels of education than the general population.
We assess 10 health conditions. In both data sets, respondents were asked to self-report lifetime diagnosis with health conditions. Specifically, SPI asked, “Have you ever had…?” and NHANES asked, “Has a doctor or other health professional ever told you that you had…?” Cardiovascular risk is identified by four conditions: hypertension or high blood pressure, diabetes, obesity, and heart problems. Self-reported height and weight are used to calculate BMI (weight (lb) / [height (in)]2 x 703). Obesity is then constructed using the established CDC cutoff of a BMI of 30.0 or more (Ogden, Carroll, Kit & Flegal, 2014). The remaining conditions include asthma, kidney problems, stroke, arthritis, all-cause cancer, and sexually transmitted infections (STI).
2.3. Statistical analysis
Missing values were imputed using chained equations. The first analysis reports the disparity between black and white adults for each physical health problem across age strata using predicted probabilities. Accordingly, the sampling weights were mean centered with respect to each population. Analyses are also stratified by sex because the population of incarcerated women is more select than incarcerated men and is determined by a unique pathway (Belknap & Holsinger, 2006), and the prison context differs by sex such that incarcerated women have less access to health services while they are incarcerated (Eliason, Taylor & Williams, 2004). Second, we estimate models separately for incarcerated and noninstitutionalized populations using logistic regression with the respective mean centered weights controlling for age and education. Adjusted odds ratios and 95% confidence intervals are reported for each health condition.
To examine statistical significance for the differences between incarcerated and noninstitutionalized populations, we combine the data sets and include an interaction term (race X incarcerated status) to test whether incarceration modifies race disparities in health. We mean centered the full distribution of sampling weights. In this manner, the relatively smaller population of prisoners and the design effects of each respective study are accounted for when characterizing the standard errors for the interaction term between race and incarceration status for each health problem. Only the p-value associated with the interaction term is reported. We estimated the same models using linear probability models as a sensitivity test and found similar results. In the third analysis, frequency weights are used to estimate the number of adults in the population with each morbidity. We first estimate the noninstitutionalized population at risk for black and white women and men. We then estimate the populations to see how the prevalence of health conditions would change if the adult prison population was included. All analyses are conducted using Stata 13 (StataCorp, 2013).
3. Results
Table 1 provides the prevalence for each health condition across age strata and stratified by sex, race, and incarceration status. For most health conditions prisoners report worse health than their noninstitutionalized counterparts, and the differences are larger for whites than blacks. For example, 12.9% of white male prisoners report heart problems compared to 4.9% in the general population, whereas 7.5% of black male prisoners report hypertension compared to 4.2% in the general population. White women experience an even more dramatic increase in the prison sample (13.3% vs. 2.8%) whereas black women experience a smaller increase (9.5% vs. 4.5%). The largest disparity among the incarcerated populations is the risk of sexually transmitted infection (STI), in which there is no significant race difference among non-institutionalized men and a 3.2% point difference among noninstitutionalized women, but a large difference among prisoners. For example, 34.9% of black male prisoners report STI compared to 23.8% of white males; these numbers are 20.1% and 13.4% for black and white female prisoners, respectively.
Table 1.
Predicted Probability (%) of Health Conditions among Incarcerated and Noninstitutionalized Adults Stratified by Sex and Race.
|
Panel A. Men |
Panel B. Women |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Incarcerated |
Noninstitutionalized |
Incarcerated |
Noninstitutionalized |
|||||||||
| White | Black | p | White | Black | p | White | Black | p | White | Black | p | |
| Hypertension | 24.3 (20.2, 28.4) | 22.7 (19.5, 26.0) | 22.6 (20.6, 24.6) | 25.8 (22.7, 28.9) | 20.9 (18.2, 23.5) | 27.0 (23.8, 30.2) | ** | 21.1 (19.2, 23.1) | 31.8 (28.7, 35.0) | *** | ||
| Age 18–33 | 15.7 (9.2, 22.1) | 15.4 (11.5, 19.3) | 10.2 (7.7, 12.7) | 11.7 (7.9, 15.6) | 15.1 (11.4, 18.9) | 16.8 (12.7, 20.8) | 8.5 (6.2, 10.9) | 14.3 (10.5, 18.2) | ** | |||
| Age 34–49 | 19.7 (14.2, 25.1) | 25.2 (19.8, 30.6) | 21.1 (17.7, 24.4) | 23.3 (18.4, 28.1) | 22.2 (18.5, 26.0) | 31.0 (26.2, 35.7) | ** | 17.6 (14.4, 20.7) | 33.5 (28.2, 38.8) | *** | ||
| Age 50+ | 45.9 (35.5, 56.2) | 52.5 (39.2, 65.7) | 38.6 (34.5, 42.8) | 55.3 (48.3, 62.3) | *** | 47.5 (35.8, 59.2) | 66.4 (52.9, 80.0) | * | 39.9 (35.8, 43.9) | 62.0 (55.3, 68.8) | *** | |
| Diabetes | 6.0 (3.6, 8.4) | 5.4 (3.5, 7.2) | 5.0 (3.9, 6.0) | 7.2 (5.4, 8.9) | * | 7.2 (5.5, 8.5) | 5.5 (3.9, 7.1) | 3.9 (3.0, 4.8) | 9.6 (7.7, 11.5) | *** | ||
| Age 18–33 | 0.2 (0.1, 0.3) | 1.8 (0.3, 3.3) | *** | 0.1 (0.0, 0.1) | 0.1 (0.0, 0.2) | 5.1 (2.9, 7.3) | 3.1 (1.2, 5.0) | 1.0 (0.2, 1.7) | 2.1 (0.6, 3.7) | |||
| Age 34–49 | 4.1 (1.4, 6.8) | 4.9 (2.2, 7.6) | 4.1 (2.5, 5.7) | 4.2 (2.0, 6.5) | 8.1 (5.7, 10.6) | 6.1 (3.8, 8.5) | 2.7 (1.4, 4.1) | 9.6 (6.3, 12.8) | *** | |||
| Age 50+ | 17.7 (9.2, 26.3) | 26.8 (14.7, 38.9) | 11.2 (8.5, 13.9) | 23.6 (17.6, 29.7) | *** | 13.7 (5.5, 21.9) | 17.5 (7.0, 27.9) | 8.7 (6.2, 11.1) | 23.6 (17.9, 29.4) | *** | ||
| Obesity | 18.0 (14.4, 21.7) | 27.7 (24.3, 31.2) | *** | 27.4 (25.3, 29.6) | 25.8 (22.7, 28.9) | 22.9 (20.2, 25.7) | 40.9 (37.3, 44.5) | *** | 26.5 (24.4, 28.7) | 45.0 (41.6, 48.5) | *** | |
| Age 18–33 | 16.1 (9.4, 22.7) | 24.6 (19.9, 29.4) | 20.2 (16.8, 23.5) | 22.7 (17.9, 27.4) | 21.9 (17.7, 26.2) | 35.5 (30.0, 41.0) | *** | 17.8 (14.6, 21.1) | 39.1 (33.7, 44.5) | *** | ||
| Age 34–49 | 16.2 (11.3, 21.1) | 32.2 (26.5, 38.0) | *** | 29.5 (25.7, 33.2) | 25.4 (20.3, 30.5) | *** | 23.7 (19.8, 27.6) | 45.9 (40.8, 51.1) | *** | 29.1 (25.3, 32.8) | 47.2 (41.6, 52.8) | *** |
| Age 50+ | 23.9 (15.1, 32.7) | 26.2 (14.8, 37.6) | 32.7 (28.7, 36.8) | 32.0 (25.5, 38.5) | 23.6 (13.7, 33.5) | 35.0 (21.9, 48.0) | 32.7 (28.7, 36.7) | 52.3 (45.5, 59.2) | *** | |||
| Heart Problems | 12.9 (9.7, 16.1) | 7.5 (5.4, 9.7) | ** | 4.9 (3.9, 5.9) | 4.2 (2.9, 5.6) | 13.3 (11.0, 15.5) | 9.5 (7.4, 11.7) | * | 2.8 (2.1, 3.6) | 4.5 (3.2, 5.9) | * | |
| Age 18–33 | 3.5 (0.5, 6.5) | 4.9 (2.6, 7.3) | 0.5 (0.0, 1.0) | 0.5 (0.0, 1.3) | 7.7 (4.9, 10.5) | 6.2 (3.4, 9.1) | 0.1 (0.0, 0.4) | 0.8 (0.0, 01.8) | ||||
| Age 34–49 | 11.9 (7.3, 16.5) | 8.3 (4.7, 11.9) | 2.5 (1.2, 3.7) | 3.3 (1.2, 5.3) | 15.8 (12.4, 19.2) | 10.7 (7.5, 13.8) | * | 1.9 (0.8, 2.9) | 4.1 (1.9, 6.3) | * | ||
| Age 50+ | 27.1 (17.9, 36.4) | 18.1 (7.3, 28.9) | 13.3 (10.5, 16.1) | 12.6 (8.1, 17.1) | 29.3 (18.7, 39.3) | 22.9 (10.3, 35.4) | 7.1 (5.0, 9.2) | 12.5 (8.1, 17.0) | * | |||
| Asthma | 10.2 (7.4, 13.1) | 13.4 (10.8, 16.1) | 11.2 (9.7, 12.7) | 12.7 (10.4, 15.0) | 21.8 (19.2, 14.5) | 21.6 (18.6, 24.6) | 15.0 (13.3, 16.8) | 14.1 (11.7, 16.4) | ||||
| Age 18–33 | 12.2 (6.5, 17.8) | 13.6 (9.9, 17.3) | 14.6 (11.7, 17.5) | 15.8 (11.8, 19.9) | 21.6 (17.5, 25.8) | 21.7 (17.1, 26.3) | 15.8 (12.8, 18.8) | 16.5 (12.5, 20.4) | ||||
| Age 34–49 | 9.9 (5.8, 14.0) | 13.7 (9.4, 18.1) | 8.2 (6.0, 10.5) | 10.4 (6.8, 14.0) | 22.7 (18.9, 26.4) | 21.8 (17.7, 25.9) | 14.8 (11.9, 17.7) | 10.6 (7.1, 14.1) | ||||
| Age 50+ | 8.5 (2.7, 14.3) | 11.2 (2.6, 19.8) | 11.6 (8.8, 14.3) | 10.8 (6.6, 15.1) | 16.7 (8.4, 25.0) | 19.5 (7.9, 31.1) | 14.5 (11.6, 17.4) | 15.9 (10.9, 21.0) | ||||
| Kidney Problems | 7.7 (5.2, 10.3) | 3.9 (2.4, 5.4) | ** | 1.1 (0.6, 1.6) | 2.9 (1.8, 4.0) | *** | 14.4 (12.0, 16.7) | 9.9 (7.5, 12.2) | ** | 1.3 (0.8, 1.8) | 3.0 (1.8, 4.1) | ** |
| Age 18–33 | 5.2 (1.3, 9.1) | 3.4 (1.4, 5.4) | ** | 0.7 (0.1, 2.3) | 0.0 (0.0, 0.0) | * | 13.4 (9.9, 16.9) | 8.4 (5.1, 11.8) | 1.3 (0.4, 2.3) | 1.4 (0.1, 2.7) | ||
| Age 34–49 | 5.6 (2.4, 8.8) | 4.4 (1.8, 7.0) | 0.6 (0.0, 1.1) | 4.2 (1.9, 6.6) | *** | 14.7 (11.4, 18.1) | 9.9 (6.6, 13.1) | * | 0.7 (0.6, 1.3) | 2.8 (1.0, 4.5) | * | |
| Age 50+ | 16.1 (8.2, 23.9) | 4.8 (0.0, 10.6) | 2.2 (1.0, 3.4) | 5.6 (2.6, 8.6) | * | 17.7 (9.2, 26.2) | 21.3 (8.4, 34.3) | 2.2 (1.1, 3.4) | 6.0 (2.8, 9.3) | * | ||
| Stroke | 5.8 (3.5, 8.2) | 2.7 (1.4, 4.0) | * | 1.0 (0.5, 1.4) | 1.8 (1.0, 2.6) | 6.8 (5.2, 8.4) | 3.5 (2.2, 4.8) | ** | 1.6 (1.0, 2.2) | 2.8 (1.7, 3.9) | * | |
| Age 18–33 | 4.7 (0.9, 8.4) | 1.2 (0.0, 2.5) | * | 0.7 (0.1, 1.2) | 0.2 (0.0, 0.4) | 5.2 (2.8, 7.5) | 1.5 (0.5, 2.6) | ** | 0.8 (0.0, 1.4) | 0.7 (0.0, 1.3) | ||
| Age 34–49 | 5.4 (2.2, 8.7) | 3.1 (0.8, 4.5) | 0.6 (0.0, 1.3) | 2.2 (0.5, 3.8) | 7.3 (5.0, 9.5) | 4.6 (2.3, 6.9) | 1.6 (0.5, 2.6) | 1.9 (0.4, 3.5) | ||||
| Age 50+ | 8.2 (2.5, 13.9) | 9.1 (1.2, 17.0) | 1.9 (1.0, 2.9) | 4.1 (1.6, 6.7) | 13.6 (5.9, 21.3) | 10.7 (1.4, 20.0) | 2.8 (1.5, 4.1) | 8.9 (4.9, 12.9) | *** | |||
| Arthritis | 21.7 (17.6, 25.8) | 10.1 (7.7, 12.6) | *** | 16.9 (15.1, 18.6) | 11.7 (9.6, 13.9) | *** | 25.7 (22.9, 28.6) | 22.0 (18.9, 25.1) | 20.6 (18.7, 22.5) | 18.0 (15.4, 20.5) | ||
| Age 18–33 | 11.1 (5.6, 16.6) | 4.2 (2.0, 6.4) | * | 5.5 (3.5, 7.5) | 2.5 (0.7, 4.2) | * | 11.9 (8.6, 15.3) | 12.6 (8.7, 16.4) | 5.7 (3.8, 7.6) | 6.5 (3.6, 9.3) | ||
| Age 34–49 | 21.0 (15.3, 26.6) | 12.5 (8.3, 16.8) | * | 15.8 (12.8, 18.7) | 10.0 (6.5, 13.5) | * | 33.7 (29.4, 38.0) | 25.7 (21.1, 30.2) | * | 17.5 (14.4, 20.6) | 16.3 (12.3, 20.4) | |
| Age 50+ | 37.1 (27.2, 46.9) | 32.5 (20.6, 44.5) | 31.1 (27.2, 35.1) | 31.1 (24.7, 37.4) | 53.7 (42.1, 65.4) | 57.0 (42.8, 71.1) | 41.1 (37.1, 45.2) | 42.9 (36.2, 49.7) | ||||
| All-Cause Cancer | 4.6 (2.6, 6.6) | 0.6 (0.0, 1.2) | *** | 5.0 (3.9, 6.0) | 2.1 (1.2, 3.0) | *** | 13.1 (10.9, 15.2) | 3.3 (2.1, 4.5) | *** | 8.4 (7.1, 9.7) | 4.3 (2.9, 5.6) | *** |
| Age 18–33 | 0.3 (0.0, 1.1) | 0.0 (0.0, 0.0) | ** | 0.3 (0.0, 0.7) | 0.4 (0.0, 1.2) | 8.3 (5.6, 10.9) | 2.7 (0.9, 4.5) | ** | 2.3 (0.9, 3.7) | 2.1 (0.6, 3.7) | ||
| Age 34–49 | 2.9 (0.6, 5.2) | 0.9 (0.0, 2.1) | 3.7 (2.1, 5.3) | 1.4 (0.0, 2.8) | 16.7 (13.3, 20.1) | 3.4 (1.8, 5.0) | *** | 7.4 (5.3, 9.5) | 5.3 (2.7, 7.8) | |||
| Age 50+ | 14.1 (6.9, 21.2) | 2.1 (0.0, 5.5) | * | 11.9 (9.3, 14.6) | 6.1 (3.3, 9.0) | * | 16.3 (8.5, 24.2) | 6.4 (0.8, 23.9) | 16.5 (13.4, 19.5) | 6.4 (3.1, 9.6) | *** | |
| Sexually Transmitted Infection | 23.8 (11.6, 36.0) | 34.9 (24.3, 45.4) | *** | 6.5 (5.2, 7.8) | 8.4 (6.1, 10.8) | 13.4 (11.2, 15.5) | 20.1 (17.1, 23.1) | *** | 10.8 (9.0, 12.7) | 14.0 (11.6, 16.5) | * | |
| Age 18–33 | 9.5 (4.2, 14.8) | 15.1 (11.2, 19.0) | 5.2 (3.3, 7.2) | 9.0 (5.4, 12.6) | 15.8 (12.3, 19.3) | 20.5 (15.9, 25.1) | 10.4 (7.6, 13.2) | 16.6, 12.1, 21.1) | * | |||
| Age 34–49 | 7.3 (3.7, 11.0) | 18.4 (13.6, 23.3) | *** | 7.0 (4.9, 9.2) | 8.1 (4.7, 11.5) | 12.2 (9.2, 15.2) | 21.6 (17.4, 25.8) | *** | 12.6 (9.7, 15.5) | 12.3 (8.5, 16.0) | ||
| Age 50+ | 5.1 (0.7, 9.5) | 15.0 (5.2, 24.7) | * | 7.2 (4.5, 10.0) | 7.9 (3.1, 12.8) | 5.6 (1.4, 9.8) | 6.4 (1.4, 11.4) | 8.9 (6.1, 11.8) | 12.5 (7.1, 17.9) | |||
Percentages are adjusted with sampling weights.
Incarcerated data from the 2004 Survey of Inmates in State and Federal Correctional Facilities.
Noninstitutionalized data from the 2002 & 2004 National Health and Nutrition Examination Survey.
p≤0.05;
p≤0.01;
p≤0.001
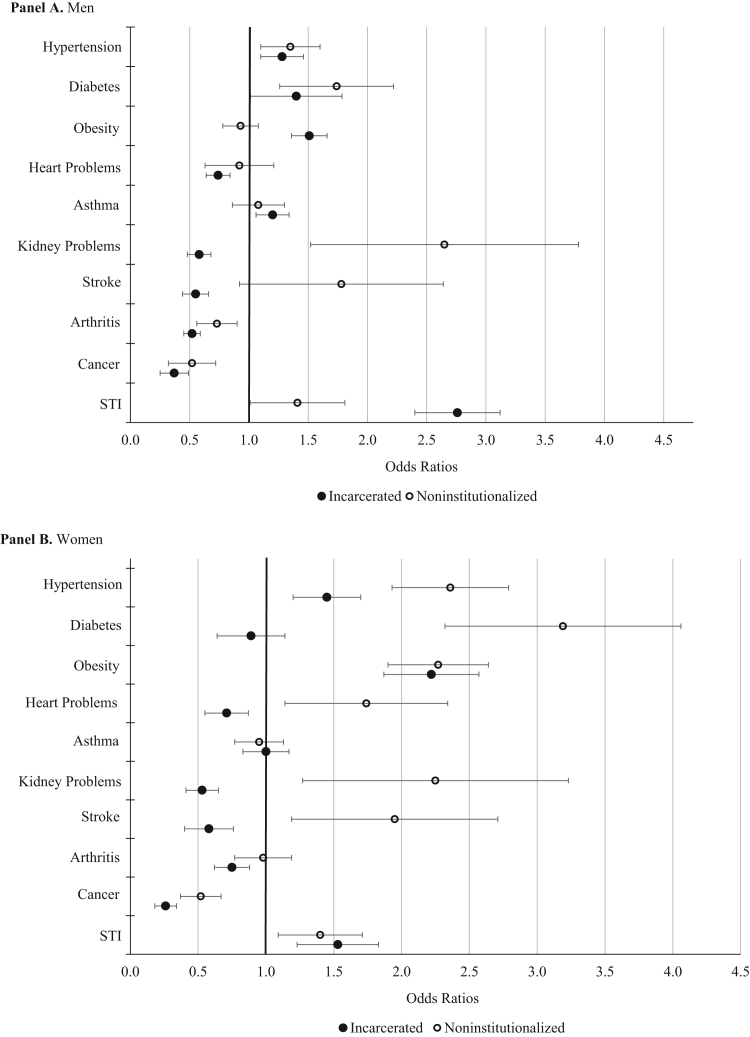
Table 2 presents the odds-ratios for health disparities within the incarcerated and noninstitutionalized adult samples. The corresponding p-value denotes whether the health disparity (OR1 vs. OR2) differs significantly for incarcerated and noninstitutionalized adults. These findings are also presented graphically in Fig. 1. Among men, disparities are significantly lower in prison for three health conditions: kidney problems, stroke, and arthritis. In the general population, black men (2.9%) and white men (1.1%) report similar rates of kidney problems overall (Table 1). When adjusting for age and education, there is almost a three-fold increase in the odds of reporting a kidney problem for blacks compared to whites (Odds Ratio (OR2) = 2.65, 95% Confidence Interval (CI): 1.52, 4.62). Both black (3.9%) and white (7.7%) male prisoners report higher rates of kidney problems compared to their noninstitutionalized counterparts (Table 1), but the increase is greater for whites, resulting in a reversal of the disparity: black prisoners report significantly lower odds of kidney problems compared to white prisoners (OR1 = 0.58, CI: 0.48, 0.70). The difference in odds ratios (OR1 = 0.58, OR2 = 2.65) is significant at the p ≤ 0.001 level. This relationship is shown graphically in Fig. 1 Panel A. The odds ratio for kidney problems for noninstitutionalized men is on the right side of the 1.0 line whereas the odds ratio for incarcerated men is to the left of the 1.0 line. Similar patterns emerged for stroke and arthritis.
Table 2.
Odds Ratios Comparing Blacks to Whites for Adults Aged 18–65 Stratified by Sex and Inmate Status Controlling for Age and Education.
|
Panel A. Men (n = 13,592) |
Panel B. Women (n = 6086) |
|||||
|---|---|---|---|---|---|---|
| Incarcerated (n=10,734) | Noninstitutional (n=2858) | Incarcerated vs. Noninstitutionala | Incarcerated (n=2983) | Noninstitutional (n=3171) | Incarcerated vs. Noninstitutionala | |
| Hypertension | 1.28 (1.15, 1.42) | 1.35 (1.10, 1.65) | 0.648 | 1.45 (1.20, 1.76) | 2.36 (1.93, 2.89) | 0.001 |
| Diabetes | 1.40 (1.14, 1.72) | 1.74 (1.26, 2.39) | 0.211 | 0.89 (0.64, 1.22) | 3.19 (2.32, 4.40) | 0.000 |
| Obesity | 1.51 (1.36, 1.68) | 0.93 (0.78, 1.12) | 0.000 | 2.22 (1.87, 2.65) | 2.27 (1.90, 2.70) | 0.862 |
| Heart Problems | 0.74 (0.64, 0.85) | 0.92 (0.63, 1.35) | 0.413 | 0.71 (0.55, 0.92) | 1.74 (1.14, 2.67) | 0.001 |
| Asthma | 1.20 (1.06, 1.35) | 1.08 (0.86, 1.36) | 0.458 | 1.00 (0.83, 1.22) | 0.95 (0.77, 1.17) | 0.746 |
| Kidney Problems | 0.58 (0.48, 0.70) | 2.65 (1.52, 4.62) | 0.000 | 0.53 (0.41, 0.68) | 2.25 (1.27, 4.00) | 0.000 |
| Stroke | 0.55 (0.44, 0.68) | 1.78 (0.92, 3.44) | 0.001 | 0.58 (0.40, 0.83) | 1.95 (1.19, 3.17) | 0.000 |
| Arthritis | 0.51 (0.45, 0.58) | 0.73 (0.56, 0.94) | 0.013 | 0.75 (0.62, 0.90) | 0.98 (0.77, 1.25) | 0.079 |
| All-Cause Cancer | 0.37 (0.25, 0.53) | 0.52 (0.32, 0.86) | 0.284 | 0.26 (0.18, 0.36) | 0.52 (0.37, 0.74) | 0.004 |
| Sexually Transmitted Infection | 2.76 (2.40, 3.18) | 1.41 (1.01, 1.96) | 0.000 | 1.53 (1.23, 1.90) | 1.40 (1.09, 1.79) | 0.496 |
Adjusted Odds Ratios (95% Confidence Interval).
Incarcerated data from the 2004 Survey of Inmates in State and Federal Correctional Facilities.
Noninstitutionalized data from the 2002 & 2004 National Health and Nutrition Examination Survey.
p-value for interaction term (inmate#race). Sensitivity tests were performed by estimating linear probability models.
Fig. 1.
Odds Ratios Comparing Blacks to Whites for Adults Aged 18–65 Stratified by Sex and Inmate Status Panel A. Men Panel B. Women.
Disparities among men are significantly larger in prisons for obesity and STI. There are no black-white differences in obesity in the general population (OR2 = 0.93, CI: 0.78, 1.12). In the prison population, black men have 51% higher odds of being obese compared to white men (OR1 = 1.51, 95% CI: 1.36, 1.68). Similarly, there are marginal race differences in STI in the general population (OR2 = 1.41, CI: 1.01, 1.96) but in the prison population blacks have almost three times the odds of reporting an STI (OR1 = 2.76, CI: 2.40, 3.18). The difference in odds ratios for STI between the prison and noninstitutionalized populations is significant at the p ≤ 0.001 level.
A more pronounced pattern is found among women, especially at older ages. Disparities are significantly smaller among incarcerated women compared to women in the general population for a number of health conditions including hypertension, diabetes, heart problems, kidney problems, and stroke. For each of these health conditions, incarcerated white women report a significantly higher prevalence (p ≤ 0.001; not shown) compared to white women in the general population, whereas rates among black women in and out of prison remain unchanged or only slightly increased (Table 1). Thus, the race disparity gap is largely closed among incarcerated women due to the increasingly worse health of white women who are incarcerated.
Examining the prevalence of these health conditions by age group shows an even more pronounced effect among the 50 years of age and older group. For example, overall rates of diabetes show that white women in the community report a prevalence rate of 3.9% overall, which is about a third as much as black women (9.6%). In the oldest age group, the reported prevalence is 8.7% and 23.6%, respectively. However, in prisons, white women report an overall rate of 7.2% compared to 5.5% of black women in prison who have lower rates than their noninstitutionalized counterparts.
Table 2 shows that noninstitutionalized black women have over a three-fold increase in the odds of reporting diabetes compared to noninstitutionalized white women (OR2 = 3.19, CI: 2.32, 4.40). However, there is no significant difference in diabetes prevalence rates among black and white women in prison (OR1 = 0.89, CI: 0.64, 1.22). The interaction term indicates that these odds ratios are significantly different (p ≤ 0.001) (see Fig. 1 Panel B). Comparable patterns are present for hypertension, heart problems, kidney problems, and stroke.
Similar to men, black-white disparities in STI are larger among women in prison. In the general population, black women report an overall STI prevalence of 14.0% compared to 10.8% for white women (Table 1). In the prison population, black women report much higher rates (20.1%) while rates for white women increase only slightly (13.4%). Table 2 confirms that black-white disparities are marginally different in the general population controlling for age and education (OR2 = 1.40, CI: 1.09, 1.79), yet there is a 53% increase in the odds of reporting an STI in the prison population (OR1 = 1.53, CI: 1.23, 1.90), although the race by inmate interaction term is not statistically significant (p = 0.496).
These findings are particularly important when you take into account the health selection process with respect to the incarcerated and noninstitutionalized populations for each group. Consider the values presented in Table 1 that describe the prevalence of each health problem for black and white men and women. The prevalence for each in the general population can be used to derive the standard deviation for each health problem. One can then compare the prevalence in the incarcerated population to the prevalence (and standard deviation) in the general population as a standardized level. The average of these for the 10 health problems that we consider provides an estimate of 0.21 for white male prisoners which is comparable to a cumulative probability of 0.59 in a standard normal curve. That is, the average health burden in the prison population is representative of the 59th percentile of the non-institutionalized white male population. This number nicely characterizes the magnitude of the health differences between prisoners and non-prisoners. Importantly, this number is somewhat lower (54th percentile) among black male prisoners and black female prisoners (53th percentile), suggesting that the health selection mechanisms related to incarceration are less pronounced among black adults compared to white men. The health burden among incarcerated white women places them in the 62th percentile of poor health among the noninstitutionalized white female population providing, again, strong evidence that the selection mechanisms of poor health among prisoners is the most pronounced among white women.
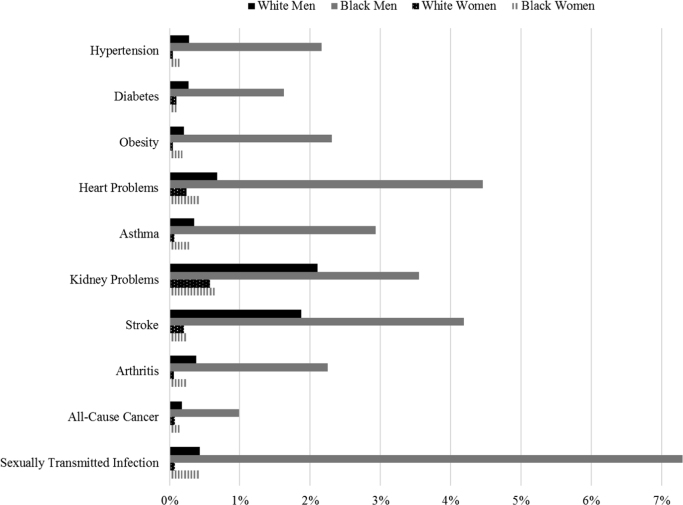
Finally, we more closely examine the selective process of incarceration with a descriptive exercise shown in Table 3 and Fig. 2. Here, we examine the number of adults with each specific morbidity in the U.S. population and the extent to which these numbers would change if the prison population were included in population estimates. The results show important increases in the population of unhealthy adults for all of the morbidities and they detail the anticipated change in health disparities among U.S. adults. For example, if all of these inmates were included in population health estimates, the number of adults with hypertension would increase by 78,428 for white men, 105,074 for black men, 12,812 for white women, and 12,181 for black women (Table 3). Even though black men account for a much smaller percentage of the U.S. adult population than white men, they would contribute more cases to the overall population health profile. Thus, given the overrepresentation of black men in prison, the population estimates for this group would be most affected. The population of black men with health problems increases by 1 to 7% (Fig. 2).
Table 3.
U.S. Adult Population (age 18–65) with Morbidity and the Population with Morbidity Adjusted to Include State and Federal Prison Inmates.
|
Panel A. White Men |
Panel B. Black Men |
|||||
|---|---|---|---|---|---|---|
| Noninstitutional | Adjusted | Change | Noninstitutional | Adjusted | Change | |
| Hypertension | 27,803,999 | 27,882,427 | 78,428 | 4,848,579 | 4,953,653 | 105,074 |
| Diabetes | 6,030,762 | 6,046,977 | 16,215 | 1,305,056 | 1,326,305 | 21,249 |
| Obesity | 33,695,518 | 33,764,397 | 68,879 | 4,812,387 | 4,923,423 | 111,036 |
| Heart Problems | 5,920,686 | 5,960,832 | 40,146 | 788,665 | 823,790 | 35,125 |
| Asthma | 13,782,688 | 13,831,255 | 48,567 | 2,387,620 | 2,457,706 | 70,086 |
| Kidney Problems | 1,292,322 | 1,319,589 | 27,267 | 536,658 | 555,692 | 19,034 |
| Stroke | 1,147,207 | 1,168,679 | 21,472 | 327,637 | 341,365 | 13,728 |
| Arthritis | 20,558,743 | 20,636,628 | 77,885 | 2,188,199 | 2,237,444 | 49,245 |
| All-Cause Cancer | 6,040,438 | 6,050,998 | 10,560 | 390,527 | 394,379 | 3,852 |
| Sexually Transmitted Infection | 6,281,647 | 6,308,612 | 26,965 | 1,044,437 | 1,120,700 | 76,263 |
| Panel C. White Women | Panel D. Black Women | |||||
| Noninstitutional | Adjusted | Change | Noninstitutional | Adjusted | Change | |
| Hypertension | 26,211,969 | 26,224,781 | 12,812 | 7,409,244 | 7,421,425 | 12,181 |
| Diabetes | 4,693,153 | 4,697,550 | 4,397 | 2,170,766 | 2,173,220 | 2,454 |
| Obesity | 32,394,227 | 32,408,202 | 13,975 | 10,379,537 | 10,398,300 | 18,763 |
| Heart Problems | 3,415,495 | 3,423,662 | 8,167 | 1,037,150 | 1,041,439 | 4,289 |
| Asthma | 18,732,668 | 18,746,080 | 13,412 | 3,280,371 | 3,290,163 | 9,792 |
| Kidney Problems | 1,534,723 | 1,543,586 | 8,863 | 678,798 | 683,305 | 4,507 |
| Stroke | 2,003,552 | 2,007,721 | 4,169 | 645,176 | 646,759 | 1,583 |
| Arthritis | 25,363,132 | 25,378,922 | 15,790 | 4,146,632 | 4,156,558 | 9,926 |
| All-Cause Cancer | 10,322,945 | 10,330,939 | 7,994 | 963,924 | 965,385 | 1,461 |
| Sexually Transmitted Infection | 10,666,245 | 10,674,410 | 8,165 | 2,145,930 | 2,155,044 | 9,114 |
Fig. 2.
Percent Increase in Prevalence of Health Conditions with Prison Inmates Included with the Noninstitutionalized Population.
4. Discussion
One of the goals for Health People 2020 is to reduce health disparities for people of color. Yet, it is unclear how the criminal justice system can contribute to this goal (Freudenberg & Heller, 2016). Moreover, incarcerated persons are excluded from national health surveys and correctional facilities often have an inadequate surveillance system for providing valid and reliable data on the health status of inmates. The 2002 National Commission on Correctional Health Care report on the health status of inmates that was presented to the U.S. Congress concludes that there is a tremendous and largely unexploited opportunity to benefit public health by illuminating health disparities among inmates and improving correctional health care practices. Understanding the health profile and healthcare needs of the incarcerated population is imperative for achieving health equity and maintaining the public health of the local communities from which inmates are drawn. Compared to 16 high-income nations, the United States ranks last in life expectancy, relatively poorly (and in many instances last) on virtually all indicators of health, and health improvements in the United States have not kept pace with that in other high-income countries (National Research Council & Institute of Medicine [NRC/IOM], 2013). To better understand why Americans fare so poorly relative to individuals in other high-income countries in terms of health, we argue that incarceration rates should be considered when comparing health within and among countries (see Wildeman, 2016).
In this paper, we show that prisoners report worse health than their noninstitutionalized counterparts. Incarceration is associated with a higher prevalence of hypertension, diabetes, heart problems, asthma, kidney problems, stroke, arthritis, and STI, with differences larger for whites than blacks, especially among women. Some support is found for the main hypothesis that race disparities are muted in prisons than the general community. After adjusting for age and education, we find that male prisons have smaller black-white disparities for kidney problems, stroke, and arthritis compared to men in the general population. For women the hypothesis is supported for hypertension, diabetes, heart problems, kidney problems, and stroke. Black-white disparities are actually larger in prisons for obesity among both men and women and for STI for men. Overall, these findings are consistent with previous studies (Binswanger et al., 2009, Binswanger et al., 2010, Harris et al., 2007, Wilper et al., 2009); however, our study provides further confirmation by stratifying by both sex and race among U.S. prisoners. This study demonstrates that the poor health documented among prisoners is not necessarily due to the overrepresentation of people of color within prisons. These results provide evidence that the selection of more unhealthy persons into prisons is only moderately stronger among white compared to black men but noteworthy among white compared to black women.
At the beginning of the paper we noted several mechanisms that contribute to health disparities. Specific morbidities, however, are more likely than others to respond to these mechanisms. While the mechanisms for health disparities are not directly tested in this paper, we can discuss the findings in light of current knowledge. For instance, neighborhood environmental exposures are best characterized by cancer and asthma and we see that patterns of disparities are nearly identical in and out of prison. The only exception is disparities in cancer among female inmates in which the gap between white and black women is wider in prisons, with white women having higher odds of cancer. Similarly, arthritis—a leading cause of disability in the United States (CDC, 2016)—is likely unrelated to imprisonment per se and the only significant difference found in patterns of disparities is among male prisoners.
On the other hand, hypertension, heart problems, and stroke are the most proximate morbidities linked to stress and discrimination. Changes in the links between race and health in this domain would shed light on health disparities. The findings show that among women in the noninstitutionalized population, blacks have significantly higher odds of reporting hypertension, heart problems, and stroke compared to whites on the order of 1.74–2.36 times as high. Among women in the prison population, however, the black-white disparity is significantly reduced for hypertension and reversed for heart problems and stroke so that white women have significantly higher odds of reporting these conditions compared to black women. Among men, only the black-white disparities for stroke is reversed in prisons. The mechanisms linking stress and physical health appear to operate differently in prisons, in general, at least among women, suggesting incomplete understanding of stress and health. Importantly, hypertension and diabetes are leading risk factors for kidney disease, which effects about 10% of the U.S. population (CDC, 2014) and is the 9th leading cause of death in the U.S. (Kochanek, Murphy, Xu & Tejada-Vera, 2016). Individuals who advance to kidney failure require regular dialysis or kidney transplantation—expensive costs for correctional institutions. African Americans have three times the risk of developing kidney disease compared to non-Hispanic whites in the noninstitutionalized population, but in prisons, this disparity is reversed.
Diabetes, obesity, and STI are sensitive to lifestyle factors such as sexual practices, nutrition, and exercise. Therefore, we might expect to see diminished disparities in prison because these behaviors are neutralized among inmates. But obesity and STI are the exact opposite for black men as well as STI for black women (the disparities are worse in prison). Contagion theory and a social network perspective (Christakis & Fowler, 2012) may help explain this pattern. For example, research on HIV transmission among prisoners demonstrates that the prison itself is a high risk setting for transmission of HIV/AIDS due to high-risk sexual activity (both consensual and nonconsensual), injection drug use, and tattooing (Blackenship et al., 2005, Krebs, 2006, Krebs and Melanie, 2002, Okie, 2007). There are, however, uncertainties about the extent and the nature of infectious disease transmission within prisons (Hammett, 2006). Nevertheless, disparities in HIV/AIDS are likely due to the fact that blacks have a greater likelihood of being exposed to the prison environment and then return to their communities (Blackenship et al., 2005). Mass incarceration is concentrated in prison “feeder communities” (Drucker, 2011). For example, the Justice Mapping Center found that in the state of New York 75% of the entire prison population came from only seven neighborhoods in New York City characterized by poverty and a high proportion of racial/ethnic minorities (Drucker, 2011). The serial incarceration that is characteristic of these neighborhoods disrupts social networks and increases the transmission of HIV/AIDS in these communities (Drucker, 2011). Laumann & Youm (1999) posit that the higher rates of STIs among African Americans is partly explained by an intra racial network effect: compared to white sexual partner choices, black choices are more segregated (limited to other blacks) and dissortative (sexually inexperienced individuals are more likely to interact with much more experienced sexual partners). This intra racial network effect may be more pronounced for blacks who contract STIs in prison and then return to their community-based social networks. Contagion processes may also operate for obesity (Christakis & Fowler, 2007; see Cohen-Cole & Fletcher, 2008 for a critique).
In sum, even though prisons are theoretically a neutralizing force for health, the varying etiologies of health conditions interact with the prison context differently. Moreover, there is a racialized and gendered health selection process into prison. All inmates are drawn from unhealthy segments of the population, but white women, in particular, are drawn from the most select and unhealthiest segment of the population compared to white men and black men and women. Given the nearly universal structure of residential segregation across the United States, it is important, as Schnittker, Massoglia & Uggen (2011) highlight, to consider how these disparities will play out in terms of the concentration of specific morbidities in highly segregated neighborhoods.
4.1. Limitations
We consider four limitations when interpreting these findings. First, the health conditions rely on self-report. While the SPI is the best data set available to answer the research questions because it is the only large, nationally representative U.S. survey of prisoners extant, this limitation is important because some have shown that black inmates may be more likely than white inmates to use healthcare services when incarcerated (Rosen et al. 2012). Thus, black inmates may be more likely to report ill health because of a recent diagnosis or test result. Further, although the NHANES includes the results of medical and laboratory examinations, it excludes institutionalized populations. The difference in wording between the surveys may also contribute to biased results. The SPI asked, “Have you ever had…?” which may lead to an overestimation since the question does not specify a medical diagnosis. On the other hand, NHANES asked, “Has a doctor or other health professional ever told you that you had…?” which may lead to an underestimate of the “true” prevalence. Taken together, it is possible that these differences are driving the study findings, although this is unlikely given the well-established health differences between incarcerated and noninstitutionalized adults (e.g., Binswanger et al. 2009; Wilper et al. 2009). Prospective data with objective measures of health are needed to help uncover the complex relationship between incarceration and health. A third important limitation is that STI is the only comparable infectious disease between the data sets. The study would be strengthened if additional infectious diseases, such as HIV, hepatitis, and tuberculosis, were included.
A final limitation is that the NHANES study does not ask about prior incarcerations. Therefore, it is impossible to exclude noninstitutionalized persons who have previously been incarcerated, although this population is also likely to be underrepresented in household surveys (Pettit, 2012). Nevertheless, given the large number of prisoners released (approximately 650,000) from state prison every year (Carson, 2014), this could bias the study estimates. Even though this paper treats incarcerated and noninstitutionalized adults as distinct populations, the incarcerated population can more accurately be conceptualized as a flow of individuals in and out of prison. If all correctional facilities are included (e.g., state prisons, federal prisons, juvenile correctional facilities, local jails, Indian Country jails, military prisons, immigration detention facilities, civil commitment centers, and prisons in U.S. territories), it is estimated that over 2.4 million people are currently incarcerated (Wagner & Sakala, 2014). But this number does not accurately capture the population flows. For example, during the 12 months ending midyear 2012, 11.6 million people were admitted to local county jails, even though only 744,524 were incarcerated on June 30, 2012 (Minton, 2013). Related, this paper examines only one institutionalized population, which makes up 1% of the total U.S. population (PEW Center, 2008), but 11.4% of all black men aged 20–34 (the age group most at risk for incarceration), and 37.2% of black men aged 20–34 with less than a high school education (Pettit, 2012). Future research should include the correctional population in national estimates of mortality and morbidity, and, in general, consider the how patterns of health disparities may be biased by excluding institutionalized populations, such as active duty military, which comprise 0.5% of the population (Pew Research Center, 2012), and those living in nursing homes, 3.6% of the 65 and older population (U.S. Department of Health & Human Services, 2012).
5. Conclusion
The incarcerated population generally has worse health than the noninstitutionalized population, especially for hypertension, heart problems, asthma, kidney problems, stroke, arthritis, and cancer. Thus, the poor international ranking of the United States on health characteristics would worsen if the incarcerated populations were included in the estimates. Furthermore, the exceptionally high rates of incarceration may also worsen health for the noninstitutionalized population due to spillover effects (Brinkley-Rubenstein, 2013, Schnittker et al., 2015, Wildeman, 2016). The high rates of hypertension, diabetes, and STIs experienced in prison may contribute to high rates in the community, especially as prisoners with poor health conditions are released back into the community. For example, some individuals may contract STIs in prison and infect others in the community upon their release.
True understanding of the health consequences of mass incarceration on population health and health disparities requires improved data collection such as the inclusion of questions about incarceration on upcoming cycles of national health surveys. This will provide consistent and accurate information on the prevalence of health conditions for former inmates, the health care needs for former inmates, and how these prevalence’s and needs differ across groups. We also encourage researchers to evaluate incarceration histories in greater detail so that it is possible to compare selection into prison as a function of health and change in health over time as a function of prison exposure (conditional on these selective factors). This would require data on individuals with comparable criminal histories and comparable propensities for incarceration but different treatments (e.g., prison or no prison). Then one could make a stronger statement about the contours of selective forces into prison as a function of health and how these factors vary among white and black adults.
Our results demonstrate the importance of considering the composition of populations when incarcerated adults are not included in the estimates, especially the implications for health disparities research. But we are also aware that there are many institutional mechanisms in place that complicate the selection into the prison population and we encourage researchers to elaborate on these mechanisms in future health research. Overall, a better understanding of prisoner health can provide needed insight into the health and wellbeing of the general U.S. population. In sum, we cannot fully understand the health of the nation—especially racial minority health—if we continue to exclude the prison population from health research and reporting.
Acknowledgements
Previous versions of this manuscript were presented at the 2016 Population Association of America annual meeting in Washington, DC, and the 2015 Southern Demographic Association annual meeting in San Antonio, Texas. Administrative and computing support for this study was provided to the authors by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) funded University of Colorado Population Center (2P2CHD066613-06). Nowotny was supported by the NIH Ruth L. Kirschstein National Research Service Award Individual Fellowship (F31 DA037645) funded by the National Institute on Drug Abuse (NIDA), the National Science Foundation (NSF) SBE Doctoral Dissertation Research Improvement Grant (#1401061), and the NIDA-funded Criminal Justice Research Training Program (R25 DA026401). The NIDA, NSF, and NICHD had no role in the study design; the collection, analysis and interpretation of data; the writing of the report; or the decision to submit the paper for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of NSF or NIH. Publication of this article was funded by the University of Colorado Boulder Libraries Open Access Fund.
Contributor Information
Kathryn M. Nowotny, Email: kathryn.nowotny@miami.edu.
Richard G. Rogers, Email: richard.rogers@colorado.edu.
Jason D. Boardman, Email: boardman@colorado.edu.
References
- Adler N.E., Rehkopf D.H. U.S. disparities in health: Descriptions, causes, and mechanisms. Annual Review of Public Health. 2008;29:235–252. doi: 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- Ahalt C., Binswanger I.A., Steinman M., Tulsky J., Williams B.A. Confined to ignorance: The absence of prisoner information from nationally representative health data sets. Journal of General Internal Medicine. 2011;27(2):160–166. doi: 10.1007/s11606-011-1858-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asad A.L., Clair M. Racialized legal status as a social determinant of health. Social Science & Medicine. 2017:1–10. doi: 10.1016/j.socscimed.2017.03.010. http://dx.doi.org/10.1016/j.socscimed.2017.03.010 forthcoming. [DOI] [PubMed] [Google Scholar]
- Baillargeon J., Black S.A., Pulvino J., Dunn K. The disease profile of Texas prison inmates. Annals of Epidemiology. 2000;10(2):74–80. doi: 10.1016/s1047-2797(99)00033-2. [DOI] [PubMed] [Google Scholar]
- Beckett K., Nyrop K., Pfingst L. Race, drugs, and policing: understanding disparities in drug delivery arrests. Criminology. 2006;44(1):105–137. [Google Scholar]
- Belknap J., Holsinger K. The gendered nature of risk factors for delinquency. Feminist Criminology. 2006;1(1):48–71. [Google Scholar]
- Binswanger I.A., Krueger P.M., Steiner J.F. Prevalence of chronic medical conditions among jail and prison inmates in the USA compared with the general population. Journal of Epidemiology and Community Health. 2009;63(11):912–919. doi: 10.1136/jech.2009.090662. [DOI] [PubMed] [Google Scholar]
- Binswanger I.A., Merrill J.O., Krueger P.M., White M.C., Booth R.E., Elmore J.G. Gender differences in chronic medical, psychiatric, and substance-dependence disorders among jail inmates. American Journal of Public Health. 2010;100(3):476–482. doi: 10.2105/AJPH.2008.149591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binswanger I.A., Redmond N., Steiner J.F., Hicks L.S. Health disparities and the criminal justice system: An agenda for further research and action. Jounral of Urban Health. 2011;89(1):98–107. doi: 10.1007/s11524-011-9614-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackenship K.M., Smoyer A.B., Bray S.J., Mattocks K. Black-white disparities in HIV/AIDS: The role of drug policy and the corrections system. Journal of Health Care for the Poor and Underserved. 2005;16(4B):140–156. doi: 10.1353/hpu.2005.0110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonzcar T.P. Bureau of Justice Statistics; Washington DC: 2003. Prevalence of Imprisonment in the U.S. Population, 1974–2001. [Google Scholar]
- Bridges G.S., Steen S. Racial disparities in official assessments of juvenile offenders: Attributional stereotypes as mediating mechanisms. American Sociological Review. 1998;63(4):554–570. [Google Scholar]
- Brinkley-Rubenstein L. Incarceration as a catalyst for worsening health. Health and Justice. 2013;1(3):1–17. [Google Scholar]
- Carson, E. A. (2014). Prisoners in 2013. In Office of Justice Programs U.S. Department of Justice (Ed.). Washington, DC: Bureau of Justice Statistics.
- Centers for Disease Control and Prevention (CDC) US Department of Health and Human Services, Centers for Disease Control and Prevention; Atlanta, GA: 2016. At a Glance 2016: Imroving the quality of life for people with arthritis. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) US Department of Health and Human Services, Centers for Disease Control and Prevention; Atlanta, GA: 2014. National chronic kidney disease fact sheet: General information and national estimates on chronic kidney disease in the United States, 2014. [Google Scholar]
- Christakis N.A., Fowler J.H. The spread of obesity in a large social network over 32 years. New England Journal of Medicine. 2007;357(4):370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- Christakis N.A., Fowler J.H. Social contagion theory: Examining dynamic social networks and human behavior. Statistics in Medicine. 2012;32:556–577. doi: 10.1002/sim.5408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clear T. Oxford University Press; New York, NY: 2007. Imprisoning Communities: How mass incarceration makes disadvantaged neighborhoods worse. [Google Scholar]
- Cohen-Cole E., Fletcher J.M. Is obesity contagious? Social networks vs. environmental factors in the obesity epidemic. Journal of Health Economics. 2008;27:1382–1387. doi: 10.1016/j.jhealeco.2008.04.005. [DOI] [PubMed] [Google Scholar]
- Drucker E. The New Press; New York: 2011. A plague of prisons: The epidemiology of mass incarceration in America. [Google Scholar]
- Dumont D.M., Brockmann B., Dickman S., Alexander N., Rich J.D. Public health and the epidemic of incarceration. Annual Review of Public Health. 2012;33:325–339. doi: 10.1146/annurev-publhealth-031811-124614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eliason M.J., Taylor J.Y., Williams R. Physical health of women in prison: Relationship to oppression. Journal of Correctional Health Care. 2004;10(2):175–203. [Google Scholar]
- Fazel S., Danesh J. Serious mental disorder in 23,000 prisoners: A systematic review of 62 surveys. The Lancet. 2002;359:545–550. doi: 10.1016/S0140-6736(02)07740-1. [DOI] [PubMed] [Google Scholar]
- Freudenberg N., Heller D. A review of opportuntities to improve the health of people involved in the criminal justice system in the United States. Annual Review of Public Health. 2016;37:313–333. doi: 10.1146/annurev-publhealth-032315-021420. [DOI] [PubMed] [Google Scholar]
- Frisbie W.P., Song S.-E., Powers D.A., Street J.A. The increasing racial disparity in infant mortality: Respiratory distress syndrome and other causes. Demography. 2004;41(4):773–800. doi: 10.1353/dem.2004.0030. [DOI] [PubMed] [Google Scholar]
- Geruso M. Black-white disparities in life expectancy: How much can the standard SES variables explain? Demography. 2012;49:553–574. doi: 10.1007/s13524-011-0089-1. [DOI] [PubMed] [Google Scholar]
- Goffman E. Archer Books; New York: 1961. Asylums: Essays on the social situation of mental patients and other inmates. [Google Scholar]
- Gostin L.O. Biomedical research involving prisoners: Ethical values and legal regulation. JAMA. 2007;297(7):737–740. doi: 10.1001/jama.297.7.737. [DOI] [PubMed] [Google Scholar]
- Greenfeld L.A., Snell T.L. U.S. Department of Justice; Washington DC: 1999. Women offenders. [Google Scholar]
- Hammett T.M. HIV/AIDS and other infectious diseases among correctional inmates: Transmission, burden, and an appropriate response. American Journal of Public Health. 2006;96:974–978. doi: 10.2105/AJPH.2005.066993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammett T.M., Harmon M.P., Rhodes W. The burden of infectious disease among inmates of and releasees from US correctional facilities, 1997. American Journal of Public Health. 2002;92(11):1789–1794. doi: 10.2105/ajph.92.11.1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper S., Lynch J., Burris S., Smith G.D. Trends in the black-white life expectancy gap in the United States, 1983–2003. JAMA. 2007;297(11):1224–1232. doi: 10.1001/jama.297.11.1224. [DOI] [PubMed] [Google Scholar]
- Harris F., Hek G., Condon L. Health needs of prisoners in England and Wales: The implications for prison healthcare of gender, age, and ethnicity. Health and Social Health Care. 2007;15(1):56–66. doi: 10.1111/j.1365-2524.2006.00662.x. [DOI] [PubMed] [Google Scholar]
- Hayward M.D., Miles T.P., Crimmins E.M., Yang Y. The significance of socioeconomic status in explaining the racial gap in chronic health conditions. American Sociological Review. 2000;65(6):910–930. [Google Scholar]
- Houle B. Obesity disparities among disadvantaged men: National adult male inmate prevalence pooled with non-incarcerated estimates, United States 2002–2004. Social Science & Medicine. 2011;72(10):1667–1673. doi: 10.1016/j.socscimed.2011.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hummer R.A. Black-white differences in health and mortality: A review and conceptual model. The Sociological Quarterly. 1996;37(1):102–125. [Google Scholar]
- Hummer R.A., Rogers R.G., Nam C.B., LeClere F.B. Race/ethnicity, nativity, and U.S. adult mortality. Social Science Quarterly. 1999;80(1):136–153. [Google Scholar]
- James D.J., Glaze L.E. Department of Justice Bureau of Justice Statistics; Washington DC: 2006. Mental health problems of prison and jail inmates. (Special Report) [Google Scholar]
- Kirk D.S. The neighborhood context of racial and ethnic disparities in arrest. Demography. 2008;45(1):55–77. doi: 10.1353/dem.2008.0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochanek Kenneth D., Murphy Sherry L., Xu Jiaquan, Tejada-Vera Betzaida. Deaths: Final data for 2014. National Vital Statistics Reports. 2016;65(4):1–122. [PubMed] [Google Scholar]
- Krebs C. Inmate factors associates with HIV transmission in prison. Criminology Public Policy. 2006;5(1):113–136. [Google Scholar]
- Krebs C.P., Melanie S. Intraprison HIV transmission: An Assessment of whether it occurs, how it occurs, and who is at risk. AIDS Education and Prevention. 2002;14(B):53–64. doi: 10.1521/aeap.14.7.53.23865. [DOI] [PubMed] [Google Scholar]
- Laumann E.O., Youm Y. Racial/ethnic group differences in the prevalence of sexually transmitted diseases in the United States: A network explanation. Sexually Transmitted Diseases. 1999;26(5):250–261. doi: 10.1097/00007435-199905000-00003. [DOI] [PubMed] [Google Scholar]
- Link B.G., Phelan J. Social conditions as fundamental causes of diease. Journal of Health and Social Behavior. 1995;35:80–94. [PubMed] [Google Scholar]
- Massoglia M. Incarceration as exposure: The prison, infectious disease, and other stress-related illnesses. Journal of Health and Social Behavior. 2008;49:56–71. doi: 10.1177/002214650804900105. [DOI] [PubMed] [Google Scholar]
- Massoglia M. Incarceration, health, and racial disparities in health. Law Society Review. 2008;42(2):275–306. [Google Scholar]
- Massoglia M., Pridemore W.A. Incarceration and Health. Annual Review of Sociology. 2015;41:291–310. doi: 10.1146/annurev-soc-073014-112326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minton, T. D. (2013). Jail inmates at midyear 2012 - statistical tables. In Office of Justice Programs U.S. Department of Justice (Ed.) Washington, DC: Bureau of Justice Statistics.
- Moore L.D., Elkavich A. Who’s using and who’s doing time. American Journal of Public Health. 2008;98:782–786. doi: 10.2105/AJPH.2007.126284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mumola C. Bureau of Justice Statistics; Washington DC: 2007. Medical causes of death in state prisons, 2001–2004. [Google Scholar]
- National Center for Health Statistics (NCHS) (2002, 2004). National health and nutrition examination survey data. Hyattsville, MD: National Center for Health Statistics, 2001-2002 and 2003-2004.
- National Research Council and Institute of Medicine . U.S. health in international perspective: Shorter lives, poorer health. In: Woolf Steven H., Aron Laudan., editors. Panel on understanding cross-national health differences among high-income countries. National Academies Press; Washington, DC: 2013. [PubMed] [Google Scholar]
- Nowotny K.M. Race/ethnic disparities in the utilization of treatment by drug dependent inmates in state correctional facilities. Addictive Behaviors. 2015;40:148–153. doi: 10.1016/j.addbeh.2014.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden C.L., Carroll M.D., Kit B.K., Flegal K.M. Prevalence of childhood and adult obesity in the United States, 2011–2012. Journal of the American Medical Association. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okie S. Sex, drugs, prisons, and HIV. The New England Journal of Medicine. 2007;356(2):105–108. doi: 10.1056/NEJMp068277. [DOI] [PubMed] [Google Scholar]
- Pampel F.C., Krueger P.M., Denney J.T. Socioeconomic disparities in health behaviors. Annual Review of Sociology. 2010;36:349–370. doi: 10.1146/annurev.soc.012809.102529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson E.J. Incarcerating death: mortality in U.S. State correctional facilities, 1985–1998. Demography. 2010;47(3):587–607. doi: 10.1353/dem.0.0123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson E.J. The dose-response of time served in prison on mortality: New York State, 1989–2003. American Journal of Public Health. 2013;103(3):523–528. doi: 10.2105/AJPH.2012.301148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson E.J., Wildeman C. Mass Imprisonment and the life course revisited: Cumulative years spent imprisoned and marked for working-age black and white men. Social Science Research. 2015;53:325–337. doi: 10.1016/j.ssresearch.2015.06.011. [DOI] [PubMed] [Google Scholar]
- Pettit B. Russell Sage Foundation; New York, NY: 2012. Invisible men: Mass incarceration and the myth of black progress. [Google Scholar]
- Pew Charitable Trusts (2008). One in 100: Behind Bars in America. Pew Charitable Trusts: Washington, DC. Retrieved from 〈http://www.pewtrusts.org/~/media/legacy/uploadedfiles/wwwpewtrustsorg/reports/sentencing_and_corrections/onein100pdf.pdf〉.
- Pew Research Center . Pew Research Center; Washington, DC: 2012. Small share of Americans in active military duty numbers, facts, and trends shaping your world.http://www.pewresearch.org/fact-tank/2012/05/23/small-share-of-americans-in-active-military-duty/ [Google Scholar]
- Phelan J.C., Link B.G., Tehranifar P. Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications. Journal of Health and Social Behavior. 2010;51(1S):S28–S40. doi: 10.1177/0022146510383498. [DOI] [PubMed] [Google Scholar]
- Porter L.C. Incarceration and post-release health behavior. Journal of Health and Social Behavior. 2014;55(2):234–249. doi: 10.1177/0022146514531438. [DOI] [PubMed] [Google Scholar]
- Richie B.E. Challenges incarcerated women face as they return to their communities: Findings from life history interviews. Crime & Delinquency. 2001;47:369–389. [Google Scholar]
- Roettger M.E., Swisher R.R. Association of fathers' history of incarceration with sons' delinquency and arrest among black, white, and hispanic males in the United States. Criminology. 2011;49(4):1109–1147. [Google Scholar]
- Rosen D.L., Wohl D.A., Schoenbach V.J. All-cause and cause-specific mortlaity among black and white North Carolina state prisoners, 1995–2005. Annals of Epidemiology. 2011;21(10):719–726. doi: 10.1016/j.annepidem.2011.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnittker J., John A. Enduring stigma: The long-term effects of incarceration on health. Journal of Health and Social Behavior. 2007;48(2):115–130. doi: 10.1177/002214650704800202. [DOI] [PubMed] [Google Scholar]
- Schnittker J., Massoglia M., Uggen C. Incarceration and the health of the African American community. Du Bois Review: Social Science Research on Race. 2011;8(1):133–141. [Google Scholar]
- Schnittker J., Uggen C., Shannon S.K.S., McElrath S.M. The institutional effects of incarceration: Spillovers from criminal justice to health care. The Milbank Quarterly. 2015;93(3):516–560. doi: 10.1111/1468-0009.12136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon L., Flynn C., Much K., Vertefeuille J. Prevalence of HIV, syphilis, hepatitis B, and Hepatitis C among entrants to maryland correctional facilities. Journal of Urban Health. 2004;81(1):25–37. doi: 10.1093/jurban/jth085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stapleton D., Honeycutt T., Schechter B. Out of sight, out of mind: Including group quarters residents with household residents can change what we know about working-age people with disabilities. Demography. 2011;49:267–289. doi: 10.1007/s13524-011-0071-y. [DOI] [PubMed] [Google Scholar]
- StataCorp . StataCorp LP; College Station, TX: 2013. Stata statistical software: Release 13. [Google Scholar]
- Steadman H.J., Osher F.C., Clark Robbins P., Case B., Samuels S. Prevalence of Serious mental illness among jail inmates. Psychiatric Services. 2009;60(6):761–765. doi: 10.1176/ps.2009.60.6.761. [DOI] [PubMed] [Google Scholar]
- Steffensmeier D., Ulmer J., Kramer J. The interaction of race, gender, and age in criminal sentencing: The punishment cost of being young, black, and male. Criminology. 1998;36(4):763–798. [Google Scholar]
- Turney K. Unmet health care needs among children exposed to parental incarceration. Maternal Child Health Journal. 2017;21(5):1194–1202. doi: 10.1007/s10995-016-2219-2. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (2012). A profile of older Americans: 2012. Washington, DC.
- United States Department of Justice. Bureau of Justice Statistics (2007). Survey of inmates in state and federal correctional facilities, 2004. ICPSR04572-v1. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor]. 2007-02-28.
- Wagner P., Sakala L. The Prison Policy Institute; Northampton, MA: 2014. Mass Incarceration: The whole pie a prison policy initiative briefing. [Google Scholar]
- Wakefield S., Uggen C. Incarceration and Stratification. Annual Reivew of Sociology. 2010;36:387–406. [Google Scholar]
- Wang E.A., Green J. Incarceration as a key variable in racial disparities of asthma prevalence. BMC Public Health. 2010;10:290–299. doi: 10.1186/1471-2458-10-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang E.A., Wildeman C. Studying health disparities by including incarcerated and formerly incarcerated individuals. JAMA. 2011;305(16):1708–1709. doi: 10.1001/jama.2011.532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner D.F., Hayward M.D. Early-life origins of the race gap in men’s mortality. Journal of Health and Social Behavior. 2006;47:209–226. doi: 10.1177/002214650604700302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Western B. Russell Sage Foundation; New York: 2006. Punishment and Inequality in America. [Google Scholar]
- Wildeman C. Incarceration and population health in wealthy democracies. Criminology. 2016;54(2):360–382. [Google Scholar]
- Wildeman C., Muller C. Mass imprisonment and inequality in health and family life. Annual Reivew of Law and Social Science. 2012;8:11–30. [Google Scholar]
- Wildeman C., Wang E.A. Mass incarceration, public health, and widening inequlaity in the USA. The Lancet. 2017;389:1464–1474. doi: 10.1016/S0140-6736(17)30259-3. [DOI] [PubMed] [Google Scholar]
- Williams D.R., Jackson P.B. Social sources of racial disparities in health. Health Affairs. 2005;24(2):325–334. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]
- Williams D.R., Mohammed S.A. Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine. 2009;32:20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilper A.P., Woolhandler S., Boyd J.W., Lasser K.E., McCormick D., Bor D.H., Himmelstein D.U. The health and health care of US prisoners: Results of a nationwide survey. American Journal of Public Health. 2009;99(4):666–672. doi: 10.2105/AJPH.2008.144279. [DOI] [PMC free article] [PubMed] [Google Scholar]