Keywords: nerve regeneration, cerebral ischemia/reperfusion, magnetic resonance imaging, diffusion weighted imaging, signal transducer and activator of transcription 3, phosphorylated signal transducer and activator of transcription 3, apparent diffusion coefficient, relative apparent diffusion coefficient, immunohistochemistry, western blot assay, neural regeneration
Abstract
Signal transducer and activator of transcription (STAT) is a unique protein family that binds to DNA, coupled with tyrosine phosphorylation signaling pathways, acting as a transcriptional regulator to mediate a variety of biological effects. Cerebral ischemia and reperfusion can activate STATs signaling pathway, but no studies have confirmed whether STAT activation can be verified by diffusion-weighted magnetic resonance imaging (DWI) in rats after cerebral ischemia/reperfusion. Here, we established a rat model of focal cerebral ischemia injury using the modified Longa method. DWI revealed hyperintensity in parts of the left hemisphere before reperfusion and a low apparent diffusion coefficient. STAT3 protein expression showed no significant change after reperfusion, but phosphorylated STAT3 expression began to increase after 30 minutes of reperfusion and peaked at 24 hours. Pearson correlation analysis showed that STAT3 activation was correlated positively with the relative apparent diffusion coefficient and negatively with the DWI abnormal signal area. These results indicate that DWI is a reliable representation of the infarct area and reflects STAT phosphorylation in rat brain following focal cerebral ischemia/reperfusion.
Introduction
Cerebral ischemia/reperfusion injury is an important pathophysiological process that underlies cerebrovascular disease. Magnetic resonance imaging (MRI) can reveal ischemic brain tissue. In hyperacute cerebral infarction (< 6 hours), the infarcted area can be seen in diffusion-weighted MRI (DWI), and magnetic resonance perfusion imaging can show the location and extent of the ischemic zone at around 10 minutes (Beck et al., 2014).
Cerebral ischemia/reperfusion can activate signal transducers and activators of transcription (STATs) (Li et al., 2015b). The Janus kinase (JAK)-STAT pathway is activated after cerebral ischemia. Membrane receptor signaling by various ligands induces activation of JAK kinases, which then leads to tyrosine phosphorylation of various STAT transcription factors (Kim et al., 2017). STAT1 and STAT3 are members of the STAT family, and phosphorylated (p-)STAT3 is the activated form of STAT3 (Jia et al., 2017). These proteins play an important role in neuronal survival and antiapoptosis. p-STAT3 is a mediator of growth factors, hormones and cytokines, and exerts its protective and regenerative effects in cerebral ischemia/reperfusion partly through transcriptional upregulation of neuroprotective and neurotrophic genes (Jiang et al., 2012). In the present study, we analyzed the changes in DWI, STAT3 and p-STAT3 in the ischemic injury zone in a rat model of focal cerebral ischemia/reperfusion injury.
Materials and Methods
Animals
A total of 110 healthy male Sprague-Dawley rats, 45–60 days old and weighing 290–330 g, were provided by the Animal Center of Xuzhou Medical University, Jiangsu Province, China. The rats were randomized into three groups: sham (n = 10), 2-hour ischemia (n = 50), and 6-hour ischemia (n = 50). Rats in the ischemia groups underwent 2- or 6-hour ischemia followed by reperfusion for 0, 0.5, 2, 6, or 24 hours (n = 10 rats per time point). All rats were housed under diurnal lighting and had free access to food and water before the experiments. The protocols were approval by the Committee on Animal Experimental Guidelines of the Affiliated Hospital of Xuzhou Medical University (XZMU-A201204-057R).
Focal cerebral ischemia injury modeling
A rat model of unilateral middle cerebral artery occlusion was established using the modified Longa method (Longa et al., 1989). Rats were anesthetized intraperitoneally with 10% chloral hydrate (3 mL/kg). The left common, external, and internal carotid arteries were exposed via an incision in the neck and separated under a surgical microscope. The external carotid artery was ligated 0.8–1.0 cm from the common carotid artery, and the internal carotid artery was occluded. A 3-0 surgical monofilament nylon suture, blunted at the end, was gently inserted into the internal carotid artery through a small incision at the bifurcation. When the thread was extended 17–19 mm from the bifurcation and a slight resistance was felt, this indicated that the thread had been inserted into the origin of the middle cerebral artery at the circle of Willis, blocking blood flow in the middle cerebral artery trunk. The thread was ligated with a slipknot in the internal carotid artery, and the incision was sutured. The rats were returned to their cages with food and water and allowed to recover. Body temperature was maintained near 37°C using a heat pad. After 2 or 6 hours, the thread was withdrawn by approximately 10 mm to begin reperfusion. For the sham group, the procedure was identical except the thread was only inserted to a depth of 5 mm.
MRI scan
3.0 T MRI examination (Signa HD 3.0, GE Healthcare, Chicago, IL, USA) was performed at various time points after ischemia/perfusion. A rat coil (Chenguang Medical Technology Co., Ltd., Shanghai, China) was used as the receiver coil. The rats were anesthetized by an intraperitoneal injection of 10% chloral hydrate. Their heads were then placed in the center of the coil in the prone position. Echo planar imaging was used with the following parameters: repetition time, 6,800 ms; echo time, 93 ms; field of view, 8 cm × 6 cm; matrix, 64 × 64; number of excitations, 2; thickness, 2.4 mm; slice gap, 0.2 mm. After the scan, DWI data were transmitted to the workstation for postprocessing to obtain apparent diffusion coefficient (ADC) profiles. The relative ADC (rADC) for the abnormal signal area on a slice with marked ischemia in the region of interest (ROI) was calculated as follows: rADC = ADCROI / ADCcontralateral × 100%. The ratio of the DWI abnormal signal area (rS-DWI) on the selected slice (with marked ischemia) to that in the whole-brain slice area was calculated. Brains were removed after scanning.
Immunohistochemistry
After MRI, the whole brain from five rats in each group was removed immediately en bloc and postfixed for 24 hours in 4% paraformaldehyde in phosphate-buffered saline (PBS). The tissue was then frozen, and 12-μm consecutive coronal sections were prepared. Microwave antigen retrieval was performed in citrate buffer (pH 6.0), and the sections were then incubated in 3% hydrogen peroxide at 37°C to block endogenous peroxidase activity. Normal goat serum was added dropwise to block nonspecific binding, and STAT3 (1:100) and p-STAT3 (1:100) rabbit polyclonal antibodies (both from Cell Signaling Technology, Danvers, MA, USA) were added and incubated at 4°C overnight. Biotin-labeled goat anti-rabbit IgG (1:30; Yu Bo Biological Technology, Shanghai, China) was then added dropwise at 37°C for incubation for 25 minutes, followed by dropwise addition of horseradish peroxidase-labeled streptavidin working solution. Diaminobenzidine was added for color development, and hematoxylin was applied as a counterstain. PBS (0.01 M) was added instead of primary antibody for the negative control sections. Cells with a brown-stained nucleus or cytoplasm under a light microscope (Olympus, Tokyo, Japan) were considered positive.
Western blot assay
After MRI, five rats in each group were decapitated and their brains quickly removed. The ROI on the slice with the largest ischemic area revealed by MRI was rapidly separated. Nuclear proteins were extracted, and equal amounts of protein sample were separated by 7% sodium dodecyl sulfate polyacrylamide gel electrophoresis, then wet-transferred onto nitrocellulose membranes. The membranes were then blocked with 3% bovine serum albumin, incubated overnight at 4°C with diluted primary antibody (rabbit anti-STAT3 or rabbit anti-p-STAT3, both 1:100; Cell Signaling Technology) with freshly prepared PBS containing 3% skim milk powder, and then incubated with alkaline phosphatase-conjugated goat anti-rabbit IgG (1:30; Yu Bo Biological Technology). Nitroblue tetrazolium-5-bromo-4-chloro-3-indolyl phosphate (NBT-BCIP) was used for color development. Bands were analyzed using ImageJ software (National Institutes of Health, Bethesda, MD, USA). Relative optical density was calculated as: optical density of ischemic ROI/optical density of equivalent region in the sham group.
Statistical analysis
SPSS 16.0 for Windows (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Experimental data are expressed as the mean ± SD. One-way analysis of variance was used to compare DWI and ADC before and after cerebral ischemia/reperfusion, and STAT3 and p-STAT3 expression. The relationship between p-STAT3 expression and rADC or rS-DWI was analyzed by Pearson correlation analysis. P < 0.05 was considered statistically significant.
Results
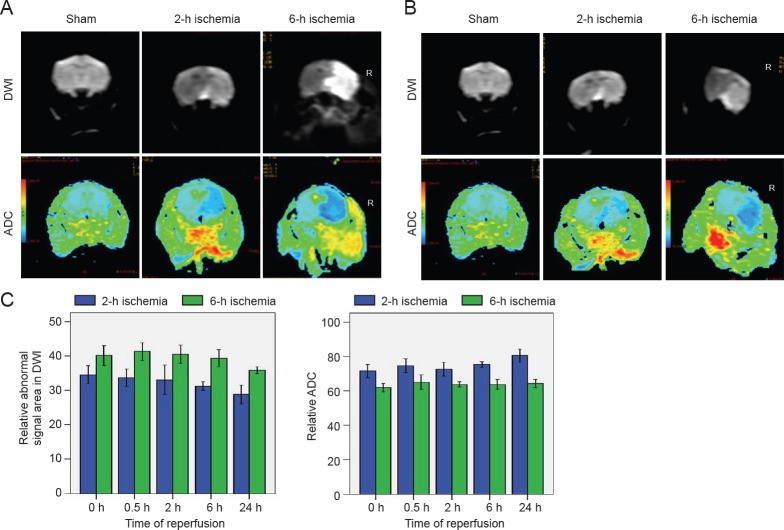
DWI in rat brain before and after acute cerebral ischemia/reperfusion
In the sham group, DWI findings were as expected, and ADC values were similar across both cerebral hemispheres. In both ischemia groups, before reperfusion, DWI showed patchy hyperintensity in the right corpus striatum and frontoparietal cortex, and ADC pseudocolor images showed an abnormal blue signal with blurred edges. The 6-hour ischemia group had larger rS-DWI and smaller ADC values than the 2-hour ischemia group (Figure 1). In the 2-hour ischemia group, after 24 hours of reperfusion, the rS-DWI was significantly smaller than before reperfusion, and the ADC was partially restored. After 24 hours of reperfusion in the 6-hour group, the rS-DWI was slightly lower than before reperfusion, and the ADC value was slightly greater (Figure 1).
Figure 1.
Brain diffusion-weighted magnetic resonance imaging (DWI) and apparent diffusion coefficient (ADC) in rat models of focal cerebral ischemia/reperfusion injury.
(A) Before reperfusion. In sham-operated animals, DWI findings were as expected and ADC values were similar across both cerebral hemispheres. In animals that underwent ischemia for 2 or 6 h, DWI showed patchy hyperintensity in the right hemisphere, and ADC pseudocolor images showed an abnormal blue signal with blurred edges. (B) After 24 h of reperfusion, the relative abnormal signal area was smaller in the 2- and 6-h ischemia groups than before reperfusion. (C) DWI relative abnormal signal area (%). (D) Relative ADC in region of interest (%). Data are expressed as the mean ± SD. *P < 0.05, vs. 0 h (before reperfusion) (one-way analysis of variance). h: Hours.
Changes in STAT3 expression and activation after acute cerebral ischemia/reperfusion
Immunohistochemistry showed that p-STAT3-positive cells were rarely expressed in brain tissue from sham-operated rats, but in rats with ischemia, expression in the ischemic area increased with reperfusion time. The positive cells were circular or oval, and mainly astrocytes, followed in number by neurons. After 24 hours of reperfusion, there was neural nuclear condensation, cell body shrinkage and deformation, and larger astrocytes with abundant cytoplasm (Figure 2).
Figure 2.
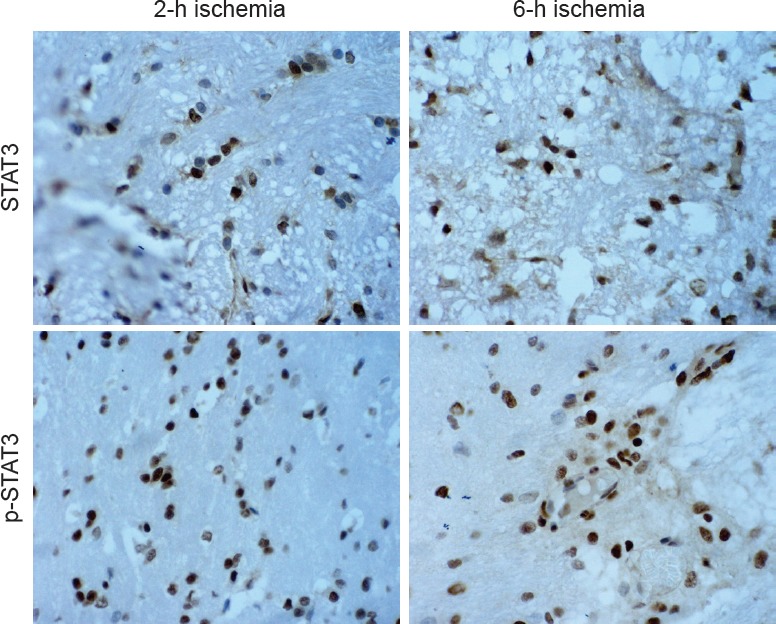
Immunohistochemical staining of STAT3 and p-STAT3 in the brain 24 h after reperfusion (× 400).
STAT3-positive cells were round or oval. The yellow-brown immunoreactive products were distributed in the cytoplasm. p-STAT3-positive cells were elliptical, and mainly astrocytes and neurons. The yellow-brown immunoreactive products were mainly distributed in the nucleus. h: Hours; STAT3: signal transducer and activator of transcription 3; p-STAT3: phosphorylated-STAT3.
In the western blot assay, a low level of p-STAT3 was detected in brain tissue from sham-operated rats. In rats with ischemia, expression increased significantly after 0.5 hours of reperfusion, decreased slightly after 2 hours, and peaked at 24 hours (Figure 3).
Figure 3.
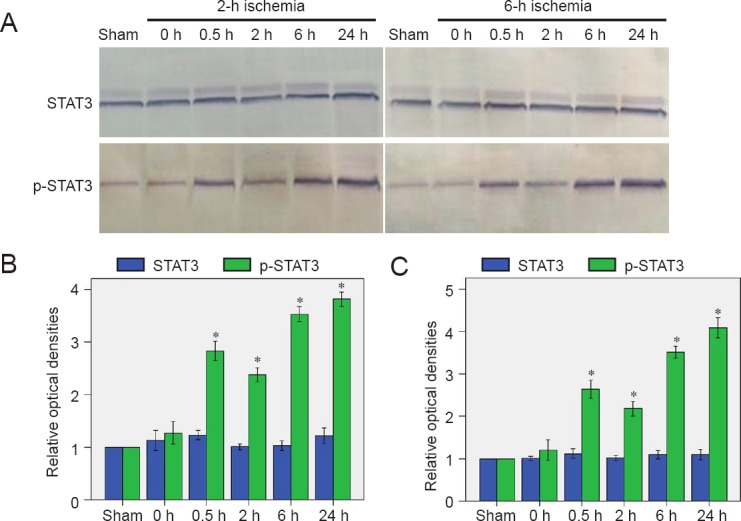
Changes in STAT3 expression and activation in the brain after acute cerebral ischemia/reperfusion.
(A) Western blot assay of STAT3 and p-STAT3. (B, C) Relative optical densities of STAT3 and p-STAT3 in the 2-h (B) and 6-h (C) ischemia groups (n = 10). (C) Relative optical densities of STAT3 and p-STAT3 in the 6-h ischemia group (n = 10). Data are expressed as the mean ± SD. *P < 0.05, vs. 0 h (before reperfusion) (one-way analysis of variance). h: Hour(s); STAT3: signal transducer and activator of transcription 3; p-STAT3: phosphorylated-STAT3.
Correlation between p-STAT3 expression and DWI
Data from different time points after reperfusion showed that p-STAT3 expression was positively correlated with rADC (2-hour ischemia group: r = 0.803, P < 0.05; 6-hour ischemia group: r = 0.697, P < 0.05) and negatively correlated with the rS-DWI (2-hour ischemia group: r = −0.680, P < 0.05; 6-hour ischemia group: r = −0.678, P < 0.05) (Figure 4).
Figure 4.
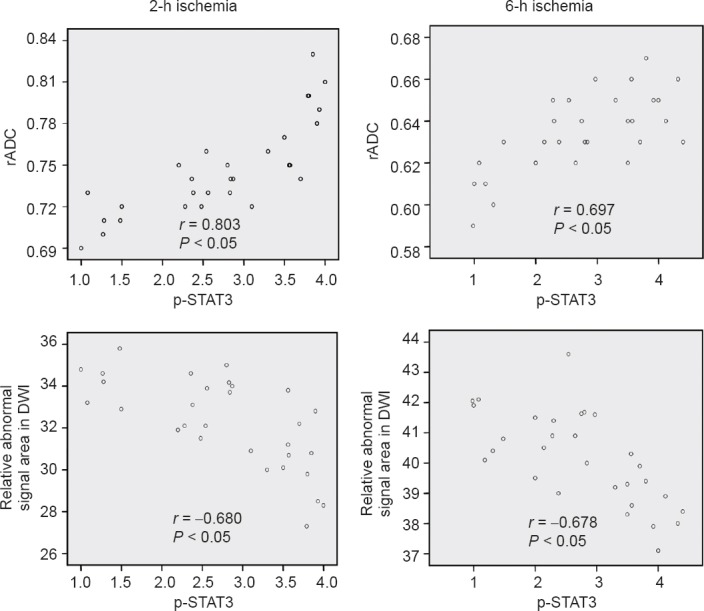
Correlation of phosphorylated signal transducer and activator of transcription 3 (p-STAT3) with relative apparent diffusion coefficient (rADC) and relative abnormal signal area in diffusion-weighted magnetic resonance imaging at different reperfusion time points.
p-STAT3 expression (expressed as relative optical density) showed a positive correlation with rADC and a negative correlation with relative abnormal signal area in diffusion-weighted magnetic resonance imaging. h: Hours.
Discussion
The JAK-STAT pathway has been clearly described in recent years (Jiang et al., 2013). As a family of cytoplasmic proteins capable of binding to DNA in the regulatory region of target genes, STATs are important downstream targets of JAKs (Liu et al., 2014). After binding to the corresponding ligand, cytokine receptors on the cell membrane induce mutual phosphorylation of JAK in the cell body. Cytoplasmic STAT has an SH2 domain, by which STAT is translocated to the specific tyrosine phosphorylation site of the receptor complex and becomes activated. Activated STAT separates from the receptor to form homo- or heterodimers and translocates to the nucleus where it initiates gene transcription (Yang et al., 2010). STAT3 is in a class of DNA-binding proteins involved in regulating various physiological functions, such as cell growth, malignant transformation, and apoptosis. Hoffmann et al. (2015) reported that STAT3 nuclear translocation in astrocytes in the cerebral cortex induced a variety of changes in glial cells after ischemia. In the present study, immunohistochemistry confirmed that non-activated STAT3 was expressed in the cytoplasm. p-STAT3-positive cells were rarely expressed in sham-operated rat brain tissue, but increased with longer ischemia/reperfusion times. Most immunoreactive products were observed in the nuclei of astrocytes, followed in number by neurons. This finding is likely associated with the mechanism by which activated STAT3 mediates gene transcription by forming homo- or heterodimers and translocating to the nucleus. However, the reason for high STAT3 protein expression and activation after cerebral ischemia remains unclear. It may be related to the rapid synthesis and expression induction of interleukin-6 and its receptors by neuronal and glial cells during cerebral ischemia.
Semi-quantitative western blot assay revealed that STAT3 protein expression did not change significantly with different reperfusion periods following ischemia for 2 or 6 hours. By contrast, p-STAT3 expression increased gradually, whereas it was barely detectable in the sham group. The increase in p-STAT3 levels after 0.5 hours of reperfusion may be related to the involvement of STAT3, c-Fos, and c-Jun in the transcriptional regulation of immediate early genes in neurons (Amantea et al., 2011). The significant increase in p-STAT3 levels after 24 hours of reperfusion may be related to ATP depletion during ischemia and significantly increased ATP levels after reperfusion; conversely, a marked proliferation of reactive glial cells and microglia was induced by ischemic brain damage, and increased cytokines and growth factors were released as reperfusion continued.
The basic pathology of the rS-DWI is that Na+/K+–ATP enzyme pump function is reduced due to ischemia and hypoxia, which leads to sodium retention and consequent cytotoxic edema, resulting in slowed molecular diffusion; this is demonstrated by the low ADC and DWI hyperintensity (Kim et al., 2006; Cereda et al., 2015; Lago et al., 2015; Song et al., 2015; Aoki et al., 2016; Freitag et al., 2016; Grams et al., 2016; Jiang et al., 2016; Kaseka et al., 2016; Kohno et al., 2016; Kvistad et al., 2016; Onofrj et al., 2016; Tamura et al., 2016; Xin and Han, 2016; Zhang et al., 2016; Zhou et al., 2016; Abdelgawad et al., 2017; Bekiesinska-Figatowska et al., 2017; Heiss and Zaro Weber, 2017). The decrease in ADC was highly consistent with the ATP-labeled defect area and decreased tissue pH area; and the decrease in ADC in ischemic brain damage was consistent with the level of cytotoxic edema caused by cell energy metabolism disorders (Anticoli et al., 2015; Baron et al., 2015; Brown et al., 2015; Eom et al., 2015; Gory et al., 2015; Kate et al., 2015; Landais, 2015; Li et al., 2015a; Makin et al., 2015; Mawet et al., 2015; Michałowska et al., 2015; Odland et al., 2015; Ostwaldt et al., 2015; Sasai et al., 2015; Yaghi et al., 2015). As infarction time increases (> 24 hours), there are corresponding increases in vasogenic edema, extracellular space water, diffusion speed, and ADC values (Maruyama et al., 2015).
As the JAK-STAT signaling pathway is activated during cerebral ischemia, JAK1 expression in cortical pyramidal neurons and striatal cells increases, and STAT3 nuclear translocation also increases, in rats with focal cerebral ischemia/reperfusion injury; this results in extensive proliferation of reactive microglia and macrophages (Li and Zhang, 2003; Zechariah et al., 2010; Jiang et al., 2013; Feng et al., 2015; Jung et al., 2015; Deng et al., 2016). Previous studies have demonstrated that the gp130-STAT signaling pathway could be activated by the nuclear translocation of STAT3, and that this activation in astrocytes correlates closely with gp130 expression (Jang et al., 2014; Song et al., 2014; Xu et al., 2015; Zhang et al., 2015; Guo et al., 2016). Selection of the samples used in the present experiment was based on MRI findings. STAT3 activation levels before and after ischemia/reperfusion correlated with the rS-DWI in the ischemic region and rADC. This finding indicated that with aggravation of cytotoxic and vasogenic edema, the status of some membrane channels changed, which affected certain cell signaling pathways and STAT3 activation. This correlation helps to identify biochemical changes of JAK-STAT signaling in brain tissue after ischemia/reperfusion. Further research is needed to determine whether blocking STAT3 phosphorylation could prevent neuronal necrosis or apoptosis due to ischemia to achieve neuroprotective effects and minimize ischemia/reperfusion injury, and whether it could be reflected in MRI. This correlation also provides a theoretical and experimental basis for the clinical treatment of cerebral ischemia.
Footnotes
Conflicts of interest: There is no conflict of interest of any authors in relation to the submission. This article is freely available online through the J Neurosci Author Open Choice option.
Research ethics: The study protocol was approved by the Committee on Animal Experimental Guidelines of the Affiliated Hospital of Xuzhou Medical University, China (approval No. XZMU-A201204-057R). The study followed the National Institutes of Health Guide for the Care and Use of Laboratory animals (NIH Publications No. 8023, revised 1978), and “Consensus Author Guidelines on Animal Ethics and Welfare” produced by the International Association for Veterinary Editors (IAVE). The article was prepared in accordance with the “Animal Research: Reporting of In Vivo Experiments Guidelines” (ARRIVE Guidelines).
Contributor agreement: A statement of “Publishing Agreement” has been signed by an authorized author on behalf of all authors prior to publication.
Plagiarism check: This paper has been checked twice with duplication-checking software iThenticate.
Peer review: A double-blind and stringent peer review process has been performed to ensure the integrity, quality and significance of this paper.
Copyedited by Slone-Murphy J, de Souza M, Yu J, Li CH, Qiu Y, Song LP, Zhao M
References
- 1.Abdelgawad EA, Higazi MM, Abdelbaky AO, Abdelghany HS. Diagnostic performance of CT cerebral blood volume colour maps for evaluation of acute infarcts; comparison with diffusion-weighted MRI within 12hours of major stroke onset. J Neuroradiol. 2017;44:10–16. doi: 10.1016/j.neurad.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 2.Amantea D, Tassorelli C, Russo R, Petrelli F, Morrone LA, Bagetta G, Corasaniti MT. Neuroprotection by leptin in a rat model of permanent cerebral ischemia: effects on STAT3 phosphorylation in discrete cells of the brain. Cell Death Dis. 2011;2:e238. doi: 10.1038/cddis.2011.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anticoli S, Pezzella FR, Pozzessere C, Gallelli L, Bravi MC, Caso V, Siniscalchi A. Transient ischemic attack fast-track and long-term stroke risk: role of diffusion-weighted magneticresonance imaging. J Stroke Cerebrovasc Dis. 2015;24:2110–2116. doi: 10.1016/j.jstrokecerebrovasdis.2015.05.016. [DOI] [PubMed] [Google Scholar]
- 4.Aoki J, Sakamoto Y, Kimura K. Intravenous thrombolysis increases the rate of dramatic recovery in patients with acute stroke with an unknown onset time and negative FLAIR MRI. J Neuroimaging. 2016;26:414–419. doi: 10.1111/jon.12323. [DOI] [PubMed] [Google Scholar]
- 5.Baron CA, Kate M, Gioia L, Butcher K, Emery D, Budde M, Beaulieu C. Reduction of diffusion-weighted imaging contrast of acute ischemic stroke at short diffusion times. Stroke. 2015;46:2136–2141. doi: 10.1161/STROKEAHA.115.008815. [DOI] [PubMed] [Google Scholar]
- 6.Beck C, Kruetzelmann A, Forkert ND, Juettler E, Singer OC, Köhrmann M, Kersten JF, Sobesky J, Gerloff C, Fiehler J, Schellinger PD, Röther J, Thomalla G. A simple brain atrophy measure improves the prediction of malignant middle cerebral artery infarction by acute DWI lesion volume. J Neurol. 2014;261:1097–1103. doi: 10.1007/s00415-014-7324-9. [DOI] [PubMed] [Google Scholar]
- 7.Bekiesinska-Figatowska M, Duczkowska A, Szkudlinska-Pawlak S, Duczkowski M, Madzik J, Cabaj A, Krupa K, Peczkowski P, Bragoszewska H. Diffusion restriction in the corticospinal tracts and the corpus callosum in neonates after cerebral insult. Brain Dev. 2017;39:203–210. doi: 10.1016/j.braindev.2016.10.003. [DOI] [PubMed] [Google Scholar]
- 8.Brown TA, Luby M, Shah J, Giannakidis D, Latour LL. Magnetic resonance imaging in acute ischemic stroke patients with mild symptoms: an opportunity tostandardize intravenous thrombolysis. J Stroke Cerebrovasc Dis. 2015;24:1832–1840. doi: 10.1016/j.jstrokecerebrovasdis.2015.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cereda CW, Christensen S, Campbell BC, Mishra NK, Mlynash M, Levi C, Straka M, Wintermark M, Bammer R, Albers GW, Parsons MW, Lansberg MG. A benchmarking tool to evaluate computer tomography perfusion infarct core predictions against a DWI standard. J Cereb Blood Flow Metab. 2015;36:1780–1789. doi: 10.1177/0271678X15610586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Deng R, Zhao FY, Zhang L, Li DY, Mu DZ. Role of STAT3 signaling pathway in hypoxic-ischemic brain damage of neonatal rats. Zhongguo Dang Dai Er Ke Za Zhi. 2016;18:78–84. doi: 10.7499/j.issn.1008-8830.2016.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eom KS, Kim DW, Kang S. Emergency microsurgical embolectomy in acute ischemic stroke with diffusion-negative MRI. Neurol Neurochir Pol. 2015;49:432–435. doi: 10.1016/j.pjnns.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 12.Feng Q, Wang YI, Yang Y. Neuroprotective effect of interleukin-6 in a rat model of cerebral ischemia. Exp Ther Med. 2015;9:1695–1701. doi: 10.3892/etm.2015.2363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Freitag MT, Bickelhaupt S, Ziener C, Meier-Hein K, Radtke JP, Mosebach J, Kuder TA, Schlemmer HP, Laun FB. Selected clinically established and scientific techniques of diffusion-weighted MRI. In the context of imaging in oncology. Radiologe. 2016;56:137–147. doi: 10.1007/s00117-015-0066-6. [DOI] [PubMed] [Google Scholar]
- 14.Gory B, Sivan-Hoffmann R, Riva R, Labeyrie PE, Eldesouky I, Sadeh-Gonike U, Signorelli F, Turjman F. DWI lesions reversal in posterior circulation stroke after reperfusion: Two illustrative cases and review of the literature. J Neuroradiol. 2015;42:184–187. doi: 10.1016/j.neurad.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 15.Grams RW, Kidwell CS, Doshi AH, Drake K, Becker J, Coull BM, Nael K. Tissue-negative transient ischemic attack: is there a role for perfusion MRI? Am J Roentgenol. 2016;207:157–162. doi: 10.2214/AJR.15.15447. [DOI] [PubMed] [Google Scholar]
- 16.Guo H, Zhou H, Lu J, Qu Y, Yu D, Tong Y. Vascular endothelial growth factor: an attractive target in the treatment of hypoxic/ischemic brain injury. Neural Regen Res. 2016;11:174–179. doi: 10.4103/1673-5374.175067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Heiss WD, Zaro Weber O. Validation of MRI determination of the penumbra by PET measurements in ischemic stroke. J Nucl Med. 2017;58:187–193. doi: 10.2967/jnumed.116.185975. [DOI] [PubMed] [Google Scholar]
- 18.Hoffmann CJ, Harms U, Rex A, Szulzewsky F, Wolf SA, Grittner U, Lättig-Tünnemann G, Sendtner M, Kettenmann H, Dirnagl U, Endres M, Harms C. Vascular signal transducer and activator of transcription-3 promotes angiogenesis and neuroplasticity long-term after stroke. Circulation. 2015;131:1772–1782. doi: 10.1161/CIRCULATIONAHA.114.013003. [DOI] [PubMed] [Google Scholar]
- 19.Jang SS, Choi JH, Im DS, Park S, Park JS, Park SM, Joe EH, Jou I, Suh YH. The phosphorylation of STAT6 during ischemic reperfusion in rat cerebral cortex. Neuroreport. 2014;25:18–22. doi: 10.1097/WNR.0000000000000022. [DOI] [PubMed] [Google Scholar]
- 20.Jia L, Wang F, Gu X, Weng Y, Sheng M, Wang G, Li S, Du H, Yu W. Propofol postconditioning attenuates hippocampus ischemia-reperfusion injury via modulating JAK2/STAT3 pathway in rats after autogenous orthotropic liver transplantation. Brain Res. 2017;1657:202–207. doi: 10.1016/j.brainres.2016.12.015. [DOI] [PubMed] [Google Scholar]
- 21.Jiang C, Xu Q, Xu K, Dai H, Zhang Z, Wu W, Ni J. The effect of erythropoietin on focal cerebral ischemia reperfusion in rats by observing STAT1, STAT3 protein and MRI expression. Linchuang Fangshe Xue Zazhi. 2012;31:1036–1040. [Google Scholar]
- 22.Jiang C, Xu Q, Xu K, Dai H, Zhang Z, Wu W, Ni J. Effects of erythropoietin on STAT1 and STAT3 levels following cerebral ischemia-reperfusion in rats. Int J Neurosci. 2013;123:684–690. doi: 10.3109/00207454.2013.817409. [DOI] [PubMed] [Google Scholar]
- 23.Jiang CJ, Wang ZJ, Zhao YJ, Zhang ZY, Tao JJ, Ma JY. Erythropoietin reduces apoptosis of brain tissue cells in rats after cerebral ischemia/reperfusion injury: a characteristic analysis using magnetic resonance imaging. Neural Regen Res. 2016;11:1450–1455. doi: 10.4103/1673-5374.191219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jung JE, Karatas H, Liu Y, Yalcin A, Montaner J, Lo EH, van Leyen K. STAT-dependent upregulation of 12/15-lipoxygenase contributes to neuronal injury after stroke. J Cereb Blood Flow Metab. 2015;35:2043–2051. doi: 10.1038/jcbfm.2015.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaseka ML, Moharir M, deVeber G, MacGregor D, Askalan R, Dlamini N. Prognostication value of descending corticospinal tract DWI signal in neonatal cerebral sinovenous thrombosis. Pediatr Neurol. 2016;59:90–94. doi: 10.1016/j.pediatrneurol.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 26.Kate MP, Riaz P, Gioia L, Sivakumar L, Jeerakathil T, Buck B, Beaulieu C, Butcher K. Dynamic evolution of diffusion-weighted imaging lesions in patients with minor ischemic stroke. Stroke. 2015;46:2318–2321. doi: 10.1161/STROKEAHA.115.009775. [DOI] [PubMed] [Google Scholar]
- 27.Kim EY, Ryoo JW, Roh HG, Lee KH, Kim SS, Song IC, Chang KH, Na DG. Reversed discrepancy between CT and diffusion-weighted MR imaging in acute ischemic stroke. Am J Neuroradiol. 2006;27:1990–1995. [PMC free article] [PubMed] [Google Scholar]
- 28.Kim HC, Kim E, Bae JI, Lee KH, Jeon YT, Hwang JW, Lim YJ, Min SW, Park HP. Sevoflurane postconditioning reduces apoptosis by activating the JAK-STAT pathway after transient global cerebral ischemia in rats. J Neurosurg Anesthesiol. 2017;29:37–45. doi: 10.1097/ANA.0000000000000331. [DOI] [PubMed] [Google Scholar]
- 29.Kohno N, Okada K, Yamagata S, Takayoshi H, Yamaguchi S. Distinctive patterns of three-dimensional arterial spin-labeled perfusion magnetic resonance imaging in subtypes of acute ischemic stroke. J Stroke Cerebrovasc Dis. 2016;25:1807–1812. doi: 10.1016/j.jstrokecerebrovasdis.2016.03.035. [DOI] [PubMed] [Google Scholar]
- 30.Kvistad CE, Oygarden H, Logallo N, Thomassen L, Waje-Andreassen U, Moen G, Naess H. A stress-related explanation to the increased blood pressure and its course following ischemic stroke. Vasc Health Risk Manag. 2016;12:435–442. doi: 10.2147/VHRM.S109032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lago A, Tembl JI, López-Cuevas R, Vallés J, Santos MT, Moscardó A, Parkhutik V. Characterisation of DWI-MRI confirmed cerebral infarcts in patients with subarachnoid haemorrhage and their association with MMP-9 levels. Neurol Res. 2015;37:688–692. doi: 10.1179/1743132815Y.0000000045. [DOI] [PubMed] [Google Scholar]
- 32.Landais A. Reversible splenium diffusion weighted MRI changes associated with hypoglycemia. J Diabetes Complications. 2015;29:607–610. doi: 10.1016/j.jdiacomp.2015.02.012. [DOI] [PubMed] [Google Scholar]
- 33.Li HC, Zhang GY. Activation of STAT3 induced by cerebral ischemia in rat hippocampus and its possible mechanisms. Sheng Li Xue Bao. 2003;55:311–316. [PubMed] [Google Scholar]
- 34.Li JL, Li CS, Fu JH, Zhang K, Xu R, Xu WJ. Evaluation of cranial and cervical arteries and brain tissue in transient ischemic attack patients with magnetic resonance angiography and diffusion-weighted imaging. Med Sci Monit. 2015a;21:1726–1731. doi: 10.12659/MSM.894388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li L, Li H, Li M. Curcumin protects against cerebral ischemia-reperfusion injury by activating JAK2/STAT3 signaling pathway in rats. Int J Clin Exp Med. 2015b;8:14985–14991. [PMC free article] [PubMed] [Google Scholar]
- 36.Liu X, Zhang X, Zhang J, Kang N, Zhang N, Wang H, Xue J, Yu J, Yang Y, Cui H, Cui L, Wang L, Wang X. Diosmin protects against cerebral ischemia/reperfusion injury through activating JAK2/STAT3 signal pathway in mice. Neuroscience. 2014;268:318–327. doi: 10.1016/j.neuroscience.2014.03.032. [DOI] [PubMed] [Google Scholar]
- 37.Longa EZ, Weinstein PR, Carlson S, Cummins R. Reversible middle cerebral artery occlusion without craniectomy in rats. Stroke. 1989;20:84–91. doi: 10.1161/01.str.20.1.84. [DOI] [PubMed] [Google Scholar]
- 38.Makin SD, Doubal FN, Dennis MS, Wardlaw JM. Clinically confirmed stroke with negative diffusion-weighted imaging magnetic resonance imaging:longitudinal study of clinical outcomes, stroke recurrence, and systematic review. Stroke. 2015;46:3142–3148. doi: 10.1161/STROKEAHA.115.010665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Maruyama D, Fukuda K, Kataoka H, Morita Y, Nishimura K, Kawamura Y, Iihara K. Evaluation of carotid artery outward remodeling by T1-weighted magnetic resonance imaging in carotid endarterectomy and stenting. J Vasc Surg. 2015;61:1464–1471.e1. doi: 10.1016/j.jvs.2015.01.029. [DOI] [PubMed] [Google Scholar]
- 40.Mawet J, Eikermann-Haerter K, Park KY, Helenius J, Daneshmand A, Pearlman L, Avery R, Negro A, Velioglu M, Arsava EM, Ay H, Ayata C. Sensitivity to acute cerebral ischemic injury in migraineurs: A retrospective case-control study. Neurology. 2015;85:1945–1949. doi: 10.1212/WNL.0000000000002166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Michałowska I, Furmanek MI, Smaga E, Juraszyński Z, Zieliński T, Chełstowska S, Kuśmierczyk M, Szpakowski E, Mierzyńska A, Walecki JM. Evaluation of brain lesions in patients after coronary artery bypass grafting using MRI with the emphasis on susceptibility-weighted imaging. Kardiochir Torakochirurgia Pol. 2015;12:1–7. doi: 10.5114/kitp.2015.50560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Odland A, Særvoll P, Advani R, Kurz MW, Kurz KD. Are the current MRI criteria using the DWI-FLAIR mismatch concept for selection of patients with wake-up stroke to thrombolysis excluding too many patients? Scand J Trauma Resusc Emerg Med. 2015;23:22. doi: 10.1186/s13049-015-0101-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Onofrj V, Delli Pizzi S, Franciotti R, Taylor JP, Perfetti B, Caulo M, Onofrj M, Bonanni L. Medio-dorsal thalamus and confabulations: Evidence from a clinical case and combined MRI/DTI study. Neuroimage Clin. 2016;12:776–784. doi: 10.1016/j.nicl.2016.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ostwaldt AC, Usnich T, Nolte CH, Villringer K, Fiebach JB. Case report of a young stroke patient showing interim normalization of the MRI diffusion-weighted imaging lesion. BMC Med Imaging. 2015;15:33. doi: 10.1186/s12880-015-0077-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sasai H, Shimozawa N, Asano T, Kawamoto N, Yamamoto T, Kimura T, Kawamoto M, Matsui E, Fukao T. Successive MRI findings of reversible cerebral white matter lesions in a patient with cystathionine β-synthase deficiency. Tohoku J Exp Med. 2015;237:323–327. doi: 10.1620/tjem.237.323. [DOI] [PubMed] [Google Scholar]
- 46.Song CG, Yang X, Min LQ, Liu CX, Zhao CS. The effect of procyanidin on expression of STAT1 in type 2 diabetes mellitus SD rats with focal cerebral ischemia. Neuro Endocrinol Lett. 2014;35:68–72. [PubMed] [Google Scholar]
- 47.Song RR, Yu XF, Yerfan J, Sun JZ, Mao YY, Guo Y, Chen ZC, Zhang MM. Cerebral lesions of DWI hyperintensity in patients with subacute stroke assessed by intravoxel incoherent motion technique. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2015;44:632–637. doi: 10.3785/j.issn.1008-9292.2015.11.06. 644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tamura G, Ihara S, Morota N. Reversible diffusion weighted imaging hyperintensities during the acute phase of ischemic stroke in pediatric moyamoya disease: a case report. Childs Nerv Syst. 2016;32:1531–1535. doi: 10.1007/s00381-016-3052-z. [DOI] [PubMed] [Google Scholar]
- 49.Xin Y, Han FG. Diagnostic accuracy of computed tomography perfusion in patients with acute stroke: A meta-analysis. J Neurol Sci. 2016;360:125–130. doi: 10.1016/j.jns.2015.11.046. [DOI] [PubMed] [Google Scholar]
- 50.Xu Q, Jiang C, Rong Y, Yang C, Liu Y, Xu K. The effects of fludarabine on rat cerebral ischemia. J Mol Neurosci. 2015;55:289–296. doi: 10.1007/s12031-014-0320-9. [DOI] [PubMed] [Google Scholar]
- 51.Yaghi S, Herber C, Willey JZ, Andrews HF, Boehme AK, Marshall RS, Lazar RM, Boden-Albala B. Itemized NIHSS subsets predict positive MRI strokes in patients with mild deficits. J Neurol Sci. 2015;358:221–225. doi: 10.1016/j.jns.2015.08.1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yang YL, Zhu WX, chen YH, Chen MN. Protection of erythropoietin on cerebral ischemia/reperfusion injury. Zhongguo Yingyong Shenglixue Zazhi. 2010;26:152–153. [PubMed] [Google Scholar]
- 53.Zechariah A, ElAli A, Hermann DM. Combination of tissue-plasminogen activator with erythropoietin induces blood-brain barrier permeability, extracellular matrix disaggregation, and DNA fragmentation after focal cerebral ischemia in mice. Stroke. 2010;41:1008–1012. doi: 10.1161/STROKEAHA.109.574418. [DOI] [PubMed] [Google Scholar]
- 54.Zhang S, Yao Y, Shi J, Tang X, Zhao L, Zhu W. The temporal evolution of diffusional kurtosis imaging in an experimental middle cerebral artery occlusion (MCAO) model. Magn Reson Imaging. 2016;34:889–895. doi: 10.1016/j.mri.2016.04.016. [DOI] [PubMed] [Google Scholar]
- 55.Zhang Y, Zheng J, Zhou Z, Zhou H, Wang Y, Gong Z, Zhu J. Fractalkine promotes chemotaxis of bone marrow-derived mesenchymal stem cells towards ischemic brain lesions through Jak2 signaling and cytoskeletal reorganization. FEBS J. 2015;282:891–903. doi: 10.1111/febs.13187. [DOI] [PubMed] [Google Scholar]
- 56.Zhou IY, Guo Y, Igarashi T, Wang Y, Mandeville E, Chan ST, Wen L, Vangel M, Lo EH, Ji X, Sun PZ. Fast diffusion kurtosis imaging (DKI) with Inherent COrrelation-based Normalization (ICON) enhances automatic segmentation of heterogeneous diffusion MRI lesion in acute stroke. Nmr Biomed. 2016;29:1670–1677. doi: 10.1002/nbm.3617. [DOI] [PMC free article] [PubMed] [Google Scholar]