Abstract
We conducted four studies to examine the relationship between over-exercise and suicidality. Study 1 investigated whether over-exercise predicted suicidal behavior after controlling for other eating disorder behaviors in a patient sample of 204 women (144 with Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) Bulimia Nervosa [BN]). Study 2 tested the prospective association between over-exercise and acquired capability for suicide (ACS) in a sample of 171 college students followed for 3–4 weeks. Study 3 investigated whether pain insensitivity accounted for the relationship between over-exercise and ACS in a new sample of 467 college students. Study 4 tested whether ACS accounted for the relationship between over-exercise and suicidal behavior in a sample of 512 college students. In Study 1, after controlling for key covariates, over-exercise was the only disordered eating variable that maintained a significant relationship with suicidal behavior. In Study 2, Time 1 over-exercise was the only disordered eating behavior that was associated with Time 2 ACS. In Study 3, pain insensitivity accounted for the relationship between over-exercise and ACS. In Study 4, ACS accounted for the relationship between over-exercise and suicidal behavior. Over-exercise appears to be associated with suicidal behavior, an association accounted for by pain insensitivity and the acquired capability for suicide; notably, this association was found across a series of four studies with different populations.
Keywords: Bulimia nervosa, Disordered eating, Exercise, Over-exercise, Compulsivity, Suicidal behavior, Suicide
1. Introduction
Eating disorders convey a substantial mortality risk. Although the mortality rate for bulimia nervosa (BN) is lower than for anorexia nervosa (3.9% as compared to 10%, respectively; American Psychiatric Association, 2000; Crow et al., 2009), it is still elevated as compared to the general population. Further, suicide rates among individuals with BN are higher than in the general population (Preti et al., 2011). Specifically, in their recent meta-analysis, Preti et al. (2011) found that the standardized mortality rate (i.e., the ratio of the number of deaths observed in a sample compared with the number of deaths expected in the population) for individuals with BN was 7.5. Additionally, approximately one-third of women with BN attempt suicide at least once during their lifetime (e.g., Bulik et al., 1999; Corcos et al., 2002; Franko and Keel, 2006). This elevated rate of suicidal behavior within BN populations is no table given that the single best predictor of completed suicide is a previous attempt (e.g., Jenkins et al., 2002).
The interpersonal-psychological theory of suicide (IPTS) identifies three essential variables that must be in place before one can enact a lethal suicide attempt: thwarted belongingness, perceived burdensomeness, and the acquired capability for suicide (Joiner, 2005). Thwarted belongingness refers to feelings of loneliness and the perception that one does not have meaningful relationships. Perceived burdensomeness occurs when someone makes the miscalculation that his or her death is worth more to others than his or her life, and results from external factors—job loss, physical illness, and family conflict (Van Orden et al., 2010). The acquired capability for suicide refers to the ability to inflict potentially lethal self-harm and is attained by repeatedly subjecting the body to painful and provocative experiences. According to the theory, when individuals repeatedly experience pain and/or provocation, they habituate to physical pain and become less fearful of pain and death. They are then more readily able to inflict physical harm upon themselves, should they desire to do so (Joiner, 2005). As such, repeated engagement in self-injurious behavior may eventually lead to greater acquired capability for suicide. In combination with thwarted belongingness and perceived burdensomeness (the determinants of suicidal desire, according to the theory), having the acquired capability for suicide increases one's risk for death by suicide (Joiner, 2005; Joiner et al., 2009).
Thus far the IPTS has been investigated in past attempters (Van Orden et al., 2008), undergraduates (e.g., Davidson et al., 2011), military populations (e.g., Bryan and Anestis, 2011), and suicidal young adults (Joiner et al., 2009). Recently, one study tested a component of the IPTS, the acquired capability for suicide, in a population of women with anorexia nervosa (AN) (Selby et al., 2010). Across two studies, the authors found that dietary restraint was associated with suicidal behavior (i.e., number of previous attempts) among individuals with AN-restricting subtype. Provocative behaviors (e.g., binging, purging, self-injury, substance use), however, linked AN-binge/purge subtype to suicidal behavior.
To our knowledge, no study has tested constructs of the IPTS in a sample of people with symptoms of BN, despite the fact that individuals with BN display increased rates of suicidal behavior compared to the general population (Bulik et al., 1999; Corcos et al., 2002; Franko and Keel, 2006; Preti et al., 2011). Various symptoms of BN may be both provocative and painful. Specifically, the use of self-induced vomiting, laxatives, and over-exercise may cause physical pain through esophagitis, abdominal cramping and exercise-induced injury (Mehler and Weiner, 1994). Given the recurrent nature of these behaviors in eating disorders, repeated exposure to pain during purging and non-purging episodes may contribute to the acquired capability for suicide. Using the IPTS framework, the present project examines whether acquired capability mediates the relationship between painful eating disorder behaviors and suicidal behavior. We were specifically interested at looking at the disordered eating behavior of over-exercise due to its noted association with pain tolerance (e.g., Ryan and Kovacic, 1966) and suicidality (e.g., Brown and Blanton, 2002), and because over-exercise often results in pain and injury (e.g., Veale, 1987; McKenzie, 1999). Behaviors such as vomiting and laxative abuse involve pain and bodily damage (e.g., erosion of dental enamel and cavities, abrasions to the back of the hand [Russell's sign], esophagitis and risk of esophageal tear, intense abdominal cramping, light headedness and headache, marked edema and fluid retention). Further, prolonged periods of restriction require one to overcome hunger pains and intense discomfort. However, we hypothesized that over-exercise would be a stronger predictor of acquired capability for suicide than other compensatory behaviors. We further predicted that the acquired capability for suicide would mediate the relationship between over-exercise and suicidality. For the current studies, “over-exercise” was defined as vigorous exercise engaged in as a means of controlling shape and weight.
Several lines of research implicate over-exercise as a potentially potent predictor of suicidal behavior, over and above other compensatory behaviors. First, over-exercise can result in serious physical damage (e.g., Veale, 1987; McKenzie, 1999), and one's history of experiences with pain is believed to be associated with increased levels of acquired capability for suicide (Joiner, 2005). Healthy exercise is extolled as beneficial for physical health and emotional wellbeing, and in fact has been found to decrease depression (e.g., Mota-Pereira et al., 2011). However, over-exercise is frequently associated with painful outcomes, including a pattern of symptoms called “overtraining syndrome.” Overtraining syndrome is the result of intense workouts, which eventually lack any health benefit and lead to a host of problems including fatigue and increased rates of physical illness (Smith, 2003). Additionally, overuse injuries, such as stress fractures (Sidiropoulos, 2007), tendonitis, and apophysitis (or an inflammation of the growth plate in the heel) represent painful, and sometimes chronic injuries that occur during and after over-exercise (Committee on Sports Medicine and Fitness, 2000). Furthermore, some overuse injuries, like compartment syndrome, are characterized by pain that rarely subsides without surgical intervention (Reneman, 1975).
Second, over-exercise appears to lead to a degree of habituation to pain, or an increase in pain tolerance. In fact, athletes have been found to have greater pain tolerance than non-athletes. For example, Ryan and Kovacic (1966) found that athletes engaging in contact sports (e.g., football, wrestling) had greater pain tolerance than athletes who did not engage in contact sports (e.g., golf, tennis), and these non-contact athletes in turn had greater pain tolerance than non-athletes. Length of training among athletes has also been found to be related to pain tolerance; athletes with greater amounts of training have higher pain tolerance than athletes with less training (Paparizos et al., 2005). Such findings align well with the IPTS, in that the repeated exposure to pain as a result of over-exercise may increase one's acquired capability for suicide and thus increase risk of suicidal behavior.
Third, two lines of research suggest that over-exercise is related to suicidal behavior via its relationship with anxiety sensitivity (Broman-Fulks et al., 2004; Capron et al., 2012a, 2012b). Specifically, Capron et al. (2012a) found that low physical concerns (a component of anxiety sensitivity) were related to suicidal ideation and attempts. In another study, it was found that low physical concerns trended toward predicting suicidality in a sample of adults with HIV (Capron et al., 2012b). Importantly, Broman-Fulks et al. (2004) found that only high-intensity exercise (vs. low-intensity) reduced fear of anxiety-related physical concerns. Thus, by reducing anxiety-related body sensations, over-exercise may increase the risk for suicidal behavior.
Finally, research has found support for the association between over-exercise and suicidal behavior. Wade et al. (2006) used latent profile analysis in a community sample of 1002 twins to determine the number of distinct weight and eating profiles that emerged from their analysis. The authors found a clear five-class solution, with the fourth class displaying greater symptom severity compared to the other classes. The fourth class also displayed a greater likelihood of having lifetime major depression and suicidality. Notably, this fourth class, which had elevated suicidality, also had a higher likelihood of endorsing over-exercise than the other profile groups. Further, college women who engaged in frequent, vigorous exercise were two times more likely to engage in suicidal behavior as compared to women who did not exercise regularly (Brown and Blanton, 2002). Unger (1997) found that adolescent girls who exercised frequently (i.e., six to seven days per week) had higher rates of suicidal behavior as compared to girls who did not engage in physical activity. Additionally, even moderately active women were more likely to report suicidal behavior than women who were not active exercisers (Brown and Blanton, 2002).
To our knowledge, this is the first theory-driven investigation of the relationship between bulimic behaviors and suicidal behavior. In a series of four studies, we tested four primary hypotheses: (1) that over-exercise is uniquely associated with suicidal behavior in BN participants, over and above other types of compensatory mechanisms, (2) that over-exercise is uniquely associated with acquired capability for suicide, over and above other types of compensatory mechanisms, (3) that pain insensitivity accounts for the relationship between over-exercise and acquired capability for suicide, and (4) that acquired capability for suicide accounts for the relationship between over-exercise and suicidal behavior (see Fig. 1).
Fig. 1.
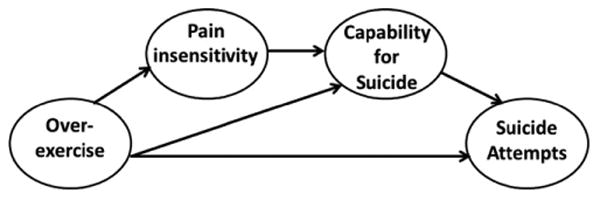
Proposed model for the relationship between over-exercise, pain insensitivity, acquired capability for suicide, and suicide attempts. Note: it is possible that over-exercise is also related to suicidality via thwarted belongingness and perceived burdensomeness; however, these pathways are not depicted as the focus of the current paper is on the acquired capability component of the IPTS.
2. Study 1
2.1. Methods
Participants were recruited through eating disorder clinics and the community. Advertisements specified that only women over age 18 “with symptoms of BN (i.e., binge eating and purging)” were eligible to participate. Potential participants contacted research personnel by phone. Study procedures were explained to the potential participants, at which point verbal consent was obtained and a trained interviewer administered diagnostic interviews, including the Structured Clinical Interview for DSM-IV, Patient Edition (SCID-P; First et al., 2002). The SCID-P was used to determine whether participants met DSM-IV criteria for BN. Eligible participants who expressed an interest in participating in the remainder of the study were then scheduled to attend an in-person assessment during which they provided written informed consent and completed a battery of self-report questionnaires. All participants were paid $50 for their involvement in the study, which was approved by the institutional review boards at each of the participating three sites.
2.1.1. Participants
There were 204 female participants; age ranged from 18 to 57 (M=25.67, S.D.=8.85). The sample was predominantly Caucasian (90.7%, n=185); the remainder of the sample divided as follows: 3.4% Asian (n=7), 2.5% African American (n=5), 2.0% other (n=4), and 1.5% Hispanic (n=3). Additionally, 70.6% (n=144) of the participants met full criteria for a current DSM-IV diagnosis of BN. The remainder of participants met criteria for partial syndrome BN (i.e., they exhibited bulimic symptoms at a lower frequency than the twice per week threshold).
2.1.2. Measures: predictor variables
2.1.2.1. The Eating Disorder Examination Questionnaire-4 (EDEQ-4)
The EDEQ-4 (Fairburn and Beglin, 1994) is a 36-item self-report questionnaire based upon the Eating Disorder Examination interview (EDE; Fairburn and Cooper, 1993) which assesses eating disorder symptomatology. The interview yields four subscales (Restraint, Eating Concern, Shape Concern, and Weight Concern) as well as a global score. Items in this questionnaire focus on symptom levels during the previous 28 days. Item 28, which measures the number of times participants have engaged in “hard exercise as a means of controlling shape or weight,” was used as a predictor variable. The majority of participants (60%) reported engaging in hard exercise over the past 28 days, with a range from one episode to 84 episodes. Although only one item assessed over-exercise, other studies that have used different questions have found that using one or two items to assess eating disorder related variables is a reliable approach (e.g., Mechanic and Hansell, 1987; Joiner and Tickle, 1998; Tanasescu et al., 2002; Keel and Heatherton, 2010). The restraint subscale (α=0.70) consists of five items measuring the degree to which participants attempted to avoid consuming food. In addition to the restraint subscale, Items 22 and 24 were used as covariates. These two items assess the frequency of engaging in self-induced vomiting and laxative use. These items were chosen because they represent potentially painful and provocative experiences and, as such, could contribute to a participant's acquired capability for suicide (Joiner, 2005).
2.1.3. Measures: dependent variables
2.1.3.1. Suicidal gestures and attempts
Suicidal gestures and attempts were assessed with the Impulsive Behavior Scale (IBS; Rosotto et al., 1998), a 25-item self-report questionnaire examining the frequency with which individuals have engaged in maladaptive behaviors throughout their lives. Responses are coded on a one (Never) to five (Regularly) scale. Because this measure is comprised of a list of behaviors it has been found to have utility as a measure of independent dysregulated behaviors (Anestis et al., 2011). In this study, Item 7 (“Have you had any suicide gestures [non-lethal]?”) and Item 12 (“Have you made any suicide attempts?”) were used as measures of suicidal gestures and attempts, respectively. With respect to suicide gestures, 15.8% of the sample reported engaging in this behavior once and 24.6% reported making suicide gestures more than once. With respect to suicide attempts, 14.3% of the sample reported engaging in this behavior once and 13.3% reported attempting engaging in this behavior more than once.
2.2. Results
Means, standard deviations, and intercorrelations are presented in Table 1. Hierarchical linear regression models were used to determine whether frequency of over-exercise significantly predicted suicidal gestures and suicide attempts. Frequency of vomiting episodes, frequency of laxative abuse, restraint (all as measured by the EDEQ-4), and age were entered in step 1. In step 2, frequency of over-exercise (as measured by the EDEQ-4) was added as the independent variable. Over-exercise significantly predicted suicidal gestures, even when controlling for frequency of vomiting episodes, frequency of laxative abuse, restraint, and age (β=0.16, t=2.17, p=0.03, f2=0.05). However, prior to adding over-exercise in step 2, restraint significantly predicted suicide attempts (p=0.02) and trended toward significance in the prediction of suicide gestures (p=0.07). The same analysis was run using suicide attempts as the dependent variable. Again, over-exercise significantly predicted suicide attempts, even when controlling for frequency of vomiting episodes, frequency of laxative abuse, restraint, and age (β=0.17, t=2.17, p=0.02, f2=0.07). Table 2 summarizes these analyses.
Table 1. Study 1 means and standard deviations for, and intercorrelations between, measures.
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. EDEQ exercise | – | ||||||
| 2. EDEQ restraint | 0.22** | – | |||||
| 3. EDEQ vomiting | −0.09 | 0.07 | – | ||||
| 4. EDEQ laxative | −0.06 | 0.18* | 0.01 | – | |||
| 5. IBS suicide gestures | 0.14* | 0.11 | −0.03 | 0.07 | – | ||
| 6. IBS suicide attempts | 0.18* | 0.17* | 0.03 | 0.06 | 0.76** | – | |
| 7. Age | − 0.18** | − 0.18** | − 0.10* | 0.03 | 0.09 | 0.05 | – |
| M | 6.79 | 3.92 | 22.45 | 2.75 | 1.73 | 1.44 | 25.67 |
| S.D. | 10.67 | 1.26 | 36.43 | 6.28 | 1.00 | 0.81 | 8.85 |
| Range | 0–84 | 0–6 | 0–300 | 0–28 | 0–20+ | 0–20 | 18–57 |
Note: n=204.
p< 0.05.
p< 001.
Table 2. Over-exercise predicting suicidal gestures and suicide attempts, controlling for age, restraint, vomiting episodes, and laxative use.
| Predictor | Dependent variables | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Suicide gestures | Suicide attempts | |||||||
|
|
|
|||||||
| β | ΔR2 | t | p | β | ΔR2 | t | p | |
| Step 1 | 0.03 | 0.04 | ||||||
| (constant) | 2.95 | <0.01 | 2.86 | 0.01 | ||||
| Age | 0.11 | 1.54 | 0.13 | 0.08 | 1.17 | 0.24 | ||
| EDEQ restraint | 0.13 | 1.81 | 0.07 | 0.18 | 2.43 | 0.02 | ||
| EDEQ vomiting | −0.03 | −0.45 | 0.65 | 0.03 | 0.35 | 0.73 | ||
| EDEQ laxative | 0.04 | 0.58 | 0.56 | 0.02 | 0.34 | 0.74 | ||
| Step 2 | 0.02* | 0.03* | ||||||
| (constant) | 2.74 | <0.01 | 2.63 | 0.01 | ||||
| Age | 0.13 | 1.86 | 0.07 | 0.11 | 1.51 | 0.13 | ||
| EDEQ restraint | 0.10 | 1.30 | 0.20 | 0.14 | 1.88 | 0.06 | ||
| EDEQ vomiting | −0.01 | −0.18 | 0.86 | 0.05 | 0.65 | 0.52 | ||
| EDEQ laxative | 0.80 | 0.80 | 0.43 | 0.04 | 0.57 | 0.57 | ||
| EDEQ over-exercise | 0.16 | 2.17 | 0.03 | 0.17 | 2.33 | 0.02 | ||
p< 0.05 for ΔR2.
2.3. Study 1 discussion
The aim of Study 1 was to determine if certain compensatory behaviors were associated with greater risk for suicidal behavior in BN. As predicted, engagement in over-exercise was significantly associated with suicidal behaviors, including suicidal gestures and suicide attempts, over and above other commonly employed compensatory behaviors (i.e., vomiting, dietary restraint, and laxative abuse) and other demographic factors (i.e. age).
These results may help explain the increased rate of suicidal behavior displayed by people with BN. According to the IPTS, repeated engagement in painful and provocative behaviors habituates individuals to pain and makes them less fearful about death. Given that over-exercise is pain-inducing and can cause extensive physical damage, according to the theory it follows that this type of behavior should increase suicide risk by elevating the acquired capability for suicide. Although exercise can have beneficial health effects, the type of exercise in which some individuals with symptoms of BN engage may be of a different degree and/or severity. We want to emphasize that having the acquired capability for suicide does not necessarily mean that an individual wants to die by suicide, but rather that the individual is physically capable of dying by suicide should the desire develop. However, because individuals with BN display elevated levels of suicidal ideation (e.g., Favaro and Santonastaso, 1997; Milos et al., 2004) it is particularly important to consider factors, such as over-exercise, that may increase one's acquired capability for suicide.
There were some important limitations of note with Study 1. First, the cross-sectional nature of the study precludes conclusions of causality and temporal precedence. Related to this limitation, the over-exercise measure assessed the past 28 days, whereas the measures of suicidality were in reference to an individual's lifetime. Second, over-exercise was measured by a single item and suicidality was measured by two items. Utilizing a one-item measurement of over-exercise limits the ability to draw conclusions about this construct, as we were unable to assess duration or the compulsive nature of the exercise. However, it should be noted that other studies have found using one or two items to assess similar constructs to be a reliable approach (e.g., Mechanic and Hansell, 1987; Joiner and Tickle, 1998). Third, we did not test whether over-exercise predicted suicidal behavior over and above other well-established predictors of suicidal behavior (e.g., substance abuse, depression). We believe this is a fruitful area for future research but outside the scope of the current paper, which attempted to specifically examine disordered eating behaviors and their relation to suicidal activity. Fourth, we did not directly measure acquired capability in this particular sample and, as such, interpretations of the results involving this construct should be considered with caution. Fifth, our sample was somewhat heterogeneous as not all women met DSM-IV criteria for BN. Finally, this sample consisted entirely of women, most of whom were Caucasian; thus, it is not clear whether these results will generalize to other populations.
3. Study 2
The results of Study 1 suggest that among women with symptoms of BN, over-exercise is associated with suicidal behavior. However, the conclusions of Study 1 were constrained by the limitations noted above. We sought to address some of these limitations in Study 2. Specifically, we used a psychometrically sound measure of over-exercise and examined the correlation between this measure and our single item measure of over-exercise from Study 1. We also hoped to replicate the effect in a nonclinical sample. We hypothesized that Time 1 over-exercise would predict Time 2 acquired capability while controlling for other types of bulimic behaviors, such as vomiting, dietary restraint, and laxative abuse.
3.1. Method
Participants were asked to participate in a two-part study requiring them to fill out questionnaires on two separate occasions, 3–4 weeks apart. Participants completed Time 1 questionnaires online via a secure website that time stamped their completion. Participants completed Time 2 questionnaires on the computer in the laboratory using MediaLab software.
3.1.1. Participants
Our sample consisted of 171 undergraduates from a large southeastern university. Only participants who completed both the Time 1 and Time 2 portions of the study were included in the analysis. All subjects who failed to participate at both time points (n=25) were eliminated from the analyses. A one-way ANOVA was performed to test for differences between those who were included in the analyses and those who were excluded. This test revealed no significant differences between these two groups on any of the variables used in the analyses. The sample was primarily female (80.1%). The ethnic composition was 83.4% Non-Hispanic and 16.6% Hispanic. The racial composition was 87.3% Caucasian, 9.1% African American, 3% Asian American, and 0.6% American Indian/Alaskan Native. The ethnic/racial composition of this sample was generally representative of the university student body, which has been reported to be 77% Caucasian, 10% Hispanic/Latino, 6% African, 3% Asian, and 3% other ethnicity (see Fink et al., 2010). The participants' ages ranged from 18 to 56 (M=19.25, S.D.=3.21).
3.1.2. Time 1 measures
3.1.2.1. The Eating Disorder Examination Questionnaire-4 (EDEQ-4)
Item 28, which measures the number of times participants have engaged in “hard exercise as a means of controlling shape or weight,” was used as a predictor variable. In addition to the Restraint (α=0.90) subscale, items 22 and 24, which measure the frequency with which participants self-induce vomiting and abuse laxatives, were used as covariates. As with Study 1, these items were chosen because they represent potentially painful and provocative experiences and, as such, could contribute to a participant's acquired capability for suicide (Joiner, 2005).
Using the recommended clinical cut-off (≥4.0; Carter et al., 2001; Mond et al., 2004), 6.6% of our participants scored in the clinical range for the Restraint subscale, 2.4% scored in the clinical range for the Eating Concern subscale, 10.2% scored in the clinical range for the Shape Concern subscale, and 6.6% scored in the clinical range for the Weight Concern subscale.
3.1.2.2. Obligatory Exercise Questionnaire (OEQ)
The Obligatory Exercise Questionnaire (Thompson and Pasman, 1991; α=0.91) is a 20-item self-report instrument that assesses compulsory attitudes towards exercise, effort expended while exercising, and behaviors engaged in while exercising. Examples of items include, “Sometimes, I feel a need to exercise twice in one day, even though I may feel a little tired” and “I frequently push myself to the limits.” Item 28 from the EDEQ-4 was significantly correlated with the Obligatory Exercise Questionnaire at Time 1 (r=0.57, p<0.001). The robust correlation demonstrates criterion validity for our single item measure of over-exercise in Study 1.
3.1.3. Time 2 measures
3.1.3.1. Acquired Capability for Suicide Scale (ACSS)
The Acquired Capability for Suicide Scale (Van Orden et al., 2008; Bender et al., 2011; α=0.85) is a 20-item measure designed to assess one's fearlessness about lethal self-injury and ability to tolerate pain. Individuals are asked to rate each item on a one (not at all like me) to five (very much like me) scale. Examples of items include, “Things that scare most people don't scare me” and “I can tolerate more pain than most people.” This scale was only administered at Time 2 due to the nature of this construct. Specifically, we would not expect much change in acquired capability over the 3–4 week interval of the study, as acquired capability is believed to increase gradually over the course of one's lifetime (Van Orden et al., 2010).
3.2. Results
Means and standard deviations for Time 1 and Time 2 variables as well as their intercorrelations can be found in Table 3. Regression analyses were used to predict Time 2 ACSS scores, controlling for Time 1 vomiting frequency, dietary restraint, and laxative use (as measured by the EDEQ-4). Over-exercise (measured by Item 28 of the EDEQ-4 and the OEQ total score) served as the independent variables in separate analyses. For each analysis, in the first step Time 1 vomiting frequency, dietary restraint, and laxative use were entered as covariates. For the first analysis, Item 28 of the EDEQ-4 was entered in step 2 as the independent variable. Time 1 over-exercise (as measured by the EDEQ-4) significantly predicted Time 2 ACSS (β=0.19, t=2.00, p=0.05, f2=0.03; see Table 4). For the second analysis, OEQ total score was entered as the independent variable in step 2. Time 1 OEQ also predicted Time 2 ACSS (β=0.19, t=1.96, p=0.05, f2=0.03; see Table 5).
Table 3. Study 2 means and standard deviations for, and intercorrelations between, measures.
| Measure | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. T1 EDEQ restraint | – | |||||
| 2. T1 EDEQ vomiting | 0.23** | – | ||||
| 3. T1 EDEQ laxative | 0.21** | −0.02 | – | |||
| 4. T1 EDEQ exercise | 0.56** | 0.03 | 0.10 | – | ||
| 5. T1 OEQ | 0.57** | 0.13 | 0.05 | 0.57** | – | |
| 6. T2 ACSS | − 0.03 | − 0.06 | − 0.02 | 0.12 | 0.10 | – |
| M | 1.03 | 0.26 | 0.05 | 1.46 | 39.30 | 47.70 |
| S.D. | 1.37 | 1.78 | 0.47 | 4.47 | 9.83 | 13.22 |
| Range | 0–6 | 0–20 | 0–6 | 0–28 | 21–75 | 16–72 |
Note: n=171.
p<0.001.
Table 4. Time 1 over-exercise (as measured by the EDEQ) predicting Time 2 acquired capability for suicide controlling for Time 1 restraint, vomiting episodes, and laxative use.
| Predictors in the set | B | ΔR2 | t | p |
|---|---|---|---|---|
| Step 1 | <0.01 | |||
| (constant) | 37.43 | <0.001 | ||
| T1 EDEQ restraint | −0.01 | −0.16 | 0.88 | |
| T1 EDEQ vomiting | −0.06 | −0.69 | 0.49 | |
| T1 EDEQ laxative | −0.02 | −0.24 | 0.82 | |
| Step 2 | 0.02* | |||
| (constant) | 37.78 | <0.001 | ||
| T1 EDEQ restraint | −0.12 | −1.25 | 0.22 | |
| T1 EDEQ vomiting | −0.04 | 0.45 | 0.65 | |
| T1 EDEQ laxative | −0.01 | −0.18 | 0.85 | |
| T1 EDEQ exercise | 0.19 | 1.99 | 0.05 |
p<0.05 for ΔR2.
Table 5. Time 1 over-exercise (as measured by the OEQ) predicting Time 2 acquired capability for suicide controlling for Time 1 restraint, vomiting episodes, and laxative use.
| Predictors in the set | B | ΔR2 | t | p |
|---|---|---|---|---|
| Step 1 | 0.01 | |||
| (constant) | 38.22 | <0.001 | ||
| T1 EDEQ restraint | −0.03 | −0.41 | 0.69 | |
| T1 EDEQ vomiting | −0.06 | −0.74 | 0.46 | |
| T1 EDEQ laxative | −0.02 | −0.23 | 0.82 | |
| Step 2 | 0.02* | |||
| (constant) | 8.82 | <0.001 | ||
| T1 EDEQ restraint | −0.14 | −1.44 | 0.15 | |
| T1 EDEQ vomiting | −0.06 | −0.78 | 0.44 | |
| T1 EDEQ laxative | −0.004 | −0.05 | 0.96 | |
| T1 OEQ exercise | 0.19 | 1.96 | 0.05 |
p<0.05 for ΔR2.
3.3. Study 2 discussion
In Study 2 we found that over-exercise predicted acquired capability for suicide even when including other eating disorder covariates (i.e., vomiting frequency, dietary restraint, and laxative use). The results of Study 2 further suggest that of the various types of disordered eating behaviors, over-exercise is a unique contributor to the acquired capability for suicide. Although most, if not all, types of disordered eating behaviors are likely to result in some level of discomfort and pain, it appears that over-exercise may be a particularly potent way to increase pain and reduce fearlessness about death. A design consideration for Study 2 was that acquired capability for suicide was only measured at Time 2. This was necessary given the time frame of the study, as it takes repeated exposure to physically painful and/or fear-inducing experiences for the habituation to pain and the attendant fearlessness of death to develop (Van Orden et al., 2010).
To summarize, Study 1 supported a relationship between over-exercise and suicide attempts and gestures in a clinical sample of women with symptoms of BN, and Study 2 supported a relationship between over-exercise and acquired capability in a non-clinical sample. However, we were unable to examine how the variables of over-exercise, pain insensitivity, acquired capability, and suicide attempts may inter-relate, because suicide attempts were not present in the Study 2 sample and acquired capability for suicide was not assessed in Study 1. The goal of the next two studies was to examine the relationships among these variables more closely.
4. Study 3
The IPTS posits that the capability for suicide is comprised of increased physical pain tolerance and reduced fear of death. The goal of Study 3 was to determine whether over-exercise was associated with pain insensitivity. It was hypothesized that over-exercise would retain a significant association with pain insensitivity, even after controlling for other disordered eating behaviors. Further, we believed that pain insensitivity would account for the relationship between over-exercise and acquired capability for suicide.
4.1. Method
Participants arrived at the laboratory and half of the participants completed the self-report questionnaires prior to the pain threshold assessment. The other half completed the tasks in the reverse order. No order effects were found.
4.1.1. Participants
The Study 3 sample consisted of 437 undergraduates (57% female) from a large northern university. The ethnic composition was 95.7% Non-Hispanic, 2.7% Hispanic, and 1.6% unreported. The racial composition was 84% Caucasian, 4.3% African American, 10.3% Asian American, 1.6% American Indian/Alaskan Native, and 0.5% Native Hawaiian/Pacific Islander. The participants' ages ranged from 18 to 39 (M=19.60, S.D.=2.43). This sample was generally representative of the student body, which is primarily Caucasian (86%; North Dakota State University Student Demographic Information, 2008).
4.1.2. Measures: predictor variables
4.1.2.1. Over-exercise
In this study, two summed Z-scored items were used to measure over-exercise: the first was Item 28 from the EDEQ-4, which measures the number of times participants have engaged in “hard exercise as a means of controlling shape or weight” over the past 28 days. The second was an item created by the authors, “Have you kept on exercising even though you were very sick (e.g., had the flu) or in a lot of physical pain (e.g., had an injury)?” Responses for the latter item were coded on a one (Never) to five (Regularly) scale.
4.1.2.2. Bulimic disordered eating behaviors
A measure assessing for lifetime history of compensatory behaviors was used, due to low base rates on the EDEQ-4, as the EDEQ-4 only assesses for symptom occurrence over the past 28 days. These items were created by two of the study authors and comprise a scale that currently is in the development process (Gordon and Smith, in preparation). Specifically, we used the following items as individual covariates of compensatory behaviors, “Have you taken diet pills, laxatives, or diuretics (i.e. “water pills”) for the purpose of losing weight?,” “Have you made yourself vomit?,” “Have you gone 24 h without eating?.” Responses for these items were coded on a one (Never) to five (Regularly) scale. With respect to the frequency of engagement in these behaviors, 27% reported vomiting at least once, 15.6% reported taking diet pills, laxatives, or diuretics at least once, and 48% reported going 24 h without eating.
4.1.3. Measures: dependent variables
4.1.3.1. Pain threshold
The NeuroSensory Analyzer (NSA; TSA-II, Medoc, Durham, North Carolina) is a computerized pain perception assessment device that uses a thermode to administer heat- and cold-induced pain. In the current study, we only used heat-induced pain as we encountered a ceiling effect on the cold-induced pain. The thermode was placed beneath the first knuckle of the index finger on the right hand and held in place with an elastic strap. The baseline temperature of the thermode was 25 °C, at which point the participant felt neither warmth nor cold. For each trial, participants were instructed to depress a computer mouse button when they first felt pain. Once each trial started, the temperature level of the thermode increased at a rate of 1 °C per second until it reached a temperature of 50.5 °C or the participant pressed the mouse button. After pressing the button, the temperature decreased at a rate of 10 °C per second until it returned to the baseline temperature. Participants completed five trials with thirty seconds between each trial. Cronbach's alpha (with trials viewed as items measuring an underlying construct) for this sample was 0.95, and pain threshold data were available for all participants. We averaged the five trials to create a pain insensitivity variable.
4.1.3.2. Acquired Capability for Suicide Scale (ACSS)
See Study 2; the alpha coefficient for the Study 3 sample was 0.82.
4.2. Results
4.2.1. Over-exercise as a predictor of pain insensitivity
A hierarchical linear regression model was used to determine whether frequency of over-exercise significantly predicted pain insensitivity, controlling for restraint, vomiting, and use of laxatives, diet pills, and diuretics. In step 1, the covariates of age, restraint, vomiting, and use of laxatives, diet pills, and diuretics were added to the equation. In step 2, over-exercise was added as the independent variable. Over-exercise was the only significant predictor of pain insensitivity (β=0.12, t=2.26, p=0.02, f2=0.01), see Table 6.
Table 6. Over-exercise (as measured by the EPPES and EDEQ-4) predicting pain insensi-tivity controlling for age, restraint, vomiting episodes, and laxative use.
| Predictor | B | ΔR2 | t | p |
|---|---|---|---|---|
| Step 1 | 0.02 | |||
| (constant) | 31.15 | <0.001 | ||
| Age | 0.02 | 0.38 | 0.70 | |
| Diet pills/laxatives/diuretics | −0.04 | −0.74 | 0.46 | |
| Vomiting | −0.07 | 1.22 | 0.22 | |
| Restraint | 0.10 | 1.83 | 0.07 | |
| Step 2 | 0.01* | |||
| (constant) | 31.12 | <0.001 | ||
| Age | 0.04 | 0.68 | 0.50 | |
| Diet pills/laxatives/diuretics | −0.05 | −0.96 | 0.34 | |
| Vomiting | 0.05 | 0.81 | 0.42 | |
| Restraint | 0.09 | 1.73 | 0.08 | |
| Over-exercise | 0.12 | 2.27 | 0.02 |
p<0.05 for ΔR2.
4.2.2. Pain insensitivity as a predictor of acquired capability for suicide
A linear regression model was used to determine whether pain insensitivity significantly predicted acquired capability for suicide. Pain insensitivity significantly predicted acquired capability for suicide (β=0.18, t=3.73, p<0.001, f2=0.03).
4.2.3. Pain insensitivity as a mediator between over-exercise and acquired capability for suicide
In order to test the mediational impact of pain insensitivity on the relationship between over-exercise and acquired capability the PRODCLIN program was used. Developed by MacKinnon et al. (2007), this program tests mediational effects while circumventing problems inherent in other methods of testing for mediation (e.g. inflated rates of Type I error, see MacKinnon et al., 2002). PRODCLIN examines the product of the unstandardized path coefficients divided by the pooled standard error of the path coefficients (αβ/σαβ) and a confidence interval is generated. A statistically significant mediation effect is indicated by the absence of zero from the confidence interval. The unstandardized path coefficients and standard errors of the path coefficients for the indirect effects of over-exercise on acquired capability were entered into PRODCLIN to yield the following 95% confidence interval: 0.023–0.351. Because zero was not included in the confidence interval, we concluded that the relationship between over-exercise and suicide attempts was statistically accounted for by acquired capability for suicide. Due to the cross-sectional nature of our data, we were unable to use true tests of mediation; however, variables in cross-sectional analyses can provide useful preliminary data capable of serving as a foundation for future longitudinal examinations.
4.3. Study 3 discussion
In line with prediction, our analyses revealed that over-exercise was related to pain insensitivity over and above other types of compensatory behaviors (i.e., restraint, vomiting, and use of laxative, diet pills, and diuretics) and demographic variables (i.e., age) in a sample of undergraduate students. Additionally, we found evidence for a relationship between over-exercise and acquired capability for suicide that was statistically accounted for by pain insensitivity. However, a limitation of this study was that we measured pain insensitivity, rather than pain tolerance. Specifically, although the two constructs are related (Van Orden et al., 2010), pain insensitivity refers to a lack of pain perception, whereas pain tolerance refers to the maximum level of pain that a person can tolerate. Future studies should examine how various aspects of pain insensitivity might operate differently as indices of acquired capability for suicide, though our results are in accordance with other studies that have used a pain tolerance task (e.g., Anestis et al., 2011). Additionally, although we tested models of statistical mediation, Study 3 was cross-sectional. Thus, we cannot conclude that over-exercise causes pain insensitivity, or that pain insensitivity causes acquired capability. Longitudinal studies are needed to clarify this relationship.
5. Study 4
Given the results of the first three studies, a logical next step was to clarify the relationship among over-exercise, acquired capability, and suicide attempts. The goal of Study 4 was to test a model in which acquired capability was hypothesized to account for the relationship between over-exercise and suicide attempts, which was initially observed in Study 1.
5.1. Method
Participants completed all questionnaires online via a secure website.
5.1.1. Participants
Our sample consisted of a new sample of 512 undergraduates from a large southeastern university (80% female), which was representative of the university student body. The ethnic composition was 86.6% Non-Hispanic, 12.6% Hispanic, and 0.08% unreported. The racial composition was 79.3% Caucasian, 14.4% African American, 4.7% Asian American, and 1% American Indian/Alaskan Native. The participants' ages ranged from 17 to 35 (M=18.89, S.D.=2.70).
5.1.2. Measures
5.1.2.1. Acquired Capability for Suicide Scale-Short Version (ACSS)
In this study, an abbreviated eight-item version of the ACSS was used. The alpha coefficient for the Study 4 sample was 0.73.
5.1.2.2. Over-exercise
In this study we used two brief indices of exercise created by the authors: over-exercise and exercise duration. Over-exercise was assessed by the two items: “Has exercising ever interfered with school, work, or social functioning?” and “Have you ever exercised when you were sick or injured?” Additionally, exercise duration was assessed by three items: “How many years have you been exercising?,” “How many times a week do you exercise?,” and “How many minutes do you exercise per session?”
5.1.2.3. Lifetime suicide attempts
As assessed in previous studies (e.g., Pettit et al., 2004, 2006), lifetime suicide attempts were measured by asking participants the number of times they had attempted suicide.
5.2. Results
5.2.1. Over-exercise as a predictor of acquired capability for suicide
A least squares linear regression model was used to determine whether over-exercise significantly predicted acquired capability for suicide. Over-exercise significantly predicted acquired capability for suicide (β=0.15, t=3.36, p=0.001, f2=0.02). Exercise duration also significantly predicted acquired capability for suicide (β=0.14, t=3.12, p=0.002, f2=0.02)
5.2.2. Acquired capability for suicide as a predictor of suicide attempts
A least squares linear regression model was used to determine whether acquired capability significantly predicted suicide attempts, which was supported (β=0.15, t=3.34, p=0.001, f2=0.02).
5.2.3. Acquired capability for suicide as a mediator between over-exercise and suicide attempts
The unstandardized path coefficients and standard errors of the path coefficients for the indirect effects of over-exercise on suicide attempts were entered into PRODCLIN to yield the following 95% confidence interval: 0.002 to 0.012. Because zero was not included in the confidence interval, we concluded that the relationship between over-exercise and suicide attempts was significantly accounted for by acquired capability for suicide. Next, the unstandardized path coefficients and standard errors of the path coefficients for the indirect effects of exercise duration on suicide attempts were entered into PRODCLIN to yield the following 95% confidence interval: 0.0001–0.001. Again, we were able to conclude that the acquired capability significantly statistically accounted for the relationship between exercise duration and suicide attempts, as zero was not included in the confidence interval.
5.3. Study 4 discussion
Building off the findings from the previous three studies, Study 4 constituted an important test of the overall model proposed. In our final study we found that acquired capability statistically accounted for the relationship between over-exercise and suicide attempts. Overall, the results of four studies converge to suggest that over-exercise is related to suicide attempts through its association with pain insensitivity and the acquired capability for suicide.
Similar to Study 3, given the cross-sectional design we are unable to draw conclusions about the directionality of the effects. Further, although the sample size was large, it was drawn from a college population; thus, the results may not generalize to other populations.
6. General discussion
Over the course of these studies four main hypotheses were investigated. In Study 1 we tested our first hypothesis that over-exercise is uniquely associated with suicidal behavior in participants with symptoms of BN over and above other types of compensatory mechanisms. In Study 2 a test of the second hypothesis that over-exercise is uniquely associated with acquired capability for suicide over and above other types of compensatory mechanisms was conducted. The third hypothesis that pain insensitivity accounts for the relationship between over-exercise and acquired capability for suicide was investigated in Study 3. Finally, in Study 4, our final aim was to determine whether the acquired capability for suicide accounts for the relationship between over-exercise and suicidal behavior. In Study 1 over-exercise emerged as the only significant predictor of suicidal gestures and suicide attempts in a clinical sample of individuals with symptoms of BN. In Study 2, over-exercise was again the only significant predictor of acquired capability for suicide in a non-clinical sample. Study 3 attempted to further clarify the relationship among over-exercise, pain insensitivity, and the acquired capability for suicide. Specifically, pain insensitivity was found to account for the relationship between over-exercise and acquired capability in a non-clinical sample. Study 4 tested and found evidence for a pivotal piece of our model—that the relationship between over-exercise and suicidal behavior was accounted for by the acquired capability for suicide.
These results suggest that over-exercise can be hazardous to individuals not only directly—via overuse injuries—but also indirectly, via the acquired capability for suicide. Conclusions based on the current studies concerning the prospective association between over-exercise and elevated acquired capability are tentative, however and require replication with longitudinal designs. Even so, these results suggest that the pain and discomfort involved in over-exercise may increase pain insensitivity. This in turn could increase one's acquired capability for suicide, perhaps through a corresponding increase in pain tolerance.
Given these findings, an important treatment target for individuals with BN who are engaging in over-exercise may be to teach healthy exercise, as continued over-exercise could further increase their acquired capability for suicide. This is especially important given that over-exercise often precedes eating disorder onset and is one of the last disordered eating symptoms to abate (e.g., Davis et al., 1994, 1997). Further, there is accruing evidence that over-exercise is associated with negative outcomes in people with eating disorders, such as greater length of hospitalization (Solenberger, 2001) and earlier relapse (Carter et al., 2004). One study employing a healthy exercise program (Calogero and Pedrotty, 2004) found that the program was successful in reducing the emotional commitment, involvement, and rigidity of exercise among women with eating disorders (Calogero and Pedrotty, 2004). Additionally, Dialectical Behavior Therapy (DBT), which has received support as a treatment for BN (Safer et al., 2001; Chen et al., 2008), emphasizes the concept of balance. Balance could be highlighted when discussing the concept of healthy exercise with patients with BN. Of course, it would be of critical importance to make sure patients are medically cleared before recommending their engagement in any type of healthy exercise regimen.
There were several limitations to these studies. Importantly, all of these data are essentially cross-sectional. Currently, this is a necessary constraint given the constructs and the nature of the model we are testing. According to the IPTS, by the time individuals engage in serious suicidal behavior, they have accumulated their acquired capability over an extended period of time. Given the recency of this theoretical model, longitudinal data sets with long durations of follow-up have not yet included these measures over sufficient time to evaluate the fully proposed model.
A second important limitation has to do with the construct of over-exercise, as there were variations in its definition from study to study. Studies 1 and 3 used one and two items, respectively, to operationalize over-exercise; thus, various components of the construct (e.g., the compulsive nature of the exercise, exercising to the exclusion of other activities or when one is sick or injured) were not included. Also, without an exercise duration component in three of the four studies, it is even more difficult to determine whether the behavior that participants were reporting truly represented over-exercise. It is important to consider this measurement issue when interpreting the results. Although this is problematic from an assessment standpoint, it also reflects a problem within the field, as the definition of over-exercise tends to vary from study to study (e.g., Long et al., 1995). The lack of measurement consistency and specificity across studies is a limitation; however, it is also no table that our results were consistent across different measures. This consistency suggests that the findings generalize across measures. It will be important for future work in this area to use a consistent and comprehensive operationalization of over-exercise.
Third, only one of the four studies used a clinical sample, though some participants in the other studies displayed clinical levels of eating pathology. Given the use of collegiate samples in Studies 2–4, it is unclear whether these results would generalize to a clinical population. Further, although research on undergraduates has significant value, this type of research may lack external validity. An additional limitation is that the effect sizes reported in all four studies were typically small and, as such, a substantial amount of variance remains unexplained.
Despite these limitations, these studies also have several no table strengths. Strengths of this study include the large sample sizes across the four trials, inclusion of individuals from multiple sites, use of a clinical sample in Study 1, and use of an objective measure of pain insensitivity. Study 2 demonstrated a unique relationship between over-exercise and acquired capability. The results of Studies 3 and 4 corroborate those reported in Studies 1 and 2, and also suggest that increased pain insensitivity and the resultant increased acquired capability may be important mechanisms by which over-exercise eventually leads to suicide attempts. Perhaps most importantly, the results of all four studies converge to suggest that over-exercise represents a dangerous disordered eating behavior that consistently is related to both acquired capability and suicide attempts, even when controlling for a host of other painful behaviors relevant to eating disorders.
Although many people with eating disorders engage in over-exercise (up to one-quarter of people with BN; Shroff et al., 2006), there is a relative dearth of research on over-exercise in this population. The results of these studies suggest that engagement in over-exercise is associated with elevated suicidality in BN. We suggest that some individuals with BN may engage in a form of exercise that is particularly strenuous, and that this type of exercise is a potent way to increase acquired capability for suicide. Future research should continue to explore the proposed mechanism in longitudinal designs, as well as examine whether the study findings hold for other eating disorder populations, such as individuals with AN. Moreover, it would be worthwhile to examine if and how the type and intensity of exercise has effects on the acquired capability for suicide. Additionally, it will be important to examine whether over-exercise might affect burdensomeness and belongingness. According to the IPTS, when experienced separately perceived burdensomeness and thwarted belongingness produce passive suicidal ideation; however, when they are experienced conjointly they produce active suicidal desire. It is possible that over-exercise may have adverse effects on belongingness if it is done in a solitary manner or to such an extent that social relationships are neglected. Further, monopolizing resources in order to support an intense exercise regimen could impact feelings of burdensomeness as well. In future research it would also be interesting to examine the role of emotion regulation in over-exercise. Although exercise is often associated with beneficial effects, it appears over-exercise may have significant deleterious effects among individuals, particularly those with symptoms of BN.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th. APA; Washington, DC: 2000. Text Revision. [Google Scholar]
- Anestis MS, Bagge CL, Tull MT, Joiner TE. Clarifying the role of emotion dysregulation in the interpersonal-psychological theory of suicidal behavior in an undergraduate sample. Journal of Psychiatric Research. 2011;45:603–611. doi: 10.1016/j.jpsychires.2010.10.013. [DOI] [PubMed] [Google Scholar]
- Anestis MS, Fink EL, Bender TW, Selby EA, Smith AR, Witte TW, Joiner TE. Re-considering the association between negative urgency and suicidality. Personality and Mental Health. 2011;6:138–146. [Google Scholar]
- Bender TW, Gordon KH, Bresin K, Joiner TE. Impulsivity and suicidality: the mediating role of painful and provocative experiences. Journal of Affective Disorders. 2011;129:301–307. doi: 10.1016/j.jad.2010.07.023. [DOI] [PubMed] [Google Scholar]
- Broman-Fulks JJ, Berman ME, Rabian BA, Webster MJ. Effects of aerobic exercise on anxiety sensitivity. Behaviour Research and Therapy. 2004;42:125–136. doi: 10.1016/S0005-7967(03)00103-7. [DOI] [PubMed] [Google Scholar]
- Brown DR, Blanton CJ. Physical activity, sports participation, and suicidal behavior among college students. Medicine and Science in Sports and Exercise. 2002;34:1087–1096. doi: 10.1097/00005768-200207000-00006. [DOI] [PubMed] [Google Scholar]
- Bryan C, Anestis M. Reexperiencing symptoms and the interpersonal-psychological theory of suicidal behavior among deployed service members evaluated for traumatic brain injury. Journal of Clinical Psychology. 2011;67:856–865. doi: 10.1002/jclp.20808. [DOI] [PubMed] [Google Scholar]
- Bulik CM, Sullivan PF, Joyce PR. Temperament, character and suicide attempts in anorexia nervosa, bulimia nervosa and major depression. Acta Psychiatrica Scandinavica. 1999;100:27–32. doi: 10.1111/j.1600-0447.1999.tb10910.x. [DOI] [PubMed] [Google Scholar]
- Calogero RM, Pedrotty KN. The practice and process of healthy exercise: an investigation of the treatment of exercise abuse in women with eating disorders. Eating Disorders: The Journal of Treatment and Prevention. 2004;12:273–291. doi: 10.1080/10640260490521352. [DOI] [PubMed] [Google Scholar]
- Carter JC, Blackmore E, Sutandar-Pinnock K, Woodside DB. Relapse in anorexia nervosa: a survival analysis. Psychological Medicine. 2004;34:671–679. doi: 10.1017/S0033291703001168. [DOI] [PubMed] [Google Scholar]
- Carter JC, Stewart DA, Fairburn CG. Eating disorder examination questionnaire: norms for young adolescent girls. Behavior Research and Therapy. 2001;39:625–632. doi: 10.1016/s0005-7967(00)00033-4. [DOI] [PubMed] [Google Scholar]
- Capron DW, Cougle JR, Ribeiro JD, Joiner TE, Schmidt NB. An interactive model of anxiety sensitivity relevant to suicide attempt history and future suicidal ideation. Journal of Psychiatric Research. 2012;46:174–180. doi: 10.1016/j.jpsychires.2011.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capron DW, Gonzalez A, Parent J, Zvolensky MJ, Schmidt NB. Suicidality and anxiety sensitivity in adults with HIV. AIDS Patient Care and STDs. 2012;26:298–303. doi: 10.1089/apc.2011.0429. [DOI] [PubMed] [Google Scholar]
- Chen E, Matthews L, Allen C, Kuo JR, Linehan MM. Dialectical behavior therapy for clients with binge-eating disorder or bulimia nervosa and borderline personality disorder. International Journal of Eating Disorders. 2008;41:505–512. doi: 10.1002/eat.20522. [DOI] [PubMed] [Google Scholar]
- Committee on Sports Medicine Fitness. Intensive training and sports specialization in young athletes. Pediatrics. 2000;106:154–157. [PubMed] [Google Scholar]
- Corcos M, Taieb O, Benoit-Lamy S, Paterniti S, Jeammet P, Flament MF. Suicide attempts in women with bulimia nervosa: frequency and characteristics. Acta Psychiatrica Scandinavica. 2002;106:381–386. doi: 10.1034/j.1600-0447.2002.02318.x. [DOI] [PubMed] [Google Scholar]
- Crow S, Peterson CB, Swanson SA, Raymond NC, Specker S, Eckert ED, Mitchell JE. Increased mortality in bulimia nervosa and other eating disorders. American Journal of Psychiatry. 2009;166:1342–1346. doi: 10.1176/appi.ajp.2009.09020247. [DOI] [PubMed] [Google Scholar]
- Davidson CL, Wingate LR, Grant DM, Judah MR, Mills AC. Interpersonal suicide risk and ideation: the influence of depression and social anxiety. Journal of Social and Clinical Psychology. 2011;30:842–855. [Google Scholar]
- Davis C, Katzman DK, Kaptein S, Kirsh C, Brewer H, Kalmbach K, Olmsted MP, Woodside DB, Kaplan AS. The prevalence of high-level exercise in the eating disorders: etiological implications. Comprehensive Psychiatry. 1997;38:321–326. doi: 10.1016/s0010-440x(97)90927-5. [DOI] [PubMed] [Google Scholar]
- Davis C, Kennedy SH, Ravelski E, Dionne M. The role of physical activity in the development and maintenance of eating disorders. Psychological Medicine. 1994;24:957–967. doi: 10.1017/s0033291700029044. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Beglin SJ. Assessment of eating disorders: interview or self-report questionnaire? International Journal of Eating Disorders. 1994;16:363–370. [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge Eating: Nature, Assessment and Treatment. 12th. Guilford Press; New York: 1993. [Google Scholar]
- Favaro A, Santonastaso P. Suicidality in eating disorders: clinical and psychological correlates. Acta Psychiatrica Scandinavica. 1997;95:508–514. doi: 10.1111/j.1600-0447.1997.tb10139.x. [DOI] [PubMed] [Google Scholar]
- Fink EL, Anestis MD, Selby EA, Joiner TE. Negative urgency fully mediates the relationship between alexithymia and dysregulated behaviours. Personality and Mental Health. 2010;4:284–293. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P) Biometrics Research, New York State Psychiatric Institute; New York, NY: 2002. [Google Scholar]
- Franko D, Keel P. Suicidality in eating disorders: occurrence, correlates, and clinical implications. Clinical Psychology Review. 2006;26:769–782. doi: 10.1016/j.cpr.2006.04.001. [DOI] [PubMed] [Google Scholar]
- Gordon K, Smith AR. Psychometric properties of the eating disorder painful and provocative events scale. in preparation. [Google Scholar]
- Jenkins GR, Hale R, Papanastassiou M, Crawford MJ, Tyrer P. Suicide rate 22 years after parasuicide: cohort study. British Medical Journal. 2002;325:1155. doi: 10.1136/bmj.325.7373.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joiner TE. Why People Die by Suicide. Harvard University Press; Massachusetts Cambridge, MA: 2005. [Google Scholar]
- Joiner TE, Tickle JJ. Exercise and depressive and anxious symptoms: what is the nature of their interrelations? Journal of Occupational Rehabilitation. 1998;8:191–198. [Google Scholar]
- Joiner TE, Van Orden KA, Witte TK, Selby EA, Ribeiro JD, Lewis R, Rudd MD. Main predictions of the interpersonal-psychological theory of suicidal behavior: empirical tests in two samples of young adults. Journal of Abnormal Psychology. 2009;118:634–646. doi: 10.1037/a0016500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keel PK, Heatherton TF. Weight suppression predicts maintenance and onset of bulimic syndromes at 10-year follow-up. Journal of Abnormal Psychology. 2010;119:268–275. doi: 10.1037/a0019190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long CG, Hollin Clive R. Assessment and management of eating disordered patients who over-exercise: a four-year follow-up of six single case studies. Journal of Mental Health. 1995;4:309–317. [Google Scholar]
- MacKinnon DP, Fritz MS, Williams J, Lockwood CM. Distribution of the product confidence limits for the indirect effect: program PRODLIN. Behavior Research Methods. 2007;39:384–389. doi: 10.3758/bf03193007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenzie DC. Markers of excessive exercise. Canadian Journal of Applied Physiology. 1999;24:66–73. doi: 10.1139/h99-007. [DOI] [PubMed] [Google Scholar]
- Mechanic D, Hansell S. Adolescent competence, psychological well-being, and self-assessed physical health. Journal of Health and Social Behavior. 1987;28:364–374. [PubMed] [Google Scholar]
- Mehler PS, Weiner KL. Frequently asked medical questions about eating disorder patients. Eating Disorders: The Journal of Treatment and Prevention. 1994;2:22–30. [Google Scholar]
- Milos G, Spindler A, Hepp U, Schnyder U. Suicide attempts and suicidal ideation: links with psychiatric comorbidity in eating disorder subjects. General Hospital Psychiatry. 2004;26:129–135. doi: 10.1016/j.genhosppsych.2003.10.005. [DOI] [PubMed] [Google Scholar]
- Mond JM, Hay PJ, Rodgers B, Owen C. Eating Disorder Examination Questionnaire (EDE-Q): norms for young adult women. Behavior Research and Therapy. 2004;44:53–62. doi: 10.1016/j.brat.2004.12.003. [DOI] [PubMed] [Google Scholar]
- Mota-Pereira J, Silverio J, Carvalho S, Ribeiro JC, Fonte D, Ramos J. Moderate exercise improves depression parameters in treatment-resistant patients with major depressive disorder. Journal of Psychiatric Research. 2011;45:1005–1011. doi: 10.1016/j.jpsychires.2011.02.005. [DOI] [PubMed] [Google Scholar]
- North Dakota State University Student Demographic Information. 2008 Available From: < http://www.ndsu.edu/fileadmin/diversity/Student_Demographics_Fall_2008.pdf>.
- Paparizos AL, Tripp DA, Sullivan ML, Rubenstein M. Catastrophizing and pain perception in recreational ballet dancers. Journal of Sport Behaviour. 2005;28:35–50. [Google Scholar]
- Pettit JW, Joiner TE, Rudd DM. Kindling and behavioral sensitization: are they relevant to recurrent suicide attempts? Journal of Affective Disorders. 2004;83:249–252. doi: 10.1016/j.jad.2004.08.010. [DOI] [PubMed] [Google Scholar]
- Pettit JW, Paukert AL, Joiner TE, Rudd DM. Pilot sample of very early onset bipolar disorder in a military population moderates the association of negative life events and non-fatal suicide attempts. Bipolar Disorders. 2006;8:475–484. doi: 10.1111/j.1399-5618.2006.00353.x. [DOI] [PubMed] [Google Scholar]
- Preti A, Rocchi MBL, Sisti D, Camboni MV, Miotto P. A comprehensive meta-analysis of the risk of suicide in eating disorders. Acta Psychiatrica Scandinavica. 2011;124:6–17. doi: 10.1111/j.1600-0447.2010.01641.x. [DOI] [PubMed] [Google Scholar]
- Reneman RS. The anterior and the lateral compartmental syndrome of the leg due to intensive use of muscles. Clinical Orthopedics and Related Research. 1975;113:69–80. doi: 10.1097/00003086-197511000-00011. [DOI] [PubMed] [Google Scholar]
- Rosotto E, Yager J, Rorty M. The impulsive behavior scale. In: Vanderlin-den J, Vandereycken W, editors. Trauma, Dissociation, and Impulsive Dyscontrol in Eating Disorders. Brunner/Mazel; Pennsylvania: 1998. [Google Scholar]
- Ryan ED, Kovacic CR. Pain tolerance and athletic participation. Perceptual and Motor Skills. 1966;22:383–390. [Google Scholar]
- Safer DL, Telch CF, Agras WS. Dialectical behavior therapy for bulimia nervosa. The American Journal of Psychiatry. 2001;158:632–634. doi: 10.1176/appi.ajp.158.4.632. [DOI] [PubMed] [Google Scholar]
- Selby E, Smith AR, Bulik CM, Olmsted MP, Thornton L, McFarlane TL, Berrettini WH, Brandt HA, Crawford S, Fichter MM, Halmi KA, Jacoby GE, Johnson CL, Jones I, Kaplan AS, Mitchell JE, Nutzinger DO, Strober M, Treasure J, Woodside DB, Kaye WH, Joiner TE., Jr Habitual starvation and provocative behaviors: two potential routes to extreme suicidal behavior in Anorexia Nervosa. Behavior Research and Therapy. 2010;48:634–645. doi: 10.1016/j.brat.2010.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shroff H, Reba L, Thornton LM, Tozzi F, Klump KL, Berrettini WH, Brandt H, Crawford S, Crow S, Fichter MM, Halmi KA, Johnson C, Kaplan AS, Keel P, LaVia M, Mitchell J, Rotondo A, Strober M, Treasure J, Woodside DB, Kaye WH, Bulik CM. Features associated with excessive exercise in women with eating disorders. International Journal of Eating Disorders. 2006;39:454–461. doi: 10.1002/eat.20247. [DOI] [PubMed] [Google Scholar]
- Sidiropoulos M. Anorexia nervosa: the physiological consequences of starvation and the need for primary prevention efforts. McGill Journal of Medicine. 2007;10:20–25. [PMC free article] [PubMed] [Google Scholar]
- Smith LL. Overtraining, excessive exercise, and altered immunity. Sports Medicine. 2003;33:347–364. doi: 10.2165/00007256-200333050-00002. [DOI] [PubMed] [Google Scholar]
- Solenberger SE. Exercise and eating disorders: a 3-year inpatient hospital records analysis. Eating Behaviors. 2001;2:151–168. doi: 10.1016/s1471-0153(01)00026-5. [DOI] [PubMed] [Google Scholar]
- Tanasescu M, Leitzmann MF, Rimm EB, Willett WC, Stampfer MJ, Hu FB. Exercise type and intensity in relation to coronary heart disease in men. Journal of the American Medical Association. 2002;288:1994–2000. doi: 10.1001/jama.288.16.1994. [DOI] [PubMed] [Google Scholar]
- Thompson JK, Pasman L. The Obligatory Exercise Questionnaire. Behavior Therapist. 1991;14:137. [Google Scholar]
- Unger JB. Physical activity, participation in team sports, and risk of suicidal behavior in adolescents. American Journal of Health Promotion. 1997;12:90–93. doi: 10.4278/0890-1171-12.2.90. [DOI] [PubMed] [Google Scholar]
- Wade TD, Crosby RD, Martin NG. Use of latent profile analysis to identify eating disorder phenotypes in an adult Australian twin cohort. Archives of General Psychiatry. 2006;63:1377–1384. doi: 10.1001/archpsyc.63.12.1377. [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Gordon KH, Bender TW, Joiner TE. Suicidal desire and the capability for suicide: tests of the interpersonal-psychological theory of suicidal behavior among adults. Journal of Consulting and Clinical Psychology. 2008;76:72–83. doi: 10.1037/0022-006X.76.1.72. [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE. The interpersonal theory of suicide. Psychological Review. 2010;117:575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veale DMW. Exercise dependence. British Journal of Addiction. 1987;82:735–740. doi: 10.1111/j.1360-0443.1987.tb01539.x. [DOI] [PubMed] [Google Scholar]


