Abstract
Introduction
The use of Masquelet technique is a serious option to consider for biologic reconstruction of severe bone loss. Here is exposed a continuous and prospective study on bone loss management using that technique. The aims of this study were to assess epidemiology of bone loss due either to trauma or to non-unions and to give preliminary results.
Patients and methods
It was a prospective study from April 2015 to december 2016 involving patients treated using the induced membrane technique for a diaphyseal bone defect due either to trauma or non-unions. AO plates or Orthofix external fixators were used for osteosynthesis. Bone healing was radiologically assessed and any complications were listed.
Results
During the study period, 11 patients were treated using the induced membrane technique. There were 8 males and 3 females. Their mean age was 40.45 years (21–59). The skeletal segments concerned were 2 humerus, 6 femurs and 3 tibias with a mean bone defect length of 4,45 cm (2.5–8). The delay between reconstruction and trauma was 8 months (20 days − 3 years). After a mean follow-up of 6.54 months (3–11) six patients presented a good radiological healing (4 femurs, 2 humerus) whereas in four patients, autograft osteointegration was still ongoing (2 femurs, 2 tibias). A tibia secondary infection was observed in a patient with the graft partial resorption. In another patient, an initial gangrene lead to a leg amputation.
Conclusion
The induced membrane technique is an excellent option for bone defect reconstruction compared to other usual bone graft techniques. It helped us to manage large bone loss in various skeletal segments.
Keywords: Bone reconstruction, induced membrane, bone loss
1. Introduction
Diaphyseal bone defects are rare.1 They are still frequent in developing countries and they are to surgeons a surgical and functional challenge. The trauma mechanism, osteosynthesis complications,2 or the patients’ initial visits to bone-setters explain the important morbidity. The use of bone reconstruction technique as described by Masquelet,3 is a serious option to consider for biologic reconstruction of severe bone loss. We report here a prospective and preliminary series about 11 cases of bone loss treated by the induced membrane technique. This study aims to assess epidemiology of bone losses and to bring out preliminary results.
2. Patients and Methods
2.1. Patients
It was a continuous, prospective and monocentric study about 11 patients (3 females, 8 males) treated in our department for a segmental bone loss using the Masquelet induced membrane technique from April 2015 to December 2016. Their mean age was 40.45 years (21–59). Aetiologies were a trauma (one case) and non-unions (10 cases). Tumors and congenital mal-unions were not included in the study. The trauma date and cause and the period of reconstruction were listed. The bone loss lenght, the involved skeletal segment and the type of graft used are listed on Table 1.
Table 1.
Epidemiological characteristics of the series, aetiological factors, bone concerned, defect size.
| Case | Age (years) | Sex | Etiology | Bone concerned | Defect (cm) |
|---|---|---|---|---|---|
| 1 | 21 | F | Traumatic/avulsion on nail | Tibia | 8 |
| 2 | 46 | M | non-union on nail | Femur | 4 |
| 3 | 59 | M | nonunion on plate | Femur | 5 |
| 4 | 28 | M | Septic non-union | Tibia | 7 |
| 5 | 52 | M | non-union orthopedic treatment | Tibia | 4 |
| 6 | 34 | F | non-union | Humerus | 2,5 |
| 7 | 30 | F | bilateral non-union | Humerus | 3 |
| 8 | 42 | M | non-union on plate | Femur | 3 |
| 9 | 55 | M | non-union on plate | Femur | 4 |
| 10 | 37 | M | nonunion on nail | Femur | 5 |
| 11 | 41 | M | non-union | Femur | 3,5 |
2.2. Surgical Technique
Bone reconstruction was performed as described by Masquelet,3 in two operating stages.
The first stage consisted in the interposition of an acrylic cement spacer inside the bone loss associated either to an internal or external rigid fixation and with sometimes a cutaneous flap when necessary on the leg. Sometimes, when achieving osteosynthesis and when the size of the bone loss was very large we allowed a bone shortening of 1 to 2 cm. This stage was preceded by excision of the infected or devitalized tissues inside the defect. Medullary canal was re-sealed and the bone ends edged. The surgical approach was closed under an aspirative drainage.
The second operation was carried out from 6 up to 8 weeks later, using the same approach. This step consisted in a careful removal of the spacer respecting its membrane. A decortication of the bone ends was then carried out before filling of the biological cavity using fragmented cortical and cancellous bone grafts harvested from the anterior iliac crest. In all cases, it was not possible to suture the membrane. The surgical approach was closed under an aspirative drainage.
Antibioprophylaxy or antibiotherapy associated to preventive anticoagulation were administered postoperatively. The drain was removed the second day after operation and there was a first period of non-weight bearing.
2.3. Patients follow-up method
The bone defect length was measured intraoperatively in the first surgical stage; Sometimes underestimated because large proportions would involve the use of large quantity of autografts. Patients were followed-up as outpatients after 6 weeks, 3 months and 1 year. Bone healing process was assessed on antero-posterior and lateral X-rays of the affected limb segment. Follow-up duration was considered from the second operative stage and the complications were then listed.
3. Results
The 11 patients of our study had a mean follow-up of 6.54 months (3–11). Radiological healing was observed in 6 patients (4 femurs and 2 humerus). The mean healing period was 8.5 months (5–11), after the second stage. Bone osteo-integration is ongoing in 4 patients (2 femurs and 2 tibias). The mean period between trauma and reconstruction was 8 months (20 days–3 years). The listed complications were: a case of trans tibial amputation not related to the technique itself but due to an initial gangrene, and a case of secondary infection with partial resorption of the graft. In one case, osteosynthesis was modified because of bad impaction. The plate was replaced with an Orthofix external fixator. Table 2 summarizes the results of the series.
Table 2.
Stabilization Mode, type of transplant performed, complications and consolidation time.
| Case | Stabilization Mode | Graft Additional | complications/ Gestures | Consolidation (months) |
|---|---|---|---|---|
| 1 | FE | Anterior iliac crest | Tibial Amputation | |
| 2 | Plate | Anterior iliac crest | - | 10 |
| 3 | Plate | Anterior iliac crest | Delay | |
| 4 | FE | Anterior iliac crest | septic resurgence | Delay |
| 5 | FE | Anterior iliac crest | Shred | Delay |
| 6 | Plate | Anterior iliac crest | - | 5 |
| 7 | Plate | Anterior iliac crest | - | 6 |
| 8 | Plate | Anterior iliac crest | - | 11 |
| 9 | Plate | Anterior iliac crest | - | 10 |
| 10 | Plate/FE | Anterior iliac crest | plate rupture | 9 |
| 11 | Plate | Anterior iliac crest | - | Delay |
FE: external fixator.
4. Discussion
The induced membrane technique described by Masquelet offers a new option in the management of bone loss. We have been able to treat iterative defects on various limb segments. This therapeutic strategy was chosen so to avoid failures in the treatment of non-unions due either to bone implants release or to osteopenia caused by bone-setters who prescribed several months of fracture immobilization (Fig. 1). This method has been proved to bring required substances for a bone good healing process. There are: the presence of a periosteal-like membrane and a cortical and cancellous graft.3, 4 Our study had two limitations. The first limitation is our weak technical platform: in one hand we faced difficulties in importing acrylic cement and in the other hand bone allograft is not available in our country; that reduced the number of patients included in this study. The second limitation is our empirical use of the available volume of harvested grafts after shortening the defect length; that explains why we did not calculate the bone index to be reconstructed. Young patients are more exposed to bone loss lesions. The mean age found in our series (40.45 years), agrees with that of Zappatera,5 and Medjamed and Khaznadar6 who found respectively 41.4 years (17-63) and 32 years (17-65). Our results in terms of healing confirm the importance of the biological cavity produced by the membrane when regenerating.3, 4 It has reduced the grafts resorption reported in conventional techniques. This technique is already done worldwide in traumatic bone loss,7, 8 and its indications have been extended to non-traumatic bone loss.9, 10, 11 Several series have been reported in order to assess the results of this technique. The largest series reported 84 patients (43 recent lesions and 41 non-unions) with a healing rate of 90%, and no failure was reported for recent lesions.12 The healing rate in our series was comparable to that of the recent series.4, 5, 12 Among the 11 patients 6 consolidated (Fig. 2) within a healing period of 8.5 months (5-11) and osteo-integration was ongoing in four others. A case of infectious complication was noted (Fig. 3). Biau et al.;13 Villemagne et al. 14 used cortical autograft (tibial) combined with allograft to increase the volume of the graft in the reconstruction of large bone losses. Another interesting perspective is the use of grafts harvested from the medullary canal of a long bone by the RIA (Reamer Irrigator Aspirator) process. It increases bone reconstruction capacities.15 In our series, we have empirically chosen a cortical and cancellous massive autograft harvested from the crest and fragmented, a material of reference. In one case, an impaction complication was noted and the osteosynthesis was performed with an Orthofix external fixation device (Fig. 4): that resulted in a corticalisation within 9 months. It seems, as suggested by Begué and Masquelet16 in their comparative study, that the option of external fixation is to be favored. Another complication at the beginning of the first stage of the technique was related to a post-traumatic gangrene of the leg but this had no relationship with the technique itself. This series seems too narrow for us to draw relevant conclusions. However the results obtained in a short term seem to show a satisfying bone reconstruction in this study and commit us to continue this technique in spite of our less performant technical platform.
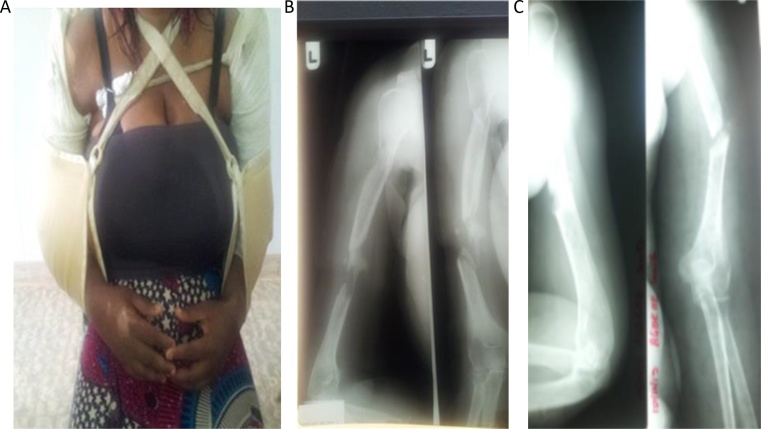
Fig. 1.
unconventional treatment (healer) bilateral humerus fracture in a woman 30 years (A). X-rays of the face and left humerus and right profile showing nonunion with consecutive losses to reboutage defect (B), (C).
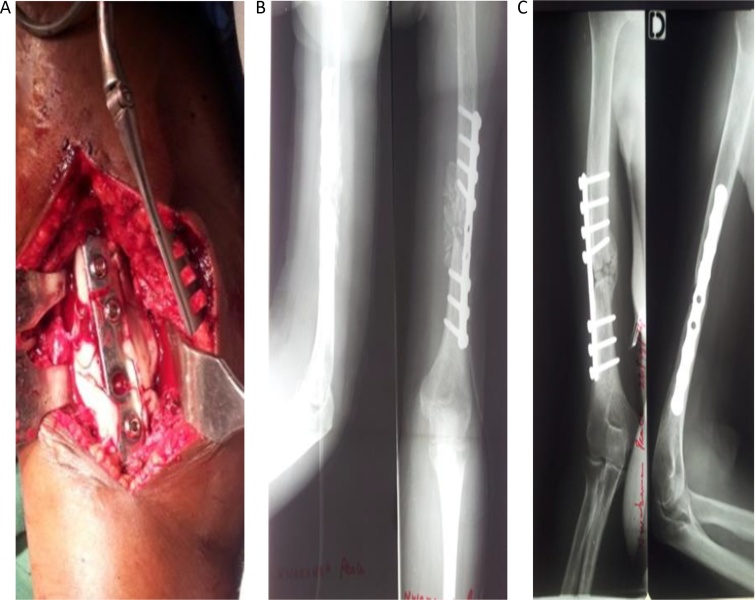
Fig. 2.
Reconstruction of a bone loss of 3 cm of the humerus in the treatment of an iterative nonunion. Establishment of a spacer acrylic cement, after a plate osteosynthesis (A), graft fragmented corticocancellous filling the defect (B), remote Radiography (5 months of transplantation) with an in corticalization (C).
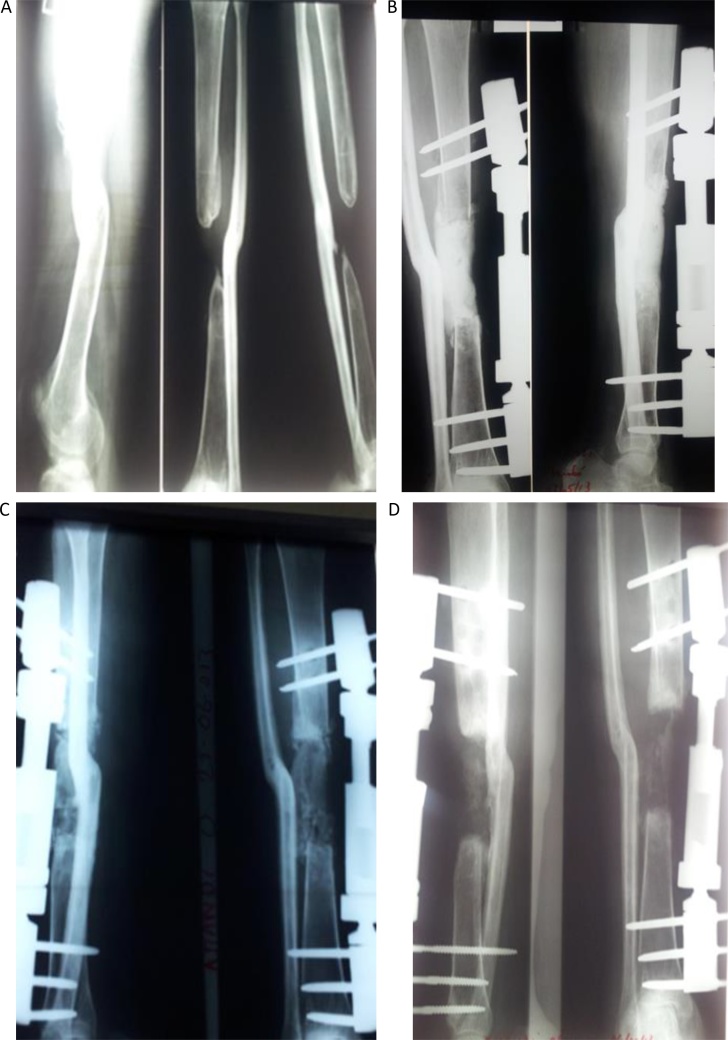
Fig. 3.
Reconstruction of a bone defect of the tibia in the treatment of septic nonunion (A). Bone by an external fixator with introduction of a spacer acrylic cement (B). X-ray after the cortico-cancellous graft fragmented (C). Radiograph (two months of transplantation) Resurgent Infectious partial resorption of grafts (D).
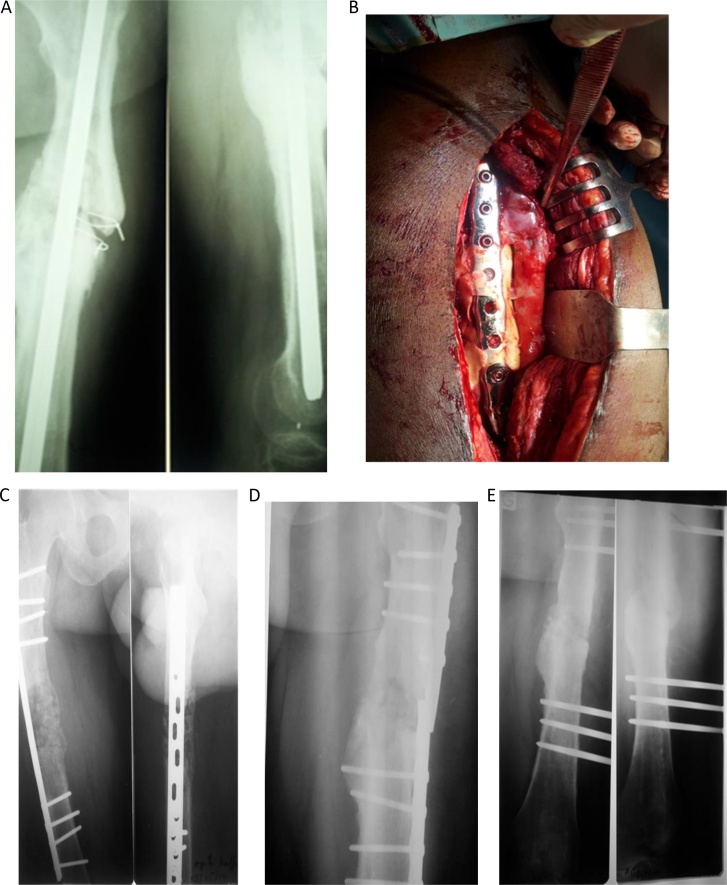
Fig. 4.
Pseudarthrosis on iterative hardware (A). Explantation of the nail, establishment of a acrylic spacer cement after plate fixation (B). Reconstruction of a loss of 5 cm defect with cancellous grafts fragmented cortical (C). Out of the plate (D). Radiography 9 months after stabilization by an external fixator. The femur is consolidated (E).
5. Conclusion
The technique of the induced membrane described by Masquelet enables to maintain the length of bone losses and then to reconstruct the volume of the preserved defect. It is an interesting alternative so to limit grafts resorption. This method allowed us to reconstruct bone loss due to conventional treatments failures. Our preliminary results encourage us to continue to perform this technique.
Conflict of Interest
None.
Contributor Information
Noufanangue Kanfitine Kombate, Email: kludovick67@yahoo.fr.
Atchi Walla, Email: atchi.walla@yahoo.fr.
Gamal Ayouba, Email: gamal702003@yahoo.fr.
B. Moïse Bakriga, Email: bakriga@yahoo.fr.
Yaovi Yannick Dellanh, Email: yandellanh@yahoo.fr.
Anani Grégoire Abalo, Email: abalgreg@yahoo.fr.
Assang Michel Dossim, Email: adossim@gmail.com.
References
- 1.Keating J.F., Simpson A.H.R.W., Rbinson C.M. The management of fractures with bone loss. J Bone Joint Surg (Br) 2005;87-B:142–150. doi: 10.1302/0301-620x.87b2.15874. [DOI] [PubMed] [Google Scholar]
- 2.Obert L., Couesmes A., Lepage D., Paul- chot J. Bone healing and nonunion of long bones: the contribution of BMP. e – memories of the National Academy of Surgery. 2007;6(2):24–30. [Google Scholar]
- 3.Masquelet A.C., Fitousi F., Bégué T., Muller G.P. Reconstruction of long bone induced by membrane and autologous spongy. Ann Chir Plast Esthet. 2000;45:346–353. [PubMed] [Google Scholar]
- 4.Masquelet A.C., Bégué T. The concept of induced membrane for reconstruction of long bone defects. Orthop Clin North Am. 2010;41:27–37. doi: 10.1016/j.ocl.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 5.Zappatera T. reconstruction of bone defects of upper limb loss. Prospective study about 9 cases. Orthop Surg Traumatol Res. 2010;96(7):125–130. [Google Scholar]
- 6.Medjamed M., Khaznadar M.S. Loss of post-traumatic bone. Rev Chir Orthop Alg. 2010;2:9–13. [Google Scholar]
- 7.Sales de Gauzy J., Fitoussi F., Jouve J.L., Karger C. Traumatic diaphyseal bone defects in children. Orthop Surg Traumatol Res. 2012;98:220–226. doi: 10.1016/j.otsr.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 8.Chong K.W., Woon C.Y., Wong M.K. Induced membrane technology of staged bone grafting for segmental bone loss: surgical technology. J Bone Joint Surg Am. 2011;93(suppl 1):85–91. doi: 10.2106/JBJS.J.01251. [DOI] [PubMed] [Google Scholar]
- 9.Chotel F., Nguiabadan L., Braillon P., Kohler R. Induced membrane technology for reconstruction after-bone tumor resection in children: a preliminary study. Orthop Surg Traumatol Res. 2012;98:301–308. doi: 10.1016/j.otsr.2011.11.008. [DOI] [PubMed] [Google Scholar]
- 10.Pannier S. Congenital pseudarthrosis of the tibia. Orthop Surg Traumatol Res. 2011;97:750–761. doi: 10.1016/j.otsr.2011.09.001. [DOI] [PubMed] [Google Scholar]
- 11.Gouron R., Deroussen F., Juvet-Segarra M. Reconstruction of congenital pseudarthrosis of the clavicle with use of the technical Masquelet a postponement boxes. J Bone Joint Surg Am Case Connector. 2012;2:E77. doi: 10.2106/JBJS.CC.L.00095. [DOI] [PubMed] [Google Scholar]
- 12.Karger C., Kishi T., Schneider L., Fitoussi F. Treatment of posttraumatic bone defects induced by the technical membrane. Orthop Surg Traumatol Res. 2012;98:97–102. doi: 10.1016/j.otsr.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 13.Biau D.J., Pannier S., Masquelet A.C., Glorion C. Case report: reconstruction of a 16 cm defect after-daiphyseal Ewing's resection in a child. Clin Orthop Relat Res. 2009;467:572–577. doi: 10.1007/s11999-008-0605-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Villemagne T., Bonnard C., Accadbled F., Kaissi M. Intercalary segmental reconstruction of long bones after-malignant bone tumor resection using methyl methacrylate cement spacer primary and secondary bone grafting interposition: the induced membrane technology. J Pediatric Orthop. 2011;31:570–576. doi: 10.1097/BPO.0b013e31821ffa82. [DOI] [PubMed] [Google Scholar]
- 15.Stafford P.R., Noris B.L. Irrigator-aspirator Reamer-bone graft and technical Masquelet for bi-segmental bone nonunion defect: a review of 25 cases. Injury. 2010;41(Suppl 2):72–77. doi: 10.1016/S0020-1383(10)70014-0. [DOI] [PubMed] [Google Scholar]
- 16.Begué T., Masquelet A.C. 2011. Osteosynthesis of Reconstruction after Bone Loss Substance segmental or cavitary: Comparative study of plates, external fixators and nailing. 10.1016/j.rcot.2011.08.132. [Google Scholar]