Abstract
Objectives To compare the efficacy of standard treatment, standard treatment plus acupuncture, and standard treatment plus stabilising exercises for pelvic girdle pain during pregnancy.
Design Randomised single blind controlled trial.
Settings East Hospital, Gothenburg, and 27 maternity care centres in Sweden.
Participants 386 pregnant women with pelvic girdle pain.
Interventions Treatment for six weeks with standard treatment (n = 130), standard treatment plus acupuncture (n = 125), or standard treatment plus stabilising exercises (n = 131).
Main outcome measures Primary outcome measure was pain (visual analogue scale); secondary outcome measure was assessment of severity of pelvic girdle pain by an independent examiner before and after treatment.
Results After treatment the stabilising exercise group had less pain than the standard group in the morning (median difference = 9, 95% confidence interval 1.7 to 12.8; P = 0.0312) and in the evening (13, 2.7 to 17.5; P = 0.0245). The acupuncture group, in turn, had less pain in the evening than the stabilising exercise group (-14, -18.1 to -3.3; P = 0.0130). Furthermore, the acupuncture group had less pain than the standard treatment group in the morning (12, 5.9 to 17.3; P < 0.001) and in the evening (27, 13.3 to 29.5; P < 0.001). Attenuation of pelvic girdle pain as assessed by the independent examiner was greatest in the acupuncture group.
Conclusion Acupuncture and stabilising exercises constitute efficient complements to standard treatment for the management of pelvic girdle pain during pregnancy. Acupuncture was superior to stabilising exercises in this study.
Introduction
Pelvic girdle pain is a common complaint among pregnant women worldwide,1 and it causes severe pain in one third of affected women.2,3 Strenuous work, previous low back pain, and previous pelvic girdle pain are known risk factors.3,4
Pelvic girdle pain generally arises in relation to pregnancy, trauma, or reactive arthritis. Pain is experienced between the posterior iliac crest and the gluteal fold, particularly in the vicinity of the sacroiliac joints. The pain may radiate in the posterior thigh and can occur in conjunction or separately in the symphysis. The endurance capacity for standing, walking, and sitting is diminished.5 After pregnancy problems remain serious in about 7% of women with pelvic girdle pain, causing severe discomfort and reducing ability to work.3,6
Most studies do not distinguish between lumbar back pain and pelvic girdle pain.6 Unspecified diagnosis is a problem, as the two conditions differ with respect to prognosis and treatment.2,5 If a patient with pelvic girdle pain is treated for low back pain, the symptoms may be aggravated.2 Pelvic girdle pain must be reproducible by specific pain provocation tests.3,5,7,8 The posterior pelvic pain provocation test and Patrick's fabere test have the best sensitivity if pain is evident in the sacroiliac joints.5,8 Modified Trendelenburg's test and palpation of the symphysis have better sensitivity if pain is evident in the symphysis pubis.8 These tests have high intertester reliability.5,8
Standard treatment may consist of a pelvic belt, a home exercise programme, and patient education. A systematic review has shown that the efficacy of these interventions remains questionable.9 Current treatment increasingly includes stabilising exercises and acupuncture.10-12 However, insufficient evidence is available to give strong recommendations for or against any particular treatment modality for pelvic girdle pain.13 We compared the efficacy of acupuncture or stabilising exercises as an adjunct to standard treatment with standard treatment alone for the treatment of pelvic girdle pain in pregnant women.
Methods
The study was a randomised single blind trial done at East Hospital, Sahlgrenska Academy, and at 27 maternity care centres in the hospital's reference area in Gothenburg, Sweden, from 2000 to 2002.
Participants
Doctors and midwifes at the 27 maternity care centres preselected consecutive patients. Participants filled in a previously validated questionnaire2 and a diary for baseline information for one week before the inclusion visit. An independent specially trained physiotherapist then assessed patients who were eligible and willing to participate in the study. This assessment included a detailed standardised physical examination and collection of baseline data. The tests used were the posterior pelvic pain provocation test, Patrick's fabere test, a modified Trendelenburg's test, Lasegue test, and palpation of the symphysis pubis.5,8 The main inclusion criteria were healthy women at 12-31 completed gestational weeks, well integrated in the Swedish language, with singleton fetuses and defined pregnancy related pelvic girdle pain. We excluded patients with other pain conditions, systemic disorders, or contraindications to treatment. The participants gave informed consent.
Randomisation
A research assistant used a computer generated random table to determine the allocation sequence before the study. Groups were coded, and the allocation was transferred to a series of presealed opaque envelopes. The independent examiner randomised the patients individually after doing the baseline assessment.
Treatment protocols
The study comprised a one week baseline period, six weeks of treatment, and follow up one week after the last treatment. Patients were asked to avoid other treatments during the intervention period. Three experienced physiotherapists gave standard treatment, two experienced medical acupuncturists did acupuncture, and two experienced physiotherapists gave the stabilising exercises. All possible adverse events were recorded.
Standard treatment group—Standard treatment consisted of general information about the condition and anatomy of the back and pelvis. Adequate advice was given about activities of daily living. The physiotherapist made sure that the patient understood and respected the relation between impairment, load demand, and actual loading capacity as well as the importance of necessary rest. The purpose of this information was to reduce fear and to enable patients to become active in their own treatment. The patients were given a pelvic belt (Puff Igång AB, Sweden) and a home exercise programme designed to increase strength in the abdominal and gluteal muscles.
Acupuncture—Patients received the same treatment as in the standard group but in addition had acupuncture. Local acupuncture points were selected individually after diagnostic palpation to identify sensitive spots.14 A total of 10 segmental points and seven extrasegmental points were used (table 1). The needles (Hegu AB, Landsbro, Sweden) were made of stainless steel (Ø 0.30) and inserted intramuscularly to a depth of 15-70 mm to evoke needle sensation (De Qi), described as tension, numbness, and often a radiating sensation from the point of insertion, reflecting activation of muscle-nerve afferents. The needles were left in situ for 30 minutes and manually stimulated every 10 minutes. Treatment was given twice a week over six weeks. Fetal heart rate and maternal heart rate and blood pressure were monitored before and after all treatments.
Table 1.
Acupuncture points, their anatomical position, and their innervation
| Points | Segmental innervation | Muscle localisation |
|---|---|---|
| GV 20 | Nn trigeminus (V), occipitalis minor (C2), occipitalis major (C2-3) | Aponeurosis epicrani tissue |
| LI 4 bilateral | Nn ulnaris medianus (C8, Th 1) | Mm interosseus dorsalis I, lumbricalis II, adductor pollicis |
| BL 26 bilateral | Nn thoracodorsalis (C6-8) toracicus (Th 9-12), lumbalis (L1-3) | NN thoracolumbalis, m erector spinae |
| BL 32 bilateral | Nn thoracodorsalis (C6-8), toracicus (Th 9-12), lumbalis (L1-3) | Fascia thoracolumbalis, m erector spinae |
| BL 33 bilateral | Nn thoracodorsalis (C6-8), toracicus (Th 9-12), lumbalis (L1-3) | Fascia thoracolumbalis, m erector spinae |
| BL 54 bilateral | N gluteus inferior (L5, S1-2) | M gluteus maximus |
| KI 11 bilateral | N thoracius (Th 6-12), subcostalis | Vagina m recti abdominis |
| BL 60 bilateral | N suralis (S2) | Fibrotic tissue |
| EX 21 bilateral | Nn lumbalis, sacralis (L4-5, S1-2) | Fascia thoracolumbalis, m erector spinae |
| GB 30 bilateral | N gluteus inferior (L5, S1), obturatorius internus (L4-5, S1) | Mm gluteus maximus, gemellus superior, piriformis |
| SP 12 bilateral | Nn thoracicus, lumbalis (Th 7-12, L1) | Aponeurosis mm obliquus externus, abdominus internus |
| ST 36 bilateral | N peroneus profundus (L4-5) | M tibialis anterior |
BL=bladder channel; EX-extra channel; GB=gall bladder channel; GV=govenor vessel channel; KI=kidney channel; LI=large intestine channel; SP=spleen channel; ST=stomach channel.
Stabilising exercises—Patients received the same treatment as in the standard group but in addition did stabilising exercises modified because of the pregnancy (box).15,16 The training programme started by emphasising activation and control of local deep lumbopelvic muscles. Training of more superficial muscles in dynamic exercises to improve mobility, strength, and endurance capacity was gradually included. Patients received treatments individually for a total of six hours during six weeks. They were told to integrate the exercises in daily activities and to exercise in short sessions on several occasions during the day.
Outcome measures
Primary outcome measure—Patients scored their current intensity of pelvic pain related to motion on a 100 point visual analogue scale every morning and every evening in the diaries.
Secondary outcome measures—The independent examiner assessed recovery from symptoms. Patients were asked not to reveal any information about their treatment during assessment.
Statistical analysis
When planning the study we assumed that the mean pain score related to motion at baseline would be 60 mm (visual analogue scale) in all three groups. We did not expect any treatment effect in the standard group. We assumed that the mean pain score after treatment would be 60 mm in the standard group, 50 mm in one treatment group, and 40 mm in the other. To achieve a 90% power of detecting a significance (at the two sided 5% level), with an assumed standard deviation of 40, we needed 103 patients for each study group. To compensate for an anticipated loss to follow up of 20%, we needed 386 patients. When analysing the study we decided to apply the Mann-Whitney U test for comparing changes in pain scores, with Bonferroni's correction (P values multiplied by three). The power achieved with that method was 86% for comparison of the two most extreme groups, provided that Δμ/σ = 0.5.
Personnel from an independent institution coded all results from the study and entered them into a database. Analyses were done by intention to treat. The statistician who did the analysis was blinded to group and treatment. In the analysis of the pain diaries we defined the median visual analogue scale baseline levels in the mornings and in the evenings for each patient by calculating the median for the days before treatment (five to seven days). The same calculations of median pain were done for the first week after the end of treatment.
Treatment protocol for the stabilising exercise group
Additional information about anatomy and the genesis of pelvic pain and discussion about how the basic written regimen could be integrated at home and at work
Exercises for stabilising the pelvis and back—that is, training of the transversus abdominis and the multifides facilitated by contractions of the pelvic floor muscles, according to Richardson and Jull but modified because of the pregnancy.16 While the standard positions (prone and supine) were not suitable the pressure biofeedback unit was not used. The exercises were done with the patient lying on her side, four point kneeling, sitting, and standing. Arm and leg movements were added when the basic movement was correct
Exercises for increasing circulation in hip rotator muscles. The exercises were done with many repetitions during low force and in a limited range of motion in a side lying position with a pillow between the legs or sitting without foot support
Massage, effleurage, and petrissage of hip extensors and rotators
Stretching of hip external rotators and extensors in the sitting position: 20 sec/stretch
We calculated the medians, quartiles, means, and standard deviations when possible. We used the Mann-Whitney U test to compare differences between the groups for continuous variables and χ2 for categorical variables. Adjustments (multiplication by three) of the P values due to multiple comparisons were done by Bonferroni's method. We considered an adjusted P value < 0.05 to be statistically significant. We calculated median differences and confidence intervals for the differences between medians on the basis of the Mann-Whitney U test. We also did an analysis of treatment effects in patients divided into four subgroups17: one sided sacroiliac pain, double sided sacroiliac pain, one sided sacroiliac pain plus symphysis pubis pain, and pelvic girdle syndrome (double sided sacroiliac pain plus symphysis pubis pain). The results were analysed with the SAS software package, version V8.
Results
Randomisation and progress through the trial
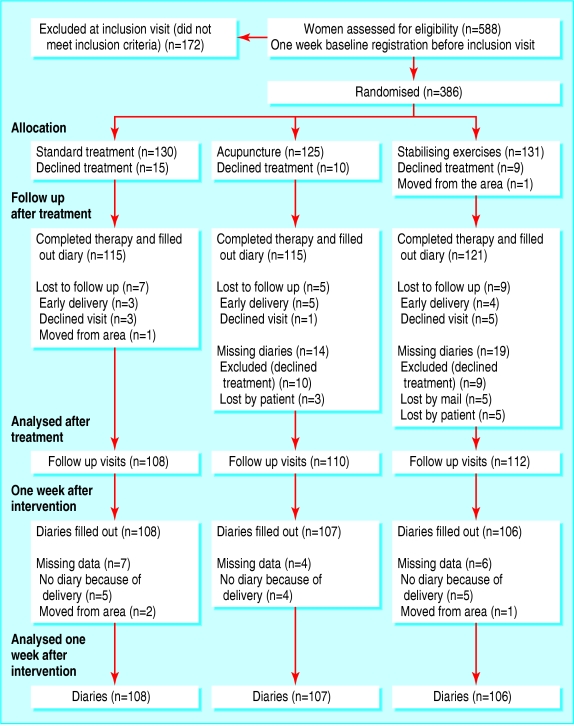
Of 558 women referred for the first assessment, 172 did not meet the inclusion criteria; 386 women were included in the trial. Baseline characteristics were similar in the three treatment groups (table 2). The figure show the progress of patients through the trial and withdrawals from the study.
Table 2.
Characteristics of 386 pregnant women with pelvic girdle pain included in trial. Values are numbers (percentages) unless stated otherwise
| Characteristic | Standard group (n=130) | Acupuncture group (n=125) | Stabilising exercise group (n=131) |
|---|---|---|---|
| Mean (SD) maternal age (years) | 30.8 (4.8) | 30.6 (4) | 30.0 (4) |
| Gestation weeks (+ days) at inclusion | 24 (+3) | 24 (+3) | 24 (+3) |
| First pregnancy | 33 (25) | 34 (27) | 36 (27) |
| Full time work | 71 (55) | 72 (58) | 76 (58) |
| Smoker | 12 (9) | 11 (9) | 13 (10) |
| Previous low back pain | 90 (69) | 89 (71) | 84 (64) |
| Physical activity during leisure before pregnancy:
|
|
|
|
| Not at all | 29 (22) | 36 (29) | 30 (23) |
| Once a week | 52 (40) | 37 (30) | 50 (38) |
| More than twice a week | 50 (38) | 51 (41) | 50 (38) |
| Lifting heavy objects >10 times a day | 59 (45) | 50 (40) | 53 (40) |
| No or rare ability to take rest breaks | 76 (58) | 72 (58) | 68 (52) |
Figure 1.
Participants' progress through trial and withdrawals
Primary outcome measure
Table 3 shows improvements in pain scores. The reduction in pain was most pronounced in the evening in the acupuncture group one week after the end of treatment, compared with the other treatment groups.
Table 3.
Primary outcome measure: pain on visual analogue scale related to motion one week after treatment compared with baseline measurements
|
Standard group
|
Acupuncture group
|
Stabilising exercise group
|
Group comparisons
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| Pain | No | Median (25th-75th centile) | No | Median (25th-75th centile) | No | Median (25th-75th centile) | Comparison | Differences of medians (95% CI) | *P values |
| Morning: | |||||||||
| Baseline | 131 | 23 (13-41) | 125 | 23 (15-44) | 130 | 22 (13-43) | |||
| One week after treatment | 108 | 27 (12-58) | 107 | 15 (7-29) | 106 | 18 (9-37) | S-ACU:
|
12 (5.9 to 17.3)
|
<0.001
|
| S-SE:
|
9 (1.7 to 12.8)
|
0.0312
|
|||||||
| ACU-SE: | −3 (−7.8 to 0.3) | NS | |||||||
| Evening: | |||||||||
| Baseline | 131 | 63 (49-75) | 125 | 65 (47-76) | 130 | 60 (4-73) | |||
| One week after treatment | 108 | 58 (40-74) | 107 | 31 (12-58) | 106 | 45 (21-68) | S-ACU:
|
27 (13.3 to 29.5)
|
<0.001
|
| S-SE:
|
13 (2.7 to 17.5)
|
0.0245
|
|||||||
| ACU-SE: | −14 (−18.1 to −3.3) | 0.0130 | |||||||
ACU-acupuncture; S=standard; SE=stabilising exercise.
P values from Mann-Whitney U test. All original two tailed P values were multiplied by three (Bonferroni's correction); NS=not significant.
Secondary outcome measures
Table 4 shows that attenuation of pelvic girdle pain assessed by the independent examiner was greatest in the acupuncture group. Three of four subgroups of pelvic girdle pain improved after acupuncture compared with standard treatment and one of four subgroups improved compared with the stabilising exercise group.
Table 4.
Secondary outcome measure: assessment of severity of pelvic girdle pain by an independent examiner before intervention and at follow up after last treatment. Values are numbers (percentages) unless stated otherwise
|
Standard group
|
Acupuncture group
|
Stabilising exercise group
|
Group comparisons after treatment
|
|||||
|---|---|---|---|---|---|---|---|---|
| Inclusion (n=130) | Follow up (n=108) | Inclusion (n=125) | Follow up (n=110) | Inclusion (n=131) | Follow up (n=112) | Comparison | P value* | |
| Tests for assessment of pelvic girdle pain | ||||||||
| Positive pain drawing | 130 (100) | 100 (93) | 125 (100) | 94 (85) | 131 (100) | 97 (87) | NS | |
| Posterior pelvic pain provocation test | 130 (100) | 92 (85) | 125 (100) | 72 (65) | 131 (100) | 95 (85) | ACU-S
|
0.0021
|
| ACU-SE | 0.0024 | |||||||
| Pain when turning in bed | 130 (100) | 95 (88) | 125 (100) | 73 (66) | 131 (100) | 80 (71) | ACU-S
|
<0.001
|
| SE-S | 0.0072 | |||||||
| Palpation of public symphysis | 47 (36) | 50 (46) | 51 (41) | 32 (29) | 62 (47) | 39 (35) | ACU-S | 0.0261 |
| Patrick's fabere test | 65 (50) | 57 (53) | 69 (55) | 36 (33) | 74 (56) | 47 (42) | ACU-S | 0.0084 |
| Trendelenburg's test | 51 (39) | 43 (40) | 52 (42) | 30 (27) | 45 (34) | 30 (27) | NS | |
| Subgroups of pelvic girdle pain | ||||||||
| Pelvic girdle syndrome | 34 (26) | 33 (31) | 43 (34) | 20 (18) | 49 (37) | 25 (22) | NS | |
| Double sided sacroiliac pain | 47 (36) | 50 (46) | 51 (41) | 32 (29) | 62 (47) | 39 (35) | ACU-S | 0.0261 |
| One sided sacroiliac pain + symphysis pubis pain | 49 (38) | 45 (42) | 51 (41) | 23 (21) | 63 (48) | 36 (32) | ACU-S | 0.0027 |
| One sided sacroiliac pain | 130 (100) | 92 (85) | 125 (100) | 72 (65) | 131 (100) | 95 (85) | ACU-S
|
0.0021
|
| ACU-SE | 0.0024 | |||||||
ACU=acupuncture; S=standard; SE=stabilising exercise.
P values from χ2 test. All original P values were multiplied by three (Bonferroni's correction); NS=not significant.
Side effects
No serious complication occurred during treatments or during the follow up period after any of the treatments.
Discussion
The main finding of this study was that acupuncture or stabilising exercises as an adjunct to standard treatment offer clear clinical advantages over standard treatment alone for reduction of pain in pregnant women with pelvic girdle pain. This is supported by the patients' own estimates and by independent examiners. Our results are also supported by earlier findings that showed beneficial effects of stabilising exercises for women with pelvic girdle pain after pregnancy.10 The training was aimed at affecting dysfunction of the muscle-tendon-fascia system that controls force closure of the pelvis.18 Exactly how the exercises influence this system is unknown, but research has shown that contraction of the transversus abdominis decreases the laxity of the sacroiliac joint.15 The exercises were intended to affect mainly the local stability system, but whether an addition of global stabilising muscle exercises could have provided the same effect is not known. No major differences exist between current recommendations about stabilisation training and the exercises given in our study.15
The stabilisation group also got additional treatment of stretching exercises of specific muscles plus massage. All treatment was more or less multifactorial, and massage as well as stretching may have had some contributory effect. The main training, however, was the stabilisation exercises that were done on several occasions during the day, in contrast to the stretching or massage that was done only at the visits.
In the standard group, pain remained constant during treatment. This is in line with earlier findings that indicated lack of evidence for the effect of standard treatment for pelvic girdle pain.9
Previous studies of acupuncture for low back pain in pregnancy reported pain relief.11,12 However, these studies had methodological shortcomings, as the type of back pain was not clearly defined. Furthermore, the acupuncture stimulation given previously must be considered weak compared with that given in studies of men and non-pregnant women. One of the studiesused almost exclusively auricular acupuncture11; the other study used segmental points, but no extrasegmental points were used and no further stimulation after insertion was given.12 Our findings that acupuncture gives acceptable pain relief in women with pelvic girdle pain is supported by physiological models explaining the mechanisms in the treatment of both acute and chronic pain conditions.14,19
What is already known on this topic
No cure exists for pelvic girdle pain during pregnancy
No studies have been published on the effects of acupuncture on well defined isolated pelvic girdle pain during pregnancy
What this study adds
This study shows large treatment effects on pain among pregnant women with well defined isolated pelvic girdle pain
Acupuncture was the treatment of choice for patients with one sided sacroiliac pain, one sided sacroiliac pain combined with symphysis pubis pain, and double sided sacroiliac pain
Pain may be inhibited at the segmental level, and for this reason the acupuncture points were selected in muscle segments according to the patient's pain drawing, including diagnostic palpation to identify sensitive spots. The aim was to establish control of pelvic pain to prevent dysfunction of muscles of the spine and pelvis. Speculatively, this was achieved through activation of both the segmental pain inhibitory system, involving the so called gate control mechanism, and the central pain inhibitory system, involving secretion of endogenous opioids.14 Extrasegmental points to the lumbosacral area were used to strengthen and lengthen the effect of the central control systems. In addition, well known general pain relieving points were selected. Whether the choice of acupuncture points and the method of stimulation in this study are optimal remains to be elucidated.
Earlier research found that poor muscle function in the back and pelvis at the beginning of pregnancy is related to severe pain and disability throughout pregnancy.20 This could be the case for the patients in the standard and stabilising exercise groups, as the acupuncture group estimated significantly lower visual analogue scale ratings after treatment. The acupuncture treatment succeeded in establishing control of the pain, and this may have been important in preventing dysfunction of muscles. Our results are supported by earlier research on acupuncture for low back pain.21,22
This study shows that methods other than structured physiotherapy may be effective in treating pelvic girdle pain in pregnancy and that acupuncture represents an effective alternative. A combination of several methods is probably even better. Each method needs to be evaluated individually, however, before combinations can be recommended for future research, and only after that should recommendations for treatment be made.
We conclude that acupuncture as well as stabilising exercises constitute effective complements to standard treatment for pregnant women with pelvic girdle pain. Acupuncture was superior to stabilising exercises in this study. The findings are of particular importance because no previous study has shown such marked treatment effects among pregnant women with well defined pelvic girdle pain.
We thank physiotherapists E Roos-Hansson and G Zetherstrom for invaluable help with assessment of the patients. We thank physiotherapists T Larsson and K Wettergren and midwife K Frygner for treating the patients. We also express our appreciation to all the women for their contributions to this study.
Contributors: HE initiated and coordinated the study, did most of the data collection, and contributed to study design and interpretation of results. LL advised on data collection and assisted in study design. MFO assisted in study design and gathered data. H-CO guided the scientific process, assisted in study design, provided advice on the epidemiology of pelvic girdle pain, and obtained funding. HH guided the scientific process and assisted in study design. All investigators contributed to data interpretation and preparation of the manuscript. H-CO and HH are the guarantors.
Funding: The Vardal Foundation, the Dagmar Foundation, the Trygg-Hansa Insurance Company, and Sahlgrenska University Foundation provided funding. The study sponsors had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Competing interests: None declared.
Ethical approval: The local ethics committee approved the study.
References
- 1.Bjorklund K, Bergstrom S. Is pelvic pain in pregnancy a welfare complaint? Acta Obstet Gynecol Scand 2000;79: 24-30. [DOI] [PubMed] [Google Scholar]
- 2.Ostgaard HC, Roos-Hansson E, Zetherstrom G. Regression of back and posterior pelvic pain after pregnancy. Spine 1996;21: 2777-80. [DOI] [PubMed] [Google Scholar]
- 3.Wu WH, Meijer MO, Uegaki K, Mens JM, van Dieen JH, Wuisman PI, et al. Pregnancy-related pelvic girdle pain (PPP), I: terminology, presentation, and prevalence. Eur Spine J 2004;13: 575-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ostgaard HC, Zetherstrom G, Roos-Hansson E, Svanberg B. Reduction of back and posterior pelvic pain in pregnancy. Spine 1994;19: 894-900. [DOI] [PubMed] [Google Scholar]
- 5.Ostgaard HC, Zetherstrom G, Roos-Hansson E. The posterior pelvic pain provocation test in pregnant women. Eur Spine J 1994;3: 258-60. [DOI] [PubMed] [Google Scholar]
- 6.Ostgaard HC, Zetherstrom G, Roos-Hansson E. Back pain in relation to pregnancy: a 6-year follow-up. Spine 1997;22: 2945-50. [DOI] [PubMed] [Google Scholar]
- 7.Kristiansson P, Svardsudd K. Discriminatory power of tests applied in back pain during pregnancy. Spine 1996;21: 2337-43. [DOI] [PubMed] [Google Scholar]
- 8.Albert H, Godskesen M, Westergaard J. Evaluation of clinical tests used in classification procedures in pregnancy-related pelvic joint pain. Eur Spine J 2000;9: 161-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stuge B, Hilde G, Vollestad N. Physical therapy for pregnancy-related low back and pelvic pain: a systematic review. Acta Obstet Gynecol Scand 2003;82: 983-90. [DOI] [PubMed] [Google Scholar]
- 10.Stuge B, Veierod MB, Laerum E, Vollestad N. The efficacy of a treatment program focusing on specific stabilizing exercises for pelvic girdle pain after pregnancy: a two-year follow-up of a randomized clinical trial. Spine 2004;29: E197-203. [DOI] [PubMed] [Google Scholar]
- 11.Wedenberg K, Moen B, Norling A. A prospective randomized study comparing acupuncture with physiotherapy for low-back and pelvic pain in pregnancy. Acta Obstet Gynecol Scand 2000;79: 331-5. [PubMed] [Google Scholar]
- 12.Kvorning N, Holmberg C, Grennert L, Aberg A, Akeson J. Acupuncture relieves pelvic and low-back pain in late pregnancy. Acta Obstet Gynecol Scand 2004;83: 246-50. [DOI] [PubMed] [Google Scholar]
- 13.Young G, Jewell D. Interventions for preventing and treating pelvic and back pain in pregnancy. Cochrane Database Syst Rev 2002;(1): CD001139. [DOI] [PubMed]
- 14.Melzack R, Wall PD. Pain mechanism: a new theory. Science 1965;150: 971-9. [DOI] [PubMed] [Google Scholar]
- 15.Richardson CA, Snijders CJ, Hides JA, Damen L, Pas MS, Storm J. The relation between the transversus abdominis muscles, sacroiliac joint mechanics, and low back pain. Spine 2002;27: 399-405. [DOI] [PubMed] [Google Scholar]
- 16.Richardson CA, Jull GA. Muscle control-pain control: what exercises would you prescribe? Man Ther 2000;1: 2-10. [DOI] [PubMed] [Google Scholar]
- 17.Albert HB, Godskesen M, Westergaard JG. Incidence of four syndromes of pregnancy-related pelvic joint pain. Spine 2002;27: 2831-4. [DOI] [PubMed] [Google Scholar]
- 18.Pool-Goudzwaard AL, Vleeming A, Stoeckart R, Snijders CJ, Mens JM. Insufficient lumbopelvic stability: a clinical, anatomical and biomechanical approach to `a-specific' low back pain. Man Ther 1998;3: 12-20. [DOI] [PubMed] [Google Scholar]
- 19.Andersson S, Lundeberg T. Acupuncture—from empiricism to science: functional background to acupuncture effects in pain and disease. Med Hypotheses 1995;45: 271-81. [DOI] [PubMed] [Google Scholar]
- 20.Sihvonen T, Huttunen M, Makkonen M, Airaksinen O. Functional changes in back muscle activity correlate with pain intensity and prediction of low back pain during pregnancy. Arch Phys Med Rehabil 1998;79: 1210-12. [DOI] [PubMed] [Google Scholar]
- 21.Coan RM, Wong G, Ku SL, Chan YC, Wang L, Ozer FT, et al. The acupuncture treatment of low back pain: a randomized controlled study. Am J Chin Med 1980;8: 181-9. [DOI] [PubMed] [Google Scholar]
- 22.Carlsson CP, Sjolund BH. Acupuncture for chronic low back pain: a randomized placebo-controlled study with long-term follow-up. Clin J Pain 2001;17: 296-305. [DOI] [PubMed] [Google Scholar]