Abstract
Objective
We investigated whether number of recent stressful life events is associated with incident cardiovascular disease (CVD) and whether this relationship is stronger in adults with a history of clinical depression.
Methods
Prospective data from 28,583 U.S. adults (mean age = 45 years) initially free of CVD who participated in Waves 1 (2001–2002) and 2 (2004–2005) of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) were examined. Number of past-year stressful life events (Wave 1), lifetime depressive disorder (Wave 1), and incident CVD (Wave 2) were determined by structured interviews.
Results
There were 1,069 cases of incident CVD. Each additional stressful life event was associated with a 15% increased odds of incident CVD [Odds Ratio (OR) = 1.15, 95% Confidence Interval (CI): 1.11, 1.19]. As hypothesized, a stressful life events by lifetime depressive disorder interaction was detected (P = 0.003). Stratified analyses indicated that stressful life events had a stronger association with incident CVD among adults with (OR = 1.18, 95% CI: 1.10, 1.27, n = 4,908) versus without (OR = 1.10, 95% CI: 1.07, 1.14, n = 23,675) a lifetime depressive disorder.
Conclusion
Our findings suggest that a greater number of recent stressful life events elevates the risk of new-onset CVD and that this risk is potentiated in adults with a history of clinical depression.
Keywords: life change events, stress, psychological, depressive disorder, cardiovascular diseases, prospective studies, epidemiologic studies
Introduction
A growing body of evidence supports a prospective relationship between chronic stress in adulthood and an increased risk of developing atherosclerotic cardiovascular disease (CVD) – i.e., clinical conditions that result from atherosclerosis including coronary artery disease (CAD), myocardial infarction (MI), arteriosclerosis, and angina. The majority of these studies have focused on overall perceived stress (1) or specific types of stress, such as work stress (2–5) or relationship stress (5–8). Fewer studies have examined the prospective link between the number of stressful life events and incident CVD, and the existing results are mixed. In the Multiple Risk Factor Intervention Trial involving only men, annual accumulation of stressful life events was positively associated with incident angina but not incident MI or CAD death (9). In the Copenhagen City Heart Study, a longitudinal relationship was observed between accumulation of adulthood stressful life events and incident stroke but not incident CAD or MI (10, 11). Finally, in two recent investigations, the Women’s Health Initiative which measured past-year stressful life events and the Multi-Ethnic Study of Atherosclerosis which measured ongoing stressful life events with durations longer than 6 months, stressful life events was associated with both incident CAD and stroke (12–14). Thus, it remains unclear whether number of stressful life events is associated with incident CVD. Moreover, no study to date has examined the stressful life events-CVD relationship in a large and diverse sample that is sociodemographically representative of the U.S. adult population.
The stressful life events-CVD relationship may be more pronounced in certain groups. Depressed adults may be one such group, as they exhibit altered physiologic and behavioral responses to stressors. First, depressed adults display delayed sympathetic (15), hypothalamic-pituitary-adrenal (HPA) axis (16), cardiovascular (17, 18), and inflammatory (19) recovery from laboratory-induced stress, suggesting that depression may interfere with normal homeostatic suppression of these physiologic stress response systems after a stressor has terminated (20). Indeed, ruminative perseverative cognition is a core feature of depression (21, 22), which may contribute to a prolonged stress response across autonomic, endocrine, cardiovascular, and inflammatory systems (23). Second, depressed adults are more likely than their nondepressed counterparts to engage in poor behavioral strategies to cope with stress (22), such as avoidance-based emotional eating and substance use (24, 25). In turn, these altered responses to stressors may promote the development and progression of atherosclerosis (20, 26, 27), thereby potentiating the effect of stressful life events on CVD in depressed adults. However, to our knowledge, no study has investigated whether depression moderates the relationship between stressful life events and incident CVD.
Accordingly, our objectives were to examine whether number of stressful life events is prospectively associated with new-onset CVD and whether depression moderates this relationship in a large sample of American men and women. We hypothesized that (a) number of recent stressful life events would be positively associated with incident CVD and (b) this association would be stronger in adults with versus without a lifetime history of a depressive disorder. We analyzed data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), a prospective cohort study of a large probability sample representative of the U.S. population. NESARC provided a good opportunity to test our hypotheses, given that this survey included measures of stressful life events and lifetime depressive disorder diagnoses at baseline, as well as clinical CVD at baseline and the 3-year follow-up.
Methods
Study Design and Sample
NESARC was conducted by the National Institute on Alcohol Abuse and Alcoholism to determine the prevalence of alcohol use disorders and associated disabilities in the U.S. civilian noninstitutionalized population ≥18 years (28–30). NESARC received ethical approval by the U.S. Census Bureau and the U.S. Office of Management and Budget. With involvement of the U.S. Census for sample design and field work, NESARC surveyed a representative sample of the U.S. adult population from counties across the 50 states, oversampling non-Hispanic Black people, Hispanic/Latino people, and young adults aged 18–24 years. Data were weighted to adjust for probabilities of selection, nonresponse, and oversampling. Weighted data were further adjusted to represent the U.S. civilian population for various sociodemographic variables, including region, age, sex, race, and ethnicity, based on the 2000 Decennial Census. Respondents underwent two waves of face-to-face, computer-assisted, home interviews separated by three years (mean = 36.6 months) assessing substance use disorders, psychiatric disorders, and medical conditions. Wave 1 (2001–2002) consisted of 43,093 respondents (81.0% response rate) and Wave 2 (2004–2005) consisted of 34,653 (86.7%) of the eligible Wave 1 respondents (70.2% cumulative response rate). To the Wave 2 sample, we applied four exclusion criteria. Respondents were excluded if: (1) CVD status at Wave 1 was missing (n = 1,719) or positive (n = 1,742), (2) CVD status at Wave 2 was missing (n = 1,112), (3) stressful life events or lifetime depressive disorder at Wave 1 was missing (n = 196), or (4) any covariates at Wave 1 were missing (n = 1,301). Table 1 displays the characteristics of our final sample of 28,583 U.S. adults.
Table 1.
Characteristics of sample (N = 28,583).
| Age, years, mean (SD) | 44.8 (17.0) |
| Female, % | 57.6 |
| Race/Ethnicity | |
| Non-Hispanic White, % | 58.2 |
| Non-Hispanic Black, % | 18.6 |
| Hispanic or Latino, % | 18.7 |
| Other, % | 4.5 |
| Education Level | |
| Less than High School, % | 15.2 |
| High School or Equivalent, % | 28.5 |
| Some College or Associate’s Degree | 30.6 |
| Bachelor’s Degree or Higher, % | 25.7 |
| Hypertension, % | 18.1 |
| Hypercholesterolemia, % | 19.2 |
| Diabetes, % | 8.0 |
| Tobacco Use, % | 25.6 |
| Body Mass Index, kg/m2, mean (SD) | 27.0 (5.6) |
| Number of Past-Year Stressful Life Events, mean (SD) | 1.6 (1.6) |
| Lifetime Depressive Disorder, % | 17.2 |
| Lifetime Major Depressive Disorder, % | 16.4 |
| Lifetime Dysthymic Disorder, % | 3.9 |
| Incident CVD, % | 3.7 |
| Incident Arteriosclerosis, % | 1.2 |
| Incident Angina, % | 2.6 |
| Incident Myocardial Infarction, % | 0.6 |
Measures
Stressful Life Events
NESARC developed a list of 12 stressful life events by adapting items from two existing measures: the List of Threatening Experiences (31) and the Schedule of Recent Events (31, 32). According to a previous factor analysis, these events fall into one of four stress domains: health, social, job, and legal (33). During the Wave 1 interview, respondents reported whether or not they had experienced the 12 stressful life events in the past year (see Figure 1 for the yes-no questions). This one-year recall period is recommended in order to capture a reasonable estimate of variability in event exposure and to avoid substantive decline in the ability of respondents to recall events beyond one year (34). From the stressful life events data, we computed a continuous stressful life events variable by summing the number of events and merging six or more events into a single category due to sparseness of data at higher values (number of past-year events: 0, 1, 2, 3, 4, 5, or 6+). This approach to constructing a continuous stressful life events variable has been utilized previously with NESARC data (35). Notably, test-retest correlations for stressful life events checklists are fairly stable (approximate r range for test-retest intervals of 6 months or more: 0.4 to 0.7), despite the longer recall period at retest likely reducing respondents recall ability (34).
Figure 1.
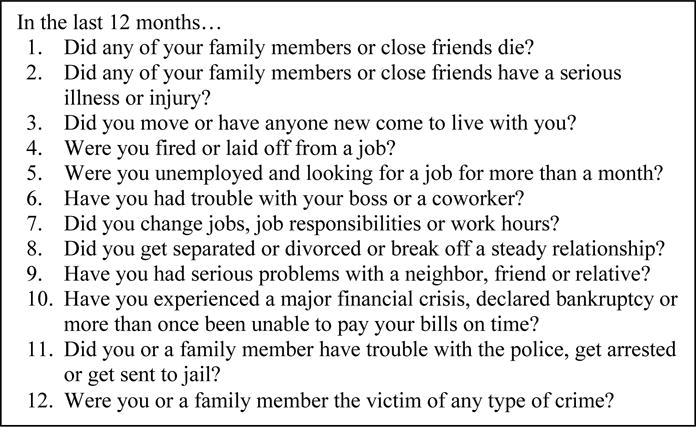
Questions assessing the number of past-year stressful life events at Wave 1 (2001–2002) of the National Epidemiologic Survey on Alcohol and Related Conditions.
Lifetime Depressive Disorder
The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV) was administered by lay interviews at Wave 1 to assess lifetime major depressive disorder and dysthymic disorder (36). The AUDADIS-IV, a fully structured diagnostic interview based on DSM-IV criteria, has demonstrated good test-retest reliability for depressive disorders and good agreement with clinician evaluations (30, 37). NESARC personnel coded diagnostic variables for the past year or prior to the past year. From the NESARC depression variables that excluded illness-induced and substance-induced disorders and ruled out bereavement (28), we calculated a dichotomous lifetime depressive disorder variable as follows: (1) yes: respondents coded as positive for major depressive disorder or dysthymic disorder in past year or prior to the past year; (2) no: respondents coded as negative for major depressive disorder and dysthymic disorder in past year and prior to the past year.
Incident CVD
We computed a composite incident CVD variable comprised of new-onset arteriosclerosis, angina, or MI from the NESARC Medical Conditions and Practices questionnaire administered at Wave 2. In Part A of this questionnaire, respondents were asked, “In the last 12 months, did you have: (1) hardening of the arteries or arteriosclerosis? (2) chest pain or angina pectoris? (3) a heart attack or myocardial infarction?” If the answer to Part A was “yes,” in Part B respondents were asked, “Did a doctor or other health professional tell you that you had (name of condition)?” We coded respondents as positive for incident CVD if they answered “yes” to Parts A and B for at least one CVD question, and we coded respondents as negative if they answered “no” to all three Part A questions. Those who were coded as “unknown” for Part A or B for one or more questions and who did not answer “yes” to Part A and B for at least one question were coded as missing for incident CVD and were excluded. The same coding scheme within each cardiovascular condition was used to compute separate variables for incident arteriosclerosis, angina, and MI. We also applied the same coding scheme to the identical Wave 1 CVD questions to compute a baseline CVD variable. We only included respondents coded negative for baseline CVD in our sample, as our focus is new-onset CVD. Epidemiologic surveys often assess CVD by self-report of physician diagnoses, and agreement between self-reported and medical record-ascertained clinical CVD has been found to be acceptable to good (38–43).
Covariates
Demographic covariates were age (years), sex (0 = male, 1 = female), race/ethnicity, and education level, and CVD risk factor covariates were hypertension, hypercholesterolemia, diabetes, tobacco use, and body mass index (BMI). With the exception of hypercholesterolemia and diabetes (assessed at Wave 2 only), all covariates were assessed at Wave 1. Due to the low percentage of respondents in the American Indian/Alaskan Native and the Asian/Native Hawaiian categories, we merged these categories with the Other category, resulting in a four-level race/ethnicity variable (non-Hispanic White, non-Hispanic Black, Hispanic or Latino, other). Next, we dummy coded race/ethnicity by creating three variables with non-Hispanic White as the reference category. We computed a four-level education variable (less than high school, high school or equivalent, some college or Associate’s degree, Bachelor’s degree or higher) using responses to the question, “Highest grade or year of school completed?” We then dummy coded education level by creating three variables with less than high school as the reference category. We coded respondents as positive for hypertension, hypercholesterolemia, and diabetes, respectively, if they answered “yes” to “In the past 12 months, have you had: (1) high blood pressure or hypertension? (2) high cholesterol? (3) diabetes or sugar diabetes?” and “yes” to “Did a doctor or other health professional tell you that you had (name of condition)?” We coded respondents as negative for each condition if they answered “no” to the first question. Those coded by NESARC personnel as “unknown” for either question were coded as missing for that condition and were excluded. We recoded NESARC’s tobacco use variable from a three-level variable (current user, former user, lifetime nonuser) to a dichotomous variable (0 = not a current user, 1 = current user). BMI (kg/m2) was calculated from self-reported height (in feet and inches) and weight (in pounds).
Data analysis
To test our first hypothesis, we constructed a logistic regression model examining the association between number of past-year stressful life events and incident CVD. Covariates were age, sex, race/ethnicity (3 dummy variables), education level (3 dummy variables), hypertension, hypercholesterolemia, diabetes, tobacco use, and BMI. A parallel set of exploratory models were constructed for incident MI, angina, and arteriosclerosis separately.
To test our second hypothesis, we first computed a stressful life events (z scored) by lifetime depressive disorder cross-product interaction term. We then entered this interaction term, stressful life events and lifetime depressive disorder main effects, and all of the covariates, in a logistic regression model with incident CVD as the dependent variable. Once again, a parallel set of exploratory models were constructed for incident MI, angina, and arteriosclerosis. To probe interactions, we re-ran the models examining associations between number of past-year stressful life events and incident CVD variables after stratifying by lifetime depressive disorder status.
All analyses were conducted with SAS statistical software, version 9.3. Models were adjusted using NESARC sample weights to account for oversampling, probabilities of selection, and nonresponse. Weighted models provide estimates for U.S. civilian noninstitutionalized population based on the 2000 Decennial Census (30).
Results
As can be seen in Figure 2, there was good variability in the number of past-year stressful life events in our final sample, with ~30% reporting zero events and ~3% reporting six or more events. The mean number of past-year events was 1.6. We identified 4,908 (17.2%) cases of lifetime depressive disorder: 3,805 with major depressive disorder only, 226 with dysthymic disorder only, and 877 with both disorders. We also identified 1,069 (3.7%) cases of incident CVD: 252 with arteriosclerosis only, 602 with angina only, 68 with MI only, 52 with arteriosclerosis and angina, 9 with arteriosclerosis and MI, 57 with angina and MI, and 29 with all three outcomes.
Figure 2.
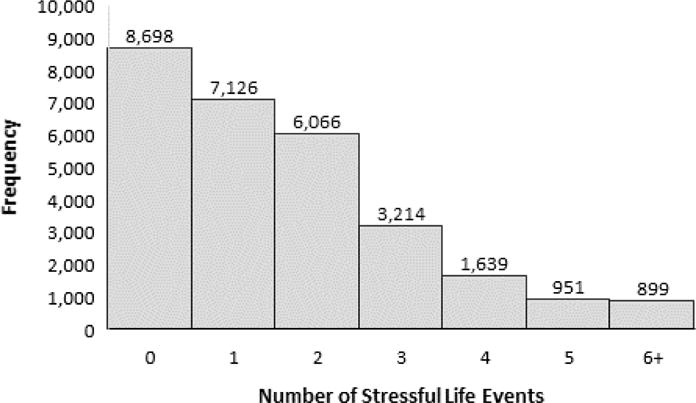
Histogram for the number of past-year stressful life events at Wave 1 (2001–2002) of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC; N = 28,583).
As is shown in Figure 3, the logistic regression model testing our first hypothesis revealed that the number of past-year stressful life events was positively associated with incident CVD (P < 0.001). Specifically, we found that each additional stressful life event was associated with a 15% greater odds of incident CVD. Exploratory logistic regression models examining each CVD type indicated that number of past-year stressful life events was associated with incident arteriosclerosis (8% greater odds per event, P = 0.033) and incident angina (17% greater odds per event, P < 0.001) but not incident MI (P = 0.37).
Figure 3.
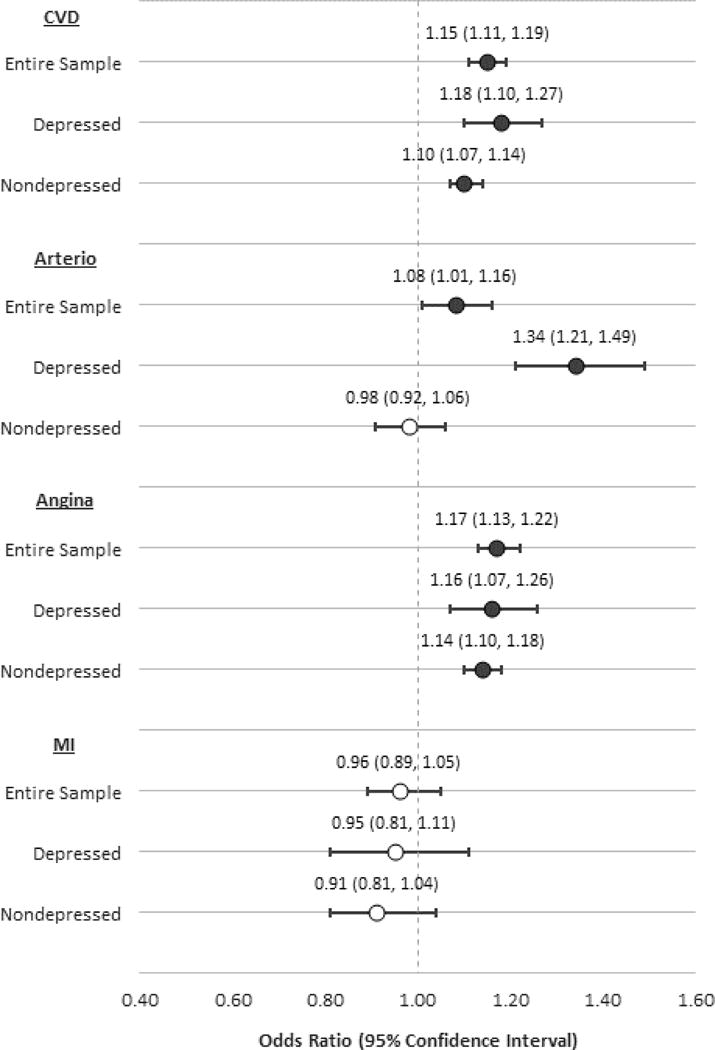
Prospective associations of number of past-year stressful life events with incident cardiovascular disease (CVD), arteriosclerosis (Arterio), angina, and myocardial infarction (MI), in the entire sample (N = 28,583), the depressed subsample (n = 4,908), and the nondepressed subsample (n = 23,675). All models are adjusted for age, sex, race/ethnicity, education level, hypertension, hypercholesterolemia, diabetes, tobacco use, body mass index, and the NESARC sampling design.
The logistic regression model testing our second hypothesis revealed a significant stressful life events by lifetime depressive disorder interaction for incident CVD (P = 0.003). As is shown in Figure 3, models stratified by lifetime depressive disorder status indicated that the association between stressful life events and incident CVD was stronger in depressed versus nondepressed adults (18% versus 10% greater odds per event, both Ps < 0.001). Exploratory logistic regression models also revealed a significant stressful life events by lifetime depressive disorder interaction for incident arteriosclerosis (P < 0.001) but not for incident angina (P = 0.18) or incident MI (P = 0.23). Stratified models (see Figure 3) indicated that stressful life events: had a stronger association with incident arteriosclerosis in depressed (34% greater odds per event, P < 0.001) versus nondepressed (P = 0.69) adults; was similarly associated with incident angina in depressed and nondepressed groups (16% versus 14% greater odds per event, both Ps < 0.001); and was not associated with incident MI in either group (both Ps > 0.19).
Discussion
This examination of prospective NESARC data collected from a large sample representative of the U.S. population supported both our hypotheses. First, we found that number of past-year stressful life events was independently associated of new-onset CVD, as an increase of one stressful life event conferred a 15% greater odds of incident CVD after adjustment for demographic and CVD risk factors. Second, we found that stressful life events had a stronger association with new-onset CVD in adults with, versus without, a lifetime history of a depressive disorder. Specifically, an increase of one stressful life event was associated with an 18% greater odds of incident CVD in depressed adults as compared to only a 10% greater odds in nondepressed adults. Results of exploratory models stratified by CVD type indicate that this interaction effect was driven by incident arteriosclerosis and not incident angina and incident MI (see Figure 3). In total, our findings suggest that a greater number of recent stressful life events elevates the risk of new-onset CVD and that this risk is more pronounced in adults with a history of a depressive disorder.
The present results extend to the U.S. population prior results linking stressful life events to future CVD (9–14). Because the incident CVD outcomes differed across previous studies, we conducted exploratory analyses examining each type of incident CVD separately, which revealed that stressful life events was associated with angina and arteriosclerosis but not MI. This pattern of results is consistent with previous studies findings that stressful life events are associated with angina (9) and stroke (11, 14) but not CAD events, such as MI or CVD death (9–11). The two studies in this literature reporting an association between stressful life events and CAD events used measures that combined number of stressful life events with perceived impact of each event (12, 13). This methodological difference may explain the divergent results, as perceived stress has been more consistently associated with CAD events than stressful life events (1). In addition, those two studies also had the oldest cohorts, with mean ages of 63 (12) and 62 (13) years. In contrast, the present study had a relatively young mean age of 45 years. This may explain our lower incidence of CVD events, which may have compromised our ability to detect associations with the incident MI outcome, in particular.
A greater number of recent stressful life events may elevate the risk of new-onset CVD by promoting atherosclerosis (27). First, recurrent stress can induce sympathetic and HPA axis dysregulation (20, 26), which can result in increased inflammation, endothelial dysfunction, and, ultimately, atherosclerosis (44, 45). Second, chronic exposure to stress may instigate atherogenic behaviors, including tobacco use and alcohol abuse, high fat and carbohydrate consumption, and physical inactivity (46, 47). Further supporting these candidate mechanisms, stressful life events have been cross-sectionally associated with increased endothelial dysfunction (48), and chronic work stress has been prospectively related to progression of subclinical atherosclerosis (49). However, in the current study, which is limited by two waves of data collection, we did not investigate these candidate mechanisms. Therefore, future studies, ideally with three or more waves, are needed to rigorously test these possible pathways. Of note, the atherogenic impact of chronic stress is distinct from the cardiac impact of acute stress, which can trigger coronary events (50, 51). This distinction provides a potential explanation for our results stratified by CVD type – i.e., number of stressful life events may promote the development of arteriosclerosis and corresponding symptoms of angina but may not influence the triggering of acute coronary events.
Although our study is the first to examine depression as a moderator of the stressful life events-incident CVD relationship, our results are consistent with two recent investigations examining the joint influence of depression and perceived stress on CVD events (52, 53). In both studies, the likelihood of CVD events was numerically greater among those with both perceived stress and depressive symptoms than among those with either perceived stress or depressive symptoms alone. An important difference between our study and these recent investigations is that we tested the stressful life events by depression interaction, and thus our results provide preliminary support for the synergistic effect of these factors on incident CVD. The stressful life events-incident CVD relationship may have been more pronounced in adults with a history of a depressive disorder because depressed adults tend to exhibit atherogenic responses to stress (20, 26, 27), including prolonged activation of physiologic stress response systems (15–19) and increased utilization of poor behavioral coping strategies, such as emotional eating and substance use (24, 25). Importantly, while our lifetime depressive disorder variable captured any depressive episode across the lifespan, it is unlikely that these are isolated occurrences. Rather, depression is often a chronic condition due to a high recurrence rate (15-year recurrence rate of 85% in mental health settings and 35% in the general population) (54) and frequent persistence of residual symptoms after remission of a depressive episode (55). Moreover, adults with a lifetime history of depression, but currently in remission, also exhibit altered and potentially atherogenic responses to stress (56). Consequently, adults with a lifetime depressive disorder, whether ongoing or in remission, may be particularly vulnerable to the cardiotoxic effects of stressful life events.
NESARC has methodological strengths that bolster confidence in our findings, such as the longitudinal design, the structured interview assessments of psychiatric disorders, and the large nationally representative sample that provides results generalizable to the U.S. adult population. However, there are limitations that should be considered. First, epidemiologic surveys, including NESARC, often assess medical conditions, including CVD, by self-report of physician diagnoses, which will yield some degree of misclassification. Even so, the majority of literature has observed acceptable to good agreement between self-reported and medical record-ascertained clinical CVD (39–43, 57), lending support to this approach. Second, some incident CVD events were not captured. Fatal events were not captured because the respondents who died between Waves 1 and 2 were excluded from the Wave 2 cohort, and cause of death information is not available. Additionally, some nonfatal events may not have been captured because the Wave 2 questions inquired about CVD diagnoses in the past 12 months only. While these issues likely resulted in some MIs going uncaptured, they are less of a concern for angina and arteriosclerosis because these are chronic conditions and not discrete and/or fatal events. The suboptimal capture of MIs could explain why we did not observe a relationship between stressful life events and incident MI. Of note, our primary composite outcome of incident CVD protects against misclassification, as respondents who suffered nonfatal MIs between Waves 1 and 2, but prior to the past 12 months at Wave 2, may have also been diagnosed with one of the other CVD conditions during follow-up. Third, it is possible that the presence of stressful life events could increase the detection of CVD conditions. Stress has been associated with increased symptom reporting, illness behaviors, and healthcare utilization (58–61), which could lead to higher referral rates for CVD assessments, potentially resulting in CVD diagnoses. Consequently, there is a need for prospective studies examining the association of stressful life events with more direct measures of atherosclerosis, such as carotid intima-media thickness or coronary artery calcification, that are not susceptible to this potential detection issue.
In conclusion, we report that a greater number of recent stressful life events elevates the risk of new-onset CVD in U.S. adults, especially among those with a history of a depressive disorder. Regarding research implications, the present findings underscore the importance of examining the combined influence of psychosocial factors, which have been traditionally examined in isolation (62), on CVD outcomes. They also provide further support for future clinical trials testing whether successful treatment of psychosocial factors lowers CVD risk. Concerning clinical implications, our findings highlight the potential utility of screening for stressful life events and depression in clinical settings where CVD risk is managed. Moreover, they raise the possibility that CVD primary prevention efforts should be initiated earlier and/or intensified in adults reporting a high number of stressful life events, especially in adults with a history of clinical depression.
Highlights.
In a sample representative of the U.S. adult population, we examined whether stressful life events is associated with incident CVD and whether this relationship is stronger in adults with a depression history.
Each additional stressful life event was associated with a 15% increased odds of CVD.
Stressful life events and CVD had a stronger association among adults with versus without a lifetime depressive disorder.
Greater numbers of stressful life events may elevate the risk of new-onset CVD, especially in adults with a history of depression.
Acknowledgments
Source of Funding: NESARC is funded by the National Institute on Alcohol Abuse and Alcoholism with supplemental support from the National Institute on Drug Abuse. A portion of Dr. Stewart’s time was supported by the National Heart, Lung, and Blood Institute under Award Number R01HL122245. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest
None of the remaining authors has any possible conflicts of interest to declare.
References
- 1.Richardson S, Shaffer JA, Falzon L, Krupka D, Davidson KW, Edmondson D. Meta-analysis of perceived stress and its association with incident coronary heart disease. Am J Cardiol. 2012;110(12):1711–6. doi: 10.1016/j.amjcard.2012.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Backé EM, Seidler A, Latza U, Rossnagel K, Schumann B. The role of psychosocial stress at work for the development of cardiovascular diseases: a systematic review. Int Arch Occup Environ Health. 2012;85(1):67–79. doi: 10.1007/s00420-011-0643-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kivimaki M, Kawachi I. Work Stress as a Risk Factor for Cardiovascular Disease. Curr Cardiol Rep. 2015;17(9):630. doi: 10.1007/s11886-015-0630-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Steptoe A, Kivimaki M. Stress and cardiovascular disease: an update on current knowledge. Annu Rev Public Health. 2013;34:337–54. doi: 10.1146/annurev-publhealth-031912-114452. [DOI] [PubMed] [Google Scholar]
- 5.Renzaho AM, Houng B, Oldroyd J, Nicholson JM, D’Esposito F, Oldenburg B. Stressful life events and the onset of chronic diseases among Australian adults: findings from a longitudinal survey. Eur J Public Health. 2014;24(1):57–62. doi: 10.1093/eurpub/ckt007. [DOI] [PubMed] [Google Scholar]
- 6.Engström G, Khan FA, Zia E, et al. Marital dissolution is followed by an increased incidence of stroke. Cerebrovasc Dis. 2004;18(4):318–24. doi: 10.1159/000080770. [DOI] [PubMed] [Google Scholar]
- 7.Kriegbaum M, Christensen U, Lund R, Prescott E, Osler M. Job loss and broken partnerships: do the number of stressful life events influence the risk of ischemic heart disease in men? Ann Epidemiol. 2008;18(10):743–5. doi: 10.1016/j.annepidem.2008.04.010. [DOI] [PubMed] [Google Scholar]
- 8.Lund R, Rod NH, Christensen U. Are negative aspects of social relations predictive of angina pectoris? A 6-year follow-up study of middle-aged Danish women and men. J Epidemiol Community Health. 2012;66(4):359–65. doi: 10.1136/jech.2009.106153. [DOI] [PubMed] [Google Scholar]
- 9.Hollis JF, Connett JE, Stevens VJ, Greenlick MR. Stressful life events, Type A behavior, and the prediction of cardiovascular and total mortality over six years. J Behav Med. 1990;13(3):263. doi: 10.1007/BF00846834. [DOI] [PubMed] [Google Scholar]
- 10.Andersen I, Diderichsen F, Kornerup H, Prescott E, Rod NH. Major life events and the risk of ischaemic heart disease: does accumulation increase the risk? Int J Epidemiol. 2011;40(4):904–13. doi: 10.1093/ije/dyr052. [DOI] [PubMed] [Google Scholar]
- 11.Kornerup H, Osler M, Boysen G, Barefoot J, Schnohr P, Prescott E. Major life events increase the risk of stroke but not of myocardial infarction: results from the Copenhagen City Heart Study. Eur J Cardiovasc Prev Rehabil. 2010;17(1):113–8. doi: 10.1097/HJR.0b013e3283359c18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kershaw KN, Brenes GA, Charles LE, et al. Associations of stressful life events and social strain with incident cardiovascular disease in the Women’s Health Initiative. J Am Heart Assoc. 2014;3(3):e000687. doi: 10.1161/JAHA.113.000687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kershaw KN, Diez Roux AV, Bertoni A, Carnethon MR, Everson-Rose SA, Liu K. Associations of chronic individual-level and neighbourhood-level stressors with incident coronary heart disease: the Multi-Ethnic Study of Atherosclerosis. J Epidemiol Community Health. 2015;69(2):136–41. doi: 10.1136/jech-2014-204217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Everson-Rose SA, Roetker NS, Lutsey PL, et al. Chronic stress, depressive symptoms, anger, hostility, and risk of stroke and transient ischemic attack in the multi-ethnic study of atherosclerosis. Stroke. 2014;45(8):2318–23. doi: 10.1161/STROKEAHA.114.004815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gold SM, Zakowski SG, Valdimarsdottir HB, Bovbjerg DH. Higher Beck depression scores predict delayed epinephrine recovery after acute psychological stress independent of baseline levels of stress and mood. Biol Psychol. 2004;67(3):261–73. doi: 10.1016/j.biopsycho.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 16.Burke HM, Davis MC, Otte C, Mohr DC. Depression and cortisol responses to psychological stress: a meta-analysis. Psychoneuroendocrinology. 2005;30(9):846–56. doi: 10.1016/j.psyneuen.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 17.Salomon K, Clift A, Karlsdottir M, Rottenberg J. Major depressive disorder is associated with attenuated cardiovascular reactivity and impaired recovery among those free of cardiovascular disease. Health Psychol. 2009;28(2):157–65. doi: 10.1037/a0013001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ehrenthal JC, Herrmann-Lingen C, Fey M, Schauenburg H. Altered cardiovascular adaptability in depressed patients without heart disease. World J Biol Psychiatry. 2010;11(3):586–93. doi: 10.3109/15622970903397714. [DOI] [PubMed] [Google Scholar]
- 19.Miller GE, Rohleder N, Stetler C, Kirschbaum C. Clinical depression and regulation of the inflammatory response during acute stress. Psychosom Med. 2005;67(5):679–87. doi: 10.1097/01.psy.0000174172.82428.ce. [DOI] [PubMed] [Google Scholar]
- 20.McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338(3):171–9. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 21.Ottaviani C, Shahabi L, Tarvainen M, Cook I, Abrams M, Shapiro D. Cognitive, behavioral, and autonomic correlates of mind wandering and perseverative cognition in major depression. Front Neurosci. 2014;8:433. doi: 10.3389/fnins.2014.00433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clin Psychol Rev. 2010;30(2):217–37. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 23.Brosschot JF, Gerin W, Thayer JF. The perseverative cognition hypothesis: a review of worry, prolonged stress-related physiological activation, and health. J Psychosom Res. 2006;60(2):113–24. doi: 10.1016/j.jpsychores.2005.06.074. [DOI] [PubMed] [Google Scholar]
- 24.Kuyken W, Brewin CR. Stress and coping in depressed women. Cognit Ther Res. 1994;18(5):403–12. [Google Scholar]
- 25.Maltby J, Day L. Depressive symptoms and religious orientation: Examining the relationship between religiosity and depression within the context of other correlates of depression. Pers Individ Dif. 2000;28(2):383–93. [Google Scholar]
- 26.McEwen BS. Stress, adaptation, and disease: Allostasis and allostatic load. Ann N Y Acad Sci. 1998;840(1):33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- 27.Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99(16):2192–217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 28.Grant BF, Stinson FS, Hasin DS, et al. Prevalence, correlates, and comorbidity of bipolar I disorder and axis I and II disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2005;66(10):1205–15. doi: 10.4088/jcp.v66n1001. [DOI] [PubMed] [Google Scholar]
- 29.Grant BF, Goldstein RB, Chou SP, et al. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol Psychiatry. 2009;14(11):1051–66. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hasin DS, Grant BF. The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Waves 1 and 2: review and summary of findings. Soc Psychiatry Psychiatr Epidemiol. 2015;50(11):1609–40. doi: 10.1007/s00127-015-1088-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brugha T, Bebbington P, Tennant C, Hurry J. The List of Threatening Experiences: a subset of 12 life event categories with considerable long-term contextual threat. Psychol Med. 1985;15(01):189–94. doi: 10.1017/s003329170002105x. [DOI] [PubMed] [Google Scholar]
- 32.Holmes TH, Rahe RH. The social readjustment rating scale. J Psychosom Res. 1967;11(2):213–8. doi: 10.1016/0022-3999(67)90010-4. [DOI] [PubMed] [Google Scholar]
- 33.Dawson DA, Grant BF, Ruan WJ. The association between stress and drinking: modifying effects of gender and vulnerability. Alcohol and alcoholism. 2005;40(5):453–60. doi: 10.1093/alcalc/agh176. [DOI] [PubMed] [Google Scholar]
- 34.Turner RJ, Wheaton B. Checklist measurement of stressful life events. In: Cohen S, Kessler RC, Gordon LU, editors. Measuring stress: A guide for health and social scientists. New York, NY: Oxford University Press; 1995. pp. 29–58. [Google Scholar]
- 35.Slopen N, Williams DR, Fitzmaurice GM, Gilman SE. Sex, stressful life events, and adult onset depression and alcohol dependence: are men and women equally vulnerable? Soc Sci Med. 2011;73(4):615–22. doi: 10.1016/j.socscimed.2011.06.022. [DOI] [PubMed] [Google Scholar]
- 36.Ruan WJ, Goldstein RB, Chou SP, et al. The alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend. 2008;92(1–3):27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71(1):7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- 38.Barr E, Tonkin A, Welborn T, Shaw J. Validity of self-reported cardiovascular disease events in comparison to medical record adjudication and a statewide hospital morbidity database: the AusDiab study. Intern Med J. 2009;39(1):49–53. doi: 10.1111/j.1445-5994.2008.01864.x. [DOI] [PubMed] [Google Scholar]
- 39.Bergmann MM, Byers T, Freedman DS, Mokdad A. Validity of self-reported diagnoses leading to hospitalization: a comparison of self-reports with hospital records in a prospective study of American adults. Am J Epidemiol. 1998;147(10):969–77. doi: 10.1093/oxfordjournals.aje.a009387. [DOI] [PubMed] [Google Scholar]
- 40.Heckbert SR, Kooperberg C, Safford MM, et al. Comparison of Self-Report, Hospital Discharge Codes, and Adjudication of Cardiovascular Events in the Women’s Health Initiative. Am J Epidemiol. 2004;160(12):1152–8. doi: 10.1093/aje/kwh314. [DOI] [PubMed] [Google Scholar]
- 41.Lampe FC, Walker M, Lennon LT, Peter HW, Shah E. Validity of a self-reported history of doctor-diagnosed angina. J Clin Epidemiol. 1999;51(1):73–81. doi: 10.1016/s0895-4356(98)00146-2. [DOI] [PubMed] [Google Scholar]
- 42.Machon M, Arriola L, Larranaga N, et al. Validity of self-reported prevalent cases of stroke and acute myocardial infarction in the Spanish cohort of the EPIC study. J Epidemiol Community Health. 2013;67(1):71–5. doi: 10.1136/jech-2011-200104. [DOI] [PubMed] [Google Scholar]
- 43.Okura Y, Urban LH, Mahoney DW, Jacobsen SJ, Rodeheffer RJ. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol. 2004;57(10):1096–103. doi: 10.1016/j.jclinepi.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 44.Pickering TG. Stress, inflammation, and hypertension. J Clin Hypertens. 2007;9(7):567–71. doi: 10.1111/j.1524-6175.2007.06301.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gu HF, Tang CK, Yang YZ. Psychological stress, immune response, and atherosclerosis. Atherosclerosis. 2012;223(1):69–77. doi: 10.1016/j.atherosclerosis.2012.01.021. [DOI] [PubMed] [Google Scholar]
- 46.Dallman MF, Pecoraro N, Akana SF, et al. Chronic stress and obesity: a new view of “comfort food”. Proc Natl Acad Sci U S A. 2003;100(20):11696–701. doi: 10.1073/pnas.1934666100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jackson JS, Knight KM. Race and self-regulatory health behaviors: the role of the stress response and the HPA axis in physical and mental health disparities. In: Schaie KW, Cartensen LL, editors. Social structures, aging, and self-regulation in the elderly. New York, NY: Springer; 2006. pp. 189–207. [Google Scholar]
- 48.Kershaw KN, Lane-Cordova AD, Carnethon MR, Tindle HA, Liu K. Chronic Stress and Endothelial Dysfunction: The Multi-Ethnic Study of Atherosclerosis (MESA) Am J Hypertens. 2017;30(1):75–80. doi: 10.1093/ajh/hpw103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wilson MD, Conroy LM, Dorevitch S. Occupational stress and subclinical atherosclerosis: a systematic review. Int J Occup Environ Health. 2014;20(4):271–80. doi: 10.1179/2049396714Y.0000000076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kop WJ. Chronic and acute psychological risk factors for clinical manifestations of coronary artery disease. Psychosom Med. 1999;61(4):476–87. doi: 10.1097/00006842-199907000-00012. [DOI] [PubMed] [Google Scholar]
- 51.Schwartz BG, French WJ, Mayeda GS, Burstein S, Economides C, Bhandari AK, et al. Emotional stressors trigger cardiovascular events. Int J Clin Pract. 2012;66(7):631–9. doi: 10.1111/j.1742-1241.2012.02920.x. [DOI] [PubMed] [Google Scholar]
- 52.Cummings DM, Kirian K, Howard G, et al. Consequences of Comorbidity of Elevated Stress and/or Depressive Symptoms and Incident Cardiovascular Outcomes in Diabetes: Results From the REasons for Geographic And Racial Differences in Stroke (REGARDS) Study. Diabetes Care. 2016;39(1):101–9. doi: 10.2337/dc15-1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sumner JA, Khodneva Y, Muntner P, et al. Effects of Concurrent Depressive Symptoms and Perceived Stress on Cardiovascular Risk in Low- and High-Income Participants: Findings From the Reasons for Geographical and Racial Differences in Stroke (REGARDS) Study. J Am Heart Assoc. 2016;5(10) doi: 10.1161/JAHA.116.003930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hardeveld F, Spijker J, De Graaf R, Nolen W, Beekman A. Prevalence and predictors of recurrence of major depressive disorder in the adult population. Acta Psychiatrica Scandinavica. 2010;122(3):184–91. doi: 10.1111/j.1600-0447.2009.01519.x. [DOI] [PubMed] [Google Scholar]
- 55.Nierenberg A, Husain M, Trivedi M, et al. Residual symptoms after remission of major depressive disorder with citalopram and risk of relapse: a STAR* D report. Psychol Med. 2010;40(01):41–50. doi: 10.1017/S0033291709006011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Höhne N, Poidinger M, Merz F, et al. Increased HPA axis response to psychosocial stress in remitted depression: the influence of coping style. Biol Psychol. 2014;103:267–75. doi: 10.1016/j.biopsycho.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 57.Barr EL, Tonkin AM, Welborn TA, Shaw JE. Validity of self-reported cardiovascular disease events in comparison to medical record adjudication and a statewide hospital morbidity database: the AusDiab study. Intern Med J. 2009;39(1):49–53. doi: 10.1111/j.1445-5994.2008.01864.x. [DOI] [PubMed] [Google Scholar]
- 58.Macleod J, Smith GD, Heslop P, Metcalfe C, Carroll D, Hart C. Psychological stress and cardiovascular disease: empirical demonstration of bias in a prospective observational study of Scottish men. BMJ. 2002;324(7348):1247–51. doi: 10.1136/bmj.324.7348.1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mechanic D. Social psychologic factors affecting the presentation of bodily complaints. N Engl J Med. 1972;286:1132–9. doi: 10.1056/NEJM197205252862105. [DOI] [PubMed] [Google Scholar]
- 60.Mechanic D, Volkart EH. Stress, illness behavior, and the sick role. Am Sociol Rev. 1961;26:51–8. [Google Scholar]
- 61.Pilisuk M, Boylan R, Acredolo C. Social support, life stress, and subsequent medical care utilization. Health Psychol. 1987;6(4):273. doi: 10.1037//0278-6133.6.4.273. [DOI] [PubMed] [Google Scholar]
- 62.Suls J, Bunde J. Anger, anxiety, and depression as risk factors for cardiovascular disease: the problems and implications of overlapping affective dispositions. Psychol Bull. 2005;131(2):260–300. doi: 10.1037/0033-2909.131.2.260. [DOI] [PubMed] [Google Scholar]


