Abstract
Objectives
This critical review aimed to identify, consolidate and evaluate the quality of Willingness to Pay (WTP) studies applied to clinical contexts in the field of dentistry.
Methods
PubMed and Web of Science databases were systematically searched for relevant publications. Screening and data extraction was then performed. Primary literature in English-language were included to assess the WTP for oral health interventions, when the valuations were applied to a clinical measure. Twenty-six publications met the inclusion criteria.
Results
WTP was elicited mainly via face-to-face interviews (13 publications) and questionnaires (12 publications). The majority (24) of publications selected an out-of-pocket payment vehicle. Eleven publications adopted a bidding method, nine publications adopted an open-ended format, and the remaining six studies adopted a payment card or choice method. Pre-testing was reported in only nine publications, and few studies accounted for starting point bias. Eight of 11 publications found that higher incomes were associated with higher WTP values. The female gender, a younger age and higher education levels were associated with a higher WTP in select studies.
Conclusions
Only a small minority of the studies used strategies to avoid well documented biases related to WTP elicitation. Cost versus benefit of many clinical scenarios remain uninvestigated.
Clinical significance
WTP studies in dentistry may benefit from pre-testing and the inclusion of a script to minimise hypothetical bias. They may also be better conducted face-to-face and via a shuffled payment card method. Income levels, and potentially education levels, gender and age, should be assessed for their influence on WTP values.
Introduction
Expenditure on dental care is substantial globally [1–3]. This expense is financed through insurance, government funding, out-of-pocket payments by individuals or a combination of these [4]. Given that financial resources are limited, it is important that they are used efficiently. Economic evaluation can help ensure efficiency especially when prioritizing the care delivered with the available resources. In order to undertake economic evaluations, it is necessary to obtain an accurate and reliable measurement of the value placed on dental procedures.
Many studies have attempted to determine valuations in healthcare [5, 6]. These valuations include willingness to pay (WTP), Health Years Equivalent (HYE), Quality-adjusted tooth years (QATY) and Quality-adjusted life years (QALY). As there is a lack of preference based measures (such as QALY) [7], WTP remains an important measure of valuation that is applicable and available to dentistry that allows for economic evaluations that enable meaningful comparisons across various healthcare provision scenarios.
Willingness to pay (WTP) is a popular approach to the valuation of healthcare benefits [6]. Willingness to pay refers to the maximum amount in monetary terms that an individual would be willing to sacrifice in order to obtain the benefits of a program [8]. It may be elicited through a revealed preference approach, i.e. observed consumer choices, or through an expressed or stated preference approach – the contingent valuation method (CVM) [9]. CVM allows for estimation of individuals’ WTP even in the absence of actual markets, such as in the valuation of public goods or new product developments. In principle, WTP allows us to capture the full economic value including non-use and passive benefits, and opportunity costs of an intervention; reflects individuals’ treatment preferences among potential alternative uses of monetary resources, and permits comparisons across interventions with entirely different outcome natures [10]. WTP also allows for a direct cost-benefit analysis (CBA). When the costs and benefits of each intervention are known and correct decision making framework is applied, a thorough CBA aids resource allocation with maximisation of benefits out of a fixed budget [11]. WTP may also be used in pricing and demand forecasts for individual healthcare services, or to determine the viability of healthcare programmes when used in conjunction with cost-effectiveness and cost-utility analyses (e.g. WTP per QALY) [12].
Despite its strengths, WTP has its share of criticisms [13]. WTP elicitations are susceptible to biases, such as hypothetical bias, compliance bias, strategic bias, warm glow effect, yea saying bias, starting point bias and range bias. These are explained in detail elsewhere [14]. Carson (2012) elaborated on the need for well-designed contingent valuation studies control for biases and yield more reliable measurements [15]. Content validity in WTP studies, or the provision of adequate information to ensure respondents understand correctly what is asked of them, may be improved by providing a detailed description of the intervention, the objective of the WTP question, and pre-testing. Piloting of the survey ensures that respondents understand the benefits of the intervention, and give their true WTP value rather than a fair price of the intervention (incentive compatibility) [16]. Other study parameters include an appropriate sample size and demographic distribution, acceptability to respondents, internal consistency, and reproducibility. WTP measures have been shown to have acceptable temporal stability over a short term and variable longer term stability [17, 18]. The sampling frame also requires consideration, as patients may have more familiarity with procedures, while the general population may provide a less biased perspective for the overall population. [19, 20].
The WTP elicitation format may also influence the reliability of results. Contingent valuation can be carried out in a few ways, namely: (1) Open-ended format (OE), (2) Bidding game format (BG), (3) Payment card format (PC), (4) Dichotomous-choice format (DC) and (5) Double-bounded dichotomous-choice format (DBDC) [21]. OE valuations are unrealistic and predisposed to strategic bias [22], while DC methods are susceptible to “yea-saying” bias [23], and have not been widely used in healthcare as they require a large and costly sample size [24]. Alternatively, WTP can be determined using conjoint analysis as part of a Discrete Choice Experiment. The modes of WTP elicitation include survey questionnaires – mailed, online, paper copy, phone interviews, and face-to-face interviews. Besides critiquing elicitation methods such as open ended questions, Arrow et al. (1993) recommended the adoption of in-person interviews by experienced professional interviewers to motivate respondents to pay close attention to the details of WTP scenarios [22].
Studies pertaining to oral healthcare involve the elicitation of WTP values for periodontal treatments, orthodontic appliances, prosthodontic tooth replacements, oral medicine and oral surgery interventions, preventive care, as well as novel dental products and services. While the scope and number of dental-related WTP studies has expanded in recent years, there is a lack of studies that summarise and examine the quality of these WTP studies. This review therefore seeks to identify, consolidate, and evaluate the existing literature on Willingness to Pay applied to clinical contexts in the field of dentistry.
Methodology
This study reports a critical review that utilized a systematic search. It sought to identify and evaluate publications that assessed willingness to pay for oral health interventions in a clinical context.
Inclusion and Exclusion criteria
Only original, English-language publications that included a primary study to assess WTP for oral health interventions applied in a clinical context were selected. Here the clinical context was operationalized as the administration of oral healthcare by oral health professionals in a healthcare facility. Reviews, including systematic and literature reviews, were examined to identify additional clinical publications and references, but were not included in the list of publications selected. Case reports, case studies, poster presentations, conference presentations, letters, news and editorials were similarly excluded. Studies that relied on simulations with hypothetical WTP values, without a direct WTP elicitation from respondents, were also excluded.
Various methods of measuring WTP were included in this review. They included, but were not limited to, direct measurements of WTP, conjoint analyses, discrete choice experiments, and contingent valuation. Valuations of benefit, in the form of WTP, made by direct recipients and/or payors (e.g. parents of school children) of oral health interventions were accepted. WTP elicitation from healthcare providers was also considered for inclusion. The payment vehicles included payment out-of-pocket, insurance payments and contributions to public tax-funded programmes.
Search Strategy
An initial search was conducted on 2nd June 2016 to identify the relevant keywords. Searches for relevant publications were carried out using PubMed (MEDLINE) and Web of Science (WOS) databases. The PubMed database was searched using a combination of Medical Subject Headings (MeSH) terms, and general search terms/keywords in “All Fields” (non-field restricted search). The search strategy used the following search query: “Willingness to pay” OR WTP OR “Cost benefit analysis” (MeSH) OR “Time trade off” OR TTO OR “Discrete choice experiment” OR DCE OR “Conjoint analysis” AND “Dentistry”(MeSH) OR “Dent*”. Web of Science was searched using “All Databases”. The search query used was: ("Willingness to pay” OR WTP OR “Cost benefit analysis” OR “Time trade off” OR TTO OR “Discrete choice experiment” OR DCE OR “Conjoint analysis”) AND TOPIC:(Dent*). Time span was set to include “All years”, and the search language was English.
Management of records
The search results from each database were downloaded and imported in to EndNote X7.3.1. Duplicate records were removed, and relevant publications were retrieved. The selection of publications for inclusion was conducted first by title and abstract screening. If any publication did not have an abstract, the full article was used for screening. Titles and abstracts were reviewed by ST. Publications that met all the inclusion criteria were selected. For publications that met some, but not all the inclusion criteria, or were thought to be of questionable relevance, a second reviewer (RN) conducted an independent review and a consensus was sought. Full texts were retrieved for the selected publications and independently reviewed by the reviewers for inclusion. A final decision of the inclusion or non-inclusion of the publication was finalised thereafter, and the reasons for exclusion were recorded.
Selection of studies
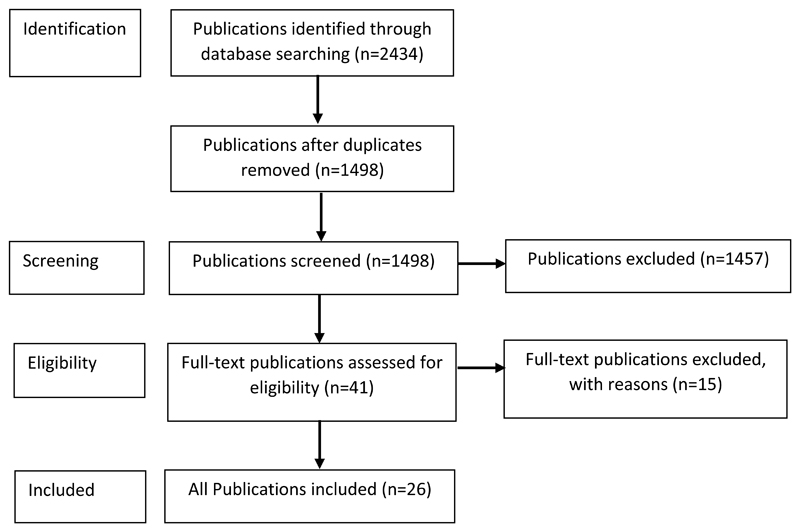
A total of 2434 publications were identified, out of which 1246 were from PubMed, and 1188 from WOS. After removing duplicates, 1498 publications remained. Forty one publications were selected after the title and abstract screening. Nineteen publications were short-listed for a second review by RN. The full-text for these publications were extracted, and examined. ST and RN came to a consensus on the exclusion of 15 of the 19 publications and including the rest of the publications (Fig 1). Three publications [25–27] appeared to have used the same data set of WTP values. The publications originated from a survey of 205 parents of primary school children in Thailand. As two of the publications analysed different aspects of WTP – the influence of dental setting and treatment modality, a sub-column was included to present the separate result findings in Table 1. The third publication [25] was excluded. Two publications in Canada also appeared to interview a common study sample of 196 respondents from the general population. As one of the publications additionally compared the WTP results with that of 97 periodontal recall patients [28], the other publication was excluded [29]. In order to account for the various publications from one dataset, a distinction between the use of publications versus studies is maintained in this review. Here, the study refers to the overall research work that resulted in a dataset, and a study might result in multiple publications.
Figure 1.
Flow of studies through the inclusion process.
Table 1.
Description of key methodologies and findings reported in studies that used a bidding methodology
| Publication Title | Author (Year of Publication) Location | Sample Group (Sample Size) | Methodology: Pre-testing, Reliability | Mode of WTP elicitation | Results (key findings on WTP) |
|---|---|---|---|---|---|
| Different Dental Care Setting: Does Income Matter | Tianviwat, S., Chongsuvivat wong, V. et al (2008a) Thailand | Parents (205) | Content validity and understandability of WTP questionnaire tested beforehand (10 dentists and 10 non-clinical stuff) Pilot study (27 parents) Construct validity tested |
Face-to-face interview | Multilevel linear regression analyses reported higher WTP among higher income subjects for sealants in permanent teeth, fillings in permanent teeth, and extractions in primary teeth. However, the difference in WTP between the income groups was less for services provided in the mobile setting than for those provided in the hospital setting. |
| Prevention versus cure: Measuring parental preferences for sealants and fillings as treatment for childhood caries in Southern Thailand | Tianviwat, S., Chongsuvivat wong, V. et al (2008b) Thailand | Multilevel linear modelling reported that mean WTP values in Thai Baht for sealants (Unadjusted Mean(SE)=225.3(188.2)) and fillings (Unadjusted Mean(SE)=225.6(203.0)) were not significantly different (p=0.97). | |||
| Factors affecting patient valuation of caries prevention: Using and validating the willingness to pay method | Vernazza, C.R., Wildman, J.R. et al (2015) UK, Germany | Patients (112) | Questionnaire piloted, minor changes to wording and layout made | Questionnaire | Mean WTP for the coating was £96.41 (SD=60.61). Based on linear regression analysis, no demographic or dental history factors were significantly associated with WTP. |
| Factors affecting the willingness to pay for implants: A study of patients in Riyadh, Saudi Arabia | Al Garni, B., Pani, S.C. et al (2012) Saudi Arabia | Patients (100) | - | Face-to-face interview | 67% of respondents said they would be willing to pay the median price for the placement of an implant. Logistic regression analyses found that the WTP amount increased proportionately with the family income. A higher mean WTP was found for private clinics compared to government dental clinics (B=1.073; p=0.03). |
| Patient evaluation of a Novel Non-Injectable Gel | van Steenberghe, D., Bercy, P. et al (2004) Finland | Patients (157) | Appropriateness of questions and scales pre-tested in pilot study (258 subjects) Pre-testing to ensure wording of questions and response options were easily understood and interpreted (10 Dutch speaking and 10 French speaking subjects) |
Questionnaire (Electronic) | 70% of patients preferred anesthetic gel, while 22% of patients preferred injection anesthesia. A conservative estimate of median WTP was $10. |
| Perspectives towards Oral Mucositis prevention from parents and health care professionals in pediatric cancer | Ethier, M. C., Regier, D.A. et al (2012) Canada | Parents (82), Health care professionals (HCP) (60) | - | Face-to-face interview | Interval regression analyses found no statistically significant differences in the WTP of parents and health care professionals (HCPs) to prevent severe mucositis (Average median WTP=CAN$5,499 vs. CAN$5,180; p=0.81), although both groups were willing to pay large amounts of money to prevent one episode of severe mucositis. HCPs were however, willing to pay significantly less than parents to prevent mild mucositis (β(SE)=-0.69(0.21); p=0.03). |
| Prosthetic restoration in the single-tooth gap: patient preference and analysis of the WTP index | Augusti, D., Augusti, G. et al (2013) Italy | Patients (107) | - | Face-to-face interview | WTP median values for implant-supported crowns (ISC) were €3000 and €2500 in the anterior and posterior areas, respectively. Linear regression analyses reported that high oral care was associated with a higher WTP for the estimation of both anterior (B(95%CI)= 831.1(392.3-1269.9); p<0.001), and posterior areas (B(95% CI)= 841.1(433.2-1249.1); p<0.001). |
| Putting Your Money Where Your Mouth is: Willingness to Pay for Dental Gel | Matthews, D., Rocchi, A. et al (2002) Canada | Patients (97 -periodont al recall, 196 -general population) | Content of the decision aid was tested by 3 expert panels. Participants were questioned about their perception of the tool; its length, ease of use, interest level and comprehension of the clinical information | Questionnaire (Electronic) | Median WTP for dental gel was Can$20.00 (mean=Can$22.56) per visit for the general population, and Can$10.00 (mean=Can$16.67) for the recall population. The median WTP for monthly insurance premium for dental gel was Can$2.00 per month for both groups. Logistic regression showed that anxiety about future needles was associated with higher user-based WTP (p= 0.02), while concern about dental pain (p= 0.003) and the anxiety about past needles (p=0.04) were significantly associated with insurance-based WTP. |
| The management of an endodontically abscessed tooth: patient health state utility, decision-tree and economic analysis | Balevi, B., & Shepperd, S. (2007) Canada | Teachers (40) | - | Face-to-face interview | The mean willingness-to-pay (Can$) for the restoration of a maxillary central incisor with a conventional crown, single tooth implant, conventional dental bridge and removable partial denture was 1782.05, 1871.79, 1605.13 and 1351.28 respectively. No statistical significance was found between willingness-to-pay utilities for the fixed restorative treatment and RPD options for molars and incisors based on one-way ANOVA. A weak positive correlation was noted between the standard gamble and willingness-to-pay utility for maxillary central incisors (Pearson's r=0.217; p=0.006), and mandibular 1st molars (Pearson's r=0.196; p=0.01). |
| Willingness to pay for implant therapy: a study of patient preference | Leung, K. C., & McGrath, C. P. (2010) Hong Kong | Patients (51) | - | Face-to-face interview | Mean WTP amounts for anterior and posterior tooth replacement were HK$11,000 and HK$10,000 respectively. No statistical difference was found between the two using the Wilcoxon”s signed rank test. Linear regression models found a lower WTP for a posterior missing tooth was associated with the presence of missing teeth (B(SE)=-6686.9(1813.2); p=0.001). |
| Willingness to pay for periodontal therapy: Development and testing of an instrument | Matthews, D.C., Birch, S. et al (1999) Canada | Patients (24), Faculty (18) | Content and face validity assessed by 4 periodontists, 2 prosthodontists, and 2 general dentists Construct validity tested Test-retest reliability, repeat questionnaire after 14-23 days |
Face-to-face interview | Subjects were willing to pay more for coverage for themselves than for others. Periodontal surgery was the preferred treatment for moderate to advanced periodontal disease, and was preferred over other choices (i.e. a higher WTP) for all income groups. Based on ANOVA, WTP was reported to be positively related to income level. |
Out of the other 13 publications excluded, one publication was not available in English [30]. We were unable to locate the full text for two publications [31, 32]. Two publications were meeting abstracts [33, 34] rather than published studies, while another two publications used conjoint analyses that did not include WTP measurements [35, 36]. Three publications did not measure WTP directly, but instead ran cost-effectiveness analyses at various hypothetical WTP levels [37–39]. A publication on the WTP for community water fluoridation [40] and another for toothbrushes [41], were excluded as they were interventions that were aimed at a community or group rather than individual clinical interventions. Another publication that measured WTP in terms of ‘desired cost’ for dental check-ups instead of the maximum price that respondents would pay was also excluded [42]. Thus a total of 26 publications were included in the final selection.
Reporting of results
Results were presented in tables, with author(s), year of publication, and major findings listed. The publications were grouped according to their contingent valuation method, and the presence and mode of pre-testing, and mode of WTP elicitation were extracted and described. The effect of potential factors influencing WTP values were also summarized from multivariate analyses.
Results
The 26 included publications were published between 1999 and 2015. Most studies were conducted in Canada (six publications), and the United Kingdom (four publications). The total sample size of the studies ranged from 36 to 990. Four publications assessed preventive interventions [43–46], another four were related to implants [47–50], three were related to orthodontics [51–53], and the remaining assessed clinical interventions in other topic areas.
Twelve publications used written or electronic questionnaires to elicit WTP. Thirteen publications assessed WTP using face-to-face interviews, whereas one publication used a telephone interview. Eight of the 26 publications elicited proxy WTP values. Four of these publications elicited the WTP from parents for interventions pertaining to their children [26, 27, 46, 54]. Two publications interviewed respondents for their WTP both for themselves and their children [51, 52], one publication elicited WTP for respondents themselves and their “immediate family and co-workers” [4], and two publications elicited WTP from healthcare providers, in addition to respondents [4, 54]. Another publication elicited WTP for a one-off donation for a public dental check-up programme for children [43]. The remaining publications elicited the WTP for interventions solely for the respondants themselves. In five of the 26 publications, respondents were recruited from existing randomized controlled trials. WTP was collected during treatment in one of the studies [46], after treatment in three of the studies [55–57], and both before and after treatment in the remaining study [58]. As for payment scenarios, a majority of the publications selected an out-of-pocket payment vehicle, with the exception of three publications that additionally elicited WTP either in terms of total premium [28, 47] or the additional premium for insurance [59], and one publication that additionally elicited WTP in terms of tax contribution for a public healthcare program [47]. Two studies elicited WTP solely in terms of additional insurance premium [4, 57]. Probability-based sampling was reported in seven publications [26–28, 44, 45, 59, 60], and convenience sampling was acknowledged in five publications [4, 47, 48, 50, 53]. Sampling methods were briefly described with limited details in the rest of the studies.
Pre-testing was reported in nine publications. This includes discussions with specialists to assess content validity [4, 26–28, 47], and pilot testing with a sample group to ensure the comprehensibility and face validity of the survey [26–28, 44, 45, 47, 57, 61], and the construct validity of decision aids [26, 27]. Follow-up questions were asked in three publications when zero values were given during WTP elicitation [44, 57, 62]. Responses were classified as “true or protest” depending on the reason selected for the zero value [62]. All “no” responses to the initial bid of $0 were treated as protest responses and excluded from analysis in the study by Ethier, Regier [54].
Patients were asked to consider their ability to pay while reporting their WTP in one study [45], and to answer a separate ability to pay question in two studies [53, 60]. Other studies called for a “realistic” and “budget-constrained response” [62], and emphasized that respondents “have this much less money per month to spend or save” [4], and are to “assume payment” is “from (their) own money” or loan “funds from bank” [47]. On the other hand, one study asked patients to mark out on a line the amount they would be willing to pay for a ‘miracle treatment’ in a hypothetical scenario where they struck $100,000 in lottery [63].
The test-retest reliability of WTP results was examined in three publications. The intraclass coefficient was found to be above 0.7 following a repeat survey at six to eight weeks [53], and 0.78 for a repeat interview after 14-23 days [4]. In the pilot study by Birch et al. [59], the Pearson’s correlation coefficient was found to be 0.96, with no difference in mean WTP values. Intrarater reliability was found to be 0.88 in the study by Rosvall, Fields [51]. In addition to WTP, Esfandiari et al. [56] elicited the willingness to accept value for the retraction of an administered dental intervention.
Eleven publications used a bidding method to elicit WTP from their participants (Table 1). Of these, nine publications reported on publications that used bidding methodology with sequentially increasing or decreasing bids [4, 26, 27, 29, 48, 50, 57, 64, 65]. One publication used a ping-pong method [54], and another one was not described in the article [61]. The starting bid was randomly selected for one of the publications [57], whereas it was a fixed starting point for the others. Among the publications that had fixed starting points, there was a study that had two starting points to examine the possibility of starting point bias [29].
Nine studies used an open-ended format (Table 2). One study allowed patients to consider their willingness to pay at various listed prices prior to the open-ended WTP elicitation [55], while another study required respondents to select an interval of payment amount before indicating their precise WTP amount [45]. Two studies [44, 56] asked participants if they would be willing to pay a given price for the intervention in a yes-no close-ended question prior to the open-ended WTP question.
Table 2.
Description of key methodologies and findings reported in studies that used an open-ended methodology.
| Publication Title | Author (Year of Publication) Location | Sample Group (Sample Size) | Methodology: Pre-testing, Reliability | Mode of WTP elicitation | Results (key findings on WTP) |
|---|---|---|---|---|---|
| Baseline Characteristics and Treatment Preferences of Oral Surgery Patients | Atchison, K. A., Gironda, M.W. et al (2007) USA | Patients (98 - mandibular fracture, 105 - third molar) | - | Questionnaire (form) | Patients receiving treatment for mandibular fractures (Median(SD)=$37.4K(31.2K)) were willing to pay more for a special treatment to restore function for a jaw fracture without scarring or nerve damage than patients scheduled for third molar removals (Median(SD)=$30.6K(28.7K)). |
| Cost effectiveness of personalized plaque control for managing the gingival manifestations of oral lichen planus | Stone, S. J., McCracken, G.I. et al (2013) UK | Patients (39 - intervention group) | - | Questionnaire | All patients stated a positive maximum WTP value (range £65–£1500). |
| Evaluation of three methods assessing the relative value of a dental program | Tuominen, R. (2008) Finland | Medical/Dental Students (120 - medical, 36 - dental) | - | Questionnaire (written) | Respondents were willing to make the highest donations for running the helicopter ambulance service (38.90 euros) and least for the dental check-up programme for 7-year-olds (14.34 euros). An independent sample T-test reported a statistically significant difference (p<0.01). |
| Implant Overdentures for edentulous elders: study of patient preferences | Esfandiari, S., Lund, J.P. et al (2009) Canada | Patients (23 - implant overdenture, 13 - conventional denture) | - | Face-to-face interview | Wilcoxon signed rank test reported that the median supplemental amount above $1200 for another type of denture that the implant group would pay for an implant-supported denture was $1000 (range $100-3800), which was significantly higher (p<0.001) than that for the conventional denture group ($300). 89% of respondents were willing to pay more to receive implant treatment if they could make monthly instalments. |
| The value of caries preventive care among 19-year olds using the contingent valuation method within a cost-benefit approach | Oscarson, N., Lindholm, L. et al (2007) Sweden | Adolescents (30 - high risk group, 52 – control group) | Pilot test interview (5 participants) | Questionnaire | Linear regression models showed that the mean monthly WTP for preventive dental care among those with high caries risk (117.12SEK) was significantly higher than those with low caries risk (90.58SEK) (B(SE)=26.54(12.22); p=0.03). Net social benefit was >0. |
| Willingness and ability of Bulgarian consumers to pay for improved public health care services | Pavlova, M., Groot, W. et al (2004) Bulgaria | General public (990) | Questionnaire tested in pilot study | Face-to-face interview | WATP (Willingness and Ability To Pay) for a dental check-up (Median=2.00BGL; Mean=2.67BGL; SD=2.75) was lower than that for filling/treatment of a tooth (Median=10.00BGL; Mean=11.44BGL; SD= 9.24), extraction of a tooth (Median=10.00BGL; Mean=9.58BGL; SD=8.73), and placement of dental prostheses (Median=15.00, Mean=15.85; SD=15.01). Based on Tobit regression, a higher family budget was associated with a higher WATP for a dental check-up (β(SE)=0.0005(0.000); p<0.05), a filling (β(SE)=0.0005(0.000); p<0.05), an extraction (β(SE)=0.0005(0.000); p<0.05), and the placement of dental prostheses (β(SE)= 0.0004(0.000); p<0.05). Staying in a village rather than in the city was associated with a lower WATP for filling (β(SE)=-0.1057(0.035); p<0.05) and extraction (β(SE)=-0.1320(0.041); p<0.05 |
| Willingness and ability to pay for unexpected dental expenses by Finnish adults | Widström, E. & Seppälä, T. (2012) Finland | General public (704) | - | Questionnaire (postal) | For immediate replacement of a lost filling, 93.2% of respondents were willing to pay the lower price charged in the Public Dental Service and 46.2% were willing to pay the private fee. Logistic regression analysis for willingness to pay the same or a higher price than the replacement of a lost filling would have cost (after reimbursement) in the private sector (80 €) showed that a higher yearly income (EUR 25 to >50k) was positively associated with WTP [25-50k vs <10k] (B(95% CI)=1.254(0.247-2.261); p=0.02); [>50k vs <10k] (B(95% CI)=1.893(0.761-3.025); p=0.001). |
| Willingness to pay for dental fear treatment. Is supplying dental fear treatment socially beneficial? | Halvorsen, B. & Willumsen, T. (2004) Norway | Patients (62) | - | Telephone survey | While only 24% of the patients were willing to pay the actual cost of the treatment before attending, 71% were willing to pay afterwards. Ordinary least squares regression reported that higher incomes, benefits from dental treatment (B=1041; p<0.05), and changes in dental health capital [treated surfaces] (B=165; p<0.01) were significantly associated with WTP for dental/dental fear treatment. |
| Willingness to pay for dentin regeneration in a sample of dentate adults | Birch, S., Sohn, W. et al (2004) USA | General public (611) | Test–retest reliability (40 adults) | Questionnaire (Computer aided home interview, self-administered questionnaire) | At a success rate of 95%, the mean WTP for dentin regeneration was $262.70 (non-insured subjects) and $11.00 per month (insured subjects). For a success rate of 75%, the corresponding values were $210.90 and $9.20 per month. Linear regression analysis showed that while regular dental visit was significantly associated with WTP for dentin regeneration among non-insured subjects (β(SE)=95.2(44.7); p=0.03), individuals’ valuations of treatments involve substantial unexplained variation. |
Six studies were conducted via a payment card or choice method (Table 3). Respondents were asked select their WTP [46], their maximum WTP [51, 53], or incremental WTP [52], from a list of various price options. Only one study was designed for respondents to select either ‘yes’ or ‘no’ to paying for a treatment intervention at multiple different price options [47]. A “shuffled payment card” method was adapted from Smith RD (2006) in the study by Vernazza, Steele [62].
Table 3.
Description of key methodologies and findings reported in studies that used a payment card and choice methodology
| Publication Title | Author (Year of Publication) Location | Sample group (Sample Size) | Methodology: Pre-testing, Reliability | Mode of WTP elicitation | Results (key findings on WTP) |
|---|---|---|---|---|---|
| Are people who still have their natural teeth willing to pay for mandibular two-implant overdentures? | Srivastava, A., Feine, J.S. et al (2014) Canada | General Public (39) | Questionnaire was discussed with two experts in the fields of health economics and prosthodontics for content validity Pretested to assess comprehensibility and the time needed (2 individuals) |
Questionnaire (web-based) | Average WTP out of pocket for implant overdentures was CAD$5419 for a 90% success rate. Respondents were willing to pay an average CAD$169 as one-time payment for private dental insurance, with a 20% chance of becoming edentate. WTP amounts increased with the probability of success of implant overdenture therapy. For an out of pocket payment method (at 90% success rate), Linear regression analysis showed that opting for implants (β=2.01; p= 0.045) was significantly associated with a higher WTP than not opting for implants and a less than university education respectively. |
| Attractiveness, acceptability, and value of orthodontic appliances | Rosvall, M.D., Fields, H.W. et al (2009) USA | General public (for self, child) (50) | 3 image-rating pages shown twice to evaluate intrarater reliability (all respondents) | Questionnaire (computerized) | Adults were willing to pay an additional mean estimate of $629 for lingual orthodontics, and $167 for hybrid self-ligating appliances. |
| Esthetic perception and economic value of orthodontic appliances by lay Brazilian adults | Feu, D., Catharino, F. et al (2012) Brazil | General public (for self, child) (252) | - | Face-to-face interview | The correlation between WTP and aesthetic perception was weak (Rho=0.141; p=0.002). |
| Factors affecting direction and strength of patient preferences in treatment of molar teeth with nonvital pulps | Vernazza, C.R., Steele, J.G. et al (2015) UK | Patients (potential) (503) | - | Face-to-face interview | 53% of the sample wished to save the tooth with a mean WTP of £372.79 (SD=991.46). Under the Heckman’s selection model of WTP, it was found that a high income was associated with a higher WTP than that for middle and low income (B(95%CI)=213.56(59.33-367.80); p=0.007) |
| Putting your money where your mouth is: Parents' valuation of good oral health of their children | Vermaire, J.H., van Exel, N.J.A. et al. (2012) Netherlands | Parents (290) | - | Questionnaire (Written) | Although parents overall highly valued oral health for their child, 12% of parents were unwilling to spend any money to maintain good oral health for their children. Linear regression analyses found that willingness to invest time in brushing (β=0.292; p<0.001) and willingness to invest time in visits to the dentist (=0.198; p=0.03) were significantly correlated with WTP. |
| Which factors influence willingness-to-pay for orthognathic treatment | Smith, A.S. & Cunningham, S.J. (2004) UK | General public (100), Orthogna thic patients (88) | Repeat interview after 6-8 weeks (20 respondents) | Interview | Patients were willing to pay €2750 more than members of the general public for orthognathic treatment (p=0.009). Linear regression analysis showed that malocclusion type was significantly associated with WTP (p=0.03). Class II div I patients were prepared to pay €3130 more than those with Class III malocclusions. |
Income, gender, age and education were commonly tested as variables that were potentially associated with WTP values and were often adjusted in regression analyses. Eleven publications tested for income (Table 4). Eight of these publications tested for household income [26, 27, 47, 48, 57, 58, 62, 63], while the remaining three tested for annual income (not explicitly stated if household or personal) [28, 59, 60]. WTP was found to be positively associated with income in eight publications [26, 27, 47, 48, 58, 60, 62, 63]. Three studies [28, 57, 59] did not find any statistically significant asociation between WTP and income. In the study by Srivastava, Feine [47], higher income was associated with higher WTP in a public funding scenario, but no statistically significant relationship was detected for an out-of-pocket payment scenario. In the study by Atchison, Gironda [63], a WTP-income relationship was noted for third molar surgery patients with a preference for jaw wiring, but not for the other patient groups. This was similar in the study by Vernazza, Wildman [61], where a positive relationship was reported among respondents who selected RCT or extraction with implants, but not among respondents who preferred extraction without replacement. In the study by Widström, et. Al (2012) [60], an annual income of EUR 25,000 to more than 50,000 was positively associated with a higher WTP when compared to an income of less than EUR 10,000, although this was not so for incomes between EUR 10,000-25,000. A related concept, socioeconomic status, was tested in two publications [46, 52]. A better socioeconomic status was associated with a higher WTP in both studies based on bivariate analyses. A higher family budget was also associated with a higher willingness and ability to pay [45].
Table 4.
Common factors associated with reported WTP amounts
| Variables that influence WTP | Statistically Significant Relationship1 | ||
|---|---|---|---|
| Yes (Higher WTP) | No | ||
| Income | Higher income | Lower income | |
| Tianviwat, S., Chongsuvivatwong, V. et al. (2008a) [sealants in permanent teeth] (B(95% CI)= 0.009(0.003-0.015); p=0.006); [fillings in permanent teeth] (B(95% CI)= 0.011(0.003-0.018); p=0.006); [extractions in primary teeth] (B(95% CI)= 0.005(0.001-0.009); p=0.03), Tianviwat, S., Chongsuvivatwong, V. et al. (2008b) (B(SE)= 58.71(27.90); p=0.04), Al Garni, B., Pani, S.C. et al. (2012) (B=-1.105; p=0.002), Atchison, K. A., Gironda, M.W. et al. (2007) [third molar/wire preference patients] (B=5720.45; p=0.04), Widström, E. & Seppälä, T. (2012) [25-50k vs <10k] (B(95% CI)=1.254(0.247-2.261); p=0.02); [>50k vs <10k] (B(95% CI)=1.893(0.761-3.025); p=0.001), Halvorsen, B. & Willumsen, T. (2004) (B=8.6; p<0.01), Srivastava, A., Feine, J.S. et al. (2014) [public-funded] [60-120k vs <60k] (β=0.117; p=0.033); [>120k vs <60k] (β=0.187; p=0.021), Vernazza, C.R., Steele, J.G. et al. (2015) [RCT, extract + implant] (B(95%CI)=213.56(59.33-367.80); p=0.007) | None | van Steenberghe, D., Bercy, P. et al. (2004)2, Matthews, D., Rocchi, A. et al (2002)2, Atchison, K. A., Gironda, M.W. et al. (2007) [third molar/surgery preference patients] (B=-7005.3; p=0.22); [fracture/wire preference patients] (B=6317.21; p=0.09; [fracture/surgery preference patients] (B=11931; p=0.12), Widström, E. & Seppälä, T. (2012) [10-25k vs <10k] (B(95% CI)=0.548(-0.418-1.513); p=0.27), Birch, S., Sohn, W. et al. (2004) [20-40k vs <20k] (β(SE)=-42.2(36.3); p=0.15); [40-60k vs <20k] (β(SE)=65.8(67.7); p=0.15); [>60k vs <20k] (β(SE)=69.2(65.5); p=0.15), Srivastava, A., Feine, J.S. et al. (2014) [out-of-pocket] [60-120k vs <60k] (β=0.006; p=0.98); [>120k vs <60k] (β=0.103; p=0.70), Vernazza, C.R., Steele, J.G. et al. (2015) [extract + leave gap]2 | |
| Gender | Female | Male | |
| Augusti, D., Augusti, G. et al. (2014) [posterior tooth] (B(95% CI)= -195.3(-381.6--9.0); p=0.04), Leung, K. C., & McGrath, C. P. (2010) [anterior missing tooth] (B(95% CI)=5541(1398.9-9683); p=0.01); [posterior missing tooth] (B(95% CI)=4836.5(1044.2-8628.7); p=0.01), Vernazza, C.R., Steele, J.G. et al. (2015) [Root Canal Treatment]2 | None | Tianviwat, S., Chongsuvivatwong, V. et al. (2008a) [sealants in permanent teeth] (B(95% CI)= -11.565(-60.593-37.462); p=0.64); [fillings in permanent teeth] (B(95% CI)= -17.549(-77.171-42.073); p=0.56); [extractions in primary teeth] (B(95% CI)= -14.011(-46.945-18.923); p=0.40), Vernazza C.R., Wildman J.R. et al. (2015) (B(95% CI)= 14.31(-20.21-48.84); p=0.41), Al Garni, B., Pani, S.C. et al. (2012) (B=-0.319; p=0.63), van Steenberghe, D., Bercy, P. et al. (2004) 2, Augusti, D., Augusti, G. et al. (2014) [anterior tooth] (B(95% CI)= -154.3(-354.7-46.0); p=0.13), Matthews, D., Rocchi, A. et al (2002)2, Atchison, K. A., Gironda, M.W. et al. (2007) [third molar/wire preference patients] (B=-522.82; p=0.93); [third molar/surgery preference patients] (B=3209.94; p=0.83); [fracture/wire preference patients] (B=4887.44; p=0.70); [fracture/surgery preference patients] (B=5691.23; p=0.75), Oscarson, N., Lindholm, L. et al. (2007) (B(SE)= -18.12(12.18); p=0.14), Pavlova, M., Groot, W. et al. (2004) [dental check-up] (β(SE)=-0.0224(0.051); p>0.05); [filling] (β(SE)=-0.0107(0.061); p>0.05); [extraction] (β(SE)=0.0657(0.061); p>0.05); [placement of dental prostheses] (β=-0.0026; p>0.05), Widström, E. & Seppälä, T. (2012) (B(95% CI)=-0.069(-0.465-0.327); p=0.73), Birch, S., Sohn, W. et al. (2004) (β(SE)=40.3(34.0); p=0.24), Srivastava, A., Feine, J.S. et al. (2014) (β=-0.063; p=0.73), Vernazza, C.R., Steele, J.G. et al. (2015) [extract + implant/leave gap]2 | |
| Age | Younger | Older | |
| Tianviwat, S., Chongsuvivatwong, V. et al. (2008a) [>50 years vs <50] [sealants in permanent teeth] (B(95% CI)=-84.396 (-159.417--9.375; p=0.027); [fillings in permanent teeth] (B(95% CI)= -99.403(-190.636--8.170); p=0.03); [extractions in primary teeth] (B(95% CI)=-54.899(-105.293—4.504); p=0.03)), Tianviwat, S., Chongsuvivatwong, V. et al., 2008b) [<30 years vs >50] (B(SE)= 132.04(47.63); p=0.01); [30-40 years vs >50] (B(SE)= 135.46(36.63); p<0.01) | None | Vernazza, C. R., Wildman, J.R. et al (2015) (B(95% CI)= 0.06(-1.54-1.66); p=0.95), van Steenberghe, D., Bercy, P. et al. (2004) 2, Augusti, D., Augusti, G. et al. (2014) (B(95% CI)= -2.0(-22.8-18.8); p=0.8488), Matthews, D., Rocchi, A. et al (2002)2, Atchison, K. A., Gironda, M.W. et al. (2007) [third molar/wire preference patients] (B=-553.47; p=0.25); [third molar/surgery preference patients] (B=-62.59; p=0.951); [fracture/wire preference patients] (B=-102.13; p=0.78); [fracture/surgery preference patients] (B=1054.19; p=0.10), Pavlova, M., Groot, W. et al. et al. (2004) [dental check-up] (β(SE)=-0.0032(0.002); p>0.05); [filling] (β(SE)=0.0001(0.002); p>0.05); [extraction] (β(SE)=0.0009(0.002); p>0.05); [placement of dental prostheses] (β(SE)=0.9919(0.002); p>0.05), Widström, E. & Seppälä, T. (2012) [birth year 1948 vs 1960] (B(95% CI)=-0.110(-0.677-0.457); p=0.70); [birth year 1954 vs 1960] (B(95% CI)=-0.479(-1.019-0.061); p=0.08); [birth year 1957 vs 1960] (B(95% CI)=0.078(-0.458-0.614); p=0.78), Birch, S., Sohn, W. et al. (2004) [30-50 years vs <20] (β(SE)=2.1(40.7); p=0.47); [≥50 years vs <20] (β(SE)=-46.6(41.2); p=0.47), Srivastava, A., Feine, J.S. et al. (2014) (β=-0.113; p=0.66), Smith, A.S. & Cunningham, S.J. (2004)2 | |
| Education | Higher | Lower | |
| Tianviwat, S., Chongsuvivatwong, V. et al. (2008b) [secondary school or higher vs primary school] (B(SE)= 60.77(27.61); p=0.03), Leung, K. C., & McGrath, C. P. (2010) [secondary or above vs nil/primary, anterior missing tooth] (B(95% CI)=4971.9(184-9759.9); p=0.04), Pavlova, M., Groot, W. et al. (2004) [university vs no education][dental check-up] (β(SE)=0.0638(0.025); p<0.05), [filling] (β(SE)=0.0830(0.028); p<0.05), Srivastava, A., Feine, J.S. et al. (2014) [graduate university or higher vs less than university, out of pocket] (β=0.437; p= 0.05) | None | Tianviwat, S., Chongsuvivatwong, V. et al. (2008a) [secondary school or higher vs primary school] [sealants in permanent teeth] (B(95% CI)= 30.621(-13.162-74.403); p=0.169); [fillings in permanent teeth] (B(95% CI)= 10.633(-42.611-63.878); p=0.69), [extractions in primary teeth] (B(95% CI)= 11.712(-17.699-4.112); p=0.433), Al Garni, B., Pani, S.C. et al. (2012) (B=0.091; p=0.78), Augusti, D., Augusti, G. et al. (2014) (B(95% CI)= 207.7(-124.6-540.1); p=0.22), Matthews, D., Rocchi, A. et al (2002)2, Atchison, K. A., Gironda, M.W. et al. (2007) [third molar/wire preference patients] (B=-259.05; p=0.95); [third molar/surgery preference patients] (B=8091.06; p=0.34); [fracture/wire preference patients] (B=-2129.21; p=0.70); [fracture/surgery preference patients] (B=-8716.41; p=0.38), Pavlova, M., Groot, W. et al. (2004) [extraction] (β(SE)=0.0497(0.034); p>0.05); [placement of dental prostheses] (β(SE)=0.0573(0.034); p>0.05), Widström, E. & Seppälä, T. (2012) [basic education, comprehensive school vs matriculation] (B(95% CI)=-0.303(-0.790-0.183); p=0.22); [professional training, vocational qualification, school level vs university or corresp. school level] (B(95% CI)=-0.265(-0.980-0.450); p=0.47); [professional training, vocational qualification, technical college vs university or corresp. school level] (B(95% CI)=-0.275(-0.753-0.202); p=0.26), Birch, S., Sohn, W. et al. (2004) [12 years vs <12] (β(SE)=51.4(52.0); p=0.31); [>12 years vs <12] (β(SE)=79.1(51.4); p=0.31), Srivastava, A., Feine, J.S. et al. (2014) [university degree vs less than university/ out-of-pocket] (β=0.418; p=0.15) | |
p value ≤ 0.05, from multivariable/multivariate analyses
No statistical data (beta, B, p-values) provided.
In terms of gender, no statistically significant difference in WTP was found between females and males in 13 publications (Table 4). Of the three studies that found a significant difference, females exclusively had a higher WTP [50, 62, 65]. However, the statistically significant association was limited to respondents who selected RCT, and for posterior tooth replacements only, in the studies by Vernazza, Steele [62] and Augusti, Augusti [65] respectively. Age was not related to WTP in 10 publications [45, 47, 53, 57, 59–61, 63, 65, 66]. Among the two publications that found a relationship [26, 27], older respondents were found to have a lower WTP. Finally, higher education was positively related to a higher WTP in four publications [26, 45, 50, 67]. WTP values were compared between respondents with a minimum of a graduate university [47], university [45], or secondary school education [26, 50], and respondents with a highest level of education below that. Education was not found to be associated with WTP in nine publications [27, 28, 45, 47, 48, 59, 60, 63, 65]. One publication found a positive WTP-education level relationship for respondents paying out-of-pocket for the intervention, but not for respondents paying via private insurance [47]. Another publication found a positive association between WTP and education levels for dental check-ups and fillings, but not for extractions and placement of dental prostheses [45].
Discussion
Though WTP has several limitations, it remains important for value measurements in dental care due to the theoretical difficulties [68] and suggested absence of other suitable measures [69]. In order to overcome its limitations, several overall methods and specific strategies have been recommended. Pre-testing is an important strategy for reducing bias and improving the content validity of WTP studies [16]. Pre-testing could also limit range bias, if implemented for assessing a suitable range of values, for all methods other than the open ended format. Pre-testing was described only in about a third (nine) of the publications. In particular for face-to-face interviews, pre-testing may help to mitigate interviewer effects and “social desirability” bias [22]. Face-to-face interviews were also recommended over mail surveys, as they allow for the use of graphic aids, provide adequate range of options and maintain respondent motivation [22]. Half (13) of the publications used questionniares with no interactive elements, like those present in a payment card format or a bidding format. A majority of the publications did not conduct pre-testing, and the use of mailed questionnaires may have increased the bias in WTP for these studies.
During the consideration of WTP by participants, emphasizing budgetary constraints can limit hypothetical bias. This was reported explicitly by four publications [4, 45, 47, 61]. None of the studies relied on the other proposed methods to minimize hypothetical bias. After the participants have expressed their WTP amounts, the identification and management of “protest zeros” [22] is important in minimizing skewed results. The management of zero WTP values was described in only four studies. Besides these strategies, other methods are available to calibrate hypothetical WTP to match real WTP. Such methods include the use of a statistical bias function [70], a quantitative or qualitative certainty scale [71], and dissonance-minimizing treatment [72]. Compliance, strategic, warm glow, and yea-saying bias may be minimized through interviewer calibration, the avoidance of sponsorship and remuneration for respondents, and warranting that respondents commit to their payment obligations [16].
The predominant methodology implemented in oral healthcare was different from that in overall healthcare. While payment card was the most frequently used methodology in healthcare [73], this was not the case in our review of dental publications. The bidding method was most commonly adopted, followed by the open-ended elicitation format. Ten of the 11 publications with a bidding format had a fixed starting point, which may result in starting point bias [16]. While two starting points were used in the study by Matthews, Rocchi [28], no further validation test results were reported. Proposed methods to overcome starting point bias include pre-testing, randomization of starting bids, and accounting for the bias statistically in multivariate analyses [74]. Pre-testing was carried out to various extents in the oral health situations, where some reported more details than others.
Nine publications relied on the open-ended format for WTP elicitation. Criticisms of the open-ended format include the lack of realism, significant bias, and tendency towards overstatement [22]. While two publications included a (single value) close-ended dichotomous yes/no question prior to the open-ended WTP elicitation, no validations of, or direct comparisons between, the two formats were made. Though the implementation of open-ended format may be the easiest, its criticisms should limit its further use for the measurement of WTP.
Expressed WTP values elicited using the randomly shuffled payment card method were found to be “more likely to reflect ‘true’ WTP” than methods where values were listed from high-to-low, or from low-to-high [75]. Nevertheless, only one study adopted the shuffled payment card method. The majority of payment card studies in our review required respondents to pick a WTP value from a list, although this method has greater deviations and biases than if respondents considered each price option in turn [76].
Since test-retest reliability estimates for WTP were found to be greater than 0.7 in three publications, there appears to be a “strong agreement” between self-reported values over two time periods. However, the stability of WTP values was not tested over a longer term of more than eight weeks.
Since WTP is associated with the ability to pay, some postulate that it may lead to skewed resource allocations that favour the rich rather than the majority of the population [77]. This would especially be true in cases where the sampling is not representative of the target population. Suggestions to circumvent this include an examination of preferences across different social classes when eliciting preferences for close substitutes and/or disparate healthcare interventions, and the application of distributional weights where preference structures differ.
As seen in the included studies, monetary valuations can be elicited from patients, caregivers, or the general public who may be taxpayers and/or potential users of the health services in future [19]. Patients may be more familiar with the interventions being valued, although the general public may provide less biased valuations [20]. This choice of sampling frame also depends in part on how the intervention is funded. A societal perspective and a representative sampling frame may be adopted for public funded interventions, whereas a more focused sampling frame may be more appropriate for individually funded interventions.
Factors influencing WTP
Many of the studies that assessed other factors and their effects on WTP were not planned for these analyses. Thus there may be sampling, study design, statistical testing strategies and sample-size considerations that may have limited their ability to report statistically significant relationships. Only factors derived from multivariate analyses were included in this review due to the limitations of bivariate analyses [78]. These related variables can help in planning future studies and help account for the factors during the design and analyses phases for a more accurate measurement of WTP.
In eight of 11 studies that assessed income, there was a statistically significant association between income and WTP. In cases where income was related to WTP, the tendency is for higher WTP values with higher incomes. In one study, a higher income was said to be associated with a lower mean bid price, but the data reported from regression analysis indicate an inverse relationship [48]. Where an education-WTP value association was found, higher WTP values were exclusively associated with groups with higher minimum education levels. Among these, one study reported a significant relationship and a p-value=0.05 [47]. This may have been due to rounding off errors, and was reported here as such. The rest of the studies did not find a statistically significant relationship. This may indicate a trend, where education may play an important role in only some situations and samples. This contrasts with the findings of a literature review on WTP studies on diagnostic technologies in healthcare where higher income and education were in general associated with higher WTP values [79]. A majority of the studies that examined the influence of gender found no significance, although in select studies, females reported higher WTP. A similar trend was found when age was investigated, with younger respondents citing higher WTP values in studies. As most of the included studies were not specifically planned to test the effect of various variables on WTP, these trends in results suggest the importance of assessing relevant income related variables, and other variables related to socio-economic status, in WTP studies.
Conclusion
Based on available evidence, WTP studies in oral health would reduce biases with the use of pre-testing, face-to-face elicitation, a well tested script, and avoidance of open-ended questions. Out of the 26 available dental studies on willingness to pay, the two most common WTP elicitation modes in dental studies were self-completed questionnaires and face-to-face interviews. Bidding game, open-ended and payment card WTP elicitation formats were frequently used. Most studies investigated WTP in an out-of-pocket payment scenario. Pretesting was only reported in nine publications on WTP, and few studies reported measures to address starting point bias and hypothetical bias directly.
In studies where statistical significance of factors influencing WTP was reported, the trend suggested that higher income was, associated with a higher WTP. A majority of studies found no association between gender, age, education and WTP, and the ones that were significant reported an association between female gender, younger ages and higher education levels with higher WTP.
Overall, there have been a significant number of WTP studies in oral health and some good practice was observed. But many studies adopted sub-optimal methodology.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
N.B.: C. R. Vernazza is funded by a Clinician Scientist award supported by the National Institute for Health Research. This paper details independent research and the views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.
Contributor Information
Dr Sharon Hui Xuan Tan, Ministry of Health Holdings, Singapore, 1 Maritime Square, Singapore 099253, Tel: +6598358734.
Dr Christopher R Vernazza, Centre for Oral Health Research, Newcastle University, Framlington Place, Newcastle upon Tyne. NE2 4BW Tel: 01912088396.
Dr Rahul Nair, ARCPOH, Adelaide Dental School, University of Adelaide, Address: Level 1, 122 Frome Street, The University of Adelaide, SA 5005 Australia, Tel: +61 415 691 949.
References
- 1.Wall T, Vujicic M. U.S. dental spending continues to be flat. Health Policy Institute Research Brief; 2015. [cited http://www.ada.org/~/media/ADA/Science%20and%20Research/HPI/Files/HPIBrief_1215_2.ashx 3 May 2016] [Google Scholar]
- 2.Australian Institute of Health and Welfare and the Dental Statistics, R.U., Australian Research Centre for Population Oral Health, University of Adelaide. Cost of dental care. [cited 2016 3rd May];2013 http://www.aihw.gov.au/dental/cost/
- 3.Singapore DOS. Table 19A Average Monthly Household Expenditure by Type of Goods and Services and Household Size. H.E.S. 2012/13, editor. 2012/2013 http://www.tablebuilder.singstat.gov.sg/publicfacing/sortOnColumn.action, H.E.S. 2012/13, Editor.
- 4.Matthews DC, et al. Willingness to pay for periodontal therapy: development and testing of an instrument. J Public Health Dent. 1999;59(1):44–51. doi: 10.1111/j.1752-7325.1999.tb03234.x. [DOI] [PubMed] [Google Scholar]
- 5.Klose T. The contingent valuation method in health care. Health Policy. 1999;47(2):97–123. doi: 10.1016/s0168-8510(99)00010-x. [DOI] [PubMed] [Google Scholar]
- 6.Hanley N, Ryan M, Wright R. Estimating the monetary value of health care: lessons from environmental economics. Health Econ. 2003;12(1):3–16. doi: 10.1002/hec.763. [DOI] [PubMed] [Google Scholar]
- 7.Birch S, Ismail AI. Patient preferences and the measurement of utilities in the evaluation of dental technologies. Journal of Dental Research. 2002;81(7):446–450. doi: 10.1177/154405910208100702. [DOI] [PubMed] [Google Scholar]
- 8.Sloan FA. Valuing Health Care: Costs, Benefits, and Effectiveness of Pharmaceuticals and Other Medical Technologies. Cambridge University Press; 1996. [Google Scholar]
- 9.Johannesson M. Theory and Methods of Economic Evaluation of Health Care. Springer; US: 2013. [PubMed] [Google Scholar]
- 10.Nunes PA, van den Bergh JC. Economic valuation of biodiversity: sense or nonsense? Ecological economics. 2001;39(2):203–222. [Google Scholar]
- 11.Birch S, Donaldson C. Cost-benefit analysis: dealing with the problems of indivisible projects and fixed budgets. Health Policy. 1987;7(1):61–72. doi: 10.1016/0168-8510(87)90047-9. [DOI] [PubMed] [Google Scholar]
- 12.Nimdet K, et al. A systematic review of studies eliciting willingness-to-pay per quality-adjusted life year: does it justify CE threshold? PLoS One. 2015;10(4):e0122760. doi: 10.1371/journal.pone.0122760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cookson R. Willingness to pay methods in health care: a sceptical view. Health Econ. 2003;12(11):891–4. doi: 10.1002/hec.847. [DOI] [PubMed] [Google Scholar]
- 14.Mitchell RC, Carson RT. Using Surveys to Value Public Goods: The Contingent Valuation Method. Resources for the Future. 1989 [Google Scholar]
- 15.Carson RT. Contingent Valuation: A Practical Alternative when Prices Aren’t Available. Journal of Economic Perspectives. 2012;26(4):27–42. [Google Scholar]
- 16.Jareinpituk S. Developing willingness to pay and a prepayment oral care plan: An application to pre-school children in Thailand. ProQuest, UMI Dissertations Publishing; 2004. [Google Scholar]
- 17.Carson RT, Hanemann WM, Kopp RJ, Krosnick JA, Mitchell RC, Presser S, Ruud PA, Smith VK, Conaway M, Martin K. Temporal Reliability of Estimates from Contingent Valuation. Land Economics. 1997;73(2):151–163. [Google Scholar]
- 18.Brouwer R, Bateman IJ. Temporal stability and transferability of models of willingness to pay for flood control and wetland conservation. Water Resources Research. 2005;41(3):n/a–n/a. [Google Scholar]
- 19.Dolan P. Whose preferences count? Med Decis Making. 1999;19(4):482–6. doi: 10.1177/0272989X9901900416. [DOI] [PubMed] [Google Scholar]
- 20.Whitehead SJ, Ali S. Health outcomes in economic evaluation: the QALY and utilities. British Medical Bulletin. 2010;96(1):5–21. doi: 10.1093/bmb/ldq033. [DOI] [PubMed] [Google Scholar]
- 21.O'Brien B, Gafni A. When Do the “Dollars” Make Sense? Medical Decision Making. 1996;16(3):288–299. doi: 10.1177/0272989X9601600314. [DOI] [PubMed] [Google Scholar]
- 22.Arrow K, Solow Robert, Portney Paul R, Leamer Edward E, Radner Roy, Shuman Howard. Report of the NOAA Panel on Contingent Valuation. Federal Register; 1993. pp. 4601–4614. [Google Scholar]
- 23.Kanninen BJ. Bias in Discrete Response Contingent Valuation. Journal of Environmental Economics and Management. 1995;28:114–125. [Google Scholar]
- 24.Kjær T. A review of the discrete choice experiment-with emphasis on its application in health care. Health Economic Papers. Vol. 2005. University of Denmark: 2005. p. 1. [Google Scholar]
- 25.Tianviwat S, Chongsuvivatwong V, Birch S. Optimizing the mix of basic dental services for Southern Thai schoolchildren based on resource consumption, service needs and parental preference. Community Dent Oral Epidemiol. 2009;37(4):372–80. doi: 10.1111/j.1600-0528.2009.00481.x. [DOI] [PubMed] [Google Scholar]
- 26.Tianviwat S, Chongsuvivatwong V, Birch S. Prevention versus cure: measuring parental preferences for sealants and fillings as treatments for childhood caries in Southern Thailand. Health Policy. 2008;86(1):64–71. doi: 10.1016/j.healthpol.2007.09.016. [DOI] [PubMed] [Google Scholar]
- 27.Tianviwat S, Chongsuvivatwong V, Birch S. Different dental care setting: does income matter? Health Econ. 2008;17(1):109–18. doi: 10.1002/hec.1237. [DOI] [PubMed] [Google Scholar]
- 28.Matthews D, Rocchi A, Gafni A. Putting your money where your mouth is: willingness to pay for dental gel. Pharmacoeconomics. 2002;20(4):245–55. doi: 10.2165/00019053-200220040-00003. [DOI] [PubMed] [Google Scholar]
- 29.Matthews D, et al. Use of an interactive tool to assess patients' willingness-to-pay. J Biomed Inform. 2001;34(5):311–20. doi: 10.1006/jbin.2002.1032. [DOI] [PubMed] [Google Scholar]
- 30.Koberlein J, Klingenberger D. Foreign dentures and dental tourism--willingness-to-pay and factors influencing the demand for foreign dental prosthesis in Germany. Gesundheitswesen. 2011;73(7):e111–8. doi: 10.1055/s-0030-1254174. [DOI] [PubMed] [Google Scholar]
- 31.Cunningham SJ, Hunt NP. Relationship between utility values and willingness to pay in patients undergoing orthognathic treatment. Community Dent Health. 2000;17(2):92–6. [PubMed] [Google Scholar]
- 32.Cunningham MA, et al. Using choice-based conjoint to determine the relative importance of dental benefit plan attributes. J Dent Educ. 1999;63(5):391–9. [PubMed] [Google Scholar]
- 33.Willumsen T. Patient' willingness to pay for treatment of dental phobia. Journal of Dental Research. 2000;79:145–145. [Google Scholar]
- 34.Goldstein M, Sumner W, Littenberg B. Preferences and willingness to pay for painless dental laser drill. Medical Decision Making. 1998;18(4):457–457. [Google Scholar]
- 35.Ryan M, Farrar S. Using conjoint analysis to elicit preferences for health care. Bmj. 2000;320(7248):1530–3. doi: 10.1136/bmj.320.7248.1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chakraborty G, Gaeth GJ, Cunningham M. Understanding consumers' preferences for dental service. J Health Care Mark. 1993;13(3):48–58. [PubMed] [Google Scholar]
- 37.Listl S, Tu YK, Faggion CM., Jr A cost-effectiveness evaluation of enamel matrix derivatives alone or in conjunction with regenerative devices in the treatment of periodontal intra-osseous defects. J Clin Periodontol. 2010;37(10):920–7. doi: 10.1111/j.1600-051X.2010.01611.x. [DOI] [PubMed] [Google Scholar]
- 38.Chun JS, et al. The analysis of cost-effectiveness of implant and conventional fixed dental prosthesis. J Adv Prosthodont. 2016;8(1):53–61. doi: 10.4047/jap.2016.8.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Speight PM, et al. The cost-effectiveness of screening for oral cancer in primary care. Health Technol Assess. 2006;10(14):1–144. doi: 10.3310/hta10140. iii-iv. [DOI] [PubMed] [Google Scholar]
- 40.Dixon S, Shackley P. Estimating the benefits of community water fluoridation using the willingness-to-pay technique: results of a pilot study. Community Dent Oral Epidemiol. 1999;27(2):124–9. doi: 10.1111/j.1600-0528.1999.tb02001.x. [DOI] [PubMed] [Google Scholar]
- 41.Re D, et al. Is a new sonic toothbrush more effective in plaque removal than a manual toothbrush? Eur J Paediatr Dent. 2015;16(1):13–8. [PubMed] [Google Scholar]
- 42.Tamaki Y, et al. Characteristics and willingness of patients to pay for regular dental check-ups in Japan. J Oral Sci. 2004;46(2):127–33. doi: 10.2334/josnusd.46.127. [DOI] [PubMed] [Google Scholar]
- 43.Tuominen R. Evaluation of three methods assessing the relative value of a dental program. Acta Odontol Scand. 2008;66(2):82–7. doi: 10.1080/00016350801958274. [DOI] [PubMed] [Google Scholar]
- 44.Oscarson N, Lindholm L, Kallestal C. The value of caries preventive care among 19-year olds using the contingent valuation method within a cost-benefit approach. Community Dent Oral Epidemiol. 2007;35(2):109–17. doi: 10.1111/j.1600-0528.2007.00306.x. [DOI] [PubMed] [Google Scholar]
- 45.Pavlova M, Groot W, Van Merode G. Willingness and ability of Bulgarian consumers to pay for improved public health care services. Applied Economics. 2004;36(10):1117–1130. [Google Scholar]
- 46.Vermaire JH, et al. Putting your money where your mouth is: parents' valuation of good oral health of their children. Soc Sci Med. 2012;75(12):2200–6. doi: 10.1016/j.socscimed.2012.08.018. [DOI] [PubMed] [Google Scholar]
- 47.Srivastava A, Feine JS, Esfandiari S. Are people who still have their natural teeth willing to pay for mandibular two-implant overdentures? J Investig Clin Dent. 2014;5(2):117–24. doi: 10.1111/jicd.12057. [DOI] [PubMed] [Google Scholar]
- 48.Al Garni B, et al. Factors affecting the willingness to pay for implants: A study of patients in Riyadh, Saudi Arabia. Dent Res J (Isfahan) 2012;9(6):719–24. [PMC free article] [PubMed] [Google Scholar]
- 49.Esfandiari S, et al. Implant overdentures for edentulous elders: study of patient preference. Gerodontology. 2009;26(1):3–10. doi: 10.1111/j.1741-2358.2008.00237.x. [DOI] [PubMed] [Google Scholar]
- 50.Leung KC, McGrath CP. Willingness to pay for implant therapy: a study of patient preference. Clin Oral Implants Res. 2010;21(8):789–93. doi: 10.1111/j.1600-0501.2009.01897.x. [DOI] [PubMed] [Google Scholar]
- 51.Rosvall MD, et al. Attractiveness, acceptability, and value of orthodontic appliances. Am J Orthod Dentofacial Orthop. 2009;135(3):276.e1–12. doi: 10.1016/j.ajodo.2008.09.020. discussion 276–7. [DOI] [PubMed] [Google Scholar]
- 52.Feu D, et al. Esthetic perception and economic value of orthodontic appliances by lay Brazilian adults. Dental Press Journal of Orthodontics. 2012;17(5):102–114. [Google Scholar]
- 53.Smith AS, Cunningham SJ. Which factors influence willingness-to-pay for orthognathic treatment? Eur J Orthod. 2004;26(5):499–506. doi: 10.1093/ejo/26.5.499. [DOI] [PubMed] [Google Scholar]
- 54.Ethier MC, et al. Perspectives toward oral mucositis prevention from parents and health care professionals in pediatric cancer. Support Care Cancer. 2012;20(8):1771–7. doi: 10.1007/s00520-011-1274-x. [DOI] [PubMed] [Google Scholar]
- 55.Stone SJ, et al. Cost-effectiveness of personalized plaque control for managing the gingival manifestations of oral lichen planus: a randomized controlled study. J Clin Periodontol. 2013;40(9):859–67. doi: 10.1111/jcpe.12126. [DOI] [PubMed] [Google Scholar]
- 56.Esfandiari S, et al. Implant overdentures for edentulous elders: study of patient preference. Gerodontology. 2009;26(1):3–10. doi: 10.1111/j.1741-2358.2008.00237.x. [DOI] [PubMed] [Google Scholar]
- 57.van Steenberghe D, et al. Patient evaluation of a novel non-injectable anesthetic gel: a multicenter crossover study comparing the gel to infiltration anesthesia during scaling and root planing. J Periodontol. 2004;75(11):1471–8. doi: 10.1902/jop.2004.75.11.1471. [DOI] [PubMed] [Google Scholar]
- 58.Halvorsen B, Willumsen T. Willingness to pay for dental fear treatment. Is supplying dental fear treatment socially beneficial? Eur J Health Econ. 2004;5(4):299–308. doi: 10.1007/s10198-004-0238-1. [DOI] [PubMed] [Google Scholar]
- 59.Birch S, et al. Willingness to pay for dentin regeneration in a sample of dentate adults. Community Dent Oral Epidemiol. 2004;32(3):210–6. doi: 10.1111/j.1600-0528.2004.00156.x. [DOI] [PubMed] [Google Scholar]
- 60.Widstrom E, Seppala T. Willingness and ability to pay for unexpected dental expenses by Finnish adults. BMC Oral Health. 2012;12:35. doi: 10.1186/1472-6831-12-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Vernazza CR, et al. Factors affecting patient valuations of caries prevention: Using and validating the willingness to pay method. J Dent. 2015;43(8):981–8. doi: 10.1016/j.jdent.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 62.Vernazza CR, et al. Factors affecting direction and strength of patient preferences for treatment of molar teeth with nonvital pulps. Int Endod J. 2015;48(12):1137–46. doi: 10.1111/iej.12413. [DOI] [PubMed] [Google Scholar]
- 63.Atchison KA, et al. Baseline characteristics and treatment preferences of oral surgery patients. J Oral Maxillofac Surg. 2007;65(12):2430–7. doi: 10.1016/j.joms.2007.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Balevi B, Shepperd S. The management of an endodontically abscessed tooth: patient health state utility, decision-tree and economic analysis. BMC Oral Health. 2007;7:17. doi: 10.1186/1472-6831-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Augusti D, Augusti G, Re D. Prosthetic restoration in the single-tooth gap: patient preferences and analysis of the WTP index. Clinical Oral Implants Research. 2014;25(11):1257–1264. doi: 10.1111/clr.12264. [DOI] [PubMed] [Google Scholar]
- 66.Matthews D, Rocchi A, Gafni A. Putting your money where your mouth is - Willingness to pay for dental gel. Pharmacoeconomics. 2002;20(4):245–255. doi: 10.2165/00019053-200220040-00003. [DOI] [PubMed] [Google Scholar]
- 67.Srivastava A, Feine JS, Esfandiari S. Are people who still have their natural teeth willing to pay for mandibular two-implant overdentures? Journal of investigative and clinical dentistry. 2014;5(2):117–24. doi: 10.1111/jicd.12057. [DOI] [PubMed] [Google Scholar]
- 68.Birch S, Ismail A. Patient preferences and the measurement of utilities in the evaluation of dental technologies. Journal of dental research. 2002;81(7):446–450. doi: 10.1177/154405910208100702. [DOI] [PubMed] [Google Scholar]
- 69.Nair R, Ai-Min A-MN. A conceptual framework (Cat-4) for estimating clinical relevance of evidence related to oral diagnosis. Journal of Interdisciplinary Dentistry. 2015;5(3):114. [Google Scholar]
- 70.Blackburn M, Harrison G, Rutstrom E. Statistical Bias Functions and Informative Hypothetical Surveys. American Journal of Agricultural Economics. 1994;76:1084–1088. [Google Scholar]
- 71.Champ PA, B R, Brown TC, McCollum DW. Using donation mechanisms to value nonuse benefit from public goods. J Environ Econ Manage. 1997;33:151–162. [Google Scholar]
- 72.Mark Morrison TB. Testing the Effectiveness of Certainty Scales, Cheap Talk, and Dissonance-Minimization in Reducing Hypothetical Bias in Contingent Valuation Studies. Environmental & Resource Economics. 2009;44(3):307–326. [Google Scholar]
- 73.Smith RD. The discrete-choice willingness-to-pay question format in health economics: should we adopt environmental guidelines? Med Decis Making. 2000;20(2):194–206. doi: 10.1177/0272989X0002000205. [DOI] [PubMed] [Google Scholar]
- 74.McNamee P, et al. A game of two halves? Incentive incompatibility, starting point bias and the bidding game contingent valuation method. Health Econ. 2010;19(1):75–87. doi: 10.1002/hec.1448. [DOI] [PubMed] [Google Scholar]
- 75.Smith RD. It's not just what you do, it's the way that you do it: the effect of different payment card formats and survey administration on willingness to pay for health gain. Health Econ. 2006;15(3):281–93. doi: 10.1002/hec.1055. [DOI] [PubMed] [Google Scholar]
- 76.Vossler CA, M M. Induced-value tests of contingent valuation elicitation mechanisms. Environmental & Resource Economics. 2006;35:137–168. [Google Scholar]
- 77.Donaldson C. Eliciting patients’ values by use of ‘willingness to pay’: letting the theory drive the method. Health Expectations. 2001;4:180–188. doi: 10.1046/j.1369-6513.2001.00126.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Spicer J. Making Sense of Multivariate Data Analysis: An Intuitive Approach. SAGE Publications; 2005. [Google Scholar]
- 79.Lin PJ, et al. Willingness to pay for diagnostic technologies: a review of the contingent valuation literature. Value Health. 2013;16(5):797–805. doi: 10.1016/j.jval.2013.04.005. [DOI] [PubMed] [Google Scholar]