Abstract
Purpose of review
In this paper we review the epidemiology, diagnosis and pathogenesis of fractures and renal osteodystrophy.
Recent findings
The role of bone quality in the pathogenesis of fracture susceptibility in CKD is beginning to be elucidated. Bone quality refers to bone material properties, such as cortical and trabecular microarchitecture, mineralization, turnover, microdamage, and collagen content and structure. Recent data has added to our understanding of the effects of CKD on alterations to bone quality, emerging data on the role of abnormal collagen structure on bone strength, the potential of non-invasive methods to inform our knowledge of bone quality and how we can use these methods to inform strategies that protect against bone loss and fractures. However, more prospective data is required.
Summary
Chronic kidney disease (CKD) is associated with abnormal bone quality and strength which results in high fracture incidence.
Keywords: Bone quality, bone mineral density, renal osteodystrophy, kidney, fracture, dialysis
Introduction
Chronic Kidney Disease – Mineral and Bone Disorder
The term CKD-mineral and bone disorder (CKD-MBD) was coined by the Kidney Disease Improving Global Outcomes (KDIGO) working group to refer more broadly to the systemic disorder of mineral and bone metabolism due to CKD; it is manifested by either one or a combination of (1) abnormalities of calcium, phosphorus, parathyroid hormone (PTH), or vitamin D metabolism; (2) abnormalities of bone turnover, mineralization, volume, linear growth or strength; and (3) vascular or other soft tissue calcification1.
Renal osteodystrophy (ROD) is the bone component of CKD-MBD. It is a disorder of bone quality and strength secondary to effects of metabolic and hormonal disturbances that occur with kidney failure, including: hyperphosphatemia, hypocalcemia, secondary hyperparathyroidism (HPT), 25(OH)D deficiency and decreased renal synthesis of 1,25(OH)2D, chronic metabolic acidosis, chronic inflammation and premature hypogonadism. These abnormalities impair bone turnover and mineralization, collagen structure, and cortical and trabecular microarchitecture (Figure 1). Collectively, these effects increase fracture risk by reducing both bone mass and quality. Bone “quality” is a catchall term for the numerous properties influencing bone’s mechanical function outside of bone mass, i.e. if two bones are of the same size but of dissimilar fracture resistance, this difference can be attributed to differences in quality.
Figure 1.
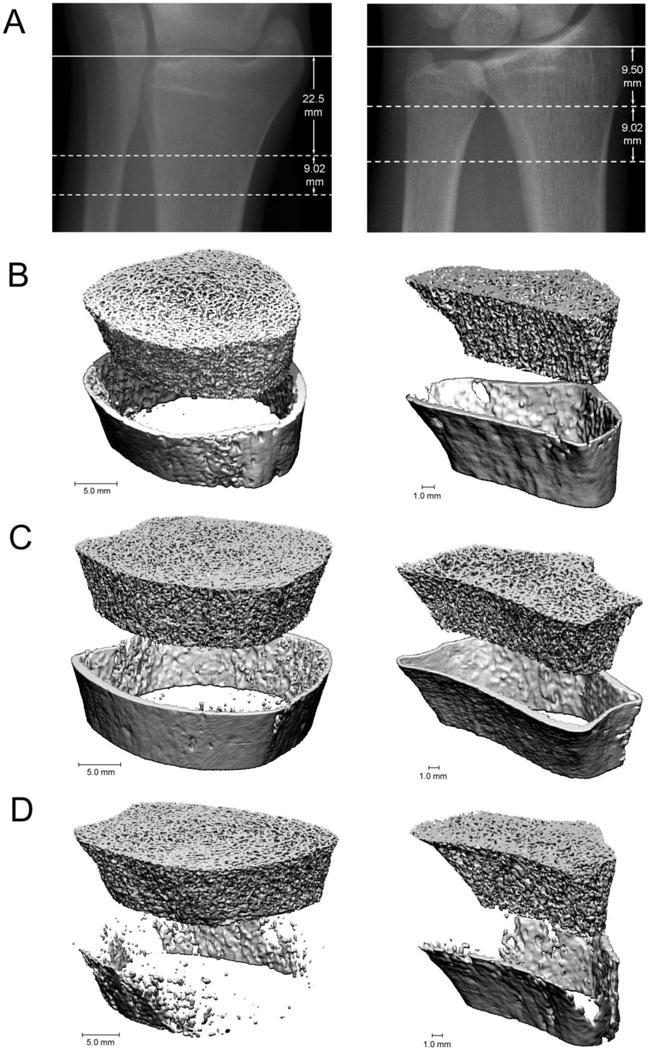
35: HR-pQCT provides detailed images of bone geometry and microarchitecture at the radius (left) and tibia (right). (A) Scout view represents the reference line position (solid line) and the measurement site (dotted line). (B) Images from a healthy, post-menopausal white woman. (C) Images from a pre-dialysis female patient with CKD and without fracture. (D) Images from a pre-dialysis female patient with CKD and with prevalent fracture.
Fracture epidemiology in chronic kidney disease
Fractures are 2- to 14-fold more common in CKD patients than in the general population2–4, and have been reported to increase in prevalence5 and incidence6 as kidney function worsens (Figure 2). In patients on dialysis with end stage renal disease (ESRD), fracture incidence at the hip was reported to have peaked in 2004 at 21.9 events per 1,000 person-years, with subsequent decline to 16.6 per 1,000 person-years in 20107. In contrast, rates of peripheral (arm and leg) fractures were reported to have increased continuously between 1992 and 2009, and the majority of increased fracture risk occurred in Caucasian patients8. Kidney transplant recipients are also susceptible to increased fractures9–12: early after transplantation hip fracture risk is 34% higher than in patients on dialysis11; risk of hip and spine fracture are more than 4- and 23- fold higher12 than in the general population; and about 25% of recipients experience a fracture within the 5-years of their transplant9. Recent data suggests that improved management of CKD-MBD before and after transplantation have resulted in a 3-fold reduction of fracture incidence during the first post-transplant year13.
Figure 2.

Hip fracture incidence increases with progressive CKD. As patients age in the general population there is an increased incidence of hip fracture. This incidence increases with progression of CKD. Data from Alem et al for dialysis patients and the general population from Olmstead Minnesota3, Naylor et al for CKD stages 3–45. Pt-yrs = patient years.
Fractures in CKD patients are associated with excess morbidity, mortality and health economic costs14–17. In one study, one-third to almost one-half of patients with ESRD with a fracture admission to the hospital were discharged to a skilled-nursing facility. In the year following discharge, patients had an adjusted mean of 3.8–5.2 additional hospitalizations, comprising on average an extra 33–52 inpatient days compared to patients without fracture18. After hip fracture, mortality risk was reported to increase by 16%18 to 60%15, and healthcare associated costs have been estimated to exceed $100 and $500 billion for patients with ESRD and predialysis CKD respectively17. Therefore, improved identification and management of increased fracture risk in CKD patients could significantly reduce both the morbidity and economic burdens of CKD-MBD.
CKD impairs bone quality and strength
Bone strength (and fracture risk) is defined by both its mass and quality. Bone mineral density (BMD) is a determination of its mass or quantity and is measured in the clinic by dual energy X-ray absorptiometry (DXA). Bone quality is defined by bone material properties and includes bone turnover, microarchitecture, mineralization, accumulation of microdamage (microscale cracks), and collagen properties (such as glycation and crosslinking). The hormonal and metabolic disturbances associated with CKD cause defects in all aspects of bone quality (Table 1).
Table 1.
Bone changes associated with hormonal and metabolic disturbances of renal osteodystrophy
Decreased bone density and microarchitecture
|
Decreased bone quality
|
Alterations in bone turnover affect bone strength and quality by controlling bone mass, microstructure, and the balance and spatial distribution of newly formed, mature, and aged or damaged areas of tissue19. Microdamage, advanced glycation endproducts (AGEs), mineralization, mineral carbonate substitution, and mineral crystallinity can all increase or accumulate with time and influence bone mechanical properties20, 21. The presence of microcracks of sufficient size and/or number is thought to reduce bone’s ability to withstand larger impacts22. AGEs form crosslinks in the collagen matrix, limit fibril stretching and slipping, and can embrittle the tissue23. Increased mineralization and carbonate substitution stiffen the bone matrix and may also contribute to brittleness in older bone24. In healthy bone, areas of aged or damaged bone are targeted for turnover, an ongoing repair process that removes problem areas and maintains the mean tissue age and properties of the bone. A disruption in the balance of turnover, and therefore this repair process, occurs in both high and low turnover ROD patients. As such, it is not surprising that bone quality is impaired in CKD-MBD. In addition to turnover-related effects on bone quality, CKD may directly affect the composition and quality of bone through factors including altered mineral metabolism and oxidative stress.
Measurement of Bone Mass
Dual energy X-ray absorptiometry
DXA is the clinical standard to measure bone mass and fracture risk in the general population. The use of DXA to predict fractures in patients with CKD has been controversial; however, the recent 2016 KDIGO Guideline updates now recommend DXA to predict fracture (out for public review). Longitudinal studies in patients with CKD stages 3 through 5D25–27 and after kidney transplantation28 demonstrated that low areal BMD measured by DXA at the forearm, hip (total and femoral neck) and spine predicts future fracture. These studies also indicate the World Health Organization T-score cut offs for osteopenia and osteoporosis can be used for CKD patients as for the general population. It is important to note that DXA does not assess either bone tissue quality or the type of renal osteodystrophy; thus, bone biopsy remains the gold standard to inform treatment decisions in patients with CKD.
High resolution imaging in CKD-MBD
In addition to DXA discussed above, QCT and HR-pQCT are imaging tools that measure 3-dimesional bone density and structural aspects of bone quality. They do not measure remodeling or mineralization. Therefore, they cannot be used to inform type of treatment since they are unable to determine ROD type.
High-resolution imaging tools assess cortical and trabecular 3-dimensional (volumetric) density, geometry, microarchitecture, and strength. They allow us to explore the pathogenesis of bone fragility due to CKD or other metabolic bone diseases non-invasively. QCT has a resolution of 300 μm3 and quantifies volumetric density and geometry of cortical and trabecular bone. Using QCT, studies have found that in CKD patients cortical deficits predominate29, 30 and cortical abnormalities both discriminate29 and predict fracture31.
Similarly, HR-pQCT separately quantifies cortical and trabecular volumetric density and geometry, but its higher nominal resolution of 60 to 82 μm3 permits measurement of trabecular number, thickness and separation. Finite element analysis, a computational method to measure bone mechanical competence (i.e., strength), is applied to 3-dimensional HR-pQCT datasets to assess biomechanical characteristics of either whole bone or individual cortical and trabecular compartments. Advanced HR-pQCT processing methods also permit characterization of cortical porosity32, 33 and trabecular plate-rod structure34.
Our group and others have shown that measures of bone density, geometry and microarchitecture at the ultradistal radius and tibia from HR-pQCT both discriminated and predicted fractures35–39, identified abnormalities in bone quality that negatively impacted bone strength40–42, and elucidated underlying microstructural defects that resulted in abnormalities of bone density measured by DXA40, 41. For example, in a longitudinal study of 54 patients with CKD stages 2 through 5D (ESRD) we found that mean annualized losses of bone density by DXA at the radius was 2.9%40. With HR-pQCT, we determined the bone loss by DXA was characterized by loss of cortical area (−2.9%), density (−1.3%) and thickness (−2.8%) and a significant increase in cortical porosity (+4.2%).
Measurement of Bone Quality
Tetracycline double-labeled transiliac crest bone biopsy with histomorphometry is the standard to determine bone quality. Histomorphometric analyses quantify volume and microarchitecture of cancellous and cortical compartments, microdamage, characteristics of mineralization, turnover, and collagen structure. In CKD, these abnormalities may include defects in bone volume and microarchitecture (cortical porosity, thinning and trabecularization, and trabecular thinning and dropout); in mineralization (osteomalacia); in turnover (low or high turnover); and in collagen structure (accumulation of advanced glycation end-products).
Unfortunately, bone biopsy is invasive, expensive, not widely available, and physicians performing this procedure require specialized training1, 43, 44. Also the biopsy only provides data about the type of ROD at one site (the anterior iliac crest) and at a single time-point. Due to these limitations of bone biopsy, non-invasive approaches that can be applied in the clinic to diagnose bone disease and monitor treatment responses would be helpful.
Assessing bone turnover and osteomalacia
Because treatment of ROD is based on turnover and the presence or absence of osteomalacia, their assessment is essential in determining bone quality in ROD. Pharmacologic agents that may prevent fractures in moderate CKD alter remodeling rates45–47. While anti-resorptive agents may be used in patients with high turnover, they should not be used in patients with low turnover or adynamic bone disease. Similarly, while osteoanabolic agents may be used in patients with low turnover, they are contraindicated in patients with high turnover.
Because bone biopsy may not be possible or practical, a non-invasive approach to turnover assessment would be helpful. Despite multiple limitations (discussed below), noninvasive assessment of remodeling can be achieved with reasonable accuracy by measuring circulating levels of parathyroid hormone (PTH) and bone turnover markers (BTMs)48–54. Bone formation markers, such as bone specific alkaline phosphatase (BSAP), osteocalcin, and procollagen type-1 N-terminal propeptide (P1NP) are markers of osteoblast function. Bone resorption markers, such as tartrate-resistant acid phosphatase 5b (Trap-5b) and C-terminal telopeptides of type I collagen (CTX) are markers of osteoclast number and function, respectively.
PTH and BSAP are the most commonly used markers of turnover in CKD-MBD. Generally, extremes of PTH predict extremes of bone turnover both in pre-dialysis52 and dialysis-dependent53, 54 patients. Unfortunately, prediction of underlying histology is poor when PTH levels are within the middle range. For BTMs, reference ranges in patients with CKD do not exist. Some markers are cleared by the kidney (osteocalcin, P1NP monomer and CTX); therefore, their application to ROD diagnostics is challenging. Prediction of ROD type can be improved if levels are at the extremes of their ranges. Combing PTH with BTMs may also provide diagnostic insight. Low vitamin D levels, and low levels of PTH in conjunction with high levels of BSAP have been reported to associate with osteomalacia.
Measurement of PTH and BTMs may have more applicability in the prediction of bone loss and fractures than in determining ROD-type27, 36, 40, 41, 55. For example, longitudinal studies in CKD patients have shown that high levels of PTH and BTMs predicted loss of cortical and trabecular bone and decreases in bone strength40, 41.
In a cross-sectional study of CKD patients, higher levels of PTH and BTMs were associated with lower cortical and trabecular density, thinner cortices and trabeculae36, and higher levels of BTMs discriminated fracture36. A longitudinal study of ESRD patients found that fracture risk was greater in patients with both low (<150 pg/mL) and high (>300 pg/mL) PTH levels, and with higher BSAP levels27. In a study of kidney transplant patients PTH levels ≥130 pg/mL 3-months after transplantation predicted fractures55. These data indicate that higher bone turnover, measured by PTH and BTMs, result in loss of bone density and microarchitecture and predict fracture. Longitudinal studies are needed to validate the findings of these small studies. Furthermore, longitudinal trends in BTMs have not been correlated against changes in bone histology, and correlations between changes in BTMs and changes in fracture risk have not been studied.
Can we non-invasively assess bone disease in CKD?
Non-invasive characterization of ROD needs to assess important aspects of bone quality (e.g., bone microarchitecture, mineralization and turnover), guide therapeutic choices, and predict clinical outcomes and responses to treatment. Studies have investigated how combining bone imaging with markers of bone turnover can assess bone disease severity and fracture status, important limitations need to be resolved. Non-invasive tools that identify osteomalacia and that accurately define bone turnover are lacking. Furthermore, although we know that low BMD and impaired cortical and trabecular microarchitecture predict fracture, it is not known whether increases in BMD and improvements in microarchitecture due to bone therapies predict decreases in fracture risk. In addition, the best intervals for bone disease monitoring has not been established. Thus, in the current era, the decision to treat and to monitor treatment response in a CKD patient managed with vitamin D analogs, or anti-resorptive or osteoanabolic agents may not be completely possible without a bone biopsy.
Biochemistries and DXA are non-invasive measures and provide insight into bone health, but neither approach directly tests bone material or mechanical properties. In recent years, efforts have been made to develop minimally invasive aproaches to directly probe bone material properties through the modification of traditional indentation material testing for in vivo use. Two devices, the BioDent (targeted for research) and OsteoProbe (targeted for clinical use), use small sharp probes inserted through the skin at the midshaft of the tibia to indent the bone surface56, 57. The OsteoProbe has shown promise in distinguishing patient populations of differing fracture risk or history58–62, but questions remain regarding the interpretation and meaning of the device’s outcome measure, “bone material strength index”, or BMSi63. It remains to be seen whether one or both devices will successfully be translated to the clinic and if they might provide new insight into bone quality differences in CKD patients.
Conclusion
ROD is a complex bone disorder that occurs in patients with kdiney disease and results in high risk of fracture. The best method to determine ROD type and overall bone health in CKD is bone biopsy. However, bone biopsy is not a practial diagnostic method due to its expense and lack of availability. In the office, DXA can classify fracture risk in CKD patients, but it cannot be used as a sole method either to assess bone quality or to inform therapeutic decisions. Markers of bone remodeling can provide information on turnover status and help determine whether treatment with an anabolic or anti-resorptive agent might be appropriate. Prospective randomized clinical trials are needed to best assess diagnosis and management of CKD-MBD.
Footnotes
Conflict of Interest
Thomas Nickolas and Erin McNerny declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest, published recently, have been highlighted as:
*Of importance
**Of major importance
- 1.Moe S, Drueke T, Cunningham J, Goodman W, Martin K, Olgaard K, Ott S, Sprague S, Lameire N, Eknoyan G, Kidney Disease: Improving Global, O Definition, evaluation, and classification of renal osteodystrophy: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO) Kidney Int. 2006;69:1945–1953. doi: 10.1038/sj.ki.5000414. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/16641930. [DOI] [PubMed] [Google Scholar]
- 2.Nickolas TL, McMahon DJ, Shane E. Relationship between Moderate to Severe Kidney Disease and Hip Fracture in the United States. J AmSocNephrol. 2006;17:3223–3232. doi: 10.1681/ASN.2005111194. Retrieved from PM:17005938. [DOI] [PubMed] [Google Scholar]
- 3.Alem AM, Sherrard DJ, Gillen DL, Weiss NS, Beresford SA, Heckbert SR, Wong C, Stehman-Breen C. Increased risk of hip fracture among patients with end-stage renal disease. Kidney Int. 2000;58:396–399. doi: 10.1046/j.1523-1755.2000.00178.x. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10886587. [DOI] [PubMed] [Google Scholar]
- 4.Dooley AC, Weiss NS, Kestenbaum B. Increased risk of hip fracture among men with CKD. Am J Kidney Dis. 2008;51:38–44. doi: 10.1053/j.ajkd.2007.08.019. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18155531. [DOI] [PubMed] [Google Scholar]
- 5*.Naylor KL, McArthur E, Leslie WD, Fraser LA, Jamal SA, Cadarette SM, Pouget JG, Lok CE, Hodsman AB, Adachi JD, Garg AX. The three-year incidence of fracture in chronic kidney disease. Kidney Int. 2014 doi: 10.1038/ki.2013.547. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/24429401. This study uses administrative data from Canada to describe fracture incidence stratified by CKD stage and gender. It demonstrates that fracture rates are higher in patients with more severe kidney disease. [DOI] [PubMed]
- 6.Isakova T, Craven TE, Scialla JJ, Nickolas TL, Schnall A, Barzilay J, Schwartz AV, Action to Control Cardiovascular Risk in Diabetes, T Change in estimated glomerular filtration rate and fracture risk in the Action to Control Cardiovascular Risk in Diabetes Trial. Bone. 2015;78:23–27. doi: 10.1016/j.bone.2015.04.037. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/25937184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arneson TJ, Li S, Liu J, Kilpatrick RD, Newsome BB, St Peter WL. Trends in hip fracture rates in US hemodialysis patients, 1993–2010. Am J Kidney Dis. 2013;62:747–754. doi: 10.1053/j.ajkd.2013.02.368. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/23631997. [DOI] [PubMed] [Google Scholar]
- 8.Wagner J, Jhaveri KD, Rosen L, Sunday S, Mathew AT, Fishbane S. Increased bone fractures among elderly United States hemodialysis patients. Nephrol Dial Transplant. 2014;29:146–151. doi: 10.1093/ndt/gft352. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/24078333. [DOI] [PubMed] [Google Scholar]
- 9.Nikkel LE, Hollenbeak CS, Fox EJ, Uemura T, Ghahramani N. Risk of fractures after renal transplantation in the United States. Transplantation. 2009;87:1846–1851. doi: 10.1097/TP.0b013e3181a6bbda. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/19543063. [DOI] [PubMed] [Google Scholar]
- 10.Alem AM, Sherrard DJ, Gillen DL, Weiss NS, Beresford SA, Heckbert SR, Wong C, Stehman-Breen C. Increased risk of hip fracture among patients with end-stage renal disease. Kidney International. 2000;58:396–399. doi: 10.1046/j.1523-1755.2000.00178.x. Retrieved from http://www.blackwell-synergy.com/loi/kid. [DOI] [PubMed] [Google Scholar]
- 11.Ball AM, Gillen DL, Sherrard D, Weiss NS, Emerson SS, Seliger SL, Kestenbaum BR, Stehman-Breen C. Risk of Hip Fracture Among Dialysis and Renal Transplant Recipients. JAMA: The Journal of the American Medical Association. 2002;288:3014–3018. doi: 10.1001/jama.288.23.3014. Retrieved from http://jama.ama-assn.org/cgi/content/abstract/288/23/3014. [DOI] [PubMed] [Google Scholar]
- 12.Vautour LM, Melton LJ, 3rd, Clarke BL, Achenbach SJ, Oberg AL, McCarthy JT. Long-term fracture risk following renal transplantation: a population-based study. Osteoporos Int. 2004;15:160–167. doi: 10.1007/s00198-003-1532-y. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/14666400. [DOI] [PubMed] [Google Scholar]
- 13.Perrin P, Kiener C, Javier RM, Braun L, Cognard N, Gautier-Vargas G, Heibel F, Muller C, Olagne J, Moulin B, Caillard S. Recent changes in chronic kidney disease-mineral and bone disorders (CKD-MBD) and associated fractures after kidney transplantation. Transplantation. 2016 doi: 10.1097/TP.0000000000001449. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/27547867. [DOI] [PubMed]
- 14.Mittalhenkle A, Gillen DL, Stehman-Breen CO. Increased risk of mortality associated with hip fracture in the dialysis population. AmJ Kidney Dis. 2004;44:672–679. Retrieved from PM:15384018. [PubMed] [Google Scholar]
- 15.Abbott KC, Oglesby RJ, Hypolite IO, Kirk AD, Ko CW, Welch PG, Agodoa LY, Duncan WE. Hospitalizations for fractures after renal transplantation in the United States. Ann Epidemiol. 2001;11:450–457. doi: 10.1016/s1047-2797(01)00226-5. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11557176. [DOI] [PubMed] [Google Scholar]
- 16.Tentori F, McCullough K, Kilpatrick RD, Bradbury BD, Robinson BM, Kerr PG, Pisoni RL. High rates of death and hospitalization follow bone fracture among hemodialysis patients. Kidney Int. 2014;85:166–173. doi: 10.1038/ki.2013.279. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/23903367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim SM, Long J, Montez-Rath M, Leonard M, Chertow GM. Hip Fracture in Patients with Non-Dialysis-Requiring Chronic Kidney Disease. Journal of Bone and Mineral Research. 2016:n/a–n/a. doi: 10.1002/jbmr.2862. Retrieved from http://dx.doi.org/10.1002/jbmr.2862. [DOI] [PubMed]
- 18.Nair SS, Mitani AA, Goldstein BA, Chertow GM, Lowenberg DW, Winkelmayer WC. Temporal trends in the incidence, treatment, and outcomes of hip fracture in older patients initiating dialysis in the United States. Clin J Am Soc Nephrol. 2013;8:1336–1342. doi: 10.2215/CJN.10901012. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/23660182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Burr DB. The complex relationship between bone remodeling and the physical and material properties of bone. Osteoporosis International. 2015;26:845. doi: 10.1007/s00198-014-2970-4. [DOI] [PubMed] [Google Scholar]
- 20.Bala Y, Seeman E. Bone’s Material Constituents and their Contribution to Bone Strength in Health, Disease, and Treatment. Calcified tissue international. 2015;97:308–326. doi: 10.1007/s00223-015-9971-y. [DOI] [PubMed] [Google Scholar]
- 21.Schaffler MB, Choi K, Milgrom C. Aging and matrix microdamage accumulation in human compact bone. Bone. 1995;17:521–525. doi: 10.1016/8756-3282(95)00370-3. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8835305. [DOI] [PubMed] [Google Scholar]
- 22.Reilly GC, Currey JD. The effects of damage and microcracking on the impact strength of bone. Journal of biomechanics. 2000;33:337–343. doi: 10.1016/s0021-9290(99)00167-0. [DOI] [PubMed] [Google Scholar]
- 23.Vashishth D, Gibson G, Khoury J, Schaffler M, Kimura J, Fyhrie DP. Influence of nonenzymatic glycation on biomechanical properties of cortical bone. Bone. 2001;28:195–201. doi: 10.1016/s8756-3282(00)00434-8. [DOI] [PubMed] [Google Scholar]
- 24.Akkus O, Adar F, Schaffler MB. Age-related changes in physicochemical properties of mineral crystals are related to impaired mechanical function of cortical bone. Bone. 2004;34:443–453. doi: 10.1016/j.bone.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 25.Yenchek RH, Ix JH, Shlipak MG, Bauer DC, Rianon NJ, Kritchevsky SB, Harris TB, Newman AB, Cauley JA, Fried LF. Bone mineral density and fracture risk in older individuals with CKD. Clin J Am Soc Nephrol. 2012;7:1130–1136. doi: 10.2215/CJN.12871211. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=22516286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.West SL, Lok CE, Langsetmo L, Cheung AM, Szabo E, Pearce D, Fusaro M, Wald R, Weinstein J, Jamal SA. Bone mineral density predicts fractures in chronic kidney disease. J Bone Miner Res. 2015;30:913–919. doi: 10.1002/jbmr.2406. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/25400209. [DOI] [PubMed] [Google Scholar]
- 27.Iimori S, Mori Y, Akita W, Kuyama T, Takada S, Asai T, Kuwahara M, Sasaki S, Tsukamoto Y. Diagnostic usefulness of bone mineral density and biochemical markers of bone turnover in predicting fracture in CKD stage 5D patients–a single-center cohort study. Nephrol Dial Transplant. 2012;27:345–351. doi: 10.1093/ndt/gfr317. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/21652550. [DOI] [PubMed] [Google Scholar]
- 28.Akaberi S, Simonsen O, Lindergard B, Nyberg G. Can DXA predict fractures in renal transplant patients? Am J Transplant. 2008;8:2647–2651. doi: 10.1111/j.1600-6143.2008.02423.x. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/18853956. [DOI] [PubMed] [Google Scholar]
- 29.Jamal SA, Gilbert J, Gordon C, Bauer DC. Cortical pQCT measures are associated with fractures in dialysis patients. J Bone MinerRes. 2006;21:543–548. doi: 10.1359/jbmr.060105. Retrieved from PM:16598374. [DOI] [PubMed] [Google Scholar]
- 30.Leonard MB. A structural approach to skeletal fragility in chronic kidney disease. Seminars in Nephrology. 2009;29:133–143. doi: 10.1016/j.semnephrol.2009.01.006. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/19371804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Denburg MR, Tsampalieros AK, de Boer IH, Shults J, Kalkwarf HJ, Zemel BS, Foerster D, Stokes D, Leonard MB. Mineral metabolism and cortical volumetric bone mineral density in childhood chronic kidney disease. The Journal of clinical endocrinology and metabolism. 2013;98:1930–1938. doi: 10.1210/jc.2012-4188. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/23547048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nishiyama KK, Macdonald HM, Buie HR, Hanley DA, Boyd SK. Postmenopausal women with osteopenia have higher cortical porosity and thinner cortices at the distal radius and tibia than women with normal aBMD: an in vivo HR-pQCT study. J Bone Miner Res. 2010;25:882–890. doi: 10.1359/jbmr.091020. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/19839766. [DOI] [PubMed] [Google Scholar]
- 33.Nishiyama KK, Macdonald HM, Hanley DA, Boyd SK. Women with previous fragility fractures can be classified based on bone microarchitecture and finite element analysis measured with HR-pQCT. Osteoporos Int. 2013;24:1733–1740. doi: 10.1007/s00198-012-2160-1. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/23179565. [DOI] [PubMed] [Google Scholar]
- 34.Liu XS, Stein EM, Zhou B, Zhang CA, Nickolas TL, Cohen A, Thomas V, McMahon DJ, Cosman F, Nieves J, Shane E, Guo XE. Individual trabecula segmentation (ITS)-based morphological analyses and microfinite element analysis of HR-pQCT images discriminate postmenopausal fragility fractures independent of DXA measurements. J Bone Miner Res. 2012;27:263–272. doi: 10.1002/jbmr.562. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/22072446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nickolas TL, Stein E, Cohen A, Thomas V, Staron RB, McMahon DJ, Leonard MB, Shane E. Bone mass and microarchitecture in CKD patients with fracture. J Am Soc Nephrol. 2010;21:1371–1380. doi: 10.1681/ASN.2009121208. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/20395370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36*.Nickolas TL, Cremers S, Zhang A, Thomas V, Stein E, Cohen A, Chauncey R, Nikkel L, Yin MT, Liu XS, Boutroy S, Staron RB, Leonard MB, McMahon DJ, Dworakowski E, Shane E. Discriminants of prevalent fractures in chronic kidney disease. J Am Soc Nephrol. 2011;22:1560–1572. doi: 10.1681/ASN.2010121275. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/21784896. This cross sectional study in patients with moderate to severe CKD demonstrated that bone imaging by DXA and higher levels of bone turnover markers discriminated fractures, and that discrimination by DXA was improved by combining measures of bone mineral density with bone turnover markers. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jamal S, Cheung AM, West S, Lok C. Bone mineral density by DXA and HR pQCT can discriminate fracture status in men and women with stages 3 to 5 chronic kidney disease. Osteoporos Int. 2012;23:2805–2813. doi: 10.1007/s00198-012-1908-y. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/22297732. [DOI] [PubMed] [Google Scholar]
- 38.Cejka D, Patsch JM, Weber M, Diarra D, Riegersperger M, Kikic Z, Krestan C, Schueller-Weidekamm C, Kainberger F, Haas M. Bone microarchitecture in hemodialysis patients assessed by HR-pQCT. Clin J Am Soc Nephrol. 2011;6:2264–2271. doi: 10.2215/CJN.09711010. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/21737853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Trombetti A, Stoermann C, Chevalley T, Van Rietbergen B, Herrmann FR, Martin PY, Rizzoli R. Alterations of bone microstructure and strength in end-stage renal failure. Osteoporos Int. 2012 doi: 10.1007/s00198-012-2133-4. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/23100118. [DOI] [PubMed]
- 40*.Nickolas TL, Stein EM, Dworakowski E, Nishiyama KK, Komandah-Kosseh M, Zhang CA, McMahon DJ, Liu XS, Boutroy S, Cremers S, Shane E. Rapid cortical bone loss in patients with chronic kidney disease. J Bone Miner Res. 2013;28:1811–1820. doi: 10.1002/jbmr.1916. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/23456850. This propsective study in patients demonstarted that in patients with moderate to severe CKD bone loss occurred in the cortical rather than the trabecular compartments, and that elevated levels of PTH and bone turnover markers predicted the severity of cortical losses. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Iyer SNL, Nishiyama K, Dworakowski E, Cremers S, Zhang A, McMahon DJ, Boutroy S, Liu XS, Ratner L, Cohen D, Guo XE, Shane E, Nickolas TL. Kidney transplantation with early corticosteroid withdrawal: paradoxical effects at the central and peripheral skeleton. J Am Soc Nephrol. 2014 doi: 10.1681/ASN.2013080851. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Boutroy SNT, Stein EM, Cohen A, Shane E. ASN. San Diego, CA: 2010. Impaired cortical bone in predialysis CKD patients is even more marked in those with fragility fracture. [Google Scholar]
- 43.Parfitt AM. A structural approach to renal bone disease. J Bone Miner Res. 1998;13:1213–1220. doi: 10.1359/jbmr.1998.13.8.1213. [DOI] [PubMed] [Google Scholar]
- 44.Jee WS. The past, present, and future of bone morphometry: its contribution to an improved understanding of bone biology. Journal of bone and mineral metabolism. 2005;23(Suppl: 1) doi: 10.1007/BF03026316. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=15984407. [DOI] [PubMed] [Google Scholar]
- 45.Jamal SA, Ljunggren O, Stehman-Breen C, Cummings SR, McClung MR, Goemaere S, Ebeling PR, Franek E, Yang YC, Egbuna OI, Boonen S, Miller PD. Effects of denosumab on fracture and bone mineral density by level of kidney function. J Bone Miner Res. 2011;26:1829–1835. doi: 10.1002/jbmr.403. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/21491487. [DOI] [PubMed] [Google Scholar]
- 46.Miller PD, Schwartz EN, Chen P, Misurski DA, Krege JH. Teriparatide in postmenopausal women with osteoporosis and mild or moderate renal impairment. Osteoporos Int. 2007;18:59–68. doi: 10.1007/s00198-006-0189-8. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17013567. [DOI] [PubMed] [Google Scholar]
- 47.Miller PD, Roux C, Boonen S, Barton IP, Dunlap LE, Burgio DE. Safety and efficacy of risedronate in patients with age-related reduced renal function as estimated by the cockcroft and gault method: a pooled analysis of nine clinical trials. J Bone MinerRes. 2005;20:2105–2115. doi: 10.1359/JBMR.050817. Retrieved from PM:16294264. [DOI] [PubMed] [Google Scholar]
- 48.Couttenye MM, D’Haese PC, Van Hoof VO, Lemoniatou E, Goodman W, Verpooten GA, De Broe ME. Low serum levels of alkaline phosphatase of bone origin: a good marker of adynamic bone disease in haemodialysis patients. Nephrol Dial Transplant. 1996;11:1065–1072. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8671970. [PubMed] [Google Scholar]
- 49.Bervoets AR, Spasovski GB, Behets GJ, Dams G, Polenakovic MH, Zafirovska K, Van HV, De Broe ME, D’Haese PC. Useful biochemical markers for diagnosing renal osteodystrophy in predialysis end-stage renal failure patients. AmJ Kidney Dis. 2003;41:997–1007. doi: 10.1016/s0272-6386(03)00197-5. Retrieved from PM:12722034. [DOI] [PubMed] [Google Scholar]
- 50.Coen G, Ballanti P, Bonucci E, Calabria S, Centorrino M, Fassino V, Manni M, Mantella D, Mazzaferro S, Napoletano I, Sardella D, Taggi F. Bone markers in the diagnosis of low turnover osteodystrophy in haemodialysis patients. NephrolDialTransplant. 1998;13:2294–2302. doi: 10.1093/ndt/13.9.2294. Retrieved from PM:9761512. [DOI] [PubMed] [Google Scholar]
- 51.Lehmann G, Ott U, Kaemmerer D, Schuetze J, Wolf G. Bone histomorphometry and biochemical markers of bone turnover in patients with chronic kidney disease Stages 3–5. Clin Nephrol. 2008;70:296–305. doi: 10.5414/cnp70296. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/18826854. [DOI] [PubMed] [Google Scholar]
- 52.Lehmann G, Stein G, Huller M, Schemer R, Ramakrishnan K, Goodman WG. Specific measurement of PTH (1–84) in various forms of renal osteodystrophy (ROD) as assessed by bone histomorphometry. Kidney Int. 2005;68:1206–1214. doi: 10.1111/j.1523-1755.2005.00513.x. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/16105052. [DOI] [PubMed] [Google Scholar]
- 53.Herberth J, Branscum AJ, Mawad H, Cantor T, Monier-Faugere MC, Malluche HH. Intact PTH combined with the PTH ratio for diagnosis of bone turnover in dialysis patients: a diagnostic test study. Am J Kidney Dis. 2010;55:897–906. doi: 10.1053/j.ajkd.2009.12.041. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/20347512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sprague SM, Bellorin-Font E, Jorgetti V, Carvalho AB, Malluche HH, Ferreira A, D’Haese PC, Drueke TB, Du H, Manley T, Rojas E, Moe SM. Diagnostic Accuracy of Bone Turnover Markers and Bone Histology in Patients With CKD Treated by Dialysis. Am J Kidney Dis. 2015 doi: 10.1053/j.ajkd.2015.06.023. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/26321176. [DOI] [PubMed]
- 55.Perrin P, Caillard S, Javier RM, Braun L, Heibel F, Borni-Duval C, Muller C, Olagne J, Moulin B. Persistent hyperparathyroidism is a major risk factor for fractures in the five years after kidney transplantation. Am J Transplant. 2013;13:2653–2663. doi: 10.1111/ajt.12425. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/24034142. [DOI] [PubMed] [Google Scholar]
- 56.Diez-Perez A, Guerri R, Nogues X, Caceres E, Pena MJ, Mellibovsky L, Randall C, Bridges D, Weaver JC, Proctor A, Brimer D, Koester KJ, Ritchie RO, Hansma PK. Microindentation for in vivo measurement of bone tissue mechanical properties in humans. J Bone Miner Res. 2010;25:1877–1885. doi: 10.1002/jbmr.73. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/20200991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bridges D, Randall C, Hansma PK. A new device for performing reference point indentation without a reference probe. Rev Sci Instrum. 2012;83:044301. doi: 10.1063/1.3693085. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/22559552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Farr JN, Drake MT, Amin S, Melton LJ, 3rd, McCready LK, Khosla S. In vivo assessment of bone quality in postmenopausal women with type 2 diabetes. J Bone Miner Res. 2014;29:787–795. doi: 10.1002/jbmr.2106. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/24123088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Furst JR, Bandeira LC, Fan WW, Agarwal S, Nishiyama KK, McMahon DJ, Dworakowski E, Jiang H, Silverberg SJ, Rubin MR. Advanced Glycation Endproducts and Bone Material Strength in Type 2 Diabetes. The Journal of clinical endocrinology and metabolism. 2016;101:2502–2510. doi: 10.1210/jc.2016-1437. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/27115060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mellibovsky L, Prieto-Alhambra D, Mellibovsky F, Guerri-Fernandez R, Nogues X, Randall C, Hansma PK, Diez-Perez A. Bone Tissue Properties Measurement by Reference Point Indentation in Glucocorticoid-Induced Osteoporosis. J Bone Miner Res. 2015;30:1651–1656. doi: 10.1002/jbmr.2497. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/25736591. [DOI] [PubMed] [Google Scholar]
- 61.Malgo F, Hamdy NA, Papapoulos SE, Appelman-Dijkstra NM. Bone material strength as measured by microindentation in vivo is decreased in patients with fragility fractures independently of bone mineral density. The Journal of clinical endocrinology and metabolism. 2015;100:2039–2045. doi: 10.1210/jc.2014-4346. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/25768670. [DOI] [PubMed] [Google Scholar]
- 62.Duarte Sosa D, Vilaplana L, Guerri R, Nogues X, Wang-Fagerland M, Diez-Perez A, E FE. Are the High Hip Fracture Rates Among Norwegian Women Explained by Impaired Bone Material Properties? J Bone Miner Res. 2015;30:1784–1789. doi: 10.1002/jbmr.2537. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/25900016. [DOI] [PubMed] [Google Scholar]
- 63.Allen MR, McNerny EMB, Organ JM, Wallace JM. True Gold or Pyrite: A Review of Reference Point Indentation for Assessing Bone Mechanical Properties In Vivo. Journal of Bone and Mineral Research. 2015;30:1539–1550. doi: 10.1002/jbmr.2603. Retrieved from http://dx.doi.org/10.1002/jbmr.2603. [DOI] [PMC free article] [PubMed] [Google Scholar]


