Significance
The prevalence of obesity reflects a major public health challenge in the United States and many other parts of the world. The current studies adopt a life history theory (LHT) perspective to explain in part the root causes of obesity. This research identifies exposure to unpredictable environments during childhood as a distal factor that contributes to obesity in adulthood. Exposure to childhood unpredictability is linked to the development of a fast life-history strategy, one marked by impulsivity and a focus on short-term goals. LHT provides a valuable conceptual framework for understanding the behavioral mechanisms that underlie dysregulated patterns of eating and, ultimately, the development of weight-management problems in adulthood. This research also provides insight into pathways for obesity prevention.
Keywords: evolutionary psychology, evolutionary medicine, life history theory, health behavior, obesity
Abstract
The association between low socioeconomic status (SES) and obesity is well documented. In the current research, a life history theory (LHT) framework provided an explanation for this association. Derived from evolutionary behavioral science, LHT emphasizes how variability in exposure to unpredictability during childhood gives rise to individual differences in a range of social psychological processes across the life course. Consistent with previous LHT research, the current findings suggest that exposure to unpredictability during childhood (a characteristic common to low SES environments) is associated with the adoption of a fast life-history strategy, one marked by impulsivity and a focus on short-term goals. We demonstrate that a fast life-history strategy, in turn, was associated with dysregulated weight-management behaviors (i.e., eating even in the absence of hunger), which were predictive of having a high body mass index (BMI) and being obese. In both studies, findings held while controlling for participants’ current socioeconomic status, suggesting that obesity is rooted in childhood experiences. A serial mediation model in study 2 confirmed that effects of childhood SES on adult BMI and obesity can be explained in part by exposure to unpredictability, the adoption of a fast life-history strategy, and dysregulated-eating behaviors. These findings suggest that weight problems in adulthood may be rooted partially in early childhood exposure to unpredictable events and environments. LHT provides a valuable explanatory framework for understanding the root causes of obesity.
More than one third of American adults and about one third of children and adolescents are currently obese, and an even greater number are overweight (1). Obesity is a risk factor for many negative health outcomes including heart disease, type 2 diabetes, hypertension, liver disease, cancer, and stroke (2). Consequently, identifying the behavioral factors that increase obesity is a key goal for research.
This article provides an evolutionary perspective on obesity by using a life history theory (LHT) approach. Derived from evolutionary biology, LHT suggests that adaptive psychological processes are calibrated early in life to help people maximize their reproductive potential across the lifespan, given the contingencies they encounter in their local childhood environment (3, 4).
Although existing epidemiological research has used a life-course perspective to understand how childhood psychosocial variables contribute to adult disease (5), no studies to our knowledge have adopted a LHT approach. Recognizing developmental factors suggested by LHT not only enhances our theoretical understanding of obesity but also generates insight into possible interventions.
Work in the LHT tradition finds that the degree of unpredictability in an organism’s early-life environment influences behavior in a variety of domains throughout the life course (6). LHT is rooted in the idea that organisms have a finite energy budget that must be allocated in a way that maximizes overall reproductive fitness. LHT emphasizes that an organism’s fitness-maximizing strategy is adaptively calibrated to the level of unpredictability it encounters early in its development. A high level of unpredictability signals that the future is uncertain, increasing the extent to which the organism invests in short-term pursuits tied to immediate reproduction. A low level of unpredictability signals that the future is relatively certain and that the organism can afford to adopt a strategy marked by a longer time horizon and greater investment in somatic effort over the long term. These responses to early developmental unpredictability are referred to as “fast” and “slow” life-history strategies, respectively. Hence, life-history strategies vary on a continuum from fast to slow and serve to optimize an organism’s reproductive success given the level of unpredictability encountered early in development.
Faster life-history strategies are characterized by behaviors that increase immediate reproduction, such as having more sexual partners earlier in life and a larger number of total offspring and displaying an orientation toward impulsivity, risk-taking, and short-term rewards (7, 8). Conversely, slower life-history strategies are characterized by behaviors that emphasize long-term investment in fewer offspring, such as delaying reproduction until later in life, having fewer sexual partners, and delaying gratification in favor of long-term rewards (9).
LHT provides insight into the psychological processes underlying obesity. Growing up in an environment characterized by unpredictability means not knowing when resources will be available in the future and so activates psychological processes that promote the consumption of resources when they are immediately available. This mindset may lead people to consume food when it is available, regardless of whether they currently require the nourishment. If the availability of food in the future is uncertain, it may behoove one to consume as much as possible when one has access to it. This behavior would have been highly functional in ancestral times, when attaining enough food was a persistent challenge (10).
The potential role of life-history strategies in obesity is indicated by the well-known association between low socioeconomic status (SES) and obesity (11–13). Conditions associated with low SES include uncertainty and resource scarcity, reflecting the type of harsh and unpredictable conditions that promote the development of fast life-history strategies. Indeed, recent work showed that low childhood SES is associated with a tendency among adults to eat even when nourishment is not currently needed (14; also see ref. 15). Although such behavior may have been adaptive in ancestral environments, it sets the stage for dysfunctional patterns of overeating in modern environments. Moreover, even when individuals from low-SES environments improve their circumstances and transition into more stable, higher-SES environments, their faster life-history strategy may persist, promoting a continued tendency to eat in the absence of current energy needs.
Despite recent laboratory evidence documenting overeating among low-SES people (14), we are aware of no previous studies examining the role of LHT in predicting a tendency to be overweight or obese. Moreover, although previous research is consistent with hypotheses derived from LHT, studies often have used low SES as a proxy for childhood unpredictability and have fallen short of directly examining the role of unpredictable childhood environments. The current research addresses these important gaps in the literature.
Study 1 leveraged data from a longitudinal study of an ethnically and racially diverse sample of 226 individuals (113 married couples) to examine the association between childhood SES and participants’ weight and obesity status in adulthood. We predicted that lower childhood SES would be associated with higher weight and a greater likelihood of being obese in adulthood. Study 2 used a large online sample (n = 400) to test a serial mediation model accounting for the associations among childhood SES, childhood unpredictability, life-history strategy, the presence of dysregulated eating behaviors, and obesity. That study also allowed us to test a critical theoretical assumption that to our knowledge has been left untested—that effects of low SES on weight problems are caused in part by exposure to unpredictability in childhood.
In both studies, we conducted analyses controlling for current SES. These analyses allowed us to isolate the role of childhood experiences and rule out the possibility that weight problems in adulthood simply reflect low current levels of SES. Other studies have shown that the associations between childhood SES and many chronic health conditions are eliminated when controlling for current SES (16). The current research sought to show that current SES does not account for the link between childhood unpredictability and adult weight.
Study 1: Results and Interim Discussion
Before testing our primary prediction, we first used growth-curve modeling to estimate participants’ body mass index (BMI) trajectories. We estimated the following first level of a three-level model using the Hierarchical Linear Modeling 7 computer program (17):
| [1] |
in which (i) t indexes time, i indexes individuals, and c indexes couples; (ii) time represents the wave of assessment and was coded from 0 to 6 (so that the intercept represented initial BMI at the start of marriage); (iii) the autocorrelation from repeated assessments was controlled in level 2, and the shared variance between husbands’ and wives’ data was controlled in level 3; and (iv) all level 2 estimates and the level 3 intercept were allowed to vary randomly. We used restricted maximum likelihood estimation and placed no restrictions on the autoregressive error structures.
Both men and women reported mean BMI levels that fell in the overweight range at the beginning of the study (for men, π = 28.02, SE = 0.68; for women, π = 27.50, SE = 0.78) and, on average, experienced significant increases in BMI over the three-and-a-half-year study (for men, π = 0.25, SE = 0.06; for women, π = 0.28, SE = 0.06). Men and women reported similar initial BMIs [b = −0.52, SE = 0.79, t(78) = −0.65, P = 0.515] and similar increases in BMI over the course of the study [b = 0.03, SE = 0.09, t(78) = 0.33, P = 0.740].
Notably, we observed substantial between-subjects variability in both initial BMI [χ2 (2) = 481.99, P < 0.001] and change in BMI [χ2 (2) = 10.41, P = 0.006]. The primary analysis examined whether childhood family income partially accounted for this variability. We predicted that individuals whose families had relatively few financial resources during childhood (controlling for current income) would report higher levels of BMI and steeper increases in BMI over time. To test these predictions, parameters estimated in Eq. 1 (initial BMI and change in BMI) were regressed onto childhood family income in level 2. We controlled (i) participants’ current income (grand-centered) at level 1 to isolate the effect of childhood family income and (ii) a dummy code of whether the childhood income variable was assessed at baseline (coded 0) or at time 4/time 6 (coded 1) at the level-2 intercept (Table 1).
Table 1.
Relationship between childhood family income and BMI
| Variable | Coefficient | Standard error | P value | Effect size, r |
| Intercept | 27.85 | 0.63 | ||
| Time of income assessment | −0.80 | 1.00 | 0.424 | 0.09 |
| Childhood family income | −0.01 | 0.00 | 0.014 | 0.28 |
| Time | 0.25 | 0.04 | <0.001 | 0.54 |
| Childhood family income | −0.00 | 0.00 | 0.074 | 0.20 |
| Current income | 0.00 | 0.00 | 0.429 | 0.07 |
Level 1 coefficients are πs; level 2 coefficients are bs; df = 102 for intercept; df = 77 for time, time of income assessment, and childhood family income variables; df = 135 for current income variable.
Consistent with predictions, individuals whose families had less (compared with more) money during childhood had higher BMIs at the start of their first marriages. Further, childhood family income was marginally associated with changes in BMI over time, such that those from lower-income childhoods reported greater increases in BMI over the 3.5 y of the study. Notably, these associations (i) were not moderated by participant sex [for initial BMI: b = −0.30, SE = 0.69, t(73) = −0.43, P = 0.667; for change in BMI: b = 0.16, SE = 0.17, t(73) = 0.92, P = 0.360] and (ii) remained unchanged when we no longer included participants’ current income as a level 1 covariate or the dummy code for time of childhood income assessment as a level 2 covariate [for initial BMI: b = −0.01, SE = 0.00, t(78) = −2.44, P = 0.017; for change in BMI: b = −0.00, SE = 0.00, t(78) = −1.84, P = 0.070].
We conducted similar analyses that replaced BMI as the dependent variable with a dichotomous variable reflecting participants’ obesity status. Results mirrored those for BMI scores. Childhood family income was associated with obesity status at study initiation [b = −0.00, SE = 0.00, t(77) = −2.00, P = 0.049]. Although childhood family income was unassociated with changes in participants’ obesity status over the course of the study [β = −0.00, SE = 0.00, t(77) = −0.94, P = 0.351], childhood family income remained associated with participants’ obesity status at the end of the study [b = −0.00, SE = 0.00, t(77) = −3.38, P = 0.001]. That is, individuals whose families had less money during childhood were more likely to be obese at the start of their first marriages, and this difference remained 3.5 y later. These intercept and slope associations (i) were not moderated by participant sex [for initial obesity status: b = −0.18, SE = 0.30, t(73) = −0.59, P = 0.557; for change in obesity status: b = −0.09, SE = 0.14, t(73) = −0.67, P = 0.507] and (ii) remained unchanged when we no longer included participants’ current income as a level 1 covariate or the dummy code for time of childhood income assessment as a level 2 covariate [for initial obesity status: b = −0.01, SE = 0.00, t(78) = −1.95, P = 0.054; for change in obesity status: b = −0.00, SE = 0.00, t(78) = −0.99, P = 0.324].
Thus, in a demographically diverse sample, childhood family income predicted participants’ weight and obesity status in adulthood. Moreover, childhood family income predicted increases in BMI over 3.5 y. Importantly, these associations emerged independent of current income, indicating that they do not simply reflect the well-known association between current SES and obesity. Rather, findings are consistent with the hypothesis that early childhood experiences calibrate behavior such that those exposed to unpredictable environments are more likely than those from predictable environments to be obese in adulthood.
Several limitations of this study warrant caution, however. First, rather than measuring childhood unpredictability directly, we used the measure of childhood SES. Although the two constructs are related, a more rigorous test would include a measure of childhood unpredictability. In fact, our theoretical framework suggests a measure of unpredictability should account for the association between childhood SES and weight/obesity. Second, we did not directly examine the role of life-history strategy, instead basing our interpretation on the assumption that lower SES promotes a faster life-history strategy (7). Third, we did not examine the role of dysregulated-eating behaviors, which presumably serve as proximate causes of obesity in those pursuing a fast life-history strategy. Study 2 addressed each of these limitations.
Study 2 Results
Table 2 presents zero-order correlations among all variables.
Table 2.
Zero-order correlations among key variables in study 2
| Key variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| 1. Childhood SES | — | ||||||
| 2. Current SES | 0.23*** | — | |||||
| 3. Unpredictability | −0.29*** | −0.06 | — | ||||
| 4. Life-history strategy | 0.10* | 0.29*** | −0.32*** | — | |||
| 5. Dysregulated eating | −0.04 | −0.09+ | 0.004 | −0.13** | — | ||
| 6. BMI | −0.13* | −0.14** | 0.05 | −0.04 | 0.32*** | — | |
| 7. Obesity | −0.14** | −0.18*** | 0.09+ | −0.09+ | 0.31*** | 0.78*** | — |
Significance: ***P < 0.001; **P < 0.01; *P < 0.05; +P < 0.10.
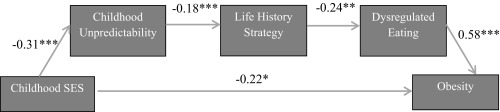
To assess the predicted relationships among childhood SES, childhood unpredictability, life-history strategy, dysregulated eating, and obesity status, we used the Process macro (18) within a multiple regression framework to conduct a serial mediation analysis (Fig. 1). We entered childhood unpredictability, life-history strategy, and dysregulated-eating behavior as putative mediators of the relationship between SES and obesity. (Similar analyses treating BMI as the outcome variable closely mirrored those reported here and can be found in SI Study 2, Mediational Model of BMI.) As predicted, lower childhood SES was associated with significantly higher unpredictability [b = −0.31, t(398) = −6.11, P < 0.001]. We also observed the expected association between greater childhood unpredictability and a faster life-history strategy [b = −0.18, t(397) = −6.42, P < 0.001]. Consistent with the idea that childhood unpredictability accounts for the effect of childhood SES on life-history strategy, there was no direct effect of childhood SES on life-history strategy [b = 0.003, t(397) = 0.10, P = 0.917]. Next, entering childhood SES, childhood unpredictability, and life-history strategy as predictors of dysregulated eating confirmed that a faster life-history strategy was associated with more dysregulated eating [b = −0.24, t(396) = −2.80, P = 0.005]; consistent with the idea that life-history strategy is the more proximal predictor of dysregulated eating, neither childhood SES [b = −0.04, t(396) = −0.86, P = 0.392] nor childhood unpredictability [b = −0.05, t(396) = −1.03, P = 0.302] had a direct effect on dysregulated eating. Finally, entering childhood SES, childhood unpredictability, life-history strategy, and dysregulated eating as predictors of obesity revealed an association between dysregulated eating and obesity [b = 0.58, z = 5.71, P < 0.001] and a direct effect of childhood SES [b = −0.22, z = −2.27, P = 0.023]; consistent with the idea that dysregulated eating is the more proximal predictor of obesity, neither life-history strategy [b = −0.12, z = −0.72, P = 0.470] nor childhood unpredictability [b = 0.90, z = 0.98, P = 0.325] had a direct effect on obesity.
Fig. 1.
Study 2: Path model of a serial mediation analysis linking childhood SES to obesity via childhood unpredictability, life-history strategy, and dysregulated-eating behaviors. Numbers refer to unstandardized regression weights. *P < 0.05, **P < 0.01, ***P < 0.001.
To provide a direct test of serial mediation (i.e., the indirect effect of childhood SES on obesity, as mediated through childhood unpredictability, life-history strategy, and dysregulated eating, respectively), a bootstrapping analysis with 5,000 resamples indicated a significant indirect effect, with a point estimate of −0.008 and a 95% bias-corrected CI of (−0.020, −0.002). The data thus are consistent with the hypothesis that participants who experienced lower childhood SES experienced greater levels of childhood unpredictability, which was associated with a faster life-history strategy, which in turn was associated with dysregulated eating, which was ultimately associated with an increased likelihood of obesity in adulthood.
We tested three alternative models, none of which demonstrated good fit to the data. First, childhood SES was not indirectly associated with likelihood of obesity in adulthood merely through dysregulated-eating behaviors [point estimate = −0.025, 95% bootstrap CI = (−0.094, 0.037)]. Second, childhood SES was not indirectly associated with likelihood of obesity merely through childhood unpredictability [point estimate = −0.027, 95% bootstrap CI = (−0.105, 0.023)]. Third, and finally, childhood SES was not indirectly associated with likelihood of obesity merely through life-history strategy [point estimate = −0.0004, 95% bootstrap CI = (−0.015, 0.010)]. These null effects are important because they help rule out alternative models that otherwise would be plausible given the cross-sectional nature of the data. Only the full mediational model fit the data well.
Again suggesting that results are unique to childhood SES, findings remained unchanged when controlling for participants’ current SES: All reported paths remained significant, and a bootstrapping analysis with 5,000 resamples indicated a significant indirect effect, with a point estimate of −0.007 and a 95% bias-corrected CI of (−0.018, −0.0008). Full results of the serial mediation analysis controlling for current SES can be found in SI Study 2, Mediational Model of BMI Controlling for Current SES.
Discussion
The high prevalence of obesity represents a major public health challenge. LHT provides a potentially valuable conceptual framework for understanding the behavioral mechanisms that underlie high rates of obesity. The current work suggests that effects of low SES on adult health outcomes can be partially explained by exposure to unpredictable environments in childhood. We observed a higher likelihood of obesity among adults from low SES childhoods, even after controlling for current SES (study 1), and our findings directly implicate the role of childhood unpredictability as it pertains to the development of a fast life-history strategy and ultimately to dysregulated eating (study 2). Taken together, these studies suggest that exposure to unpredictable environments in childhood may calibrate people’s behavior in ways that promote dysregulated eating and obesity in adulthood.
Even though life-history strategies are calibrated in childhood to help people maximize the benefits of their current environments, those strategies can be maladaptive when the environment changes, as it often does when people grow into adulthood. With regard to obesity, even if food (and other social and material resources) is readily available in adulthood, behavior nevertheless may be calibrated to the availability and predictability of resources experienced as a child. Moreover, those strategies ultimately have been designed through evolution to optimize outcomes in the context of ancestral environments and so may not be well-calibrated to modern environments in which high-calorie food is often abundant. Thus, although fast life-history strategies may be adaptive at some level, they can be quite dysfunctional in many current contexts.
LHT provides a theoretical framework for understanding a range of developmental variables that appear to underlie adult eating dysregulation. For example, research has documented a robust link between childhood trauma (e.g., abuse, neglect, parental alcoholism) and obesity in adulthood (19). Viewed through the lens of the current research, such findings can be explained by the fact that forms of childhood trauma are likely to instill a sense of unpredictability and uncertainty in children. Also consistent with a LHT approach are findings suggesting that early menarche in women—an indicator of early sexual maturation and a correlate of fast life-history strategies (20)—is associated with higher BMI during adolescence and into adulthood (11). Thus, LHT provides a unifying framework for understanding a range of early developmental factors associated with obesity.
As such, LHT helps generate predictions about additional factors that might contribute to adult obesity. For example, growing up in a household in which the father leaves the family (e.g., because of divorce) has been identified as a determinant of fast life-history strategies in women (3, 21). Similarly, frequent residential changes and changes in parents’ employment status serve as determinants of fast life-history strategies in both sexes (22). Consequently, research may benefit from investigating the link between these factors and adult obesity. Moreover, research suggests that it is unpredictability in childhood, rather than living in a harsh or stressful environment, that determines life-history strategies (6, 22). This finding highlights the importance of differentiating between factors characterized by stressful but predictable conditions (e.g., consistently lacking wealth) and those marked by uncertainty, turbulence, and frequent change. Thus, the current research has important implications for identifying factors that place children at risk for experiencing obesity later in life.
The current research also has implications for developing childhood interventions to combat obesity and identifying the persons most likely to benefit from them. People’s life-history strategies appear to be calibrated mainly by exposure to unpredictability during the first 5 y of life (6). Interventions may benefit from targeting children and early adolescents who experience unpredictable environments in those early years. Such interventions could target social-structural factors, in particular sources of uncertainty or unpredictability, that serve as early developmental precursors to obesity later in life. As noted earlier, LHT implies that fast life-history strategies are produced not by low SES or by a lack of resources per se but rather by unpredictable life events (6). Therefore, interventions aimed at addressing some of the antecedents to obesity may benefit from increasing the presence of structure, certainty, and stability in the lives of at-risk children and adolescents.
Such interventions could also help reduce a larger constellation of behavioral problems characteristic of fast life-history strategies, including risk-taking, competitiveness, impulsivity, and low-investment parenting behaviors (23). Moreover, the same forms of childhood trauma known to promote obesity also have been shown to promote other negative health outcomes, including risky sexual behavior (24) and drug use (25). Therefore aside from their implications for reducing obesity, interventions that reduce childhood unpredictability could ameliorate a range of problematic behavioral outcomes known to reflect fast life-history strategies.
The current findings are limited by their reliance on cross-sectional data and retrospective self-report measures. This research is also limited by its lack of focus on other factors shown to contribute to obesity, including structural and lifestyle factors such as the availability of calorie-dense foods, the use of exercise as a weight-management strategy, and cultural norms pertaining to weight (26). Indeed, results of study 2 show that, even after accounting for people’s life-history strategy, SES still exhibited a direct relationship with obesity status, and that relationship might be accounted for by the presence of such factors. Future research would benefit from examining how life-history strategies might interact with such factors. For example, the link between fast life-history strategies and dysregulated eating might be exacerbated by the presence of cultural standards that normalize being overweight or by a lack of access to nutritious foods and means of exercise. Considering such factors within the broader framework of LHT provides an integrative framework with which to understand both proximate and developmental factors that contribute to obesity in adulthood.
The current work is also limited by its lack of focus on genetic and prenatal factors. Some personality traits (e.g., impulsivity) associated with life-history strategies are partially heritable (27), and heritable factors could work in concert with developmental factors to shape eating behavior over the lifespan. Future work would profit from delineating heritable causes underlying adult obesity from developmental causes. Likewise, prenatal calibration of fetal development by the mother could play a role in shaping offspring behavior. Moreover, low birth weight could be correlated with both prenatal development and childhood unpredictability, and the potential role of low birth weight in adult obesity should be a focus of future research. Indeed, future work may benefit from examining the independent (and possibly interactive) roles played by genetic, prenatal, and developmental processes. Future research should also consider alternative theoretical perspectives in addition to the LHT viewpoint that childhood ecological conditions prepare people to operate effectively, assuming that conditions are similar later in life (28, 29). For example, harsh and unpredictable childhood conditions might also influence behavior because those conditions negatively impact people’s health, and people may compensate for that impact by speeding up their life course because of the risk of early mortality (30, 31).
Future empirical work would also benefit from including biometric indicators of life-history strategies (e.g., age of menarche, age at the birth of the first child) in addition to psychometric indicators. Psychometric indicators reveal the psychological processes underlying life-history strategies, whereas biometric indicators reveal life-history outcomes, and thus the two types of measures complement one another in important ways (32).
Future research also should continue to examine relationships among particular psychological processes and outcomes thought to reflect fast versus slow life histories. For example, although variables such as valuing long-term committed relationships are generally thought to reflect slow life-history strategies, long-term relationships also afford biparental care and would have been especially adaptive in ancestral environments thought to promote fast life-history strategies (e.g., high prevalence of natural hazards such as predators). Attending carefully to specific psychological processes in future research may reveal relationships with fast versus slow strategies that are nuanced and potentially moderated by context (e.g., the harshness of the environment). In turn, understanding those relationships may shed additional light on links between childhood variables and adult outcomes related to health and well-being.
Finally, it is worth noting that some of the associations documented in this research reflect relatively small effect sizes. Nevertheless, it is also worth noting that even small associations can have considerable importance for public health, particularly for health problems that are highly prevalent in the population (e.g., ref. 33). Given the very high prevalence and public health costs associated with obesity, if even a small proportion of the variance in weight can be accounted for by factors in our model, interventions designed to reduce obesity could be meaningfully improved by taking those factors into consideration.
Materials and Methods
Study 1 Method.
Participants.
Participants were 226 first-married newlywed spouses (113 couples) participating in a broader longitudinal study investigating relationship processes. Participants were recruited through invitations sent to couples who had applied for marriage licenses in counties near the study location. Three hundred eighty-nine couples were screened via telephone interviews to ensure the couples met the following criteria, given broader goals of the study: (i) they had been married for less than 4 mo, and both partners could attend a laboratory session within the first 4 mo of marriage; (ii) neither partner had been previously married; (iii) they were at least 18 y of age; and (iv) they spoke English (to ensure comprehension of the questionnaires). One hundred fifty-nine couples did not meet eligibility criteria. Of the 226 individuals who participated, 51 failed to provide complete data [21 husbands (18.6%) and 22 wives (19.5%) failed to provide an estimate of childhood family income; two (1.8%) husbands and four wives (3.5%) failed to provide height and weight at baseline and all follow-up assessments]. Thus, the final sample consisted of 90 husbands and 87 wives (of 103 couples).
At baseline, husbands were 27.76 (SD = 5.25) years of age and had completed 15.68 (SD = 2.74) years of education. Seventy-seven percent were employed full time, and 13% were full-time students. Mean income of husbands was $46,696 (SD = $49,455) per year. Wives were 26.93 (SD = 4.13) years of age and had completed 16.40 (SD = 2.59) years of education. Sixty percent were employed full time, and 13% were full-time students. Mean income of wives was $36,731 (SD = $37,649) per year. The sample was relatively diverse; 55% of husbands and 58% of wives self-identified as Caucasian, 19% of husbands and 20% of wives self-identified as Black or African American, 17% of husbands and 12% of wives self-identified as Hispanic or Latino/a, 3% of husbands and 6% of wives self-identified as Asian, and 5% of husbands and 4% of wives self-identified as another race/ethnicity (one husband and one wife did not report their race/ethnicity). Twenty-one percent of the couples had children. Approximately 27% of the sample (n = 61) was obese at baseline; an additional 24% was overweight at baseline.
Procedure.
Couples were either mailed a packet of surveys to complete at home or were emailed a link to complete their surveys online. Surveys included an informed consent form approved by the Florida State University Institutional Review Board, measures of childhood family income, current income, height and weight (from which BMI was calculated), and other measures beyond the scope of the current analyses (SI Study 1 for a full list of measures). At their laboratory sessions, participants completed a variety of tasks beyond the scope of the current analyses and were compensated $100 for completing the surveys and session.
At ∼6-mo intervals subsequent to the initial assessment, couples were contacted by telephone and were mailed measures assessing height and weight (and, at the fourth and sixth follow-up assessments, an additional measure assessing childhood family income). Spouses completed six follow-up assessments, and thus the study spanned the first 3.5 y of marriage. After completing each follow-up assessment, couples were mailed a $30 check for participating.
Materials.
Childhood family income.
To assess childhood family income at baseline, spouses provided a numerical estimate in response to the question: “How much money did your parents earn (combined income) while you were growing up (if you were raised by only one parent who did not receive child support, what was the income of that parent)?” Sixty-nine spouses failed to respond to this question, many of whom indicated that they did not know how much money their parents earned. Thus, in an effort to reduce missing data, we again assessed childhood family income at the fourth and sixth follow-up assessments (∼18 mo and 30 mo, respectively, into the marriages) using a different format. Specifically, spouses responded to the question: “What was your household income when you were growing up?” using an eight-point scale on which 1 = $15,000 or less, 2 = $15,001–$25,000, 3 = $25,001–$35,000, 4 = $35,001–$50,000, 5 = $50,001–$75,000, 6 = $75,001–$100,000, 7 = $100,001–$150,000, and 8 = $150,001 and above. Twenty-six spouses who had failed to provide a numerical estimate at baseline responded to this question (24 additional spouses provided data at the fourth assessment; two additional spouses provided data at the sixth assessment). Responses were converted by averaging the endpoints of the ranges provided. For example, spouses who indicated that their parents earned approximately $25,001–$35,000 yearly were coded $30,000. Responses provided at the first assessment were used when available, and responses provided at the fourth and sixth assessments were used when data were missing from the first assessment. Although this methodology may have introduced some degree of measurement error, such error did not pose a problem for detecting the hypothesized effect.
Body mass.
At baseline and all subsequent follow-up assessments, we calculated indices of body mass by converting the self-reported height and weight into a standard index, the BMI (kg/m2).
Obesity status.
Obesity status was defined based on guidelines provided by the Centers for Disease Control (34). Participants with BMI scores above 30.0 were categorized as obese. Participants with BMI scores above 25.0 were categorized as overweight.
Current income.
To ensure that any effects of childhood family income were independent of participants’ current income, we assessed and controlled for current income in all analyses. At baseline and all subsequent follow-up assessments, participants provided a numerical estimate in response to the question: “How much money did you earn last year, before taxes?”
Study 2 Method.
Participants.
We recruited 400 participants from Amazon’s Mechanical Turk (211 women, 188 men, 1 other/unspecified; mean age = 35.66 y, SDe = 11.34 y). In this sample, 77.8% self-identified as Caucasian, 8.0% self-identified as African American or Black, 7.2% self-identified as Asian, 5.3% self-identified as Hispanic, and 1.8% self-identified as other. Approximately 21.5% of the sample (n = 86) was obese; an additional 30% of the sample was overweight.
Design and procedure.
After providing online informed consent (the consent procedure was approved by the Northwestern University Institutional Review Board), participants completed measures including items assessing their childhood environment and their life-history strategy (full measures are provided in SI Study 2, Additional Measures). Participants completed a four-item measure of childhood SES (e.g., “My family usually had enough money for things when I was growing up”: 1 = strongly disagree, 7 = strongly agree; α = 0.86, mean = 3.69, SD = 1.49) (35) and a three-item measure of current SES (e.g., “I have enough money to buy the things I want”: 1 = strongly disagree, 7 = strongly agree; α = 0.85, mean = 3.72, SD = 1.59) (34). Participants completed an eight-item measure of childhood unpredictability (e.g., “My family life was generally inconsistent and unpredictable from day-to-day”: 1 = strongly disagree, 7 = strongly agree; α = 0.93, mean = 2.63, SD = 1.56) (36). To assess participants’ life-history strategy, each participant completed the 20-item Mini-K scale which assesses a single factor that differentiates between fast (low-K) and slow (high-K) life-history strategies (e.g., “I avoid taking risks,” “I would rather have one than several sexual relationships at a time”: 1 = strongly disagree, 7 = strongly agree; α = 0.84, mean = 4.74, SD = 0.87) (37). The Mini-K shows good internal consistency and convergent validity with other measures aimed at assessing life-history strategy (38, 39).
Participants also reported their height in inches (mean = 67.58, SD = 3.98) and current weight in pounds (mean = 172.37, SD = 42.54), which we used to calculate their BMI (mean = 26.43, SD = 5.79) and obesity status. Participants also completed a three-item measure of dysregulated-eating behavior that assessed the extent to which they regulated their eating behavior based on their hunger levels [“I only eat when I’m hungry” (reverse-coded), “I rely on my levels of hunger to decide when and how much to eat” (reverse-coded), and “I eat even when I’m not hungry”: 1 = strongly disagree, 7 = strongly agree; α = 0.79, mean = 3.57, SD = 1.41]. Higher values indicate a greater tendency to eat regardless of current hunger levels.
SI Study 1
In addition to measures reported in the main text, the following were assessed: three measures of relationship satisfaction; inventory of marital problems; four measures of commitment; sexual satisfaction; two measures of depression; self-esteem; relationship constraint; forgiveness; relationship attribution; social desirability; relational self-construal; survey of life events; conflict tactics; satisfaction with life; a general personality scale; two measures of attachment; self-compassion; narcissism; relational self-efficacy; self-control; distress; motivation to resolve problems; approach and avoidance motivations; ambivalent sexism; gratitude; implicit theories of weight; mate guarding; maximizing; sex-role orientation; relationship trust; health motivations; sociosexuality; body esteem; eating attitudes; perfectionism; three measures of sexual objectification; self-motivation; multidimensional health locus of control; lifetime exercise; eating attitudes test; three measures assessing people’s reasons for eating and exercising; two measures assessing physical health; sleep and fatigue anxiety; relational power; free will and determinism; jealousy; passionate love; willingness to sacrifice; ability to adopt a third-party perspective; menstrual-cycle information (women only); various demographic information.
SI Study 2
Additional Measures.
In addition to the key measures, participants completed several additional measures. Participants responded to a five-item measure of concern with food and eating (e.g., “Would a weight fluctuation of five pounds affect the way you live your life?”: 1 = not at all, 4 = very much, α = 0.73, mean = 2.35, SD = 0.75), a three-item measure of internal cues of meal cessation (e.g., “I usually stop eating when I want to leave room for dessert”: 1 = strongly disagree, 7 = strongly agree, α = 0.29, mean = 4.57, SD = 1.10) (40), and a three-item measure of external cues of meal cessation (e.g., “I usually stop eating when the TV show I’m watching is over”: 1 = strongly disagree, 7 = strongly agree, α = 0.51, mean = 3.00, SD = 1.14) (40).
Mediational Model of BMI.
To assess the predicted relationships among childhood SES, childhood unpredictability, life-history strategy, dysregulated eating, and BMI, we used the Process macro (18) within a multiple regression framework to conduct a serial mediation analysis. We entered childhood unpredictability, life-history strategy, and dysregulated-eating behavior as putative mediators of the relationship between SES and BMI.
These analyses revealed the predicted relationship between childhood SES and exposure to unpredictability: Lower childhood SES was associated with greater childhood unpredictability [b = −0.31, t(398) = −6.11, P < 0.001]. Next, entering both childhood SES and childhood unpredictability as predictors of life-history strategy revealed that greater childhood unpredictability was associated with a faster life-history strategy [b = −0.18, t(397) = −6.42, P < 0.001]. There was no direct link between childhood SES and life-history strategy [b = 0.003, t(397) = 0.10, P = 0.917]. Next, entering childhood SES, childhood unpredictability, and life-history strategy as predictors of dysregulated-eating behavior revealed an effect of life-history strategy, such that faster life-history strategies were associated with more dysregulated eating [b = −0.24, t(396) = −2.80, P = 0.005]; there was no direct effect of childhood unpredictability [b = −0.05, t(396) = −1.03, P = 0.302] or childhood SES [b = −0.04, t(396) = −0.86, P = 0.392] on dysregulated eating. Next, entering childhood SES, childhood unpredictability, life-history strategy, and dysregulated eating as predictors of BMI revealed an effect of dysregulated eating [b = 1.30, t(395) = 6.61, P < 0.001] and a direct effect of childhood SES [b = −0.42, t(395) = −2.20, P = 0.029] on BMI; there was no direct effect of life-history strategy [b = 0.15, t(395) = 0.45, P = 0.653] or childhood unpredictability [b = 0.08, t(395) = 0.40, P = 0.693].
To provide a direct test of mediation within the serial mediation model (i.e., the indirect effect of childhood SES on BMI as mediated by childhood unpredictability, life-history strategy, and dysregulated eating), a bootstrapping analysis with 5,000 resamples indicated a significant indirect effect, with a point estimate of −0.017 and a 95% bias-corrected CI of (−0.043, −0.004). Given that the CI does not contain zero, the data are consistent with the hypothesis that participants who experienced lower childhood SES experienced greater levels of childhood unpredictability, which were associated with developing a significantly faster life-history strategy, which was in turn associated with dysregulated-eating behaviors that were ultimately associated with higher BMI in adulthood.
We tested three plausible alternative models, none of which demonstrated good fit to the data. First, childhood SES was not indirectly associated with current BMI simply through dysregulated-eating behaviors [point estimate = −0.055, 95% bootstrap CI = (−0.201, 0.073)]. Second, childhood SES was not indirectly associated with current BMI simply through childhood unpredictability [point estimate = −0.023, 95% bootstrap CI = (−0.142, 0.091)]. Third, and finally, childhood SES was not indirectly associated with current BMI simply through life-history strategy [point estimate = 0.0005, 95% bootstrap CI = (−0.017, 0.029)]. These null effects are important because they help rule out alternative models that otherwise would be plausible given the cross-sectional nature of the data. The full hypothesized mediation model was the only one that fit the data well.
It is also important to note that the serial mediation results do not change when controlling for participants’ current socioeconomic status: All the previously reported paths remained significant. Furthermore, results of the serial mediation test remain substantively unchanged: A bootstrapping analysis with 5,000 resamples indicated a significant serial indirect effect, with a point estimate of −0.015 and a 95% bias-corrected confidence interval of (−0.040, −0.002). This analysis suggests that results are unique to participants’ childhood SES and are not merely concomitant to participants’ current SES.
Mediational Model of BMI Controlling for Current SES.
To assess the predicted relationships among childhood SES, childhood unpredictability, life-history strategy, dysregulated eating, and BMI, when controlling for current SES, we used the Process macro (18) within a multiple regression framework to conduct a serial mediation analysis. We entered childhood unpredictability, life-history strategy, and dysregulated-eating behavior as putative mediators of the effect of SES on BMI and current SES as a control variable.
These analyses revealed a significant relationship between childhood SES and exposure to unpredictability; as predicted, lower childhood SES was associated with greater childhood unpredictability [b = −0.31, t(397) = −5.96, P < 0.001] but current SES was not [b = 0.004, t(397) = 0.81, P = 0.935]. Next, entering both childhood SES and childhood unpredictability as predictors of life-history strategy revealed that greater childhood unpredictability was associated with a faster life-history strategy [b = −0.18, t(396) = −6.73, P < 0.001]. There was no direct association between childhood SES and life-history strategy [b = −0.03, t(396) = −1.20, P = 0.229]. However, there was a direct association between current SES and life-history strategy [b = 0.15, t(396) = 6.04, P < 0.001]. Next, entering childhood SES, childhood unpredictability, and life-history strategy as predictors of dysregulated-eating behavior revealed an effect of life-history strategy, such that faster life-history strategies were associated with more dysregulated eating [b = −0.22, t(395) = −2.44, P = 0.015]; there was no direct effect of childhood unpredictability [b = −0.05, t(395) = −0.95, P = 0.343], childhood SES [b = −0.03, t(395) = −0.65, P = 0.518], or current SES [b = −0.04, t(395) = −0.84, P = 0.402] on dysregulated eating. Next, entering childhood SES, childhood unpredictability, life-history strategy, and dysregulated eating as predictors of BMI revealed a significant effect of dysregulated eating [b = 1.28, t(394) = 6.54, P < 0.001], a marginal direct effect of childhood SES [b = −0.33, t(394) = −1.68, P = 0.093], and a significant direct effect of current SES [b = −0.39, t(394) = −2.10, P = 0.037] on BMI; there was no direct effect of life-history strategy [b = 0.36, t(394) = 1.03, P = 0.305] or childhood unpredictability [b = 0.11, t(394) = 0.59, P = 0.553].
The three alternative models we tested do not demonstrate good fit to the data even when controlling for current SES. First, childhood SES was not indirectly associated with current BMI as mediated only through dysregulated-eating behaviors [point estimate = −0.042, 95% bootstrap CI = (−0.182, 0.089)]. Second, childhood SES was not indirectly associated with current BMI simply through childhood unpredictability [point estimate = −0.035, 95% bootstrap CI = (−0.161, 0.078)]. Third, and finally, childhood SES was not indirectly associated with current BMI simply through life-history strategy [point estimate = −0.012, 95% bootstrap CI = (−0.072, 0.008)]. These null effects are important because they help rule out alternative interpretations that otherwise would be plausible given the cross-sectional nature of the data.
Mediational Model of Obesity Status Controlling for Current SES.
We conducted a similar set of analyses to investigate factors contributing to obesity status. We assessed the predicted relationships among childhood SES, childhood unpredictability, life-history strategy, dysregulated eating, and obesity, controlling for current SES using the Process macro (18). We entered childhood unpredictability, life-history strategy, and dysregulated-eating behaviors as putative mediators and current SES as a control variable. We observed the expected association between childhood SES and childhood unpredictability; as observed in the analyses predicting BMI, higher childhood SES was associated with significantly less childhood unpredictability [b = −0.31, t(397) = −5.96, P < 0.001], but current SES was not [b = 0.004, t(397) = 0.81, P = 0.935]. As in the analysis for BMI, we again observed an association between childhood unpredictability and life-history strategy; as predicted, greater childhood unpredictability was associated with a faster life-history strategy [b = −0.18, t(396) = −6.73, P < 0.001]. Childhood SES was unassociated with life-history strategy [b = −0.034, t(396) = −1.20, P = 0.229]. However, current SES was associated with life-history strategy [b = 0.15, t(396) = 6.04, P < 0.001]. Next, entering childhood SES, childhood unpredictability, and life-history strategy as predictors of dysregulated eating revealed an association between life-history strategy and dysregulated eating, such that a faster life-history strategy was associated with more dysregulated eating [b = −0.22, t(395) = −2.44, P = 0.015]; there was no direct effect of childhood SES [b = −0.03, t(395) = −0.65, P = 0.518], childhood unpredictability [b = −0.05, t(395) = −0.95, P = 0.343], or current SES [b = −0.04, t(395) = −0.84, P = 0.402] on dysregulated eating. This pattern mirrored the previous analyses for BMI. Entering childhood SES, childhood unpredictability, life-history strategy, and dysregulated eating as predictors of obesity revealed an association between dysregulated eating and obesity [b = 0.58, P < 0.001], a marginal direct effect of childhood SES [b = −0.16, P = 0.096], and a significant direct effect of current SES [b = −0.24, P = 0.008] on obesity; there was no effect of life-history strategy [b = 0.005, P = 0.979] or childhood unpredictability [b = 0.12, P = 0.197] on obesity.
Notably, the three alternative models we tested did not demonstrate good fit to the data when controlling for current SES. First, childhood SES was not indirectly associated with likelihood of obesity in adulthood through dysregulated-eating behaviors [point estimate = −0.019, 95% bootstrap CI = (−0.089, 0.044)]. Second, childhood SES was not indirectly associated with likelihood of obesity in adulthood through childhood unpredictability [point estimate = −0.036, 95% bootstrap CI = (−0.104, 0.026)]. Third, and finally, childhood SES was not indirectly associated with the likelihood of obesity in adulthood through life-history strategy [point estimate = −0.0002, 95% bootstrap CI = (−0.019, 0.015)]. These null effects are important because they help rule out alternative interpretations that otherwise would be plausible given the cross-sectional nature of the data.
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1620482114/-/DCSupplemental.
References
- 1.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 2.National Institutes of Health 1998 Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report (National Heart, Lung, and Blood Institute, Bethesda), NIH Publication No. 98–4083. Available at https://www.nhlbi.nih.gov/health-pro/guidelines/archive/clinical-guidelines-obesity-adults-evidence-report. Accessed May 1, 2016.
- 3.Belsky J, Steinberg L, Draper P. Childhood experience, interpersonal development, and reproductive strategy: An evolutionary theory of socialization. Child Dev. 1991;62:647–670. doi: 10.1111/j.1467-8624.1991.tb01558.x. [DOI] [PubMed] [Google Scholar]
- 4.Ellis BJ, Figueredo AJ, Brumbach BH, Schlomer GL. Fundamental dimensions of environmental risk. Hum Nat. 2009;20:204–268. doi: 10.1007/s12110-009-9063-7. [DOI] [PubMed] [Google Scholar]
- 5.Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: Conceptual models, empirical challenges and interdisciplinary perspectives. Int J Epidemiol. 2002;31:285–293. [PubMed] [Google Scholar]
- 6.Simpson JA, Griskevicius V, Kuo SI, Sung S, Collins WA. Evolution, stress, and sensitive periods: The influence of unpredictability in early versus late childhood on sex and risky behavior. Dev Psychol. 2012;48:674–686. doi: 10.1037/a0027293. [DOI] [PubMed] [Google Scholar]
- 7.Griskevicius V, et al. When the economy falters, do people spend or save? Responses to resource scarcity depend on childhood environments. Psychol Sci. 2013;24:197–205. doi: 10.1177/0956797612451471. [DOI] [PubMed] [Google Scholar]
- 8.White AE, Li YJ, Griskevicius V, Neuberg SL, Kenrick DT. Putting all your eggs in one basket: Life-history strategies, bet hedging, and diversification. Psychol Sci. 2013;24:715–722. doi: 10.1177/0956797612461919. [DOI] [PubMed] [Google Scholar]
- 9.Ellis BJ. Timing of pubertal maturation in girls: An integrated life history approach. Psychol Bull. 2004;130:920–958. doi: 10.1037/0033-2909.130.6.920. [DOI] [PubMed] [Google Scholar]
- 10.Marlowe FW, Berbesque JC. Tubers as fallback foods and their impact on Hadza hunter-gatherers. Am J Phys Anthropol. 2009;140:751–758. doi: 10.1002/ajpa.21040. [DOI] [PubMed] [Google Scholar]
- 11.Laitinen J, Power C, Järvelin MR. Family social class, maternal body mass index, childhood body mass index, and age at menarche as predictors of adult obesity. Am J Clin Nutr. 2001;74:287–294. doi: 10.1093/ajcn/74.3.287. [DOI] [PubMed] [Google Scholar]
- 12.Olson CM, Bove CF, Miller EO. Growing up poor: Long-term implications for eating patterns and body weight. Appetite. 2007;49:198–207. doi: 10.1016/j.appet.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 13.Singh GK, Siahpush M, Hiatt RA, Timsina LR. Dramatic increases in obesity and overweight prevalence and body mass index among ethnic-immigrant and social class groups in the United States, 1976–2008. J Community Health. 2011;36:94–110. doi: 10.1007/s10900-010-9287-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hill SE, Prokosch ML, DelPriore DJ, Griskevicius V, Kramer A. Low childhood socioeconomic status promotes eating in the absence of energy need. Psychol Sci. 2016;27:354–364. doi: 10.1177/0956797615621901. [DOI] [PubMed] [Google Scholar]
- 15.Brisbois TD, Farmer AP, McCargar LJ. Early markers of adult obesity: A review. Obes Rev. 2012;13:347–367. doi: 10.1111/j.1467-789X.2011.00965.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pavela G, Latham K. Childhood conditions and multimorbidity among older adults. J Gerontol B Psychol Sci Soc Sci. 2016;71:889–901. doi: 10.1093/geronb/gbv028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Raudenbush SW, Bryk AS, Cheong YF, Congdon RT, du Toit M. HLM 7: Hierarchical Linear and Nonlinear Modeling. Scientific Software International Inc.; Lincolnwood, IL: 2011. [Google Scholar]
- 18.Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Guilford; New York: 2013. [Google Scholar]
- 19.Williamson DF, Thompson TJ, Anda RF, Dietz WH, Felitti V. Body weight and obesity in adults and self-reported abuse in childhood. Int J Obes Relat Metab Disord. 2002;26:1075–1082. doi: 10.1038/sj.ijo.0802038. [DOI] [PubMed] [Google Scholar]
- 20.Tither JM, Ellis BJ. Impact of fathers on daughters’ age at menarche: A genetically and environmentally controlled sibling study. Dev Psychol. 2008;44:1409–1420. doi: 10.1037/a0013065. [DOI] [PubMed] [Google Scholar]
- 21.Del Giudice M. Sex, attachment, and the development of reproductive strategies. Behav Brain Sci. 2009;32:1–21; discussion 21–67. doi: 10.1017/S0140525X09000016. [DOI] [PubMed] [Google Scholar]
- 22.Belsky J, Schlomer GL, Ellis BJ. Beyond cumulative risk: Distinguishing harshness and unpredictability as determinants of parenting and early life history strategy. Dev Psychol. 2012;48:662–673. doi: 10.1037/a0024454. [DOI] [PubMed] [Google Scholar]
- 23.Szepsenwol O, Simpson JA, Griskevicius V, Raby KL. The effect of unpredictable early childhood environments on parenting in adulthood. J Pers Soc Psychol. 2015;109:1045–1067. doi: 10.1037/pspi0000032. [DOI] [PubMed] [Google Scholar]
- 24.Hillis SD, Anda RF, Felitti VJ, Marchbanks PA. Adverse childhood experiences and sexual risk behaviors in women: A retrospective cohort study. Fam Plann Perspect. 2001;33:206–211. [PubMed] [Google Scholar]
- 25.Dube SR, et al. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: The adverse childhood experiences study. Pediatrics. 2003;111:564–572. doi: 10.1542/peds.111.3.564. [DOI] [PubMed] [Google Scholar]
- 26.O’Dea JA. Gender, ethnicity, culture and social class influences on childhood obesity among Australian schoolchildren: Implications for treatment, prevention and community education. Health Soc Care Community. 2008;16:282–290. doi: 10.1111/j.1365-2524.2008.00768.x. [DOI] [PubMed] [Google Scholar]
- 27.Sherman DK, Iacono WG, McGue MK. Attention-deficit hyperactivity disorder dimensions: A twin study of inattention and impulsivity-hyperactivity. J Am Acad Child Adolesc Psychiatry. 1997;36:745–753. doi: 10.1097/00004583-199706000-00010. [DOI] [PubMed] [Google Scholar]
- 28.Gluckman PD, Hanson MA, Spencer HG. Predictive adaptive responses and human evolution. Trends Ecol Evol. 2005;20:527–533. doi: 10.1016/j.tree.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 29.Gluckman PD, Hanson MA, Pinal C. The developmental origins of adult disease. Matern Child Nutr. 2005;1:130–141. doi: 10.1111/j.1740-8709.2005.00020.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jones JH. Fetal programming: Adaptive life-history tactics or making the best of a bad start? Am J Hum Biol. 2005;17:22–33. doi: 10.1002/ajhb.20099. [DOI] [PubMed] [Google Scholar]
- 31.Nettle D, Frankenhuis WE, Rickard IJ. The evolution of predictive adaptive responses in human life history. Proc Biol Sci. 2013;280:20131343. doi: 10.1098/rspb.2013.1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Figueredo AJ, et al. Methodologically sound: Evaluating the psychometric approach to the assessment of human life history [reply to Copping, Campbell, and Muncer, 2014] Evol Psychol. 2015;13:299–338. doi: 10.1177/147470491501300202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Künzli N, et al. Clinically “small” effects of air pollution on FVC have a large public health impact. Swiss Study on Air Pollution and Lung Disease in Adults (SAPALDIA) - team. Eur Respir J. 2000;15:131–136. doi: 10.1183/09031936.00.15113100. [DOI] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention (2016) Defining adult overweight and obesity. Available at https://www.cdc.gov/obesity/adult/defining.html. Accessed July 1, 2016.
- 35.Griskevicius V, Delton AW, Robertson TE, Tybur JM. Environmental contingency in life history strategies: The influence of mortality and socioeconomic status on reproductive timing. J Pers Soc Psychol. 2011;100:241–254. doi: 10.1037/a0021082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mittal C, Griskevicius V, Simpson JA, Sung S, Young ES. Cognitive adaptations to stressful environments: When childhood adversity enhances adult executive function. J Pers Soc Psychol. 2015;109:604–621. doi: 10.1037/pspi0000028. [DOI] [PubMed] [Google Scholar]
- 37.Figueredo AJ, et al. Consilience and life history theory: From genes to brain to reproductive strategy. Dev Rev. 2006;26:243–275. [Google Scholar]
- 38.Figueredo AJ, et al. The Psychometric assessment of human life history strategy: A meta-analytic construct validation. Evol Behav Sci. 2014;8:148–185. [Google Scholar]
- 39.Olderbak S, Gladden P, Wolf PSA, Figueredo AJ. Comparison of life history strategy measures. Pers Individ Dif. 2014;58:82–88. [Google Scholar]
- 40.Wansink B, Payne CR, Chandon P. Internal and external cues of meal cessation: The French paradox redux? Obesity (Silver Spring) 2007;15:2920–2924. doi: 10.1038/oby.2007.348. [DOI] [PubMed] [Google Scholar]