Abstract
Objective
This randomized controlled trial evaluates the feasibility of using an Embodied Conversational Agent (ECA) to teach lifestyle modifications to urban women.
Methods
Women were randomized to either 1) an ECA (content included: mindfulness, stress management, physical activity, and healthy eating) or 2) patient education sheets mirroring same content plus a meditation CD/MP3 once a day for one month. General outcome measures included: number of stress management techniques used, physical activity levels, and eating patterns.
Results
Sixty-one women ages 18 to 50 were enrolled. On average, 51% identified as white, 26% as black, 23% as other races; and 20% as Hispanic. The major stress management techniques reported at baseline were: exercise (69%), listening to music (70%), and social support (66%). After one month, women randomized to the ECA significantly decreased alcohol consumption to reduce stress (p = 0.03) and increased daily fruit consumption by an average of 2 servings compared to the control (p = 0.04).
Conclusion
It is feasible to use an ECA to promote health behaviors on stress management and healthy eating among diverse urban women.
Practice implications
Compared to patient information sheets, ECAs provide promise as a way to teach healthy lifestyle behaviors to diverse urban women.
Keywords: Embodied conversational agent, Mindfulness, Mindfulness based stress reduction, Stress management, Healthy eating, Nutrition, Physical activity
1. Introduction
Clinicians often address multiple health behaviors simultaneously and supplement office visits with additional health education through written materials, such as patient information sheets or brochures [1, 2]. Although these sheets are considered standard of care, the content and readability may not necessarily benefit patients with cultural or economic differences or lower literacy [3]. Furthermore, many clinicians endorse lifestyle changes or assist in managing chronic stress related problems (e.g. obesity, alcohol, and tobacco abuse) which require patients to change several behaviors at a time [4].
Today, technology-based interventions are becoming increasingly popular for delivering health-related behavioral changes [5–7]. To date, most automated health behavior change interventions are designed to only address a single behavior [8, 9]. Little is known about the practicality of using a technology-based intervention to deliver a multi-behavioral change intervention in racially diverse women [10, 11].
Providing specifically tailored information on multiple health behaviors may prove useful for patients to improve their overall well-being. One technology, called the embodied conversational agent (ECA), shows particular promise for conveying behavioral change strategies to patients [9, 12]. This paper reports on a feasibility study that compares an ECA delivering content on mindfulness, stress management, healthy eating, and physical activity to patient education sheets with the same content.
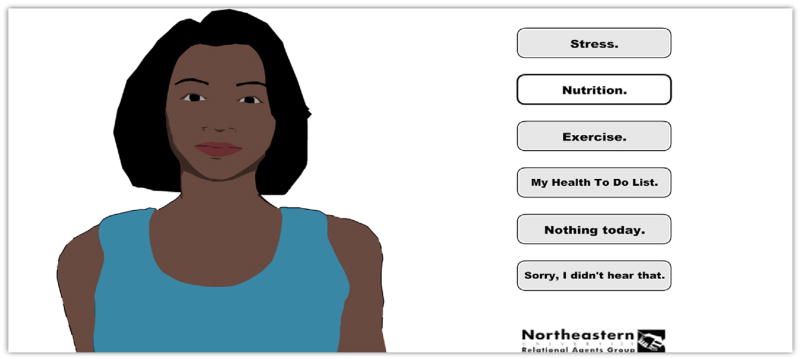
The ECA is an animated conversational character that simulates face-to-face interaction with a patient (Fig. 1) [12–16]. The system is comprised of a networked server with a conversational database responding to patient’s interactions and a patient education system. The ECA is an animated African American female character programmed to deliver culturally aware patient strategies and health information (e.g. recommending specific popular recipes or foods, mentioning prayer or spiritual traditions) to increase skills in self-management. The language used is dynamically composed, based on each patient’s data (e.g. name, gender, history of past interactions and responses). The agent also answers questions and tests patient understanding of key health facts. Prior pilots have demonstrated acceptability of ECAs in both inpatient [17–19] and outpatient settings [20, 21]. Other studies have also yielded positive outcomes for ECAs to deliver health education on topics such as: exercise, eating fruits and vegetables, and preconception care [12, 16, 21–24].
Fig. 1.
Gabby Embodied Conversational Agent (ECA) Interface.
Based on our previous studies, we have shown it is feasible for young African American women ages 18 to 34 years to benefit from an ECA delivering health information on dietary supplements and stress management as part of a larger preconception patient education ECA system [16, 24]. We do not know, however, whether the ECA can be used to deliver lifestyle strategies (mindfulness, stress management, healthy eating, and physical activity) in an urban outpatient setting with racially diverse women ages 18 to 50 years. This two-arm randomized control trial (RCT) newly introduces the ECA to female patients in person and compares the acceptability and satisfaction of the ECA to patient information sheets plus a meditation CD/MP3 among peri-menopausal women recruited from Boston. The outcomes being studied are feasibility and satisfaction with the ECA versus patient information sheets (control group).
2. Methods
2.1. Design and implementation
2.1.1. The Gabby System
The ECA system for this study was adapted from the Gabby Preconception Health Care system’s dialogue scripts and media (Version 2); the detailed curriculum is in Table 1 [16]. The scripts included motivational interviewing dialogue, dialogue to simulate shared decision making interactions, and additional longitudinal interaction using techniques such as goal setting, problem solving, tips, and homework (Appendix A).
Table 1.
Curriculum content of the ECA (Gabby) system.
| Stress management | Nutrition | Physical activity |
|---|---|---|
| Stress 101 content | Healthy Eating content | Activity content |
|
|
|
| Mind Body Techniques | Supplements Content | |
|
|
The healthy eating promotion dialogue was based on previous ECA studies engaging women in preconception care [16, 24], the Five Fruit and Vegetables recommendation [25], the Harvard School of Public Health’s healthy eating plate [26], and the principles of the Diabetes Prevention Program [27]. Information on stress management was adapted from principles of Mindfulness Based Stress Reduction (MBSR) [16], a promising mind-body intervention [28–31]. The major techniques included were: being present in the moment, responding and not reacting to stress, awareness of breath meditations (two versions: short 10 min; long 25 min), body scan, mindful eating, and mindful yoga. A recent systematic review identified 21 RCTs of MBSR: eleven of these studies showed improvement in mental health measures compared to waitlist or standard care controls, and improved pain scores and mental health status for patients with chronic pain [32]; other studies have also shown similar results [33–36]. Additional stress management exercises included progressive muscle relaxation and guided imagery. Finally, physical activity recommendations were based on governmental guidelines for physical activity [20, 21, 37, 38].
The ECA system is accessed over the web in a standard browser through a username and secure password login. Each interaction with the system consisted of a personal greeting from Gabby, an ECA, followed by educational content and behavior change counseling related to stress management, healthy eating, and physical activity, any or all of which could be selected by the participant (Fig. 1). The system also contains an auto logout feature after a period of user inactivity.
If participants were randomized to the intervention, the research assistant (RA) enrolled them into the ECA system, specifying baseline information (e.g. name, age), and then taught them how to use the system for 60 min. Participants were asked to log on once a day for 30 days and to interact with Gabby for as long as they wished.
2.1.2. Patient information sheets and meditation CD/MP3
If participants were randomized to the control, the RA reviewed patient information sheets in person for 60 min, which mirrored the content from the Gabby system. These sheets were written at a fifth grade level to accommodate a spectrum of health literacy. We also prepared a CD/MP3 with the same meditations and exercises offered by the ECA. Control group meditations were recorded by a live meditation teacher in contrast to Gabby’s electronic voice. Women were encouraged to listen to the recordings once a day for 30 days and to read the sheets as many times as they wished.
2.2. Recruitment, enrollment and randomization
Participants were recruited from primary care outpatient clinics at Boston Medical Center (BMC). Recruitment flyers were placed in clinical exam rooms, and recruitment materials were available to clinicians to hand out as appropriate. We also posted in the weekly BMC online newsletter. Patients self-referred themselves to the study by calling the study phone number listed on flyers within clinics. We included participants who self-identified as women, were 18–50 years of age, had access to a telephone and computer with internet, were English-speaking, and were not pregnant, to enroll in the study. We excluded participants who refused to consent, were not able to complete the study due to health reasons, including mental health or substance abuse problems, or did not speak English.
All participants completed enrollment with a trained RA, which took 30 min to complete. The RA explained the study, including the purpose, risks, and benefits, and asked each potential participant a question about each of those points to confirm that she was capable of providing informed consent. Participants gave verbal informed consent, since the enrollment process was completed. Data were collected by the RA for all participants at baseline and at one month follow-up. Participants were enrolled into the study on a rolling basis and as such, participant study durations were tracked individually based upon the date of baseline completion. After obtaining baseline information, participants were randomized to either the intervention or control using a computer-generated permuted block method. The RA was not blinded to group allocation.
All participants received a reminder phone call/e-mail at 14 days after enrollment to assess for safety and address any questions. After one month from baseline, the RA conducted post-study interviews in person or by phone. Participants received a gift card for their participation in the study and reimbursement for transportation and were also entered into a raffle.
2.3. Outcome measures
2.3.1. Primary outcomes
A primary goal of this study was to gather feasibility data on ECA utilization among multiracial women ages 18 to 50 years within an outpatient setting in order to design a larger fully powered RCT. The primary outcomes were as follows: number of recruited participants in a 12-month period; proportion of participants who were racial minorities (non-white); number of participants who completed the study from baseline to follow-up; number of participants for whom outcome data can be collected; and participants’ satisfaction with the intervention or control.
2.3.2. Demographic and secondary outcomes
The following information was collected by the RA through an interview both at baseline and post-study: demographics (including age, race, ethnicity, education, work status, income, self-reported height and weight, BMI; clinical factors such as health conditions, medication use, smoking status, alcohol use, and pain levels); physical and mental health statuses by the Short Form Health Survey (SF-12) [39] and depression levels by the Patient Health Questionnaire (PHQ-9) [40]. We asked questions assessing eating patterns, physical activity routines, and stress management levels at baseline and post-intervention.
Adapting questions from the National Health and Nutrition Examination Survey (NHANES), participants reported the total number of fruit and vegetable servings they consumed daily; the frequency of consuming regular soda/sugary drinks, caffeinated drinks, snack foods, calcium and dairy, whole grains, red meat, and fish per week; the frequency of eating breakfast per week; and intake of vitamins or minerals, folic acid, and herbal supplements [41]. We showed an image of a food label and asked participants if they read Nutrition Fact labels on grocery items regularly. We assessed their nutrition knowledge (Appendix B), and inquired about food access and assistance programs using the Household Food Insecurity Access Scale (HFIAS) [42].
Based on the Stanford Patient Education Research Center’s Exercise Behaviors Questionnaire, we compiled the total amount of time, in minutes, participants reported engaging in physical activity during a typical week [43]. Specific activity routines included stretching, strengthening and aerobic activities (e.g. walking, running or jogging, aquatics, and other). We also collected information on participants’ self-efficacy to participate in physical activity with the Self-Efficacy for Exercise Scale (SEE) [44].
For stress management, we asked participants to report self-perceived stress levels using the Perceived Stress Scale (PSS-4) [45]. For types of stress management, we asked: “in the past week, how many times did you do stress management or relaxation techniques?” Then we asked them to describe techniques they utilized to manage their stress on a weekly basis (see Section 3.2.2).
For all three overarching topics, we asked participants to rate their confidence in their ability to eat healthy, to exercise at least an hour per week, or to manage stress. Higher scores indicated greater confidence to perform such activities.
At the end of the study, participants were also asked to provide feedback on their assigned intervention. Questions included incorporation and relevance of suggestions on diet and nutrition; effects of the intervention on stress; exercise; benefits and difficulties of interacting with the intervention; and any other feedback they wished to share.
Specifically for ECA users, we collected system utilization data including number of logins, duration of use (in min), and user satisfaction after one month. Following a semi-structured interview guide, we also asked open ended questions regarding participants’ impressions of an ECA delivering health information.
2.4. Data analysis
2.4.1. Preliminary analysis
Effectiveness of randomization was assessed by comparing sociodemographic factors between the intervention and control using Chi-square tests for dichotomous and categorical variables and two-sample t-tests for continuous variables.
2.4.2. Primary and secondary analyses
Descriptive statistics were used to analyze primary outcome measures. This feasibility study lacked the statistical power to measure the difference in adherence to plan between intervention and control patients. An exploratory analysis using a Chi-square test was conducted to compare the adherence to plan (e.g. increase in stress management techniques used, increase in healthy eating, and increase in activity) between intervention and control patients. Two sample t-tests were used to compare satisfaction scores between the two groups. Normally distributed data were analyzed using two sample t-tests and data not normally distributed were analyzed using Wilcoxon Rank Sum tests. All analyses were conducted using SAS 9.3.
Interview responses were documented on a data collection sheet and reviewed to identify similarities among responses. Responses reported by two or more participants were identified for further analysis and categorized into three overarching themes: perceived helpfulness, benefits, and challenges using the assigned intervention. The study was approved by the BMC Institutional Review Board.
3. Results
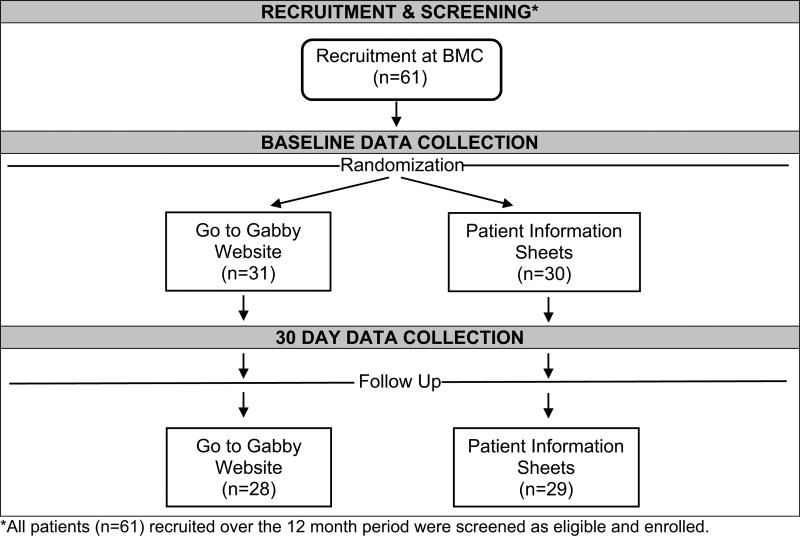
3.1. Study consort diagram
We recruited 61 participants in a 12-month period; all 61 recruited women were screened eligible and enrolled into the study for one month. We collected outcome data from baseline to follow-up on 57 participants (Fig. 2).
Fig. 2.
Study consort diagram.
3.2. Quantitative results
3.2.1. Baseline demographic and clinical characteristics
The demographic and clinical characteristics of the 61 women enrolled in this study are presented in Table 2. On average, participants were 35 years old; 51% identified as white, 26% as black, 2% as Asian/Pacific Islander, and 21% as other races; and 20% identified as Hispanic. Eighty-four percent of participants primarily spoke English at home, while 11% primarily spoke Spanish. Seventy-nine percent of women had completed at least some college, and 89% of them worked full-time or part-time. In regards to yearly household income, 44% reported making less than $49,000, and another 46% reported making more than $50,000. Ten percent of participants refused to disclose their income status.
Table 2.
Baseline Demographic and Clinical Characteristics of Participants.
| Variable | Total Baseline (N = 61) n (%) |
Gabby Baseline (N = 31) n (%) |
Control Baseline (N = 30) n (%) |
p-valuea |
|---|---|---|---|---|
| Age (23–50) | μ = 35 (σ = 8.4) | μ = 33 (σ = 8.1) | μ = 37 (σ = 8.4) | 0.08 |
| Race | 0.78 | |||
| White | 31 (51) | 15 (48) | 16 (53) | |
| Black | 16 (26) | 8 (26) | 8 (27) | |
| Asian/Pacific Islander | 1 (2) | 1 (3) | 0 (0) | |
| Other | 13 (21) | 7 (23) | 6 (20) | |
| Ethnicity | 0.22 | |||
| Hispanic | 12 (20) | 8 (26) | 13 (4) | |
| Non-Hispanic | 49 (80) | 23 (74) | 87 (26) | |
| Language | 0.79 | |||
| English | 51 (84) | 26 (84) | 83 (25) | |
| Spanish | 7 (11) | 3 (10) | 14 (4) | |
| Other | 3 (5) | 2 (7) | 3 (1) | |
| Education | 0.38 | |||
| High School/GED | 13 (21) | 8 (26) | 17 (5) | |
| College | 48 (79) | 23 (74) | 83 (25) | |
| Work | 0.32 | |||
| Full/Part Time | 54 (89) | 28 (90) | 86 (26) | |
| Unemployed | 5 (8) | 3 (10) | 7 (2) | |
| Disabled | 2 (3) | 0 (0) | 7 (2) | |
| Income | 0.88 | |||
| Less than $10K | 6 (10) | 3 (10) | 10 (3) | |
| $10K–$49K | 21 (34) | 12 (38) | 30 (9) | |
| $50K–$99K | 15 (25) | 8 (26) | 23 (7) | |
| $100K or more | 13 (21) | 5 (16) | 27 (8) | |
| Refuse/Don’t Know | 6 (10) | 3 (10) | 10 (3) | |
| BMI | μ = 28 (σ = 6.6) | μ = 27 (σ = 5.6) | μ = 29 (σ = 7.5) | 0.37 |
| Pain Score | μ = 3 (σ = 3) | μ = 3 (σ = 3.4) | μ= 3 (σ = 2.6) | 0.97 |
| PHQ-9 Score | μ = 7 (σ = 4.6) | μ = 7 (σ = 4.7) | μ = 7 (σ = 4.6) | 0.82 |
| SF-12 | ||||
| PCS Score | μ = 56 (σ = 10.2) | μ = 56 (σ = 10.8) | μ = 56 (σ = 9.6) | 0.95 |
| MCS Score | μ = 59 (σ = 10.7) | μ = 61 (σ = 11.6) | μ = 59 (σ = 9.8) | 0.46 |
| Health Conditions that Cause Pain | 0.71 | |||
| Yes | 27 (44) | 13 (42) | 14 (47) | |
| Chronic Health Problems | 0.52 | |||
| Yes | 18 (30) | 8 (26) | 10 (33) | |
| Take Prescribed Medications | 0.93 | |||
| Yes | 41 (67) | 21 (68) | 20 (67) | |
| Smoking | 0.98 | |||
| Yes | 2 (3) | 1 (3) | 1 (3) | |
| Alcohol Use | 0.30 | |||
| Yes | 43 (70) | 20 (65) | 23 (77) |
Continuous variables were analyzed using two-sample t-tests and categorical/dichotomous variables were analyzed using Chi-square tests of independence.
On average, women in the study had a BMI of 28 kg/m3 and scored a 7 on the PHQ-9 assessment; 30% reported having chronic health problems, and 67% regularly took prescribed medication. An average BMI score of 28 kg/m3 is classified as being overweight, while a PHQ-9 score greater than 5 denotes mild depression [40]. Three percent of participants reported smoking, and 70% reported drinking alcohol at least once a month or more. There were no significant differences in demographics or clinical characteristics between groups.
3.2.2. Stress management techniques
In Table 3, the most popular stress management techniques at baseline among participants included: engaging in physical activity (69%), listening to music (70%),and spending time with friends (66%). At one month, there was no significant difference in the number of adaptive coping techniques between groups. The proportion of women who reported eating as a coping technique did decrease, although not significantly (55% to 29% for intervention, 50% to 38% for control).
Table 3.
Stress Management Techniques.
| Variable | Total Baseline (N = 61) n (%) |
Gabby Baseline (N = 31) n (%) |
Gabby Follow- up (N = 28) n (%) |
Control Baseline (N = 30) n (%) |
Control Follow- up (N = 29) n (%) |
p-valuea |
|---|---|---|---|---|---|---|
| Adaptive coping | ||||||
| Deep breathing/meditation | 37 (61) | 20 (65) | 21 (75) | 17 (57) | 23 (79) | 0.35 |
| Exercise | 42 (69) | 19 (61) | 20 (71) | 23 (77) | 24 (83) | 0.51 |
| Eat | 32 (52) | 17 (55) | 8 (29) | 15 (50) | 11 (38) | 0.12 |
| Listen to music | 43 (70) | 21 (68) | 19 (68) | 22 (73) | 20 (69) | 0.81 |
| Pray | 30 (49) | 13 (42) | 10 (36) | 17 (57) | 14 (48) | 1 |
| Spend time with friends | 40 (66) | 22 (71) | 17 (61) | 18 (60) | 15 (52) | 0.49 |
| Go shopping | 27 (44) | 14 (45) | 7 (25) | 13 (43) | 10 (34) | 0.89 |
| Play video games | 4 (7) | 1 (3) | 0 (0) | 3 (10) | 3 (10) | c |
| Go for a walk | 34 (56) | 18 (58) | 19 (68) | 16 (53) | 18 (62) | 0.72 |
| Watch TV | 38 (62) | 19 (61) | 14 (50) | 19 (63) | 21 (72) | 0.19 |
| Otherb | 16 (26) | 9 (29) | 5 (18) | 7 (23) | 6 (21) | 0.6 |
| Maladaptive coping | ||||||
| Drink alcohol | 41 (67) | 11 (35) | 4 (14) | 9 (30) | 9 (31) | 0.03 |
| Smoke cigarettes | 3 (5) | 2 (6) | 1 (4) | 1 (3) | 1 (3) | c |
| Smoke marijuana | 2 (7) | 2 (6) | 5 (18) | 0 (0) | 0 (0) | c |
| How many times did you do stress management techniques in the past week? | μ = 2 (σ = 2.3) | μ = 1 (σ = 2) | μ = 4 (σ = 3) | μ = 2 (σ = 2.6) | μ = 3 (σ = 3.3) | 0.17 |
| (0–10 scale) | ||||||
| Perceived Stress Score (0–4 scale) | μ = 18 (σ = 3.6) | μ = 17 (σ = 3.7) | μ = 20 (σ = 3.1) | μ = 18 (σ = 3.5) | μ = 19 (σ = 3.1) | 0.07 |
Dichotomous variables were analyzed using two group McNemar tests of differential change for intervention and control groups. Continuous variables were analyzed using two-sample t-tests.
Includes traveling, drawing, sleeping, reading, family time, thinking and counseling.
No statistics were computed because there were zero participants in at least one group changed from baseline to follow-up.
At baseline, 67% of participants reported drinking alcohol at least once a month or more to manage their stress. At 30 days, there was a significant decrease in the number of women who used alcohol for stress management in the intervention compared to the control group (35% to 14% for intervention, 30% to 31% for control; p = 0.03). The number of stress management techniques increased in both groups, though there was no significant difference (μ = 1 to 4 for intervention, μ=2 to 3 for control). There was no significant difference in the perceived stress scale in the intervention compared to the control group.
At baseline, women in both groups were identified as being mildly depressed, with an average PHQ-9 score of 7. At follow-up, PHQ-9 and SF-12 scores did not differ significantly between the two groups (p = 0.36 and p = 0.28, respectively). However, it is worth noting that PHQ-9 scores decreased by two units in the ECA group compared to a one unit decrease in the control group.
3.2.3. Food and nutrition
Specific eating patterns are documented in Table 4. Analysis revealed that ECA users significantly increased the average amount of fruit servings they ate compared to women using patient information sheets (μ = 2 to 4 for intervention, μ = 2 to 2 for control; p = 0.04). The amount of vegetable servings increased for both groups, but not significantly. There were trends in the reduction of weekly caffeine and snack consumptions after 30 days for women in the ECA group compared to the control group, although statistically insignificant. Consumption of whole grains, red meat, and fish did not differ significantly between the two groups from baseline to follow-up. There was no significant difference in food knowledge, food insecurity, and breakfast consumption between groups (p = 0.15, p = 0.99, and p = 0.11, respectively).
Table 4.
Daily Food Consumption and Nutrition.
| Variable | Total Baseline (N = 61) n (%) |
Gabby Baseline (N = 31) n (%) |
Gabby Follow-up (N = 28) n (%) |
Control Baseline (N = 30) n (%) |
Control Follow-up (N = 29) n (%) |
p-valuea |
|---|---|---|---|---|---|---|
| Fruits | μ = 2 (σ = 1.1) | μ = 2 (σ = 1.1) | μ = 3 (σ = 1.1) | μ = 2 (σ = 1.1) | μ = 2 (σ = 0.9) | 0.04 |
| Vegetables | μ = 2 (σ = 1) | μ = 2 (σ = 1) | μ = 3 (σ = 0.9) | μ = 2 (σ = 1) | μ = 3 (σ = 1) | 0.74 |
| Soda | 0.34 | |||||
| No | 42 (69) | 21 (68) | 15 (54) | 21 (70) | 21 (72) | |
| Yes | 19 (32) | 10 (32) | 13 (46) | 9 (30) | 8 (28) | |
| Caffeine | 0.08 | |||||
| No | 4 (7) | 1 (3) | 3 (11) | 3 (10) | 2 (7) | |
| Yes | 56 (93) | 29 (97) | 25 (89) | 21 (70) | 27 (93) | |
| Snacks | 0.09 | |||||
| No | 2 (3) | 1 (3) | 6 (21) | 1 (3) | 1 (3) | |
| Yes | 59 (97) | 30 (97) | 22 (79) | 29 (97) | 28 (97) | |
| Whole Grains | 0.71 | |||||
| No | 3 (5) | 2 (7) | 1 (3) | 1 (3) | 1 (3) | |
| Yes | 58 (95) | 29 (93) | 27 (97) | 29 (97) | 28 (97) | |
| Red Meat | 0.72 | |||||
| No | 19 (31) | 12 (39) | 11 (39) | 7 (23) | 5 (17) | |
| Yes | 42 (69) | 19 (61) | 17 (61) | 23 (77) | 24 (83) | |
| Fish | 0.17 | |||||
| No | 18 (30) | 8 (26) | 11 (39) | 10 (33) | 9 (31) | |
| Yes | 43 (70) | 23 (74) | 17 (61) | 20 (67) | 20 (69) |
Continuous variables were analyzed using two-sample t-tests. Dichotomous variables were analyzed using two group McNemar tests of differential change for intervention and control groups.
3.2.4. Patient satisfaction of assigned intervention
At follow-up, participants were asked to evaluate their satisfaction of their assigned intervention based on topics of healthy eating, physical activity, and stress management (Table 5). Women favored using Gabby to improve stress management and increase physical activity more than women using patient information sheets. Sixty-nine percent utilized suggestions from Gabby to improve healthy eating, 52% to increase physical activity, and 70% to manage stress: all of which were greater–but not statistically significant–relative frequencies than participants using patient information sheets (66%, 49% and 66%, respectively). There was no significant difference in self-confidence to manage stress, to engage in physical activity, and to eat healthy between groups. Although statistically insignificant, duration of exercise increased in both groups for stretching/ strengthening (p = 0.18) and aerobic exercise (p = 0.27).
Table 5.
Satisfaction and Confidence in using Gabby versus Patient Information Sheets on Healthy Eating, Physical Activity and Stress Management.
| Variable | Gabby (N = 27) n (%) |
Patient Information Sheets (N = 29) n (%) |
p-valuea |
|---|---|---|---|
| How satisfied were you in using the resource for improving ….? | |||
| (1: Not Satisfied – 7: Very Satisfied) | |||
| Healthy Eating | μ = 5 (σ = 1.7) | μ = 5 (σ = 1.4) | 0.92 |
| Physical Activity | μ = 6 (σ = 1.8) | μ = 5 (σ = 1.5) | 0.62 |
| Stress Management | μ = 6 (σ = 1.8) | μ = 5 (σ = 1.6) | 0.07 |
| Did you use any of the suggestions from the resource to improve ….? | |||
| Healthy Eating | 18 (69) | 19 (66) | 0.93 |
| Physical Activity | 14 (52) | 14 (49) | 0.88 |
| Stress Management | 19 (70) | 19 (66) | 0.89 |
| Do you think that you will use some of the resource’s suggestions in the future to improve ….? | |||
| (1: Definitely No – 7: Definitely Yes) | |||
| Healthy Eating | μ = 6 (σ = 2) | μ = 6 (σ = 1.2) | 0.53 |
| Physical Activity | μ = 5 (σ = 2.1) | μ = 5 (σ = 1.7) | 0.94 |
| Stress Management | μ = 6 (σ = 1.9) | μ = 5 (σ = 2) | 0.29 |
| How confident do you feel that you can continue the changes you made based on the resource’s recommendations for ….? | |||
| (1: Not Confident – 7: Very Confident) | |||
| Healthy Eating | μ = 6 (σ = 1.3) | μ = 6 (σ = 1.4) | 0.10 |
| Physical Activity | μ = 6 (σ = 1.7) | μ = 6 (σ = 1.4) | 0.22 |
| Stress Management | μ = 6 (σ = 1.7) | μ = 6 (σ = 1.5) | 0.25 |
Continuous variables analyzed using two-sample t-tests. Categorical variables analyzed using Chi-square tests.
3.2.5. ECA system utilization
For one month, ECA users spent a median total of 52 min (interquartile range [IQR] = 101.4, N = 31) interacting with Gabby and logged in 5 times (IQR = 7, N = 31). The average time spent per individual session was 12.1 min (σ = 6.1, min = 3.9, max = 25.8).
3.3. Qualitative results
Findings suggest that most participants perceived the health information they received to be helpful, and intervention participants identified specific benefits and challenges to using an ECA. Users from both groups generally highlighted that their assigned intervention was very informative, easy to use, and served as a good reminder to keep their health status in check through mindfulness, physical activity and healthy eating. Interestingly, a majority of ECA users commented that Gabby was most relevant in regards to stress management. For example, intervention participants reported: “It definitely gave me more tools for stress management”"She helped me relax”, and “She reminded me to take care of myself even when I’m in the midst of a crazy work life”. Additionally, the majority of those who interacted with Gabby described her as empowering and relatable. One participant stated, “She relates to my stress … you can tailor it to your specific interests and needs”. In contrast, control group participants generally found it difficult to use the patient information sheets due to reported lack of accountability and follow-up. For example, some control group participants commented: “No accountability, no checking to see if you made improvements” and “Sheets were easy to ignore”.
For the intervention group only, participants highlighted specific benefits and challenges to using the ECA system. The majority of users perceived Gabby to be a fast, reliable, and credible source of information. Participants’ comments to support this finding included: “The right answer is always there no matter what … I don’t have to wait for a doctor” and “I did not think she shared incorrect or unsupportive info”. Challenges using the Gabby system included the sound and quality of her voice, time commitment to use the system, and program accessibility. Several participants described Gabby’s voice as “robotic”; one participant in particular commented that they “could not stand how slowly she talked”. Intervention participants also found it difficult “having the time and sitting in front of the computer to do it”, and highlighted her laptop and desktop accessibility limitations, stating “she was only on a computer, not a phone”.
4. Discussion and conclusion
4.1. Discussion
In this study, we demonstrated that it is feasible to use ECA technology to deliver multiple healthy lifestyle recommendations on physical activity, healthy eating, mindfulness, and stress management techniques among diverse urban women. Among our study sample, interaction with an ECA was shown to be effective in decreasing alcohol consumption for stress and increasing daily fruit consumption. There was also a trend increase in the number of stress management techniques used.
Adherence to a healthy lifestyle includes stress management; however, fewer than 10% of adults in the United States follow this pattern, including women [46]. Gabby users reported utilizing more stress management techniques from baseline, and 70% of them responded that they used Gabby’s suggestions to improve their stress. In the qualitative data, both groups reported being more knowledgeable about managing their stress post-intervention. Similarly, one pilot study implemented a virtual coach to provide mindfulness training, and found that participants who had coach-based training performed the techniques more effectively and regularly than participants who had to teach themselves the same techniques using paper and audio materials [22]. There was no statistically significant difference in perceived stress among women in the Gabby group compared to the control group. However, our study was not adequately powered to detect such a difference; therefore, an adequately powered clinical trial is necessary to determine efficacy in stress reduction.
Our results also show a significant decrease in alcohol use for stress management (63%) for women who interacted with Gabby compared to the control group. Research has found the use of technologies among non-dependent alcoholic drinkers to be promising [47, 48]. In several studies to reduce alcohol use among college students, participants who received tailored text messages were more likely to report a reduction in alcohol consumption and an increased awareness to manage drinking behaviors [49–51]. Furthermore, mindfulness training has been shown to help decrease stress levels and as a result, may partially decrease engagement in alcohol use [52–55]. In light of our findings and previous studies, we believe that aspects of Gabby, including personalization and face-to-face engagement [16], may promote healthy decision making on stress management among its users. More research is needed to prioritize which aspects of the system are important in supporting patients beyond the dissemination of information on stress management.
Generally, healthy eating habits improved in both the intervention and control groups. Specifically, increased fruit consumption was statistically significant for Gabby users. Only 13% of the adults in the United States consume the recommended daily amount of fruits (4 to 5 servings) [56, 57]. Very few technologies have been developed to support healthy eating habits among disparate populations: one study found that a web-based nutrition program led to increased–but not statistically significant–fruit consumption compared to a traditional in-person nutrition education among low-income adults [58]; another study revealed that female ethnic minority college students ate more servings of fruit when they received motivational text messages [59]. With Gabby, we find that women were actually consuming an increased amount of fruit servings relative to those who were given patient information sheets–results consistent with these two studies mentioned above.
Based on our qualitative feedback, we believe that users would have utilized the ECA system more had it been available on multiple technology platforms, such as mobile devices. With smartphone ownership increasing steadily [60], having the Gabby system installed on a frequently used device would provide more opportunities for patients to engage in learning and practicing meaningful health behaviors. Use of technology, such as having access to the Internet or owning cell phones with data, is common among underserved racially diverse populations [5]. The National Standards for Culturally and Linguistically Appropriate Services in Health and Health Care encourage healthcare organizations and providers to use multimedia when communicating health information to culturally diverse patients [61]. However, more information is needed on how technology can be used to create healthy behavior changes for such racially and culturally diverse patient populations.
Limitations to this feasibility study include a small sample size, short duration of the intervention, specific inclusion criteria, and self-reported information. By including only women who had access to the internet, we may have biased the sample towards women who have favorable use of technology. The Gabby system was also developed in English, excluding participants who are not fluent in English. Lastly, participants could have inaccurately reported their health behaviors due to a lack of knowledge or feeling uncomfortable sharing information with a web-based system.
4.2. Conclusion
Feasibility data on the Gabby system are encouraging, and show that ECA technology can help improve education on lifestyle information on physical activity, healthy eating, mindfulness and stress management methods for diverse, urban women.
4.3. Practice implications
In medical settings, clinicians give patients after-visit summary plans that usually include patient information sheets. ECAs are an encouraging way to provide patient information in a customized interactive format. ECAs may help patients adhere to behavioral changes through improved decision making and experiential learning as opposed to passive reading.
Acknowledgments
Funding
This work was supported by the National Center for Complementary & Integrative Health (Grant Number K07AT005463, 2016). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Complementary & Alternative Medicine or the National Institutes of Health.
Appendix A. Dialogue Script
Gabby: Hi there! My name is Gabrielle, but you can call me Gabby. (pause 2 s)
On the right hand side of the screen you will see some buttons, just let me know that you can see them by pressing on any one of the responses.
Hi Gabby!
Okay
Could you repeat that?
Gabby: <USER’s NAME>, have I got that right?
Yes!
No
Gabby: Great. So, <USER’s NAME>, I’m here every day to go over topics for your health! I want our interactions to be like a conversation. I am here to support you as you learn new ways to care for your health.
Okay
Could you repeat that?
Each time we meet I will offer you a menu of topics to choose from. By asking you questions and listening to your responses, I will be able to coach you better. Answer my questions by clicking the buttons I show on the right side of your screen. The only way for our chats to move forward will be by you pressing a button.
Sounds good
I can do that
Could you repeat that?
Gabby: It is fun for me to share pictures and tips with you about stress, nutrition, and exercise.
Sounds fun!
Okay
Could you repeat that?
Gabby: I am excited to take this journey to better health with you. Together we are team. I hope that you can check in with me daily. But that’s up to you! The more time we spend together the more I can support you in the changes you are making in reducing your stress and improving your health.
Great
Okay
Could you repeat that?
Appendix B. Nutrition Knowledge Quiz
The following questions are about food knowledge:
Please answer true or false.
-
34
Beans contain only a few useful nutrients, therefore their health benefit is not great. T F
-
35
A healthy meal should consist of half meat, a quarter vegetables, and a quarter side dishes. T F
-
36
Fat is always bad for your health; you should therefore avoid all fat. T F
-
37
Oily fish (salmon, mackerel) contain healthier fats than red meat. T F
-
38
How much folic acid should women of childbearing age take every day to help prevent birth defects?
-
□
None
-
□
200 micrograms (mcg)
-
□
400 micrograms (mcg)
-
□
1000 micrograms (mcg)
-
□
-
39
Good advice for eating healthy includes all of the following except?
-
□
Cut back on foods with added sugars, salt and fat.
-
□
Eat fish 1–2 times a week
-
□
Save half your plate for fruits and vegetables.
-
□
Eat packaged foods
-
□
Snack on nuts like almonds
-
□
-
40
How many servings of fruits and veggies should you get each day?
-
□
1 servings
-
□
2 servings
-
□
5 servings
-
□
10 servings
-
□
Another amount: ____ servings
-
□
-
41
What 1 vitamin or mineral is important for having strong bones?
-
□
Calcium
-
□
Iron
-
□
Omega-3 Fatty Acids
-
□
Fiber
-
□
Vitamin B
-
□
-
42
What 1 vitamin or mineral is most important for having healthy blood?
-
□
Calcium
-
□
Iron
-
□
Omega-3 Fatty Acids
-
□
Fiber
-
□
Vitamin B
-
□
-
43
What are some good sources of omega-3 fatty acids?
-
□
Fish
-
□
Walnuts
-
□
Olive oil
-
□
Avocados
-
□
All of the above
-
□
Footnotes
Conflict of interest
The authors declare no conflict of interest.
Authors’ contributions
Contributions were as follow: PMG, BWJ, LYN and TWB contributed to conception of the study; KDM managed data collection; PMG, LMN, LFW, and TC conducted data analyses; TC and PMG drafted the manuscript; PMG, TC, KDM, LFW, TWB, and LYN revised the manuscript critically. All authors have read and approved the final version for submission.
Statements
The authors confirm all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the story.
References
- 1.Buck ML. Providing patients with written medication information. Ann. Pharmacother. 1998;32:962–969. doi: 10.1345/aph.17455. [DOI] [PubMed] [Google Scholar]
- 2.Harvey I, O'Brien M. Addressing health disparities through patient education: the development of culturally-tailored health education materials at Puentes de Salud. J. Community Health Nurs. 2011;28:181–189. doi: 10.1080/07370016.2011.614827. [DOI] [PubMed] [Google Scholar]
- 3.Kutner M, Greenburg E, Jin Y, Paulsen C. National Center for Education Statistics. 2006. The Health Literacy of America's Adults: Results from the 2003 National Assessment of Adult Literacy. NCES 2006-483. [Google Scholar]
- 4.Khusid MA, Vythilingam M. The emerging role of mindfulness meditation as effective self-management strategy, part 1: clinical implications for depression, post-traumatic stress disorder, and anxiety. Mil. Med. 2016;181:961–968. doi: 10.7205/MILMED-D-14-00677. [DOI] [PubMed] [Google Scholar]
- 5.Gibbons CM. Use of health information technology among racial and ethnic underserved communities. Perspect. Health Inf. Manag. 2011 Winter;8 [PMC free article] [PubMed] [Google Scholar]
- 6.Matthews J, Win KT, Oinas-Kukkonen H, Freeman M. Persuasive technology in mobile applications promoting physical activity: a systematic review. J. Med. Syst. 2016;40:72. doi: 10.1007/s10916-015-0425-x. [DOI] [PubMed] [Google Scholar]
- 7.Harris J, Felix L, Miners A, Murray E, Michie S, Ferguson E, Free C, Lock K, Landon J, Edwards P. Adaptive e-learning to improve dietary behavior: a systematic review and cost-effectiveness analysis. Health Technol. Assess. 2011;15:1–8. doi: 10.3310/hta15370. doi:http://dx.doi.org/10.3310/hta15370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Monroe CM, Bassett DR, Jr, Fitzhugh EC, Raynor HA, Thompson DL. Effect of adding online social support tools to an adult walking program: a pilot randomized controlled trial. Health Promot. Pract. 2016 doi: 10.1177/1524839915626674. [DOI] [PubMed] [Google Scholar]
- 9.King AC, Bickmore TW, Campero MI, Pruitt LA, Yin JL. Employing virtual advisors in preventive care for underserved communities: results from the COMPASS study. J. Health Commun. 2013;18:1449–1464. doi: 10.1080/10810730.2013.798374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosal MC, Heyden R, Mejilla R, Capelson R, Chalmers KA, Rizzo DePaoli M, Veerappa C, Wiecha JM. A virtual world versus face-to-face intervention format to promote diabetes self-management among african american women: a pilot randomized clinical trial. JMIR Res. Protoc. 2014;24:e54. doi: 10.2196/resprot.3412. doi: http://dx.doi.org/10.2196/resprot.3412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Valle CG, Deal AM, Tate DF. Preventing weight gain in African American breast cancer survivors using smart scales and activity trackers: a randomized controlled pilot study. J. Cancer Surviv. 2016:1–16. doi: 10.1007/s11764-016-0571-2. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bickmore TW, Schulman D, Sidner C. Automated interventions for multiple health behaviors using conversational agents. Patient Educ. Couns. 2013;92:142–148. doi: 10.1016/j.pec.2013.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bickmore T, Gruber A, Picard R. Establishing the computer-patient working alliance in automated health behavior change interventions. Patient Educ. Couns. 2005;59:21–30. doi: 10.1016/j.pec.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 14.Bickmore T, Giorgino T. Health dialog systems for patients and consumers. J. Biomed. Inform. 2006;39:556–571. doi: 10.1016/j.jbi.2005.12.004. (Epub 2006 Jan. 20) [DOI] [PubMed] [Google Scholar]
- 15.Bickmore TW, Puskar K, Schlenk EA, Pfeifer LM, Sereika SM. Maintaining reality: relational agents for antipsychotic medication adherence. Interact. Comput. 2010;22:276–288. [Google Scholar]
- 16.Gardiner P, Hempstead MB, Ring L, Bickmore T, Yinusa-Nyahkoon L, Tran H, Paasche-Orlow M, Damus K, Jack B. Reaching women through health information technology: the Gabby preconception care system. Am. J. Health Promot. 2013;27:eS11–20. doi: 10.4278/ajhp.1200113-QUAN-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bickmore TW, Pfeifer LM, Byron D, Forsythe S, Henault LE, Jack BW, Silliman R, Paasche-Orlow MK. Usability of conversational agents by patients with inadequate health literacy: evidence from two clinical trials. J. Health Commun. 2010;15:197–210. doi: 10.1080/10810730.2010.499991. [DOI] [PubMed] [Google Scholar]
- 18.Ehrenfeld J, Sandberg W, Warren L, Kwo J, Bickmore T. Use of a computer agent to explain anesthesia concepts to patients. Annual Meeting of the American Society of Anesthesiologists. 2010;3 [Google Scholar]
- 19.Bickmore TW, Pfeifer LM, Jack BW. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems 2009. ACM; 2017. Taking the time to care: empowering low health literacy hospital patients with virtual nurse agents; pp. 1265–1274. [Google Scholar]
- 20.Ellis T, Latham N, DeAngelis T, Thomas CA, Saint-Hilaire M, Bickmore TW. Feasibility of a virtual exercise coach to promote walking in community-dwelling persons with Parkinson Disease. Am. J. Phys. Med. Rehabil. 2013;92:472–485. doi: 10.1097/PHM.0b013e31828cd466. quiz 482-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bickmore TW, Silliman RA, Nelson K, Cheng DM, Winter M, Henault L, Paasche-Orlow MK. A randomized controlled trial of an automated exercise coach for older adults. J. Am. Geriatr. Soc. 2013;61:1676–1683. doi: 10.1111/jgs.12449. [DOI] [PubMed] [Google Scholar]
- 22.Hudlicka E. Virtual training and coaching of health behavior: example from mindfulness meditation training. Patient Educ. Couns. 2013;92:160–166. doi: 10.1016/j.pec.2013.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morie JF, Antonisse J, Bouchard S, Chance E. Virtual worlds as a healing modality for returning soldiers and veterans. Stud. Health Technol. Inform. 2009;144:273–276. [PubMed] [Google Scholar]
- 24.Jack B, Bickmore T, Hempstead M, Yinusa-Nyahkoon L, Sadikova E, Mitchell S, Gardiner P, Adigun F, Penti B, Schulman D, Damus K. Reducing preconception risks among African American women with conversational agent technology. J. Am. Board Fam. Med. 2015;28:441–451. doi: 10.3122/jabfm.2015.04.140327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gardiner PM, Nelson L, Shellhaas CS, Dunlop AL, Long R, Andrist S, Jack BW. The clinical content of preconception care: nutrition and dietary supplements. Am. J. Obstet. Gynecol. 2008;199:S345–56. doi: 10.1016/j.ajog.2008.10.049. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization. Promoting Fruit and Vegetable Consumption Around the World. Global Strategy on Diet. [Accessed Sept 10 2016];Physical Activity and Health. 2016 Retrieved from http://www.who.int/dietphysicalactivity/fruit/en/
- 27.Department of Nutrition. Harvard School of Public Health. [Accessed Sept 10 2016];Healthy Eating Plate & Healthy Eating Pyramid. The Nutrition Source. 2016 Retrieved from https://www.hsph.harvard.edu/nutritionsource/healthy-eating-plate/
- 28.National Institute of Diabetes and Digestive and Kidney Diseases. Diabetes Prevention Program. Diabetes. Diabetes Prevention Program; 2008. [Accessed Sept 10 2016]. Retrieved from https://www.niddk.nih.gov/about-niddk/research-areas/diabetes/diabetes-prevention-program-dpp/Pages/default.aspx. [Google Scholar]
- 29.Reiner K, Tibi L, Lipsitz JD. Do mindfulness-based interventions reduce pain intensity? A critical review of the literature. Pain Med. 2013;14:230–242. doi: 10.1111/pme.12006. [DOI] [PubMed] [Google Scholar]
- 30.Cramer H, Haller H, Lauche R, Dobos G. Mindfulness-based stress reduction for low back pain: a systematic review. BMC Complement. Altern. Med. 2012;12:162. doi: 10.1186/1472-6882-12-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Niazi AK, Niazi SK. Mindfulness-based stress reduction: a non-pharmacological approach for chronic illnesses. N. Am. J. Med. Sci. 2011;3:20–23. doi: 10.4297/najms.2011.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fjorback L, Arendt M, Ørnbøl E, Fink P, Walach H. Mindfulness-based stress reduction and mindfulness-based cognitive therapy – a systematic review of randomized controlled trials. Acta Psychiatr. Scand. 2011;124:102–119. doi: 10.1111/j.1600-0447.2011.01704.x. [DOI] [PubMed] [Google Scholar]
- 33.Cavanagh K, Strauss C, Cicconi F, Griffiths N, Wyper A, Jones F. A randomized controlled trial of a brief online mindfulness-based intervention. Behav. Res. Ther. 2013;51:573–578. doi: 10.1016/j.brat.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 34.Glück TM, Maercker A. A randomized controlled pilot study of a brief web-based mindfulness training. BMC Psychiatry. 2001;1(11):175. doi: 10.1186/1471-244X-11-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Krusche A, Cyhlarova E, Williams JMG. Mindfulness online: an evaluation of the feasibility of a web-based mindfulness course for stress, anxiety and depression. BMJ Open. 2013;3:e003498. doi: 10.1136/bmjopen-2013-003498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Morledge TJ, Allexandre D, Fox E, Fu AZ, Higashi MK, Kruzikas DT, Pham SV, Reese PR. Feasibility of an online mindfulness program for stress management—a randomized, controlled trial. Ann. Behav. Med. 2013;46:137–148. doi: 10.1007/s12160-013-9490-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.US Department of Health and Human Services. Physical Activity Guidelines for Americans. US Department of Health and Human Services; 2008. [Google Scholar]
- 38.Centers for Disease Control and Prevention. How Much Physical Activity Do Adults Need? [Accessed Sept 10 2016];Physical Activity. 2015 Retrieved from http://www.cdc.gov/physicalactivity/basics/adults/index.htm.
- 39.Ware JE, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med. Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 40.Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr. Ann. 2002;32:509–515. [Google Scholar]
- 41.National Center for Health Statistics (US) National Health and Nutrition Examination Survey, US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. 2008. [Google Scholar]
- 42.Coates J, Swindale A, Bilinsky P. Food and Nutrition Technical Assistance Project. Academy for Educational Development; Washington, DC: 2007. Household Food Insecurity Access Scale (HFIAS) for Measurement of Food Access: Indicator Guide. [Google Scholar]
- 43.Stanford Patient Education Research Center, Exercise Behaviors. [Accessed on Sept 10 2016];Research Instruments Developed, Adapted or Used by the Stanford Patient Education Research Center. 2017 Retrieved from http://patienteducation.stanford.edu/research/exercise.pdf.
- 44.Resnick B, Jenkins LS. Testing the reliability and validity of the self-efficacy for exercise scale. Nurs. Res. 2000;49:154–159. doi: 10.1097/00006199-200005000-00007. [DOI] [PubMed] [Google Scholar]
- 45.Cohen S, Williamson G. Perceived stress in a probability sample of the United States. Soc. Psychol. Health. 1988;3:1–67. [Google Scholar]
- 46.King DE, Mainous AG, III, Carnemolla M, Everett CJ. Adherence to healthy lifestyle habits in US adults, 1988–2006. Am. J. Med. 2009;122:528–534. doi: 10.1016/j.amjmed.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 47.Sankaranarayanan J, Sallach RE. Rural patients' access to mobile phones and willingness to receive mobile phone-based pharmacy and other health technology services: a pilot study. Telemed. J. E Health. 2014;20:182–185. doi: 10.1089/tmj.2013.0150. [DOI] [PubMed] [Google Scholar]
- 48.Fowler LA, Holt SL, Joshi D. Mobile technology-based interventions for adult users of alcohol: a systematic review of the literature. Addict. Behav. 2016;62:25–34. doi: 10.1016/j.addbeh.2016.06.008. [DOI] [PubMed] [Google Scholar]
- 49.Mason M, Ola B, Zaharakis N, Zhang J. Text messaging interventions for adolescent and young adult substance use: a meta-analysis. Prev. Sci. 2015;16:181–188. doi: 10.1007/s11121-014-0498-7. [DOI] [PubMed] [Google Scholar]
- 50.Witkiewitz K, Desai SA, Bowen S, Leigh BC, Kirouac M, Larimer ME. Development and evaluation of a mobile intervention for heavy drinking and smoking among college students. Psychol. Addict. Behav. 2014;28:639–650. doi: 10.1037/a0034747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Weitzel JA, Bernhardt JM, Usdan S, Mays D, Glanz K. Using wireless handheld computers and tailored text messaging to reduce negative consequences of drinking alcohol. J. Stud. Alcohol Drugs. 2007;68:534–537. doi: 10.15288/jsad.2007.68.534. [DOI] [PubMed] [Google Scholar]
- 52.Bodenlos JS, Noonan M, Wells SY. Mindfulness and alcohol problems in college students: the mediating effects of stress. J. Am. Coll. Health. 2013;61:371–378. doi: 10.1080/07448481.2013.805714. [DOI] [PubMed] [Google Scholar]
- 53.Zgierska A, Rabago D, Chawla N, Kushner K, Koehler R, Marlatt A. Mindfulness meditation for substance use disorders: a systematic review. Subst. Abus. 2009;30:266–294. doi: 10.1080/08897070903250019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sinha R. The role of stress in addiction relapse. Curr. Psychiatry Rep. 2007;9:388–395. doi: 10.1007/s11920-007-0050-6. [DOI] [PubMed] [Google Scholar]
- 55.Marcus MT, Fine PM, Moeller FG, Khan MM, Pitts K, Swank PR, Liehr P. Changes in stress levels following mindfulness based stress reduction in a therapeutic community. Addict. Disord. Their Treat. 2003;2:63–68. [Google Scholar]
- 56.American Heart Association, Suggested Servings from Each Food Group. [Accessed Feb 15 2017];Healthy Living. 2015 Retrieved from http://www.heart.org/HEARTORG/HealthyLiving/HealthyEating/HealthyDietGoals/Suggested-Servings-from-Each-Food-Group_UCM_318186_Article.jsp#.WKR36tIrKUl.
- 57.Centers for Disease Control and Prevention. [Accessed Feb 15 2017];Overview: BRFSS 2013. Behavioral Risk Factor Surveillance System. 2013 Retrieved from http://www.cdc.gov/brfss/annual_data/2013/pdf/overview_2013.pdf.
- 58.Neuenschwander LM, Abbott A, Mobley AR. Comparison of a web-based vs in-person nutrition education program for low-income adults. J. Acad. Nutr. Diet. 2013;113:120–126. doi: 10.1016/j.jand.2012.07.034. [DOI] [PubMed] [Google Scholar]
- 59.Rodgers RF, Pernal W, Matsumoto A, Shiyko M, Intille S, Franko DL. Capitalizing on mobile technology to support healthy eating in ethnic minority college students. J. Am. Coll. Health. 2016;64:125–132. doi: 10.1080/07448481.2015.1085055. [DOI] [PubMed] [Google Scholar]
- 60.Poushter J. Smartphone Ownership and Internet Usage Continues to Climb in Emerging Economies. Pew Research Center: Global Attitudes & Trends. 2016 [Google Scholar]
- 61.Office of Minority Health. National Standards for Culturally and Linguistically Appropriate Services (CLAS) in Health and Health Care: A Blueprint for Advancing and Sustaining CLAS Policy and Patience. US Department of Health and Human Services; Washington (DC): 2013. [Google Scholar]