Abstract
Background: Underweight chronic obstructive pulmonary disease (COPD) patients with involuntary weight loss have a poor prognosis; no effective therapy is currently available. We conducted the first clinical trial seeking to determine whether combination therapy with an appetite stimulant and an anabolic steroid would have beneficial effects on body composition for patients with COPD cachexia.
Methods: We conducted a 12–week pilot study in which 4 men and 5 women (age 64±10 y, forced expiratory volume in 1 second [FEV1] 31±9 %pred., body mass index [BMI] 18±3 kg/m2) with low-normal testosterone levels (average 532±45ng/dl in men and 12.4±5.3ng/dl in women) and weight loss ≥10 lbs over the previous year were treated with oral megestrol acetate 800mg/day plus weekly testosterone enanthate injections, initially 125 mg in men and 40 mg in women, with doses subsequently adjusted targeting circulating nadir testosterone levels of 850 and 300 ng/dl, respectively.
Results: On treatment, nadir testosterone level increases averaged 160±250 ng/dl (NS) in men and 322±49 (p<0.001) ng/dl in women. Body weight increased in all individuals, with average end-intervention weight gain of 3.1±2.2 kg (p<0.005). Two women and 2 men had COPD exacerbations and did not complete the 12-week study. In the 5 individuals who completed, dual energy x ray absorptiometry (DEXA) scans revealed an average 2.0±1.5 kg lean mass and 2.3±1.7 kg fat mass increase (each p<0.05). No adverse effects of treatment were detected.
Conclusions: Combination therapy reversed the trajectory of involuntary weight loss and increased lean mass in cachectic COPD patients. Though the interventions were apparently well tolerated, participant drop-out rate was high. Larger randomized placebo-controlled long-term studies with functional outcomes are needed.
Keywords: body composition, cachexia, chronic obstructive pulmonary disease, megesterol, testosterone
Introduction
Note: Parts of the findings of this study were presented at the European Respiratory Society Annual Meeting in Amsterdam in 2011.
Recent consensus guidelines have refined the definition of cachexia, a manifestation of the end-stage of a number of chronic diseases.1 Involuntary weight loss is central to the definition. In addition, other manifestations are commonly seen, including decreased muscle strength, fatigue, anorexia, low muscle mass and abnormal biochemistry (e.g., elevation of circulating inflammatory markers, anemia, low albumin).
Cachexia is a complication of advanced stages of chronic obstructive pulmonary disease (COPD), associated with high mortality and poor health-related quality of life.2 The prevalence of COPD cachexia in the United States has been estimated to be as high as 3.2 million individuals3 but such estimates reflect much less rigorous definitions than that given above; the prevalence is undoubtedly lower.4-8 No therapies have been demonstrated to improve outcomes in COPD cachexia. In particular, nutritional supplementation of underweight COPD patients has generally been shown to have no or only modest effect on body weight or functionality.9,10 Further, the mechanisms underlying COPD cachexia (and of the cachexia syndrome in general) remain unclear.3,11
Acknowledging the limitations of therapy in a condition in which the underlying mechanisms are unclear, we reasoned that improving appetite and increasing skeletal muscle mass would be important therapeutic targets and that a combination of pharmacologic agents might hold promise. As one agent, we chose megestrol acetate which has been shown to improve appetite in underweight COPD patients12 as well as in patients with other chronic diseases and cancer.13-16 In a multicenter double-blind placebo controlled trial of megestrol acetate in 145 underweight COPD patients with average body mass index (BMI) of 18.3 kg/m2, 800 mg/day of megestrol acetate for 2 months increased appetite and body weight.12 However, megestrol acetate substantially decreased serum testosterone levels, denying these patients the anabolic stimulus needed to utilize consumed nutritional intake to build muscle. As a result, the weight gain following megestrol acetate administration is mainly increased body fat and not muscle mass.12,17-20
As a second agent, we chose the anabolic steroid, testosterone, for its anabolic effects on muscle in patients with chronic disease, including those with cachexia.21-25Anabolic steroids, however, yield decline in body fat mass26 that, in itself, may be detrimental in cachectic patients, in whom loss of fat mass is often marked.
We hypothesized that combined administration of testosterone and megestrol acetate would be capable of reversing the trajectory of involuntary weight loss in men and women with COPD cachexia through increase in both lean and fat mass. In order to examine this hypothesis, we conducted a 12-week pilot study, in which we examined changes in body weight and body composition following combined administration of testosterone and megestrol acetate to patients with COPD cachexia.
Methods
We performed a prospective, single group longitudinal interventional study with outcome measures planned before, during and after 12 weeks treatment administration.
Participant Selection
This study received approval from the Los Angeles Biomedical Research Institute Institutional Review Board; participants provided written informed consent. Participants were men and women with COPD aged between 55 and 85 years who had a BMI ≤22 kg/m2 for men and ≤20 kg/m2 for women accompanied by a history of at least 10 lbs (4.5 kg) weight loss over the previous year, documented by review of medical records (including pulmonary function laboratory records). They also subjectively had fatigue as a prominent symptom and presented with anorexia. Further inclusion criteria were that participants had forced expiratory volume in one second (FEV1) ≤55 % predicted.27 Participants were included if testosterone at screening was in the low ranges of normal or reduced: ≤600 ng/dl in men and ≤40 ng/dl in women. Participants needed to be capable of attending weekly visits to the research center and could not have had an exacerbation within 4 weeks prior to screening. Participants could not be participating in a formal exercise program. Individuals were excluded if they had clinically significant cardiovascular disease (e.g., uncontrolled hypertension, congestive heart failure, peripheral vascular disease, exertional angina, complex arrhythmias, or ischemic changes on stress electrocardiogram), history of hypercoagulable state, deep venous thrombosis or pulmonary embolism, history of diabetes mellitus or endocrine disorders associated with hypogonadism (e.g., pituitary tumors, hyperprolactinemia), history of heavy alcohol or illegal drug use. Men were excluded who had symptomatic prostatic hyperplasia, history of prostate cancer or serum prostate specific antigen (PSA) levels >4μg/L or prostate exam at screening suggestive of prostate cancer; women were excluded for history of breast or uterine cancer within 10 years. We also excluded individuals with hematocrit >48%, those with elevation in transminase levels (AST or ALT > twice the upper limit of normal), with neurologic impairment (e.g., Parkinson's disease, stroke) or with mental states that would preclude protocol compliance (e.g., senile dementia), or who required oral prednisone at >10 mg/day, had neoplastic disease anticipated to influence survival, or had used an investigational agent or appetite stimulant within 30 days of enrollment.
Testosterone Administration and Dose Adjustment
Male participants received an initial dose of 125 mg of testosterone enanthate (Paddock, Laboratories, Minneapolis, Minnesota) by intramuscular injection weekly. This dose was mildly higher than the dose chosen for our previous study of COPD men (100 mg/week),26 which resulted in nadir (immediately before the next dose) circulating testosterone levels in the lower ranges of those seen in healthy young men (500-1000 ng/dl). We reasoned that a somewhat higher dose would be needed to counteract the tendency for megesterol acetate to dramatically decrease endogenous testosterone production.12 In female participants, an initial weekly dose was 40 mg, somewhat higher than the 25 mg dose we found capable of increasing circulating testosterone levels to above the physiologic range in older women (roughly 100 ng/dl) without yielding virilization.28 Testosterone levels were obtained immediately before the second and fourth injections and dose adjustments applied (if necessary) with the third and fifth injections targeting a level of 800 and 350 ng/dl in men and women, respectively. Testosterone administration was held on the week following a scheduled measurement if testosterone level was >1500 ng/dl in men or >500 ng/dl in women. Subsequently, testosterone dose was adjusted.
Megestrol Acetate Administration
Megestrol acetate was administered in liquid form at a dose of 800 mg/day (Par Pharmaceuticals, Woodcliff Lake, New Jersey). Compliance was assessed by weighing bottles returned at each visit. Serum cortisol was monitored at weeks 4 and 8 of the intervention and participants took declining doses in the 4 weeks following the 12-week intervention to avoid the possibility of adrenal insufficiency.
Advising on Dietary Intake
Participants completed a 3-day food record prior to the intervention period and were counseled by a nutritionist to consume a balanced diet and to increase caloric intake.
Assessments
Spirometry was performed after inhalation of 4 puffs of albuterol29; lung volumes by body plethysmography and diffusing capacity by single breath carbon monoxide uptake (DLCO) (Vmax 229 and Autobox 6200; SensorMedics; Yorba Linda, California) were performed according to American Thoracic Society (ATS)/ European Respiratory Society (ERS) standards.30,31 Whole body mass, fat mass and bone mineral mass were measured by dual emission x-ray absorptiometry (DEXA) (Hologic fan-beam QDR-4500-Delphi-A; software used was QDR version 12.4, Hologic Inc., Bedford, Massachusetts); non-fat non-bone (designated as lean) mass was calculated by subtraction.
Participants were evaluated for adverse events at each weekly visit. Specifically, women were carefully examined for signs of virilization and men had a PSA level drawn after 6 and 12 weeks. Transaminase levels were monitored 4 and 8 weeks after the start of the intervention.
Statistical Analysis
Data were entered in Microsoft Excel (Microsoft Corporation, Redmond, Washington). For statistical analyses and graphical display, SigmaPlot 12.0 (Systat Software, Inc., Chicago, Illinois) was used. Dispersion about the mean was expressed as ±SD in the text and ±SE in the figures. Change from baseline conditions was evaluated by paired t-tests. Statistical significance was set at p <0.05. A formal power analysis to establish sample size was not conducted in this pilot study.
Results
A total of 16 patients were screened for this study. Six did not meet inclusion/exclusion criteria and 1 withdrew during screening. Four men and 5 women entered the study protocol; 5 were Caucasian, 3 African-American and 1 Asian. Of these 9 participants, 2 men and 2 women were hospitalized for COPD exacerbation or pneumonia during the 12-week study and therefore, did not complete all post-intervention measures; one of these participants died 7 days after hospital admission. One participant elected to exit the study at 10 weeks and 1 at 11 weeks; both completed post-intervention measures. Table 1 describes the characteristics of the 9 individuals who entered the study. Baseline body weight was 52.8±13.1 kg; BMI was 18.4±3.4 kg/m2; both fat mass index and fat-free mass index were low. Mean FEV1 and DLCO were 31.3 and 35.2 percent predicted, respectively, consistent with severe to very severe COPD.
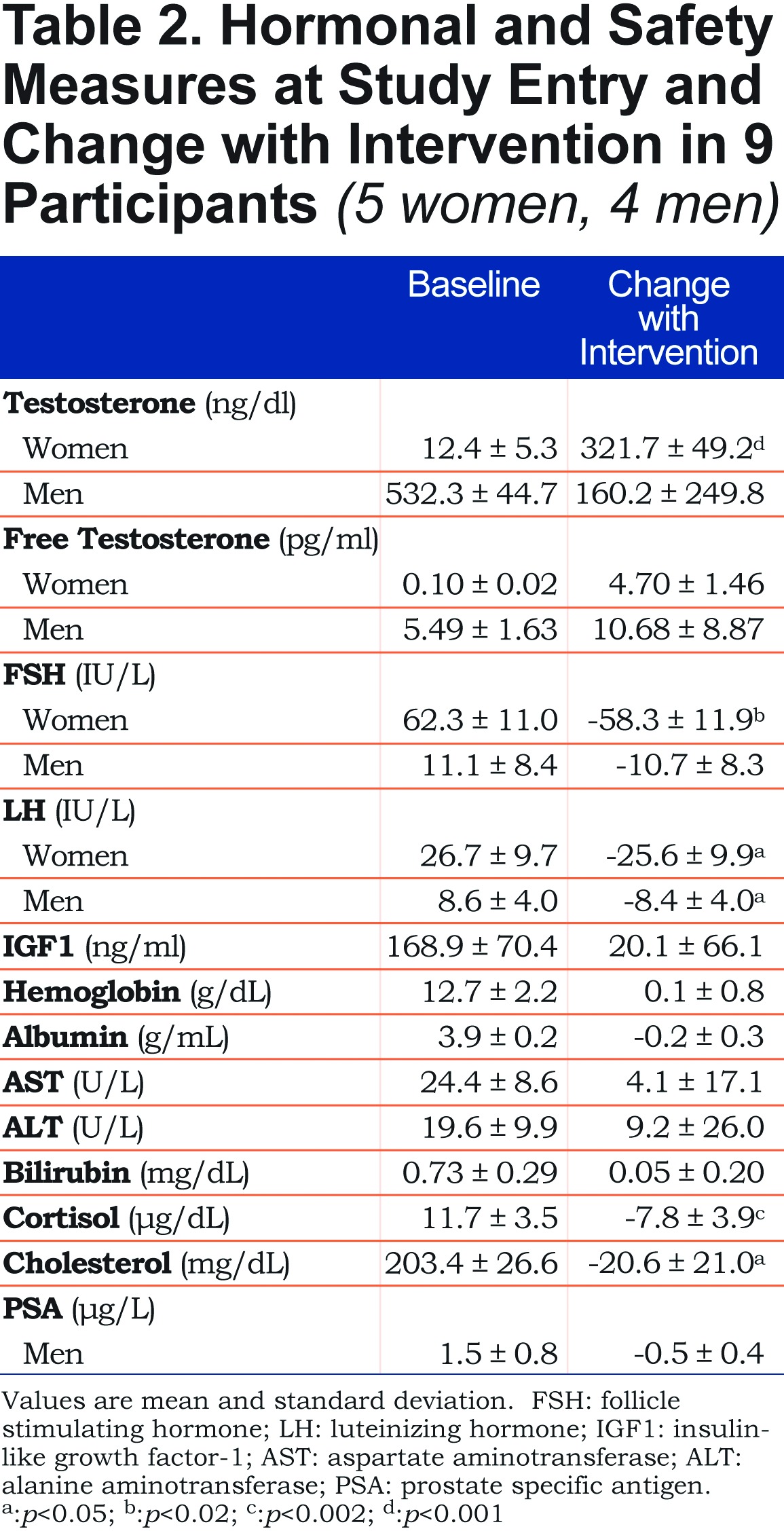
As a result of dose adjustments, the 5 women received an average weekly testosterone entanthate dose of 42±7 mg; the 4 men received 140±58 mg. Table 1 shows serum testosterone levels before and during the treatment with testosterone plus megestrol. During treatment, levels are averaged values from samples drawn just prior to the next dose (nadir level) at several visits. In men, weekly injection of testosterone enanthate increased the mean serum testosterone level from 532±45 ng/d at baseline to a nadir value of 693±120 ng/dl, though this increase did not achieve statistical significance. In women, mean serum testosterone level increased from 12±5 ng/dl to a nadir value of 334±72 ng/dl (p<0.001). Free testosterone increases paralleled increases in testosterone levels in both men and women. As expected, exogenous testosterone administration inhibited both luteinizing and follicle stimulating hormone secretion in both men and women. Insulin-like growth factor-1, the predominant mediator of growth hormone’s action on muscle, did not change significantly. Cortisol levels fell by an average of 67%, consistent with previous reports of megestrol acetate administration.12
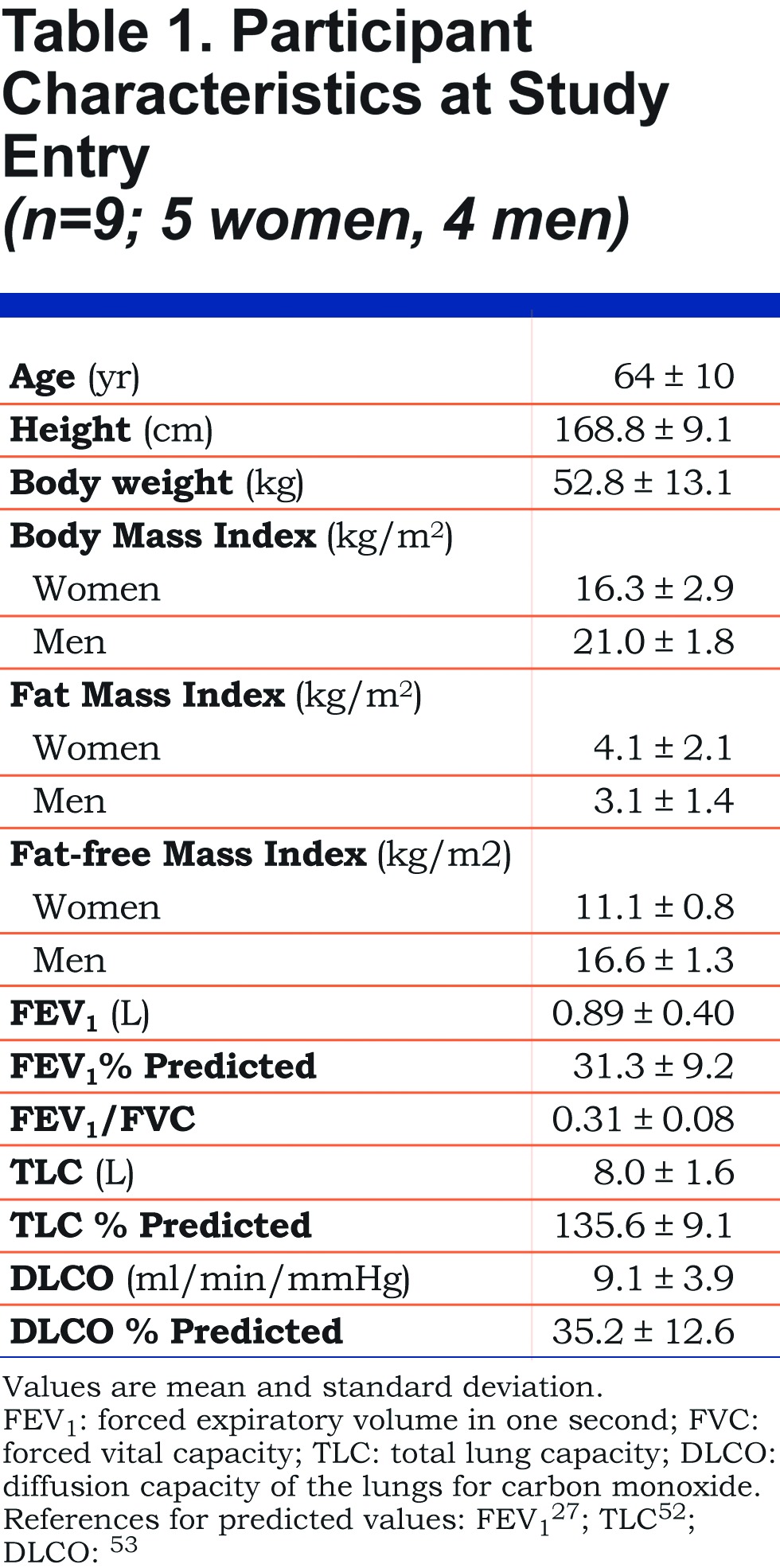
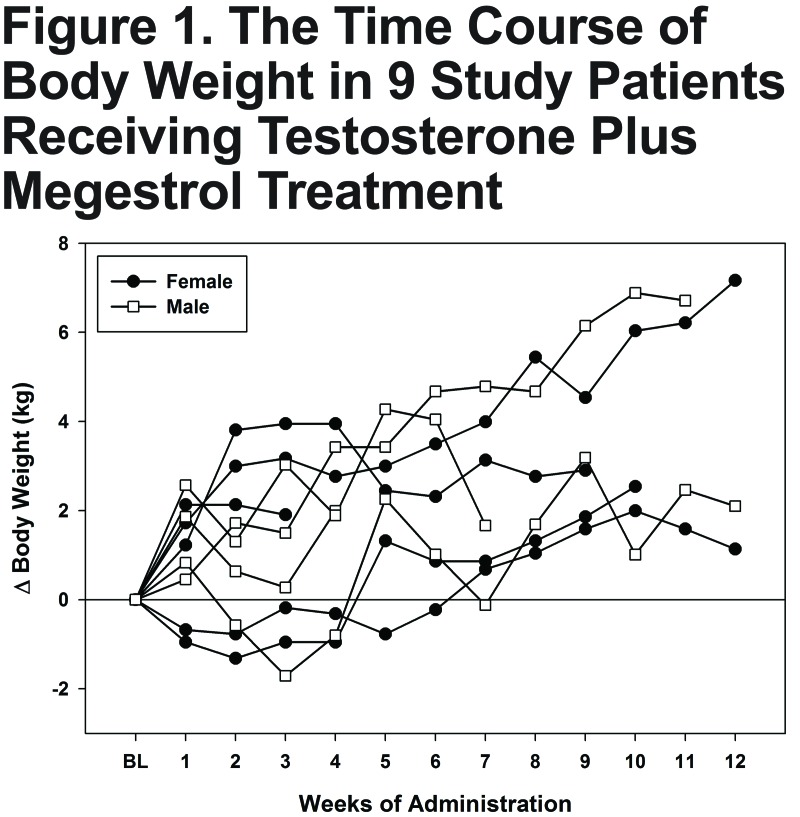
Figure 1 illustrates the individual temporal changes in total body weight in 4 men and 5 women across the 12-week study period. Body weight increased in all participants. By the end of the first week, weight increased 0.5 to 2.5 kg in all but 2 participants (both women). These women manifested weight gain by weeks 5-7.
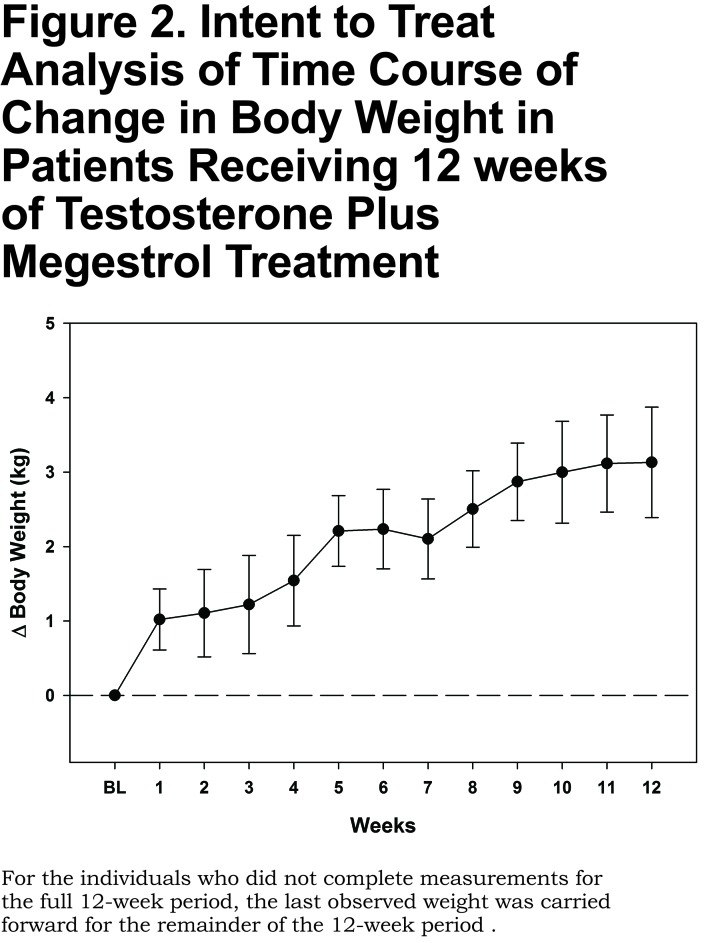
Average end-intervention weight gain (the last observation made in each of the 9 participants) was 3.1±2.2 kg (p<0.005). Figure 2 plots the time course of the intention-to-treat trend in weight change (with the last observation carried forward for those not completing the full 12 weeks); body weight increase averaged about 1 kg at the end of the first week of the intervention; the trend continued upward through the study period.
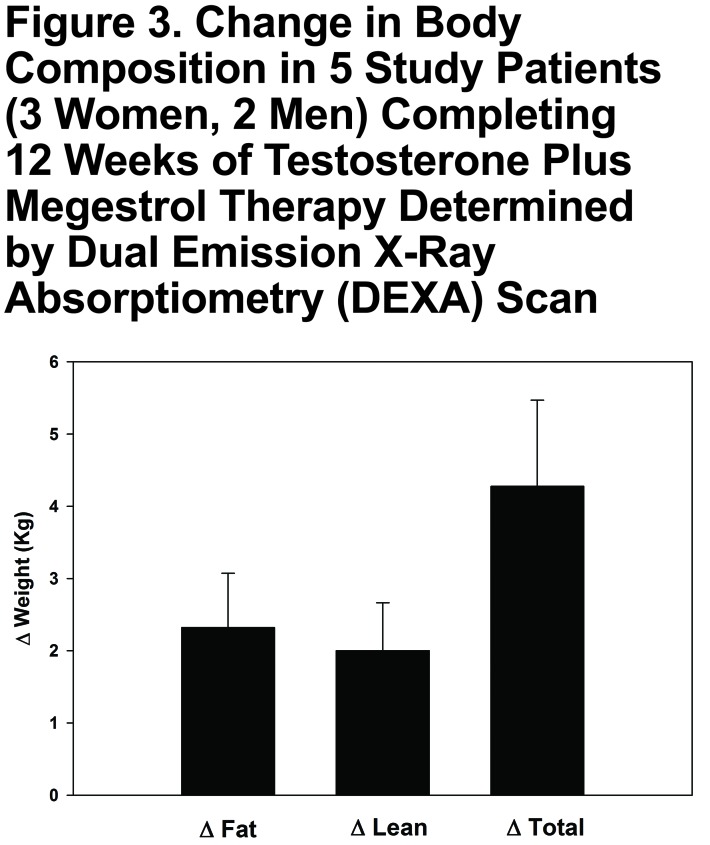
Figure 3 shows the results of DEXA scans performed before and at the end of participation for the 5 individuals who completed 12 weeks of testosterone + megestrol treatment. On average, total body mass increased 4.3±2.7 kg, fat mass increased 2.3±1.7 kg and lean body mass increased 2.0±1.5 kg (each p<0.05).
Safety evaluation: No signs of virilization were detected in women participants; no change in prostate examination was palpated in men. No individual had participation terminated for increase in liver transaminases (AST or ALT >150 units), hematocrit (>18 g/dL), or (in men) PSA (>0.75 μg/L above baseline). Average baseline and on-treatment values for safety assays are presented in Table 2.
Discussion
This is the first clinical study evaluating the combined effects of testosterone enanthate plus megestrol acetate in COPD cachexia. This 12-week pilot study revealed that weekly injection of testosterone enanthate plus daily oral megestrol acetate administration in underweight men and women with involuntary weight loss and severe COPD yielded increased body weight. This combination therapy reversed the trajectory of involuntary weight loss and increased both lean mass and fat mass in these cachectic COPD patients. No apparent adverse effects of therapy were observed though a high dropout rate due to COPD exacerbation was observed.
Cachexia is a constellation of metabolic abnormalities commonly seen in advanced stages of many chronic diseases including heart failure, rheumatoid arthritis, cancer, AIDS, chronic kidney disease, as well as in COPD.32-38 Cachexia is a challenging multifaceted metabolic syndrome whose underlying mechanism is not well delineated; it is associated with reduced physical function, poor quality of life and high mortality.39 Factors that are suggested as contributing to the cachexia syndrome include anorexia, inflammation, insulin resistance, anemia, and hypogonadism.1 Anorexia and consequent decreased food intake yields body fat loss; hypogonadism, inflammation and insulin resistance lead to muscle wasting. Though rational treatment for a syndrome such as cachexia should ideally be based on an understanding of the underlying mechanisms, aiming to address as wide a spectrum of the disease manifestations as possible seems a reasonable approach. To date, however, most clinical trials have investigated only a single therapeutic measure.
Complicating the interpretation of the literature, many previous investigations of COPD cachexia have utilized low BMI or low muscle mass as the sole indicator of cachexia (e.g.,11,40,41. The participant group so recruited may include those whose disease is not severe and whose habitual state may be to have low body weight (or low muscle mass). The prognosis of such individuals is markedly better than underweight individuals with involuntary weight loss and severe disease.42 This recruitment pattern for these previous studies may have stemmed from lack of consensus on the diagnostic criteria for cachexia, 1,43,44 and also that recruiting patients to clinical trials with well documented loss of body weight or (especially) loss of muscle mass is not easily feasible.32 For example, in a pilot study of infliximab in 16 cachectic COPD patients, the selection criterion was low muscle mass, while the average BMI was 23 kg/m2 and no history of weight loss was reported.45 Another study reported salutary effect of ghrelin on reversal of COPD cachexia in 33 COPD men and women with BMI <21 kg/m2.40 In this study too, no data on weight history was presented. Another recent study examining the effects of pulmonary rehabilitation in 10 cachectic patients with COPD defined cachexia as fat-free mass index less than 17 kg/m2(.41 Study participants averaged BMIs of 22 kg/m2 and had pulmonary function tests and exercise tolerance only mildly worse than the non-cachectic group.41 In the current study, we recruited severe COPD patients with BMI <21 kg/m2 (average 18.4±3.4 kg/m2) and with a documented history of at least 10 lb (~4.5 kg) weight loss in the past year. This active weight loss documentation in underweight COPD patients is more consistent with recent definitions of cachexia. We view the high proportion of individuals who experienced an exacerbation during the 12-week study period as evidence of their poor prognosis cachectic condition.
In our study, the combination of testosterone and megestrol acetate increased both fat and lean body mass. This is in marked contrast with studies in which megestrol acetate was administered alone and no lean mass increase was observed. Megestrol acetate, administered alone, was shown to reduce circulating testosterone levels in men with COPD from 403 to 73 ng/dL.12 In our study, concomitant testosterone administration was successful in preventing this fall. The increase in nadir testosterone levels in the male participants, however, did not achieve statistical significance, perhaps because of the competing effects of megestrol. It is true, however, that nadir levels underestimate the average testosterone level during a given dosing interval; male participants likely experienced appreciably increased testosterone levels over the course of the treatment period. On the other hand, testosterone when administered alone has a lipolytic effect, reducing fat mass.46 This was likely abrogated by the concomitant administration of megestrol acetate.
A few clinical trials of combined megestrol and anabolic steroid administration have been reported in other conditions, with mixed results. In older (non-cachectic) men receiving megestrol therapy, addition of testosterone therapy did not alter thigh muscle cross-section or body composition change.47 In HIV-positive men who were underweight or had weight loss, the addition of testosterone to megestrol therapy did not enhance lean body mass accrual.48 In contrast, in HIV-positive men with documented weight loss, nandrolone in combination with megestrol induced weight gain and fat-free mass increase.49
It should be acknowledged that increasing body mass of cachectic patients carries theoretical risks. For example, in a previous study of megestrol administration to underweight COPD patients,12 , the accrual of fat mass was accompanied by a trend for reduction in 6 minute walk distance. Further, testosterone administration has been associated with improvements in muscle strength, but not endurance.26 Therefore, the potential gains of this therapy do not likely extend to common tasks, such as ability to ambulate, but may improve strength-related functionality (e.g., balance, rising from a chair).
Our study should be considered in light of its limitations. Primary among them is the small sample size and lack of a control group. We were unable to perform an a priori sample size estimate; no estimates of the variability of response in the outcomes studied are available for this participant population (it is hoped that the responses observed in this pilot study will help inform sample size estimates of future studies). Lack of a control group is especially of concern because we cannot be sure that the high rate of COPD exacerbations experienced by study participants was not somehow related to the treatment regimen. Further, the length of follow up is not sufficient to ensure that the salutary effects we observed will persist. Importantly, we were unable to evaluate more long-term, patient-centered outcomes, such as quality of life, exacerbation frequency and mortality. Future studies might evaluate the effect of this combined intervention on other biomarkers and clinical outcomes such as inflammatory and metabolic markers, muscle structure and biochemistry, respiratory function, exercise tolerance and muscle strength. Finally, though we did not observe untoward effects of this treatment regimen, long-term safety studies would be required before recommending this strategy as a routine treatment option. In fact, long-term treatment with both testosterone therapy50 and megestrol acetate therapy51 has been reported to be associated with risk of adverse effects.
In summary, COPD cachexia is a poor prognosis condition for which no effective therapy is available. This pilot study demonstrates the feasibility of combination therapy of testosterone and megestrol acetate. Twelve weeks of treatment reversed the trajectory of weight loss and induced significant gains in both lean and fat mass. Although no treatment-related adverse reactions were evident, drop-out rate due to COPD exacerbation was high in this ill patient group. Larger long-term, randomized, placebo-controlled trials with evaluation of functional outcomes and metabolic biomarkers seem warranted.
Abbreviations
chronic obstructive pulmonary disease, COPD; forced expiratory volume in 1 second, FEV1; body mass index, BMI; dual emission x-ray absorptometry, DEXA; prostate specific antigen, PSA; diffusion capacity of the lungs for carbon monoxide, DLCO; American Thoracic Society, ATS; European Respiratory Society, ERS; forced vital capacity, FVC; total lung capacity, TLC; follicle stimulating hormone, FSH; luteinizing hormone, LH; insulin-like growth factor-1, IGF1
Funding Statement
Supported by a grant from the Pulmonary Education and Research Foundation.
References
- 1. Evans WJ,Morley JE,Argiles J,et al. Cachexia: a new definition. Clin Nutr. 2008;27(6):793-799. doi: http://dx.doi.org/10.1016/j.clnu.2008.06.013 [DOI] [PubMed] [Google Scholar]
- 2. Donahoe M. Nutritional support in advanced lung disease. The pulmonary cachexia syndrome. Clin Chest Med. 1997;18(3):547-561. doi: http://dx.doi.org/10.1016/S0272-5231(05)70401-9 [DOI] [PubMed] [Google Scholar]
- 3. Morley JE,Thomas DR,Wilson MM. Cachexia: pathophysiology and clinical relevance. Am J Clin Nutr. 2006;83(4):735-743. [DOI] [PubMed] [Google Scholar]
- 4. Koehler F,Doehner W,Hoernig S,Witt C,Anker SD,John M. Anorexia in chronic obstructive pulmonary disease--association to cachexia and hormonal derangement. Int J Cardiol. 2007;119(1):83-89. doi: http://dx.doi.org/10.1016/j.ijcard.2006.07.088 [DOI] [PubMed] [Google Scholar]
- 5. Schols AM,Soeters PB,Dingemans AM,Mostert R,Frantzen PJ,Wouters EF. Prevalence and characteristics of nutritional depletion in patients with stable COPD eligible for pulmonary rehabilitation. Am Rev Respir Dis. 1993;147(5):1151-1156. doi: http://dx.doi.org/10.1164/ajrccm/147.5.1151 [DOI] [PubMed] [Google Scholar]
- 6. Vermeeren MA,Creutzberg EC,Schols AM,et al. Prevalence of nutritional depletion in a large out-patient population of patients with COPD. Respir Med. 2006;100(8):1349-1355. doi: http://dx.doi.org/10.1016/j.rmed.2005.11.023 [DOI] [PubMed] [Google Scholar]
- 7. von Haehling S,Anker SD. Prevalence, incidence and clinical impact of cachexia: facts and numbers-update 2014. J Cachexia Sarcopenia Muscle. 2014;5(4):261-263. doi: http://dx.doi.org/10.1007/s13539-014-0164-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wilson DO,Rogers RM,Wright EC,Anthonisen NR. Body weight in chronic obstructive pulmonary disease. The National Institutes of Health Intermittent Positive-Pressure Breathing Trial. Am Rev Respir Dis. 1989;139(6):1435-1438. [DOI] [PubMed] [Google Scholar]
- 9. Collins PF,Stratton RJ,Elia M. Nutritional support in chronic obstructive pulmonary disease: a systematic review and meta-analysis. Am J Clin Nutr. 2012;95(6):1385-1395. doi: http://dx.doi.org/10.3945/ajcn.111.023499 [DOI] [PubMed] [Google Scholar]
- 10. Ferreira IM,Brooks D,Lacasse Y,Goldstein RS. Nutritional support for individuals with COPD: a meta-analysis. Chest. 2000;117(3):672-678. doi: http://dx.doi.org/10.1378/chest.117.3.672 [DOI] [PubMed] [Google Scholar]
- 11. Remels AH,Gosker HR,Langen RC,Schols AM. The mechanisms of cachexia underlying muscle dysfunction in COPD. J Appl Physiol. 2013;114(9):1253-1262. doi: http://dx.doi.org/10.1152/japplphysiol.00790.2012 [DOI] [PubMed] [Google Scholar]
- 12. Weisberg J,Wanger J,Olson J,et al. Megestrol acetate stimulates weight gain and ventilation in underweight COPD patients. Chest. 2002;121(4):1070-1078. doi: http://dx.doi.org/10.1378/chest.121.4.1070 [DOI] [PubMed] [Google Scholar]
- 13. Mantovani G,Maccio A,Bianchi A,et al. Megestrol acetate in neoplastic anorexia/cachexia: clinical evaluation and comparison with cytokine levels in patients with head and neck carcinoma treated with neoadjuvant chemotherapy. Int J Clin Lab Res. 1995;25(3):135-141. doi: http://dx.doi.org/10.1007/BF02592554 [DOI] [PubMed] [Google Scholar]
- 14. Oster MH,Enders SR,Samuels SJ,et al. Megestrol acetate in patients with AIDS and cachexia. Ann Intern Med. 1994;121(6):400-408. doi: http://dx.doi.org/10.7326/0003-4819-121-6-199409150-00002 [DOI] [PubMed] [Google Scholar]
- 15. Yeh S,Wu SY,Levine DM,et al. Quality of life and stimulation of weight gain after treatment with megestrol acetate: correlation between cytokine levels and nutritional status, appetite in geriatric patients with wasting syndrome. J Nutr Health Aging. 2000;4(4):246-251. [PubMed] [Google Scholar]
- 16. Aisner J,Parnes H,Tait N,et al. Appetite stimulation and weight gain with megestrol acetate. Semin Oncol. 1990;17(6Suppl9):2-7. [PubMed] [Google Scholar]
- 17. Inui A. Cancer anorexia-cachexia syndrome: current issues in research and management. CA Cancer J Clin. 2002;52(2):72-91. doi: http://dx.doi.org/10.3322/canjclin.52.2.72 [DOI] [PubMed] [Google Scholar]
- 18. Osoba D,Murray N,Gelmon K,et al. Phase II trial of megestrol in the supportive care of patients receiving dose-intensive chemotherapy. Oncology (Williston Park). 1994;8(3):43-49. [PubMed] [Google Scholar]
- 19. Simons JP,Schols AM,Hoefnagels JM,Westerterp KR,ten Velde GP,Wouters EF. Effects of medroxyprogesterone acetate on food intake, body composition, and resting energy expenditure in patients with advanced, nonhormone-sensitive cancer: a randomized, placebo-controlled trial. Cancer. 1998;82(3):553-560. doi: http://dx.doi.org/10.1002/(SICI)1097-0142(19980201)82:3<553::AID-CNCR18>3.0.CO;2-0 [PubMed] [Google Scholar]
- 20. Von Roenn JH. Randomized trials of megestrol acetate for AIDS-associated anorexia and cachexia. Oncology. 1994;51(Suppl1):19-24. doi: http://dx.doi.org/10.1159/000227411 [DOI] [PubMed] [Google Scholar]
- 21. Basaria S,Wahlstrom JT,Dobs AS. Clinical review 138: Anabolic-androgenic steroid therapy in the treatment of chronic diseases. J Clin Endocrinol Metab. 2001;86(11):5108-5117. doi: http://dx.doi.org/10.1210/jcem.86.11.7983 [DOI] [PubMed] [Google Scholar]
- 22. Gullett NP,Hebbar G,Ziegler TR. Update on clinical trials of growth factors and anabolic steroids in cachexia and wasting. Am J Clin Nutr. 2010;91(4):1143S-1147S. doi: http://dx.doi.org/10.3945/ajcn.2010.28608E [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lyden E,Cvetkovska E,Westin T,et al. Effects of nandrolone propionate on experimental tumor growth and cancer cachexia. Metabolism. 1995;44(4):445-451. doi: http://dx.doi.org/10.1016/0026-0495(95)90050-0 [DOI] [PubMed] [Google Scholar]
- 24. Sharma S,Arneja A,McLean L,et al. Anabolic steroids in COPD: a review and preliminary results of a randomized trial. Chron Respir Dis. 2008;5(3):169-176. doi: http://dx.doi.org/10.1177/1479972308092350 [DOI] [PubMed] [Google Scholar]
- 25. Yeh SS,DeGuzman B,Kramer T,Group MS. Reversal of COPD-associated weight loss using the anabolic agent oxandrolone. Chest. 2002;122(2):421-428. doi: http://dx.doi.org/10.1378/chest.122.2.421 [DOI] [PubMed] [Google Scholar]
- 26. Casaburi R,Bhasin S,Cosentino L,et al. Effects of testosterone and resistance training in men with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2004;170(8):870-878. doi: http://dx.doi.org/10.1164/rccm.200305-617OC [DOI] [PubMed] [Google Scholar]
- 27. Hankinson JL,Odencrantz JR,Fedan KB. Spirometric reference values from a sample of the general U.S. Population.. Am J Respir Crit Care Med. 1999;159(1):179-187. doi: http://dx.doi.org/10.1164/ajrccm.159.1.9712108 [DOI] [PubMed] [Google Scholar]
- 28. Casaburi R,Nakata J,Bistrong L,Torres E,Rambod M,Porszasz J. Treatment with megestrol acetate and testosterone increases body weight and muscle mass in COPD cachexia. Eur Respir J. 2011;38(Suppl55). [Google Scholar]
- 29. Miller MR,Hankinson J,Brusasco V,et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319-338. doi: http://dx.doi.org/10.1183/09031936.05.00034805 [DOI] [PubMed] [Google Scholar]
- 30. Macintyre N,Crapo RO,Viegi G,et al. Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur Respir J. 2005;26(4):720-735. doi: http://dx.doi.org/10.1183/09031936.05.00034905 [DOI] [PubMed] [Google Scholar]
- 31. Wanger J,Clausen JL,Coates A,et al. Standardisation of the measurement of lung volumes. Eur Respir J. 2005;26(3):511-522. doi: http://dx.doi.org/10.1183/09031936.05.00035005 [DOI] [PubMed] [Google Scholar]
- 32. Fearon K,Strasser F,Anker SD,et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 2011;12(5):489-495. doi: http://dx.doi.org/10.1016/S1470-2045(10)70218-7 [DOI] [PubMed] [Google Scholar]
- 33. Freeman LM. The pathophysiology of cardiac cachexia. Curr Opin Support Palliat Care. 2009;3(4):276-281. doi: http://dx.doi.org/10.1097/SPC.0b013e32833237f1 [DOI] [PubMed] [Google Scholar]
- 34. Moldawer LL,Sattler FR. Human immunodeficiency virus-associated wasting and mechanisms of cachexia associated with inflammation. Semin Oncol. 1998;25(1Suppl1):73-81. [PubMed] [Google Scholar]
- 35. Summers GD,Metsios GS,Stavropoulos-Kalinoglou A,Kitas GD. Rheumatoid cachexia and cardiovascular disease. Nat Rev Rheumatol. 2010;6(8):445-451. doi: http://dx.doi.org/10.1038/nrrheum.2010.105 [DOI] [PubMed] [Google Scholar]
- 36. Wagner PD. Possible mechanisms underlying the development of cachexia in COPD. Eur Respir J. 2008;31(3):492-501. doi: http://dx.doi.org/10.1183/09031936.00074807 [DOI] [PubMed] [Google Scholar]
- 37. Tisdale MJ. Mechanisms of cancer cachexia. Physiol Rev. 2009;89(2):381-410. doi: http://dx.doi.org/10.1152/physrev.00016.2008 [DOI] [PubMed] [Google Scholar]
- 38. von Haehling S,Lainscak M,Springer J,Anker SD. Cardiac cachexia: a systematic overview. Pharmacol Ther. 2009;121(3):227-252. doi: http://dx.doi.org/10.1016/j.pharmthera.2008.09.009 [DOI] [PubMed] [Google Scholar]
- 39. Schols AM,Broekhuizen R,Weling-Scheepers CA,Wouters EF. Body composition and mortality in chronic obstructive pulmonary disease. Am J Clin Nutr. 2005;82(1):53-569. doi: http://dx.doi.org/10.1016/j.rmedu.2005.09.028 [DOI] [PubMed] [Google Scholar]
- 40. Miki K,Maekura R,Nagaya N,et al. Ghrelin treatment of cachectic patients with chronic obstructive pulmonary disease: a multicenter, randomized, double-blind, placebo-controlled trial. PloS One. 2012;7(5):e35708-. doi: http://dx.doi.org/10.1371/journal.pone.0035708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Vogiatzis I,Simoes DC,Stratakos G,Kourepini E,Terzis G,Manta P,et al. Effect of pulmonary rehabilitation on muscle remodelling in cachectic patients with COPD. Eur Respir J. 2010;36(2):301-310. doi: http://dx.doi.org/10.1183/09031936.00112909 [DOI] [PubMed] [Google Scholar]
- 42. Rutten EP,Calverley PM,Casaburi R,et al. Changes in body composition in patients with chronic obstructive pulmonary disease: do they influence patient-related outcomes? . Ann Nutr Metab. 2013;63(3):239-247. doi: http://dx.doi.org/10.1159/000353211 [DOI] [PubMed] [Google Scholar]
- 43. Muscaritoli M,Anker SD,Argiles J,et al. Consensus definition of sarcopenia, cachexia and pre-cachexia: joint document elaborated by Special Interest Groups (SIG) "cachexia-anorexia in chronic wasting diseases" and "nutrition in geriatrics". Clin Nutr. 2010;29(2):154-159. doi: http://dx.doi.org/10.1016/j.clnu.2009.12.004 [DOI] [PubMed] [Google Scholar]
- 44. Rolland Y,Abellan van Kan G,Gillette-Guyonnet S,Vellas B. Cachexia versus sarcopenia. Curr Opin Clin Nutr Metab Care. 2011;14(1):15-21. doi: http://dx.doi.org/10.1097/MCO.0b013e328340c2c2 [DOI] [PubMed] [Google Scholar]
- 45. Dentener MA,Creutzberg EC,Pennings HJ,Rijkers GT,Mercken E,Wouters EF. Effect of infliximab on local and systemic inflammation in chronic obstructive pulmonary disease: a pilot study. Respiration. 2008;76(3):275-282. doi: http://dx.doi.org/10.1159/000117386 [DOI] [PubMed] [Google Scholar]
- 46. Bhasin S,Woodhouse L,Casaburi R,et al. Older men are as responsive as young men to the anabolic effects of graded doses of testosterone on the skeletal muscle. J Clin Endocrinol Metab. 2005;90(2):678-688. doi: http://dx.doi.org/10.1210/jc.2004-1184 [DOI] [PubMed] [Google Scholar]
- 47. Lambert CP,Sullivan DH,Freeling SA,Lindquist DM,Evans WJ. Effects of testosterone replacement and/or resistance exercise on the composition of megestrol acetate stimulated weight gain in elderly men: a randomized controlled trial. J Clin Endocrinol Metab. 2002;87(5):2100-2106. doi: http://dx.doi.org/10.1210/jcem.87.5.8505 [DOI] [PubMed] [Google Scholar]
- 48. Mulligan K,Zackin R,Von Roenn JH,et al. Testosterone supplementation of megestrol therapy does not enhance lean tissue accrual in men with human immunodeficiency virus-associated weight loss: a randomized, double-blind, placebo-controlled, multicenter trial. J Clin Endocrinol Metab. 2007;92(2):563-570. doi: http://dx.doi.org/10.1210/jc.2006-0954 [DOI] [PubMed] [Google Scholar]
- 49. Cuerda C,Zugasti A,Breton I,Camblor M,Miralles P,Garcia P. Treatment with nandrolone decanoate and megestrol acetate in HIV-infected men. Nutr Clin Pract. 2005;20(1):93-97. doi: http://dx.doi.org/10.1177/011542650502000193 [DOI] [PubMed] [Google Scholar]
- 50. Basaria S,Coviello AD,Travison TG,et al. Adverse events associated with testosterone administration. N Engl J Med. 2010;363(2):109-122. doi: http://dx.doi.org/10.1056/NEJMoa1000485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Bolen JC,Andersen RE,Bennett RG. Deep vein thrombosis as a complication of megestrol acetate therapy among nursing home residents. J Am Med Dir Assoc. 2000;1(6):248-252. [PubMed] [Google Scholar]
- 52. Goldman HI,Becklake MR. Respiratory function tests; normal values at median altitudes and the prediction of normal results. Am Rev Tuberc. 1959;79(4):457-467. [DOI] [PubMed] [Google Scholar]
- 53. Crapo RO,Morris AH. Standardized single breath normal values for carbon monoxide diffusing capacity. Am Rev Respir Dis. 1981;123(2):185-189. [DOI] [PubMed] [Google Scholar]