Abstract
This article serves as a CME- available, enduring material summary of the following COPD9USA presentations:
- “Lessons Learned from Pulmonary Education Program and On Track with COPD Ongoing Health Management.” Presenter: Scott Cerreta, BS, RRT
- “Cultivating Memorial Funds for Pulmonary Rehabilitation” Presenter: Valerie McLeod, RRT
- “Strategies for Success: Maintenance Program Best Practices” Presenter: David Vines, MHS, RRT
- “Strategies for Success-Maximizing Participation and Completion Rates,” Presenter: Trina M. Limberg, BS, RRT
Keywords: pulmonary rehabilitation, COPD education
Introduction
This material identifies strategies for success in organizing pulmonary rehabilitation programs and discusses limitations to access to and participation in pulmonary rehabilitation. The presentations center around the Pulmonary Education Program (PEP), avenues to establish and promote memorial finds for pulmonary rehabilitation programs, establishing effective maintenance programs, using the Chronic Care Model, and individualizing the intervention.
Lessons Learned from Pulmonary Education Program and On Track with COPD Ongoing Health Management
The goal of the COPD Foundation’s (PEP) is to offer an exceptional experience to pulmonary rehabilitation (PR) patients with COPD by providing disease-specific educational materials, improved quality of life, and lifelong engagement in the COPD Community through the PEP On Track with COPD ongoing health management program.
The PEP was launched by the COPD Foundation at the end of 2012 and has been very successful. It is a service provided after an individual graduates from a PR program. The PEP program is currently in 262 PR centers (232 active) in 44 states with more than 5000 individuals enrolled in the program in 2015.
Pulmonary rehabilitation is built around a relationship of education, exercise, coping skills, and social bonding. A patient will typically have 12-21 sessions. After graduation, they receive a graduation kit and continue to receive long term benefits. Many patients report less dyspnea, better adherence, better self-care, and better quality of life. However, at the end of the program there can also be a decrease in exercise, increased isolation, and slow loss of benefits gained. This is where the On Track Program-a part of PEP- intervenes to fill the gap.
The PEP “On Track with COPD Ongoing Support Program” makes use of a peer-to-peer coaching curriculum conducted via the COPD Info-line. Reaching out to patients through 24 monthly phone calls allows for assessment of the patient’s progress and encouragement without the need for in-person visits. These calls can help encourage exercise, reduce the feeling of patient isolation, and maintain the bond that was formed between patients and the program before graduation. Through these monthly coaching calls to patients, goals of improved quality of life and ongoing health management can be better obtained. In addition, patients are encouraged to become engaged with the COPD Foundation through the COPD360social, an interactive, collaborative community where one can join the COPD Foundation, learn about events in one’s area, participate in research, and chat with other COPD individuals and Foundation staff.1
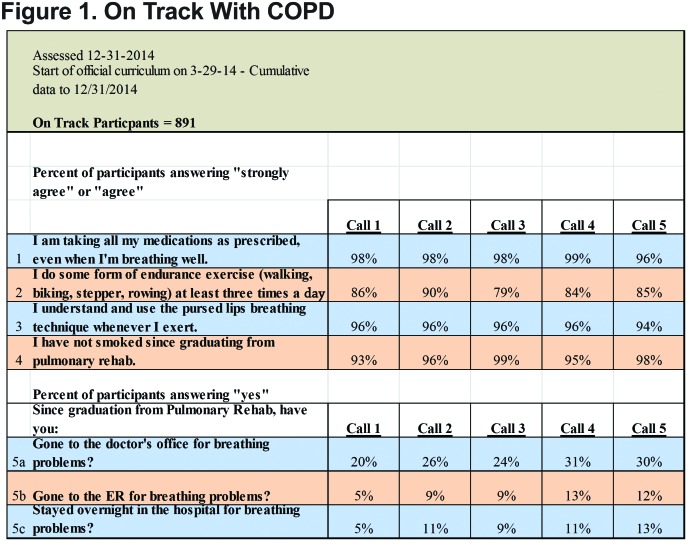
As part of the On Track coaching calls, 5 core questions are asked. See Figure 1. The aim of the calls and questions is to provide ongoing intervention and the opportunity to discuss topics to help prevent a drop in adherence to PR program life-style goals.
In the future, more PR centers will be needed along with more trained associates, improved On Track enrollment, collection of better outcomes, and increased funding.
The COPD Foundation’s cost is about $440,000/year with the 2 biggest expense components being cost of the educational materials and the cost of the Information Line. Improvements to the program are continually made to ensure long term success. The better educated patients are, the better they can manage their disease, which improves outcomes.
Cultivating Memorial Funds for Pulmonary Rehabilitation
Celebrating patients and their accomplishments, big or small, can help to build a strong personal bond which can be the first step toward establishing a successful donor/memorial fund for any PR program.
Even modest PR programs can inspire patients to attend regularly by helping the patients understand the program is genuinely interested in their success and helping them learn skills that will help them lessen the burden of their disease and adopt a lifestyle of “sit less, move more.” Hiring the right staff is crucial to PR success because as staff encourage patients to learn new skills, patients realize they can depend on the staff for support and reassurance. An important bond is formed.
This bond can be reinforced by long-term participation in maintenance exercise programs and making an effort to stay in contact with patients who require a break from PR due to extenuating life circumstances or hospital stays. There should be an emphasis on long-term relationships and forming an “extended family.” The patient-staff relationship is generally what motivates patients to recognize a program via donations.
In addition, other important steps to establishing a donor program include:
Involving the organization’s marketing department; it is important to keep the program in the forefront and visible.
Networking with the PR organization’s foundation or development department to become aware of any minimum requirements that may exist for establishing a designated fund. (Without this understanding, memorial gifts will most likely be deposited into a General Fund and may not be available for specific purchases for the PR program.)
Honoring donations with a personal handwritten thank you letter to the patient or their family.
Empowering the family or individual to provide input about how the money will be used. Patients often communicate their wishes to family members about how to best honor their memory and it is important to listen to these wishes.
Gifts for the purchase of new equipment can be given recognition via a small plaque on the machine itself, serving to not only honor the donation, but also to spark conversation among patients about memorial contributions.
Sometimes families like to make smaller donations and/or do not have specific designations in mind for their gift. In these cases, establish a plaque with name plates in a prominent place in the gym or provide a variety of inspirational plaques placed throughout the gym to motivate others while honoring contributions to the program. This can spark conversations about the program and future contributions.
Memorial gifts, big or small, are an honor to receive and can have a significant impact on a PR program. When a supportive environment is provided for patients and their families, given the opportunity, they will, in return, support the PR program.
Key components for creating a successful PR environment include:
Recruiting a staff with a passion for the work;
Having medical director and administration support;
Having adequate space and staffing;
Providing value added services (pulmonary function testing, smoking cessation, and community lung screenings)
Having patient ambassadors
Providing a year-end newsletter
Having a well-organized system in place can lead to success both for the PR program and its donor/memorial fund program.
Strategies for Success: Maintenance Program Best Practices
Finding adequate PR in rural areas is a challenge. Even when the program is complete, finding maintenance, motivation, and continued support can be an issue for many individuals.
A prospective cohort study suggested that physical activity is the strongest predictor of all-cause mortality in patients with COPD.2 The study showed that active participants have a higher probability of survival in comparison to those who are sedentary or very inactive.2 Most patients are not aware that exercise is a strong predictor of mortality. Patients need to understand the impact that their exercise can have on their survival.
One study showed that at 6 months there is a benefit in maintenance programs.3 However, systematic review of supervised exercise programs after pulmonary rehabilitation in individuals with COPD showed thatbenefits seem to be lost after 12 months.3 Health-related quality of life gains do not persist at 6 months or 12 months post rehabilitation. There are limitations to these studies including variability between programs and a high drop-out rate.
A community-based post-rehabilitation maintenance program in COPD was achieved through a partnership with the City of Toronto, Parks, Forestry and Recreation Division.4 Trained fitness instructors supervised COPD patients who attended twice a week. Case managers attended the first exercise session to supervise and assist with a modified plan if the participant was absent for 2 weeks. This led to reported improvements in exercise capacity and Chronic Respiratory Questionnaire scores at 6 months and at 1 year. Trust was built between the patients and the program. Many patients would even contact the program as a first option with health-related concerns.
Barriers to success in exercise programs for COPD patients include:
Changing health status, personal issues, lack of support, external factors, ongoing smoking, barriers to sustained physical activities5
Exacerbations, fatigue, transportation, weather6
Lower forced expiratory volume in 1 second scores, signs of depression, and shorter initial PR7
In contrast, enablers of exercise program success include:
Social support, professional support, personal benefit, control of condition, specific goals5
Improved function, and quality of life6
The Chronic Care Model (CCM)8 reminds us “we are not in this alone.” Sometimes PR is separate from primary care; these need to be integrated. Immunization status, emergency department visits, and rehab progress need to be communicated to and from the primary care team. Collaboration from the community and the health system lead to improved outcomes through productive interactions. A good maintenance program includes self-management support, delivery system design, decision support, and a clinical information system. These factors coming together lead to an informed and activated patient with a proactive practice team.
In a systematic review of the CCM in COPD prevention and management,pooled data demonstrated that patients with COPD who received interventions with 2 or more CCM components had lower rates of hospitalizations and emergency department/unscheduled visits and a shorter length of stay compared with control groups.8
Components of the CCM can be categorized into either self-management or a delivery system. Self-management includes education, behavioral support, and motivation. A delivery system is designed to provide advanced access to medical care (24 h/d, 7 d/wk) and teams to coordinate preventative measures for chronic care.8
Decision support can be provided through use of evidence-based guidelines, integrated specialty expertise, identifying barriers to care, and performance reviews. Clinical information systems can be used to facilitate clinical registries (population information databases), clinical reminders, and provider feedback.8
Telemedicine has made strides in many facets of medicine. There have been some positive results using telehealth to deliver PR to patients with COPD compared to standard PR. In addition, telehealth may play a key role in maintenance programs.
Sustained results have been difficult to maintain in maintenance programs. Barriers need to be identified and enablers should be encouraged. Best practices should include the integration of self-management, health care teams, decision support, and clinical information systems. Telemedicine may play a key role in maintenance programs.
Strategies for Success-Maximizing Participation and Completion Rates
PR has long been established as a standard of care improving dyspnea, exercise tolerance and quality of life in patients with COPD.9-11 Starting and attending frequent and lengthy therapy sessions may be more challenging for some patients. A brief review of the literature is useful in understanding why some patients may decline services or why some fail to complete the prescribed treatment. Anecdotally, having PR clinicians to conduct initial calls to referred patients may help to improve understanding of perceived benefits. Offering flexible scheduling (when possible) and promoting group interaction may help patients to engage and feel supported. Clinicians can expect to use the information to assess factors that may hamper participation in PR.
Several causes have been reported for PR dropout, some of which are beyond the patient’s control, such as acute exacerbations or hospitalizations.12 The impact of out of pocket expenses with applied co-pays remains relatively unknown in the United States. Several large-scale studies have been done in Canada with its different payor system. Selzer et al found that 3 factors played a major role in PR drop out: younger patients (average age 63), current smokers, and patients with a lower health status were at risk for dropping out.13 They also found that pulmonary function data did not predict drop outs. Perceived impairment was a stronger indicator for predicting drop outs.13
In another study looking at dropouts and attendance,14 20% of patients missed appointments due to factors beyond their control (exacerbations/hospitalizations). Still smoking, living alone, and social factors played a role. Lower fat free mass index was very predominant, as was lower confidence in the treatment. The focus of the study was that the emphasis should be placed on nutritional status and on creating a positive expectation of treatment from the very beginning.
Keating et al conducted structured interviews of patients who declined or withdrew from PR and found that a poor perception of benefit and transportation barriers were significant.15 A total of 30% of patients declined to attend even the first visit. Half of the patients reported not receiving PR information at the time of referral. In a systematic review also done by Keating et al, several major areas were identified with regards to starting PR: disruption of routine, transport/travel, influence of physician, lack of perceived benefit and inconvenient timing. Illness, comorbidities, and depression were major barriers to completing PR.16 This suggests that the area of focus should be on building confidence, improving immediate perceived benefit, and assessing readiness and access to PR.
Living alone and a lack of social support have been cited as significantly impacting the ability to attend and participate in pulmonary rehabilitation.17 Although clinical data cannot, with certainty, predict which patients are likely to decline or drop from treatment, it can aid clinicians in improving participation and completion.
Making a “caring connection” can make a difference. This can be achieved through an emphasis on improving the patient’s knowledge, skills and abilities to live well with COPD, actively listening and providing an opportunity for questions. The initial contact needs to be meaningful and may need to be a call from the ordering physician. The first face-to-face contact needs to convey compassion, caring, and that the provider possesses the competencies that can help improve the patient’s breathing and movement.
Once rehabilitation begins, tips for success include:
Offer group peer-to-peer contact. Involve family and friends; they need to feel comfortable too.
Be aware of the environment of the program. Set attainable goals at each session.
Recognize and offer encouragement when goals are achieved. Be responsive.
Individualize the program to engage the patient at the level that they need. It is important to get it right for the individual patient.
Remember that rehab should be fun! This should be an experience that patients don’t want to miss and if they do miss they want to find a way to make up the session.
Insurance/Medicare coverage for PR can play an important role in treatment and out-of-pocket costs can often serve as an inhibitor to participation. Medicare C can have high co-pays of $40-60 (more than what PR programs get paid from Medicare). Other inhibitors include the limited ability to attend sessions, work schedules (limited availability), transportation issues, poor health literacy, and the inherent barriers of sicker/older populations.
Perceived benefits are important, help patients to see the value. A positive referring physician is influential. Reach out to referrals and communicate with them. Flexibility for younger patients and the working population is important, as they may have time constraints. Provide help for current smokers who desire to quit. Good care and relationships with providers improves the experience.
Abbreviations
pulmonary education program, PEP; pulmonary rehabilitation, PR; chronic obstructive pulmonary disease, COPD;Chronic Care Model, CCM
References
- 1.COPD Foundation website/. COPD Foundation. ; [Published 2014. ]. [Accessed December 2015. ]. COPD 360 Social: It's Our Community Online. [Google Scholar]
- 2. Waschki B,Kirsten A,Holz O,et al. Physical activity is the strongest predictor of all-cause mortality in patients with COPD. Chest. 2011;140(2):331-342. doi: http://dx.doi.org/10.1378/chest.10-2521 [DOI] [PubMed] [Google Scholar]
- 3. Beauchamp MK,Evans R,Janudis-Ferreira T,Goldstein RS,Brooks D Systematic review of supervised exercise programs after pulmonary rehabilitation in individuals with COPD. Chest2013;144(4):1124-1133. doi: http://dx.doi.org/10.1378/chest.12-2421 [DOI] [PubMed] [Google Scholar]
- 4. Beauchamp MK,Francella S,Romano JM,Goldstein RS,Brooks D A novel approach to long-term respiratory care: Results of a community-based post-rehabilitation maintenance program in COPD. Respir Med. 2013;107(8):1210-1216. doi: http://dx.doi.org/10.1016/j.rmed.2013.04.014 [DOI] [PubMed] [Google Scholar]
- 5. Thorpe O,Johnston K,Kemar S Barriers and enablers to physical activity participation in patients with COPD. J Cardiopulm Rehabil Prev. 2012;32(6):359-369. doi: http://dx.doi.org/10.1097/HCR.0b013e318262d7df [DOI] [PubMed] [Google Scholar]
- 6. Desveaux L,Beauchamp M,Rolfe D,Goldstein R,Brooks D Participant experiences of a community-based maintenance program post-pulmonary rehabilitation. Chron Respir Dis. 2014;(1):23-30. doi: http://dx.doi.org/10.1177/1479972313516880 [DOI] [PubMed] [Google Scholar]
- 7. Heerema-Poelman A,Stuive I,Wempe JB Adherence to a maintenance exercise program 1 year after pulmonary rehabilitation: What are the predictors of dropout? . Cardiopulm Rehabil Prev. 2013;33(6):419-426. doi: http://dx.doi.org/10.1097/HCR.0b013e3182a5274a [DOI] [PubMed] [Google Scholar]
- 8. Adams SG,Smith PK,Allan PF,Anzueto A,Pugh JACornellJE Systematic review of the chronic care model in chronic obstructive pulmonary disease prevention and management. Arch Intern Med. 2007;167(6):551-561. doi: http://dx.doi.org/10.1001/archinte.167.6.551 [DOI] [PubMed] [Google Scholar]
- 9. Ries A,Bauldoff GS,Carlin BW,et al. Pulmonary rehabilitation: Joint ACCP/AACVPR evidenced- based clinical practice guidelines. Chest. 2007;131(5 Suppl):4S-42S. doi: http://dx.doi.org/10.1378/chest.06-2418 [DOI] [PubMed] [Google Scholar]
- 10. Nicci L,Donner C,Wouters E,et al. American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. Am J Resp Crit Care Med. 2006;173(12): 1390-1413. doi: http://dx.doi.org/10.1164/rccm.200508-1211ST [DOI] [PubMed] [Google Scholar]
- 11. Spruit MA,Singh SJ,Garvey C,et al. An official America Thoracic Society/European Respiratory Society statement: Key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8): e13-64. doi: http://dx.doi.org/10.1164/rccm.201309-1634ST [DOI] [PubMed] [Google Scholar]
- 12. Fischer M,Scharloo M,Abbink J,et al. Drop-out and attendance in pulmonary rehabilitation: The role of clinical and psychosocial variables. Respir Med. 2009;103(10):1564-1571. doi: http://dx.doi.org/10.1016/j.rmed.2008.11.020 [DOI] [PubMed] [Google Scholar]
- 13. Selzer AM,Simmonds L,Rodgers W,Wong E,Strickland K Pulmonary rehabilitation in chronic obstructive pulmonary disease: Predictors of program completion and success. COPD. 2012;9:538-545. doi: http://dx.doi.org/10.3109/15412555.2012.705365 [DOI] [PubMed] [Google Scholar]
- 14. Fischer MJ,Scharloo M,Abbink JJ,et al. Drop-out and attendance in pulmonary rehabilitation: The role of clinical and psychosocial variables. Respir Med. 2009;103(10):1564-1571. doi: http://dx.doi.org/10.1016/j.rmed.2008.11.020 [DOI] [PubMed] [Google Scholar]
- 15. Keating A,Lee AL,Holland AE Lack of perceived benefit and inadequate transport influence uptake and completion of pulmonary rehabilitation in people with chronic obstructive pulmonary disease: a qualitative study. J Physiother. 2011;57(3):183-190. doi: http://dx.doi.org/10.1016/S1836-9553(11)70040-6 [DOI] [PubMed] [Google Scholar]
- 16. Keating A,Lee AL,Holland AE What prevents people with chronic obstructive disease from attending pulmonary rehabilitation? A systemic review. Chron Respir Dis. 2011;8(2):89-99. [DOI] [PubMed] [Google Scholar]
- 17. Guo S-E,Bruce A Improving understanding of and adherence to pulmonary rehabilitation in patients with COPD: A qualitative inquiry of patient and health professional perspectives. PLoS One. 2014;9(10):e110835-e110835. doi: http://dx.doi.org/10.1371/journal.pone.0110835 [DOI] [PMC free article] [PubMed] [Google Scholar]