Abstract
This article serves as a CME available, enduring material summary of the following COPD9USA presentations:
“Computed Tomography and COPD” Presenter: George R. Washko, MD
“CT Imaging in Routine Clinical Practice: Are We Ready for Prime Time?” Presenter: Meilan K. Han, MD
“Beyond CT: What MRI can Tell Us about COPD” Presenter: R. Graham Barr, MD
Keywords: copd, computed tomography, chronic obstructive pulmonary disease, CT, MRI, magnetic resonance imaging
Introduction
Chronic obstructive pulmonary disease (COPD) is defined by airflow obstruction on spirometry and includes emphysema and chronic bronchitis.1 COPD phenotyping has been heavily influenced by the advent of advanced imaging techniques.2 While computed tomography (CT) has been used for decades to visualize lung fields, recent advances in quantitative CT imaging have made automated quantitation of emphysema, gas trapping and large airway wall thickness possible.3 Although the use of magnetic resonance imaging (MRI) for imaging the lung is technically challenging, use of hyperpolarized gases has improved our ability to obtain meaningful information from pulmonary MRI with the added advantage of functional and structural imaging of the heart which may also be affected in COPD.4 These imaging measures can serve as biomarkers for disease in COPD, and in the future can potentially be used as end points in clinical trials.5 This is a review of these imaging biomarkers.
Computed Tomography and COPD
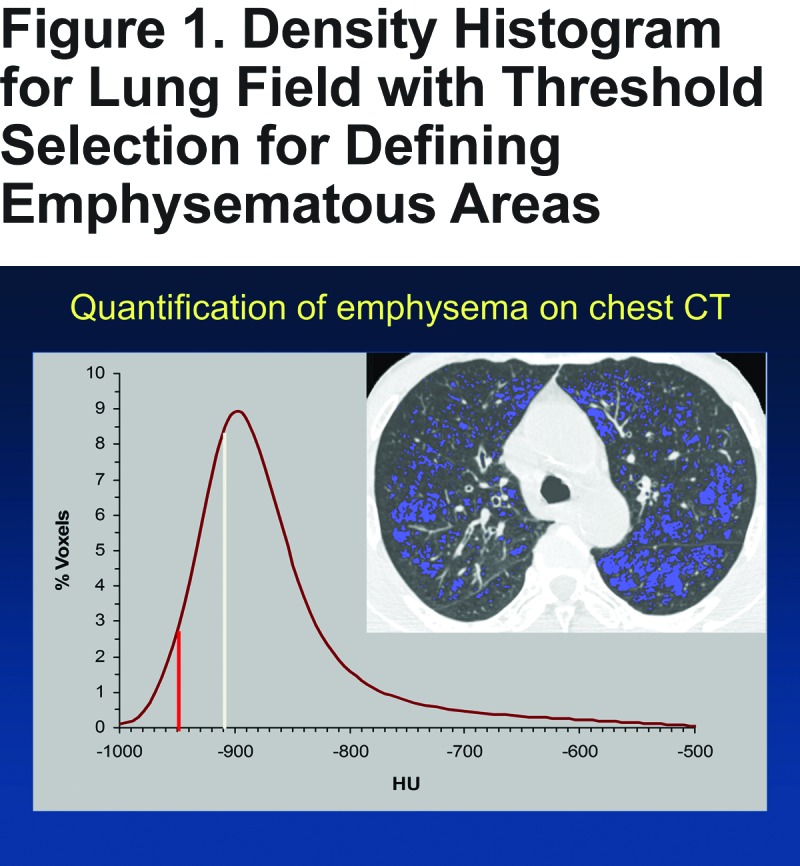
CT is increasingly utilized in the diagnosis and characterization of lung disease in COPD.5 CT has been used for the past 30 years to quantify emphysema.5 This is done using density mask analyses whereby extrapulmonary tissues are subtracted from the CT images, and all voxels within the lung are assigned a Hounsfield unit (HU) based on their density, and all voxels below a certain threshold are designated emphysematous (Figure 1).6 This threshold (Eg; -950HU) can then dichotomize the lung into emphysematous and non-emphysematous areas and provide a quantitation of percentage of lung affected. Observational studies have shown correlations between quantitative CT measurements of emphysema and airflow obstruction on spirometry, dyspnea measurements, functional capacity and exacerbations.7-9
There is an ongoing effort to use CT to phenotype COPD subtypes and also to assess whether we can use CT measurements as intermediate endpoints for clinical studies.5 For example, Stockley et al showed in an aggregate study of patients with alpha-1 antitrypsin deficiency that using CT can demonstrate differences in loss of lung tissue between patients receiving alpha-1 antitrypsin augmentation therapy and those receiving placebo (annual decline -1.73 g/L/yr versus -2.74 g/L/yr over 2.5 years of follow-up).10 CT phenotyping can inform prognosis. Using data from the London COPD cohort, Patel et al showed that COPD patients with bronchiectasis on CT tended to have greater baseline pulmonary inflammation and a prolonged time to recovery from exacerbations.11 A more recent study showed presence of bronchiectasis on CT is associated with greater risk of death at a median of 4 years (hazard ratio [HR] 2.54; 95% confidence interval [CI] 1.16-5.56; p=0.02).12 CT can also be used to assess pulmonary vascular disease in COPD. Using CT scans to measure the ratio of the diameter of the pulmonary artery (PA) to the aorta (A), Wells et al found that this ratio (PA/A) independently predicts future exacerbations .13 The pulmonary vasculature can be visualized on CT and demonstrates distal pruning in COPD, and this correlates with disease severity and a number of measures of respiratory morbidity.14
CT can also be used for assessment of extrapulmonary manifestations of COPD. It has long been recognized that spirometry alone does not adequately capture disease severity and manifestations. The Body mass index (BMI)- airflow Obstruction- Dyspnea and Exercise capacity (BODE) index was developed as a composite measure of disease severity, and has been shown to predict mortality.15 Body tissue composition is perhaps more reflective of disease than BMI. Marquis et al showed that quadriceps cross sectional area measured using CT predicted mortality better than BMI, especially in those with severe COPD.16
In summary, CT scans can provide information beyond spirometric assessment alone. It is anticipated that CT scans may be able to serve as intermediate end points in clinical trials by providing assessments of structural lung disease as well as extrapulmonary manifestations which are likely equally important in this complex multisystem disease.
CT Imaging in Routine Clinical Practice: Are We Ready for Prime Time?
Assessment of emphysema on CT images is currently being used for patient selection for lung volume reduction procedures for severe COPD.17 In this instance, CT emphysema distribution provides information on patient selection that cannot be obtained from spirometric measures of airflow obstruction alone.18 Some of the newer guidelines, such as from the COPD Foundation, have now incorporated CT emphysema as a disease domain.19 Other ways that CT may be clinically useful, particularly in early disease is a subject of ongoing investigation.
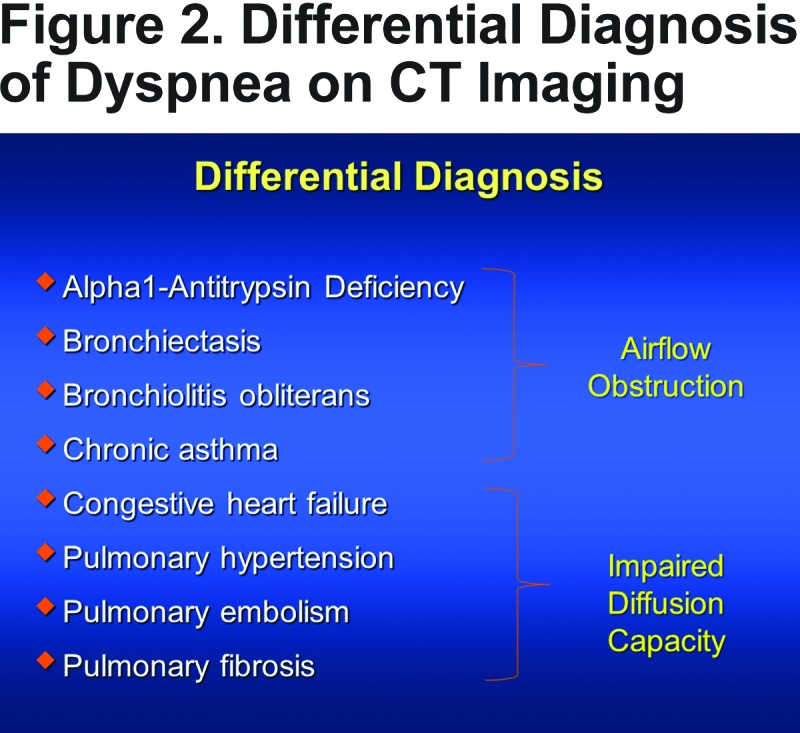
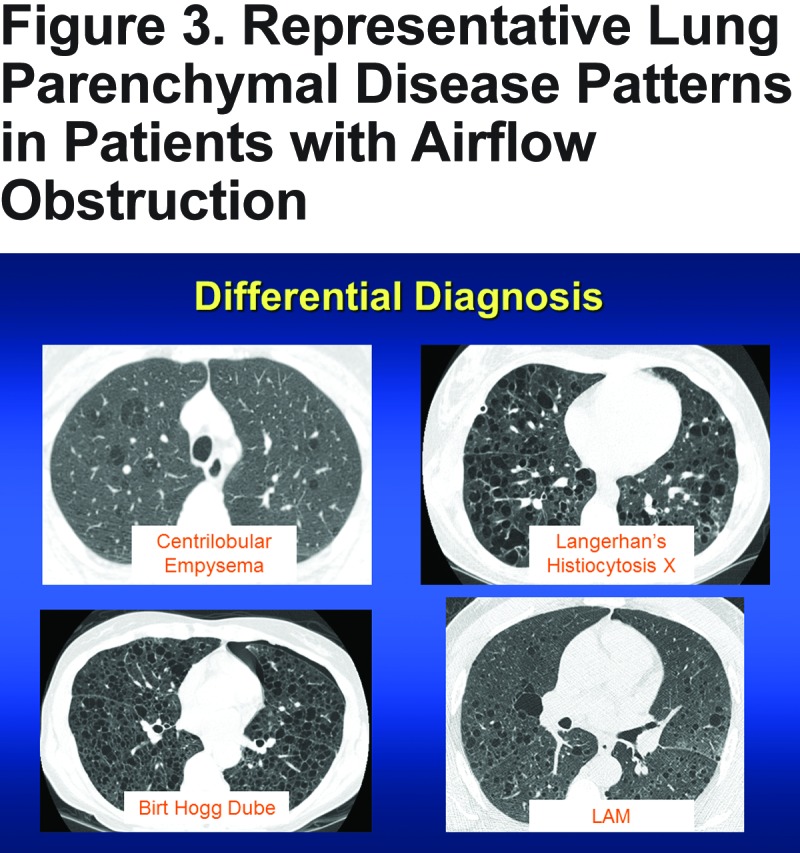
There is certainly a role for CT imaging in clinical practice, especially for differential diagnosis, prognostication and for treatment planning. The differential diagnosis of dyspnea in a smoker is broad (Figure 2). In some patients, the level of airflow obstruction may be disproportionate to smoking history or may not fit with the clinical profile, in which case CT imaging can provide more information about structural lung disease. Figure 3 illustrates examples of patients presenting with airflow obstruction, but with entirely different structural lung diseases, with different prognosis and treatment implications.
While CT is not recommended currently for routine clinical use in all COPD patients, more and more patients will be getting CT scans of the lungs for other reasons. Based on the results from the National Lung Screening Trial (NLST) demonstrating a 20% relative risk reduction in mortality from lung cancer with low dose CT screening, the Centers for Medicare & Medicaid Services (CMS) recently approved CT screening for lung cancer in individuals with at least a 30 pack year smoking history and between the ages of 55 and 77 years and hence at high risk for lung cancer.20 A significant number of individuals with COPD remain undiagnosed, and it is likely that a substantial number of patients undergoing screening CT scans will show evidence of emphysema and gas trapping.21 This has important implications for diagnosis and possible interventions such as quitting smoking.
CT can also be used to phenotype COPD beyond the global metric of airflow obstruction, and help predict important outcomes such as exacerbations and mortality.2 Imaging can help identify pulmonary vascular disease in these patients and this has significant prognostic implications in predicting future exacerbations.13 The PA/A ratio has been shown to correlate with pulmonary arterial pressures.22 In some centers, reporting PA/A ratio has become routine in clinical practice. CT imaging is already established for patient selection for lung volume reduction procedures.17 The National Emphysema Treatment Trial showed that patients with predominant upper lobe disease with low exercise capacity benefit the most from lung volume reduction with both improvements in quality of life as well as mortality.23 Commercially available software can now provide estimates of emphysema and gas trapping in the clinical setting which will open the doors for clinicians to be able to use quantitative CT imaging data currently being used largely by researchers.
Beyond CT: What MRI Can Tell Us About COPD
While CT imaging is being increasingly used clinically, MRI imaging of the lung is currently used for research and is at a preclinical stage.4 Compared to CT, the resolution of plain MRI for visualizing lung structure is poor as air is associated with very little signal on MR imaging. Although newer technology has resulted in improvements in image quality, CT is currently better for imaging lung structure.
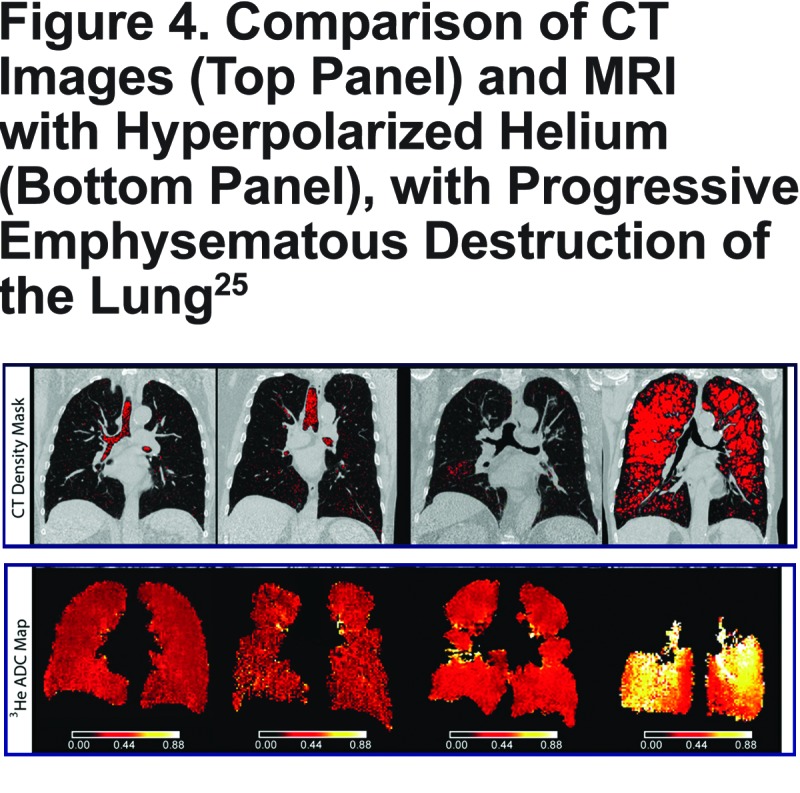
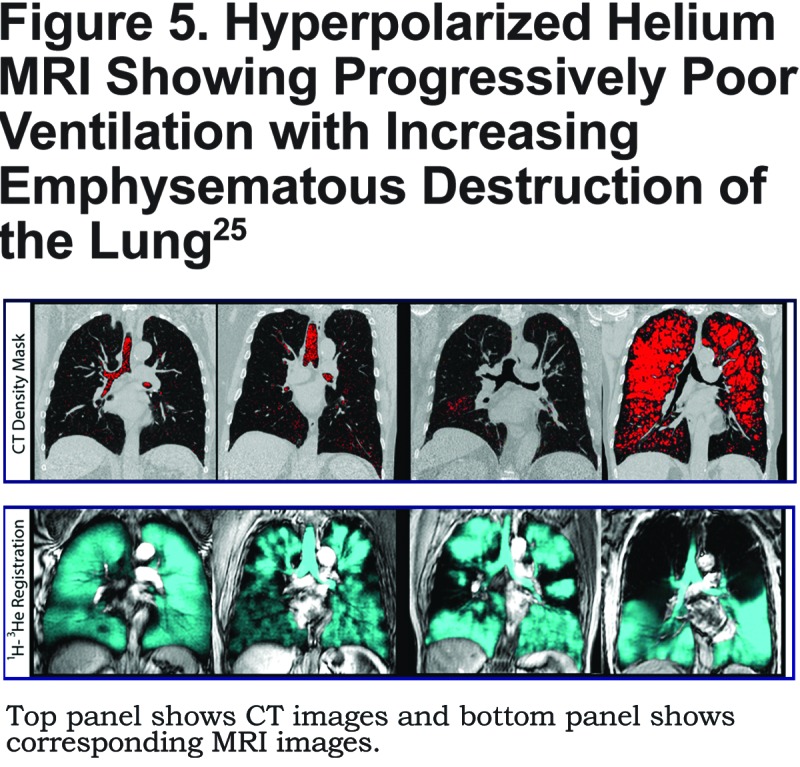
Alveolar size can be estimated using hyperpolarized gases like Helium-3.24 These gases display Brownian motion within the alveolar sacs, and this motion can be measured with MRI. With increasing alveolar distension, these metrics can reflect alveolar size and emphysema.24As seen in Figure 4, use of hyperpolarized gases can provide quantitation of emphysema.25 Early change and increased alveolar size related to passive smoke exposure have been documented with MR studies in children as young as 5 years old. The resolution permits its use in mouse models as well. Figure 5 demonstrates that with increasing emphysema severity, there are progressively lesser areas of the lung that participate in ventilation, thus providing functional assessments of lung involvement in emphysema.25 These ventilation defects can also reflect small airways disease. These changes have been shown in asthma patients to be responsive to therapy with bronchial thermoplasty,26 and since MRI is not associated with radiation risk, MR sequences can be quickly repeated following interventions.
An additional advantage of MRI is that it can provide accurate measures of cardiac structure and function in real time, allowing for assessments of cardiopulmonary interactions, overcoming some of the limitations of echocardiography such as poor windows.27 For example, multiple studies have shown a relationship between emphysema, lung hyperinflation and decreases in cardiac filling and output.28-30 Cardiac size and output are affected by lung hyperinflation and this is potentially reversible. At the American Thoracic Society meeting in May 2015, Stone et al showed that using inhaled corticosteroids/long-acting beta agonists decreased air trapping and subsequently improved right and left ventricular filling and cardiac output.31 This could be an additional mechanism by which these drugs improve symptoms, and this needs further exploration. In addition, the pulmonary microvasculature can be non-invasively assessed using gadolinium contrast27 A signal intensity map can be created as contrast enters the pulmonary vasculature and special attention can then be focused on the peripheral microvasculature. Even in patients with mild COPD, a loss of pulmonary perfusion can sometimes be appreciated in the peripheral lung fields. Progressively greater loss of pulmonary blood flow is frequently seen with greater degrees of emphysema.
In conclusion, MRI of the lungs can provide images of lung structure similar to CT without the high risk of radiation, with additional advantages of imaging pulmonary microvasculature. Functional MRI can provide estimates of cardiac function and blood flow through the pulmonary microvasculature. These measures can potentially be used as end points for clinical trials, thus shortening the duration of some trials.
Abbreviations
chronic obstructive pulmonary disease, COPD; computed tomography, CT; magnetic resonance imaging, MRI; Hounsfield unit, HU; hazards ratio, HR; confidence interval, CI; pulmonary artery, PA; aorta, A; ratio of diameter of pulmonary artery to diameter of aorta, PA/A; body mass index, BMI; Body mass index-airflow Obstruction-Dyspnea-Exercise capacity index, BODE; National Lung Screening Trial, NLST; Centers for Medicare & Medicaid Services, CMS
References
- 1. Vestbo J,Hurd SS,Agusti AG,et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4):347-365. doi: http://dx.doi.org/10.1164/rccm.201204-0596PP [DOI] [PubMed] [Google Scholar]
- 2. Han MK. Clinical correlations of computed tomography imaging in chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2013;10( Suppl):S131-137. doi: http://dx.doi.org/10.1513/AnnalsATS.201303-046AW [DOI] [PubMed] [Google Scholar]
- 3. Hoffman EA,McLennan G. Assessment of the pulmonary structure-function relationship and clinical outcomes measures: quantitative volumetric CT of the lung. Acad Radiol. 1997;4(11):758-776. [DOI] [PubMed] [Google Scholar]
- 4. Wielputz M,Kauczor HU. MRI of the lung: state of the art. Diagn Interv Radiol. 2012;18(4):344-353. doi: http://dx.doi.org/10.4261/1305-3825.DIR.5365-11.0 [DOI] [PubMed] [Google Scholar]
- 5. Washko GR. The role and potential of imaging in COPD. Med Clin North Am. 2012;96(4):729-743. doi: http://dx.doi.org/10.1016/j.mcna.2012.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Newell JD Jr. . CT of emphysema. Radiol Clin North Am. 2002;40(1):31-42. [DOI] [PubMed] [Google Scholar]
- 7. Diaz AA,Morales A,Diaz JC,et al. CT and physiologic determinants of dyspnea and exercise capacity during the six-minute walk test in mild COPD. Respir Med. 2013;107(4):570-579. doi: http://dx.doi.org/10.1016/j.rmed.2012.12.011 [DOI] [PubMed] [Google Scholar]
- 8. Bhatt SP,Washko GR,Dransfield MT,Sieren JC,Newell JD Jr. ,Hoffman EA. Comparison of spirometric thresholds in diagnosing smoking-related airflow obstruction: authors' response. Thorax. 2014;69(12):1147-1148. doi: http://dx.doi.org/10.1136/thoraxjnl-2014-206123 [DOI] [PubMed] [Google Scholar]
- 9. Han MK,Kazerooni EA,Lynch DA,Liu LX,Murray S,Curtis JL,et al. Chronic obstructive pulmonary disease exacerbations in the COPDGene study: associated radiologic phenotypes. Radiology. 2011:261-261(1):274-282. doi: http://dx.doi.org/10.1148/radiol.11110173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Stockley RA,Parr DG,Piitulainen E,Stolk J,Stoel BC,Dirksen A. Therapeutic efficacy of alpha-1 antitrypsin augmentation therapy on the loss of lung tissue: an integrated analysis of 2 randomised clinical trials using computed tomography densitometry. Respir Res. 2010;11:136-136. doi: http://dx.doi.org/10.1186/1465-9921-11-136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Patel IS,Vlahos I,Wilkinson TM,et al. Bronchiectasis, exacerbation indices, and inflammation in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2004;170(4):400-407. doi: http://dx.doi.org/10.1164/rccm.200305-648OC [DOI] [PubMed] [Google Scholar]
- 12. Martinez-Garcia MA,de la Rosa Carillo D,Soler-Cataluna JJ,et al. Prognostic value of bronchiectasis in patients with moderate-to-severe chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;187(8):823-831. doi: http://dx.doi.org/10.1164/rccm.201208-1518OC [DOI] [PubMed] [Google Scholar]
- 13. Wells JM,Washko GR,Han MK,et al. Pulmonary arterial enlargement and acute exacerbations of COPD. N Engl J Med. 2012;367(10):913-921. doi: http://dx.doi.org/10.1056/NEJMoa1203830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Estepar RS,Kinney GL,Black-Shinn JL,et al. Computed tomographic measures of pulmonary vascular morphology in smokers and their clinical implications. Am J Respir Crit Care Med. 2013;188(2):231-239. doi: http://dx.doi.org/10.1164/rccm.201301-0162OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Celli BR,Cote CG,Marin JM,et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350(10):1005-1012. doi: http://dx.doi.org/10.1056/NEJMoa021322 [DOI] [PubMed] [Google Scholar]
- 16. Marquis K,Debigare R,Lacasse Y,et al. Midthigh muscle cross-sectional area is a better predictor of mortality than body mass index in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2002;166(6):809-813. doi: http://dx.doi.org/10.1164/rccm.2107031 [DOI] [PubMed] [Google Scholar]
- 17. Slone RM,Gierada DS. Radiology of pulmonary emphysema and lung volume reduction surgery. Semin Thorac Cardiovasc Surg. 1996;8(1):61-82. [PubMed] [Google Scholar]
- 18. Regan EA,Lynch DA,Curran-Everett D,et al. Clinical and radiologic disease in smokers with normal spirometry. JAMA Intern Med. 2015;175(9):1539-1549. doi: http://dx.doi.org/10.1001/jamainternmed.2015.2735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rennard S,Thomashow B,Crapo J,et al. Introducing the COPD Foundation Guide for Diagnosis and Management of COPD, recommendations of the COPD Foundation. COPD. 2013;10(3):378-389. doi: http://dx.doi.org/10.3109/15412555.2013.801309 [DOI] [PubMed] [Google Scholar]
- 20. National Lung Screening Trial Research Team; Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365(5):395-409. doi: http://dx.doi.org/10.1056/NEJMoa1102873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mets OM,Buckens CF,Zanen P,et al. Identification of chronic obstructive pulmonary disease in lung cancer screening computed tomographic scans. JAMA. 2011;306(16):1775-1781. doi: http://dx.doi.org/10.1001/jama.2011.1531 [DOI] [PubMed] [Google Scholar]
- 22. Iyer AS,Wells JM,Vishin S,Bhatt SP,Wille KM,Dransfield MT. CT scan-measured pulmonary artery to aorta ratio and echocardiography for detecting pulmonary hypertension in severe COPD. Chest. 2014;145(4):824-832. doi: http://dx.doi.org/10.1378/chest.13-1422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Fishman A,Martinez F,Naunheim K,et al. A randomized trial comparing lung-volume-reduction surgery with medical therapy for severe emphysema. N Engl J Med. 2003;348(21):2059-73. doi: http://dx.doi.org/10.1056/NEJMoa030287 [DOI] [PubMed] [Google Scholar]
- 24. Fain S,Schiebler ML,McCormack DG,Parraga G. Imaging of lung function using hyperpolarized helium-3 magnetic resonance imaging: Review of current and emerging translational methods and applications. J Magn Reson Imaging. 2010;32(6):1398-408. doi: http://dx.doi.org/10.1002/jmri.22375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kirby M,Pike D,McCormack DG,et al. Longitudinal computed tomography and magnetic resonance imaging of COPD: Thoracic Imaging Network of Canada (TINCan) study objectives. Chronic Obstr Pulm Dis (Miami). 2014; 1(1):200-211. doi: http://dx.doi.org/10.15326/jcopdf.1.2.2014.0136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Thomen RP,Sheshadri A,Quirk JD,et al. Regional ventilation changes in severe asthma after bronchial thermoplasty with (3)He MR imaging and CT. Radiology. 2015;274(1):250-259. doi: http://dx.doi.org/10.1148/radiol.14140080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hueper K,Parikh MA,Prince MR,et al. Quantitative and semiquantitative measures of regional pulmonary microvascular perfusion by magnetic resonance imaging and their relationships to global lung perfusion and lung diffusing capacity: the multiethnic study of atherosclerosis chronic obstructive pulmonary disease study. Invest Radiol. 2013;48(4):223-230. doi: http://dx.doi.org/10.1097/RLI.0b013e318281057d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Barr RG,Bluemke DA,Ahmed FS,et al. Percent emphysema, airflow obstruction, and impaired left ventricular filling. N Engl J Med. 2010;362(3):217-227. doi: http://dx.doi.org/10.1056/NEJMoa0808836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Smith BM,Kawut SM,Bluemke DA,et al. Pulmonary hyperinflation and left ventricular mass: the Multi-Ethnic Study of Atherosclerosis COPD Study. Circulation. 2013;127(14):1503-1511. doi: http://dx.doi.org/10.1161/CIRCULATIONAHA.113.001653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Grau M,Barr RG,Lima JA,et al. Percent emphysema and right ventricular structure and function: the Multi-Ethnic Study of Atherosclerosis-Lung and Multi-Ethnic Study of Atherosclerosis-Right Ventricle Studies. Chest. 2013;144(1):136-144. doi: http://dx.doi.org/10.1378/chest.12-1779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ian SS,Neil CB,Wai-Yee J,et al. The Effect of Reducing Lung Hyperinflation with Fluticasone Furoate/Vilanterol on Cardiac Structure, Function and Arterial Stiffness: A Cardiac Magnetic Resonance Study. B95 Getting Better: Advances in COPD Therapies. American Thoracic Society International Conference Abstracts: American Thoracic Society. 2015:A3642-A-A3642-A. [Google Scholar]
- 32. Regan EA,Lynch DA,Curran-Everett D,et al. Clinical and radiologic disease in smokers with normal spirometry. JAMA Intern Med. 2015. doi: http://dx.doi.org/10.1001/jamainternmed.2015.2735 [DOI] [PMC free article] [PubMed] [Google Scholar]


