Abstract
Objective
The purpose of this study was to evaluate the clinical value of technetium-99m-red blood cell (99mTc-RBC) scintigraphy in the diagnosis of orbital cavernous hemangioma (OCH).
Patients and methods
Forty-one patients with pathologically confirmed orbital mass, of which 10 were OCH, underwent 99mTc-RBC scintigraphy in this study. The scanning procedure included an initial perfusion phase, followed by an early and a delayed blood pool phase. All patients underwent ultrasonography and computed tomography (CT), and 15 patients also underwent MRI.
Results
All 10 OCH patients had no abnormal findings on radionuclide angiographic images and early blood pool phase, but increased activity was found during delayed blood pool phase. All other non-OCH orbital tumours did not have this tracer pattern. The radioactivity ratios of tumour to nontumour were 2.96±0.05 and 1.14±0.25, respectively, which had a statistically significant difference (t=15.18, P<0.001). Although nine of 10 OCH patients were diagnosed correctly with one false-positive case using ultrasound, both CT and MRI could not provide a definitive diagnosis.
Conclusion
99mTc-RBC scintigraphy is a reliable and useful procedure for the diagnosis of OCH. It may be considered as one of the routine clinical screening tools for the diagnosis of OCH and as a complement investigation to ultrasonography and CT.
Keywords: cavernous, erythrocytes, hemangioma, orbit, pyrophosphates, radionuclide imaging
Introduction
The cavernous hemangioma is the most common benign orbital tumour in adults and accounts for 3–7% of all orbital mass lesions 1. Its common manifestation is a slowly progressive, painless, unilateral proptosis. Visual acuity or field compromise, diplopia, and extraocular muscle or papillary dysfunction can result from compression of the intraorbital contents by the hemangioma. Nowadays, the transconjunctival approach is the most used technique in the management of intraorbital masses, replacing lateral orbitotomy. With this procedure, ophthalmic surgeons have reached optimal functional and aesthetic outcome in removing most of the orbital cavernous hemangiomas (OCHs). However, when the tumour is located in the apex or in the posterior and lateral third of the orbit, a multidisciplinary surgical approach is usually proposed. Differentiating cavernous hemangiomas from other orbital tumours can provide useful information when selecting the adequate surgical technique, in relation with adjacent structures, especially vessels and nerves 2. Ultrasound imaging, computed tomography (CT) and MRI accurately illustrate the shape, size and anatomical relationship of orbital masses, but the differential diagnosis of a unilateral orbital mass that causes proptosis can be difficult. Possibilities may be schwannoma, lymphangioma, cavernous hemangioma and so on. Moreover, complete excision of the tumour seems to avoid or reduce the risk of recurrence. This explains the importance of an accurate preoperative diagnosis of a cavernous hemangioma. The purpose of this study was to evaluate the clinical value of technetium-99m-red blood cell (99mTc-RBC) scintigraphy in the diagnosis of OCH.
Patients and methods
In this retrospective case series, we reviewed the medical records of 22 female and 19 male (mean age: 39±17.3 years; age range: 7–80 years) patients affected by an orbital mass, all pathologically proven, which include 10 OCHs, seven schwannomas, six venous hemangiomas, three meningiomas, three inflammatory pseudotumours, two varices, two dermoid cysts, another lymphoid epithelioma carcinoma, non-Hodgkin’s lymphoma, hemangiopericytoma, benign mixed tumour of the lacrimal gland, squamous cell carcinoma, inverted papilloma, tuberculoma and rhabdomyosarcoma one of each. All patients underwent conventional ultrasonography and CT, and 15 patients also underwent MRI.
A perfusion study and early and delayed blood pool studies were performed: 740 MBq of 99mTc-RBCs was prepared using a commercial kit suitable for routine clinical use. Pyrophosphate and technetium were purchased from the isotope Institute of China Institute of Atomic Energy. A preparation of 10 mg of pyrophosphate dissolved in 3 ml of water for injection was administered intravenously. Thirty minutes later, 740 MBq of 99mTcO4 was also administered intravenously by means of bolus injection. Imaging instrument used was the United States GE infinia Hawkeye4 dual probe single-photon emission computed tomography, (GE Medical systems, Functional Imaging, Tirat Hacarmel, Israel) (SPECT)/CT. The paediatric activity (MBq)=(age+1)/(age+7)×adult activity (740 MBq), volume less than or equal to 0.5 ml 3. Radionuclide angiography was performed with 2 s images (30 images during 1 min in a 64×64 matrix) obtained following a bolus injection of the radiopharmaceutical using a 180°-oriented dual-headed camera in anterior and posterior projections. The perfusion study was immediately followed by an early blood pool study conducted simultaneously for the anterior, posterior and two-side lateral views. Finally, late blood pool SPECT was performed at 30 min, 1 h and 4 h following injection. Transaxial, coronal and sagittal slices were generated with iterative filtered reconstruction. Two indicative slices at the orbital and sagittal sinus levels were chosen. Three regions of interest were drawn over the slices, and mean counts were calculated. Thereafter, the radioactivity ratios of the tumour to nontumour (T/N) were calculated using the following formula: T/N=lesion-side orbit counts/normal orbit counts. Diagnosis was based on orbital increase delayed uptake with a typical scintigraphic pattern known as perfusion blood pool mismatch, which is typical of cavernous hemangiomas because of their vascular structure (Fig. 1).
Fig. 1.
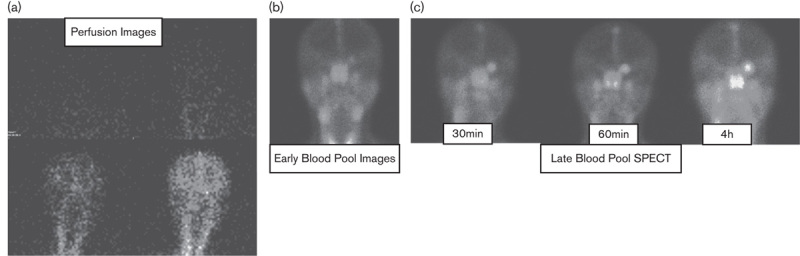
Technetium 99mTc-labelled red blood cell scintigraphy showing a typical perfusion blood pool mismatch. Radionuclide angiography (a) and early blood pool studies (b) demonstrate uptake in the normal anatomical structures. Characteristic delayed blood pool slices (c) demonstrate an intense uptake of the tracer in the right orbit. SPECT, single-photon emission computed tomography.
A statistical comparison between the groups was also made using the t-test, and a P value less than 0.05 was considered statistically significant. SPSS 11.5 was used to analyse the data.
Results
All patients showed normal images for perfusion and early blood pool studies. However, later SPECT images showed intense focal uptake in the lesion-side orbit in 10 patients, which confirmed the presence of cavernous hemangioma by means of surgical excision. All other non-OCH orbital tumours did not have abnormal findings during delayed blood pool phase. Some patients had no abnormal findings on radionuclide angiographic images, but increased activity was found on early blood pool phase, including two schwannomas, three venous hemangiomas, three lymphoid pseudotumours, two varices and one dermoid cyst. Other patients had no abnormal findings on early blood pool phase, but increased activity was found on radionuclide angiographic images, including three meningiomas, two lymphomas, one squamous cell carcinoma and one rhabdomyosarcoma. The others had no abnormal findings on each phase. The radioactivity ratios of the T/N between the group with OCH and the others were 2.96±0.05 and 1.14±0.25, respectively, which had a statistically significant difference (t=15.18, P<0.001).
Ultrasound imaging can illustrate the location, shape, size, boundary, anatomical relationship, internal echo, blood and condensability of orbital masses. Nine of 10 OCH patients were diagnosed correctly with l false-positive case by ultrasound, and one schwannoma was a misdiagnosis. CT and MRI accurately illustrate the anatomical characteristics of orbital masses, and MRI has great value in discriminating between the tumour and the optic nerve. However, CT and MRI are poor indicators of their vascular nature, which need an overview of clinical evaluations. Moreover, the exact diagnosis is often established by the pathologist after the surgical removal of the mass. Enhanced CT scan was performed for two non-OCH (lymphoid epithelioma carcinoma, inflammatory pseudotumour one for each), and enhanced MRI was performed for two OCH. Unfortunately, CT and MRI did not give qualitative diagnosis definitely.
Discussion
OCH is one of the vascular malformations. It takes the form of a clearly delineated vascular mass that contains large blood-filled spaces, which are lined with flattened endothelial cells and surrounded by a fibrous capsule. These spaces are apparently due to dilation and thickening of the walls of the capillary loops. The preoperational locational and qualitative diagnosis is important to operation method. However, the traditional techniques such as ultrasound and CT show lack of typical characteristics in some patients with OCH, which makes it difficult to differentiate the anatomical relationship of orbital masses with nearby structures. Consequently, the lateral surgical approach is performed. Nevertheless, some orbital tumour (i.e. schwannoma, neurofibromatosis) share some common characteristics on ultrasound or CT scans with OCH, but the operation method is different from OCH. This explains the importance of an accurate preoperative diagnosis of an OCH or other orbital tumour.
The typical appearance on ultrasound is oval to round, encapsulated with a density somewhat greater than that of muscle, having condensability and lacking blood signal inside the tumour on Doppler ultrasonography. The accuracy of qualitative diagnosis can reach to 94–95% 4. However, there are certain limitations on identifying the locational diagnosis of some tumours. On the basis of our study results, nine of 10 OCH patients were diagnosed correctly. CT scans are able to accurately illustrate the location, size, shape, boundary and the secondary change in nearby organization, such as proptosis, enlargement and resorption of the walls, thickening and transfer of the optic nerve, to discriminate the tumour and the nearby organization 5. However, the density difference between OCH and some benign tumours was not significant – for example, schwannoma, meningioma, leiomyoma, benign mesenchymal tumour and so on. In our study, CT can not give qualitative diagnosed definitely. MRI has great value in discriminating the tumour and the optic nerve. Thorn-Kany et al. 6 reported that isointensity relative to extraocular muscles on T1-weighted images and hyperintensity on T2-weighted images are typical findings of cavernous hemangioma. However, all other tumours have the same characteristic features, such as schwannoma, neurofibroma, hemangiopericytcoma and lymphangioma. Our results from cavernous hemangioma enhancement are homogeneous and heterogeneous, respectively.
Scintigraphy with 99mTc-RBC is commonly used in the evaluation of hepatic cavernous hemangiomas 7. The typical scintigraphic pattern known as perfusion blood pool mismatch, that is a normal image for perfusion and early blood pool studies, and a intense focal uptake for later SPECT images. Just because the cavernous hemangioma takes the form of a clearly delineated vascular mass that contains large blood-filled spaces, which are surrounded by a fibrous capsule. These vascular masses are apparently due to dilation and thickening of the walls of the capillary loops. However, because blood flow through the lesion is stagnant and independent from the orbital vascular system, the cavernous hemangioma does not fill with tracer within the perfusion and early blood pool images. After a certain period of time, the tumour was filled with 99mTc-RBC homogeneously. The technique of 99mTc-RBC scintigraphy may also be used in the noninvasive evaluation of extrahepatic vascular lesions such as vascular tumours of the orbit, which show the characteristic scintigraphic pattern, and can be diagnosed as cavernous hemangioma with a high degree of certainty 8. Sayit et al. 9 reported that, in all patients with OCH whom they studied, the preoperative diagnosis was confirmed by the typical pattern of perfusion blood pool mismatch on the 99mTc-RBC scintigraphy. Gdal-On et al. 10 performed 99mTc-RBC scintigraphy on 12 patients with OCH, all of whom were confirmed by means of histology. Polito et al. 11 performed 99mTc-RBC scintigraphy on 23 patients affected by an orbital mass previously revealed with CT and MRI and suggesting cavernous hemangioma. The results showed that the 99mTc-RBC scintigraphy results were positive in all cases of cavernous hemangioma and unfortunately also in one case of hemangiopericytoma and one case of lymphangioma. These two cases displayed increased uptake within the lesion on SPECT images (asymmetry index=4.94 and 3.68, respectively), which is probably due to the vascular nature of these tumours. This study shows that the 99mTc-RBC scintigraphy technique is a reliable tool for differentiating cavernous hemangiomas from other orbital masses (sensitivity, 100%; specificity, 86%) when ultrasound, CT, and MRI are not diagnostic. In our study, hemangiopericytoma and lymphangioma were not found; may be the two diseases have a low incidence. In the past 20 years, only eight (0.33%) hemangiopericytoma and seven (0.29%) lymphangioma were found from 2449 patients who were treated in the department of ophthalmology of the No. 2 hospital of Tianjin Medical University. In our study, the 99mTc-RBC scintigraphy in the diagnosis of OCH has high accuracy, which may be related to the small number of cases and involved orbital diseases. Therefore, the value of qualitative diagnosis with 99mTc-RBC scintigraphy still needs to increase cases and expand involved orbital diseases for further study.
All patients with OCH on the 99mTc-RBC scintigraphy displayed negative images of perfusion and early blood pool, and the positive images were found for later images. On the basis of our study, we suggest performing only the late study with SPECT at about 1 h after injection for diagnostic use. The plane delayed phase can present the typical hemangioma imaging features; however, the three-dimensional analysis was clearer and position was much better. The tomographic acquisition cannot be used as a routine diagnostic tool. Moreover, we may assert that patients with lesion-to-normal brain tissue greater than 2.5 are almost certainly affected by cavernous hemangioma. Patients with a lesion-to-normal brain tissue less than 2.0 are most probably affected by nonvascular tumours.
Conclusion
99mTc-RBC imaging is safe, relatively inexpensive, easy to perform and highly accurate. In particular, on the basis of our study results, an overview of clinical evaluations, ultrasound, CT scans or MRI studies, and scintigraphic patterns can establish the preoperative diagnosis of the orbit cavernous hemangioma. Moreover, 99mTc-RBC scintigraphy is a useful diagnostic tool in excluding tumours with a nonvascular origin responsible for unilateral painless proptosis. It may be considered as one of the routine clinical screening tools for the diagnosis of OCH and as a complement investigation to ultrasound, CT or MRI scans.
Acknowledgements
Conflicts of interest
There are no conflicts of interest.
References
- 1.Shields JA, Bakewell B, Augsburger JJ, Flanagan JC. Classification and incidence of space-occupying lesions of the orbit: a survey of 645 biopsies. Arch Ophthalmol 1984; 102:1606–1611. [DOI] [PubMed] [Google Scholar]
- 2.Missori P, Tarantino R, Delfini R, Lunardi P, Cantore G. Surgical management of orbital cavernous angiomas: prognosis for visual function after removal. Neurosurgery 1994; 35:34–38. [DOI] [PubMed] [Google Scholar]
- 3.Shen Z. Nuclear medicine [M]. Beijing, China: People’s Medical Publishing House; 1995. 230. [Google Scholar]
- 4.Yan J, Wu Z. Cavernous hemangioma of the orbit: analysis of 214 cases. Orbit 2004; 23:33–40. [DOI] [PubMed] [Google Scholar]
- 5.Guoxiang S, Hong Z. The new concept of the treatment of orbital tumor. Lin Shaoming editor In: Yuan Jiaqin, Lin Shaoming editor. Twenty-first Century frontier. Tianjin China: Tianjin science and Technology Press, 2001. 849–874. [Google Scholar]
- 6.Thorn-Kany M, Arrue P, Delisle MB, Lacroix F, Lagarrigue J, Manelfe C. Cavernous hemangiomas of the orbit: MR imaging. J Neuroradiol 1999; 26:79–86. [PubMed] [Google Scholar]
- 7.Malik MH. Blood pool SPECT and planar imaging in hepatic hemangioma. Clin Nucl Med 1987; 12:543–547. [DOI] [PubMed] [Google Scholar]
- 8.Burroni L, Borsari G, Pichierri P, Polito E, Toscano O, Grassetto G, et al. Preoperative diagnosis of orbital cavernous hemangioma: a 99mTc-RBC SPECT study. Clin Nucl Med 2012; 37:1041–1047. [DOI] [PubMed] [Google Scholar]
- 9.Sayit E, Durak I, Capakaya G, Yilmaz M, Durak H. The role of Tc-99m RBC scintigraphy in the differential diagnosis of orbital cavernous hemangioma. Ann Nucl Med 2001; 15:149–151. [DOI] [PubMed] [Google Scholar]
- 10.Gdal-On M, Gelfand YA, Israel O. Tc-99m labeled red blood cells scintigraphy: a diagnostic method for orbital cavernous hemangioma. Eur J Ophthalmol 1999; 9:125–129. [DOI] [PubMed] [Google Scholar]
- 11.Polito E, Burroni L, Pichierri P, Loffredo A, Vattimo AG. Technetium Tc 99m-labeled red blood cells in the preoperative diagnosis of cavernous hemangioma and other vascular orbital tumors. Arch Ophthalmol 2005; 123:1678–1683. [DOI] [PubMed] [Google Scholar]


