Abstract
Background
Multiple factors are believed to contribute to disruption of patients’ sleep and negatively affect clinical outcomes in the intensive care unit. Achieving restorative sleep for critically ill patients remains a challenge.
Objectives
To explore the perceptions and beliefs of staff, patients, and surrogates regarding the environmental and nonenvironmental factors in the medical intensive care unit that affect patients’ sleep.
Methods
This qualitative study included 24 medical intensive care unit staff (7 physicians, 5 respiratory therapists, 10 nurses, and 2 patient-care assistants), 8 patients, and 6 patient surrogates. Semistructured interviews were conducted, and qualitative analysis of content was used to code, categorize, and identify interview themes.
Results
Interview responses revealed 4 themes with related subthemes: (1) The overnight medical intensive care unit environment does affect sleep, (2) nonenvironmental factors such as difficult emotions and anxiety also affect sleep, (3) respondents’ erceptions about sleep quality in the medical intensive care unit were highly variable, and (4) suggestions for sleep improvement included reassuring patients and care-clustering strategies.
Conclusions
Results of this study suggest that environment is not the only factor influencing patients’ sleep. Decreases in environmental sources of disturbance are necessary but not sufficient for sleep improvement. Guideline-recommended clustered care is needed to provide adequate sleep opportunity, but patients’ emotions and anxiety also must be addressed.
Keywords: sleep, noise, critical care, anxiety
Introduction
Sleep disruption is identified as a major stressor in the intensive care unit (ICU) and is generally attributed to both environmental and patient factors such as disease acuity, stress, pain, anxiety, and pre-existing sleep disorders (1–4). Though there has been much focus on environmental sound as a source of sleep disruption (5, 6, 7), it is less clear to what degree other factors contribute to sleep disruption.
Critically ill patients are known to have disrupted sleep and circadian rhythms (5–8). Previous research has found that sleep in the ICU is characterized by short sleep time, poor quality sleep and increased daytime sleep (6, 9–12). Sleep that is sufficiently long, high quality, and timed to correspond with normal circadian rhythms is crucial to normal human physiology and is of particular importance for ICU patients who have increased anabolic requirements (13). Sleep disruption in ICU patients may contribute to adverse in-hospital and post-discharge outcomes, such as respiratory dysfunction, delirium, and post hospital syndrome (3, 14–18). Despite multidisciplinary efforts to improve the ICU environment and therefore provide adequate sleep opportunity, achieving restorative sleep remains a challenge (19). Prior studies have examined either patient’s or clinical staff’s perspectives on sleep in the ICU; few studies have used qualitative methods to compare environmental and non-environmental stressors as perceived by patients versus clinical staff. In addition, prior studies have not included members of the healthcare team such as respiratory therapists and patient care assistants who interact significantly with patients in the ICU (20).
We describe herein a qualitative study to address the following questions: (a) What are the perceptions and beliefs held by clinical staff, patients, and their surrogates about MICU environmental and non-environmental factors and the impacts on patients’ sleep? (b) What are the strategies suggested by patients, surrogates, and clinical staff to modify these factors and to improve patients’ sleep in the MICU? (c) Do differences exist among patients/surrogates and clinical staff with regard to their beliefs and perceptions of MICU stressors and the impacts on patients’ sleep?
Methods
Study Procedures
The study protocol and consent process were reviewed and approved by the institutional review board for protection of human subjects. An exploratory qualitative study was conducted using semi-structured interviews. The study was performed in a 38 bed MICU of a 1,000 bed tertiary academic hospital in the United States from June 2013 to February 2014. Eligible clinical staff for the study were defined as physicians, registered nurses, patient care assistants, and respiratory therapists who had worked overnight in the MICU and provided direct care to patients. The unit is rectangular with private patient rooms on four sides around a central core of workstations, supply closets, and conference rooms. Nurses work 12 hour shifts from 07:00–19:00 and 19:00–07:00. Daytime physician staffing utilizes several teams lead by an attending physician supported by trainees, advanced practice nurses and physician assistants. Overnight physician staff includes three intensivists and the on-call resident who work from 19:00–07:00. Visitors are allowed 24 hours a day. It is hospital policy that all patients receive a “quiet kit” which includes earplugs, an eye mask, and suggestions for being quiet after 21:00. Admissions occur around the clock.
Patients admitted to the MICU who stayed at least one night were invited to participate in the study after they were medically appropriate for transfer to the general medical floor. Patients were excluded from the study if they were: (a) less than 21 years old, (b) unable to speak English, (c) had neurological deficits (including delirium) preventing accurate verbal communication, (d) agitated or violent. The presence of delirium was identified via the confusion assessment method for the intensive care unit (CAM-ICU) (21). Surrogates of excluded patients were also invited to participate in the interview if they were able to speak English and had been present in the MICU during the patient’s admission. Sample size depended on the analysis of themes from clinical staff or the patient/surrogate categories. When no new relevant information was obtained during subsequent participant interviews (data saturation), enrollment was stopped for a given respondent category (22).
Patients were classified by gender, decade of life, race/ethnicity, length of ICU stay, and mechanical ventilation status; the collection of protected health information (PHI) was avoided. Clinical staff were classified by occupation, total years of experience, and years of ICU experience. Trained research assistants conducted the semi-structured interviews. Consistency of the topics covered was promoted by using an interview guide with questions that had been previously piloted (appendices A and B). Interviews were conducted in a private room.
Data Analysis
Interview data were transcribed and then managed via ATLAS-ti qualitative software Version 7 (www.atlasti.com, Corvallis, OR). Finalized, de-identified transcripts were analyzed using the thematic analysis method described by Braun and Clarke (23). Investigators read all the transcripts separately to preliminarily code and identify possible themes. Codes were reviewed and consolidated if overlap existed. Coding differences were discussed until consensus was reached and an original codebook was developed. Following the development of the codebook, the research team grouped the codes into themes and subthemes and produced a qualitative report. Statistical analysis of quantitative data were carried out using SAS 9.2 (SAS Institute, Cary, NC).
Results
Survey Respondent Characteristics
Eight patients, six surrogates, and twenty-four clinical staff participated in this study. Respondent characteristics are shown in Tables 1. The mean length of MICU stay for patients was 4.1 days (SD 5.2). The MICU staff represented four health profession groups: physicians (n=8; 32%), nurses (n=10; 40%), respiratory therapists (n=5; 20%), and patient care assistants (n=2; 8%). The MICU staff had an average of 4.8 years (SD=4.9) clinical experience in their reported role.
Table 1.
Participant characteristics, Patients (n=14) and Clinical Staff (n=24)
| Age of patients (years) | 21–40 Years: | n = 1 |
| 41–60 Years: | n = 7 | |
| > 60 Years: | n = 6 | |
|
| ||
| Patient gender | Female | n = 5 (36%) |
|
| ||
| Patient race | Nonwhite | n = 4 (29%) |
|
| ||
| Mechanical Ventilation during MICU Admission (yes / no) | Yes | n = 7 (50%) |
|
| ||
| Self-identified poor sleepers | n =3 (21%) | |
|
| ||
| Surrogate (n=6) relation to patient | Spouse: | n = 3 |
| Child: | n = 2 | |
| Sibling: | n = 1 | |
|
| ||
| Clinical Staff Roll | Nurse | n =10 |
| Physician | n =7 | |
| Respiratory Therapist | n =5 | |
| Patient Care Assistant | n =2 | |
|
| ||
| Staff Gender | Female | n = 16 (67%) |
|
| ||
| Staff Race | Nonwhite | N = 6 (25%) |
|
| ||
| Staff Length MICU Experience (years), mean ± standard deviation | 4.8 ± 4.9 | |
|
| ||
| Staff in training: residency, fellowship or orientation (yes / no) | 8% (yes) | |
Themes and Subthemes
Four main themes regarding overnight sleep emerged following data analysis: (1) effect of environmental factors; (2) effect of non-environmental factors; (3) perceptions of sleep quality; and (4) strategies to improve sleep. Within each main theme, a number of subthemes emerged and are reported below, along with exemplary statements from participants. Verbatim quotes from the study participants are labelled with subject role (staff, patient or surrogate) and subject identification code.
Theme 1: The MICU environment affects overnight sleep
Subtheme 1.1: The MICU environment at night is noisy with a high-level of in-room interruptions and excessive light exposure
The primary perception of the MICU environment held by staff is that the MICU is noisy; this was less pronounced in the patient/surrogate group. Among the participants in our study, 21% of patient/surrogate group and 100% of clinical staff members identified noise as the major environmental stressor that affected patient’s nighttime sleep. All respondents (100%, 38/38) noted that in-room disruptions were frequent at night. Table 2a presents the sources of noise identified by our respondents. Table 2b and c lists sources of nocturnal in-room disruptions identified by our respondents; these included routine procedures (62% of listed activities) and time-sensitive care (38% of listed activities).
Table 2.
Sources of disturbance
| % of staff (N=24) reporting n (%) |
% of patients/surrogates (N=14) reporting n (%) |
|
|---|---|---|
| a. Sources of noise | ||
| Alarms (IV pump, monitors, pagers, overhead paging) | 16 (67%) | 3 (21%) |
| Talking (providers, visitors and patients) | 3 (13%) | 1 (7%) |
| Noise from other rooms or nurse workstation including TV, phone, computer | 9 (38%) | 2 (14%) |
| Floor cleaners/moving equipment | 2 (8%) | |
| b. Disturbance from routine patient care | ||
| Blood drawn (including checking blood sugar) | 13 (54%) | 8 (57%) |
| Medication administration | 11 (46%) | 7 (50%) |
| Bathing, Skin Check, Weighing patient | 12 (50%) | 1 (7%) |
| Respiratory care/treatment | 5 (21%) | 3 (21%) |
| X-ray, CT scan, MRI | 3 (13%) | |
| Visitors | 5 (21%) | |
| c. Disturbance from time sensitive care | ||
| Emergency | 7 (29%) | |
| Patient admission or discharge | 5 (21%) | |
| Vital signs or timed RN assessment (e.g. RASS, GCS) | 7 (29%) | 7 (50%) |
| Procedures, Support device adjustment | 3 (13%) | 1 (7%) |
| Pain management, patient turns, toileting | 10 (42%) | 2 (14%) |
Subtheme 1.2: Unpredictable work flow causes overnight environmental disturbance which disturbs sleep
Participants (n=12, 48%) from the clinical staff group perceived environment disturbance caused by unpredictable work flow as contributing to sleep disturbance. Staff also indicated that work flow maybe a non-modifiable stressor on sleep and a trigger for multiple other environmental stressors such as noise, light and in-room interruptions (Table 5).
Table 5.
Clinical staff descriptions of the medical intensive care unit at night
General impression
|
Noise
|
In-room interruptions
|
Light
|
Workflow
|
Subtheme 1.3: Patients and their surrogates thought that noise and in-room interruptions are expected and reassuring
Participants from the patient and surrogate group identified noise and in-room interruptions as factors that influence overnight sleep in the MICU, but they considered these factors to be expected in the hospital (Table 3, 4). Most patients/surrogates (88%) were satisfied with the current MICU environment and 50% of patients/surrogates considered in-room interruptions necessary at night. They indicated that being monitored closely by the providers was appropriate and reassuring.
Table 3.
Patient descriptions of the medical intensive care unit at night
Noise
|
In-room Interruptions
|
Table 4.
Surrogate descriptions regarding sleep in the medical intensive care unit
Sleep
|
Theme 2: Non-environmental stressors affect overnight sleep
Subtheme 2.1. Psychological factors affected sleep more than environmental factors
Informants from both the patient/surrogate group and the staff group reported that non-environmental stressors interfered with the patients’ ability to achieve high quality sleep in the MICU. More than half of the participants (54% from the patient/surrogate group) indicated that psychological factors, especially emotional factors and cognitive factors, affect sleep more than the MICU environment. Patients expressed that uncertainty and worry about their health condition affected their sleep negatively: “I didn’t get as much sleep as I wanted… but I had a lot of things on mind… I had some bad-pretty bad news (patient, 6013).”
Subtheme 2.2. Chronic sleep loss contributed to sleep disruption
Participants from the patient group experienced sleep disturbance that was associated with pre-existing sleep disorders. Three out of fourteen (21%) patients noted that much of their sleep issues were chronic: “that’s the way I always sleep….I don’t ever sleep well at night (patient, 6005).”
Subtheme 2.3 Acute Illness affected sleep
Twelve out of twenty-four (50%) staff in the MICU noted that other factors such as illness and physical discomfort (for example pain) also contributed to sleep abnormalities in patients: “If I were a patient and I had an ET [endotracheal] tube and a Foley and lines and everything, I don’t think I’d be able to sleep very comfortably (staff, 7014).”
Theme 3: Perceptions of sleep quality and how it was achieved in the MICU were variable
Theme 3.1. Opinions about MICU patient sleep quality were mixed
Sleep quality in the MICU was described as poor by 29% of the patient/surrogate group and 63% of the clinical staff. Surprisingly, 57% of patients/surrogates indicated that they achieved good quality sleep. Both sets of respondents agreed that sleep is important to MICU patients’ recovery; yet only 8% of clinical staff reported prioritizing sleep into their routine patient care. In response to questions addressing the amount of sleep that patients were achieving, 57% of patients responded “sufficient” versus 36% who said “not enough.” About one-half of staff (54%) provided estimates that patients slept between 2 and 4 hours per night.
Theme 3.2. The amount and quality of sleep was caused by or related to sedating medications
57% of the patient/surrogate group and 21% of clinical staff assumed that the amount and quality of sleep was related to sedating medications. “He [the patient] was sleeping fine because he had medication to calm him down…he was sleeping most of the time, even during the day (surrogate, 6002).”
Theme 4: Participants offered varied strategies to improve sleep in the MICU
Subtheme 4.1. Cluster and reschedule MICU care at night
The most commonly suggested sleep promoting interventions from the staff were clustering of care (83%) and rescheduling aspects of care (96%) (Table 6). Other staff reported sleep promoting interventions including reducing noise (58%), keeping patients awake during the day so they can sleep at night (38%), promoting patient comfort, (29%) drawing the curtain to block out light or closing the sliding door to reduce noise (17%).
Table 6.
Suggestions by clinical staff regarding sleep improvement
Reschedule and Clustering of Care
|
Staff education
|
Subtheme 4.2: Staff thought that sleep related education would improve MICU sleep
Over 40% staff considered staff education on topics related to sleep and sleep improvement in MICU as a means to promote sleep in MICU (Table 6). Most of the staff who participated in this study said they were aware of the hospital’s effort to reduce environment stressors and promote sleep, but some of them expressed their interest in learning about the evidence to support sleep management practices in MICU.
Subtheme 4.3. Difficult feelings worsen sleep and reassurances from staff could assist sleep
Related to subtheme 2.1 above, participants stressed the importance of managing emotions as a strategy to improve sleep in MICU. Half of the patient/surrogate group (50%) suggested that staying in close contact with clinical staff for reassurance would improve patients’ sleep.
Subtheme 4.4 Participants recommend sedating medications for sleep improvement
Related to the perception that sedating medication promote sleep, 43% of the patient/surrogate group recommended that clinicians could prescribe sleep aids to help patients’ sleep better in MICU: “I don’t think you can help patients sleep better except for giving them a strong sleeping pill (surrogate, 6012).” Staff (21%) also thought that sedating medications helped patients to sleep.
Discussion
We investigated the perceptions of clinical staff, patients, and surrogates regarding the impact of MICU environmental on patient’s sleep, explored alternative factors contributing to poor sleep, and obtained novel suggestions on interventions for sleep improvement in the MICU. Our data showed contrasting beliefs between staff and patients and revealed that anxiety and emotion may have far higher impact on patient sleep than noise or light. Examining these qualitative data extends our understanding of patients’ sleeping experiences in the ICU.
Our study findings mimic the findings of other investigators in identifying noise and in-room disturbance as environmental factors interfering with patient sleep. Previous studies reported environmental stressors, especially noise, as the most disruptive factor contributing to poor sleep in the ICU (24, 25). However, polysomnography studies show that a minority (10%–30%) of overnight arousals occurred due to noise (7, 26, 27). Providers and patients did not reflect a belief that underlying illness can contribute to poor sleep indicating a possible knowledge gap (28). Some patient respondents did note that pre-existing sleep problems influenced their sleep during hospitalization. Importantly, we found that patients and surrogates (versus clinical staff) appeared to be more concerned with emotional and cognitive stressors. This highlights a possible misdirection in the field of ICU sleep research which has been overwhelmingly focused on environmental modification.
The findings on subjective perceptions of sleep quality are incongruent with many studies exploring quantity and quality of a patient’s sleep within the ICU. The majority of the staff in our study recognized that an ICU patient’s sleep is shortened and fragmented. In contrast, many participants in the patient/surrogate group stated that they had sufficient sleep during their MICU stay and rated their sleep quality as good. Patients did modify their responses with descriptors such as “considering it was in a hospital.” Patient responses may have been driven by low expectations and/or inability to perceive poor sleep in the context of critical illness.
Many ICU patients, including our study subjects, believe that sedatives facilitate sleep (29). However, evidence from studies exploring the effects of sedation on ICU patients’ sleep suggest that sedative medication contributes to sleep disruption (30, 31). Though benzodiazepines and opioids do increase total perceived sleep time, REM and slow wave sleep are decreased (23, 31). Therefore, patients who receive pharmacological sedation for sleep may not receive the physiologic and immunologic benefits of sleep (29). These responses indicate that there is a lack of understanding of the relationship between sleep and sedation among health care providers, surrogates and patients, and highlights an opportunity for provider training and patient education.
A wide variety of different ICU sleep improvement interventions were suggested by participants in the study. Staff focused primarily on modifying the environment, particularly noise reduction and nighttime patient-care work-flow. Current guidelines on improving sleep for hospitalized patients emphasize a multidisciplinary, integrated strategy for clustering care and reducing environmental disturbance as a means of ICU sleep promotion (32–34). This strategy will provide sleep opportunity for the patient but is likely only a first step. Participants reported a high frequency of overnight in-room patient care activity, however this study extends previous work (30, 35, 36) by documenting that frequent patient care activities signal close monitoring by staff and may therefore decrease patient anxiety. ICU studies investigating the effects of sedation on sleep quality, anxiety and depression, demonstrated that one-half of ICU patients experienced severe anxiety and depression (37, 38). As noted by our respondents, high levels of emotional and psychological distress are likely contributing to disturbed sleep patterns, and, therefore, the emotional needs of patients should be considered in developing sleep promotion protocols.
Strengths and Limitations of Study
There were several strengths of this study. This study included a diverse sample of key MICU stakeholders including patients, surrogates, physicians, nurses, respiratory therapists, and patient-care assistants. Further, the majority of studies of ICU sleep have focused primarily on investigating environmental influences on sleep, this study explored non-environmental factors that affect sleep in ICU. Finally, the use of semi-structured interviews in this study allowed more in-depth information surrounding the issue of stressors and sleep in the ICU.
Limitations of this study included the unequal proportion of patient/surrogate and clinical staff and the small number of patients and surrogates enrolled in the study. We did follow the principle of data saturation to ensure that most important perceptions were uncovered. Many of the surrogates approached did not stay the whole night in the MICU and could not provide responses. In addition, many patients were delirious at the time of MICU discharge and were unable to answer the open-ended questions. Conducting the study in only one MICU is a limitation to the generalizability of the study findings to other MICUs or non-medical ICUs. It is also possible that patients and surrogates were reluctant to make comments that might be construed as critical of their care, although they were encouraged to speak freely. Another limitation related to this study is the potential for bias in staff’s responses regarding the importance of sleep in the ICU as many of these staff were aware of the study investigators’ interest in ICU sleep promotion.
Implications for Research and Practice
Further research could employ both subjective and objective sleep measures, and compare the sleep quality of ICU patients who report psychological stress. Although it seems clear that unnecessary, disruptive care such as routine wound checks or bathing should not occur overnight, bedside activities which have a dual role of providing reassurance should not be necessarily eliminated. It may also be important to explore sleep promoting interventions that more directly address the cognitive and emotional needs of patients in the ICU. Interventions could include a more reliable evaluation of patients’ psychological stress as well as their perceptions on what they believed would be helpful to reduce anxiety and improve sleep. Relaxation skills and evidence-based stress reduction intervention can be offered. Frequent communication between staff and patient regarding change of their status and reassurance should be encouraged. Future research can be design to the test the feasibility and effect of such a holistic care intervention.
Conclusions
This exploratory qualitative study examined perceptions and beliefs about ICU stressors and how such stressors impact patient sleep. The findings demonstrate that psychological factors play an important role in ICU sleep disturbance, and may outweigh environmental factors in contributing to poor sleep. Researchers, hospital administrators, and clinicians striving to improve sleep in the ICU can design and test sleep-promoting interventions that combine cognitive-behavioral approaches with environmental modifications (Figure 1). Given the knowledge gap in understanding sleep, its impact on health outcomes, and the relationship between sleep and sedation, there is a need to promote sleep related training among ICU staff and to raise the awareness of sleep among patients and the public.
Figure 1.
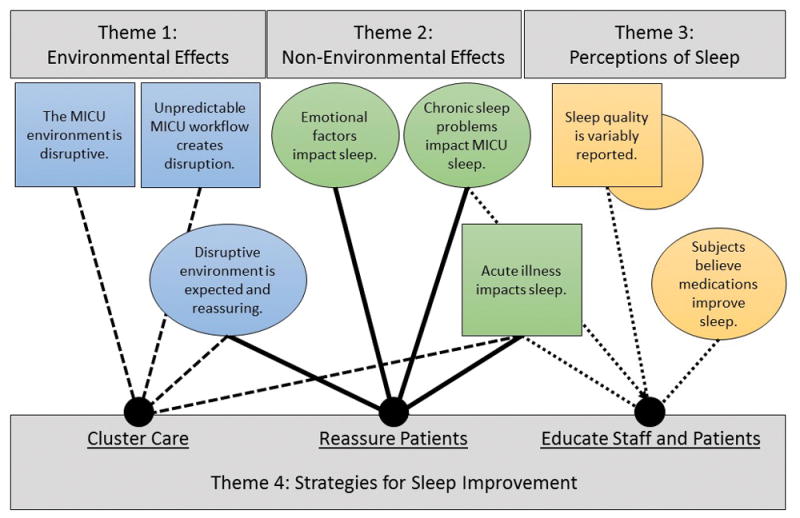
Summary of themes, subthemes and consequent design of sleep intervention. This figure shows clustering of care for sleep opportunity is important but also important is patient reassurance and staff and patient education.
Supplementary Material
Acknowledgments
The authors thank David Samuel for assisting in collecting data. We also thank the dedicated patients, families and staff who participated in the study.
Funding: This work was funded by P20NR014126.
Footnotes
Institution: This work was conducted at Yale-New Haven Hospital and Yale University Schools of Medicine and Nursing in New Haven, Connecticut.
References
- 1.Novaes MAFP, Knobel E, Bork AM, et al. Stressors in ICU: Perception of the patient, relatives and health care team. Intensive Care Medicine. 1999;25(12):1421–1426. doi: 10.1007/s001340051091. [DOI] [PubMed] [Google Scholar]
- 2.Little A, Ethier C, Ayas N, et al. A patient survey of sleep quality in the Intensive Care Unit. Minerva Anestesiol. 2012;78(4):406–414. [PubMed] [Google Scholar]
- 3.Kamdar BB, Needham DM, Collop NA. Sleep deprivation in critical illness: its role in physical and psychological recovery. J Intensive Care Med. 2012;27(2):97–111. doi: 10.1177/0885066610394322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Knauert MP, Malik V, Kamdar BB. Sleep and sleep disordered breathing in hospitalized patients. Semin Respir Crit Care Med. 2014;35(5):582–592. doi: 10.1055/s-0034-1390080. [DOI] [PubMed] [Google Scholar]
- 5.Aurell J, Elmqvist D. Sleep in the surgical intensive care unit: continuous polygraphic recording of sleep in nine patients receiving postoperative care. Br Med J (Clin Res Ed) 1985;290(6474):1029–1032. doi: 10.1136/bmj.290.6474.1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cooper AB, Thornley KS, Young GB, et al. Sleep in critically ill patients requiring mechanical ventilation. Chest. 2000;117(3):809–818. doi: 10.1378/chest.117.3.809. [DOI] [PubMed] [Google Scholar]
- 7.Freedman NS, Gazendam J, Levan L, Pack AI, Schwab RJ. Abnormal sleep/wake cycles and the effect of environmental noise on sleep disruption in the intensive care unit. Am J Respir Crit Care Med. 2001;163(2):451–457. doi: 10.1164/ajrccm.163.2.9912128. [DOI] [PubMed] [Google Scholar]
- 8.Hilton BA. Quantity and quality of patients’ sleep and sleep-disturbing factors in a respiratory intensive care unit. J Adv Nurs. 1976;1(6):453–468. doi: 10.1111/j.1365-2648.1976.tb00932.x. [DOI] [PubMed] [Google Scholar]
- 9.Elliott R, McKinley S, Cistulli P, Fien M. Characterisation of sleep in intensive care using 24-hour polysomnography: an observational study. Crit Care. 2013;17(2):R46. doi: 10.1186/cc12565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Drouot X, Cabello B, d’Ortho MP, Brochard L. Sleep in the intensive care unit. Sleep Med Rev. 2008;12(5):391–403. doi: 10.1016/j.smrv.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 11.Friese RS, Diaz-Arrastia R, McBride D, Frankel H, Gentilello LM. Quantity and quality of sleep in the surgical intensive care unit: are our patients sleeping? J Trauma. 2007;63(6):1210–1214. doi: 10.1097/TA.0b013e31815b83d7. [DOI] [PubMed] [Google Scholar]
- 12.Knauert MP, Yaggi HK, Redeker NS, et al. Feasibility study of unattended polysomnography in medical intensive care unit patients. Heart Lung. 2014;43(5):445–452. doi: 10.1016/j.hrtlng.2014.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Evans JC, French DG. Sleep and healing in intensive care settings. Dimensions of critical care nursing : DCCN. 1995;14(4):189–199. doi: 10.1097/00003465-199507000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Bourne RS, Mills GH. Sleep disruption in critically ill patients--pharmacological considerations. Anaesthesia. 2004;59(4):374–384. doi: 10.1111/j.1365-2044.2004.03664.x. [DOI] [PubMed] [Google Scholar]
- 15.Thomason JW, Shintani A, Peterson JF, et al. Intensive care unit delirium is an independent predictor of longer hospital stay: a prospective analysis of 261 non-ventilated patients. Crit Care. 2005;9(4):R375–381. doi: 10.1186/cc3729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pisani MA, Kong SY, Kasl SV, et al. Days of delirium are associated with 1-year mortality in an older intensive care unit population. Am J Respir Crit Care Med. 2009;180(11):1092–1097. doi: 10.1164/rccm.200904-0537OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krumholz HM. Post-hospital syndrome--an acquired, transient condition of generalized risk. N Engl J Med. 2013;368(2):100–102. doi: 10.1056/NEJMp1212324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kamdar BB, King LM, Collop NA, et al. The effect of a quality improvement intervention on perceived sleep quality and cognition in a medical ICU. Crit Care Med. 2013;41(3):800–809. doi: 10.1097/CCM.0b013e3182746442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sareli AE, Schwab RJ. The sleep-friendly ICU. Crit Care Clin. 2008;24(3):613–626. viii. doi: 10.1016/j.ccc.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 20.Hopper K, Fried T, Pisani M. Health care worker attitudes and identified barriers to patient sleep in the medical intensive care unit. Heart Lung. 2015;44(2):95–99. doi: 10.1016/j.hrtlng.2015.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU) JAMA. 2001;286(21):2703–2710. doi: 10.1001/jama.286.21.2703. [DOI] [PubMed] [Google Scholar]
- 22.Marshall MN. Sampling for qualitative research. Fam Pract. 1996;13(6):522–525. doi: 10.1093/fampra/13.6.522. [DOI] [PubMed] [Google Scholar]
- 23.Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3(2):77–101. [Google Scholar]
- 24.Topf M, Thompson S. Interactive relationships between hospital patients’ noise-induced stress and other stress with sleep. Heart Lung. 2001;30(4):237–243. doi: 10.1067/mhl.2001.116592. [DOI] [PubMed] [Google Scholar]
- 25.Simpson T, Lee ER, Cameron C. Relationships among sleep dimensions and factors that impair sleep after cardiac surgery. Res Nurs Health. 1996;19(3):213–223. doi: 10.1002/(SICI)1098-240X(199606)19:3<213::AID-NUR5>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 26.Gabor JY, Cooper AB, Crombach SA, et al. Contribution of the intensive care unit environment to sleep disruption in mechanically ventilated patients and healthy subjects. Am J Respir Crit Care Med. 2003;167(5):708–715. doi: 10.1164/rccm.2201090. [DOI] [PubMed] [Google Scholar]
- 27.Kahn DM, Cook TE, Carlisle CC, et al. Identification and modification of environmental noise in an ICU setting. Chest. 1998;114(2):535–540. doi: 10.1378/chest.114.2.535. [DOI] [PubMed] [Google Scholar]
- 28.McGuire BE, Basten CJ, Ryan CJ, Gallagher J. Intensive care unit syndrome: a dangerous misnomer. Arch Intern Med. 2000;160(7):906–909. doi: 10.1001/archinte.160.7.906. [DOI] [PubMed] [Google Scholar]
- 29.Peitz GJ, Balas MC, Olsen KM, Pun BT, Ely EW. Top 10 myths regarding sedation and delirium in the ICU. Crit Care Med. 2013;41(9 Suppl 1):S46–56. doi: 10.1097/CCM.0b013e3182a168f5. [DOI] [PubMed] [Google Scholar]
- 30.Weinhouse GL, Watson PL. Sedation and sleep disturbances in the ICU. Crit Care Clin. 2009;25(3):539–549. ix. doi: 10.1016/j.ccc.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 31.Boyko Y, Ording H, Jennum P. Sleep disturbances in critically ill patients in ICU: how much do we know? Acta Anaesthesiol Scand. 2012;56(8):950–958. doi: 10.1111/j.1399-6576.2012.02672.x. [DOI] [PubMed] [Google Scholar]
- 32.Walder B, Francioli D, Meyer JJ, Lancon M, Romand JA. Effects of guidelines implementation in a surgical intensive care unit to control nighttime light and noise levels. Crit Care Med. 2000;28(7):2242–2247. doi: 10.1097/00003246-200007000-00010. [DOI] [PubMed] [Google Scholar]
- 33.Dennis CM, Lee R, Woodard EK, Szalaj JJ, Walker CA. Benefits of quiet time for neuro-intensive care patients. J Neurosci Nurs. 2010;42(4):217–224. doi: 10.1097/jnn.0b013e3181e26c20. [DOI] [PubMed] [Google Scholar]
- 34.Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013;41(1):263–306. doi: 10.1097/CCM.0b013e3182783b72. [DOI] [PubMed] [Google Scholar]
- 35.Tamburri LM, DiBrienza R, Zozula R, Redeker NS. Nocturnal care interactions with patients in critical care units. Am J Crit Care. 2004;13(2):102–112. quiz 114–105. [PubMed] [Google Scholar]
- 36.Tembo AC, Parker V. Factors that impact on sleep in intensive care patients. Intensive Crit Care Nurs. 2009;25(6):314–322. doi: 10.1016/j.iccn.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 37.Treggiari-Venzi M, Borgeat A, Fuchs-Buder T, Gachoud JP, Suter PM. Overnight sedation with midazolam or propofol in the ICU: Effects on sleep quality, anxiety and depression. doi: 10.1007/BF01709334. [DOI] [PubMed] [Google Scholar]
- 38.Treggiari-Venzi M, Borgeat A, Fuchs-Buder T, Gachoud JP, Suter PM. Overnight sedation with midazolam or propofol in the ICU: Effects on sleep quality, anxiety and depression. Intensive Care Medicine. 1996;22(11):1186–1190. doi: 10.1007/BF01709334. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


