Abstract
Background
Following through on one's goals to study is essential for effective, self-regulated learning. This can be difficult for residents because of clinical demands and limited personal time. WOOP (Wish, Outcome, Obstacle, Plan) is a self-regulation strategy, also known as mental contrasting with implementation intentions. WOOP increases follow-through on goals in many domains, although it has not, to our knowledge, been evaluated in medical education.
Objective
We compared the effect of WOOP versus goal setting on time residents spent studying.
Methods
Through a prospective, randomized, comparative effectiveness study, during a 1-month, intensive care unit rotation, we clustered anesthesiology residents in single-blind fashion to WOOP versus goal setting. Both groups received organized study materials. The intervention group performed WOOP to study more; the comparison group set goals to study more. Residents tracked studying with daily diaries. The primary outcome was total time spent studying toward stated goals. Time spent studying “non-goal” medical material was a secondary outcome.
Results
Of 34 eligible residents, 100% participated. Sixteen residents were randomized to the WOOP group and 18 to the goal-setting group. The WOOP group spent significantly more time studying toward their goals compared with the goal-setting group (median = 4.3 hours versus 1.5 hours; P = .021; g = 0.66). There was no significant difference in time spent studying non-goal medical material between groups (median = 5.5 hours versus 5.0 hours, P = .99).
Conclusions
WOOP increased the time residents spent studying toward their goals as compared with setting goals alone.
What was known and gap
Self-regulated learning is a critical skill for physicians, yet few studies have explored effective approaches to increase it in resident physicians.
What is new
A cluster randomized trial of a self-regulation strategy (wish, outcome, obstacle, plan [WOOP]) showed anesthesiology residents in the intervention group spent significantly more time studying toward goals compared with a goal-setting group.
Limitations
Single specialty and single site limit generalizability; with self-reported outcomes.
Bottom line
WOOP appears to be a useful strategy for increasing self-regulated learning by residents.
Introduction
Self-regulated learning involves the autonomous selection, management, and evaluation of personal learning activities.1 Formation of relevant learning goals and subsequent execution of plans to reach those goals are critical for effective, self-regulated learning. Unfortunately, goals (ie, intentions) alone are poor predictors of subsequent behavior,2–4 and, in a meta-analysis, predicted only 28% of subsequent behavior.4 That percentage is even lower when confounders, such as prior behavior, are taken into account.
The gap between intention and action results from many factors, including failure to initiate goal-directed behaviors and the derailment of relevant efforts when distractions arise.5 This intention-action gap may be especially pronounced for residents, who are often highly absorbed in ongoing clinical duties, emotionally drained, or sleep deprived.6 Despite these obstacles, residents need to engage in self-regulated study to meet personal or program-level learning objectives. Strategies that promote follow through on goal-related behaviors should be of great interest to learners and educators alike.
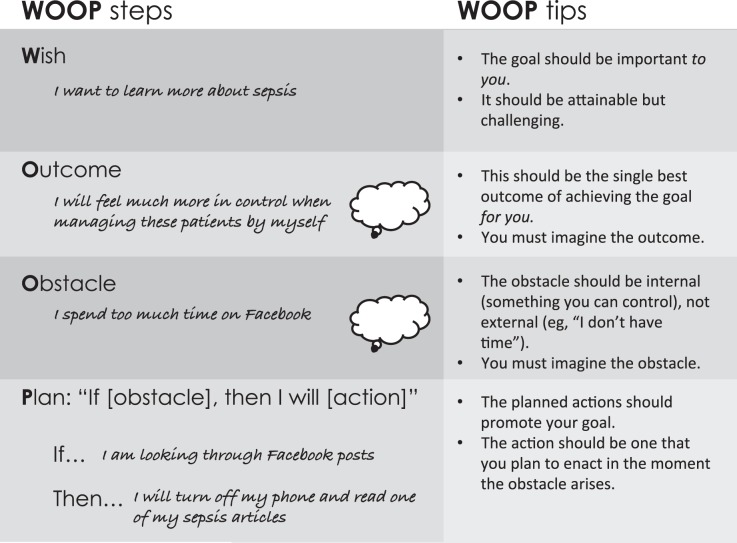
WOOP, known in the cognitive psychology literature as mental contrasting with implementation intentions, is an imagery exercise that increases goal commitment and behavioral change compared with relevant comparator groups such as goal setting.7–10 WOOP involves performing 4 sequential steps: (1) identifying a meaningful goal (Wish); (2) identifying and imagining the best outcome of accomplishing this goal (Outcome); (3) identifying and imagining the critical inner obstacle to accomplishing that goal (Obstacle); and (4) forming an “if-then” plan to overcome that obstacle in the form, “If [obstacle], then I will [action to overcome obstacle]” (Plan). An example of how WOOP is used, along with tips for each step, is illustrated in the Figure.7,8,11
Figure.
An Example of WOOP With Tips for Each Step
Note: To use WOOP, individuals must engage in 4 distinct sequential steps: (1) selecting a goal or wish (Wish); (2) identifying and imagining the single best outcome of achieving this goal (Outcome); (3) identifying and imagining the most critical inner obstacle to achieving this goal (Obstacle); and (4) identifying an action to overcome this obstacle and putting it in the form of an “if [obstacle], then I will [action]” (Plan).
WOOP increases goal attainment compared with goal setting alone, with medium-to-large effect sizes across many domains and populations.11–14 This positive impact on behaviors has been observed for up to 2 years after a single, brief training intervention, and the effect is present even for initiating unpleasant tasks necessary to achieve goals (eg, diet modification to improve health).14–16 Various mechanisms underlie the effectiveness of WOOP. For example, strong, nonconscious links are forged between obstacles and intended actions. Individuals then automatically act to overcome obstacles the moment they arise.17–20
There have been suggestions to use WOOP with medical education,2 yet, to our knowledge, no studies have assessed its use in medical education. We report the findings of a prospective, randomized, comparative effectiveness study, in which residents attempted to increase time spent studying, using either WOOP or goal setting.
Methods
Participants and Setting
From March to August 2015, we performed a prospective, cluster, randomized study of anesthesiology residents in postgraduate years 2 through 4 during a 1-month, intensive care unit (ICU) rotation at Massachusetts General Hospital. All residents were eligible to participate. Cluster randomization by month was used to decrease the chance of strategy leak between groups. The “rand()” Excel spreadsheet (Microsoft, Redmond, WA) function was used to randomly allocate participants in the first month. In this manner, all residents in the first month were randomly assigned to the comparator group, and group assignment alternated month to month thereafter. Cluster size for each month was 6. These assignments did not follow a prespecified pattern, and the clinicians involved in this study did not make the clinical assignments.
Residents were blind to their group assignment, and both groups received an intervention of similar length. Because of the in-person training, it was not possible for investigators to be blind to group assignment. Resident participation in the study was voluntary, and there was no remuneration.
Design and Intervention
Participating residents were given a diary to track their daily studying times (in hours), along with their daily assigned shift (day, night, or none). After 1 week of baseline data collection, all residents received the same digital collection of articles and resources, organized by topic. Each topic pertained to 1 of 12 different ICU subjects (eg, sepsis, delirium). Materials were saved on a network drive, allowing residents access to them on any hospital computer. Residents were asked to select 3 topics (from the original 12) that interested them the most.
Residents in the comparator group were then given a talk on the importance of goal setting and were asked to set study goals related to the topics they had selected (eg, “I intend to read 1 article each week about sepsis”). They were encouraged to make goals that were specific, actionable, and achievable. Residents in the intervention group were instead asked to use WOOP with study goals on the topics they had selected (Figure). Residents in both groups were given up to 30 minutes for intervention activities. Postintervention, residents used their daily diaries to separately track time spent studying toward their stated goals and time spent studying medical topics unrelated to their stated goals. They reported their data weekly for 3 weeks after the interventions. All participants completed a baseline survey, which collected demographic information and assessed participants on 3 domains: interest (1 item), satisfaction (3 items), and motivation (2 items). Items comprising these 3 domains were measured on 7-point, Likert-type scales with anchors from strongly disagree to strongly agree. Additionally, to control for the possible contamination of social desirability (ie, survey respondents' tendency to answer questions in a manner they think will be viewed positively by others), an index containing 4 items from the Marlowe-Crowne Social Desirability Scale21 was included. A final survey reassessed satisfaction measures using the same scales. All surveys are included as online supplemental material.
The primary outcome of this trial was total time spent studying toward residents' stated goals. Secondary outcomes included time spent studying non-goal medical material and satisfaction measures.
The study was conducted in accordance to the original protocol and was declared exempt by the Partners Human Research Committee Institutional Review Board.
Statistics
A power analysis showed that 34 residents were needed to achieve an 80% probability to detect a treatment difference of 1 SD in time spent studying. Continuous variables were compared using an unpaired t test or a Mann-Whitney U test as appropriate for the data distribution. For the primary outcome (time spent studying toward goal), the sums across all measurements (week 1, week 2, week 3) were calculated to compare group differences using a Mann-Whitney U test. Social desirability items were aggregated and correlated with the participants' report of time spent reading using Spearman's rho correlation coefficient to assess for evidence of confounding. To account for potential inflated recall of time spent studying, we recoded all data as binary for each week (ie, did, or did not, study that week). A 2 × 3 Mantel-Haenszel chi-square test was used to assess the association of that recoded binary variable between the 2 groups for each week. Effect sizes were determined using Hedges' g, with small, medium, and large effects taken to be 0.2, 0.5, and 0.8, respectively.22 All hypothesis testing was done using 2-tailed tests, and significance was determined at P < .05.
Results
Of 36 residents screened over 6 rotations, 2 were ineligible because they had already participated in the trial during a prior month. Of 34 unique residents, 100% agreed to participate, and no residents dropped out during the study. Eighteen residents were randomly assigned to the goal-setting group, and 16 to the WOOP group.
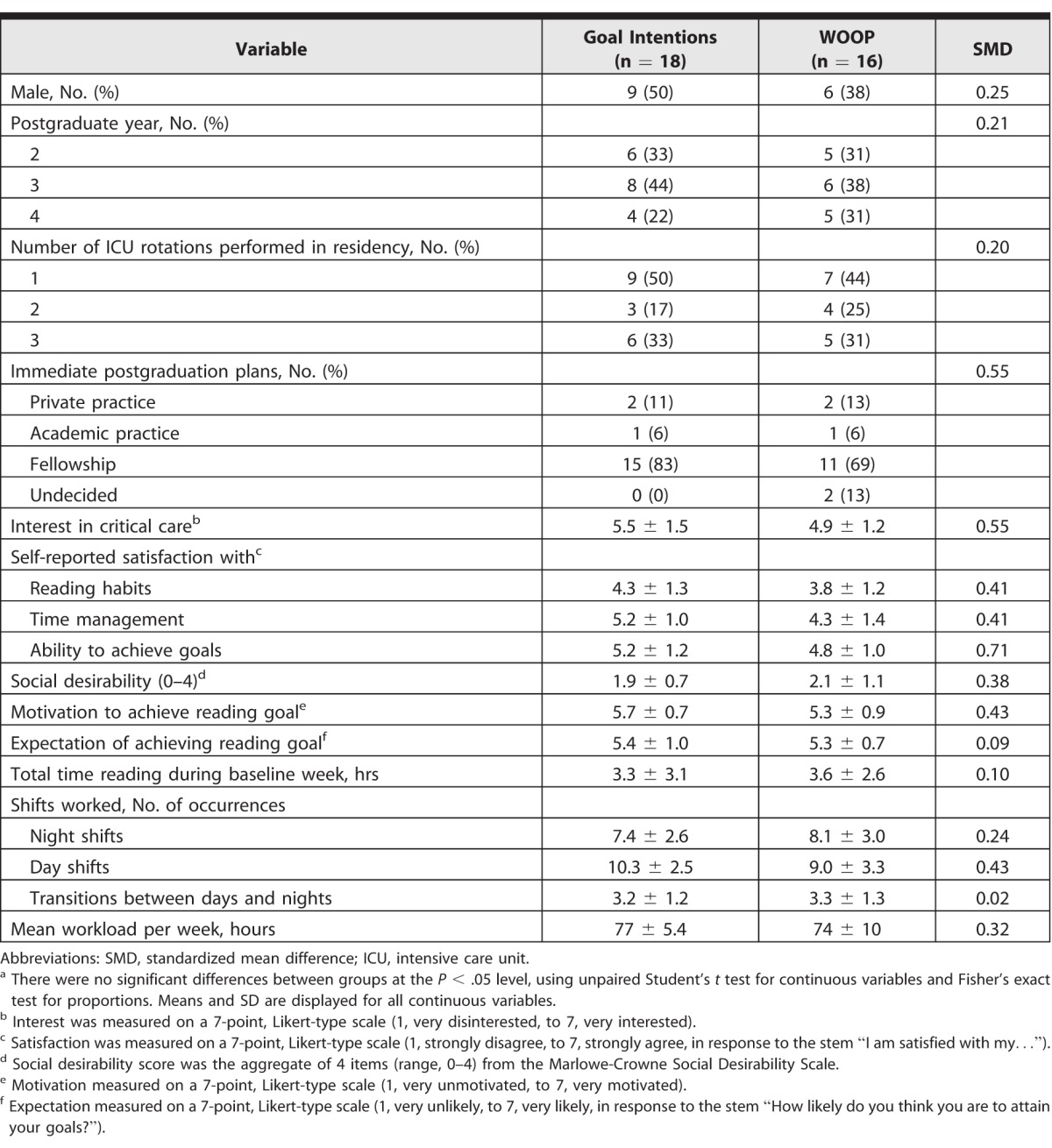
Participant Characteristics
Baseline characteristics, including interest in critical care, social desirability, motivation and expectations of achieving stated goals, and baseline readings, are shown in Table 1. There were no significant differences in clinical workload between groups during the study.
Table 1.
Baseline Characteristics of Study Participants According to Intervention Groupa
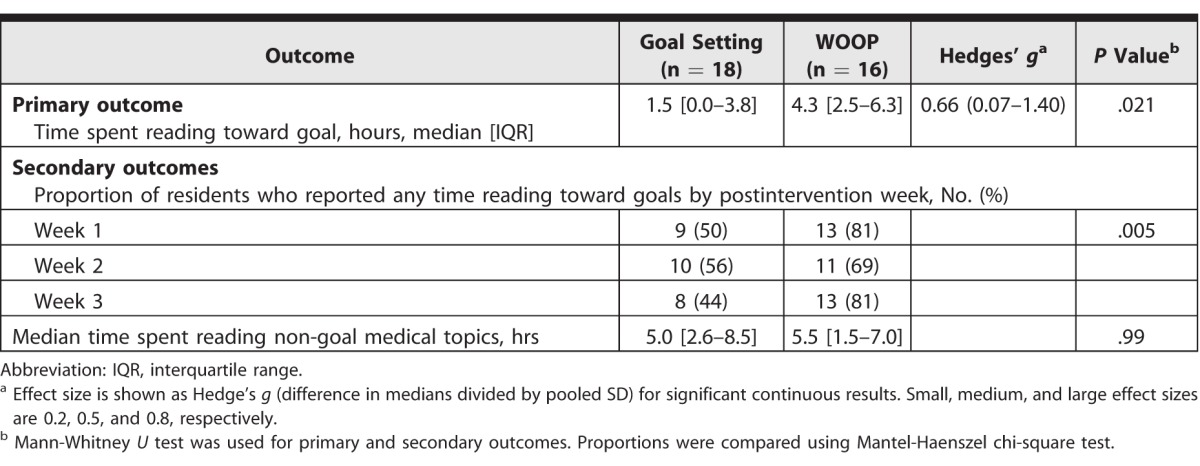
Study Habits
The WOOP group spent significantly more time studying toward their goals than the control group did (median = 4.3 hours versus 1.5 hours; P = .021; Mann-Whitney U test; Table 2). The effect size was medium to large (g = 0.66, based on medians and pooled SD). There was no evidence that social desirability influenced participants' responses. To reduce overestimation bias for time spent studying, we recoded time spent studying toward goals as a weekly binary outcome (ie, residents did, or did not, study toward their goals during the week). The percentage of residents who spent any time studying toward their goals in each postintervention week was significantly higher in the WOOP group (odds ratio [OR] = 3.32; 95% confidence interval [CI] 1.41–7.80; P = .005; Mantel-Haenszel chi-square test). The groups showed no difference in time spent studying non-goal medical material (median = 5.0 hours versus 5.5 hours; P = .99; Mann-Whitney U test; Table 2).
Table 2.
Primary and Secondary Outcomes
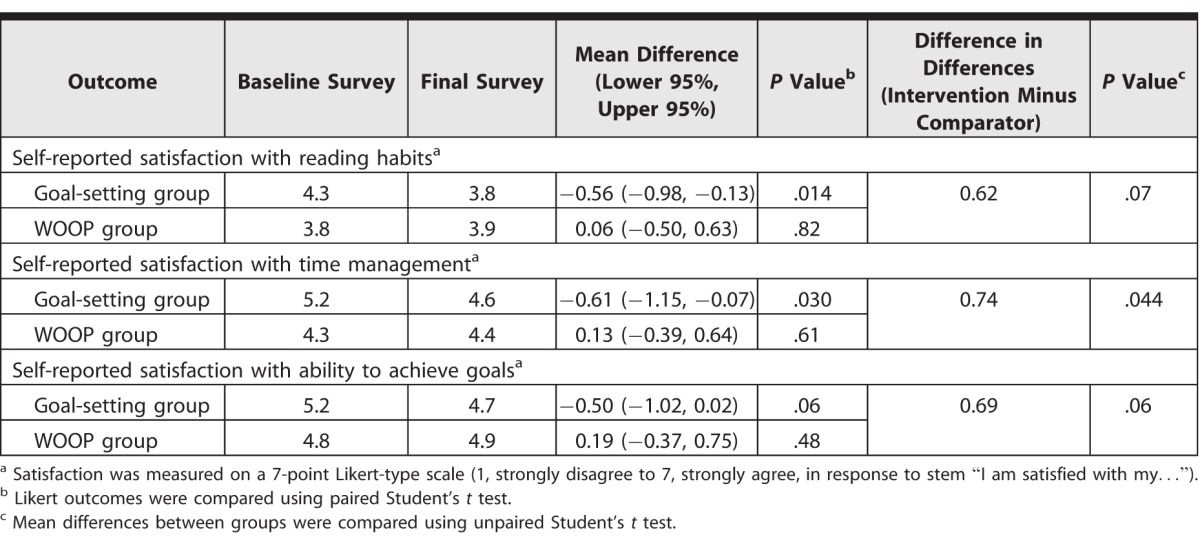
Satisfaction Measures
In the goal-setting group, satisfaction scores with reading habits and time management decreased significantly between the beginning and the end of the study period (Table 3). For residents in the WOOP group, there were no differences in satisfaction scores during the study period. Overall, there was a significant difference in the differences between groups for satisfaction with time management (−0.61 versus 0.13; P = .044; paired t test).
Table 3.
Satisfaction Measures
Discussion
In our sample of anesthesiology residents, WOOP increased goal-directed studying compared with goal setting alone. To our knowledge, this is the first study assessing the effect of WOOP in medical education. The time required for residents to receive training to use WOOP was less than 30 minutes, and the intervention did not have any additional costs. The observed medium-to-large effect (g = 0.66) on behaviors is consistent with studies that have evaluated WOOP in other domains.7,8,11,12,23–26 Importantly, increased time spent on goal-directed studying did not come at a cost of decreased time spent studying other medical-related material.
Satisfaction measures did not change for participants in the WOOP group, despite their substantial increase in goal-directed studying. It may be that progress made toward study goals prompted by WOOP went unnoticed. That would be consistent with previous work showing that WOOP acts at a nonconscious level, strategically automating intended behaviors.7,8,10,17–19,27 Alternatively, residents may overestimate their self-regulation abilities. If WOOP allows them to perform at the level they think they typically perform, it may protect them from the disappointment that would result from not meeting their expectations. Satisfaction with studying habits and time management decreased significantly over the study period for participants in the comparator group. This may have resulted from explicitly recording their study goals, which they subsequently did not attain.
Our study has several limitations. First, the primary outcomes are self-reported, and we did not externally track study times. We sought to control for that by randomization and inclusion of social desirability measures. Second, we enrolled residents from a single residency program on a specific rotation, which may limit generalizability. Third, the types of goals set in this study do not reflect all self-regulated learning goals. The goals here were relatively simple, and WOOP's effect on more complex or process-based goals (eg, seeking out more complex patients) is unknown. Additionally, prior research demonstrates that WOOP is particularly useful when goals are challenging.7,8 Residents in this study had high clinical workloads (75 h/wk), so increasing self-regulated study was likely challenging. We may not have observed the same effects in medical education settings in which increasing self-regulated learning was not as challenging. Fourth, our data did not indicate whether residents would continue to use the strategy beyond the study period. Finally, while self-reported study behaviors were increased, further research is needed to determine whether this increase improves knowledge, retention, or application. Future studies should focus on including outcomes that are not self-reported (eg, measured knowledge or behaviors), that track learners over longer periods, and that include learners from more than 1 institution or setting.
Conclusion
WOOP significantly increased goal-directed studying as compared with goal setting alone and may be a useful strategy for increasing self-regulated learning by residents.
Supplementary Material
References
- 1. Zimmerman BJ. . Self-regulated learning and academic achievement: an overview. Educ Psychol. 1990; 25 1: 3– 17. [Google Scholar]
- 2. Saddawi-Konefka D, Schumacher DJ, Baker KH, et al. Changing physician behavior with implementation intentions: closing the gap between intentions and actions. Acad Med. 2016; 91 9: 1211– 1216. [DOI] [PubMed] [Google Scholar]
- 3. Sheeran P. . Intention-behaviour relations: a conceptual and empirical review. Eur Rev Soc Psychol. 2002; 12 1: 1– 36. [Google Scholar]
- 4. Webb TL, Sheeran P. . Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychol Bull. 2006; 132 2: 249– 268. [DOI] [PubMed] [Google Scholar]
- 5. Gollwitzer PM, Sheeran P. . Implementation intentions and goal achievement: a meta-analysis of effects and processes. Adv Exp Soc Psychol. 2006; 38 1: 69– 119. [Google Scholar]
- 6. Thomas NK. . Resident burnout. JAMA. 2004; 292 23: 2880– 2889. [DOI] [PubMed] [Google Scholar]
- 7. Oettingen G. . Future thought and behaviour change. Euro Rev Soc Psychol. 2012; 23 1: 1– 63. http://www.psych.nyu.edu/oettingen/Oettingen,%20G.%20(2012).%20In%20W.%20Stroebe%20&%20M.%20Hewstone.pdf. Accessed May 26, 2017. [Google Scholar]
- 8. Oettingen G. . Rethinking Positive Thinking: Inside the New Science of Motivation. New York, NY: Penguin Random House; 2014. [Google Scholar]
- 9. Oettingen G, Wittchen M, Gollwitzer PM. . Regulating goal pursuit through mental contrasting with implementation intentions. : EA Locke, Latham GP, . New Developments in Goal Setting and Task Performance. New York, NY: Routledge; 2013: 523– 548. [Google Scholar]
- 10. Gollwitzer PM. . Implementation intentions: strong effects of simple plans. Am Psychol. 1999; 54 7: 493– 503. http://www.psych.nyu.edu/gollwitzer/99Goll_ImpInt.pdf. Accessed May 26, 2017. [Google Scholar]
- 11. Oettingen G, Kappes HB, Guttenberg KB, et al. Self-regulation of time management: mental contrasting with implementation intentions. Eur J Soc Psychol. 2015; 45 2: 218– 229. [Google Scholar]
- 12. Adriaanse MA, Oettingen G, Gollwitzer PM, et al. When planning is not enough: fighting unhealthy snacking habits by mental contrasting with implementation intentions (MCII). Eur J Soc Psychol. 2010; 40 7: 1277– 1293. [Google Scholar]
- 13. Duckworth AL, Kirby T, Gollwitzer A, et al. From fantasy to action: mental contrasting with implementation intentions (MCII) improves academic performance in children. Soc Psychol Personal Sci. 2013; 4 6: 745– 753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Stadler G, Oettingen G, Gollwitzer PM. . Intervention effects of information and self-regulation on eating fruits and vegetables over two years. Health Psychol. 2010; 29 3: 274– 283. [DOI] [PubMed] [Google Scholar]
- 15. Stadler G, Oettingen G, Gollwitzer PM. . Physical activity in women: effects of a self-regulation intervention. Am J Prev Med. 2009; 36 1: 29– 34. [DOI] [PubMed] [Google Scholar]
- 16. Christiansen S, Oettingen G, Dahme B, et al. A short goal-pursuit intervention to improve physical capacity: a randomized clinical trial in chronic back pain patients. Pain. 2010; 149 3: 444– 452. [DOI] [PubMed] [Google Scholar]
- 17. Kappes A, Singmann H, Oettingen G. . Mental contrasting instigates goal pursuit by linking obstacles of reality with instrumental behavior. J Exp Soc Psychol. 2012; 48 4: 811– 818. [Google Scholar]
- 18. Kappes A, Wendt M, Reinelt T, et al. Mental contrasting changes the meaning of reality. J Exp Soc Psychol. 2013; 49 5: 797– 810. https://psych.nyu.edu/oettingen/Kappes,%20A.,%20et%20al.%20(2013).%20 Journal%20of%20Experimental%20Social%20 Psychology.pdf. Accessed May 26, 2017. [Google Scholar]
- 19. Kappes A, Oettingen G. . The emergence of goal pursuit: mental contrasting connects future and reality. J Exp Soc Psychol. 2014; 54 2014: 25– 39. [Google Scholar]
- 20. Gollwitzer PM. . Weakness of the will: is a quick fix possible? Motiv Emot. 2014; 38 3: 305– 322. [Google Scholar]
- 21. Reynolds WM. . Development of reliable and valid short forms of the Marlowe-Crowne social desirability scale. J Clin Psychol. 1982; 38 1: 119– 125. [Google Scholar]
- 22. Cohen J. . A power primer. Psychol Bull. 1992; 112 1: 155– 159. [DOI] [PubMed] [Google Scholar]
- 23. Duckworth AL, Kirby TA, Gollwitzer A, et al. From fantasy to action: mental contrasting with implementation intentions (MCII) improves academic performance in children. Soc Psychol Personal Sci. 2013; 4 6: 745– 753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Duckworth AL, Grant H, Loew B, et al. Self regulation strategies improve self discipline in adolescents: benefits of mental contrasting and implementation intentions. Educ Psychol. 2011; 31 1: 17– 26. [Google Scholar]
- 25. Kirk D, Oettingen G, Gollwitzer PM. . Promoting integrative bargaining: mental contrasting with implementation intentions. Int J Confl Manag. 2013; 24 2: 148– 165. [Google Scholar]
- 26. Oettingen G, Marquardt MK, Gollwitzer PM. . Mental contrasting turns positive feedback on creative potential into successful performance. J Exp Soc Psychol. 2012; 48 5: 990– 996. [Google Scholar]
- 27. Bayer UC, Achtziger A, Gollwitzer PM, et al. Responding to subliminal cues: do if-then plans facilitate action preparation and initiation without conscious intent? Soc Cogn. 2009; 27 2: 183– 201. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.