Abstract
Background
Physician burnout is a problem that often is attributed to the use of the electronic health record (EHR).
Objective
To estimate the prevalence of burnout and work-life balance satisfaction in primary care residents and teaching physicians, and to examine the relationship between these outcomes, EHR use, and other practice and individual factors.
Methods
Residents and faculty in 19 primary care programs were anonymously surveyed about burnout, work-life balance satisfaction, and EHR use. Additional items included practice size, specialty, EHR characteristics, and demographics. A logistic regression model identified independent factors associated with burnout and work-life balance satisfaction.
Results
In total, 585 of 866 surveys (68%) were completed, and 216 (37%) respondents indicated 1 or more symptoms of burnout, with 162 (75%) attributing burnout to the EHR. A total of 310 of 585 (53%) reported dissatisfaction with work-life balance, and 497 (85%) indicated that use of the EHR affected their work-life balance. Respondents who spent more than 6 hours weekly after hours in EHR work were 2.9 times (95% confidence interval [CI] 1.9–4.4) more likely to report burnout and 3.9 times (95% CI 1.9–8.2) more likely to attribute burnout to the EHR. They were 0.33 times (95% CI 0.22–0.49) as likely to report work-life balance satisfaction, and 3.7 times (95% CI 2.1–6.7) more likely to attribute their work-life balance satisfaction to the EHR.
Conclusions
More after-hours time spent on the EHR was associated with burnout and less work-life satisfaction in primary care residents and faculty.
What was known and gap
Use of the electronic health record (EHR) has been associated with a negative work-life balance and physician burnout.
What is new
A study that assessed burnout and work-life balance in primary care residents and faculty as well as the impact of EHR use on both.
Limitations
Survey research, using a tool without validity evidence, and a single-item measure of burnout.
Bottom line
A sizable proportion of primary care residents and faculty reported burnout and dissatisfaction with work-life balance. More after-hours EHR use was associated with burnout and lower work-life satisfaction.
Introduction
Growing awareness of burnout among physicians and its negative effect on patient outcomes1–3 has resulted in a call to expand the Triple Aim to the Quadruple Aim, which includes the physician's experience, along with patient experience, quality, and cost of care.4 Symptoms of burnout can begin early in a physician's career, with published burnout rates among primary care residents varying from 40% to 78%.5–8 Few studies have assessed burnout rates among faculty in US residency programs.5
One potential contributor to burnout is the rapid expansion of the electronic health record (EHR),9,10 as physicians who use the highest number of both EHR features and functions report more time pressure associated with significantly more burnout, dissatisfaction, and intent to leave medicine.11 The purpose of this study was to estimate the prevalence of burnout among primary care residents and faculty, estimate work-life balance satisfaction for both groups, and examine the relationship between these 2 outcomes and EHR and other practice and individual factors.
Methods
Participants for this study were drawn from primary care residency programs in the I3 Population Health Collaborative. The I3 Collaborative comprises 24 primary care residency practices (20 family medicine, 2 internal medicine, and 2 pediatrics practices) across Virginia, North Carolina, South Carolina, and Florida. It seeks to achieve practice transformation around the Triple Aim.12
Designated faculty at each program completed a practice characteristics survey, and distributed physician surveys to faculty and residents in January and February 2015. Practice characteristics surveyed included the number of physicians, the EHR used in the practice, the amount of time the EHR had been in place, and the number of different EHRs over the previous 10 years. The physician survey (provided as online supplemental material) included 4 outcome items: a single item, 5-point burnout scale with some prior evidence of validity13; an added item (presented only to respondents who indicated burnout) that asked respondents to categorize the extent to which they believed the EHR contributed to their burnout; a question about respondents' satisfaction with their ability to maintain a healthy work-life balance; and an item on the effect of the EHR on work-life balance. Respondents were asked to estimate the number of hours they spend in a typical week performing EHR-related tasks outside of normal work hours. We also collected demographic data for respondents. The survey instrument was reviewed and pilot tested by 20 faculty members of the I3 Collaborative. No formal validity testing was performed.
The study protocol was approved by the Carolinas Healthcare System Institutional Review Board.
For analysis, all 4 outcomes were tabulated and dichotomized. We considered burnout to be positive if the respondent selected choice 3, 4, or 5 (Box). We considered satisfaction with work-life balance to be positive if the response was satisfied or very satisfied. The perceived effect of the EHR on burnout or work-life balance was coded positive if some or a lot was selected. Scaled independent variables were similarly dichotomized. Continuous variables were found to be not normally distributed (using the Shapiro-Wilk test). We summarized them using medians, and we used the Kruskal-Wallis test to assess the significance of differences. We estimated the maximum likelihood odds ratio (OR) for the outcome variable, given dichotomous categories or median splits. Bivariate relationships with P ≤ .05 were entered into a multivariate logistic regression model. All tests were performed using Stata version 10.1 (StataCorp LLC, College Station, TX).
Box Single-Item Burnout Scale13
Burnout is generally understood to involve emotional exhaustion, depersonalization, and low sense of personal accomplishment.
Considering your experience of burnout, select the statement below that best describes your situation at work.
I enjoy my work. I have no symptoms of burnout.
Occasionally I am under stress, and I don't always have as much energy as I once did, but I don't feel burned out.
I am definitely burning out and have 1 or more symptoms of burnout, such as physical and emotional exhaustion.
The symptoms of burnout that I'm experiencing won't go away. I think about frustration at work a lot.
I feel completely burned out and often wonder if I can go on. I am at the point where I may need some changes or may need to seek some sort of help.
Results
Of 22 practices initially surveyed, 3 used a unique EHR; these practices collectively represented less than 5% of responses, and were insufficient to draw valid inferences. We excluded them from further analysis. Of 866 surveys disseminated to the remaining 19 locations, 585 (68%) were returned. Respondent and program characteristics are described in Table 1.
Table 1.
Demographic Characteristics of Residency Programs and Respondents

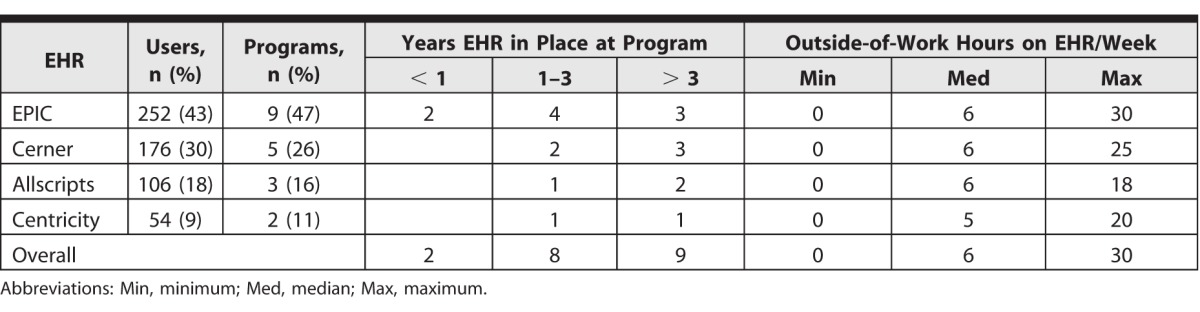
The 4 EHRs used by respondents are enumerated in Table 2, along with their years of use, and median weekly hours that providers devoted to EHR-related tasks outside of normal clinic hours. We found no statistically significant differences in self-reported outside-of-work hours among different EHRs (P = .69). We did find an impact of the time the EHR had been in use on after-hours time spent on the EHR. Users in practices where the current EHR had been in place 1 to 3 years spent a median of 7 outside-of-work hours, while those with the current EHR in place less than 1 year or more than 3 years spent a median of 6 and 5 outside-of-work hours, respectively (P = .001).
Table 2.
Electronic Health Records (EHRs) Used in Surveyed Programs by Years in Place and Weekly Outside-of-Work Hours Spent by Users
EHR and Work-Life Balance
Overall, 53% of respondents (310 of 585) indicated that they were dissatisfied or very dissatisfied with their work-life balance. A total of 85% of respondents (497 of 585) indicated that the EHR affected their work-life balance.
Table 3A shows the association between the factors we surveyed and respondents' satisfaction with work-life balance, as well as the impact of EHR use. Only out-of-work hours spent with the EHR was significantly related to satisfaction with work-life balance and EHR effect on work-life balance. Compared to respondents who spent the median 6 hours or fewer per week on EHR work outside of normal clinic hours, respondents who spent more time were one-third as likely to report satisfaction with work-life balance (OR = 0.33, 95% confidence interval [CI] 0.22–0.49) and 3.7 times more likely to indicate that their EHR affected their work-life balance (OR = 3.7, 95% CI 2.1–6.7).
Table 3A.
Factors Associated With Work-Life Balance

EHR and Burnout
A total of 37% of respondents (216 of 585) reported burnout. Of these, 75% (162 of 216) attributed their experience of burnout to their EHR to be some or a lot. Table 3B shows the associations between the survey factors, respondents' self-reported burnout, and reported impact of the EHR.
Table 3B.
Factors Associated With Burnout
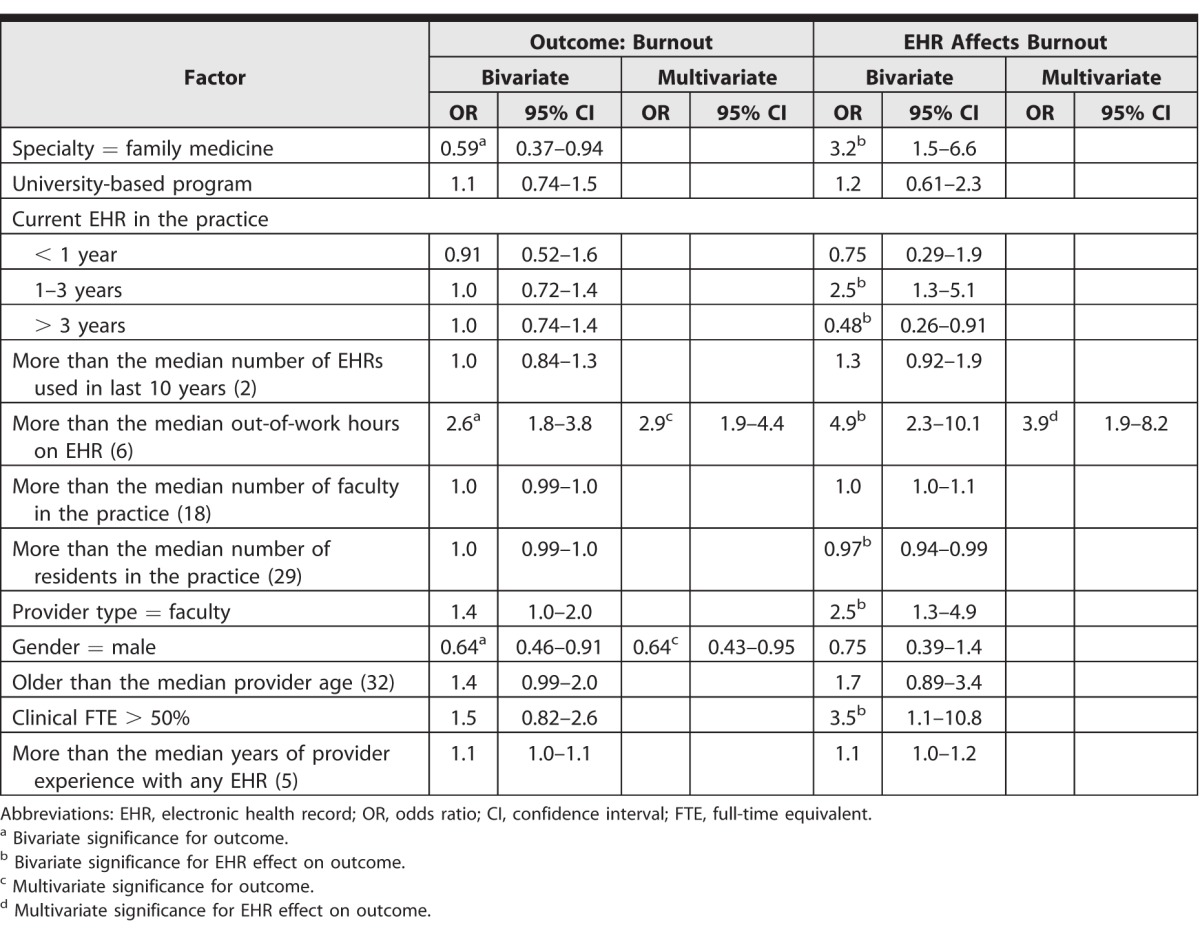
Like work-life balance, the out-of-work hours spent with the EHR was significantly associated with reported burnout, and reports on the effect of the EHR on burnout. Physicians who spent more than the median 6 hours per week on EHR work outside of normal clinic hours were nearly 3 times more likely to report burnout than those who spent 6 hours or less (OR = 2.9, 95% CI 1.9–4.4), and almost 4 times more likely to attribute it to the EHR (OR = 3.9, 95% CI 1.9–8.2). Male respondents were less likely than female respondents to report burnout (OR = 0.64, 95% CI 0.43–0.95). Specialty, sex, faculty versus resident, or prior EHR experience were not independently associated with reporting that the EHR affected burnout.
Discussion
Overall, 53% of residents and teaching physicians in this study reported dissatisfaction with their work-life balance, and 37% reported burnout, with women more likely to report burnout. Among those who reported burnout, 75% attributed some or a lot of it to their use of the EHR. Spending more than the median 6 hours a week on after-hours EHR work was strongly associated with less satisfaction with work-life balance, a greater likelihood of burnout, and the perception that the EHR affects both work-life balance satisfaction and burnout. There were no significant differences in after-hours work among the 4 EHRs in this sample.
The reported burnout and dissatisfaction with work-life balance among the study population are consistent with published literature for primary care residents across the United States and provides information about teaching physicians in residency programs. It is not surprising that increased after-hours EHR work contributes to burnout and decreased work-life balance. The number of reported after-work hours spent on EHR use in this study (0–30 hours per week) reflects significant room for improvement independent of the use of a specific EHR vendor.
EHR proficiency training has been associated with improved job satisfaction and work-life balance.14 While increasing EHR proficiency may help, there are many potential reasons for physicians to spend after-hours on the EHR, including time management issues, inadequate clinic staffing, patient complexity, lack of scribes, challenges in mastering automatic dictation systems, cosigning resident notes, messaging, and preparing records for the next day. All of these issues and their impact on burnout and work-life balance are potential areas for future research.
There are several limitations to this study. Our survey instrument lacks established validity evidence, and respondents may not have interpreted questions as we intended. The survey item regarding the effect on work-life balance satisfaction did not allow us to distinguish between the contribution of the EHR to satisfaction or dissatisfaction. Also, EHR systems cannot be compared across institutions. Finally, other factors contribute to burnout such as personality traits, lack of wellness strategies, and environmental factors, and we did not control for these potential confounders.
Conclusion
Our findings offer evidence that EHR work done after hours is negatively associated with self-reported satisfaction with work-life balance, and that physicians in teaching settings substantially attribute work-life balance satisfaction to their after-hours use of EHR. Our data also demonstrate a significant relationship between after-hours EHR work and self-reported burnout that is attributed to the use of the EHR. Efforts to reduce after-hours time spent on EHR-related activities may reduce burnout and improve work-life balance for primary care residents and faculty.
Supplementary Material
References
- 1. Wallace JE, Lemaire JB, Ghali WA. . Physician wellness: a missing quality indicator. Lancet. 2009; 374 9702: 1714– 1721. [DOI] [PubMed] [Google Scholar]
- 2. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015; 90 12: 1600– 1613. [DOI] [PubMed] [Google Scholar]
- 3. Keeton K, Fenner DE, Johnson TR, et al. Predictors of career satisfaction, work-life balance, and burnout. Obstet Gynecol. 2007; 109 4: 949– 955. [DOI] [PubMed] [Google Scholar]
- 4. Bodenheimer T, Sinsky C. . From triple aim to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014; 12 6: 573– 576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dyrbye LN, West CP, Satele D, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014; 89 3: 443– 451. [DOI] [PubMed] [Google Scholar]
- 6. Thomas NK. . Resident burnout. JAMA. 2004; 292 23: 2880– 2889. [DOI] [PubMed] [Google Scholar]
- 7. Lebensohn P, Dodds S, Benn R, et al. Resident wellness behaviors. Fam Med. 2013: 45(8);541–549. [PubMed]
- 8. Dyrbye L, Shanafelt T. . A narrative review on burnout experienced by medical students and residents. Med Educ. 2016; 50 1: 132– 149. [DOI] [PubMed] [Google Scholar]
- 9. DesRoches CM, Campbell EG, Rao SR, et al. Electronic health records in ambulatory care—a national survey of physicians. N Engl J Med. 2008; 359 1: 50– 60. [DOI] [PubMed] [Google Scholar]
- 10. Hsiao CJ, Hing E. . Use and characteristics of electronic health record systems among office-based physician practices: United States, 2001–2013. NCHS Data Brief. No. 143. January 2014. https://www.cdc.gov/nchs/data/databriefs/db143.pdf. Accessed May 11, 2017. [PubMed]
- 11. Babbott S, Manwell LB, Brown R, et al. Electronic medical records and physician stress in primary care: results from the MEMO Study. J Am Med Inform Assoc. 2014; 21 e1: e100– e106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Donahue KE, Reid A, Lefebvre A, et al. Tackling the triple aim in primary care residencies: the I3 POP Collaborative. Fam Med. 2015; 47 2: 91– 97. [PubMed] [Google Scholar]
- 13. Rohland BM, Kruse GR, Rohrer JE. . Validation of a single-item measure of burnout against the Maslach Burnout Inventory among physicians. Stress Health. 2004; 20 2: 75– 79. [Google Scholar]
- 14. Dastagir MT, Chin HL, McNamara M, et al. Advanced proficiency EHR training: effect on physicians' EHR efficiency, EHR satisfaction and job satisfaction. AMIA Annu Symp Proc. 2012; 2012: 136– 143. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


