Abstract
Background
Activity tracking devices can reinforce physical fitness and may be beneficial to resident physicians. To date, their use has not been evaluated.
Objective
To determine if use of an activity tracking device increases residents' activity, measured as steps per day.
Methods
A prospective, crossover study involved residents at 1 academic hospital system. Participants were weighed and completed a baseline survey. All participants were asked to wear an activity tracking device for 8 weeks. Residents were blinded to feedback from the device on activity level during the first 4 weeks. During the second 4-week period, participants were given access to data on activity level and were invited to join a voluntary activity tracking group.
Results
Of 104 residents invited to participate, 86 enrolled. The majority of participants were female and did not have experience using activity trackers. Almost half (49%, 51 of 104) had a body mass index greater than 25 kg/m2. The median steps per day of all participants during the blinded period was 7260. This increased to 8266 steps per day during the unblinded period. Surgical residents recorded significantly more steps than nonsurgical specialties (7938 versus 6724, P = .018). The 26 residents who joined the voluntary activity tracking group registered higher median steps per day, and wore their activity tracker more consistently.
Conclusions
Providing residents with activity trackers, increasing feedback, and providing comparisons to peers may enhance residents' physical activity levels.
Introduction
Physical activity improves overall health, prevents chronic disease, and reduces mental illness.1,2 Yet many physicians do not adequately incorporate exercise into their daily lives.3,4 Some studies have associated poor physician health with suboptimal care.5,6 Promoting physical activity for busy residents could foster positive behaviors and better equip them to counsel patients.7–9
We assessed whether use of a physical activity tracker increased physical activity measured via daily step counts for residents.
Methods
We conducted a prospective study at TriHealth Inc, an academic hospital system in Cincinnati, Ohio, between April and June 2015. Residents in obstetrics-gynecology (OG), surgery (S), family medicine (FM), and internal medicine (IM) were notified of the study via e-mail and in-person. Exclusion criteria included a disability affecting exercise. Participants provided informed consent.
Residents in the study were given a Fitbit Flex (Fitbit Inc, San Francisco, CA) and were instructed to wear it for 8 weeks. This device is an electronic activity monitor that measures step counts, and interfaces with a computer or mobile app to provide feedback. These devices are an accurate, reliable way to measure step counts in adults.10
An account was set up for each participant. The passwords were not revealed to participants. Residents were measured for height and weight at baseline, and completed a demographics questionnaire. Daily goals were set to 500 steps. For the first 4 weeks, participants were blinded to data from the activity tracker.
After 4 weeks, participants were given their password. Goals were reset to 10 000 steps per day in concordance with American Heart Association recommendations.11 Residents also were invited to join a resident-only activity tracking group, allowing them to connect and “compete.” The primary outcome measure was change in average steps per day from the blinded versus the unblinded period. Following an exit interview, the residents kept their Fitbit.
This study was approved by the Institutional Review Board.
Statistical analysis was conducted using IBM SPSS Statistics version 19 (IBM Corp, Armonk, NY). Descriptive summary statistics were calculated for all continuous and categorical data. Analyses of residents' steps were performed to compare mean steps per day on days when the Fitbit was worn, defined as 500 or more steps recorded per day. Days with less than 500 steps were considered noncompliant and excluded from the analysis. Median steps per day were compared between the blinded and unblinded period. Differences in compliance were measured using Wilcoxon signed rank test, and McNemar's test was used to compare the number of residents who achieved 10 000 steps per day between blinded and unblinded periods. The Mann-Whitney U test was used to test the difference in number of steps based on demographics. The significance level (α) for 2-group comparison was .05, and no multiple comparisons were performed.
Results
Of 104 eligible residents, 86 participated, including 32 obstetrics and gynecology, 20 surgery, 12 family medicine, and 22 internal medicine residents (Table 1). Two residents withdrew, 7 lost the Fitbit, and 3 did not wear it after 2 weeks, leaving a total of 74 residents who completed the study.
Table 1.
Baseline Demographicsa
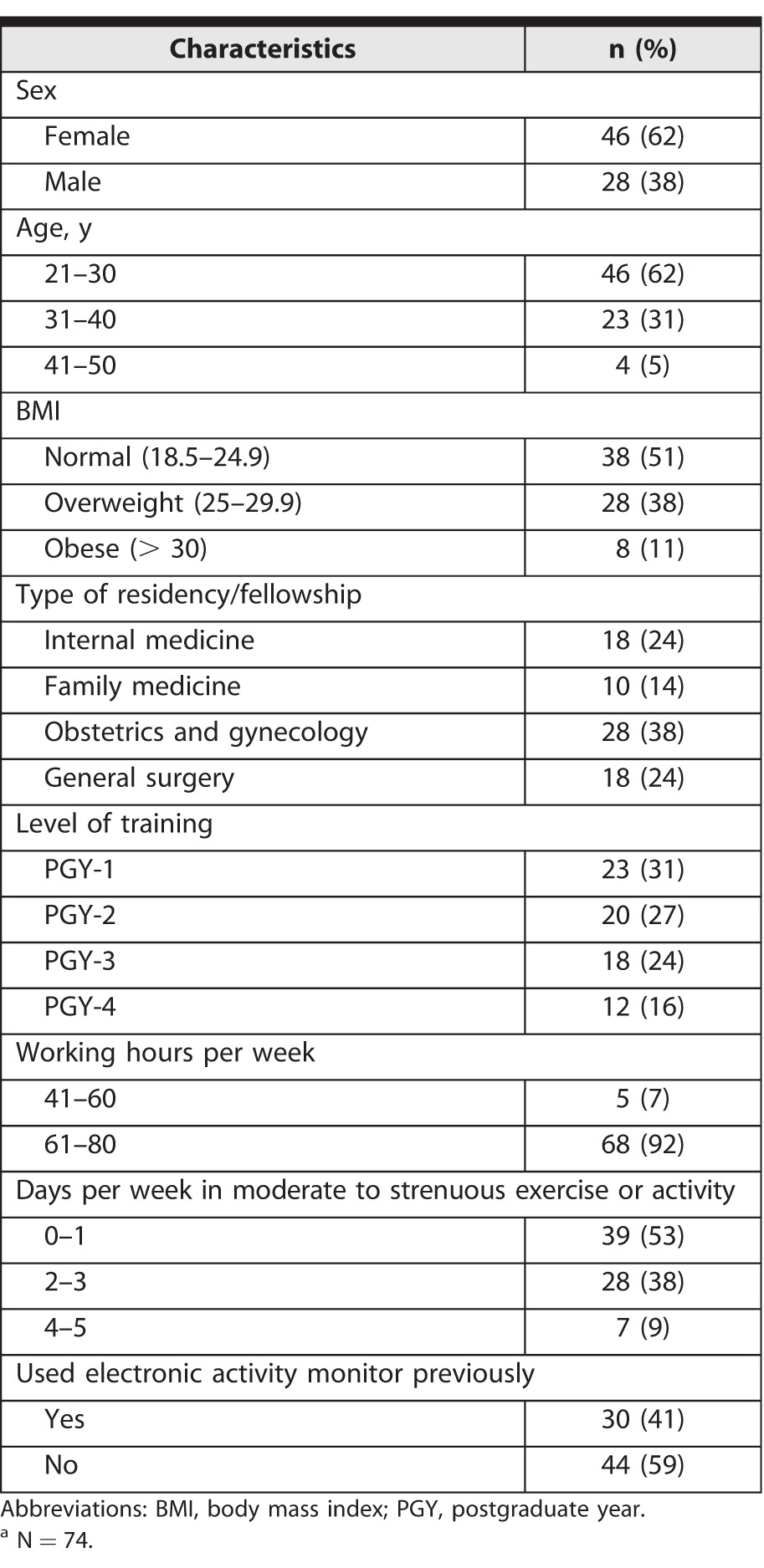
Participants' demographics are shown in Table 1. Mean body mass index (BMI) was 24.7 kg/m2, and 49% (51 of 104) had a BMI greater than 25 kg/m2; 53% (39 of 74) reported participating in “moderate to strenuous” exercise 0 to 1 day per week, and 59% (44 of 74) reported no prior experience using an activity tracker.
The median steps per day of participants during the blinded period was 7260, which increased to 8266 during the unblinded period (P = .001; Table 2). Nine residents (12%) achieved an average of 10 000 steps per day when blinded, compared to 17 residents (23%) during the period tracking data were provided (P = .040).
Table 2.
Steps per Day for Blinded and Unblinded Periods
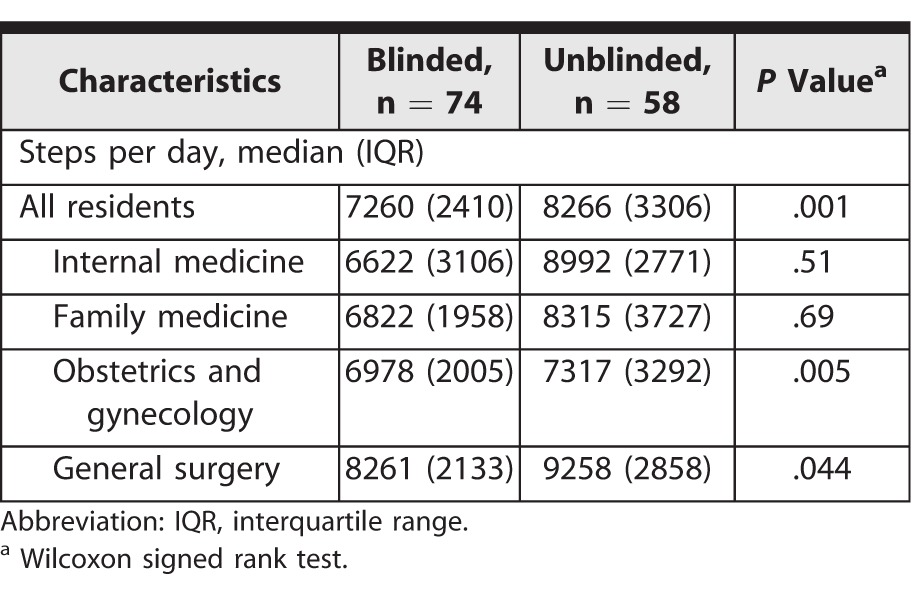
The median number of steps recorded by surgical (obstetrics and gynecology and surgery) residents was significantly higher than that recorded by nonsurgical (internal medicine and family medicine) specialties (7938 versus 6724; P = .018; Table 2).
The 26 residents (35%) who joined the voluntary activity tracking activity group during the second 4-week period had higher median steps per day, compared to those who did not join (7938 versus 7446, P = .042). Residents who volunteered for the activity tracking group were similar in their wearing of the activity tracker during the blinded and the unblinded period (90% and 91%, respectively); residents who did not volunteer for the group showed lower activity tracker use overall, and statistically lower use during the unblinded period (73% versus 51%, P < .001).
Discussion
This study shows that wearing an activity tracker with real-time feedback was associated with increased steps per day for some residents. Participants who volunteered for the activity tracking group were more physically active and tended to wear their activity tracker more.
Previous reports have evaluated resident behavior using activity monitors. One study showed 90% of emergency medicine residents did not reach 10 000 steps during a shift; another found that the addition of team competition to help encourage residents to monitor use increased activity.12,13 Our results confirm the effect of peer comparisons.
While many physicians do not incorporate exercise into their lives or meet basic physical activity goals,3,4,14 there is evidence that physicians who are more active and aware of their physical activity status are 3 times more likely to encourage exercise in patients.9,15 In our study, few residents (23%, 17 of 74) achieved 10 000 steps per day. Nevertheless, in 8 weeks our intervention increased the median steps per day for participants from 7260 to 8266, advancing them from a low active category to somewhat active, which may be clinically relevant.16 While previous studies suggest that taking 10 000 steps per day helps lower blood pressure, increase weight loss, and maintain a healthy lifestyle, higher daily step counts may also be associated with lowering long-term mortality.17,18 One study showed that an increase of just 2000 steps per day was associated with a 10% reduction in annual cardiovascular disease event rate.19
One weakness of activity monitors is potentially reduced long-term effectiveness.20 While some short-term studies support success, more recent data question the longer-term effects on physical activity.20,21 We did see a decline in compliance in the second 4 weeks (unblinded) versus the first 4 weeks (blinded) of the study. Residents who joined the voluntary activity group were more active and tended to wear their activity tracker more, potentially because they were more engaged and motivated.
There are limitations to this study. It involved a single institution, and the results may not be generalizable. A Hawthorne effect must be considered, since residents were aware of the activity tracker and the fact that they were being studied.
Further research should assess the effectiveness of incentivizing resident participation in activity groups, or working with them on setting and accomplishing a specific step goal.
Conclusion
An 8-week study of activity tracker use in residents from multiple specialties showed that access to feedback features increased daily steps. However, the number of daily steps remained inadequate for most residents, and only a minority of participants joined an activity group to enhance use.
References
- 1. Warburton DE, Nicol CW, Bredin SS. . Health benefits of physical activity: the evidence. CMAJ. 2006; 174 6: 801– 809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Toker S, Biron M. . Job burnout and depression: unraveling their temporal relationship and considering the role of physical activity. J Appl Psychol. 2012; 97 3: 699– 710. [DOI] [PubMed] [Google Scholar]
- 3. Bazargan M, Makar M, Bazargan-Hejazi S, et al. . Preventive, lifestyle, and personal health behaviors among physicians. Acad Psychiatry. 2009; 33 4: 289– 295. [DOI] [PubMed] [Google Scholar]
- 4. Hull SK, DiLalla LF, Dorsey JK. . Prevalence of health-related behaviors among physicians and medical trainees. Acad Psychiatry. 2008; 32 1: 31– 38. [DOI] [PubMed] [Google Scholar]
- 5. West CP, Tan AD, Habermann TM, et al. . Association of resident fatigue and distress with perceived medical errors. JAMA. 2009; 302 12: 1294– 1300. [DOI] [PubMed] [Google Scholar]
- 6. Fahrenkopf AM, Sectish TC, Barger LK, et al. . Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. 2008; 336 7642: 488– 491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Abramson S, Stein J, Schaufele M, et al. . Personal exercise habits and counseling practices of primary care physicians: a national survey. Clin J Sport Med. 2000; 10 1: 40– 48. [DOI] [PubMed] [Google Scholar]
- 8. Lobelo F, Duperly J, Frank E. . Physical activity habits of doctors and medical students influence their counselling practices. Br J Sports Med. 2009; 43 2: 89– 92. [DOI] [PubMed] [Google Scholar]
- 9. McKenna J, Naylor PJ, McDowell N. . Barriers to physical activity promotion by general practitioners and practice nurses. Br J Sports Med. 1998; 32 3: 242– 247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Takacs J, Pollock CL, Guenther JR, et al. . Validation of the Fitbit One activity monitor device during treadmill walking. J Sci Med Sport. 2014; 17 5: 496– 500. [DOI] [PubMed] [Google Scholar]
- 11. American Heart Association. Easy exercise ideas for a busy schedule. 2015. https://www.goredforwomen.org/live-healthy/easy-exercise-ideas-for-a-busy-schedule. Accessed May 15, 2017.
- 12. Josephson EB, Caputo ND, Pedraza S, et al. . A sedentary job? Measuring the physical activity of emergency medicine residents. J Emerg Med. 2013; 44 1: 204– 208. [DOI] [PubMed] [Google Scholar]
- 13. Thorndike AN, Mills S, Sonnenberg L, et al. . Activity monitor intervention to promote physical activity of physicians-in-training: randomized controlled trial. PLoS One. 2014; 9 6: e100251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wallace JE, Lemaire J. . Physician well being and quality of patient care: an exploratory study of the missing link. Psychol Health Med. 2009; 14 5: 545– 552. [DOI] [PubMed] [Google Scholar]
- 15. Rogers LQ, Gutin B, Humphries MC, et al. . A physician fitness program: enhancing the physician as an “exercise” role model for patients. Teach Learn Med. 2005; 17 1: 27– 35. [DOI] [PubMed] [Google Scholar]
- 16. Tudor-Locke C, Bassett DR. . How many steps/day are enough? Preliminary pedometer indices for public health. Sports Med. 2004; 34 1: 1– 8. [DOI] [PubMed] [Google Scholar]
- 17. Schneider PL, Bassett DR, Thompson DL, et al. . Effects of a 10,000 steps per day goal in overweight adults. Am J Health Promot. 2006; 21 2: 85– 89. [DOI] [PubMed] [Google Scholar]
- 18. Le Masurier GC, Sidman CL, Corbin CB. . Accumulating 10,000 steps: does this meet current physical activity guidelines? Res Q Exerc Sport. 2003; 74 4: 389– 394. [DOI] [PubMed] [Google Scholar]
- 19. Yates T, Haffner SM, Schulte PJ, et al. . Association between change in daily ambulatory activity and cardiovascular events in people with impaired glucose tolerance (NAVIGATOR trial): a cohort analysis. Lancet. 2014; 383 9922: 1059– 1066. [DOI] [PubMed] [Google Scholar]
- 20. Piwek L, Ellis DA, Andrews S, et al. . The rise of consumer health wearables: promises and barriers. PLoS Med. 2016; 13 2: e1001953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jakicic JM, Davis KK, Rogers RJ, et al. . Effect of wearable technology combined with a lifestyle intervention on long-term weight loss: the IDEA randomized clinical trial. JAMA. 2016; 316 11: 1161– 1171. [DOI] [PMC free article] [PubMed] [Google Scholar]


