Abstract
Purpose
Characterize tumor burden dynamics during PD-1 inhibitor therapy and investigate the association with overall survival (OS) in advanced melanoma.
Experimental Design
The study included 107 advanced melanoma patients treated with pembrolizumab. Tumor burden dynamics were assessed on serial CT scans using irRECIST and were studied for the association with OS.
Results
Among 107 patients, 96 patients had measurable tumor burden and 11 had non-target lesions alone at baseline. In the 96 patients, maximal tumor shrinkage ranged from -100% to 567% (median:-18.5%). Overall response rate was 44% (42/96; 5 irCR, 37 irPR). Tumor burden remained <20% increase from baseline throughout therapy in 57 patients (55%). Using a 3-month landmark analysis, patients with <20% tumor burden increase from baseline had longer OS than pts with ≥20% increase (12-month OS rate: 82 vs. 53%). In extended Cox models, patients with <20% tumor burden increase during therapy had significantly reduced hazards of death (HR=0.19, 95%CI:0.08–0.43, p<0.0001 univariate; HR=0.18, 95%CI:0.08-0.41, p<0.0001, multivariable). Four patients (4%) experienced pseudoprogression; 3 patients had target lesion increase with subsequent response, which was noted after confirmed irPD. One patient without measurable disease progressed with new lesion that subsequently regressed.
Conclusions
Tumor burden increase of <20% from the baseline during pembrolizumab therapy was associated with longer OS, proposing a practical marker for treatment decision guides that needs to be prospectively validated. Pseudoprogressors may experience response after confirmed irPD, indicating a limitation of the current strategy for immune-related response evaluations. Evaluations of patients without measurable disease may require further attention.
Keywords: PD-1 inhibitor, immune-checkpoint inhibitors, melanoma, computed tomography, tumor response
Introduction
Cancer immunotherapy using immune checkpoint inhibitors has emerged as an effective cancer treatment option for advanced malignancies, as represented by the recent FDA approvals of programmed death (PD)-1/PD-L1 inhibitors, nivolumab, pembrolizumab, and atezolizumab for different types of advanced malignancies. Anti-cancer activity of these agents is achieved by the blockade of immune inhibition by tumors, which leads to the stimulation of host immunity against tumors. Due to this unique mechanism of action, immune-targeted treatment is associated with distinct patterns of immune-related response, including initial increase of tumor burden and/or appearance of new lesions followed by subsequent decrease of tumor burden, giving rise to a phenomenon often referred to as “pseudoprogression”.(1-4) The phenomenon poses a challenge to clinicians and investigators because patients treated with immune checkpoint inhibition who exhibit pseudoprogression may be misclassified as having progressive disease (PD) by the conventional RECIST guidelines.(1, 5-8)
To account for the limitations of RECIST in evaluating therapeutic efficacy during immunotherapy, immune-related response criteria (irRC) have been proposed in 2009, based on the data of 487 melanoma patients treated with the CTLA-4 antibody, ipilimumab.(4) The major strategy of irRC to capture immune-related response patterns is to 1) include measurements of new lesions to the total tumor burden rather than immediately declaring PD at the first appearance of a new lesion, and 2) require confirmation of PD on two consecutive scans at least 4 weeks apart.(2-4) Only a few published clinical trials of PD-1 inhibitors have reported the results of immune-related response assessments and the incidence of pseudoprogression in comparison with RECIST assessments.(1, 9) Moreover, detailed tumor burden dynamics on longitudinal CT scans during PD-1 inhibitor therapy have not been fully described in clinical trial reports. Given the rapidly increasing availability of these agents in the clinical setting of oncology practice in different solid tumors, it is necessary to systematically characterize tumor burden dynamics during PD-1 inhibitor therapy, identify different patterns, and investigate their association with survival. The present study focuses on advanced melanoma as the longest studied tumor type and a paradigm for immunotherapy, which serves as an initial step to describe immune-related response phenomena across different types of tumors.
Materials and Methods
Patients
The study population consisted of 107 advanced melanoma patients (63 males, 44 females, median age: 63 years, age range: 28-89) who were treated with single-agent pembrolizumab between March 2012 and April 2016 and had baseline CT scan prior to therapy and at least one follow-up CT during therapy available for review, identified by a retrospective review of the cancer immunotherapy database at our institution. Twenty-four patients were treated with pembrolizumab on clinical trials, 4 patients were treated in the expanded access program, and 79 patients received pembrolizumab as standard of care after the FDA approval of the agent. Pembrolizumab was given at a dose of 2 mg/kg or 10 mg/kg every 3 weeks in the trials, per trial protocols. The regimen for standard of care was 2 mg/kg every 3 weeks. The medical records and imaging studies of these patients were retrospectively reviewed with the approval of the Dana Farber/Harvard Cancer Center institutional review board with the waiver for informed consent and was in compliance with Health Insurance Portability and Accountability Act.
Tumor measurements on the longitudinal scans
Baseline and all follow-up CT scans during therapy were retrospectively reviewed by a board-certified radiologist (M.N., with 12 years of experience in oncologic imaging) to quantify tumor burden changes using immune-related RECIST (irRECIST), based on the previously published studies.(3, 10-12) The use of unidimensional, RECIST-defined measurements in irRECIST was based on the higher reproducibility of the unidimensional approach compared to bidimensional measurements used in WHO and irRC, and the alignment with the RECIST-based assessments used in most trials in the past decade to define their endpoints.(11, 13-17)
In brief, target lesions (≥10 mm in the longest diameter for non-nodal lesions and ≥15 mm in short axis for nodal lesions) were selected on the baseline scans, allowing up to 2 lesions per organ and up to 5 lesions in total as in RECIST1.1.(5-7) Measurements of target lesions were performed on baseline and all follow-up CT scans throughout the duration of therapy. If new lesions were noted on the follow-up scans, the measurements of the new lesions were included in the sum of the measurements, as this is an important feature of immune-related response evaluations.(2, 4, 10, 11) Up to 2 per organ and 5 in total new lesions were allowed at each time point.(4, 10) New lesions had to be ≥10 mm in the longest diameter for non-nodal lesions and ≥15 mm in short axis for nodes to be included in the measurements.(10) Other imaging studies such as brain MRI and PET/CT scans were also reviewed to identify new lesions and assess non-target lesions, as previously described.(18)
The follow-up intervals of CT scans were predefined per trial protocol in patients treated on the respective trial (every 12 weeks in 22 patients; at 12 weeks for the first scan, then every 6 weeks until week 48, and every 12 weeks thereafter in 2 patients). Follow-up CT scans were performed per treating providers' discretion in patients treated as a part of standard clinical care and in those treated in the expanded access program. A set of the baseline scan and serial scans throughout the treatment period of each patient was reviewed and measured sequentially according to the scan dates, as in the prior studies.(18-20) The radiologist did not have access to the detailed clinical and survival data at the time of measurements.
Assessment of tumor response and progression
Best overall response (irBOR) during therapy was assigned to each patient, using the thresholds of ≥30% decrease compared to baseline for partial response (PR) and ≥20% increase compared to nadir for progressive disease (PD), based on the prior studies showing the concordance among different methods of immune-related response assessment.(3, 10, 11) Confirmation on 2 consecutive scans at least 4 weeks apart was required for irPD.(2, 4, 10, 11) Time to progression using irRECIST (irTTP) was obtained in each patient, allowing the inclusion of new lesion measurements and requiring confirmation of PD.(10, 11) As a comparison, TTP according to standard RECIST1.1 was also defined in each patient, where appearance of new lesions or tumor burden increase ≥20% and 5 mm immediately defined PD without requiring confirmation.
Spider plots of the tumor burden changes throughout therapy for all patients were generated to demonstrate different patterns of tumor response and progression during therapy.
Statistical analysis
Comparison across groups of different response and progression patterns were performed using a Fisher exact test for categorical variables and a Kruskal-Wallis test for continuous variables. TTP by RECIST1.1 and irTTP were estimated using the method of Kaplan-Meier. Three-month conditional landmark analyses were performed to assess relationships between OS and tumor burden changes during the first 3 months of therapy. Extended Cox models with time-dependent covariates were also used to evaluate associations between OS and tumor burden changes throughout therapy. Multivariable Cox models adjusted for sex and baseline tumor burden. Both univariate and multivariable extended Cox models were stratified by age divided by the median of 63 years. All p-values were two-sided, with statistical significance defined as p < 0.05.
Results
Immune-related response and tumor burden dynamics
Among the total of 107 patients, 96 patients had measurable tumor burden with at least one target lesion at baseline. The remaining 11 patients had only non-target lesions without measurable tumor burden at baseline; these patients were treated as a part of standard clinical care (n=10) or in the expanded access program (n=1). The median follow-up time was 13 months.
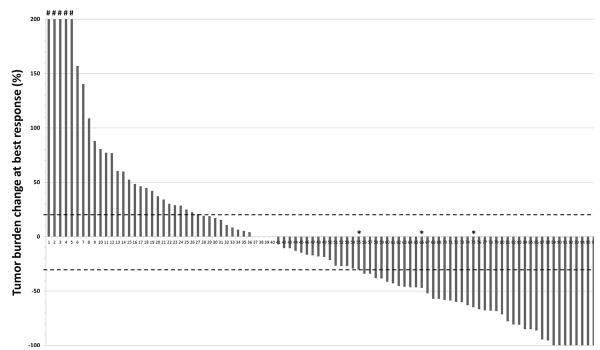
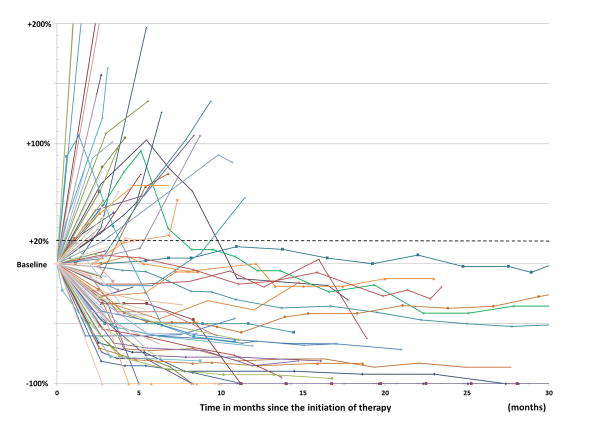
Tumor burden change comparing to baseline at the time of best overall response ranged from -100% to 567%, with a median of -18.5% (Fig. 1). Response rate by BOR throughout therapy was 44% (42/96, 95%CI: 34% to 54%; irCR in 5 and irPR in 37 patients). Progression-free rate at 12 months was 46% for TTP by RECIST1.1 and 68% for irTTP. The spiderplot demonstrated several distinct tumor burden dynamics during therapy (Fig. 2). In 57 patients (55%), tumor burden stayed below 20% increase of baseline throughout therapy (Fig. 2, lines below the dotted horizontal line at 20% of baseline). The remaining 39 patients (45%) experienced tumor burden increase of ≥20% of baseline at some point during therapy; of these, 3 patients demonstrated subsequent response with tumor burden decrease <30% of baseline, representing pseudoprogression. Given the observations of the spider plot, the threshold of 20% increase in tumor burden from baseline was applied to study its relationships with OS.
Fig. 1.
A waterfall plot of the tumor burden change of target lesions at best response (%) in reference to the baseline tumor burden in 96 patients with measurable tumor burden. Three patients noted with the asterisks experienced tumor response ≥30% decrease from baseline after experiencing initial tumor burden increase (pseudoprogression). Five patients noted with # had tumor burden increase beyond +200% (range: 211-566%). While 8 patients achieved CR for the target lesions (-100% of baseline), 3 of them had non-target lesions that did not completely respond and thus had PR for the best overall response assessment. Dotted lines at +20% and -30% represent the threshold for progression (PD) and partial response (PR).
Fig. 2.
Spider plot of tumor burden changes during pembrolizumab therapy in 96 patients with measurable tumor burden. Using a upper threshold of +20% increase from baseline tumor burden, the patients whose tumor burden stayed below 20% increase of baseline throughout therapy are noted as a distinct group with apparent treatment benefit (n=57; those below the dashed line of +20%).
Relationship between overall survival and tumor burden dynamics
Relationships between OS and quantitative tumor burden dynamics were assessed in 96 patients with measurable tumor burden. At the time of analysis, 31 patients (32.3%) had died. Based on the observations from the spider plot for tumor burden dynamics, OS was compared according to subgroups defined by the threshold of 20% increase in tumor burden from baseline, using 1) a three-month conditional landmark analysis and 2) extended Cox models.
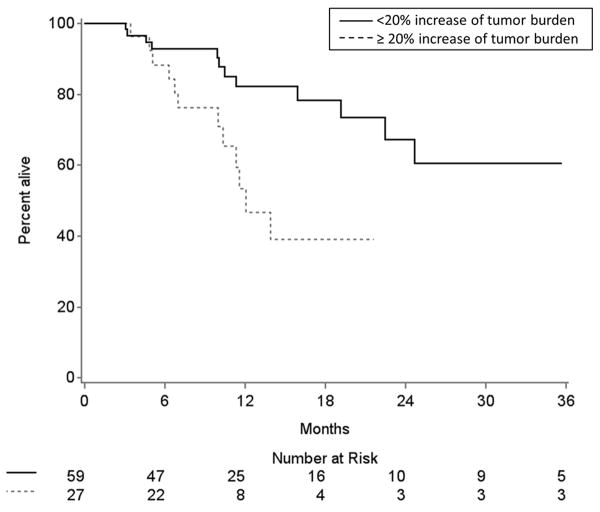
To be included in the three-month conditional landmark analysis, patients must have had survival times greater than 3 months. As a result, 10 patients with survival times of less than 3 months were removed from the analysis, leaving 86 eligible patients. Fifty-nine patients with <20% tumor burden increase between baseline and 3 months of therapy had longer OS than 27 patients with ≥20% increase within 3 months (12-month OS rate: 82 vs. 53%, respectively) (Fig. 3).
Fig. 3.
Kaplan-Meier estimates of overall survival (OS) of patients dichotomized by tumor burden changes within 3 months of therapy in the conditional landmark analysis. Patients with <20% tumor burden increase from baseline at 3 months of therapy had longer OS than patients with ≥20% increase from baseline within 3 months (12-month OS rate: 82 vs 53%, respectively).
In extended Cox models with time-dependent covariates, all 96 patients with measurable lesions (including 10 patients with survival times of less than 3 months) were analyzed and were initially classified as having tumor burden <20% increase from baseline. Any patient who experienced ≥20% increase from baseline was re-classified into the other group at that time. In this model, patients whose tumor burden stayed below 20% increase from baseline throughout therapy had significantly reduced hazards of death (HR=0.19, 95% CI: 0.08-0.43, p<0.0001) compared to those who experienced tumor burden increase ≥20% from baseline burden at any time point during therapy. The result remained significant in the multivariable analyses (HR=0.18, 95% CI: 0.08-0.41, p<0.0001) after adjusting for sex (p=0.83) and log2(baseline tumor burden) (HR=1.5, 95% CI: 1.1-2.1, p=0.01).
Pseudoprogression
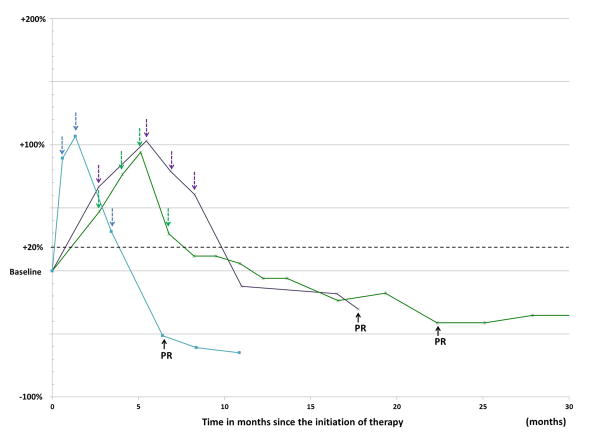
A total of 4 among the 107 patients demonstrated an unconventional response pattern, or pseudoprogression, which included 3 patients with measurable tumor burden at baseline (Fig. 4A) and one patient without measurable tumor burden at baseline. There was a trend that pseudoprogressors were younger than others (median age: 46 versus 63, respectively; Wilcoxon p=0.059). Though not statistically significant, pseudoprogressors had relatively low tumor burden at baseline; the baseline measurements of 3 patients with measurable disease were similar or lower (7.4 cm, 3.3 cm, and 1.7 cm) compared to the average baseline burden (7.1 cm) of the cohort, and the remaining one patient had only non-target lesions. Although limited due to guarantee-time bias, the median OS of the pseudoprogressors was 44.8 months compared to 24.7 months in the rest of the cohort.
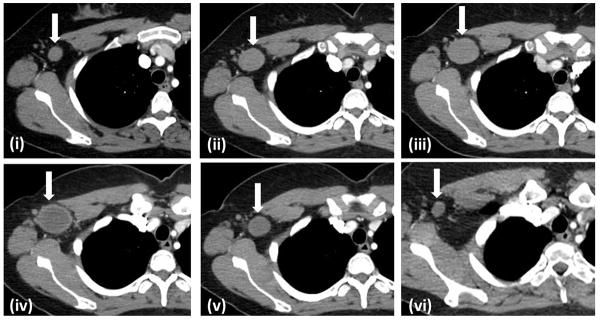
Fig. 4.
Pseudoprogressors with measurable tumor burden. A. The spider plot of tumor burden changes of 3 pseudoprogressors. All patients experienced more than 2 consecutive scans confirming PD (colored arrows) over the period longer than 4 weeks, thus meeting criteria for irPD, before achieving response to therapy (black arrows). B. A 38-year-old female with advanced melanoma with pseudoprogression, corresponding to a green line in Fig. 4A. A baseline scan showed a right axillary lymph node measuring 1.7 cm in short axis (i, arrow). The lesion increased in size on the 1st at 2.7 months (ii) and 2nd follow-up scans at 4.1 months (iii), demonstrating increase in size of the lesion more than 20% from baseline, confirming irPD. The lesion reached its maximal size at the 3rd follow-up scan at 5.5 months (iv), and then started to decrease in size on the 4th scan at 6.7 months (v). The lesion further decreased in size gradually, and met the criteria for response at 22.3 months of therapy (vi). Since then, the lesion remained small and maintained durable response over 19 months.
Notably, all 3 patients with pseudoprogression by measurable tumor burden had 2 or more consecutive scans demonstrating PD over the time frame of minimum 4 weeks, thus meeting the criteria for irPD before they experienced tumor response (Fig. 4A, B). Peak tumor burden of these patients were +103%, +106%, and +94% increase from baseline, and subsequent maximum shrinkage was -30%, -65%, and -47% from baseline, respectively. Median time to peak tumor burden was 5.5 months (range: 1.3-5.5). Median time to the first scan showing tumor burden decrease compared to the prior scan was 6.8 months (range: 3.4-6.9), and median time to the subsequent response was 17.8 months (range: 6.4-22.3). One patient without measurable tumor burden at baseline experienced pseudoprogression with a new lesion; in this patient, a new subcutaneous nodule appeared at 1.5 months of therapy, which significantly decreased in size on the subsequent scan 2 months later (Fig. 5). In all 4 pseudoprogressors, the decision of continuing therapy beyond initial tumor burden increase was due to the clinical benefits observed by the providers based on the overall assessments of clinical improvements and treatment tolerance.
Fig. 5.
Pseudoprogression in the setting of no measurable tumor burden at baseline. A 66-year-old male with advanced melanoma treated with pembrolizumab. A. The baseline scan showed no measurable tumor burden and subcentimeter, non-measurable brain metastasis. B. A follow-up scan at 1.5 months of therapy showed a new subcutaneous nodule (arrow). C. On a subsequent follow-up scan at 3.5 months of therapy, the nodule has significantly decreased in size (arrow).
Discussion
The present study of 107 advanced melanoma patients treated with the PD-1 inhibitor, pembrolizumab, as monotherapy characterized distinct patterns of tumor burden dynamics during therapy. Tumor burden increase of <20% from baseline during therapy was associated with longer OS, proposing a practical marker for survival and treatment benefits of pembrolizumab that can objectively guide therapeutic decisions. Pseudoprogression was a relatively uncommon phenomenon, seen in 4 patients (4%); 3 of these patients experienced responses that occurred after confirmed irPD, and one patient had pseudoprogression by a new lesion in the absence of measurable tumor burden.
The response rate during PD-1 inhibitor therapy was 44%, which is at the higher end of the response rate reported in the trials.(1, 21-24) This is likely explained by the fact that the present study assigned BOR based on the maximum response throughout therapy, thus capturing pseudoprogression with delayed response, in addition to responders by the conventional RECIST. Maximum tumor shrinkage also incorporated delayed response after pseudoprogression, which is not routinely reported in clinical trial results, providing additional information to further understand immune-related response phenomenon.(1)
Inspection of the spider plot has identified a distinct group of patients according to their tumor burden dynamics, where tumor burden stayed below 20% increase from baseline throughout therapy. This 20% increase threshold, identified from the spiderplot of the serial tumor measurements of all patients throughout therapy, corresponds to the conventional criteria for RECIST progression in patients who do not experience tumor decrease after initiation of therapy. Additionally, the choice of the threshold was also supported by the prior studies of interobserver variability of RECIST measurements, which have shown that 20% change of tumor burden is the smallest change that can be confidentially identified as true tumor change because it is outside of the measurement errors based on the 95% limits of agreements of the variability in the prior reports.(25, 26)
This observation was further studied for association with OS, using both the three-month conditional landmark analysis and the extended Cox models. While the landmark analysis excluded patients with survival time less than the 3-month landmark time point, the extended Cox models included all patients regardless of their survival time to complement the limitation of the landmark analysis. In both methods, tumor burden increase of <20% from baseline was associated with longer OS; therefore, this threshold may serve as a practical marker for survival and therapeutic benefits, and may provide objective guidelines for continuing pembrolizumab in advanced melanoma patients if prospectively validated in larger cohorts. It is well documented that RECIST progression does not necessarily indicate treatment failure especially in patients treated with effective targeted therapy.(27-30) This is mostly due to the fact that RECIST-PD is determined by the tumor increase in reference to the nadir (the smallest tumor burden since baseline) which is not equal to the baseline after tumor has decreased in response to therapy. Thus, for patients who have experienced initial marked tumor shrinkage, even a small increase of tumor burden thereafter can meet the criteria for PD, which is often the case for patients treated with effective therapy with durable benefit.(16-18, 27) It is important to note that the proposed threshold of 20% increase from baseline is therefore distinct from the cutpoint for RECIST-PD. Indeed, 9 patients (16%) in the group with <20% increase from baseline have met the criteria for RECIST-PD during therapy and 3 of them even had confirmed irPD, despite the fact that the tumor burden was well below the baseline burden and the therapeutic benefit in controlling the tumor burden was apparent from the spider plot.
The incidence of pseudoprogression was 9.7% (22/227) in the initial report of irRC in melanoma patients treated with ipilimumab, 10% (11/107) in nivolumab treated cohort, and was 7% (24/327) in pembrolizumab-treated cohort.(1, 4, 9) The rate of patients with pseudoprogression in this retrospective analysis (5/107, 4.7%, 95% CI [1.5 to 10.1%]) is similar to the rates from previously reported studies, confirming that pseudoprogression is a relatively uncommon event in patients treated with PD-1 inhibition.(1) In spite of the increased awareness of the possibility of pseudoprogression among oncology providers, the data indicates that this is a rare phenomenon and increase of tumor burden more likely reflect true progression than pseudoprogression in patients treated with immune-checkpoint inhibitors. There was a trend that patients with pseudoprogression may be younger than others (p=0.059), indicating that the immune system may be more reactive to exogenous stimulation in a younger population; however, this observation requires further studies in larger cohorts.
In 3 pseudoprogressors with measurable tumor burden, the peak tumor burden was about double the baseline tumor burden in these patients, an increase that is substantially greater than the threshold for progression (+20% increase). This large increase in tumor size presents a challenge to differentiate pseudoprogression from true progression during therapy. All 3 patients had two or more consecutive scans during the timeframe of more than 4 weeks, thus confirming irPD, before experiencing subsequent responses. This raises a question if the currently recommended timeframe of minimum 4 weeks for confirmed PD is adequate to capture all patients with delayed tumor shrinkage. Recently reported criteria for immune-related response evaluations in neuro-oncology trials by the Response Assessment for Neuro-Oncology (RANO) working group indicated that 4 weeks might be too early to exclude pseudoprogression based on the review of a spider plot, and recommended a 3-month period for confirmation of PD.(31) Decision of continuing therapy beyond initial tumor burden increase is often up to the discretion of clinical care providers, both in the standard care setting and in most of the recent immune-checkpoint inhibitor trials, which provide one of the largest challenges in the immuno-oncology practice. (2, 12, 16) Though the decision is mostly based on the observed clinical benefits as noted in the present study, the findings on follow-up imaging during treatment monitoring beyond progression provide key information as to when to discuss alternate therapy.(20, 27) In this regard, defining an optimal time point for a confirmatory scan after initial progression has a significant impact on treatment decisions.
Among the 3 patients in the present study, one patient had subsequent response at 3 months of therapy; however, in the other 2 patients, response was only noted after 6 months of therapy. While limited by a small number of measurable pseudoprogression cases, it is possible that the timeframe of pseudoprogression and subsequent response may have a wider range than currently assumed. It is also possible that delayed immunologic response may play some roles in these phenomena in addition to inflammatory response with tumor infiltration of immune cells, especially in patients who experience delayed tumor regression after pseudoprogression. Further studies with a larger number of patients are needed to address this possible limitation of the current immune-related assessment strategy.
One patient who had no measurable tumor burden at baseline has experienced pseudoprogression due to appearance of new lesion followed by subsequent responses. The observation may be unique to patients treated with standard care and not in clinical trials, because most trials require measurable tumor burden in their eligibility criteria for enrollment. As a consequence, pseudoprogression in the absence of baseline measurable tumor burden has not been described in the previous reports that were based on patients treated in trials. Although the original irRC does not take “unequivocal progression of non-target lesions” into consideration for overall response assessment, the guideline is limited to the scenarios where measurable tumor burden is present.(4) In the present study, 11 patients (10%), treated with standard care (n=10) or in the expanded access program (n=1), had no measurable disease at baseline per irRECIST, indicating the importance of more detailed guidelines of immune-related response evaluations in the absence of measurable tumor burden. The observation of this additional case in the present study provides insight for this under-recognized scenario that may require more attention given the increasing use immune-checkpoint inhibitors in the standard cancer care.
Of note, tumor burden assessment in the present study was performed using irRECIST utilizing unidimensional measurements rather than using the original irRC that utilizes bidimensional measurements.(4) This is based on the published prior studies from our group that have demonstrated that unidimensional measurements are more reproducible than bidimensional measurements, and that irRECIST provides highly concordant assessments compared to the original irRC.(3, 10, 11) The threshold of 20% tumor burden change, which defines progression per RECIST and was also applied in the present study, is outside of the range of variability of unidimensional measurements, while 25% increase for progression by WHO criteria and irRC is within the range of variability of bidimensional measurements and thus may not reflect true changes of tumor. The important features of irRC to capture immune-related responses (i.e., inclusion of new lesion measurements and requirement of confirmation for PD) are included in irRECIST to capture these unique phenomena. The unidimensional measurement approach in irRECIST also helps to provide direct comparisons with conventional RECIST, allowing us to focus on the differences derived from immune-related response phenomena rather than those due to the differences in measurement methods.(12, 16, 17)
The limitation of the study includes a retrospective design in a relatively small number of patients treated at a single institution. Due to the potential for guarantee-time bias in the data, the 3 pseudoprogressors with measurable tumor burden were included with those who experienced >20% increase in tumor burden relative to baseline in spite of their subsequent responses and delayed treatment benefits. This certainly indicates the limited utility of the 20% increase threshold for a minority of patients who experiences pseudoprogression and subsequent tumor regression. In addition, given the limitation of a relatively small number of patients, larger cohorts are needed to further solidify the findings. Regardless, the proposed upper threshold of <20% increase from baseline could demonstrate a significant association with longer OS in two complementary analyses with the landmark method and Cox models with time-varying covariates incorporating tumor burden changes at all time points throughout therapy. Although the validation of the threshold of 20% increase using comprehensive analyses for the optimal cut points is ideal, this was not performed given the challenges of including all time points during therapy rather than one specific time point in such analyses. In addition, the 20% threshold also has a practical advantage of being a well-known value for oncology provides who are familiar with RECIST guidelines.
Our results provide a basis to propose <20% increase from baseline as a marker of survival and treatment benefit that may guide clinical providers to continue pembrolizumab therapy, if the observation is validated in a larger prospective cohort as the next step. For those with ≥20% tumor burden increases, additional strategies are needed to identify patients with pseudoprogression, although they consist of a relatively small subpopulation. Novel imaging techniques such as immuno-PET are under active investigation to noninvasively visualize different players of cellular immunity in the tumor microenvironment and contribute to solve this challenging clinical question. International initiatives are ongoing to collect and analyze large database to further address these challenges and establish guidelines for response evaluations, patient monitoring, and clinical management decisions, as represented by the efforts by the Society for Immunotherapy of Cancer and by the RECIST working group.
In conclusion, tumor burden increase of less than 20% from baseline during therapy was associated with longer OS, proposing a practical marker for survival and therapeutic benefit of pembrolizumab that can be validated in prospective cohorts in further studies to establish an objective guide treatment decisions. Pseudoprogression was a relatively uncommon phenomenon; however, response can be noted after confirmed irPD, which indicates a limitation of the current immune-related assessment strategy. Immune-related response of patients without measurable tumor burden is an under-recognized scenario that requires further attention given the increasing use of immune-checkpoint inhibitors in the clinical setting.
Translational Relevance.
Unconventional immune-related response patterns during immune-checkpoint inhibitor therapy provide a significant challenge in immuno-oncology practice. The study characterized tumor burden dynamics in advanced melanoma patients treated with pembrolizumab, and studied their relationships with clinical outcome. Tumor burden increase of less than 20% from baseline during therapy, noted in 55% of the patient, was associated with longer OS overall survival, proposing a practical prognostic marker that may objectively guide treatment decisions. Pseudoprogression was noted in 4 patients (4%). Three patients with initial increase of target lesions experienced subsequent response after confirmed irPD, indicating a limitation of the current strategy for immune-related response assessment. One patient without measurable tumor burden progressed with new lesion that subsequently regressed, indicative of a need for increased attention to non-measurable tumor burden in the context of immunotherapy. The study provided important observations that are relevant to immuno-oncology practice, which needs to be validated in prospective cohorts.
Acknowledgments
The investigator, M.Nishino, was supported by 1K23CA157631 (National Cancer Institute) and Merck Investigator Studies Program (Merck).
References
- 1.Chiou VL, Burotto M. Pseudoprogression and Immune-Related Response in Solid Tumors. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2015;33(31):3541–3. doi: 10.1200/jco.2015.61.6870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nishino M, Jagannathan JP, Krajewski KM, O'Regan K, Hatabu H, Shapiro G, et al. Personalized tumor response assessment in the era of molecular medicine: cancer-specific and therapy-specific response criteria to complement pitfalls of RECIST. AJR American journal of roentgenology. 2012;198(4):737–45. doi: 10.2214/AJR.11.7483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nishino M, Tirumani SH, Ramaiya NH, Hodi FS. Cancer immunotherapy and immune-related response assessment: The role of radiologists in the new arena of cancer treatment. European journal of radiology. 2015;84(7):1259–68. doi: 10.1016/j.ejrad.2015.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wolchok JD, Hoos A, O'Day S, Weber JS, Hamid O, Lebbe C, et al. Guidelines for the evaluation of immune therapy activity in solid tumors: immune-related response criteria. Clinical cancer research : an official journal of the American Association for Cancer Research. 2009;15(23):7412–20. doi: 10.1158/1078-0432.CCR-09-1624. [DOI] [PubMed] [Google Scholar]
- 5.Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. Journal of the National Cancer Institute. 2000;92(3):205–16. doi: 10.1093/jnci/92.3.205. [DOI] [PubMed] [Google Scholar]
- 6.Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1) European journal of cancer (Oxford, England : 1990) 2009;45(2):228–47. doi: 10.1016/j.ejca.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 7.Nishino M, Jagannathan JP, Ramaiya NH, Van den Abbeele AD. Revised RECIST guideline version 1.1: What oncologists want to know and what radiologists need to know. AJR American journal of roentgenology. 2010;195(2):281–9. doi: 10.2214/AJR.09.4110. [DOI] [PubMed] [Google Scholar]
- 8.Nishino M, Hatabu H, Johnson BE, McLoud TC. State of the art: Response assessment in lung cancer in the era of genomic medicine. Radiology. 2014;271(1):6–27. doi: 10.1148/radiol.14122524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hodi FS, Hwu WJ, Kefford R, Weber JS, Daud A, Hamid O, et al. Evaluation of Immune-Related Response Criteria and RECIST v1.1 in Patients With Advanced Melanoma Treated With Pembrolizumab. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2016;34(13):1510–7. doi: 10.1200/JCO.2015.64.0391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nishino M, Gargano M, Suda M, Ramaiya NH, Hodi FS. Optimizing immune-related tumor response assessment: does reducing the number of lesions impact response assessment in melanoma patients treated with ipilimumab? Journal for immunotherapy of cancer. 2014;2:17. doi: 10.1186/2051-1426-2-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nishino M, Giobbie-Hurder A, Gargano M, Suda M, Ramaiya NH, Hodi FS. Developing a common language for tumor response to immunotherapy: immune-related response criteria using unidimensional measurements. Clinical cancer research : an official journal of the American Association for Cancer Research. 2013;19(14):3936–43. doi: 10.1158/1078-0432.CCR-13-0895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nishino M, Ramaiya NH, Chambers ES, Adeni AE, Hatabu H, Janne PA, et al. Immune-related response assessment during PD-1 inhibitor therapy in advanced non-small-cell lung cancer patients. Journal for immunotherapy of cancer. 2016;4:84. doi: 10.1186/s40425-016-0193-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Erasmus JJ, Gladish GW, Broemeling L, Sabloff BS, Truong MT, Herbst RS, et al. Interobserver and intraobserver variability in measurement of non-small-cell carcinoma lung lesions: implications for assessment of tumor response. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2003;21(13):2574–82. doi: 10.1200/jco.2003.01.144. [DOI] [PubMed] [Google Scholar]
- 14.Nishino M, Guo M, Jackman DM, DiPiro PJ, Yap JT, Ho TK, et al. CT tumor volume measurement in advanced non-small-cell lung cancer: Performance characteristics of an emerging clinical tool. Academic radiology. 2011;18(1):54–62. doi: 10.1016/j.acra.2010.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhao B, James LP, Moskowitz CS, Guo P, Ginsberg MS, Lefkowitz RA, et al. Evaluating variability in tumor measurements from same-day repeat CT scans of patients with non-small cell lung cancer. Radiology. 2009;252(1):263–72. doi: 10.1148/radiol.2522081593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nishino M. Immune-related response evaluations during immune-checkpoint inhibitor therapy: establishing a “common language” for the new arena of cancer treatment. Journal for immunotherapy of cancer. 2016;4:30. doi: 10.1186/s40425-016-0134-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nishino M. Pseudoprogression and Measurement Variability. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2016;34(28):3480–1. doi: 10.1200/jco.2016.67.6759. [DOI] [PubMed] [Google Scholar]
- 18.Nishino M, Cardarella S, Jackman DM, Ramaiya NH, Rabin MS, Hatabu H, et al. RECIST 1.1 in NSCLC patients with EGFR mutations treated with EGFR tyrosine kinase inhibitors: comparison with RECIST 1.0. AJR American journal of roentgenology. 2013;201(1):W64–71. doi: 10.2214/AJR.12.9668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nishino M, Dahlberg SE, Cardarella S, Jackman DM, Rabin MS, Hatabu H, et al. Tumor volume decrease at 8 weeks is associated with longer survival in EGFR-mutant advanced non-small-cell lung cancer patients treated with EGFR TKI. Journal of thoracic oncology : official publication of the International Association for the Study of Lung Cancer. 2013;8(8):1059–68. doi: 10.1097/JTO.0b013e318294c909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nishino M, Dahlberg SE, Cardarella S, Jackman DM, Rabin MS, Ramaiya NH, et al. Volumetric tumor growth in advanced non-small cell lung cancer patients with EGFR mutations during EGFR-tyrosine kinase inhibitor therapy: developing criteria to continue therapy beyond RECIST progression. Cancer. 2013;119(21):3761–8. doi: 10.1002/cncr.28290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Topalian SL, Sznol M, McDermott DF, Kluger HM, Carvajal RD, Sharfman WH, et al. Survival, durable tumor remission, and long-term safety in patients with advanced melanoma receiving nivolumab. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2014;32(10):1020–30. doi: 10.1200/JCO.2013.53.0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weber JS, D'Angelo SP, Minor D, Hodi FS, Gutzmer R, Neyns B, et al. Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): a randomised, controlled, open-label, phase 3 trial. The Lancet Oncology. 2015;16(4):375–84. doi: 10.1016/s1470-2045(15)70076-8. [DOI] [PubMed] [Google Scholar]
- 23.Weber JS, Kudchadkar RR, Yu B, Gallenstein D, Horak CE, Inzunza HD, et al. Safety, efficacy, and biomarkers of nivolumab with vaccine in ipilimumab-refractory or -naive melanoma. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2013;31(34):4311–8. doi: 10.1200/jco.2013.51.4802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wolchok JD, Kluger H, Callahan MK, Postow MA, Rizvi NA, Lesokhin AM, et al. Nivolumab plus ipilimumab in advanced melanoma. The New England journal of medicine. 2013;369(2):122–33. doi: 10.1056/NEJMoa1302369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nishino M, Jackman DM, Hatabu H, Yeap BY, Cioffredi LA, Yap JT, et al. New Response Evaluation Criteria in Solid Tumors (RECIST) guidelines for advanced non-small cell lung cancer: comparison with original RECIST and impact on assessment of tumor response to targeted therapy. AJR American journal of roentgenology. 2010;195(3):W221–8. doi: 10.2214/AJR.09.3928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krajewski KM, Nishino M, Franchetti Y, Ramaiya NH, Van den Abbeele AD, Choueiri TK. Intraobserver and interobserver variability in computed tomography size and attenuation measurements in patients with renal cell carcinoma receiving antiangiogenic therapy: implications for alternative response criteria. Cancer. 2014;120(5):711–21. doi: 10.1002/cncr.28493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nishino M, Cardarella S, Dahlberg SE, Jackman DM, Ramaiya NH, Hatabu H, et al. Radiographic assessment and therapeutic decisions at RECIST progression in EGFR-mutant NSCLC treated with EGFR tyrosine kinase inhibitors. Lung cancer. 2013;79(3):283–8. doi: 10.1016/j.lungcan.2012.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Riely GJ, Kris MG, Zhao B, Akhurst T, Milton DT, Moore E, et al. Prospective assessment of discontinuation and reinitiation of erlotinib or gefitinib in patients with acquired resistance to erlotinib or gefitinib followed by the addition of everolimus. Clinical cancer research : an official journal of the American Association for Cancer Research. 2007;13(17):5150–5. doi: 10.1158/1078-0432.ccr-07-0560. [DOI] [PubMed] [Google Scholar]
- 29.Park K, Ahn M, Yu CJ, Kim S, Lin M, Sriuranpong V, et al. ASPIRATION: first-line erlotinib until and beyond RECIST progression in Asian patients with EGFR mutation-positive NSCLC. ESMO. 2014 [Google Scholar]
- 30.Park K, Tsai CM, Ahn M, Yu CJ, Kim SW, Sriuranpong V, et al. ASPIRATION: Phase II study of continued erlotinib beyond RECIST progression in Asian patients (pts) with epidermal growth factor receptor (EGFR) mutation-positive non-small cell lung cancer (NSCLC) J Clin Oncol. 2012;30 (suppl; abstr TPS7614) [Google Scholar]
- 31.Okada H, Weller M, Huang R, Finocchiaro G, Gilbert MR, Wick W, et al. Immunotherapy response assessment in neuro-oncology: a report of the RANO working group. The Lancet Oncology. 2015;16(15):e534–42. doi: 10.1016/s1470-2045(15)00088-1. [DOI] [PMC free article] [PubMed] [Google Scholar]