Abstract
Aims
Suicidal behaviour is an under-reported and hidden cause of death in most low- and middle-income countries (LMIC) due to lack of national systematic reporting for cause-specific mortality, high levels of stigma and religious or cultural sanctions. The lack of information on non-fatal suicidal behaviour (ideation, plans and attempts) in LMIC is a major barrier to design and implementation of prevention strategies. This study aims to determine the prevalence of non-fatal suicidal behaviour within community- and health facility-based populations in LMIC.
Methods
Twelve-month prevalence of suicidal ideation, plans and attempts were established through community samples (n = 6689) and primary care attendees (n = 6470) from districts in Ethiopia, Uganda, South Africa, India and Nepal using the Composite International Diagnostic Interview suicidality module. Participants were also screened for depression and alcohol use disorder.
Results
We found that one out of ten persons (10.3%) presenting at primary care facilities reported suicidal ideation within the past year, and 1 out of 45 (2.2%) reported attempting suicide in the same period. The range of suicidal ideation was 3.5–11.1% in community samples and 5.0–14.8% in health facility samples. A higher proportion of facility attendees reported suicidal ideation than community residents (10.3 and 8.1%, respectively). Adults in the South African facilities were most likely to endorse suicidal ideation (14.8%), planning (9.5%) and attempts (7.4%). Risk profiles associated with suicidal behaviour (i.e. being female, younger age, current mental disorders and lower educational and economic status) were highly consistent across countries.
Conclusion
The high prevalence of suicidal ideation in primary care points towards important opportunities to implement suicide risk reduction initiatives. Evidence-supported strategies including screening and treatment of depression in primary care can be implemented through the World Health Organization's mental health Global Action Programme suicide prevention and depression treatment guidelines. Suicidal ideation and behaviours in the community sample will require detection strategies to identify at risks persons not presenting to health facilities.
Key words: Low- and middle-income countries, suicidal behaviour, suicidal ideation
Introduction
The World Health Organization (WHO) mortality database indicates over 800 000 annual suicide deaths worldwide, making it a leading cause of death (WHO, 2014). Suicide is a global public health issue and a serious contributor to the total global burden of disease, and its prevalence is predicted to increase in the next decade (WHO, 2012). In addition to actual suicide deaths, every year many more attempts occur and each attempt carries the possibility of subsequent attempts of increasing lethality, significant psychological suffering, long-term physical injury and death, as well as lasting negative effects on families and communities (Borges et al. 2010).
An estimated 75% of all suicides occur in low- and middle-income countries (LMIC), where limited resources are available to prevent suicidal behaviour (WHO, 2014). Paradoxically it remains a low public health priority and reliable data is largely unavailable (Värnik, 2012). Data on non-fatal suicidal behaviours – including ideation, defined as ‘thoughts of engaging in behaviour intended to end one's life’ (Nock et al. 2008a), as well as plans and attempts – are crucial to inform prevention efforts. While some studies into non-fatal suicidal behaviours exist in LMIC (Nock et al. 2008b; Oladeji & Gureje, 2011; Ojagbemi et al. 2013), this information is still sparse. Most research on suicide attempts is limited to data from small samples or psychiatric clinical populations and is thus not representative of general populations (Milner, Page, & Lamontagne, 2014). Lack of data on non-fatal suicidal behaviour reported in primary care settings is especially problematic because most patients are unlikely to be evaluated by mental health specialists given the dearth of psychiatrists and clinical psychologists in LMIC. Moreover, primary care-based strategies are among the most effective initiatives for suicide risk reduction (Mann et al. 2005).
Given this lack of information on non-fatal suicidal behaviour in LMIC, the aim of this study is to determine the 12-month prevalence of suicidal ideation, plans and attempts, as well as associated risk factors and help-seeking behaviour, within communities and primary care health facilities in five LMIC. The research was conducted within a broader initiative of developing and piloting community-based and primary care mental health services for low-resource settings.
Method
Study settings
The study population is comprised of adults in communities and health facilities in the five countries of the Programme for Improving Mental Health Care (PRIME) consortium. PRIME aims to integrate treatment services for depression, alcohol use disorders (AUDs) and psychosis into the primary health care sector in these districts. The PRIME districts in Ethiopia (Sodo District), India (Sehore District), Nepal (Chitwan District), South Africa (Dr Kenneth Kaunda District) and Uganda (Kamuli District) were selected in consultation with national Ministry of Health officials (Lund et al. 2012). These districts are characterised by their lack of specialist mental health care providers, assumed high burden of common mental disorders (Demyttenaere et al. 2004), and reasonably high accessibility of primary health care services (Jordans et al. 2013; Hanlon et al. 2014). Prior to the implementation of the district mental health care plans, consortium partners conducted population-based community surveys and facility-based surveys in order to establish baseline figures for the burden of and treatment gap for depression and AUD.
Facility survey sampling and data collection
The primary objectives of the facility surveys were to estimate the changes in clinical detection of adults with depression and AUD who attend public primary health clinics following integration of the PRIME intervention packages in the implementation areas (De Silva et al. 2015). Inclusion criteria were age of 18 years or more, present at the clinic for primary care services, ability to provide informed consent and fluency in the local language. Field workers stationed in health facilities recruited and interviewed adult participants from the waiting areas either before (Ethiopia, Uganda, South Africa, Nepal) or after clinical consultations (India).
Community survey sampling and data collection
The primary objective of the population-based community surveys were to estimate changes in the treatment gap for adults with depressive and AUDs as a consequence of implementing the PRIME intervention packages in the implementation areas (De Silva et al. 2015; Rathod et al. 2016). Inclusion criteria were: age of 18 years or more, residency in the implementation area, ability to provide informed consent and fluency in the local language. In Ethiopia, Uganda and Nepal, the sampling plan involved random selection of households in the district, enumeration of adults in the household and then random selection of one adult member of the household for recruitment into the study. In India, the sampling plan involved random selection of adults from a list of registered voters. Adults who provided informed consent were administered a structured questionnaire by an interviewer.
Questionnaire and measurements
Questionnaires used across studies and countries were largely consistent. There were variations in the sub-samples of participants who completed each section, with additional sections relevant for the participants who screened positive for depression or AUD. This analysis includes items drawn from the sections about demographic characteristics (i.e. age, sex, marital status and educational attainment), relative economic status, depression, AUD, suicidality and disability.
To create country-specific relative economic scores in Nepal and South Africa, we used principle components analysis and included a range of locally relevant assets and dummy-coded housing characteristics. The sum of weights from the first factor from principle components analysis is a Z-score on a normal distribution, which corresponds to each participant's relative wealth in comparison to the other respondents in the country dataset (Vyas & Kumaranayake, 2006). We created tertiles of these scores to classify respondents as being of lower, average or higher economic status, relative to their neighbours. In Ethiopia, respondents were asked to self-classify their economic status as being of lower, average or higher status. In India, the interviewer made an observation about the respondents housing construction quality, which we have used as a proxy measure for being of lower, average or higher economic status. In Uganda, the facility study interview schedule was such that only participants who screened positive for depression or AUD completed the section on economic status, so we have excluded the economic data from Uganda from this analysis.
To assess depressive symptoms we used the nine-item Patient Health Questionnaire (PHQ9) (Kroenke et al. 2001). The PHQ9 is a widely-validated screening tool used for the detection of major depressive disorder. Each of the nine-items corresponds to a DSM-IV (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition) symptom of major depressive disorder, and the respondent is asked to state whether the symptom has been present for the past 14 days. Each item is scored from 0 to 3. We calculated a summary score for total depression symptom score using the sum of first eight items. We excluded the 9th item from the total score, as it was a question about suicidality, which was related to our outcome of interest. In the facility survey the Cronbach's α for the eight-item summary score ranged from 0.72 in India to 0.83 in Nepal.
To identify participants with AUD we used the ten-item Alcohol Use Disorders Identification Test (AUDIT) (Saunders et al. 1993; Babor et al. 2001). The AUDIT is a widely-used screening tool for the detection of AUD and alcohol dependency. The ten items relate to the frequency and consequences of alcohol consumption that the respondent has experienced over the past 12 months. Each item is scored from 0 to 4 and the total AUDIT score is the sum of the 10 items’ scores. In the Facility Study the Cronbach's α for the AUDIT ranged from 0.67 in Uganda to 0.88 in Nepal.
Suicidality questions were adapted from the CIDI (Composite International Diagnostic Interview) suicidality module (Robins et al. 1988). Field workers asked participants about whether in the past 12 months they had thoughts of taking their own life. Those who responded affirmatively to the ideation question were asked if they had made a plan to take their own life. Those who responded affirmatively to the planning question were asked if they attempted to take their own life. Those who responded affirmatively to the suicidal attempt question were asked if they had disclosed their suicide attempt to anyone (inclusive of both informal supports, such as friends and family or formal supports such as religious leaders and health workers) and if they had sought any treatment. In Uganda, the community study interview schedule was such that only participants who screened positive for depression or AUD completed the section on suicidality, so we have excluded the Uganda community survey from this analysis.
To assess disability status we used the 12-item World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0) (Üstün et al. 2010). The WHODAS 2.0 is an internationally validated tool for measuring impairment. The 12 items pertain to the ability of the respondent to engage in specific mental and physical tasks in the past 30 days. Each item is scored from 1 to 5 and the total WHODAS score is the sum of the 12 items’ scores. In Uganda, the facility study interview schedule was such that only participants who screened positive for depression or AUD completed the section on disability, so we have excluded the disability data from Uganda from this analysis.
Statistical analysis
First, we described the demographic characteristics of the participants from each study in each country, reporting means and standard deviations for age, and estimated proportions who were female, married and had low educational attainment. Second, we reported the proportion of participants from each study in each country who provided affirmative responses to each of the five suicidality questions (i.e. ideation, planning, action, disclosure and treatment seeking), and the 95% confidence interval for suicidal ideation. To facilitate cross-country comparisons we standardised the suicidality proportions to the age structure of the International Network for the Demographic Evaluation of Populations and their Health (INDEPTH) standard population for males and females in LMIC (Ng et al. 2009; Streatfield et al. 2014). Third, we pooled data across countries and compared the proportion who responded affirmatively to each suicidality question across the two study designs. We used the two-sample test of proportions to assess whether the prevalence of suicidality behaviours (i.e. ideation, planning, action, discussion or treatment) differed by study sample (community or facility based) for the combined samples from the three countries which completed the suicidality sections in both studies (i.e. Ethiopia, India and Nepal).
Finally, to identify potential risk factors for suicidal ideation, we used log-Poisson regression models with robust standard errors (Zou, 2004) to identify the sociodemographic (i.e. age, sex, education and relative wealth) and health-related (i.e. depression, AUD and disability) correlates of suicidal ideation among facility-attending adults in each country. The models for age and sex are univariable models, while the remainder of models are multivariable models which are adjusted for age and sex. We used suicidal ideation as the outcome measure rather than planning or action because any future programme aiming to reduce suicidal ideation will consequently impact planning and action. The exponentiated coefficients from log-Poisson regression are relative risks, which we interpreted as prevalence ratios (PRs), such that a unit change in the correlate is associated with a relative change in the prevalence of reporting suicidal ideation. We converted the units of age from years to decades; the age coefficients are interpreted as the relative difference in prevalence of suicidal ideation for each additional 10 years of age. We adjusted the statistics from the community survey for each site's complex sampling designs for all analyses except cross-country comparisons. We conducted the analysis in Stata SE 14.1 (StataCorp, College Station, USA).
Ethics
For both surveys, field workers described the study's objectives to the potential participant. Participants could sign an informed consent document with their name, or if they were illiterate could sign with an ‘X’ with a witness present. The Institutional Review Boards of the WHO (Geneva, Switzerland), University of Cape Town (South Africa), Addis Ababa University (Ethiopia), Indian Council of Medical Research (New Delhi, India), Sangath (Goa, India), Nepal Health Research Council (Kathmandu, Nepal), University of KwaZulu-Natal (South Africa), Makarere University (Kampala, Uganda) and the National Council of Science and Technology (Kampala, Uganda) reviewed and approved the protocol for the PRIME Community and Facility surveys.
Results
Sociodemographic characteristics of community residents and facility attendees
The sociodemographic characteristics of participants in the community and facility studies are presented in Table 1. The mean age ranged from 31 years for facility attendees in Uganda to 47 years for facility attendees in South Africa. The majority of participants in the studies were female, aside from the study of community residents in India (45% female). A majority of participants were married or currently cohabitating (all >69%).
Table 1.
Sociodemographic characteristics of community study and facility detection study participants in PRIME implementation areas in Ethiopia, India, Nepal, South Africa and Uganda, 2013–2014
| Ethiopia | India | Nepal | South Africa | Uganda | ||||
|---|---|---|---|---|---|---|---|---|
| Community residentsa | Facility attendees | Community residentsa | Facility attendees | Community residentsa | Facility attendees | Facility attendees | Facility attendees | |
| Sample size | 1486 | 1017 | 3220 | 760 | 1983 | 1474 | 1322 | 1897 |
| Age, years (s.d.) | 39.4 (15.3) | 35.5 (15.6) | 40.2 (15.1) | 39.7 (14.8) | 39.8 (15.4) | 39.5 (15.0) | 46.9 (13.3) | 31.1 (11.7) |
| Female (%) | 50.6 | 54.2 | 45.4 | 50.8 | 60.1 | 65.8 | 75.0 | 79.6 |
| Ever married/cohabitating (%) | 84.8 | 73.2 | 89.5 | 91.5 | 86.5 | 91.4 | 69.1 | b |
| Illiterate/did not complete primary (%) | 45.6 | 39.3 | 50.9 | 50.1 | 13.2 | 36.0 | 23.3 | 9.1 |
PRIME, Programme for Improving Mental Health Care.
Community survey figures are adjusted for the complex sampling design within each site.
Marital status only asked of participants who screened positive for depression or alcohol use disorders, rather than for the full sample.
Suicidality profiles for community residents and facility attendees
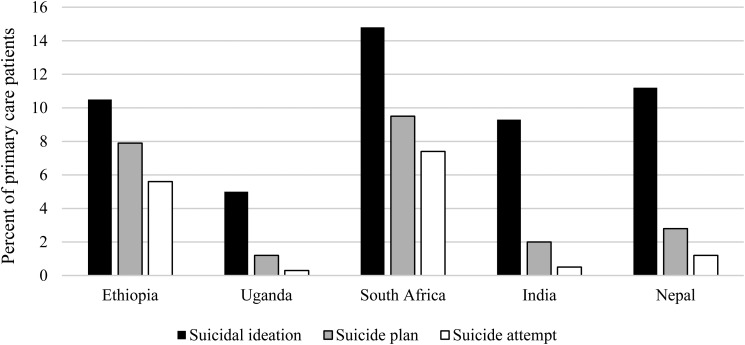
Among participants across studies, the standardised proportions of adults who reported suicidal ideation in the past 12 months ranged from 3.5% among community residents in Nepal to 14.8% of facility attendees in South Africa (Fig. 1). Suicide planning ranged from 0.9% of facility attendees in Nepal to 9.5% of facility attendees in South Africa. Suicide attempt ranged from 0.3% of facility attendees in Uganda to 7.4% of facility attendees in South Africa. Among those who reported attempted suicide, disclosure of the attempt with another person ranged from 19.6% of community residents in Nepal to 58.3% of facility attendees in Uganda. Among those who attempted suicide, help seeking was uncommon: 26% of community residents who had attempted suicide had sought help in Ethiopia, whereas 0% had done so in the India, Nepal and Uganda samples (Table 2). In addition, Table 2 reports the proportion who reported planning among those with ideation and subsequently the proportion who reported suicidal attempt among those who reported planning. Among those participants who reported suicidal ideation, the proportion who reported planning ranged from 11.7% among community residents in India to 76.6% of facility attendees in Ethiopia. Among those participants who had reported planning, the proportion who reported a suicide attempt ranged from 24.9% among facility attendees in India to 72.2% of community residents in Ethiopia.
Fig. 1.
Twelve-month prevalence of suicidal ideation, plans and attempts among primary care attendees.
Table 2.
Suicidality profiles of community study and facility detection study participants in PRIME implementation areas in Ethiopia, India, Nepal, South Africa and Uganda, 2013–2014
| Ethiopia | India | Nepal | South Africa | Uganda | ||||
|---|---|---|---|---|---|---|---|---|
| Community residents | Facility attendees | Community residents | Facility attendees | Community residents | Facility attendees | Facility attendees | Facility attendees | |
| Ideation % (95% CI) | 7.0 (5.2–9.4) | 10.5 (8.6–12.6) | 11.1 (9.6–13.0) | 9.3 (7.1–11.9) | 3.5 (2.6–4.8) | 11.2 (9.3–13.6) | 14.8 (9.8–21.7) | 5.0 (3.8–6.5) |
| Planning % (95% CI) | 4.6 (3.2–6.4) | 7.9 (6.3–9.9) | 1.1 (0.7–1.8) | 2.0 (1.2–3.2) | 0.9 (0.4–2.2) | 2.8 (1.8–4.5) | 9.5 (5.6–15.8) | 1.2 (0.8–1.8) |
| Planning % (among those with ideation) | 65.6 | 76.6 | 11.7 | 32.1 | 24.3 | 23.7 | 58.7 | 18.3 |
| Attempt % (95% CI) | 3.7 (2.4–5.5) | 5.6 (4.2–7.4) | 0.4 (0.3–0.7) | 0.5 (0.1–1.4) | 0.7 (0.2–2.1) | 1.2 (0.6–2.4) | 7.4 (3.8–14.0) | 0.3 (0.1–0.6) |
| Attempt % (among those planning) | 72.2 | 65.2 | 39.9 | 24.9 | 70.4 | 57.1 | 55.1 | 34.7 |
| Disclosure of attempt % (among those with attempt) | 45.3 | 29.2 | 35.6 | 35.1 | 19.6 | 18.3 | 51.1 | 58.3 |
| Help seeking after attempt % (among those with attempt) | 26.0 | 15.7 | 0.0 | 0.0 | 0.0 | 0.0 | 21.5 | 0.0 |
PRIME, Programme for Improving Mental Health Care.
Note: All per cent figures are standardised to the age structure for the INDEPTH 2013 male and female populations of low- and middle-income countries; per cent figures from the community survey are also adjusted for the complex sampling design within each site.
There was evidence of variation in suicidality profiles between the pooled sample of community residents and the pooled sample of facility attendees (Table 3). A higher proportion of facility attendees reported suicidal ideation than community residents (10.3 and 8.1%, respectively). The proportion of reported suicide planning and suicide attempt was also significantly higher among the facility attendees than community residents. We did not find evidence of a difference in the proportion of discussion of or help seeking for suicide attempt between the two samples (results not presented).
Table 3.
Suicidality profile comparison of adult community residents and facility attendees, in PRIME implementation areas in Ethiopia, India and Nepal, 2013–2014
| Community residents (N = 6689) N (%) | Facility attendees (N = 3251) N (%) | Prevalence difference for facilities compared with communities (%) | 95% CI | |
|---|---|---|---|---|
| Suicidal ideation | 543 (8.1) | 334 (10.3) | +2.2* | +0.9 to +3.4 |
| Suicide planning | 123 (1.8) | 128 (3.9) | +2.1* | +1.4 to +2.8 |
| Suicide attempts | 82 (1.2) | 71 (2.2) | +1.0* | +0.4 to +1.5 |
PRIME, Programme for Improving Mental Health Care.
Note: Prevalence difference and 95% CI estimated using the two-sample test of proportions; *p ≤ 0.05.
Socioeconomic- and health-related correlates of suicidal ideation among facility attendees
In univariable analysis, there did not appear to be evidence of an association between age and suicidal ideation among facility attendees in Ethiopia, India or Uganda. This was not the case in Nepal and South Africa: for each 10-year increase in age, the prevalence of suicidal ideation was 12% lower (PR 0.88, 95% CI 0.79–0.98) in Nepal and 42% lower (PR 0.58, 95% CI 0.50–0.68) in South Africa. Female facility attendees were twice more likely as male attendees to report suicidal ideation in Ethiopia (PR 2.07, 95% 1.38–3.11) and Nepal (PR = 2.03, 95% CI 1.39–2.96) (see Table 4).
Table 4.
Sociodemographic- and health-related correlates of suicidal ideation among adult facility attendees in PRIME implementation areas in Ethiopia, India, Nepal, South Africa and Uganda, 2013–2014
| Ethiopia | India | Nepal | South Africa | Uganda | |
|---|---|---|---|---|---|
| PR (95% CI) | PR (95% CI) | PR (95% CI) | PR (95% CI) | PR (95% CI) | |
| Age (10 years) | 1.00 (0.88–1.13) | 1.04 (0.93–1.18) | 0.88 (0.79–0.98)** | 0.58 (0.50–0.68)** | 0.96 (0.80–1.16) |
| Sex | |||||
| Female | 2.07 (1.38–3.11)** | 1.47 (0.95–2.26)* | 2.03 (1.39–2.96)** | 1.20 (0.77–1.87) | 1.42 (0.85–2.40) |
| Male | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| aPR (95% CI) | aPR (95% CI) | aPR (95% CI) | aPR (95% CI) | aPR (95% CI) | |
| Education | |||||
| Primary | 1.27 (0.67–2.42) | 0.58 (0.34–0.97)** | 0.54 (0.37–0.79)** | 0.63 (0.38–1.06)* | 0.82 (0.43–1.56) |
| Secondary | 1.19 (0.74–1.94) | 0.39 (0.09–1.62) | 0.30 (0.20–0.45)** | 0.71 (0.38–1.35) | 0.54 (0.26–1.13) |
| Illiterate | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Relative economic status | |||||
| Lower | 1.00 | 1.00 | 1.00 | 1.00 | |
| Average | 0.78 (0.51–1.19) | 1.42 (0.58–3.49) | 0.58 (0.28–1.18) | 0.63 (0.25–1.56) | |
| Higher | 0.66 (0.42–1.03)* | 1.92 (0.85–4.30) | 0.68 (0.29–1.57) | 0.94 (0.40–2.22) | |
| PHQ8 score | 1.22 (1.19–1.26)** | 1.21 (1.16–1.25)** | 1.22 (1.19–1.25)** | 1.18 (1.15–1.21)** | 1.28 (1.22–1.33)** |
| AUDIT score | 1.05 (1.01–1.08)** | 1.09 (1.05–1.12)** | 1.09 (1.07–1.12)** | 1.04 (1.01–1.07)** | 1.10 (1.00–1.20)** |
| WHODAS score | 1.09 (1.07–1.10)** | 1.10 (1.06–1.13)** | 1.12 (1.09–1.15)** | 1.09 (1.06–1.12)** | |
PRIME, Programme for Improving Mental Health Care; AUDIT, Alcohol Use Disorders Identification Test; PHQ8, sum of items 1–8 on the nine-item Patient Health Questionnaire; WHODAS, 12-item World Health Organization Disability Assessment Schedule 2.0; PR, prevalence ratio; aPR, prevalence ratio, adjusted for age and sex.
PRs, 95% CI and p-values are estimated using log-Poisson regression with robust standard errors; *p < 0.10 **p < 0.05.
After adjustment for age and sex, there was some evidence of lower prevalence of suicidal ideation for adults with higher levels of educational attainment other than in Ethiopia (Table 4). There was a consistent negative association between relative economic status and suicidal ideation, except in India. Across all countries, the prevalence of suicidality increased by 18–28% for each unit increase on the PHQ screen for depression, and by 4–10% for each unit increase on the AUDIT screen for AUD, and, by 9–12% for each unit increase on the WHODAS.
Discussion
We found that one out of ten persons presenting at primary care facilities in five LMIC in sub-Saharan Africa and South Asia reported suicidal ideation within the past year, and 1 out of 45 reported attempted suicide in the same period. Among those with plans, at least 24% attempted suicide across all samples, reaching over 50% in Nepal, South Africa and Ethiopia. Within the community sample, we found that nearly 40% of people with plans attempted suicide in India and more than 70% in Nepal and Ethiopia. These data point towards important opportunities to engage in suicide risk reduction, especially in primary care. We also identified high levels of suicidal ideation and behaviours in the community samples. This stresses the importance of community-level suicide prevention and detection mechanisms, especially for persons not presenting to health care.
The results illustrate that the prevalence of suicidal behaviours is quite variable within and between the five LMIC. The range and variability of suicidal ideation and behaviours we observed is similar to a cross-national study on suicidal behaviour conducted in 17 countries based on population-based samples (Nock et al. 2008b), and in particular for the sub-set of LMIC (for suicidal ideation 3.5–11.1% in the community sample in our study and 3.1–12.4% in the study by Nock et al.). The aforementioned study by Nock et al. reports estimated lifetime prevalence. Our study advances this understanding by limiting to 12-months prevalence and focusing entirely on LMIC community and facility samples, where health attendees reported suicidal ideation ranges from 5.0% in Uganda to 14.8% in South Africa. From the perspective of developing services, data on recent suicidality is arguably more relevant than lifetime suicidality. Given that lifetime prevalence of suicidal behaviour is much higher than 12 months (Nock et al. 2008a), this finding suggests that the rates found in the current study are high compared with the data from the WHO World Mental Health Survey Initiative. A reason for this may be that the current study's community samples were taken from Ethiopia, Nepal and India – a combination of countries that represent low-resource communities more so than the mainly middle-income countries included in the WHO database.
Although prevalence varied among the five countries, the risk factors associated with suicidal behaviour were highly consistent between this study and other studies, both representing high-income countries and LMIC (Vijayakumar et al. 2005; Nock et al. 2008b). Risk factors included being female, younger age, symptoms of depression or AUDs and lower educational status associated with higher prevalence of reported suicidal ideation. Adults of higher economic status in the low-income countries (i.e. Ethiopia and Nepal) were less likely to report suicidal ideation, stressing the role that poverty may play in contributing to suicidal ideation. Previous studies have already demonstrated the association between neighbourhood poverty and suicide rates (Rehkopf & Buka, 2006) and suicidal ideation (Dupéré et al. 2009). This suggests that suicide prevention programmes can be directed at these known at-risk groups.
Suicidal ideation and planning were found to be higher among health care attendees compared with community residents in the three countries where this comparison was possible. A plausible explanation for this finding is that health attendees have physical health problems for which they are seeking treatment, increasing to the perceived burden of daily life and exacerbating mental distress (and vice versa). With regard to help seeking, there is a clear divide: in Ethiopia and South Africa some help seeking is reported, comparatively in Uganda, India and Nepal no help seeking was reported at all, in both community and facility samples.
Strengths and limitations
The current study has a number of strengths. This study uniquely compares multi-country suicidal behaviour profiles from both health attendee samples and community samples. The community surveys were large and representative samples. The study is, to the best of our knowledge, the first to include both the general population and a health care attendees. This is especially relevant given that suicide prevention, including both detection and management of suicidal behaviours, will likely need to take place in both health care and community settings.
There are also some limitations to be mentioned. First, there is possible selection bias for the facility surveys: we recruited participants from facility waiting rooms or upon exiting their clinical consultation. There may be systematic differences between those who were included in our studies and those who were eligible but were not included. These differences could have unpredictable effects on our findings. Second, there is possible survival selection bias: the sociodemographic- and health-related correlates of suicidality for suicide completers may differ from our still-living participants. Third, cross-sectional data cannot establish causation but the associations we found here can generate hypotheses and identify at-risk populations for intervention. Fourth, we used suicidal ideation as the outcome measure for establishing correlates rather than planning or action. This was done because any future programme aiming to reduce suicidal ideation will consequently impact planning and action. It is important to note that a substantial proportion of people with suicidal ideation do not attempt to commit suicide. However, due to the lack of statistical power we were not able to assess risk factors for people that attempted suicide. Finally, we used the facility sample rather than the community sample to identify correlates because suicidal ideation was much higher in clinic attendees and therefore we wanted to identify correlates given that future services will most likely be initiated from health facilities.
Implications for suicide risk reduction in LMIC
This study has important implications with regards to suicide prevention and intervention. First, systematically detecting suicidal behaviour within a health care setting seems worthwhile, given the higher prevalence of suicidality among health facility attendees. Actual help seeking was very low, which may be partly explained by the unavailability of mental health services, as well as the stigma that is often associated with suicidality. Therefore, primary care screening would be needed. In high-income countries, screening for depression and suicidal ideation and treatment of depression are evidence-based risk reduction strategies (Mann et al. 2005; Fleischmann et al. 2016). Moreover, primary care health facilities increasingly are a setting for mental health care in LMIC (Kigozi et al. 2015; Lund et al. 2015; Fekadu et al. 2016; Jordans et al. 2016; Petersen et al. 2016; Shidhaye et al. 2016).
To make an impact on the population level requires also working in the community (unless most suicidal people end up making contact with health care facilities), especially given the high rates of population-level suicidal ideation compared in our study, complimented with national-level efforts through regulations that impact access to methods of suicide (Mann et al. 2005). For persons not attending primary care services, community-level case-finding might be a relevant strategy to increase detection. A large group of people (ranging from 20 to 45% in the community sample, and between 18 and 51% in the facility sample) who reported attempted suicide had had discussions about the attempt with family or others close to them. It would therefore be worthwhile exploring ways in which the tendency to discuss suicidal attempts with people close to the suicidal person (in family or community) can be transferred into increased detection and help seeking, subsequently combined with increased recognition of the signs by health workers. There is evidence from high-income settings that physician education in recognition of depression reduces suicide rates (Mann et al. 2005). A procedure for proactive case-finding for people with mental health problems has been demonstrated as accurate and feasible (Jordans et al. 2015). Future directions could involve addressing the barriers to health workers conducting such screening, for example because of negative attitudes against suicidal behaviours or thinking it is illegal (Hagaman et al. 2016).
Second, above-mentioned two-staged system (i.e. community and primary care settings) of detection fits well with the strategy of integrating mental health into primary health care, advocated by WHO. At the health facility level, the WHO mental health Global Action Programme (mhGAP) Intervention Guidelines already explicitly include the assessment of, and response to, suicidal behaviour (WHO, 2010). In a study in multiple LMIC the provision of brief intervention and contact intervention demonstrated an 18-month follow-up with significantly fewer deaths from suicide in the intervention arm than the control arm (Fleischmann et al. 2008). In all of the study countries the mhGAP Guidelines (especially focusing on depression, AUD and psychoses) are being implemented and pilot tested. Furthermore, as the current study demonstrates the strong association between both depression and AUD with suicidality, adopting mhGAP Guidelines may contribute to directly reducing suicidality via treatment of both disorders or to improved detection because clinicians can assess anyone with depression/AUD for suicidality.
Third, related to the high variability between countries, is the need to design interventions based on local evidence, and hence the need to improve suicide monitoring and research, in order to develop targeted and locally relevant interventions. Only with detailed information on prevalence, demographic patterns, means of suicide can interventions be designed that are appropriate for the culture and context (Vijayakumar et al. 2016). The high rates in South Africa are an example, where suicidal ideation may be driven by an especially at-risk population. But also other factors that may explain variations should be explored, including cultural factors around disclosing suicidal thoughts, in turn influencing measurement issues.
Acknowledgements
The views in this manuscript do not necessarily reflect the views and policies of the UK government. The authors thank Dorothy Kizza, Anup Adhikari, Rajeev Mohan, Medhin Selamu, Vaibhav Murhar and the data collection teams. They thank Ashley Hagaman for her comments on an earlier draft of this manuscript.
Financial Support
This document is an output from the PRIME Research Programme Consortium, funded by the UK Department of International Development (DFID) for the benefit of developing countries. The author BK is supported by the National Institute of Mental Health (grant no. K01MH104310).
Conflict of Interest
None.
Availability of Data and Materials
The data supporting the findings will be made available through the PRIME program's website http://www.prime.uct.ac.za/.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
References
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG (2001). AUDIT: The Alcohol Use Disorders Identification Test Guidelines for Use in Primary Care. World Health Organization: Geneva. [Google Scholar]
- Borges G, Nock M, Haro Abad J, Hwang I, Sampson N, Alonso J, Andrade L, Angermeyer M, Beautrais A, Bromet EJ (2010). Twelve-month prevalence of and risk factors for suicide attempts in the World Health Organization World Mental Health Surveys. Journal of Clinical Psychiatry 71, 1617–1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Silva MJ, Rathod SD, Hanlon C, Breuer E, Chisholm D, Fekadu A, Jordans MJD, Kigozi F, Petersen I, Shidhaye R (2015). Evaluation of district mental healthcare plans: the PRIME consortium methodology. British Journal of Psychiatry bjp. bp. 114.153858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP, Angermeyer MC, Bernert S, de Girolamo G, Morosini P, Polidori G, Kikkawa T, Kawakami N, Ono Y, Takeshima T, Uda H, Karam EG, Fayyad JA, Karam AN, Mneimneh ZN, Medina-Mora ME, Borges G, Lara C, de Graaf R, Ormel J, Gureje O, Shen Y, Huang Y, Zhang M, Alonso J, Haro JM, Vilagut G, Bromet EJ, Gluzman S, Webb C, Kessler RC, Merikangas KR, Anthony JC, Von Korff MR, Wang PS, Brugha TS, Aguilar-Gaxiola S, Lee S, Heeringa S, Pennell BE, Zaslavsky AM, Ustun TB, Chatterji S, Consortium. WWMHS. (2004). Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA 291, 2581–2590. [DOI] [PubMed] [Google Scholar]
- Dupéré V, Leventhal T, Lacourse E (2009). Neighborhood poverty and suicidal thoughts and attempts in late adolescence. Psychological Medicine 39, 1295–1306. [DOI] [PubMed] [Google Scholar]
- Fekadu A, Hanlon C, Medhin G, Alem A, Selamu M, Giorgis TW, Shibre T, Teferra S, Tegegn T, Breuer E (2016). Development of a scalable mental healthcare plan for a rural district in Ethiopia. British Journal of Psychiatry 208, s4–s12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleischmann A, Bertolote JM, Wasserman D, De Leo D, Bolhari J, Botega NJ, De Silva D, Phillips M, Vijayakumar L, Värnik A, Schlebusch L, Thanh HT. (2008). Effectiveness of brief intervention and contact for suicide attempters: a randomized controlled trial in five countries. Bulletin of the World Health Organization 86, 703–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleischmann A, Arensman E, Berman A, Carli V, De Leo D, Hadlaczky G, Howlader S, Vijayakumar L, Wasserman D, Saxena S (2016). Overview evidence on interventions for population suicide with an eye to identifying best-supported strategies for LMICs. Global Mental Health p. e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagaman AK, Maharjan U, Kohrt BA (2016). Suicide surveillance and health systems in Nepal: a qualitative and social network analysis. International Journal of Mental Health Systems 10, 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanlon C, Luitel NP, Kathree T, Murhar V, Shrivasta S, Medhin G, Ssebunnya J, Fekadu A, Shidhaye R, Petersen I, Jordans MJD, Kigozi F, Thornicroft G, Patel V, Tomlinson M, Lund C, Breuer E, De Silva M, Prince M (2014). Challenges and opportunities for implementing integrated mental health care: a district level situation analysis from five low- and middle-income countries. PLoS ONE 9, e88437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordans MJD, Luitel NP, Tomlinson M, Komproe IH (2013). Setting priorities for mental health care in Nepal: a formative study. BMC Psychiatry 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordans MJD, Kohrt BA, Luitel NP, Komproe IH, Lund C (2015). Accuracy of pro-active case finding for mental disorders by community informants in Nepal. British Journal of Psychiatry 207, 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordans MJD, Luitel NP, Pokhrel P, Patel V (2016). Development and pilot testing of a mental healthcare plan in Nepal. British Journal of Psychiatry 208, s21–s28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kigozi FN, Kizza D, Nakku J, Ssebunnya J, Ndyanabangi S, Nakiganda B, Lund C, Patel V (2015). Development of a district mental healthcare plan in Uganda. British Journal of Psychiatry bjp. bp. 114.153742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW (2001). The PHQ-9. Journal of General Internal Medicine 16, 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund C, Tomlinson M, De Silva M, Fekadu A, Shidhaye R, Jordans MJD, Petersen I, Bhana A, Kigozi F, Prince M, Thornicroft G, Hanlon C, Kakuma R, McDaid D, Saxena S, Chisholm D, Raja S, Kippen-Wood S, Honikman S, Fairall L, Patel V (2012). PRIME: a programme to reduce the treatment gap for mental disorders in five low- and middle-income countries. PLoS Medicine 9, e1001359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund C, Tomlinson M, Patel V (2015). Integration of mental health into primary care in low- and middle-income countries: the PRIME mental healthcare plans. British Journal of Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann JJ, Apter A, Bertolote JM, Beautrais A, Currier D, Haas A, Hegerl U, Lonnqvist J, Malone K, Marusic A (2005). Suicide prevention strategies: a systematic review. JAMA 294, 2064–2074. [DOI] [PubMed] [Google Scholar]
- Milner A, Page A, Lamontagne AD (2014). Cause and effect in studies on unemployment, mental health and suicide: a meta-analytic and conceptual review. Psychological Medicine 44, 909–917. [DOI] [PubMed] [Google Scholar]
- Ng N, Van Minh H, Juvekar S, Razzaque A, Bich TH, Kanungsukkasem U, Ashraf A, Ahmed SM, Soonthornthada K (2009). Using the INDEPTH HDSS to build capacity for chronic non-communicable disease risk factor surveillance in low and middle income countries. Global Health Action 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Borges G, Bromet E, Cha C, Kessler R, Lee S (2008a). Suicide and suicidal behavior. Epidemiologic Reviews 30, 133–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, Bruffaerts R, Chiu WT, De Girolamo G, Gluzman S (2008b). Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. British Journal of Psychiatry 192, 98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ojagbemi A, Oladeji BD, Abiona T, Gureje O (2013). Suicidal behaviour in old age-results from the Ibadan Study of Ageing. BMC Psychiatry 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oladeji BD, Gureje O (2011). Parental mental disorders and suicidal behavior in the Nigerian survey of mental health and well-being. Archives of Suicide Research 15, 372–383. [DOI] [PubMed] [Google Scholar]
- Petersen I, Fairall L, Bhana A, Kathree T, Selohilwe O, Brooke-Sumner C, Faris G, Breuer E, Sibanyoni N, Lund C, Patel V (2016). Integrating mental health into chronic care in South Africa: the development of a district mental healthcare plan. British Journal of Psychiatry 208, s29–s39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rathod SD, De Silva MJ, Ssebunnya J, Breuer E, Murhar V, Luitel NP, Medhin G, Kigozi F, Shidhaye R, Fekadu A (2016). Treatment contact coverage for probable depressive and probable alcohol use disorders in four low-and middle-income country districts: the PRIME cross-sectional community surveys. PLoS ONE 11, e0162038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehkopf DH, Buka SL (2006). The association between suicide and the socio-economic characteristics of geographical areas: a systematic review. Psychological Medicine 36, 145–157. [DOI] [PubMed] [Google Scholar]
- Robins LN, Wing J, Wittchen HU, Helzer JE, Babor TF, Burke J, Farmer A, Jablenski A, Pickens R, Regier DA (1988). The Composite International Diagnostic Interview: an epidemiologic instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Archives of General Psychiatry 45, 1069–1077. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De La Fuente JR, Grant M (1993). Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction 88, 791–804. [DOI] [PubMed] [Google Scholar]
- Shidhaye R, Shrivastava S, Murhar V, Samudre S, Ahuja S, Ramaswamy R, Patel V (2016). Development and piloting of a plan for integrating mental health in primary care in Sehore district, Madhya Pradesh, India. British Journal of Psychiatry 208, s13–s20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Streatfield PK, Khan WA, Bhuiya A, Alam N, Sié A, Soura AB, Bonfoh B, Ngoran EK, Weldearegawi B, Jasseh M (2014). Cause-specific mortality in Africa and Asia: evidence from INDEPTH health and demographic surveillance system sites. Global Health Action 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Üstün TB, Kostanjsek N, Chatterji S, Rehm J (2010). Measuring Health and Disability: Manual for WHO Disability Assessment Schedule WHODAS 2.0. World Health Organization: Geneva. [Google Scholar]
- Värnik P (2012). Suicide in the world. International Journal of Environmental Research and Public Health 9, 760–771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vijayakumar L, Nagaraj K, Pirkis J, Whiteford HA (2005). Suicide in developing countries: frequency, distribution, and association with socioeconomic indicators. Crisis 26, 104–111. [DOI] [PubMed] [Google Scholar]
- Vijayakumar L, Phillips MR, Silverman MM, Gunnell D, Carli V (2016). Suicide In Disease Control Priorities: Mental, Neurological, and Substance Abuse Disorders. (ed. Patel V, Chisholm D, Dua T, Laxminarayan R and Medina-Mora ME), pp. 163–181. World Bank: Washington. [Google Scholar]
- Vyas S, Kumaranayake L (2006). Constructing socio-economic status indices: how to use principal components analysis. Health Policy and Planning 21, 459–468. [DOI] [PubMed] [Google Scholar]
- WHO (2010). mhGAP Intervention Guide for Mental, Neurological and Substance use Disorders in Non-Specialized Health Settings. World Health Organization: Geneva. [PubMed] [Google Scholar]
- WHO (2012). Public Health Action for the Prevention of Suicide: a Framework. World Health Organization: Geneva. [Google Scholar]
- WHO (2014). Preventing Suicide: A Global Imperative. World Health Organization: Geneva. [Google Scholar]
- Zou G (2004). A modified Poisson regression approach to prospective studies with binary data. American Journal of Epidemiology 159, 702–706. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting the findings will be made available through the PRIME program's website http://www.prime.uct.ac.za/.