Abstract
Background
Activation of inflammatory pathways plays an important contributory role in coronary plaque instability and subsequent rupture, which can lead to the development of acute coronary syndrome (ACS). Elevated levels of serum inflammatory markers such as C-reactive protein (CRP) represent independent risk factors for further cardiovascular events. Recent evidence indicates that in addition to lowering cholesterol levels, statins also decrease levels of inflammatory markers. Previous controlled clinical trials reporting the positive effects of statins in participants with ACS were designed for very early secondary prevention. To our knowledge, no controlled trials have evaluated the potential benefits of statin therapy, beginning immediately at the time of hospital admission. A previous pilot study performed by our group focused on early initiation of cerivastatin therapy. We demonstrated a highly significant reduction in levels of inflammatory markers (CRP and interleukin-6). Based on these preliminary findings, we are conducting a clinical trial to evaluate the efficacy of another statin, fluvastatin, as an early intervention in patients with ACS.
Methods
The FACS-trial (Fluvastatin in the therapy of Acute Coronary Syndrome) is a multicenter, randomized, double-blind, placebo-controlled study evaluating the effects of fluvastatin therapy initiated at the time of hospital admission. The study will enroll 1,000 participants admitted to hospital for ACS (both with and without ST elevation). The primary endpoint for the study is the influence of fluvastatin therapy on levels of inflammatory markers (CRP and interleukin-6) and on pregnancy associated plasma protein A (PAPP-A). A combined secondary endpoint is 30-day and one-year occurrence of death, nonfatal myocardial infarction, recurrent symptomatic ischemia, urgent revascularization, and cardiac arrest.
Conclusion
The primary objective of the FACS trial is to demonstrate that statin therapy, when started immediately after hospital admission for ACS, results in reduction of inflammation and improvement of prognosis. This study may contribute to new knowledge regarding therapeutic strategies for patients suffering from ACS and may offer additional clinical indications for the use of statins.
Keywords: statin, fluvastatin, acute coronary syndrome, C-reactive protein, interleukin 6, pregnancy-associated plasma protein A
Background
During the past decade, inflammation has often been cited as a major factor in the pathogenesis of atherosclerosis and its clinical sequelae, including ischemic heart disease. It was found that traditional risk factors such as hypertension, hypercholesterolemia, diabetes, and smoking could not fully account for the development of coronary stenosis in all patients suffering from ischemic heart disease. Intensive study of the pathogenesis of coronary plaque development and rupture led to the hypothesis that inflammatory factors contribute to this process. For example, T-lymphocytes and monocytes/macrophages have been repeatedly identified in plaque lesions; elevated levels of acute phase proteins (C-reactive protein, serum amyloid A, fibrinogen), cytokines (interleukin 1, interleukin 6, interleukin 8, tumor necrosis factor), and adhesive molecules (ICAM-1) correlate with the worse prognoses in patients with ischemic heart disease [1-5]. Furthermore, the increased level of C-reactive protein (CRP) is now widely recognized as being an independent risk factor for a higher incidence of non-fatal and fatal coronary events in patients with chronic ischemic heart disease and acute coronary syndromes [6-9].
Activation of the immune reaction in acute ischemic heart disease likely derives from: (i) pathological events occurring in the arterial wall where the lesion develops, leading to plaque rupture and the subsequent clinical consequences and (ii) myocardial necrosis, which triggers processes involved in removal of the necrotic mass and replacement with scar tissue. Whereas activation of plaque inflammation (as noted above) serves as a marker for plaque instability, elevation of inflammatory factors from the second source correlates with the extent of myocardial necrosis.
Statins, 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors, lower cholesterol levels by decreasing the production of low-density lipoproteins (LDL) and up-regulating the expression of the LDL-receptor. These drugs are widely used in patients with hypercholesterolemia for primary and secondary prevention of coronary artery disease because of their efficacy in reducing cardiovascular morbidity and mortality [10-12]. Surprisingly, statin therapy also improves prognosis in patients with normal or low cholesterol levels[13]. Evaluation of the non-lipid effects of statins reveals a possible beneficial effect mediated by the reduction of inflammatory markers, namely, CRP. This effect seems to be independent of cholesterol level [1,14]. The mechanisms by which statins inhibit inflammation are not fully understood. It has been reported that they suppress production of monocyte chemotactic protein-1 (MCP-1) [15], as well as matrix metalloproteinases (MMPs) [5,16,17]. Statins also decrease macrophage expression of soluble ICAM-1 and secretion of IL-1, IL-6, TNF-alpha [5,18-23].
A number of large clinical trials have been designed to investigate the effect of statins in treating acute coronary syndromes (ACS) [24-30] Because patients in these studies were randomized later after being admitted to hospital, often after they had been clinically stabilized, these randomized, double blind trials focused more on early secondary prevention, as opposed to evaluating earlier therapy to target plaque instability in ACS. Furthermore, broad exclusion criteria in some of these trials, including coronary intervention during the index hospitalization visit, deter from the generalizability of their results to the majority of patients treated according to current clinical practice [24]. Nevertheless, these studies have shown promising results, despite the fact that the statins were administered after activation of the immune mechanisms was completed and after the inflammatory reaction was already fully developed.
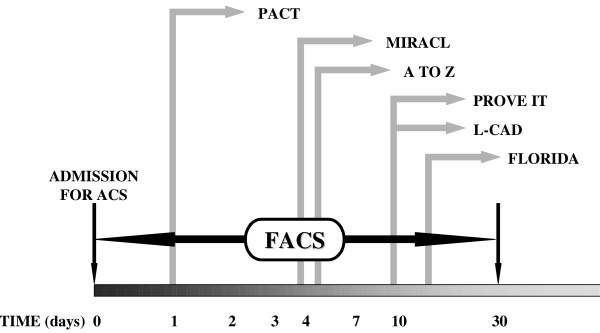
Little information is available on the efficacy of statins in treating ACS at an earlier phase, i.e., at the time of hospital admission. Recently published data from experimental projects [31-35] and from small clinical trials [36-38]) have shown a positive effect of statins when they are administered in the acute phase of ACS. Our preliminary results with cerivastatin treatment in patients with non-ST segment elevation ACS starting at the time of hospital admission have shown the safety of such a strategy as well as a decrease in inflammatory markers (CRP, IL-6) by 24-hour follow-up, as compared to the non-treated group [39]. Based on these pilot data, we are conducting a clinical trial to evaluate fluvastatin therapy administered to patients with ACS immediately at the time of admission (Figure 1).
Figure 1.
Design of the FACS trial in comparison to other trials evaluating statins in ACS patients. In the Pravastatin in Acute Coronary Treatment (PACT) trial statin, therapy was initiated within 24 hours of onset of ACS. In the Myocardial Ischemia Reduction With Aggressive Cholesterol Lowering (MIRACL) trial, patients were randomized 24 to 96 hours after ACS. In the Z-phase of the A-to-Z trial, simvastatin therapy was initiated within 5 days of the onset of ACS, after clinical stabilization. In the Pravastatin or Atorvastatin Evaluation and Infection Therapy (PROVE IT) trial, patients were randomized up to 10 days after ACS. In the Lipid-Coronary Artery Disease (L-CAD) trial, statin therapy was initiated up to ten days following the onset of ACS. In the Fluvastatin on Risk Diminishing After Acute Myocardial Infarction (FLORIDA) trial, patients were randomized up to two weeks after ACS.
Methods
Objectives
The objectives of the FACS trial are to determine:
(i) Whether initiation of fluvastatin therapy in patients with ACS immediately after hospital admission decreases levels of CRP, IL-6, and pregnancy-associated plasma protein A/ proform eosinophilic major basic protein (PAPP-A/proMBP), which represent indirect markers of plaque instability and indicators of poor prognosis; and
(ii) Whether initiation of fluvastatin therapy decreases the occurrence of ischemic events (death, nonfatal myocardial infarction, recurrent symptomatic ischemia, urgent revascularization, cardiac arrest) in patients with ACS.
Overview
This is a prospective, 30-day, multicenter, randomized, double-blind, placebo-controlled study in 1,000 patients with ACS. Patients are enrolled from 10 sites in the Czech Republic and Slovakia. At each institution, the protocol and the informed consent form are reviewed and approved by the institutional ethics committee before study initiation. Eligible patients are randomized to one of two treatment groups immediately after hospital admission (within one hour). One group is assigned 80 mg/day fluvastatin (Lescol XL), with the other group receiving placebo. Participants are followed on an intention-to-treat basis. The primary endpoint relates to levels of CRP, IL-6, and PAPP-A/proMBP. The secondary endpoint is the occurrence of an ischemic event, defined as death, nonfatal myocardial infarction (MI), recurrent symptomatic myocardial ischemia, cardiac arrest with resuscitation, and urgent revascularization.
Study population
This study will enroll high-risk patients admitted to the hospital for ACS. Eligible patients with ST elevation ACS must have resting chest pain less than 12 hours before admission and either ≥ 1 mm ST-segment elevation in 2 or more continuous leads or new left bundle branch block on ECG. Those with non-ST elevation ACS must have resting chest pain during the previous 48 hours and either ≥ 1 mm ST segment depression or negative T waves in 2 or more continuous leads.
Exclusion criteria
Subjects are excluded from study participation if they are <18 years of age or if they have concomitant active liver disease or persistent elevation of transaminases (> 3 times the upper limit of normal), a history of lipid-lowering therapy less than 30 days before the index event or a known allergy to fluvastatin or to any additives present in the drug. Other exclusions include inability to ingest oral medication, unwillingness to be followed for the duration of the study, muscle disease (e.g., myositis), and creatine kinase ≥ 5 times the upper limit of normal due to conditions other than myocardial infarction. Women of childbearing potential who are pregnant, nursing or who are not using effective contraception will also be excluded.
Follow-up
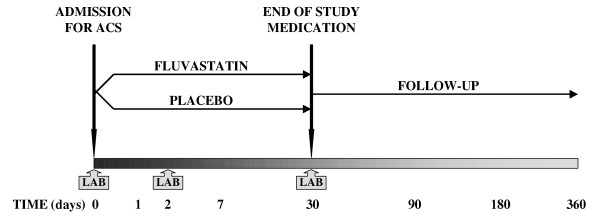
After obtaining informed consent, blood samples are taken from patients for examination of inflammatory markers (CRP, IL-6, and PAPP-A/proMBP). Patients are then randomized to 80 mg fluvastatin (Lescol XL) or to placebo immediately p.o. Medical history and physical examination, standard 12-lead ECG, blood lipid profile, and liver function tests are performed as part of participants' routine admission care. Fluvastatin 80 mg or placebo are then taken once daily for 30 days. Follow-up measurement of inflammatory markers (CRP, IL-6, and PAPP-A/proMBP) is performed on day 2 and day 30. Follow-up visits are scheduled at pre-discharge, day 30, 90, 180 and 360. Blood liver function and creatine kinase tests are done at pre-discharge and at the 30-day visits. At day 30, the lipid profile is also examined, and study medication is withdrawn. All visits include assessment of ischemic events and recent medical history since the last follow-up visit, including use of concomitant medications (Figure 2).
Figure 2.
Study design of the FACS Trial. Patients admitted with acute coronary syndrome (ACS) are randomized to either fluvastatin 80 mg or placebo for 30 days. Patients are then followed for one year. Assessments of CRP, IL-6, and PAPP-A/proMBP (LAB) are performed at admission, on day 2, and day 30.
During follow-up, no specific recommendations are made with respect to diagnostic and therapeutic strategy, except that other lipid-lowering drugs should not be given after randomization until day 30. All management decisions are left to the discretion of each patient's treating physician.
Safety
The principal safety concerns are hepatic dysfunction and myopathy. If a patient's serum transaminase levels are persistently elevated to > 3 times the upper limit of normal, the study medication is discontinued. Similarly, study medication is stopped if the patient develops muscle pain, weakness, or tenderness in association with a serum creatine kinase level > 10 times the upper limit of normal.
Sample size
The trial will enroll 1,000 patients, to ensure adequate power to detect significant treatment benefit of 80 mg fluvastatin (Lescol XL) with respect to the primary endpoint (30-day decrease of CRP and IL-6) and the combined secondary endpoint (death, nonfatal myocardial infarction, recurrent symptomatic ischemia, urgent revascularization, cardiac arrest). With 500 patients randomized to 80 mg fluvastatin (Lescol XL) and 500 patients randomized to placebo, the trial will have more than 80 % power to detect a decrease in CRP level by 1.36 μg/L and a decrease in IL-6 level by 1.09 ng/L. Calculations are based on a two-sample t-test. The estimated combined secondary endpoint rate at 30-days is 20 %. Based on comparison of proportions with p = 0.05 test significance, the trial will have more than 80 % power to detect a 33% decrease in the combined secondary endpoint.
Conclusion
The FACS trial is the first multicenter, randomized, double-blind, placebo-controlled trial investigating the effects of fluvastatin therapy started immediately after hospital admission in patients with ACS.
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
PO has made substantial contributions to the concept and design of the trial and has drafted the manuscript. DA, PH, JVej, JK, MMat, and JVes have made substantial contributions to the concept and design of the study and have been involved in revising the manuscript. PB, MW, OA, JS, EN, FH, MR, and JC have been involved in the acquisition and analysis of data. MMac and MK have given final approval of the version to be published.
Acknowledgments
Acknowledgements
Laboratory investigation of CRP, IL-6, and PAPP-A/proMBP is supported by a grant from the Czech Ministry of Health, No. 00000064203. Study medication and clinical monitoring were kindly sponsored by Novartis Pharma CR s.r.o.
Contributor Information
Petr Ostadal, Email: ostadal@yahoo.com.
David Alan, Email: david.alan@seznam.cz.
Petr Hajek, Email: petr_hajek@hotmail.com.
Jiri Vejvoda, Email: jirkavejvoda@seznam.cz.
Martin Mates, Email: mates@bon.cz.
Peter Blasko, Email: blaskopeter@hotmail.com.
Josef Veselka, Email: veselka.josef@seznam.cz.
Milan Kvapil, Email: milan.kvapil@lfmotol.cuni.cz.
Jiri Kettner, Email: jiri.kettner@medicon.cz.
Martin Wiendl, Email: mawi@medicon.cz.
Ondrej Aschermann, Email: ondrej.aschermann@homolka.cz.
Josef Slaby, Email: slaby.josef@post.cz.
Eduard Nemecek, Email: eduardn@email.cz.
Frantisek Holm, Email: frantisek.holm@nemlib.cz.
Marek Rac, Email: marekrac@orangemail.sk.
Milan Macek, Email: milan.macek@lfmotol.cuni.cz.
Jana Cepova, Email: Janacepova@seznam.cz.
References
- Whicher J, Biasucci L, Rifai N. Inflammation, the acute phase response and atherosclerosis. Clin Chem Lab Med. 1999;37(5):495–503. doi: 10.1515/CCLM.1999.080. [DOI] [PubMed] [Google Scholar]
- Barath P, Fishbein MC, Cao J, Berenson J, Helfant RH, Forrester JS. Detection and localization of tumor necrosis factor in human atheroma. Am J Cardiol. 1990;65(5):297–302. doi: 10.1016/0002-9149(90)90291-8. [DOI] [PubMed] [Google Scholar]
- Serneri GG, Abbate R, Gori AM, Attanasio M, Martini F, Giusti B, Dabizzi P, Poggesi L, Modesti PA, Trotta F, et al. Transient intermittent lymphocyte activation is responsible for the instability of angina. Circulation. 1992;86(3):790–797. doi: 10.1161/01.cir.86.3.790. [DOI] [PubMed] [Google Scholar]
- Biasucci LM, Vitelli A, Liuzzo G, Altamura S, Caligiuri G, Monaco C, Rebuzzi AG, Ciliberto G, Maseri A. Elevated levels of interleukin-6 in unstable angina. Circulation. 1996;94(5):874–877. doi: 10.1161/01.cir.94.5.874. [DOI] [PubMed] [Google Scholar]
- Blake GJ, Ridker PM. Novel clinical markers of vascular wall inflammation. Circ Res. 2001;89(9):763–771. doi: 10.1161/hh2101.099270. [DOI] [PubMed] [Google Scholar]
- Morrow DA, Rifai N, Antman EM, Weiner DL, McCabe CH, Cannon CP, Braunwald E. C-reactive protein is a potent predictor of mortality independently of and in combination with troponin T in acute coronary syndromes: a TIMI 11A substudy. Thrombolysis in Myocardial Infarction. J Am Coll Cardiol. 1998;31(7):1460–1465. doi: 10.1016/S0735-1097(98)00136-3. [DOI] [PubMed] [Google Scholar]
- Haverkate F, Thompson SG, Pyke SD, Gallimore JR, Pepys MB. Production of C-reactive protein and risk of coronary events in stable and unstable angina. European Concerted Action on Thrombosis and Disabilities Angina Pectoris Study Group. Lancet. 1997;349(9050):462–466. doi: 10.1016/S0140-6736(96)07591-5. [DOI] [PubMed] [Google Scholar]
- Liuzzo G, Biasucci LM, Gallimore JR, Grillo RL, Rebuzzi AG, Pepys MB, Maseri A. The prognostic value of C-reactive protein and serum amyloid a protein in severe unstable angina. N Engl J Med. 1994;331(7):417–424. doi: 10.1056/NEJM199408183310701. [DOI] [PubMed] [Google Scholar]
- Rifai N, Ridker PM. High-sensitivity C-reactive protein: a novel and promising marker of coronary heart disease. Clin Chem. 2001;47(3):403–411. [PubMed] [Google Scholar]
- Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S) Lancet. 1994;344(8934):1383–1389. doi: 10.1016/S0140-6736(94)92521-6. [DOI] [PubMed] [Google Scholar]
- Sacks FM, Pfeffer MA, Moye LA, Rouleau JL, Rutherford JD, Cole TG, Brown L, Warnica JW, Arnold JM, Wun CC, Davis BR, Braunwald E. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N Engl J Med. 1996;335(14):1001–1009. doi: 10.1056/NEJM199610033351401. [DOI] [PubMed] [Google Scholar]
- Shepherd J, Cobbe SM, Ford I, Isles CG, Lorimer AR, MacFarlane PW, McKillop JH, Packard CJ. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. N Engl J Med. 1995;333(20):1301–1307. doi: 10.1056/NEJM199511163332001. [DOI] [PubMed] [Google Scholar]
- Ridker PM, Rifai N, Pfeffer MA, Sacks FM, Moye LA, Goldman S, Flaker GC, Braunwald E. Inflammation, pravastatin, and the risk of coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events (CARE) Investigators. Circulation. 1998;98(9):839–844. doi: 10.1161/01.cir.98.9.839. [DOI] [PubMed] [Google Scholar]
- Ridker PM, Rifai N, Clearfield M, Downs JR, Weis SE, Miles JS, Gotto AMJ. Measurement of C-reactive protein for the targeting of statin therapy in the primary prevention of acute coronary events. N Engl J Med. 2001;344(26):1959–1965. doi: 10.1056/NEJM200106283442601. [DOI] [PubMed] [Google Scholar]
- Romano M, Diomede L, Sironi M, Massimiliano L, Sottocorno M, Polentarutti N, Guglielmotti A, Albani D, Bruno A, Fruscella P, Salmona M, Vecchi A, Pinza M, Mantovani A. Inhibition of monocyte chemotactic protein-1 synthesis by statins. Lab Invest. 2000;80(7):1095–1100. doi: 10.1038/labinvest.3780115. [DOI] [PubMed] [Google Scholar]
- Ikeda U, Shimpo M, Ohki R, Inaba H, Takahashi M, Yamamoto K, Shimada K. Fluvastatin inhibits matrix metalloproteinase-1 expression in human vascular endothelial cells. Hypertension. 2000;36(3):325–329. doi: 10.1161/01.hyp.36.3.325. [DOI] [PubMed] [Google Scholar]
- Fukumoto Y, Libby P, Rabkin E, Hill CC, Enomoto M, Hirouchi Y, Shiomi M, Aikawa M. Statins alter smooth muscle cell accumulation and collagen content in established atheroma of watanabe heritable hyperlipidemic rabbits. Circulation. 2001;103(7):993–999. doi: 10.1161/01.cir.103.7.993. [DOI] [PubMed] [Google Scholar]
- Brull DJ, Sanders J, Rumley A, Lowe GD, Humphries SE, Montgomery HE. Statin therapy and the acute inflammatory response after coronary artery bypass grafting. Am J Cardiol. 2001;88(4):431–433. doi: 10.1016/S0002-9149(01)01696-4. [DOI] [PubMed] [Google Scholar]
- Niwa S, Totsuka T, Hayashi S. Inhibitory effect of fluvastatin, an HMG-CoA reductase inhibitor, on the expression of adhesion molecules on human monocyte cell line. Int J Immunopharmacol. 1996;18(11):669–675. doi: 10.1016/S0192-0561(96)00068-9. [DOI] [PubMed] [Google Scholar]
- Ikeda U, Shimada K. Statins and monocytes. Lancet. 1999;353(9169):2070. doi: 10.1016/S0140-6736(05)77885-5. [DOI] [PubMed] [Google Scholar]
- Rosenson RS, Tangney CC, Casey LC. Inhibition of proinflammatory cytokine production by pravastatin. Lancet. 1999;353(9157):983–984. doi: 10.1016/S0140-6736(98)05917-0. [DOI] [PubMed] [Google Scholar]
- Ferro D, Parrotto S, Basili S, Alessandri C, Violi F. Simvastatin inhibits the monocyte expression of proinflammatory cytokines in patients with hypercholesterolemia. J Am Coll Cardiol. 2000;36(2):427–431. doi: 10.1016/S0735-1097(00)00771-3. [DOI] [PubMed] [Google Scholar]
- Bustos C, Hernandez-Presa MA, Ortego M, Tunon J, Ortega L, Perez F, Diaz C, Hernandez G, Egido J. HMG-CoA reductase inhibition by atorvastatin reduces neointimal inflammation in a rabbit model of atherosclerosis. J Am Coll Cardiol. 1998;32(7):2057–2064. doi: 10.1016/S0735-1097(98)00487-2. [DOI] [PubMed] [Google Scholar]
- Schwartz GG, Olsson AG, Ezekowitz MD, Ganz P, Oliver MF, Waters D, Zeiher A, Chaitman BR, Leslie S, Stern T. Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: the MIRACL study: a randomized controlled trial. Jama. 2001;285(13):1711–1718. doi: 10.1001/jama.285.13.1711. [DOI] [PubMed] [Google Scholar]
- Den Hartog FR, Van Kalmthout PM, Van Loenhout TT, Schaafsma HJ, Rila H, Verheugt FW. Pravastatin in acute ischaemic syndromes: results of a randomised placebo-controlled trial. Int J Clin Pract. 2001;55(5):300–304. [PubMed] [Google Scholar]
- Liem AH, van Boven AJ, Veeger NJ, Withagen AJ, Robles de Medina RM, Tijssen JG, van Veldhuisen DJ. Effect of fluvastatin on ischaemia following acute myocardial infarction: a randomized trial. Eur Heart J. 2002;23(24):1931–1937. doi: 10.1053/euhj.2002.3291. [DOI] [PubMed] [Google Scholar]
- Arntz HR, Agrawal R, Wunderlich W, Schnitzer L, Stern R, Fischer F, Schultheiss HP. Beneficial effects of pravastatin (+/-colestyramine/niacin) initiated immediately after a coronary event (the randomized Lipid-Coronary Artery Disease [L-CAD] Study) Am J Cardiol. 2000;86(12):1293–1298. doi: 10.1016/S0002-9149(00)01230-3. [DOI] [PubMed] [Google Scholar]
- Cannon CP, Braunwald E, McCabe CH, Rader DJ, Rouleau JL, Belder R, Joyal SV, Hill KA, Pfeffer MA, Skene AM. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004;350(15):1495–1504. doi: 10.1056/NEJMoa040583. [DOI] [PubMed] [Google Scholar]
- de Lemos JA, Blazing MA, Wiviott SD, Lewis EF, Fox KA, White HD, Rouleau JL, Pedersen TR, Gardner LH, Mukherjee R, Ramsey KE, Palmisano J, Bilheimer DW, Pfeffer MA, Califf RM, Braunwald E. Early intensive vs a delayed conservative simvastatin strategy in patients with acute coronary syndromes: phase Z of the A to Z trial. Jama. 2004;292(11):1307–1316. doi: 10.1001/jama.292.11.1307. [DOI] [PubMed] [Google Scholar]
- Thompson PL, Meredith I, Amerena J, Campbell TJ, Sloman JG, Harris PJ. Effect of pravastatin compared with placebo initiated within 24 hours of onset of acute myocardial infarction or unstable angina: the Pravastatin in Acute Coronary Treatment (PACT) trial. Am Heart J. 2004;148(1):e2. doi: 10.1016/S0002-8703(04)00315-1. [DOI] [PubMed] [Google Scholar]
- Lefer AM, Campbell B, Shin YK, Scalia R, Hayward R, Lefer DJ. Simvastatin preserves the ischemic-reperfused myocardium in normocholesterolemic rat hearts. Circulation. 1999;100(2):178–184. doi: 10.1161/01.cir.100.2.178. [DOI] [PubMed] [Google Scholar]
- Ueda Y, Kitakaze M, Komamura K, Minamino T, Asanuma H, Sato H, Kuzuya T, Takeda H, Hori M. Pravastatin restored the infarct size-limiting effect of ischemic preconditioning blunted by hypercholesterolemia in the rabbit model of myocardial infarction. J Am Coll Cardiol. 1999;34(7):2120–2125. doi: 10.1016/S0735-1097(99)00440-4. [DOI] [PubMed] [Google Scholar]
- Lefer DJ, Scalia R, Jones SP, Sharp BR, Hoffmeyer MR, Farvid AR, Gibson MF, Lefer AM. HMG-CoA reductase inhibition protects the diabetic myocardium from ischemia-reperfusion injury. Faseb J. 2001;15(8):1454–1456. doi: 10.1096/fj.00-0819fje. [DOI] [PubMed] [Google Scholar]
- Di Napoli P, Antonio Taccardi A, Grilli A, Spina R, Felaco M, Barsotti A, De Caterina R. Simvastatin reduces reperfusion injury by modulating nitric oxide synthase expression: an ex vivo study in isolated working rat hearts. Cardiovasc Res. 2001;51(2):283–293. doi: 10.1016/S0008-6363(01)00306-6. [DOI] [PubMed] [Google Scholar]
- Hayashidani S, Tsutsui H, Shiomi T, Suematsu N, Kinugawa S, Ide T, Wen J, Takeshita A. Fluvastatin, a 3-hydroxy-3-methylglutaryl coenzyme a reductase inhibitor, attenuates left ventricular remodeling and failure after experimental myocardial infarction. Circulation. 2002;105(7):868–873. doi: 10.1161/hc0702.104164. [DOI] [PubMed] [Google Scholar]
- Heeschen C, Hamm CW, Laufs U, Snapinn S, Bohm M, White HD. Withdrawal of statins increases event rates in patients with acute coronary syndromes. Circulation. 2002;105(12):1446–1452. doi: 10.1161/01.CIR.0000012530.68333.C8. [DOI] [PubMed] [Google Scholar]
- Walter DH, Fichtlscherer S, Britten MB, Auch-Schwelk W, Schachinger V, Zeiher AM. Benefits of immediate initiation of statin therapy following successful coronary stent implantation in patients with stable and unstable angina pectoris and Q-wave acute myocardial infarction. Am J Cardiol. 2002;89(1):1–6. doi: 10.1016/S0002-9149(01)02153-1. [DOI] [PubMed] [Google Scholar]
- Bybee KA, Wright RS, Williams BA, Murphy JG, Holmes DRJ, Kopecky SL. Effect of concomitant or very early statin administration on in-hospital mortality and reinfarction in patients with acute myocardial infarction. Am J Cardiol. 2001;87(6):771–4, A7. doi: 10.1016/S0002-9149(00)01501-0. [DOI] [PubMed] [Google Scholar]
- Ostadal P, Alan D, Hajek P, Horak D, Vejvoda J, Trefanec J, Mates M, Vojacek J. The effect of early treatment by cerivastatin on the serum level of C-reactive protein, interleukin-6, and interleukin-8 in the patients with unstable angina and non-Q-wave myocardial infarction. Mol Cell Biochem. 2003;246(1-2):45–50. doi: 10.1023/A:1023499727477. [DOI] [PubMed] [Google Scholar]