Abstract
Osimertinib is a third-generation tyrosine kinase inhibitor (TKI) of the epidermal growth factor receptor (EGFR) that has been approved for the treatment of metastatic non-small cell lung cancer (NSCLC) positive for the secondary T790M mutation of EGFR. In a preclinical study, it also showed efficacy against leptomeningeal carcinomatosis (LMC) derived from NSCLC resistant to first-generation and second-generation EGFR-TKIs. We now report the case of a patient aged 70 years with symptomatic LMC derived from NSCLC with the T790M mutation of EGFR who showed a clinical and radiographic response to osimertinib.
Keywords: lung cancer, egfr mutation, T790M, meningitis, osimertinib
Key questions.
What is already known about this subject?
In a preclinical study, osimertinib was shown to have activity against leptomeningeal carcinomatosis resistant to first-generation and second-generation epidermal growth factor receptor-tyrosine kinase inhibitors.
What does this study add?
We report a case of the use of osimertinib for symptomatic leptomeningeal carcinomatosis (LMC) associated with epidermal growth factor receptor T790M-positive non-small cell lung cancer, which showed clinical and radiological response to osimertinib. Although performance status of our patient was impaired due to LMC, the treatment was well tolerated.
How might this impact on clinical practice?
Our case report suggests that osimertinib is a potentially effective treatment for leptomeningeal carcinomatosis associated with epidermal growth factor receptor (EGFR) T790M-positive non-small cell lung cancer that has developed resistance to a first-generation EGFR-tyrosine kinase inhibitor, and that osimertinib is a treatment option for patients with a poor performance status due to complications of cancer progression.
Introduction
Leptomeningeal carcinomatosis (LMC) is a fatal complication of advanced cancer, the incidence of which has been increasing in association with the prolongation of survival in patients with non-small cell lung cancer (NSCLC) due to recent advances in systemic therapy. 1 Epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) have been found to be effective in patients with LMC derived from lung adenocarcinoma positive for an activating mutation of EGFR. 2-4 However, most patients who initially benefit from a first-generation EGFR-TKI eventually develop disease progression, with 50% of cases of acquired resistance due to a secondary T790M mutation of EGFR. 5 Third-generation EGFR-TKIs has recently been developed to overcome such acquired resistance. A dose-escalation phase I study (AURA) showed that the third-generation EGFR-TKI osimertinib induced a marked clinical response (response rate of 61%) in previously treated NSCLC patients with the T790M mutation. 6 Given its high efficacy, osimertinib is also expected to be effective against LMC derived from NSCLC positive for this mutation. We now report a case of LMC in a patient with T790M-positive NSCLC treated with osimertinib.
Case report
A Japanese woman aged 70 years with no smoking history was diagnosed with stage IV lung adenocarcinoma and brain and lumbar vertebral metastases. Given that the primary tumour was found to harbour an EGFR L858R mutation, the patient was treated with gefitinib as a first-line therapy and subsequently received erlotinib, the combination of pemetrexed and carboplatin, S-1, and docetaxel over the course of 4 years. She also underwent stereotactic radiosurgery for the brain metastasis four times during the treatment course. After subsequent disease progression, a rebiopsy of the primary lesion revealed the EGFR T790M mutation. Erlotinib was again administered for 8 months until disease progression in a clinical trial.
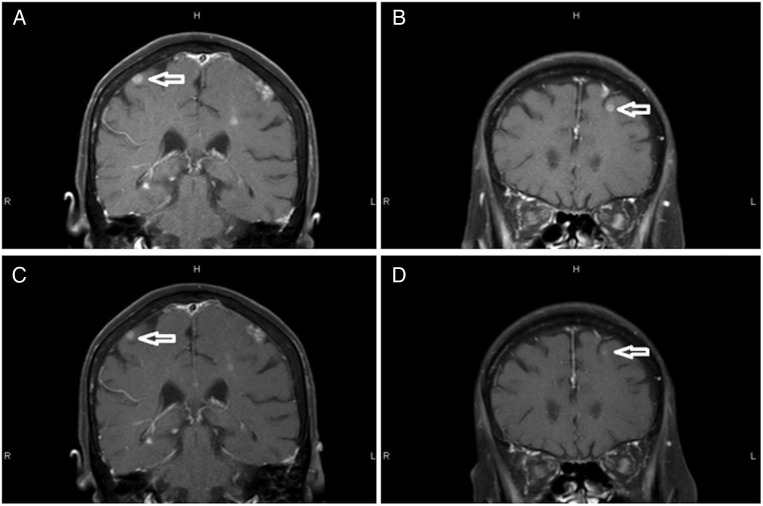
Six days after erlotinib discontinuation, the patient was urgently hospitalised as a result of severe fatigue, appetite loss and a slight headache. Her Eastern Cooperative Oncology Group performance status (PS) had deteriorated to 3 on the day of admission. MRI of the brain revealed LMC and multiple brain metastases ( figure 1 A, B). Progression at extracranial sites was not observed. As a seventh-line treatment, osimertinib was administered at a dose of 80 mg, resulting in relief of symptoms within a few days. MRI at 7 weeks after initiation of osimertinib showed shrinkage of the multiple nodular deposits in the brain ( figure 1 C, D), and treatment is currently ongoing and well tolerated.
Figure 1.
Brain MRI scans for the patient. (A,B) Brain MRI (fat-suppressed T1-weighted contrast MRI) before the initiation of osimertinib showed leptomeningeal enhancement, multiple nodular deposits in the subarachnoid space, and multiple nodules in the cerebral parenchyma. (C,D) A scan performed 7 weeks after the initiation of osimertinib revealed shrinkage of the multiple nodular deposits (arrows).
Discussion
The patient was diagnosed with LMC derived from NSCLC positive for the T790M mutation of EGFR and was successfully treated with osimertinib. The present case suggests that osimertinib is a potentially effective treatment for LMC associated with EGFR mutation-positive lung cancer that has developed resistance to a first-generation EGFR-TKI, and that osimertinib is a treatment option for patients with a poor PS due to complications of cancer progression.
Osimertinib was previously shown to have activity in a mouse model of LMC resistant to first-generation and second-generation EGFR-TKIs. 7 A phase I study of the safety of osimertinib in patients with LMC derived from NSCLC resistant to prior EGFR-TKI therapy is ongoing (NCT02228369). 8 Although little is known of the clinical efficacy of osimertinib for LMC associated with EGFR T790M-positive NSCLC, the present case supports the findings of the previous preclinical study.
Given that EGFR-TKIs induce a pronounced clinical response with an improved toxicity profile compared with chemotherapy, administration of these agents is an option for patients with a poor PS. A phase II study thus found that EGFR mutation-positive NSCLC patients with a poor PS benefited from first-line treatment with gefitinib. 9 An early-phase trial of osimertinib revealed promising efficacy for EGFR T790M-positive NSCLC and an acceptable toxicity profile. 6 The present case suggests that osimertinib is a feasible option for NSCLC patients with the T790M mutation whose PS is impaired due to complications of cancer progression.
Nevertheless, there is a limitation to our report. As we did not perform EGFR T790M mutational analysis for cerebrospinal fluid, there is a possibility of no T790M mutation in the central nervous system. 10 The good penetration of osimertinib into cerebrospinal fluid 11 might enable response even if T790M mutation was negative in the central nervous system.
In summary, we present a case of LMC associated with EGFR T790M-positive NSCLC that showed a response to osimertinib. Further studies are warranted to evaluate the efficacy of osimertinib for such patients.
Acknowledgments
The authors would like to thank patient and her family.
Footnotes
Contributors: HS and HH were responsible for clinical management of the patient, acquisition of data and drafting the manuscript. TI, YH, MT and KN were responsible for interpretation of data and critical revision of the manuscript. All authors read and approved the final version of the manuscript.
Competing interests: HH has received lecture fees from AstraZeneca K.K., Bristol-Myers Squibb, Chugai Pharmaceutical Co., Eli Lilly Japan K.K., Ono Pharmaceutical Co. and Taiho Pharmaceutical Co. as well as advisory fees from AstraZeneca K.K., Boehringer-Ingelheim Japan and Eli Lilly Japan K.K.
KN has received lecture fees and advisory fees from Chugai Pharmaceutical Co., AstraZeneca K.K. and Boehringer-Ingelheim Japan. All other authors declare no potential conflicts of interest.
Patient consent: Obtained.
Ethics approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and within the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from the patient of this study.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Lee SJ , Lee JI , Nam DH , et al. . Leptomeningeal carcinomatosis in non-small-cell lung cancer patients: impact on survival and correlated prognostic factors . J Thorac Oncol 2013. ; 8 : 185 – 91 . 10.1097/JTO.0b013e3182773f21 [DOI] [PubMed] [Google Scholar]
- 2. Wagner M , Besse B , Balleyguier C , et al. . Leptomeningeal and medullary response to second-line erlotinib in lung adenocarcinoma . J Thorac Oncol 2008. ; 3 : 677 – 9 . 10.1097/JTO.0b013e3181757a8b [DOI] [PubMed] [Google Scholar]
- 3. Katayama T , Shimizu J , Suda K , et al. . Efficacy of erlotinib for brain and leptomeningeal metastases in patients with lung adenocarcinoma who showed initial good response to gefitinib . J Thorac Oncol 2009. ; 4 : 1415 – 19 . 10.1097/JTO.0b013e3181b62572 [DOI] [PubMed] [Google Scholar]
- 4. Lee E , Keam B , Kim DW , et al. . Erlotinib versus gefitinib for control of leptomeningeal carcinomatosis in non-small-cell lung cancer . J Thorac Oncol 2013. ; 8 : 1069 – 74 . 10.1097/JTO.0b013e318294c8e8 [DOI] [PubMed] [Google Scholar]
- 5. Kosaka T , Yatabe Y , Endoh H , et al. . Analysis of epidermal growth factor receptor gene mutation in patients with non-small cell lung cancer and acquired resistance to gefitinib . Clin Cancer Res 2006. ; 12 : 5764 – 9 . 10.1158/1078-0432.CCR-06-0714 [DOI] [PubMed] [Google Scholar]
- 6. Jänne PA , Yang JC , Kim DW , et al. . AZD9291 in EGFR inhibitor-resistant non-small-cell lung cancer . N Engl J Med 2015. ; 372 : 1689 – 99 . 10.1056/NEJMoa1411817 [DOI] [PubMed] [Google Scholar]
- 7. Nanjo S , Ebi H , Arai S , et al. . High efficacy of third generation EGFR inhibitor AZD9291 in a leptomeningeal carcinomatosis model with EGFR-mutant lung cancer cells . Oncotarget 2016. ; 7 : 3847 – 56 . 10.18632/oncotarget.6758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yang JCH , Kim DW , Kim SW , et al. . Osimertinib activity in patients (pts) with leptomeningeal (LM) disease from non-small cell lung cancer (NSCLC): updated results from BLOOM, a phase I study. 2016 ASCO Annual Meeting . J Clin Oncol 2016. ; 34 : abstr 9002 . [Google Scholar]
- 9. Inoue A , Kobayashi K , Usui K , et al. . First-line gefitinib for patients with advanced non-small-cell lung cancer harboring epidermal growth factor receptor mutations without indication for chemotherapy . J Clin Oncol 2009. ; 27 : 1394 – 400 . 10.1200/JCO.2008.18.7658 [DOI] [PubMed] [Google Scholar]
- 10. Hata A , Katakami N , Yoshioka H , et al. . Spatiotemporal T790M heterogeneity in individual patients with EGFR-mutant non-small-cell lung cancer after acquired resistance to EGFR-TKI . J Thorac Oncol 2015. ; 10 : 1553 – 9 . 10.1097/JTO.0000000000000647 [DOI] [PubMed] [Google Scholar]
- 11. Ballard P , Yates JW , Yang Z , et al. . Preclinical comparison of osimertinib with other EGFR-TKIs in EGFR-mutant NSCLC brain metastases models, and early evidence of clinical brain metastases activity . Clin Cancer Res 2016. ; 22 : 5130 – 40 . Epub ahead of print . [DOI] [PubMed] [Google Scholar]