Abstract
Background:
Sleep problems, especially in the adolescent stage of development, may be associated with excessive daytime sleepiness, impaired neurocognitive function, and a host of others leading to suboptimal performance.
Objectives:
To determine the pattern of sleep problems in school-going adolescents based on the bedtime problems; excessive daytime sleepiness; awakenings during the night and problems falling back asleep; regularity and duration of sleep; sleep-disordered breathing (BEARS) sleep screening algorithm.
Materials and Methods:
This is a cross-sectional descriptive study involving 353 secondary school-going adolescents in Kano metropolis. Subjects were selected for the study using multistage sampling technique. The study lasted from March 2015 to July 2015. Sleep problems were screened for using the BEARS sleep screening algorithm. Tables were used to present the qualitative data. The various BEARS sleep patterns were assessed, and comparison between stages of adolescence was done using Chi-square test (and Fisher's exact test where necessary). A significant association was considered at P < 0.05.
Results:
Of the 353 adolescents studied, 61.8% were males while 38.2% were females with male, female ratio of 1.6:1. Early, middle, and late adolescents constituted 13.9%, 39.9%, 46.2% respectively. BEARS sleep screening revealed awakenings during the night (34.6%) as the most common sleep-related problem reported, and this was followed by excessive daytime sleepiness (21.0%). Age-group dependent sleep duration was 7.19 ± 1.26, 7.13 ± 1.13, 7.16 ± 1.28, with P > 0.05. Although 62.9% of all the adolescents watched TV/play video games until 1 h before going to bed and this was highest in late adolescence, it was not statistically significantly associated with any of the sleep problems.
Conclusion:
Both the quality and quantity of sleep in Nigerian adolescents in Kano is suboptimal. Adolescent and sleep medicine should receive more attention in our environment.
Keywords: Adolescents, bedtime problems; excessive daytime sleepiness; awakenings during the night and problems falling back asleep, regularity and duration of sleep; sleep-disordered breathing, Kano, sleep problems
INTRODUCTION
Benjamin Franklin's aphorism, “early to bed and early to rise makes a man healthy, wealthy and wise”[1] may not amount to a truism as being early to bed may not translate into a healthy life if there is any sleep problem like a difficulty in initiating or sustaining sleep. This will be particularly alarming in the adolescence age group which prima facie is a highly challenging period of life bearing in mind the developmental tasks accompanying the changes in the psychological milieu and the resultant changes in physical growth, cognition, emotional, and psychological behavior.[2] These may get dysfunctional in adolescents with sleep problems making them present with excessive daytime sleepiness, impaired neurocognitive, and psychomotor performance.[3]
While the expected average sleep duration in adolescents is 9 h,[4,5] there seems to be a global trend of suboptimal sleep duration among adolescents. Sweileh et al.[6] in Nablus, Palestine reported as low as 6.4 ± 1.1 h as the mean duration of night sleep in 400 adolescent students. In their study, poor sleep quality was significantly associated with increased frequency of nocturnal awakenings. Similarly, Gupta et al.[7] studied Indian adolescents and reported a reduced mean sleep duration of 7.8 h. They also found that 37% of these adolescents had nocturnal awakenings. Oluwole[8] and Chinawa et al.[9] in Southwest and Southeast Nigeria, respectively reported 6–7 h as the duration of night sleep among Nigerian undergraduates.
Adolescent and sleep medicine has received little attention in Nigeria. The few reported cases were not based solely on adolescents, but their study population comprises adolescents and adults. There is obviously dearth of local data on sleep problems among Nigerian adolescents. It is against this background that we seek to evaluate the quantity and quality of sleep in adolescents and ascertain the possible risk factors of sleep disorders affecting them.
MATERIALS AND METHODS
This was a cross-sectional descriptive study involving 353 secondary school-going adolescents in Kano metropolis. Three out of the 8 LGAs in the metropolis (amounting to 30%) were randomly selected. A multistage sampling technique was used to randomly select secondary schools from the school administrative zone lists obtained from Kano state ministry of education. This was followed by a simple random selection of three schools from each of the three LGAs. This resulted in a total of nine secondary schools. Ethical approval was sought from the Research Ethical Committee of Aminu Kano Teaching Hospital, Kano and that of the Kano State Secondary Schools Board and state Universal Basic Education Board of Kano State. Informed assent/consent was obtained from the study population after a careful explanation of the research and a self-administered questionnaire (with class teacher's assistance where necessary). The questionnaire had three parts; biodata, questions on sleep pattern derived from the bedtime problems; excessive daytime sleepiness; awakenings during the night and problems falling back asleep; regularity and duration of sleep; sleep-disordered breathing (BEARS) sleep screening algorithm, and the final section will address sleep hygiene practices. The BEARS sleep screening algorithm was developed by the investigators of Brown University School of Medicine, Rhode Island Hospital, USA and its reliability and validity has been assessed previously.[10,11] The adopted BEARS sleep screening questionnaire was pretested in a pilot study.
Statistical analysis
Data were analyzed using Statistical Package for Social Sciences SPSS version 20.0 (SPSS Inc. Chicago, Illinois). For descriptive statistics, frequency distribution and calculation of mean and standard deviation were done. Tables were used to present the qualitative data. Comparison of sleep patterns between stages of adolescence;[12] early (11 through 13 years of age), middle (14 through 16 years of age), and late (17 through 19 years of age) and associations with sleep hygiene practices were done using Chi-square test (and Fisher exact's test where necessary). A significant association was considered statistically significant at P < 0.05.
RESULTS
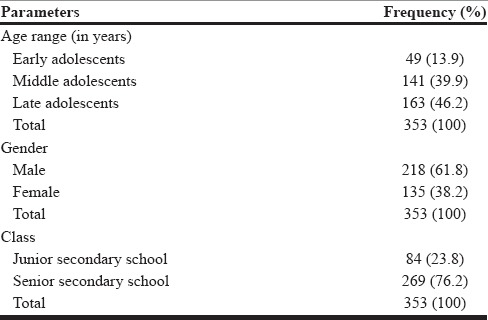
Three hundred and fifty-three adolescents responded out of a total of 400, response rate of 88.3%. The mean age of the respondents was 15.89 ± 1.93 years, and there were 218 (61.8%) males and 135 (38.2%) females with an M: F ratio of 1.6:1. Adolescents in senior secondary school constituted 76.2% of respondents while 23.8% were in junior secondary school. Early, middle, and late adolescents constituted 13.9%, 39.9%, 46.2%, respectively of the study population [Table 1].
Table 1.
Demographic profile of adolescents
Adapted BEARS sleep screening revealed that 15.3% have bedtime problems, 20.9% have excessive daytime sleepiness, 34.6% have awakenings during the night, 20.1% have problems falling back asleep, age-group dependent sleep duration is 7.19 ± 1.26, 7.13 ± 1.13, and 7.16 ± 1.28 h, respectively for early, middle, and late adolescence, and 4.9% are aware they snore at night as shown in Table 2.
Table 2.
Sleep problems compared across the three stages of adolescence
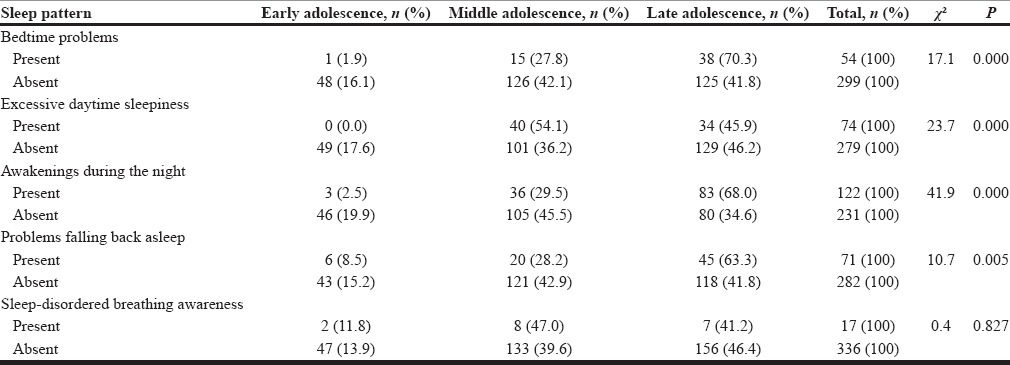
Sleep pattern
Bedtime problems
A total of 54 adolescents (15.3%) have problems falling asleep at bedtime. Among these, the late adolescence age group was most affected (70.4%), and the early adolescence age group was least affected (1.9%) while 27.8% of the middle adolescence age group also suffered bedtime problems as shown in Table 2. The occurrence of bedtime problems differ significantly across the adolescent age groups, and this was found to be statistically significant (χ2 = 17.090, P = 0.000).
Excessive daytime sleepiness
Seventy-four adolescents (20.9%) were found to have excessive daytime sleepiness. While none of those in the early adolescent age groups felt sleepy a lot during the daytime, this sleep problem was most common in middle adolescence 54.1% and 45.9% in late adolescence [Table 2]. This observation across the adolescent subgroups was statistically significant (χ2 = 17.665, P = 0.000).
Awakenings during the night
Majority of the adolescents 122, (34.6%) wake up a lot at night, and its occurrence increased progressively with increasing age group (2.5% in early adolescence, 29.5% in middle adolescence, and 68.0% in late adolescence). The difference across the age groups was statistically significant (χ2 = 41.893, P = 0.000) [Table 2].
Problems falling back asleep
Problems falling back asleep occurred in 20.1% of the adolescents. Just like frequent night awakenings, problems falling back to sleep progressed across increasing age group (8.5% in early adolescence, 28.2% in middle adolescence, and 63.4% in late adolescence), and this finding was statistically significant (χ2 = 10.670, P = 0.005) as shown in Table 2.
Sleep-disordered breathing
Only 17 adolescents (4.8%) were aware, they snore during sleep at night [Table 2]. This was most common in middle adolescence (47.1%), least in early adolescence (11.8%) while 41.2% of the late adolescence age group had sleep-disordered breathing. There is no significant difference across the age groups (χ2 = 0.381, P = 0.827).
Sleep hygiene practices
Watching TV/playing video games till <1 h before going to bed (n = 222)
Watching the television/playing video games till <1 h before going to bed was practiced by as much as 62.9% of the adolescents [Table 3]. While this poor sleep hygiene practice is most common in late adolescence, there is no significant difference across the adolescent age groups (χ2 = 1.663, P = 0.435).
Table 3.
Common sleep hygiene practices among adolescents compared across the three stages of adolescence
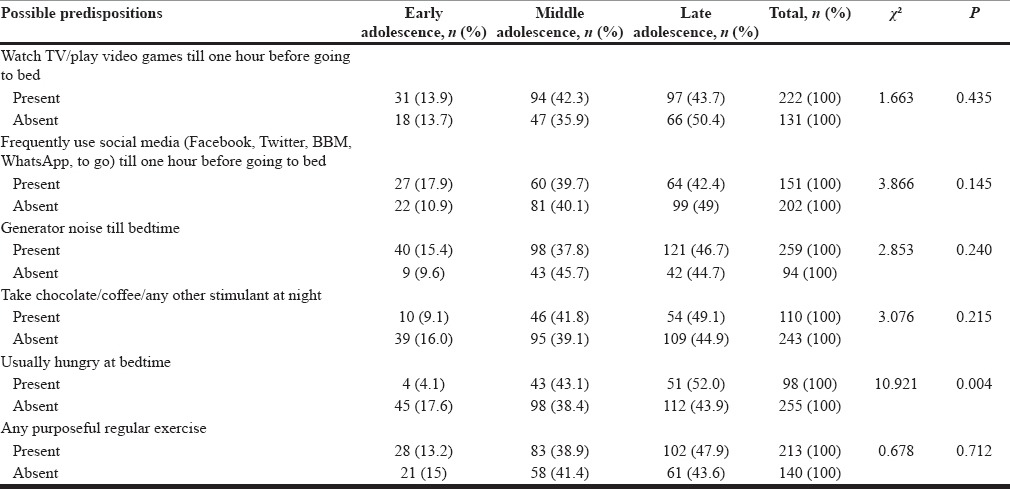
Frequent use of social media (Facebook, Twitter, BBM, WhatsApp, to go) till <1 h before going to bed (n = 151)
Up to 42.8% of the studied adolescents are frequently involved with the social media till <1 h before sleep time [Table 3]. Again this practice was most prevalent among those in the late adolescent age group though the difference across the age groups was not statistically significant (χ2 = 3.866, P = 0.145).
Exposure to generator noise till bedtime (n = 259)
About 73.4% of the adolescents were exposed to noise from a power generating set [Table 3]. We found that 15.4%, 37.8%, and 46.7% of those in the early, middle, and late adolescence age groups, respectively went to bed in a noisy environment. However, there was no significant difference across the age groups (χ2 = 2.853, P = 0.241).
Take chocolate/coffee/any other stimulant at night (n = 110)
A third of the adolescents (31.2%) took stimulant at night [Table 3]. This practice was most common in late adolescence as 49.1% of them indulge in this practice. Despite this, the difference across the age groups was no statistically significant (χ2 = 3.076, P = 0.215).
Usually hungry at bedtime (n = 98)
Hunger at bedtime was reported in 27.8% of the adolescents [Table 3]. About 52.0% of these are those in the late adolescent age groups, and this occurrence differs significantly across the age groups (χ2 = 10.921, P = 0.004).
Engaging in any purposeful regular exercise (n = 213)
Up to 60.3% of the adolescents engaged regularly in one form of purposeful exercise [Table 3]. However, this was least practiced by adolescents in the early age group though no significant difference across the age groups was found (χ2 = 0.678, P = 0.712).
Association between generator use at night till bedtime and problem falling asleep at bedtime across stages of adolescence
Although 73.4% of the adolescents are exposed to noise from an electric power generating set at bedtime, there was no significant relationship between this and having problem falling asleep (χ2 = 0.230, P = 0.816, χ2 = 0.873, P = 0.269, χ2 = 0.262, P = 0.376 for early, middle, and late stages of adolescence, respectively).
DISCUSSION
Frequent nocturnal awakening occurs in 34.6% of adolescents and is the predominant sleep problem encountered. Its occurrence was also found to progressively increase with later stages of adolescence. This finding is similar to that by Gupta et al.[7] in India, where 37% of adolescents had frequent nocturnal awakenings. In their study, the frequency of nocturnal awakenings similarly increased in higher school Grades with the twelfth Grade adolescents having significantly higher number of awakenings compared to ninth and tenth Grades. A similar pattern was also reported by Yang et al.[13] among Korean teenagers. Laberge et al.[14] in Canada reported that 26% of their study population had a frequent nocturnal awakening which is less than what we found. This difference may be accounted for by the fact that in their study, mothers were the respondents and may have underreported.
In this study, night time mean sleep duration by age group classification obtained is 7.19 ± 1.26, 7.13 ± 1.13, and 7.16 ± 1.28 h for early, middle, and late adolescence, respectively. Although there may be inter-individual sleep variation among adolescents, the expected sleep duration remains at least 9 h.[3,4] Any night time sleep duration <8 h is regarded insufficient for an adolescent while period between 8 and 9 h is considered borderline.[15] Our finding of insufficient sleep duration at night is in tandem with that of Gupta et al.[7] (7.8 h/day), Sweileh et al.[6] (6.4 ± 1.1 h), Oluwole[8] (6.2 h), and Chinawa et al.[9] (6 h). However, Sanya et al.[16] in Ilorin, Nigeria reported mean sleep duration of 9.33 ± 2.29 h during school days which is optimal in adolescence. Although our finding agrees with most others, the difference with Sanya et al.[16] may be accounted for by cultural differences as suggested by Laberge et al.[13] The unfortunate duo of frequent nocturnal awakening and suboptimal sleep duration implied that our studied adolescents have poor sleep quality.
Although it is a good sleep hygiene practice to have the 30–60 min before sleep time a quiet wind-down time, we found that as much as 73.4% of the adolescents are exposed to noise from a power generating set at bedtime. This tells of a wide spread of power generating set as power supply from electric distributors have been almost nonexistent. Interestingly, however, we found no significant relationship between this and having problem falling asleep across the adolescent age groups. This finding seems contrary to popular expectation may be an adaptation to austerity. Reiterating our austerity hypothesis is our finding that 27.8% of the adolescents were even hungry at bedtime.
The use of electronic communication gadgets is one extrinsic factor that has been reported to influence sleep among adolescents.[16,17,18,19,20,21] We also found that up to 42.8% of the adolescents are frequently involved with the social media till <1 h before sleep time. This practice was most prevalent among those in the late adolescent age group though the difference across the age groups was not statistically significant. Our finding far exceeds the reported 5.5% by Sanya et al.[16] in 2010 among adolescents in Ilorin, Nigeria. This possibly reflects a rise in social media/internet use by Nigerian adolescents. The advancement in technology and increase availability of electronic communication devices globally would have made the use of mobile phones and social media usage possible for these adolescents, the ultimate outcome which is a negative impact on sleep parameters and hygiene.
Worthy of note is our finding of 60.3% of the adolescents engaging regularly in one form of purposeful exercise as this is known to help falling asleep faster.[5] Although adolescents in the early age group least engaged in exercise, we found no significant difference across the age groups was found.
CONCLUSION
We have studied adolescents’ sleep problems and its association with common sleep hygiene practices. The results suggest that both the quality and quantity of sleep in Nigerian adolescents in Kano is suboptimal. Interventions to help adolescents with the sleep issues, promoting good sleep hygiene strategies to facilitate healthy sleep are required. Hence, adolescent and sleep medicine should receive more attention in our environment. There is a need for primary caregivers to supervise the use of technological tools such as smartphones at bedtime.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Benjamin Franklin Quotes. 2016. [Last cited on 2016 Jul 08]. Available from: http://www.brainyquote.com/quotes/quotes/b/benjaminfr564198.html .
- 2.Brand S, Kirov R. Sleep and its importance in adolescence and in common adolescent somatic and psychiatric conditions. Int J Gen Med. 2011;4:425–42. doi: 10.2147/IJGM.S11557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rocha FL, Guerra HL, Lima-Costa MF. Prevalence of insomnia and associated socio-demographic factors in a Brazilian community: The Bambuí study. Sleep Med. 2002;3:121–6. doi: 10.1016/s1389-9457(01)00119-8. [DOI] [PubMed] [Google Scholar]
- 4.Yilmaz K, Kilinçaslan A, Aydin N, Kul S. Understanding sleep habits and associated factors can help to improve sleep in high school adolescents. Turk J Pediatr. 2011;53:430–6. [PubMed] [Google Scholar]
- 5.Owens JA. Sleep medicine. In: Kliegman RM, Behrman RE, Jenson HB, Stanton BF, editors. Nelson Text Book of Pediatrics. 19th ed. Philadelphia: Elsevier Saunders; 2011. pp. 46–55. [Google Scholar]
- 6.Sweileh WM, Ali IA, Sawalha AF, Abu-Taha AS, Zyoud SH, Al-Jabi SW. Sleep habits and sleep problems among Palestinian students. Child Adolesc Psychiatry Ment Health. 2011;5:25. doi: 10.1186/1753-2000-5-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gupta R, Bhatia MS, Chhabra V, Sharma S, Dahiya D, Semalti K, et al. Sleep patterns of urban school-going adolescents. Indian Pediatr. 2008;45:183–9. [PubMed] [Google Scholar]
- 8.Oluwole OS. Sleep habits in Nigerian undergraduates. Acta Neurol Scand. 2010;121:1–6. doi: 10.1111/j.1600-0404.2009.01171.x. [DOI] [PubMed] [Google Scholar]
- 9.Chinawa JM, Chukwu BF, Obu HA. Sleep practices among medical students in Pediatrics Department of University of Nigeria Teaching Hospital, Ituku/Ozalla, Enugu, Nigeria. Niger J Clin Pract. 2014;17:232–6. doi: 10.4103/1119-3077.127565. [DOI] [PubMed] [Google Scholar]
- 10.Owens JA, Dalzell V. Use of the ’BEARS’ sleep screening tool in a pediatric residents’ continuity clinic: A pilot study. Sleep Med. 2005;6:63–9. doi: 10.1016/j.sleep.2004.07.015. [DOI] [PubMed] [Google Scholar]
- 11.Mohammadi M, Amintehran E, Ghaleh-bandi M, Reza AM, Shervan S, Babak G. Reliability and validity of Persian version of “BEARS” pediatric sleep questionnaire. Indian J Sleep Med. 2008;3:14–9. [Google Scholar]
- 12.Clark-Lempers DS, Lempers JD, Ho C. Early, middle, and late adolescents’ perceptions of their relationships with significant others. J Adolesc Res. 1991;6:296–315. [Google Scholar]
- 13.Yang CK, Kim JK, Patel SR, Lee JH. Age-related changes in sleep/wake patterns among Korean teenagers. Pediatrics. 2005;115(1 Suppl):250–6. doi: 10.1542/peds.2004-0815G. [DOI] [PubMed] [Google Scholar]
- 14.Laberge L, Petit D, Simard C, Vitaro F, Tremblay RE, Montplaisir J. Development of sleep patterns in early adolescence. J Sleep Res. 2001;10:59–67. doi: 10.1046/j.1365-2869.2001.00242.x. [DOI] [PubMed] [Google Scholar]
- 15.Gradisar M, Gardner G, Dohnt H. Recent worldwide sleep patterns and problems during adolescence: A review and meta-analysis of age, region, and sleep. Sleep Med. 2011;12:110–8. doi: 10.1016/j.sleep.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 16.Sanya EO, Kolo PM, Desalu OO, Bolarinwa OA, Ajiboye PO, Tunde-Ayinmode MF. Self-reported sleep parameters among secondary school teenagers in middle-belt Nigeria. Niger J Clin Pract. 2015;18:337–41. doi: 10.4103/1119-3077.151737. [DOI] [PubMed] [Google Scholar]
- 17.Punamäki RL, Wallenius M, Nygård CH, Saarni L, Rimpelä A. Use of information and communication technology (ICT) and perceived health in adolescence: The role of sleeping habits and waking-time tiredness. J Adolesc. 2007;30:569–85. doi: 10.1016/j.adolescence.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 18.Shochat T. Impact of lifestyle and technology developments on sleep. Nat Sci Sleep. 2012;4:19–31. doi: 10.2147/NSS.S18891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chung KF, Cheung MM. Sleep-wake patterns and sleep disturbance among Hong Kong Chinese adolescents. Sleep. 2008;31:185–94. doi: 10.1093/sleep/31.2.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Calamaro CJ, Mason TB, Ratcliffe SJ. Adolescents living the 24/7 lifestyle: Effects of caffeine and technology on sleep duration and daytime functioning. Pediatrics. 2009;123:e1005–10. doi: 10.1542/peds.2008-3641. [DOI] [PubMed] [Google Scholar]
- 21.Shochat T, Flint-Bretler O, Tzischinsky O. Sleep patterns, electronic media exposure and daytime sleep-related behaviours among Israeli adolescents. Acta Paediatr. 2010;99:1396–400. doi: 10.1111/j.1651-2227.2010.01821.x. [DOI] [PubMed] [Google Scholar]


