Abstract
Background:
To find any association between family structure and rates of hospitalization as an indicator for behavior problems in children.
Methods:
Retrospective chart review of 154 patients who were admitted to the preadolescent unit at Lincoln Prairie Behavioral Health Center between July and December 2012.
Results:
We found that only 11% of children came from intact families living with biological parents while 89% had some kind of disruption in their family structure. Two-third of the children in the study population had been exposed to trauma with physical abuse seen in 36% of cases. Seventy-one percent had reported either a parent or a sibling with a psychiatric disorder. Children coming from biologically family were less likely to have been exposed to trauma. Children coming from single/divorced families were less likely to have been exposed to sexual abuse but more likely to have a diagnosis of attention deficit hyperactivity disorder (ADHD) compared to other types of families. Strong association was found between exposure to trauma and certain diagnoses in respect to hospitalization. ADHD predicted a 4 times likelihood of having more than one previous hospitalization, with mood disorder, oppositional defiant disorder, and physical abuse increasing the risk by more than twice.
Conclusions:
Significant differences in family structure were demonstrated in our study of children being admitted to inpatient psychiatric hospitalization. The presence of trauma and family psychiatric history predicted higher rates of readmission. Our study highlighted the role of psychosocial factors, namely, family structure and its adverse effects on the mental well-being of children.
Keywords: Family structure, hospitalization rates, single parents, trauma
INTRODUCTION
The interest in family structure and its effects on children's mental health gained momentum in the 1960s and 1970s when there was a spike in divorce rates and single-parent families. The main focus was on separation and divorce and their impact on the well-being of children.[1] Over the years, there has been a change in the family structure reflected in the increased proportion of children living in a single-parent home which changed from 12% in 1960 to 28% in 2003.[2] These studies were also able to document some of the long-term effects of stress as a result of separation on children.[1] According to 2001–2007, Centers for Disease Control (CDC) estimates about half of children live with their biological parents. This does vary across race and falls down to almost 24% when dealing with African-American children.
Single parents
Reviewing the literature, it also becomes clear that single parenthood becomes a clear risk factor for mental health problems for both children and adults, leading to greater psychological distress and depression,[3] and puts women at a socioeconomic disadvantage further increasing the level of stress.[4] Several studies have also documented the link between separation and depressive disorders most likely as a result of both social and economic reasons.[5] Weisman et al. 1987 found that single Caucasian women were almost twice as likely to suffer from depression compared to married women.
Over the years, there has been a general consensus that single-parent families are at a greater disadvantage compared to more traditional homes. The factors associated with worse outcome in single-parent families maybe more complicated than first evident. Single-parent families are also suggested to have less resilience when confronting stress. Single parenthood raises further economic challenges compounding the level of stress, possibly causing more difficulties in parent–child relationships. The prevalence of poverty in single-parent family has been estimated to be as high as 50% compared to around 5% in two-parent intact families.[1] This economic disadvantage can further lead to higher rates of emotional and behavioral problems in children.[6] Factors which increase the likelihood that children will show disturbance over time include marital conflict, being raised in poverty, teen and single parenthood, parental depression, and hostile/angry parenting. Dysfunctional family backgrounds and socioeconomic adversity have also been attributed to suicide in young people. Childhood adversity including divorce and impaired parenting seems to cause both short- and long-term problems, various childhood disorders, and subsequently depression in adulthood. Single mothers have been found twice as likely to come from families where a parent had a mental health problem. Studies have also reported as high as a threefold risk of depression, and substance use in single mothers compared to married mothers. Children from single family were more than twice likely to report internalizing problems and more than three times likely to report externalizing problems compared to children from two-parent families.[1] More and more research studies have underscored the importance of early life experience in defining life trajectories.[7] Silver et al. also suggested in their study that children who lived their mother and an unrelated partner had the poorest adjustment and highest levels of conduct problems compared to children who just lived their mothers. Studies have also suggested that adjustment problems in children with mother-only families are comparable to mother and an unrelated partner or a stepfather. The risk slightly decreases with another adult like grandparent being in the family.[8]
Family structure and trauma
Disruption in family structure can lead to several adverse events impacting both the mental health of children and their parents. Not all disruptions have equal effects. More emotional and behavioral problems occur in families disrupted by divorce than compared to other types of disruptions, for example, death of a parent. Certain characteristics have been identified in caregivers as well as the children themselves that serve as risk factors for abuse. Young age, depression, substance abuse, poverty, and history of mothers being separated from their own mothers during childhood serve as risk factors. Similar risk factors are also seen in male caregivers with unrelated male partner present at home acting as an additional risk factor. Some 30% children are expected to be living with unrelated surrogate father.[2] Studies have also found that the presence of a stepparent increases the risk of being abused by a staggering factor of 20–40 times in contrast to living with single mothers where the risk was about 14 times compared to living in a biologically intact family. Some risk factors have also been identified within the children themselves such as low birth weight, physical, mental disabilities, aggression, and hyperactivity. Parents exposed to abuse in their childhood or domestic violence were also more prone to act aggressively toward their own children.[2] However, studies have not been able to decipher and document in the detail the different forms of abuse experienced by children who come from various types of disturbed family structures.
Parental mental health and its impact on children
History of parental psychopathology predisposes children to increased rates of depression and other psychopathology when compared to children of parents who do not have any affective illness. Further, studies have also indicated that the course of depression in these children may be more chronic with increased rates of relapse. It also appears that mother's affective state has a more profound effect on the child than father's illness and the difference being statistically significant. As mentioned previously, parental marital impairments also affect child's risk for psychopathology and probably intertwine with parental psychopathology further leading to marital discord.[9]
Family structure and hospitalization
A better appreciation of the web of social and psychosocial processes that surround the association between family structure and health outcomes needs to be studied. This may impact early intervention strategies targeting reduction in morbidity and mortality. There have been a limited number of studies looking into family structure as a variable. There was a large influx of studies in the 1960s and 1970s, but over the years, the interest in this area has diminished. There are also a limited number of studies looking at hospitalization as a variable with very few being published in the recent past. Yampolskaya, 2013, et al.[10] found that more than one psychiatric diagnosis and severity of maltreatment increased the odds of psychiatric readmission. It was evident during the inpatient rotation that high numbers of children admitted were from some kind of disturbed family structure with additional history of abuse.
The main aim of this study was to look at any association between family structure and hospitalizations as this has never been done. Several other factors were also studied with hospitalization being the dependent variable. We were interested in finding any link between these factors and if a certain type of family structure was predictive of higher rates of hospitalization, trauma, or specific diagnoses.
METHODS
This study was done at Lincoln Prairie Behavioral Health Center (LPBHC) inpatient unit. Exempt status was obtained from IRB/SCRIHS. We conducted retrospective chart review of 154 patient charts admitted to the preadolescent unit at LPBHC. Eleven charts were excluded for various reasons; bringing down the number to 143 charts. Inclusion criteria: children ≤12 years of age, admitted between July and December of 2012, and having a psychosocial assessment done within 24 h of admission by a therapist were included in the study. Our dependent variable was number of hospitalization, with family structure being the primary independent variable. Family psychiatric history, exposure to trauma, and diagnosis were classified as secondary independent variables.
Data were first entered into excel format and then converted to SPSS (IBM) to derive the descriptive statistics (frequencies). Another excel data set was converted to SAS to run the inferential statistics. Chi-square analysis was run between the dependent variable and the primary independent variable. Similar tests were also run between dependent variable and the secondary independent variables. Chi-square analysis served as a screening test. A logistic regression model was applied to any result that came out to be significant statistically on Chi-square analysis to find the strength of the association between the two variables.
RESULTS
Descriptive statistics
After gathering the data, a frequency analyses were run in SPSS to assess for preliminary trends in the data. Frequency data (mode) were calculated along with the corresponding percentage.
Demographic characteristics
The most common age in our study was 12 years with the majority of children lying between 7 and 12 years of age constituting about 90% of the study population. Males predominated with just over two-third of the study population. Over 76% were Caucasian with African-Americans making up only 15% [Figures 1 and 2].
Figure 1.
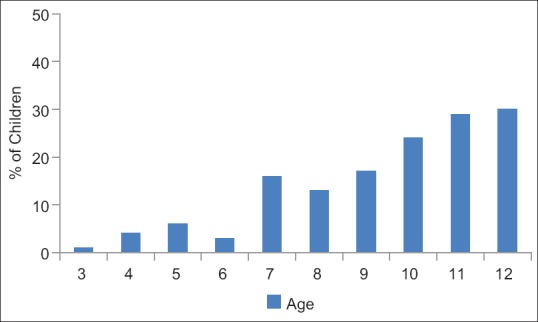
Age distribution of children
Figure 2.
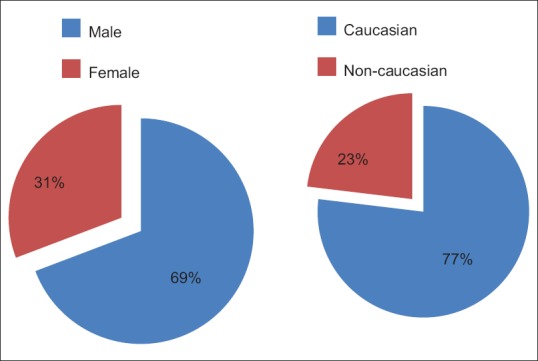
Sex and race distribution
Family structure
One of the main goals of this study was to look at the family structure and its influence on mental well-being of children. Surprisingly, only 11% of children came from intact families living with biological parents while the other 89% had some kind of variations in their family structure. Forty-four percent came from one-parent homes including single and divorced parents. Around 23% were under the care of the state including foster families and residential care, and 14% were from blended family either a combination of stepmother or father. A very small percentage (7%) of children was adopted [Figure 3].
Figure 3.
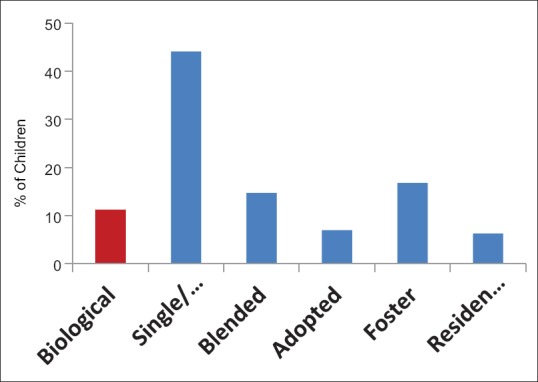
Family structure
Three-member families stood as the most common with just over quarter of the cases. The traditional four-member family or fewer constituted about 61% of the population with 5 or members making up the rest (33%) [Figure 4].
Figure 4.
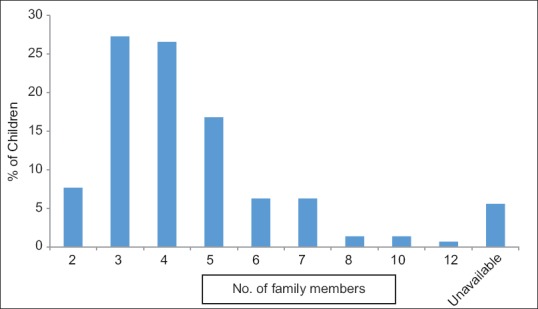
No. of family members
Hospitalization
For one-third of the children, this was their first psychiatric hospitalization, with 90% of children having three or less previous psychiatric hospitalizations. One child had thirty hospitalizations [Figure 5].
Figure 5.
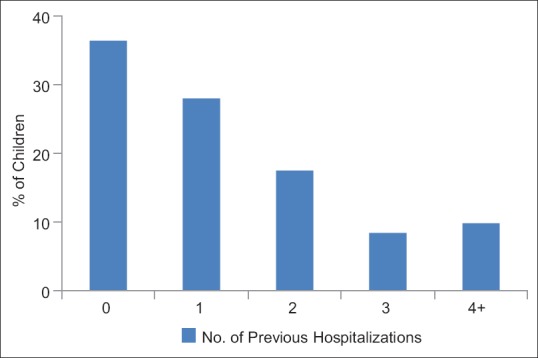
No. of previous hospitalizations
Abuse
Nearly two-third of the children in the study population had been exposed to some type of abuse in the past with almost similar number having some kind of involvement with Department of Children and Family Services either currently or in the past. Physical abuse stood out as the most common form of abuse presents in 36% of cases followed by neglect, emotional, and sexual abuse [Figure 6].
Figure 6.
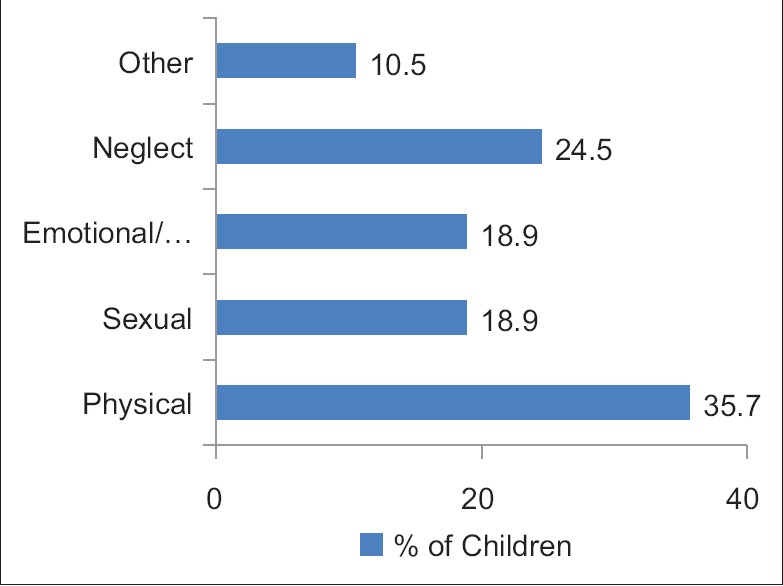
Exposure to trauma
Diagnoses
We looked at trends in both the primary diagnoses that the children had based on what was listed as the first diagnoses on their discharge summary and also the overall frequencies of all the diagnoses taken together. As expected attention deficit hyperactivity disorder (ADHD) was present in about 60% of the children as the primary diagnoses, followed by mood disorder in 25% of the children. Anxiety disorders were prevalent in <5% of population as a primary disorder with conduct and oppositional defiant disorder (ODD) making up about 7% [Figure 7].
Figure 7.
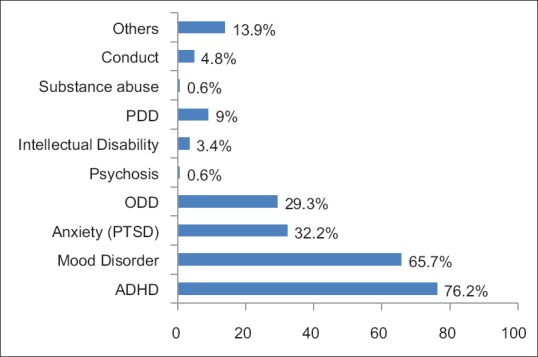
Psychiatric diagnosis among the study population
When distributions of total diagnosis were considered ADHD again came up as the most prominent one encompassing about 76% of children. Sixty-six percent of children had some kind of mood disorder including depression and bipolar disorder. Anxiety and ODD were equally present in about 30% while PDD in 10%.
Family psychiatry history
A preponderance of children (71%) had reported either a parent or a sibling with a psychiatric disorder. Mood disorder was the most common psychiatric disability in mothers present in 48% of cases followed by substance use and anxiety. Twenty-one percent of fathers had mood disorder followed by 14% with substance use issues. The most common comorbidity among siblings was ADHD, followed by mood disorder and then anxiety disorder reflecting a similar pattern to children themselves. Twenty-two percent of children reported a sibling with a psychiatric diagnosis.
Eighty-seven percent of cases had Medicaid insurance.
Inferential statistics
A Chi-square analysis was run between the family structure and hospitalization which was the dependent variable. Hospitalization was run both as an absolute count of admission and also as a dichotomous variable (no previous hospitalization vs. one or more previous hospitalizations). Absolute count of admission and dichotomous variable grouping was used for all the secondary outcome variables as well.
No significant statistical significance was found between family structure and hospitalization. However, statistically significant results were found between family psychiatric history, exposure to trauma, and diagnosis when looked at with hospitalization as a dependent variable [Table 1].
Table 1.
Child psychiatry hospitalization as a dependent variable
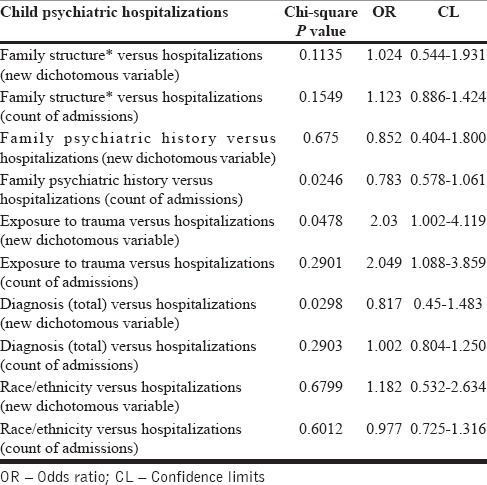
Further, logistic regression was run to look for strength of association. No association was found between family psychiatric history and number of hospitalization. Strong association was found between certain diagnosis as well as trauma in respect to hospitalization. ADHD predicted a 4 times likelihood of having more than one previous hospitalization, with mood disorder and ODD increasing the risk by more than twice [Table 2].
Table 2.
Hospitalization rates as predicted by diagnosis
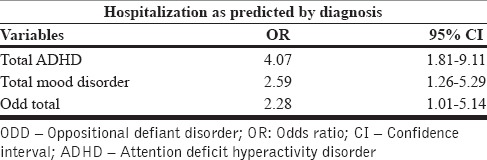
Exposure to any type of trauma and specifically physical abuse increased the likelihood of having more than one previous psychiatric hospitalization by two fold.
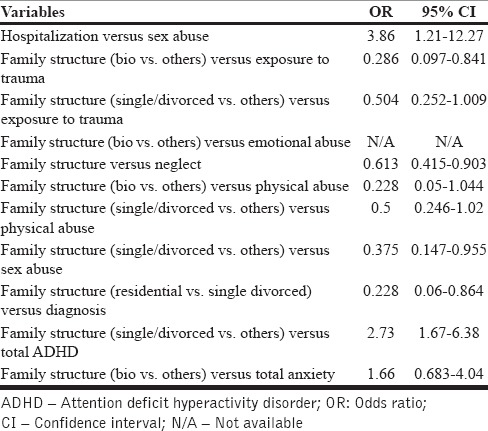
We were able to run certain other logistic regression models to look at association between types of family structure to history of abuse and diagnosis. Children coming from a biological family were less likely to have been exposed to trauma. Children coming from single/divorced families were less likely to have been exposed to sexual abuse but more likely to have a diagnosis of ADHD compared to other types of families [Table 3].
Table 3.
Family structure and its relationship to other dependent variables
DISCUSSION
This was a pilot study looking into the association between psychosocial factors and risk of hospitalization. We were able to look at various factors that may have contributed toward children having recurrent hospitalizations. In respect to family structure, significant differences were identified among the children who admitted to inpatient psychiatric unit. We were able to highlight that only to 11% of children came from biologically intact families and the remaining 89% had some kind of disruption in their family structure. This does appear to significantly contrast data from CDC when looking at distribution of children under the age of 18 years and their family structure. By various estimates, about 50% of children come from biologically intact families. This may also vary according to race with higher rates of biologically intact families among Caucasian children compared to African-American children.
In our study, we were not able to find any statistically significant association between family structure and number of hospitalization. We were, however, able to demonstrate strong associations between certain traumas and diagnosis in predicting higher rates of rehospitalization. We were also able to highlight in our study the adverse effect of certain family types and their predisposition for higher rates of exposure to trauma or carrying higher rates of a particular diagnosis.
The biopsychosocial model of health has been used extensively to understand the role of various factors in human functioning in the context of health or illness. This interrelation is important more so in the context of mental health. Psychological factors are not only interdependent on each other but also can also affect biological factors. This was clearly demonstrated in a study released by researchers at Duke University who demonstrated that “Children who experienced at least two types of exposure to violence showed significantly more telomere erosion between ages 5 and 10 than did controls subjects.” This shows that psychosocial factors can influence biological factors and stress in fact lead to significant changes in chromosome of children when they are young and most vulnerable.
Changing trajectory is a term that has been used extensively in research related to health of children. Two important variables have become important in this concept, one being early identification, the other early intervention. By the time, many adults seek mental health services, they have had to endure many years of chronic stress, and the role of primary and secondary intervention becomes obsolete. In case of children, there is a major emphasis on primary and secondary prevention that can lead to significant changes in their development trajectory and lead to normalization. This has been further emphasized in a recent statement by CDC (2013) - “More comprehensive surveillance is needed to develop a public health approach that will both help prevent mental disorders and promote mental health among children.”
We were able to arrive at the following conclusions from our study:
Significant differences in family structure were demonstrated in our study of children being admitted to inpatient psychiatric hospitalization. Only 11% were residing with biologically intact families. Significant differences were also evident between Caucasians and non-Caucasians within blended and residential groups
The presence of trauma and family psychiatric history predicted higher rates of readmission
ADHD, ODD, mood disorder, and physical trauma predicted higher rates of readmission
Children from biological families were less likely to be exposed to trauma
Children from single/divorced families were more likely to have an ADHD diagnosis but less likely to have been sexually abused.
Limitations
Sample size was limited to 143 charts which reduced the power of the study
No comparison group was present in the study
Study was based on retrospective chart review leading to recall bias
Data were based on parent report which may have led to over- or underreporting of factors and were collected by a therapist and not directly by the investigators.
In our study, we have highlighted the role of psychosocial factors, namely, family structure, trauma, and family psychiatric history and its adverse effects on the well-being of children. The importance lies in recognizing at risk populations, including children and families, and intervening early so as to get back on normal trajectory. This may impact early intervention strategies targeting reduction in morbidity and mortality.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Avison WR. Family structure and mental health. Ch. 12. London, Ontario, Canada: The University of Western Ontario; 2002. [Google Scholar]
- 2.Oliver WJ, Kuhns LR, Pomeranz ES. Family structure and child abuse. Clin Pediatr (Phila) 2006;45:111–8. doi: 10.1177/000992280604500201. [DOI] [PubMed] [Google Scholar]
- 3.Cherlin AJ, Furstenberg FF, Jr, Chase-Lansdale L, Kiernan KE, Robins PK, Morrison DR, et al. Longitudinal studies of effects of divorce on children in Great Britain and the United States. Science. 1991;252:1386–9. doi: 10.1126/science.2047851. [DOI] [PubMed] [Google Scholar]
- 4.Holden KC, Smock PJ. The economic costs of marital dissolution: Why do women bear a disproportionate cost? Annu Rev Sociol. 1991;17:51–78. doi: 10.1146/annurev.so.17.080191.000411. [DOI] [PubMed] [Google Scholar]
- 5.Brown GW, Harris T. Stressors and aetiology of depression: A comment on Hällström, March 11, 1987. Acta Psychiatr Scand. 1987;76:221–3. doi: 10.1111/j.1600-0447.1987.tb02889.x. [DOI] [PubMed] [Google Scholar]
- 6.Offord DR, Boyle MH, Jones BR. Psychiatric disorder and poor school performance among welfare children in Ontario. Can J Psychiatry. 1987;32:518–25. doi: 10.1177/070674378703200704. [DOI] [PubMed] [Google Scholar]
- 7.Turner RJ, Lloyd DA. Lifetime traumas and mental health: The significance of cumulative adversity. J Health Soc Behav. 1995;36:360–76. [PubMed] [Google Scholar]
- 8.Kellam SG, Ensminger ME, Turner RJ. Family structure and the mental health of children. Concurrent and longitudinal community-wide studies. Arch Gen Psychiatry. 1977;34:1012–22. doi: 10.1001/archpsyc.1977.01770210026002. [DOI] [PubMed] [Google Scholar]
- 9.Keller MB, Beardslee WR, Dorer DJ, Lavori PW, Samuelson H, Klerman GR. Impact of severity and chronicity of parental affective illness on adaptive functioning and psychopathology in children. Arch Gen Psychiatry. 1986;43:930–7. doi: 10.1001/archpsyc.1986.01800100020004. [DOI] [PubMed] [Google Scholar]
- 10.Yampolskaya S, Mowery D, Dollard N. Predictors for readmission into children's inpatient mental health treatment. Community Ment Health J. 2013;49:781–6. doi: 10.1007/s10597-013-9592-8. [DOI] [PubMed] [Google Scholar]


