To the Editor
Eyes with a history of refractive surgery render intraocular lens (IOL) power selection particularly difficult, but intraoperative wavefront aberrometry has shown promising results.1,2 Although it is uncommon for eyes to have significant residual corneal astigmatism after refractive surgery, such cases do exist and present an extra challenge.
We retrospectively assessed the accuracy of the ORA system for toric IOL power selection in eyes with a history of refractive surgery and significant residual astigmatism. More than 200 records of eyes that underwent cataract surgery with the ORA system were reviewed and 15 eyes were identified that underwent toric IOL implantation. Twelve eyes had a history of myopic LASIK and three of hyperopic LASIK. The ORA predictive accuracy was compared to the SRK-T formula using axial length measurements from the IOLMaster (Carl Zeiss Meditec, Dublin, CA) and keratometry values from the IOLMaster or corneal topography and the American Society of Cataract and Refractive Surgery (ASCRS) online calculator. Preoperative cylinder power and axis were calculated using the Alcon AcrySof or the Abbott Medical Optics toric calculators. Postoperatively, corrected distance visual acuity and manifest refraction 1 month after cataract surgery were recorded.
Axial length ranged from 22.67 to 27.72 mm and average keratometry values from 38.87 to 48.29 D. The IOL spherical power changed from the preoperative plan in 11 eyes, with a 1.50-D or greater change in 3 eyes. The IOL cylindrical power changed in 5 eyes (33%). Mean preoperative keratometric astigmatism was 2.09 ± 0.67 D. The mean residual astigmatic prediction using the ORA system was 0.64 ± 0.61 D and the mean postoperative manifest astigmatism was 0.74 ± 0.63 D. Twenty-seven percent of the eyes had 0.25 D or less of astigmatism postoperatively, 47% had 0.50 D or less, 60% had 0.75 D or less, and 73% had 1.00 D or less.
The mean ORA prediction error was 0.43 ± 0.33 D, compared to a mean prediction error of 0.77 ± 0.56 D for the calculated preoperative lens choice using the IOLMaster (t test, P = .03) and 0.61 ± 0.34 D using the online ASCRS calculator (t test, P = .08). As seen in Figure 1, which summarizes the postoperative spherical equivalent for all eyes, 80% of the treated eyes ended up with a spherical equivalent of 0.75 D or less, whereas only 53% of them would have achieved this if the calculated preoperative lens per IOLMaster was implanted instead.
Figure.
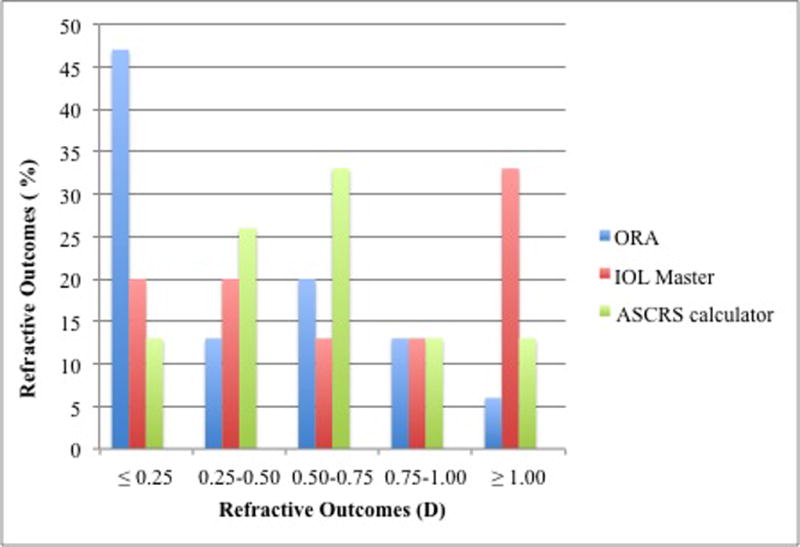
Refractive outcomes with intraoperative wavefront aberrometry (ORA), IOLMaster (Carl Zeiss Meditec, Dublin, CA), and the American Society of Cataract and Refractive Surgery calculator.
This study is the first to report the successful use of intraoperative aberrometry in eyes undergoing toric IOL implantation after refractive surgery. However, our results are limited by the retrospective design of the study and the small number of patients.
References
- 1.Ianchulev T, Hoffer KJ, Yoo SH, et al. Intraoperative refractive biometry for predicting intraocular lens power calculation after prior myopic refractive surgery. Ophthalmology. 2014;121:56–60. doi: 10.1016/j.ophtha.2013.08.041. [DOI] [PubMed] [Google Scholar]
- 2.Canto AP, Chhadva P, Cabot F, et al. Comparison of IOL power calculation methods and intraoperative wavefront aberrometer in eyes after refractive surgery. J Refract Surg. 2013;29:484–489. doi: 10.3928/1081597X-20130617-07. [DOI] [PubMed] [Google Scholar]


