Abstract
Objective
We investigated the relationship between social support and health service use among men and women with depression.
Methods
Participants were 1379 adults with symptoms of depression (Patient Health Questionnaire-9 score ≥5) in the National Health and Nutrition Examination Survey. Using the framework of the Andersen Behavioral Model of Health Services Use, multivariable regression models used social support, stratified by depression severity, to estimate association with utilization of mental health and nonmental health services. Partial F-tests examined a priori interactions between social support and gender.
Results
Among those with adequate social support, odds of seeing a nonmental health provider were much higher when depression was moderate [Odds Ratio (OR): 2.6 (1.3–5.3)] or severe [OR: 3.2 (1.2–8.7)], compared to those lacking social support. Conversely, odds of mental health service use were 60% lower among those with moderate depression [OR: 0.4 (0.2–1.0)] when social support was adequate as opposed to inadequate. Social support was unrelated to service use when depression was mild. Gender moderated the relationship between social support and health service use among individuals with severe depression.
Conclusions
Social support has opposite associations with mental and nonmental health service use among adults with clinically significant depression. This association is largely attributable to the effect of male gender on the relationship between social support and health service use.
Keywords: Depression, Social support, Health service use, NHANES, Gender
1. Introduction
Depression is a preeminent concern in health care as a common condition, leading cause of disability and significant risk factor for suicide [1–3]. Nonetheless, fewer than half of severely depressed individuals are receiving pharmacologic or behavioral treatment [4], just one in ten with persistent depression receive both appropriate medication and counseling [5], and older adults with depression are especially unlikely to utilize mental health services [6].
Among those who do seek professional treatment for depression, the severity of the condition and presence of comorbidities appear to be key factors in the decision to seek treatment [7–10]. This pattern is consistent with Andersen’s Behavioral Model of Health Services Use because in his conceptual model, perceived and evaluated need is the strongest predictor of service use [11]. Additional factors contributing to service use within this model include predisposing factors, such as gender, as well as enabling factors including social support.
Among enabling factors for health service use, social support appears to be of particular importance, but studies have had contradictory results. Some studies have concluded that there is a positive association between social support — which can be emotional (e.g., serving as a confidant), informational (e.g., providing facts on depression treatment) or instrumental (e.g., giving a ride to a doctor’s appointment) [12] — and health service use [13,14], while others have detected inverse associations [15,16]. On the one hand, social support itself — particularly emotional support — might ameliorate or prevent depression symptoms [17,18], and support from family and friends can substitute for formal health service use [19,20], particularly in milder cases of depression [21]. On the other hand, social support may provide the necessary encouragement to seek care [22] especially if loved ones feel that symptoms are severe enough to warrant formal treatment. In addition, family and friends are often willing to act as intermediaries between chronically ill adults and their health care providers [23]. Since the effect size of depression treatment is highly dependent on depression severity [24], examining the association of social support across the entire spectrum of depression severity may also be especially relevant to determination of appropriate health service use.
Women, including those diagnosed with depression [25], have greater odds of service use [6] than men. Socially mediated gender roles have a significant impact on psychosocial factors associated with risk of depression as well as coping strategies [26] and could impact help-seeking behavior [27]. Studies on health service use in men have revealed distinct themes of limited use of support from family and friends, especially from male peers except in cases where the health problem was viewed as normative (e.g. a sports-related injury); if sought, support is mostly garnered from female partners [28]. This may be due in part to the structure of men’s social networks as studies have found men’s networks to be more extensive but less intensive with comparably fewer confidants and receipt of less emotional and health-related support from children and friends [29,30].
Prior psychiatric investigations of social support and health service use have been limited by lack of clear guidance by a conceptual model, as well as inability to conduct nuanced examinations of all three levels of the Andersen model: perceived need, predisposing factors, and enabling factors. Thus, this study examined the association between social support (specifically emotional support) and utilization of health services in a population-based sample of middle-aged and older adults with symptoms of depression through the framework of Andersen’s Behavioral Model of Health Service Use. We hypothesized that this relationship was primarily moderated by the primary need factor, severity of depression. Specifically, we hypothesized that increased social support would be associated with decreased service use among those with mild depression, while increased service use would be observed along with symptoms of moderate to severe depression. We further hypothesized that gender would lead to differentiation in probability of utilizing health services. Specifically, we suspected that among depressed women, increased social support would be associated with increased health service use, while among similar men, increased social support would not be associated with health service use. This hypothesis is based on the research outlined above showing that male-gender roles and social norms shape both the quality of men’s social networks and whether or not it would be socially appropriate to admit requiring or seeking help.
2. Methods
2.1. Survey Sample
We conducted a cross-sectional analysis of data drawn from the 2005–2006 and 2007–2008 waves of the National Health and Nutrition Examination Survey (NHANES), an annual survey of health and nutritional status in the US conducted by the National Center for Health Statistics (NCHS), Centers for Disease Control and Prevention [31]. We restricted our analyses to these two waves of NHANES as they were the only to include both measurement of social support and depression severity assessed by the Patient Health Questionnaire (PHQ-9). Per NHANES protocol, trained NCHS interviewers conduct face-to-face interviews and collect physical examination data from about 5000 nationally representative children and adults each year. Complex sampling methodology is used to create a nationally representative sample. Non-Hispanic Blacks and Mexican Americans are oversampled [32]. The present analysis was limited to adults aged 40 years and older (as social support was not assessed in younger participants) who had a PHQ-9 score of 5 or greater, indicating at least mild depression (N=1426). Fifty people were excluded for missing data for any of the main predictors or outcome variables, leaving a final sample of 1376 adults.
2.2. Measures
2.2.1. Dependent Variables: Health Service Use
We constructed four binary variables for health service use in the last year: 1) Saw a nonmental health service provider; 2) saw a mental health service provider; 3) utilized antidepressants; and 4) utilized mental health services, which was defined as having seen a mental health provider and/or utilized antidepressants. Participants were initially asked how many times they saw a doctor or other healthcare professional in the past year. Those responding one or greater visits in the past year were subsequently asked if they saw or talked to a mental health professional in the past year and were given examples of a psychologist, psychiatrist, psychiatric nurse or clinical social worker. Individuals were documented as not seeing any provider if they reported less than one visit in the past year. Of those individuals reporting one or greater visits in the past year, those responding “no” to the subsequent mental health question were documented as having seen only nonmental health providers, and those responding “yes” were documented as having seen a mental health provider. Participants were asked if they have used or taken medication in the past month for which a prescription is needed. Those who answered “yes” were asked to show the interviewer the container or report the complete name of the medication. The majority of participants were able to provide the container. Medications were automatically categorized for indication, including as an antidepressant, upon entry by the interviewer into the Lexicon Plus ®.
2.2.2. Independent Variable: Social Support
Perceived adequacy of social support consisted of three levels: adequate, somewhat inadequate and inadequate. Presence of perceived social support was measured by a single question, “Can you count on anyone to provide you with emotional support?” We focus on the emotional aspect of social support because prior empirical research has demonstrated that this is a key component of social support [33] and is closely associated with depression [17]. In addition, we examine self-perceived adequacy of social support because psychometric studies of emotional support typically assess an individual’s perception of the availability of someone to discussion problems or emotional difficulties [34]. Available response options were “doesn’t need help,” “no” or “yes.” There were no individuals in our analytic sample who responded “doesn’t need help.” Those who responded “no” were classified as inadequate support. Individuals responding “yes” to this question were asked to rate the adequacy of social support via two subsequent questions. For the question “In the last 12 months, could you have used more emotional support than you received?” those who responded “no” were classified as adequate support. Those who responded “yes” were asked, “Would you say that you could have used [a little/some/a lot] more social support?” Those who responded “a little/some” were classified as somewhat inadequate support, and those who responded “a lot more” as inadequate support. These questions are based on well-validated scales from the MacArthur studies on successful aging [35].
2.2.3. Depression Severity
Depression severity was determined with the 9-item PHQ, a brief, reliable and valid measure [36–38]. The PHQ-9 assesses symptoms of a major depressive episode in the preceding 2 weeks, with a score range of 0 to 27. Participants were classified based on their total score as having mild (5–9), moderate (10–14) and moderately severe to severe depression (15–27), clinically relevant cutoffs that have been previously validated [37,38].
2.2.4. Covariates
Covariate adjustment was framed by the Andersen behavioral model of healthcare utilization [39]. Thus, we included several factors that would be considered predisposing factors (age, gender, race/ethnicity and education level), enabling factors (ratio of family income to poverty, health insurance status, marital status, whether or not individual lives alone, days of church attendance and number of close relationships) and additional need factors (general health condition and activities of daily living (ADL) score) [40]. Number of close relationships is included as a potential enabling factor because social support is derived from individuals in a person’s social network. General health condition was assessed with the question, “Would you say your health in general is excellent, very good, good, fair, or poor?” The NHANES ADL instrument is a 16-item questionnaire that measures constructs associated with locomotion and transfers, household productivity, social integration and manipulation of surroundings. Item scores range from “1” (no difficulty) to “4” (unable to do).
2.3. Statistical analyses
Analyses were conducted using Stata/IC Version 13.1 (College Station, TX, USA: StataCorp LP). Survey settings were utilized to allow for adjustment of weights, clusters and strata. Frequency and percentage were calculated for categorical variables, while mean and standard error were calculated for continuous variables. All reported percentages, means and standard errors are weighted. Tests of interaction between perceived support and severity of depression in a minimally adjusted model (sample weights, clusters and strata) were significant (P<0.1) for all outcomes. To facilitate interpretability, subsequent analyses were performed, and results were reported with depression severity stratified as mild, moderate and moderately severe to severe. For multivariable regression models, we used a backward stepwise elimination procedure and removed any variables producing a change of <10% in the independent variable’s Odds Ratio (OR) in one or more depression severity strata. Step 1 in the procedure contained predisposing variables (Model 1), Step 2 added enabling variables (Model 2) and, lastly, Step 3 further added need variables (Model 3).
Partial F-tests tested a priori interaction between perceived social support and gender. While moderation was assessed within all strata of depression severity, we focused primarily on interactions among those with moderately severe to severe depression because health service use and clinical care is most indicated for these groups. Significance of interactions was established at P<0.10 and P<0.05 for other analyses [41].
There was no more than 10% missing data for relevant variables across participants; thus, complete case data were used for analyses. We employed the use of propensity scores (PSs) to conduct a sensitivity analysis on the estimates in our final model (Model 3). Ordinal logistic regression of social support using all predisposing, enabling and need factors was conducted to compute the PS. This sensitivity analysis was conducted to address potential selection bias since our independent variable is based on one’s perception, which can be influenced by factors like culture, gender and age.
3. Results
3.1. Sample Description
The analytic sample was predominantly female, non-Hispanic White, married and insured (Table 1). The majority of participants were classified as mildly depressed (67.2%). A total of 441 (36.4%) of participants utilized mental health services in the past year; 17.1% saw a mental health provider, and 29.7% received antidepressants. More specifically, 132 (11.1%) participants reported both receiving antidepressants and having seen a mental health provider, 85 (7.5%) reported seeing a mental health provider but not receiving antidepressants, and 224 (17.8%) were receiving antidepressants yet reported not having seen a mental health provider in the past year. The majority of our sample, 814 people (55.1%), reported seeing nonmental health providers but not receiving antidepressants. One hundred twenty-one (8.5%) reported that they did not see any providers and they did not receive antidepressants.
Table 1.
Characteristics of the analytic sample stratified by perceived level of social support (N=1376): NHANES 2005–2008.a
| Total
|
Inadequate (n=337) | Somewhat inadequate (n=294) | Adequate (n=745) | |
|---|---|---|---|---|
| N (%) or mean±SE | ||||
| Predisposing factors | ||||
| Age (years) | ||||
| 40–64 | 957 (77.3) | 255 (81.7) | 224 (82.5) | 478 (77.3) |
| ≥65 | 419 (22.7) | 82 (18.3) | 70 (17.5) | 267 (22.7) |
| Female gender | 835 (62.8) | 194 (57.1) | 197 (66.4) | 444 (63.5) |
| Race/Ethnicity | ||||
| Non-Hispanic White | 706 (73.1) | 146 (63.2) | 140 (73.2) | 420 (76.7) |
| Mexican American | 213 (6.0) | 69 (9.7) | 54 (7.1) | 90 (4.2) |
| Non-Hispanic Black | 292 (11.5) | 61 (12.4) | 67 (11.7) | 164 (11.1) |
| Other | 165 (9.4) | 61 (14.7) | 33 (8.1) | 71 (8.0) |
| Education level | ||||
| Less than high school | 508 (24.8) | 148 (28.8) | 98 (21.7) | 262 (24.6) |
| High school diploma, General Educational Development or equivalent | 338 (28.6) | 76 (29.1) | 80 (28.0) | 182 (28.6) |
| Some college or more | 530 (46.6) | 113 (42.1) | 116 (50.3) | 301 (46.8) |
| Enabling factors | ||||
| Ratio of family income to poverty | ||||
| ≤99% | 419 (21.7) | 133 (31.2) | 91 (20.9) | 195 (18.6) |
| 100–299% | 609 (40.9) | 159 (47.2) | 120 (42.2) | 330 (38.0) |
| 300–499% | 193 (20.0) | 28 (11.9) | 41 (16.0) | 124 (24.6) |
| ≥500% | 155 (17.4) | 17 (9.7) | 42 (20.9) | 96 (18.8) |
| Covered by health insurance | 1097 (81.1) | 244 (69.4) | 232 (82.4) | 621 (84.9) |
| Marital status | ||||
| Married/Cohabitating | 744 (59.2) | 153 (44.6) | 160 (58.6) | 431 (64.8) |
| Divorced/Separated | 324 (23.3) | 103 (32.7) | 65 (24.4) | 156 (19.5) |
| Widowed | 190 (10.5) | 40 (10.6) | 44 (9.6) | 106 (10.8) |
| Never married | 118 (6.9) | 41 (12.0) | 25 (7.4) | 52 (4.9) |
| Lives alone in household | 302 (21.6) | 90 (30.4) | 64 (22.7) | 148 (17.9) |
| How often attends church (days) | 30.09±1.73 | 28.7±3.6 | 29.2±2.8 | 30.9±2.2 |
| Number of close relationships | ||||
| 0 | 91 (5.6) | 54 (12.2) | 13 (4.4) | 24 (2.0) |
| 1 to 4 | 704 (48.2) | 203 (61.8) | 160 (48.6) | 341 (43.1) |
| 5 to 8 | 329 (27.8) | 42 (14.8) | 68 (25.2) | 219 (33.5) |
| ≥9 | 252 (19.4) | 38 (11.2) | 53 (21.8) | 161 (21.4) |
| Need factors | ||||
| General health condition | ||||
| Very good to excellent | 230 (21.0) | 45 (16.3) | 45 (19.5) | 140 (23.2) |
| Good | 449 (36.8) | 107 (33.2) | 98 (39.6) | 244 (37.1) |
| Fair to poor | 697 (42.2) | 185 (50.5) | 151 (40.9) | 361 (39.7) |
| ADL score | 6.26±0.30 | 8.1±0.7 | 6.3±0.5 | 5.6±0.3 |
| Depression severityb | ||||
| Mild | 878 (67.2) | 159 (45.8) | 190 (70.2) | 529 (73.8) |
| Moderate | 313 (21.6) | 98 (32.9) | 69 (17.8) | 146 (19.0) |
| Moderately severe to severe | 185 (11.2) | 80 (21.3) | 35 (12.0) | 70 (7.2) |
| Dependent variables | ||||
| Saw nonmental health provider | 814 (55.1) | 170 (41.5) | 169 (52.5) | 475 (61.0) |
| Saw mental health provider | 217 (17.1) | 77 (25.0) | 55 (20.9) | 85 (12.9) |
| Utilized antidepressants | 356 (29.7) | 93 (31.2) | 80 (32.0) | 183 (28.3) |
| Utilized mental health services | 441 (36.4) | 122 (41.0) | 100 (39.6) | 219 (33.6) |
All percentages, means and standard errors are weighted using exam weights derived from NHANES 2005–2006 and 2007–2008.
Mild depression: PHQ-9, 5–9; moderate depression: PHQ-9, 10–14; moderately severe to severe depression: PHQ-9, 15–27.
3.2. Association Between Social Support and Health Service Use Across Three Strata of Depression Severity
We first examined results within individuals with mild depression. Adequately supported individuals had 50% greater odds of utilizing a nonmental health provider prior to adjustment for covariates [95% confidence interval (CI): 1.0–2.2]. The point estimate was significant after adjustment for predisposing factors (OR: 1.6; 95% CI: 1.1–2.5; Model 1: Table 2); however, the addition of further need and enabling factors (Models 2–3: Table 2) decreased the precision of the estimate such that results were no longer statistically significant.
Table 2.
Regression models of utilization of mental health care, mental health provider visits and utilization of antidepressants as a function of perceived social support stratified by depression severity.a
| Mild depression (n=878) | Moderate depression (n=313) | Moderately severe to severe depression (n=185) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||||||||
| Inadequate (N=159) | Somewhat inadequate (n=190) | Adequate (n=529) | Inadequate (N=98) | Somewhat inadequate (n=69) | Adequate (n=146) | Inadequate (N=80) | Somewhat inadequate (n=35) | Adequate (n=70) | |||||||
|
|
|
|
|
|
|
|
|
|
|||||||
| OR | OR | 95% CI | OR | 95% CI | OR | OR | 95% CI | OR | 95% CI | OR | OR | 95% CI | OR | 95% CI | |
| Unadjusted model | |||||||||||||||
| Saw nonmental health provider | Ref | 1.2 | 0.8–1.8 | 1.5 | 1.0–2.2 | Ref | 1.2 | 0.5–2.7 | 2.1 | 1.2–3.9 | Ref | 1.3 | 0.4–4.8 | 3.1 | 1.3–7.4 |
| Saw mental health provider | Ref | 0.9 | 0.4–2.2 | 0.9 | 0.4–1.9 | Ref | 1.3 | 0.5–3.1 | 0.4 | 0.2–0.9 | Ref | 1.3 | 0.5–3.8 | 0.4 | 0.2–0.8 |
| Utilized antidepressants | Ref | 1.5 | 0.8–2.8 | 1.4 | 0.8–2.6 | Ref | 1.6 | 0.7–3.5 | 1.0 | 0.5–1.8 | Ref | 0.8 | 0.3–2.3 | 0.7 | 0.3–1.7 |
| Utilized mental health services | Ref | 1.4 | 0.8–2.5 | 1.4 | 0.8–2.3 | Ref | 1.1 | 0.5–2.5 | 0.6 | 0.3–1.1 | Ref | 1.5 | 0.6–3.9 | 0.7 | 0.3–1.5 |
| Model 1b | |||||||||||||||
| Saw nonmental health provider | Ref | 1.5 | 0.9–2.3 | 1.6 | 1.1–2.5 | Ref | 1.1 | 0.5–2.4 | 2.2 | 1.2–4.0 | Ref | 1.9 | 0.5–7.2 | 3.6 | 1.4–9.1 |
| Saw mental health provider | Ref | 0.8 | 0.4–1.8 | 0.8 | 0.4–1.7 | Ref | 1.3 | 0.6–3.1 | 0.4 | 0.2–1.1 | Ref | 1.2 | 0.4–4.2 | 0.4 | 0.2–0.9 |
| Utilized antidepressants | Ref | 1.1 | 0.5–2.4 | 1.1 | 0.6–2.2 | Ref | 1.8 | 0.8–3.9 | 0.9 | 0.5–1.7 | Ref | 0.4 | 0.1–1.5 | 0.7 | 0.3–1.5 |
| Utilized mental health services | Ref | 1.1 | 0.6–2.1 | 1.2 | 0.7–2.0 | Ref | 1.2 | 0.6–2.6 | 0.6 | 0.3–1.1 | Ref | 0.8 | 0.2–3.0 | 0.6 | 0.3–1.3 |
| Model 2c | |||||||||||||||
| Saw nonmental health provider | Ref | 1.3 | 0.8–2.1 | 1.4 | 0.9–2.3 | Ref | 1.0 | 0.4–2.4 | 2.6 | 1.3–5.4 | Ref | 2.1 | 0.5–8.7 | 3.4 | 1.3–9.3 |
| Saw mental health provider | Ref | 0.9 | 0.4–2.1 | 1.0 | 0.4–2.2 | Ref | 1.3 | 0.6–3.2 | 0.4 | 0.1–1.0 | Ref | 1.0 | 0.3–3.6 | 0.5 | 0.2–1.2 |
| Utilized antidepressants | Ref | 1.1 | 0.5–2.4 | 1.1 | 0.5–2.1 | Ref | 1.4 | 0.6–3.2 | 0.5 | 0.2–1.2 | Ref | 0.4 | 0.1–1.5 | 0.5 | 0.2–1.2 |
| Utilized mental health services | Ref | 1.1 | 0.6–2.2 | 1.2 | 0.6–2.1 | Ref | 1.2 | 0.5–2.8 | 0.4 | 0.2–1.0 | Ref | 0.8 | 0.2–3.8 | 0.6 | 0.3–1.5 |
| Model 3d | |||||||||||||||
| Saw nonmental health provider | Ref | 1.3 | 0.8–2.2 | 1.4 | 0.9–2.3 | Ref | 1.0 | 0.4–2.4 | 2.6 | 1.3–5.3 | Ref | 2.3 | 0.5–9.4 | 3.2e | 1.2–8.7 |
| Saw mental health provider | Ref | 0.9 | 0.4–2.1 | 1.0 | 0.4–2.2 | Ref | 1.3e | 0.6–3.2 | 0.4 | 0.2–1.0 | Ref | 1.2e | 0.4–3.7 | 0.6 | 0.2–1.6 |
| Utilized antidepressants | Ref | 1.1 | 0.5–2.5 | 1.1 | 0.5–2.1 | Ref | 1.4 | 0.6–3.0 | 0.6 | 0.2–1.4 | Ref | 0.4 | 0.1–1.7 | 0.7e | 0.3–1.5 |
| Utilized mental health services | Ref | 1.1 | 0.6–2.2 | 1.2 | 0.6–2.1 | Ref | 1.1 | 0.5–2.7 | 0.4 | 0.2–1.0 | Ref | 0.8 | 0.2–3.1 | 0.8e | 0.3–1.9 |
Mild depression: PHQ-9, 5–9; moderate depression: PHQ-9, 10–14; moderately severe to severe depression: PHQ-9, 15–27. All presented odds ratios are pooled estimates adjusted for survey weights, sampling units, and strata.
Adjusted for predisposing factors (age, gender, race and education).
Adjusted for all variables in Model 1 as well as enabling factors (income to poverty ratio, insurance status, marital status, whether or not they live alone, days of church attendance and number of close relationships).
Adjusted for all variables in Model 2 as well as additional need factors (ADL score and general health condition).
Significant interaction with gender.
Next, we analyzed individuals with moderate depression. Adequately supported individuals were significantly more likely to see a nonmental health provider, and upon adjustment for potential confounders, this association grew such that the odds of adequately supported individuals seeing a nonmental health provider were 2.6 times the odds of those who were inadequately supported (Table 2; Model 3; 95% CI: 1.3–5.3). Conversely, adequately supported individuals had 60% lower odds of seeing a mental health provider and utilizing mental health services overall (OR: 0.4; 95% CI: 0.2–1.0 for each).
Among those with moderately severe to severe depression, the fully adjusted odds of adequately supported individuals seeing a nonmental health provider were 3.2 times the odds of those who were inadequately supported (Table 2; Model 3; 95% CI: 1.2–8.7). Conversely, odds of seeing a mental health provider were estimated to be 40% lower when social support was adequate. However this estimate was statistically significant only in the unadjusted and predisposing factor-adjusted (Model 1) models.
3.3. Moderators Among Individuals With Moderately Severe to Severe Depression
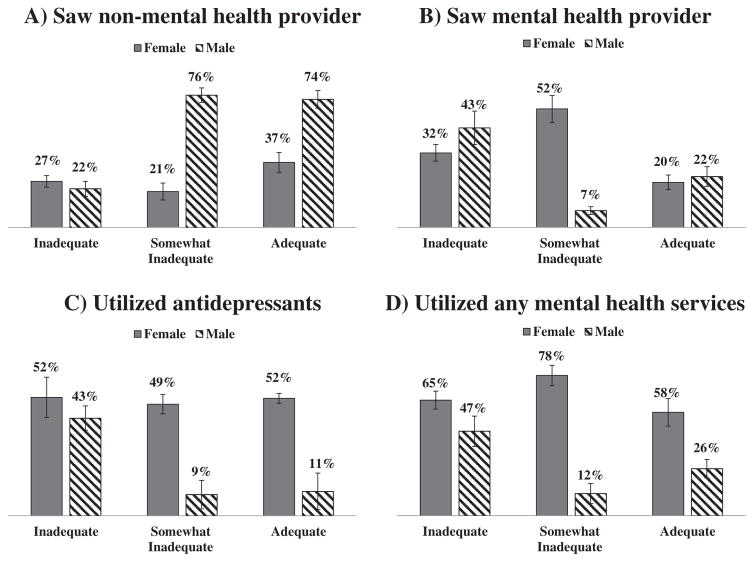
Gender was a significant moderator across all outcome measures (P for interaction of 0.044 for saw nonmental health provider, 0.061 for saw mental health provider, 0.007 for utilized antidepressants and 0.014 for utilized mental health services). Fig. 1 illustrates the proportion of females utilizing services remained largely unchanged despite changes in level of social support. However, a larger proportion of males seeing nonmental health professionals reported adequate support (OR: 12.2; 95% CI: 3.6–41.4; predicted probability: 74% adequate vs. 27% inadequate; Fig. 1a). A smaller proportion of males seeing a mental health provider (OR: 0.3; 95% CI: 0.1–1.1; Fig. 1b), utilizing anti-depressants (OR: 0.1; 95% CI: 0.01–0.4; Fig. 1c) or utilizing any mental health services (OR: 0.2; 95% CI: 0.1–0.7; Fig. 1d) reported adequate social support relative to inadequate support.
Fig. 1.
(a–d) Utilization of health services among those individuals with moderately severe to severe depression (n=185) by gender.
3.4. Sensitivity Analyses
PS were consistent in their distribution across social support strata. All significant associations in our primary analyses were unchanged, with two exceptions. First, the 60% decrease in odds of utilizing mental health services for adequately versus inadequately supported among moderately depressed people became marginally insignificant [PS-adjusted OR: 0.5 (95% CI: 0.3–1.0)]. Second, the 60% lower odds of seeing a mental health provider among severely depressed individuals perceiving adequate support became statistically significant (PS-adjusted OR: 0.4 95% CI: 0.2–0.8).
4. Discussion
This study highlights differing patterns of health service use among adults with clinical symptoms of depression, with patterns varying based on individuals’ depression severity, level of social support and gender. By stratifying results by severity of depression, this study first reveals that social support is associated with health service use almost exclusively among individuals with at least moderate depression. Our analyses further identified that in this population social support is generally associated with increased use of nonmental service use, yet has no correlation (or, in some cases, even a negative one) with mental health service use. Finally, our results suggest that in addition to being an important predisposing factor, one’s gender moderates the relationship between social support and health service use. While women were relatively consistent in their use of health services, men who endorsed adequate social support strongly favored nonmental health service use, a gender effect that may primarily account for the opposing associations between social support and nonmental health versus mental health service use.
These findings both converge with past research and extend our knowledge in several ways. In the Andersen Model need for care factors are the strongest predictors of health care utilization [42]. Our results refine this model by suggesting that need, as defined by severity of depression, does indeed influence the relationship between social support and health service use, yet that use is for other types of health services other than specialty mental health services. We were unable to determine reasons for such use in this study, but it is well known that depression exacerbates outcomes of common chronic medical conditions such as diabetes [43]; thus, it is conceivable that depressed patients are more inclined to seek care for their other medical problems. Prior studies in Europe [13,14] and among all comers with depression [44] have found similar patterns of social support being associated with increased non-mental health but decreased mental health service use among individuals with depression. This study expands on such findings by demonstrating it in a nationally representative sample of middle-aged and older adults in the United States and specifying the pattern as evident only when depression reaches a level that is clinically significant.
Our findings also offer suggestions for designing interventions or programs aimed at enhancing mental health service utilization among individuals with clinically significant depression. Primary care providers appear to be good targets for provision of depression treatment, particularly among men who may hold different normative values about depression treatment [27]. Our descriptive data suggest that the majority of American adults with depressive symptoms may be being seen in primary care settings on an annual basis, which reinforces this setting — provided availability of adequate resources — as one ripe for depression detection and treatment interventions. The collaborative care model that is being increasingly disseminated and integrates depression treatment into primary care [45] seems an especially appropriate mechanism to facilitate depression care among adult men. Primary care providers should consider that men may prefer to obtain depression care through them rather than a mental health provider.
This study has several limitations. First, the cross-sectional design prohibits any causal inferences. Second, the measurement timeframe for variables varied; self-reported health service use was over the last month and year for antidepressant use and seeing a provider, respectively, while depression symptoms were assessed over a 2-week time period. However, we feel that PHQ-9 score is a reasonable proxy for depression in general and can function as a moderator in our analysis due to the often chronic nature of depressive symptoms [46] and the fact that the best predictor for current depression is past depression [47]. Third, we have no information on the quality and content of health provider visits; thus, it is unclear whether and to what extend nonmental health providers may have been providing depression care. It is also possible that the preference for nonmental health visits among men may also reflect a greater prevalence of nonmental health problems requiring nonmental health providers than in women. This possibility is reduced by our adjustment of results by functional status and self-rated health, the latter of which correlates closely with objective ratings of individuals’ medical morbidity [48]. In addition, health service use was predominantly self-reported. Future studies could link NHANES data with administrative databases to help address these information gaps. Fourth, while we included adjustment for a number of potential confounding variables, as well as used PSs in our sensitivity analyses, remaining unmeasured or unobserved confounding variables may explain our observed associations with health service utilization. Finally, major depression remains a clinical diagnosis, and thus, the PHQ-9 cannot diagnose a specific depressive disorder, although it has been shown to be highly sensitive and specific in the diagnosis of depression in the general population [49].
5. Conclusion
This study is one of the first to examine the interplay among depression severity, perceived social support and use of different types of health services in a representative population-based cohort. Our results indicate that among individuals with mild symptoms of depression, social support has no apparent correlation with health service use. Among those individuals with severe enough depression to warrant treatment, increased social support was associated with increased nonmental health service use but decreased mental health service use. This association was largely attributable to the effect of men. Primary care providers may be important resources in encouraging treatment among adults with clinically significant depression.
Acknowledgments
The authors would like to acknowledge Tomi Mori, PhD, for her statistical guidance.
Footnotes
Disclosures
The authors declare that they have no conflict of interest. This material is the result of work supported with resources and the use of facilities at the VA Portland Health Care System and Oregon Health & Science University. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government. All authors report no competing interests.
References
- 1.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–27. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pratt LA, Brody DJ. Depression in the United States household population. NCHS Data Brief 2005–2006. 2008:1–8. [PubMed] [Google Scholar]
- 3.Fiske A, Wetherell JL, Gatz M. Depression in older adults. Annu Rev Clin Psychol. 2009;5:363–89. doi: 10.1146/annurev.clinpsy.032408.153621. http://dx.doi.org/10.1146/annurev.clinpsy.032408.153621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shim RS, Baltrus P, Ye J, Rust G. Prevalence, treatment, and control of depressive symptoms in the United States: results from the National Health and Nutrition Examination Survey (NHANES), 2005–2008. J Am Board Fam Med. 2011;24:33–8. doi: 10.3122/jabfm.2011.01.100121. http://dx.doi.org/10.3122/jabfm.2011.01.100121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Young AS, Klap R, Shoai R, Wells KB. Persistent depression and anxiety in the United States: prevalence and quality of care. Psychiatr Serv. 2008;59:1391–8. doi: 10.1176/appi.ps.59.12.1391. http://dx.doi.org/10.1176/appi.ps.59.12.1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Crabb R, Hunsley J. Utilization of mental health care services among older adults with depression. J Clin Psychol. 2006;62:299–312. doi: 10.1002/jclp.20231. http://dx.doi.org/10.1002/jclp.20231. [DOI] [PubMed] [Google Scholar]
- 7.Haarasilta L, Marttunen M, Kaprio J, Aro H. Major depressive episode and health care use among adolescents and young adults. Soc Psychiatry Psychiatr Epidemiol. 2003;38:366–72. doi: 10.1007/s00127-003-0644-1. http://dx.doi.org/10.1007/s00127-003-0644-1. [DOI] [PubMed] [Google Scholar]
- 8.Hämäläinen J, Isometsä E, Laukkala T, Kaprio J, Poikolainen K, Heikkinen M, et al. Use of health services for major depressive episode in Finland. J Affect Disord. 2004;79:105–12. doi: 10.1016/S0165-0327(02)00342-7. http://dx.doi.org/10.1016/S0165-0327(02)00342-7. [DOI] [PubMed] [Google Scholar]
- 9.Sareen J, Cox BJ, Afifi TO, Yu BN, Stein MB. Mental health service use in a nationally representative Canadian survey. Can J Psychiatry. 2005;50:753–61. doi: 10.1177/070674370505001204. [DOI] [PubMed] [Google Scholar]
- 10.Tylee A. Depression in Europe: experience from the DEPRES II survey. Depression Research in European Society. Eur Neuropsychopharmacol. 2000;10(Suppl 4):S445–8. doi: 10.1016/s0924-977x(00)00112-7. [DOI] [PubMed] [Google Scholar]
- 11.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- 12.Berkman LF, Kawachi I. Social Epidemiology. Oxford University Press; 2000. [Google Scholar]
- 13.Ten HM, Vollebergh W, Bijl R, Ormel J. Combined effect of mental disorder and low social support on care service use for mental health problems in the Dutch general population. Psychol Med. 2002;32:311–23. doi: 10.1017/s0033291701005013. [DOI] [PubMed] [Google Scholar]
- 14.McCracken C, Dalgard OS, Ayuso-Mateos JL, Casey P, Wilkinson G, Lehtinen V, et al. Health service use by adults with depression: community survey in five European countries. Evidence from the ODIN study. Br J Psychiatry. 2006;189:161–7. doi: 10.1192/bjp.bp.105.015081. http://dx.doi.org/10.1192/bjp.bp.105.015081. [DOI] [PubMed] [Google Scholar]
- 15.McGrady A, Lynch D, Nagel R, Wahl E. Application of the high risk model of threat perception to medical illness and service utilization in a family practice. J Nerv Ment Dis. 2003;191:255–9. doi: 10.1097/01.NMD.0000061146.76349.3D. http://dx.doi.org/10.1097/01.NMD.0000061146.76349.3D. [DOI] [PubMed] [Google Scholar]
- 16.Sherbourne CD. The role of social support and life stress events in use of mental health services. Soc Sci Med. 1988;27:1393–400. doi: 10.1016/0277-9536(88)90205-5. [DOI] [PubMed] [Google Scholar]
- 17.Teo AR, Choi H, Valenstein M. Social relationships and depression: ten-year follow-up from a nationally representative study. PLoS One. 2013;8:e62396. doi: 10.1371/journal.pone.0062396. http://dx.doi.org/10.1371/journal.pone.0062396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.George LK, Blazer DG, Hughes DC, Fowler N. Social support and the outcome of major depression. Br J Psychiatry. 1989;154:478–85. doi: 10.1192/bjp.154.4.478. [DOI] [PubMed] [Google Scholar]
- 19.Angermeyer MC, Matschinger H, Riedel-Heller SG. What to do about mental disorder–help-seeking recommendations of the lay public. Acta Psychiatr Scand. 2001;103:220–5. doi: 10.1034/j.1600-0447.2001.103003220.x. [DOI] [PubMed] [Google Scholar]
- 20.Griffiths KM, Crisp DA, Barney L, Reid R. Seeking help for depression from family and friends: a qualitative analysis of perceived advantages and disadvantages. BMC Psychiatry. 2011;11:196. doi: 10.1186/1471-244X-11-196. http://dx.doi.org/10.1186/1471-244X-11-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bristow K, Patten S. Treatment-seeking rates and associated mediating factors among individuals with depression. Can J Psychiatry. 2002;47:660–5. doi: 10.1177/070674370204700708. [DOI] [PubMed] [Google Scholar]
- 22.Spoont MR, Nelson DB, Murdoch M, Rector T, Sayer NA, Nugent S, et al. Impact of treatment beliefs and social network encouragement on initiation of care by VA service users with PTSD. Psychiatr Serv. 2014;65:654–62. doi: 10.1176/appi.ps.201200324. http://dx.doi.org/10.1176/appi.ps.201200324. [DOI] [PubMed] [Google Scholar]
- 23.Rosland A-M, Heisler M, Janevic MR, Connell CM, Langa KM, Kerr EA, et al. Current and potential support for chronic disease management in the United States: the perspective of family and friends of chronically ill adults. Fam Syst Health. 2013;31:119–31. doi: 10.1037/a0031535. http://dx.doi.org/10.1037/a0031535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fournier JC, DeRubeis RJ, Hollon SD, Dimidjian S, Amsterdam JD, Shelton RC, et al. Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA. 2010;303:47–53. doi: 10.1001/jama.2009.1943. http://dx.doi.org/10.1001/jama.2009.1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cohen CI, Magai C, Yaffee R, Walcott-Brown L. Comparison of users and non-users of mental health services among depressed, older, urban African Americans. Am J Geriatr Psychiatry. 2005;13:545–53. doi: 10.1176/appi.ajgp.13.7.545. http://dx.doi.org/10.1176/appi.ajgp.13.7.545. [DOI] [PubMed] [Google Scholar]
- 26.Karger A. Gender differences in depression. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2014;57:1092–8. doi: 10.1007/s00103-014-2019-z. http://dx.doi.org/10.1007/s00103-014-2019-z. [DOI] [PubMed] [Google Scholar]
- 27.Addis ME, Mahalik JR. Men, masculinity, and the contexts of help seeking. Am Psychol. 2003;58:5–14. doi: 10.1037/0003-066x.58.1.5. [DOI] [PubMed] [Google Scholar]
- 28.Tudiver F, Talbot Y. Why don’t men seek help? Family physicians’ perspectives on help-seeking behavior in men. J Fam Pract. 1999;48:47–52. [PubMed] [Google Scholar]
- 29.Stokes J, Levin I. Gender differences in predicting loneliness from social network characteristics. J Pers Soc Psychol. 1986;51:1069–74. doi: 10.1037//0022-3514.51.5.1069. [DOI] [PubMed] [Google Scholar]
- 30.Shumaker SA, Hill DR. Gender differences in social support and physical health. Health Psychol. 1991;10:102–11. doi: 10.1037//0278-6133.10.2.102. [DOI] [PubMed] [Google Scholar]
- 31. [accessed August 10, 2014];NHANES - National Health and Nutrition Examination Survey Homepage. n.d http://www.cdc.gov/nchs/nhanes.htm.
- 32. [accessed March 6, 2015];NHANES - About the National Health and Nutrition Examination Survey. n.d http://www.cdc.gov/nchs/nhanes/about_nhanes.htm.
- 33.Cohen S. Social relationships and health. Am Psychol. 2004;59:676–84. doi: 10.1037/0003-066X.59.8.676. http://dx.doi.org/10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- 34.Cyranowski JM, Zill N, Bode R, Butt Z, Kelly MAR, Pilkonis PA, et al. Assessing social support, companionship, and distress: National Institute of Health (NIH) Toolbox Adult Social Relationship Scales. Health Psychol. 2013;32:293–301. doi: 10.1037/a0028586. http://dx.doi.org/10.1037/a0028586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Seeman TE, Lusignolo TM, Albert M, Berkman L. Social relationships, social support, and patterns of cognitive aging in healthy, high-functioning older adults: MacArthur studies of successful aging. Health Psychol. 2001;20:243–55. doi: 10.1037//0278-6133.20.4.243. [DOI] [PubMed] [Google Scholar]
- 36.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. JAMA. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 37.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kroenke K, Spitzer RL, Williams JBW, Löwe B. The patient health questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen Hosp Psychiatry. 2010;32:345–59. doi: 10.1016/j.genhosppsych.2010.03.006. http://dx.doi.org/10.1016/j.genhosppsych.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 39.Dhingra SS, Zack M, Strine T, Pearson WS, Balluz L. Determining prevalence and correlates of psychiatric treatment with Andersen’s behavioral model of health services use. Psychiatr Serv. 2010;61:524–8. doi: 10.1176/ps.2010.61.5.524. http://dx.doi.org/10.1176/appi.ps.61.5.524. [DOI] [PubMed] [Google Scholar]
- 40.Cook CE, Richardson JK, Pietrobon R. Dimensionality, internal consistency, and item analysis of the national health and nutrition examination surveys activities of daily living instrument among patients with report of low back pain. J Manipulative Physiol Ther. 2006;29:183–9. doi: 10.1016/j.jmpt.2006.01.006. http://dx.doi.org/10.1016/j.jmpt.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 41.Hosmer David W, Lemeshow S, Sturdivant Rodney X. Applied logistic regression. 3. Hoboken, N.J: John Wiley & Sons, Inc; 2013. [Google Scholar]
- 42.De Boer AG, Wijker W, de Haes HC. Predictors of health care utilization in the chronically ill: a review of the literature. Health Policy. 1997;42:101–15. doi: 10.1016/s0168-8510(97)00062-6. [DOI] [PubMed] [Google Scholar]
- 43.Katon W. Depression and diabetes: unhealthy bedfellows. Depress Anxiety. 2010;27:323–6. doi: 10.1002/da.20683. http://dx.doi.org/10.1002/da.20683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Maulik PK, Eaton WW, Bradshaw CP. The role of social network and support in mental health service use: findings from the Baltimore ECA study. Psychiatr Serv. 2009;60:1222–9. doi: 10.1176/appi.ps.60.9.1222. http://dx.doi.org/10.1176/appi.ps.60.9.1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Katon W, Unützer J, Wells K, Jones L. Collaborative depression care: history, evolution and ways to enhance dissemination and sustainability. Gen Hosp Psychiatry. 2010;32:456–64. doi: 10.1016/j.genhosppsych.2010.04.001. http://dx.doi.org/10.1016/j.genhosppsych.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Klein DN, Shankman SA, Rose S. Ten-year prospective follow-up study of the naturalistic course of dysthymic disorder and double depression. Am J Psychiatry. 2006;163:872–80. doi: 10.1176/ajp.2006.163.5.872. http://dx.doi.org/10.1176/appi.ajp.163.5.872. [DOI] [PubMed] [Google Scholar]
- 47.Lewinsohn PM, Zeiss AM, Duncan EM. Probability of relapse after recovery from an episode of depression. J Abnorm Psychol. 1989;98:107–16. doi: 10.1037//0021-843x.98.2.107. [DOI] [PubMed] [Google Scholar]
- 48.Bowling A. Just one question: if one question works, why ask several? J Epidemiol Community Health. 2005;59:342–5. doi: 10.1136/jech.2004.021204. http://dx.doi.org/10.1136/jech.2004.021204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kocalevent R-D, Hinz A, Brähler E. Standardization of the depression screener patient health questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. 2013;35:551–5. doi: 10.1016/j.genhosppsych.2013.04.006. http://dx.doi.org/10.1016/j.genhosppsych.2013.04.006. [DOI] [PubMed] [Google Scholar]