Abstract
The present study examined the association between history of nonsuicidal self-injury (NSSI) and history of suicide attempts (SA) among 292 Iraq/Afghanistan veterans, half of whom carried a lifetime diagnosis of posttraumatic stress disorder (PTSD). Consistent with hypotheses, veterans who reported a history of NSSI were significantly more likely to report a history of SA than veterans without a history of NSSI. In addition, logistic regression demonstrated that NSSI remained a significant predictor of SA even after a wide range of covariates (i.e., combat exposure, traumatic brain injury, PTSD depression, alcohol dependence) were considered. Taken together, these findings suggest that clinicians working with veterans should include NSSI history as part of their standard risk assessment battery.
Keywords: Nonsuicidal self-injury, suicide, suicide attempts, suicidal ideation, PTSD, depression, veterans
1. Introduction
Nonsuicidal self-injury (NSSI) refers to the act of intentionally destroying one’s own body tissue without conscious suicidal intent (Chapman et al., 2006; Suyemoto, 1998). It is estimated that approximately 4–6% of adults in the general population engage in NSSI at some point during their lifetime (Briere and Gil, 1998; Klonsky, 2011). However, lack of a precise nomenclature for NSSI often leads to differing rates across populations (Crosby et al., 2011; Silverman et al., 2007). Common NSSI methods include cutting (35%), burning (31%), hitting (31%), and biting (31%; Klonsky, 2011), although approximately half of individuals who engage in NSSI use multiple methods (Klonsky, 2011). Notably, population-based studies indicate that NSSI is not related to gender, ethnicity, income, or education (Briere and Gil, 1998; Klonsky, 2011). These findings challenge the long-held belief that NSSI is more common in women (e.g., Miller, 1994), and indicate that this issue exists in a multitude of populations. NSSI is, however, significantly more common among individuals with a history of mental health treatment (Bentley et al., 2015; Briere and Gil, 1998; Klonsky, 2011). For instance, Briere and Gil (1998) reported that 21% of a psychiatric patient sample (73% of whom carried a diagnosis of PTSD) reported engaging in NSSI during the previous 6 months.
1.1 Nonsuicidal self-injury in veterans
Rates of NSSI in non-treatment seeking veteran samples range from 2.8%–14% (Bryan and Bryan, 2014; Kimbrel et al., 2015; Pinder et al., 2011; Swanell et al., 2014). However, rates of NSSI in veterans seeking treatment for PTSD appear to be markedly higher. For example, Sacks and colleagues (2008) examined rates of NSSI among a sample of primarily Vietnam-era veterans seeking treatment for PTSD and found that 66% reported a lifetime history of NSSI, whereas 55% reported engaging in NSSI during the past two weeks. More recently, Kimbrel and colleagues (2014a) examined the prevalence of NSSI among a sample of male Iraq/Afghanistan-era veterans seeking treatment for PTSD and found that 57% reported lifetime NSSI, whereas 45% reported NSSI during the previous two weeks. These findings are consistent with findings from the civilian literature demonstrating that PTSD is one of the psychiatric disorders that is most strongly associated with NSSI (e.g., Bentley et al., 2015).
1.2 Nonsuicidal self-injury and suicidal behavior
While inherent in the definition of NSSI is a lack of suicidal intent, a strong body of research among civilian samples indicates that NSSI is consistently associated with increased risk for engaging in suicidal behavior (e.g., Asarnow et al., 2011; Hamza et al., 2012; Klonsky et al., 2013). For example, Klonsky and colleagues (2013) recently demonstrated that NSSI was more strongly associated with history of suicide attempts (SA) than depression, anxiety, and borderline personality disorder (BPD) across multiple civilian samples. These and other similar findings (e.g., Asarnow et al., 2011; Hamza et al., 2012) are consistent with Joiner’s (2005) proposal that NSSI increases risk for suicidal behavior by increasing individuals’ acquired capability for suicide. Specifically, the repetition of bodily harm is proposed to enhance individuals’ tolerance of physiological pain and to diminish their fear of death and/or bodily harm, which, in turn, is proposed to increase their capability to engage in suicidal behavior (Joiner, 2005; Nock et al., 2006).
To date, there has been only limited research aimed at examining the association between NSSI and suicidal behavior in veterans. Specifically, Kimbrel and colleagues (2014a; 2015a) have shown that NSSI is associated with increased risk for suicidal ideation in two cohorts of Iraq/Afghanistan-era veterans, whereas Bryan and colleagues (2015) recently demonstrated that NSSI was prospectively associated with subsequent SA (HR = 2.25, p < 0.05) among 152 active-duty soldiers with a recent history of suicidal ideation or SA.
1.3 Study objective
Given the increasing evidence that veterans with PTSD and other mental health disorders are at elevated risk for suicidal behavior and death by suicide (e.g., Bullman and Kang, 1994; DeBeer et al., 2014; Kang and Bullman, 2008; U.S. Department of Veterans Affairs, 2013; Kaplan, Huguet, McFarland, and Newsom, 2007; Kimbrel et al., 2014b), there is a significant need for additional studies aimed at elucidating the association between NSSI and suicide attempts in veterans, as this important association has only been examined in one prior study with an active duty military sample (Bryan et al., 2015). Accordingly, the aim of the present research was to examine the association between history of NSSI and history of SA in a cross-sectional sample of 292 Iraq/Afghanistan-era veterans. Consistent with prior research in this area (e.g., Bryan et al., 2015; Klonsky et al., 2013), we hypothesized that NSSI would be associated with risk for SA at the bivariate level. We further expected that the hypothesized association between NSSI and SA would remain significant after a wide range of potential confounding variables were considered. Specifically, since gender, age, race, sexual orientation, combat exposure, PTSD, major depressive disorder (MDD), alcohol dependence, and traumatic brain injury (TBI) have all been previously associated with suicidal behavior (Kessler et al., 1999; Nock and Kessler, 2006; Nock et al., 2010; Remafedi et al., 1998; Bryan et al., 2013; Martin et al., 2012; Blosnich et al., 2012), we included these covariates in the logistic regression model to determine if NSSI would be uniquely associated with SA above and beyond the effects of these established predictors.
2. Method
2.1 Participants
A total of 345 Iraq/Afghanistan-era veterans were recruited from the Central Texas region of the United States to participate in the parent study. To be eligible, participants had to be U.S. veterans who had deployed in support of the conflicts in Iraq and Afghanistan following September 11th, 2001. Participants could not meet criteria for either bipolar disorder or a psychotic disorder. Participants were also required to be stable on medications and therapy at the baseline assessment to control for recent symptom fluctuations. In addition, participants could not be in acute suicidal crisis necessitating immediate intervention, nor could they be planning on moving out of the catchment area in the immediate future, as the primary goal of the parent study was to study long-term functional recovery among Iraq/Afghanistan-era veterans with more common mental health problems, particularly PTSD and depression. Accordingly, veterans with PTSD and depression (but without a diagnosis of bipolar disorder or psychosis) who were enrolled in the VA healthcare system were oversampled through targeted advertisements, mailings, and referrals from clinical providers. Women were also oversampled.
Using these criteria, a total of 309 participants were deemed eligible for the parent study (21 were ruled out due to bipolar/psychosis, 13 were unable to complete all of the assessment procedures, 1 was not an Iraq/Afghanistan-era veteran, and 1 was planning on relocating in the near future). In addition, because data concerning lifetime history of NSSI and SA were not collected from 17 of the 309 Iraq/Afghanistan-era veterans enrolled in the parent study, the current analyses were limited to the 292 eligible Iraq/Afghanistan-era veterans who had complete NSSI and SA history data available for analysis from the baseline assessment.
Approximately one-third (32.5%) of the sample was female. Approximately one-fourth of the sample was Latino (19.5%). The majority of participants were White/Caucasian (56.8%); however, African Americans (33.2%) and American Indians/Alaska Natives (5.8%) were also well represented. With respect to sexual orientation, 95.8% of the sample identified as heterosexual, 1.4% as homosexual, 0.7% as bisexual, 0.3% were unsure, and 0.3% classified themselves as “other” (categories are not mutually exclusive). In addition, approximately 3% (n = 9) of the sample chose to not answer the question concerning their sexual orientation. On average, participants had 14.2 (SD = 2.1) years of education. The majority (86.5%) of participants had served in the served in the Army; 6.3% had served in the Air Force, 5.1% in the Marine Corps, 2.8% in the Navy, and 8.7% in the National Guard (categories were not mutually exclusive).
2.2 Procedures
All procedures were approved by the Institutional Review Board prior to data collection. Following informed consent, participants completed the battery of clinical interviews and self-report measures described below. All interviews were conducted by clinical psychologists and masters-level clinicians who were required to complete extensive training procedures prior to being allowed to conduct interviews independently. In addition, all clinical interviews were reviewed during diagnostic review groups that were led by experienced clinical psychologists. Diagnostic consensus was reached on all cases.
2.3 Measures
The Columbia Suicide Severity Rating Scale (CSSRS; Posner et al., 2011) was used to assess lifetime history of NSSI and SA. Consistent with the Self-Directed Violence Classification System used in the VA healthcare system, NSSI was defined as non-suicidal self-directed violence, and SA were defined as suicidal self-directed violence (Crosby et al., 2011). Note that the current analyses were restricted to actual SA only. Thus, interrupted and aborted SA were not included in the SA variable used in the present analyses. The Clinician Administered PTSD Scale for DSM-IV (CAPS-IV; Blake et al., 1995) was used to diagnose lifetime PTSD in relation to the most severe event identified during participants’ military service as part of the Iraq and Afghanistan conflicts. The Structured Clinical Interview for DSM-IV (SCID-IV; First et al., 1994) was used to diagnose lifetime MDD and alcohol dependence. A clinician administered TBI interview (Vasterling, 2008; Morissette et al., 2011) based on American Congress of Rehabilitation Medicine guidelines (Gerberding and Binder, 2003) was used to assess TBI. The Critical Warzone Experiences Scale (CWE; Kimbrel et al., 2014c) was used to assess combat exposure. Note that the PTSD, depression, alcohol dependence, TBI, NSSI, and SA variables used in the present analyses were all lifetime history variables.
2.4 Data analytic plan
Descriptive statistics were calculated for the clinical measures. Chi-square tests and t-tests were used to examine bivariate associations between SA and predictors (Table 1). Hierarchical logistic regression was used to determine if NSSI would remain a significant predictor of SA after accounting for the potential influence of demographic variables [gender (female = 0; male = 1), age, race (non-white = 0; white = 1), sexual orientation (heterosexual = 0; non-heterosexual = 1)], combat exposure, TBI, and psychopathology (PTSD, MDD, and alcohol dependence). Lifetime history of SA served as the dependent variable. Gender, age, race, sexual orientation, and combat exposure were entered in step 1. TBI, PTSD, MDD, and alcohol dependence were entered in step 2. NSSI was entered in step 3.
Table 1.
Summary of Bivariate Associations Between Suicide Attempts and Predictors
| Bivariate Associations Between Suicide Attempts and Categorical Predictors
| |||
|---|---|---|---|
| Variable Name | Lifetime Attempts | Test Statistic | p-value |
| Gender | |||
| Female | 16.8% | χ2 (1) = 6.590 | 0.01 |
| Male | 7.1% | ||
| Race | |||
| Non-White | 10.2% | χ2 (1) = 0.000 | 0.98 |
| White | 10.2% | ||
| Sexual Orientation | |||
| Heterosexual | 9.8% | χ2 (1) = 1.064 | 0.30 |
| Non-Heterosexual | 17.6% | ||
| TBI | |||
| No History of TBI | 11.0% | χ2 (1) = 0.066 | 0.78 |
| History of TBI | 10.0% | ||
| PTSD | |||
| No History of PTSD | 7.6% | χ2 (1) = 2.379 | 0.12 |
| History of PTSD | 13.1% | ||
| Depression | |||
| No History of Depression | 3.8% | χ2 (1) = 16.001 | < 0.0001 |
| History of Depression | 18.0% | ||
| Alcohol Dependence | |||
| No History of Alcohol Dependence | 7.0% | χ2 (1) = 7.660 | 0.006 |
| History of Alcohol Dependence | 17.6% | ||
| Nonsuicidal Self-Injury | |||
| No History of Nonsuicidal Self-Injury | 6.9% | χ2 (1) = 53.779 | < 0.0001 |
| History of Nonsuicidal Self-Injury | 61.1% | ||
|
Bivariate Association Between Suicide Attempts and Years of Age | |||
| Mean (SD) | Test Statistic | p-value | |
| No History of Suicide Attempts | 39.4 (9.8) | t = 3.790 | < 0.0001 |
| History of Suicide Attempts | 32.4 (7.6) | ||
|
Bivariate Association Between Suicide Attempts and Combat Exposure | |||
| Mean (SD) | Test Statistic | p-value | |
| No History of Suicide Attempts | 5.1 (5.8) | t = −2.585 | 0.01 |
| History of Suicide Attempts | 8.1 (7.8) | ||
3. Results
3.1 Descriptive statistics
Approximately 10% (n = 30) of the sample had a history of SA, 3% (n = 10) had a history of multiple SA, and 6% (n = 18) had a history of NSSI. In addition, 50% (n = 145) of the sample met criteria for lifetime PTSD, 46% (n = 133) for lifetime depression, and 31% (n = 91) for lifetime alcohol dependence. In addition, 69% (n = 200) of the sample had experienced one or more lifetime TBIs, and 64% (n = 187) reported one or more combat experiences on the CWE.
3.2 Bivariate analyses
Bivariate associations between suicide attempts and predictors are provided in Table 1. Consistent with the main hypothesis, chi-square tests revealed that NSSI was strongly associated with history of SA, χ2(1) = 53.779, p < 0.001, including history of multiple SA, χ2(1) = 34.398, p < 0.001, at the bivariate level. As can be seen in Figure 1, 61.1% of veterans with a history of NSSI had attempted suicide at least once over the course of their lifetime. In addition, 27.8% of veterans with a history of NSSI had made multiple SA.
Figure 1.
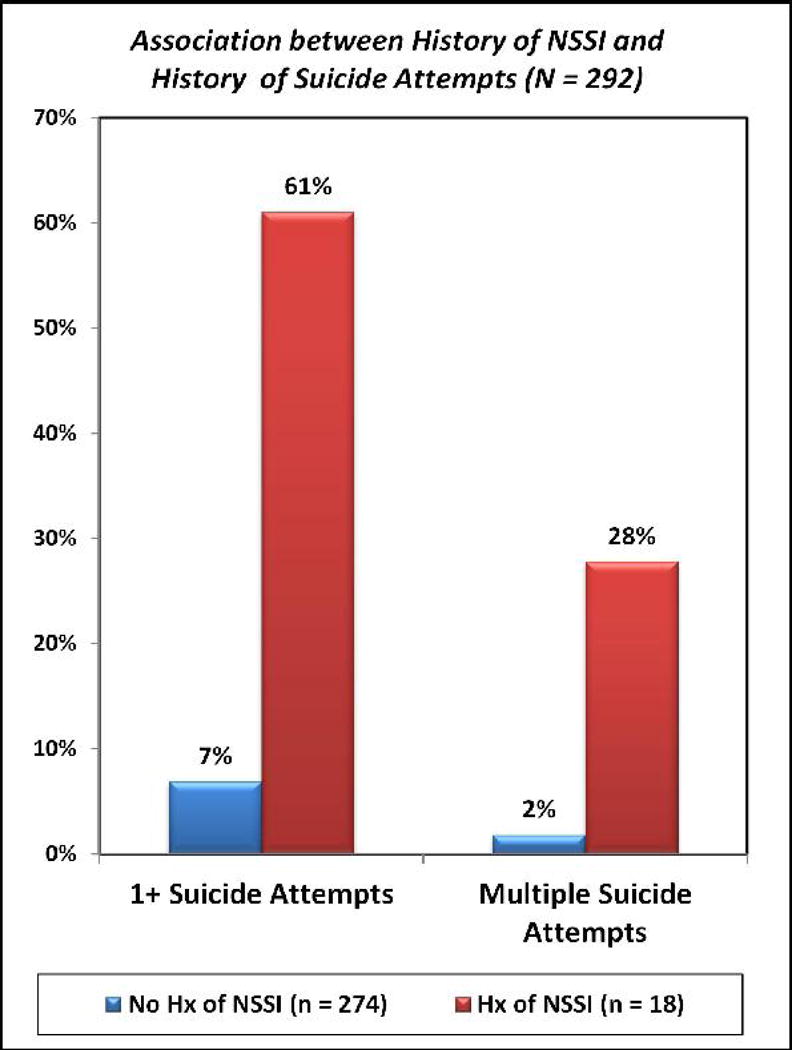
Association between Lifetime History of Nonsuicidal Self-Injury (NSSI) and Lifetime History of Suicide Attempts among Iraq/Afghanistan-era Veterans. Chi-square tests revealed that lifetime history of NSSI was positively associated with history of 1 or more suicide attempts, χ2(1) = 53.779, p < 0.001, and history of multiple suicide attempts, χ2(1) = 34.398, p < 0.001, at the bivariate level.
3.3 Logistic regression model
As can be seen in Table 2, gender, OR = 0.224, p = 0.003, age, OR = 0.910, p = 0.001, and combat exposure, OR = 1.996, p = 0.005, were significant predictors of SA in step 1 of the logistic regression model. Thus, being female, being younger, and having experienced higher levels of combat exposure were each associated with increased risk for SA. After adding TBI, PTSD, MDD, and alcohol dependence to the model in step 2, gender, OR = 0.240, p = 0.015, age, OR = 0.919, p = 0.003, and combat exposure, OR = 1.907, p = 0.027, continued to have significant effects on SA. Interestingly, MDD, OR = 3.150, p = 0.032, was the only psychopathology variable significantly associated with SA in step 2. Finally, as hypothesized, NSSI was found to be strongly associated with SA in step 3 of the model, OR = 28.494, p < 0.001. Notably, MDD no longer had a statistically significant effect on SA, OR = 2.150, p = 0.183, once NSSI was added to the model in step 3, whereas gender, OR = 0.131, p = 0.004, age, OR = 0.926, p = 0.009, and combat exposure, OR = 3.204, p = 0.002, remained significant. The final model accounted for approximately 43% of the variance in SA (Nagelkerke R2 = 0.429) and correctly classified 90.1% of participants.
Table 2.
Summary of Logistic Regression Models Predicting Suicide Attempts among Veterans
| Nagelkerke R2 | Odds Ratio | 95% Confidence Intervals | ||
|---|---|---|---|---|
| Step 1 | 0.211 | |||
|
| ||||
| Gender | 0.224** | 0.082 – 0.609 | ||
| Age | 0.910** | 0.862 – 0.962 | ||
| Race | 0.968 | 0.401 – 2.388 | ||
| Sexual Orientation | 1.475 | 0.354 – 6.153 | ||
| Combat Exposure | 1.996** | 1.238 – 3.220 | ||
|
| ||||
| Step 2 | 0.274 | |||
|
| ||||
| Gender | 0.240* | 0.076 – 0.754 | ||
| Age | 0.919** | 0.869 – 0.972 | ||
| Race | 0.873 | 0.346 – 2.203 | ||
| Sexual Orientation | 1.122 | 0.251 – 5.020 | ||
| Combat Exposure | 1.907* | 1.076 – 3.379 | ||
| Traumatic Brain Injury | 1.122 | 0.401 – 3.143 | ||
| PTSD | 0.514 | 0.178 – 1.481 | ||
| Depression | 3.150* | 1.101 – 9.010 | ||
| Alcohol Dependence | 2.186 | 0.868 – 5.502 | ||
|
| ||||
| Step 3 | 0.429 | |||
|
| ||||
| Gender | 0.131** | 0.033 – 0.524 | ||
| Age | 0.926** | 0.873 – 0.981 | ||
| Race | 0.833 | 0.304 – 2.287 | ||
| Sexual Orientation | 0.849 | 0.122 – 5.910 | ||
| Combat Exposure | 3.204** | 1.541 – 6.662 | ||
| Traumatic Brain Injury | 0.751 | 0.242 – 2.329 | ||
| PTSD | 0.364 | 0.109 – 1.217 | ||
| Depression | 2.150 | 0.696 – 6.636 | ||
| Alcohol Dependence | 1.961 | 0.696 – 5.523 | ||
| Nonsuicidal Self-Injury | 28.494*** | 6.903 – 117.614 | ||
Note: PTSD = posttraumatic stress disorder. Gender was coded as 0 = female, 1 = male. Race categories were collapsed across groups in order to increase statistical power and coded as 0 = non-white, 1 = white. Sexual orientation categories were collapsed across groups in order to increase statistical power and coded as 0 = heterosexual, 1 = non-heterosexual. The PTSD, depression, alcohol dependence, TBI, and nonsuicidal self-injury variables were all lifetime history variables.
p < 0.05;
p < 0.01;
p < 0.001.
4. Discussion
Consistent with the Interpersonal-Psychological Theory of Suicide (Joiner, 2005) and prior research examining the association between NSSI and SA (e.g., Bryan et al., 2015; Klonsky et al. 2013), the present study found that NSSI was associated with significantly increased risk for SA among Iraq/Afghanistan-era veterans at the bivariate level. Furthermore, the present study adds to the existing literature by demonstrating that NSSI remained predictive of SA, even after a wide range of covariates (e.g., demographic variables, combat exposure, TBI, psychiatric diagnoses) were considered. The latter finding is consistent with findings among civilian samples demonstrating that NSSI remained predictive of SA after accounting for anxiety and depression (Klonsky et al., 2013). The present findings, while cross-sectional in nature, are also consistent with Bryan and colleagues’ (2015) recent finding associating NSSI with SA over time in active-duty military personnel.
Interestingly, the only other variables associated with risk for SA in the final step of the model were combat exposure, gender, and age. While each of these variables has been associated with suicidal behavior in previous research, it is surprising that none of the other established predictors of suicidal behavior examined (i.e., PTSD, MDD, alcohol dependence, TBI) were statistically significant predictors in the final step of the model. While it is possible that the categorical manner in which MDD, PTSD, alcohol dependence, and TBI were assessed may have reduced their predictive power, it is noteworthy that NSSI was also assessed categorically (i.e., present/absent), but still demonstrated a robust association with SA, even after all other variables had been included in the model.
It is also noteworthy that MDD had a statistically significant effect on SA until NSSI was entered into the model. Thus, it is likely that much of the variance that is shared between MDD and SA may also be shared with NSSI. Given that the rate of lifetime NSSI (6.2%) was much lower than the rate of lifetime MDD (45.5%) in the present study, it is likely that the substantially larger effect of NSSI on SA was due in large part to its specificity in relation to SA. That is, it is likely that NSSI, due to its much lower base rate in the present study, produced far fewer false positives than MDD. Such an interpretation is consistent with other recent findings in the field indicating that NSSI is a robust predictor of SA, outperforming depression and anxiety (e.g., Klonsky et al., 2013), and, in some cases, even outperforming history of SA as a predictor of future SA (e.g., Bryan et al., 2015).
Unfortunately, this important clinical issue has been largely overlooked among veteran populations to date. Thus, additional research aimed at further elucidating the association between NSSI and SA among veterans is needed, particularly given recent findings suggesting that NSSI is highly prevalent among both Vietnam- and Iraq/Afghanistan-era veterans seeking treatment for PTSD (Kimbrel et al., 2014a; Sacks et al., 2014).
A closely related point concerns the magnitude of the association between combat exposure (OR = 3.204, p < 0.01) and SA observed in the present study, especially given the fact that combat exposure was assessed continuously. While there is clearly a strong theoretical rationale for why one might expect to find a strong relationship between combat and suicide attempts (i.e., because it increases acquired capability for suicide; Joiner, 2005; Selby et al., 2010), several prior studies have failed to find the expected association between combat and suicide risk (e.g., Bryan et al., 2013). Prior research has, however, found a fairly consistent association between combat exposure and acquired capability for suicide (e.g., Bryan and Cukrowicz, 2011; Bryan et al., 2013).
One potential explanation for the findings regarding combat and SA in the present study relates to the measure of combat exposure used. Specifically, to our knowledge, the current study is the first to examine the relationship between the CWE and suicidal behavior. This is particularly notable because the CWE was explicitly designed to assess warzone experiences that are strongly associated with the development of PTSD, depression, and anxiety in Iraq/Afghanistan-era veterans (Kimbrel et al., 2014). In addition, recent research has shown that this measure is also associated with a broad array of other types of psychiatric symptoms in veterans, including symptoms of panic disorder, obsessive-compulsive disorder, somatization, bulimia, and psychosis (Kimbrel et al., 2015b). It is possible that the unique set of warzone experiences assessed by the CWE may be more strongly associated with suicidal behavior than other warzone experiences. Preliminary support for this idea comes from the fact that, among other items, the CWE assesses the number of times that veterans were directly responsible for killing an enemy combatant during their deployment, as killing in combat has previously been found to be a unique predictor of suicidal ideation (Maguen et al., 2012). Clearly, additional research aimed at better understanding the relationship between different types of warzone experiences and suicidal behavior is needed.
4.1 Limitations
The findings from the present study should be considered within the context of several limitations. First, the present study was cross-sectional and relied on retrospective assessment of NSSI and SA. Thus, causality cannot be inferred from the present findings. Moreover, while a high quality clinical interview (Posner et al., 2011) was used to assess both NSSI and SA, additional information regarding the onset and timing of NSSI and SA in relation to military service and deployments would have been useful in helping to disentangle these associations. A second limitation concerns the sample composition. Specifically, because veterans with PTSD and depression were oversampled in the present study, whereas veterans with a diagnosis of bipolar disorder or psychosis were excluded, the sample should not be considered representative of Iraq/Afghanistan-era veterans in general. Additional epidemiological work is needed to determine the true prevalence of NSSI among veterans. A final limitation concerns our limited diagnostic battery, which precluded us from assessing borderline personality disorder (BPD), a potentially important covariate that has been strongly associated with both NSSI and suicidal behavior in civilian samples (Klonsky et al., 2013; Linehan, 1993).
4.1 Clinical implications
Despite the limitations noted above, the present research, in conjunction with other recent studies in this area (e.g., Bryan et al., 2015; Kimbrel et al., 2014a, 2015a), has important implications for clinicians who routinely work with veterans of the conflicts in Iraq and Afghanistan. First, clinicians should be aware that NSSI does not appear to be limited by gender, ethnicity, income, education, or veteran status (Briere and Gil, 1998; Klonsky, 2011; Kimbrel et al., 2014a; Sacks et al., 2008). Thus, male veterans are as likely to engage in NSSI as female veterans or female civilians (e.g., Kimbrel et al., 2014a; Sacks et al., 2008). This is especially true for male veterans seeking treatment for PTSD (Kimbrel et al., 2014a; Sacks et al., 2008). Second, as demonstrated in the present study, clinicians should be aware that NSSI is one of the most robust predictors of SA identified to date (e.g., Asarnow et al., 2011; Bryan et al., 2015; Klonsky et al., 2013). As such, routine assessment of NSSI among veterans of the conflicts in Iraq and Afghanistan is advised, especially among Iraq/Afghanistan veterans who present with mental health concerns, such as PTSD. Third, while no research to date has attempted to treat NSSI among veterans, a growing body of research among civilians suggests that treatments that target emotion regulation skills (e.g., Linehan, 1993; Gratz et al., 2014) are likely to prove useful to these clients; however, additional work aimed at treating NSSI in veterans is still needed at the present time.
4.2 Conclusion
The findings from the present research suggest that NSSI is strongly associated with history of SA among Iraq/Afghanistan veterans, even after accounting for a number of important covariates, such as combat exposure, TBI, and psychopathology. More research on this important topic is needed. Prospective studies in high-risk samples of Iraq/Afghanistan veterans would be especially useful, as well as research aimed at determining if the findings from the present study extend to veterans of other eras. In the interim, the present findings clearly suggest that clinicians who routinely work with Iraq/Afghanistan veterans should make NSSI history a part of their standard risk assessment battery.
Highlights.
-
➢
Nonsuicidal self-injury (NSSI) has received insufficient attention among veterans.
-
➢
This study examined NSSI and suicide attempts (SA) in 292 Iraq/Afghanistan veterans.
-
➢
As hypothesized, NSSI was associated with increased risk for SA.
-
➢
This association remained significant even after PTSD and depression were covaried.
-
➢
Clinicians working with veterans should assess NSSI history during risk assessments.
Acknowledgments
This work was supported by a Merit Award (I01RX000304) to Dr. Morissette from the Rehabilitation Research and Development Service of the Department of Veterans Affairs (VA) Office of Research and Development (ORD), the VA VISN 17 Center of Excellence for Research on Returning War Veterans, the Central Texas Veterans Health Care System, the VA Mid-Atlantic Mental Illness Research, Education, and Clinical Center, and the Research & Development and Mental Health Services of the Durham VA Medical Center. Dr. Kimbrel was supported by a Career Development Award (IK2 CX000525) from the Clinical Science Research and Development Service of the VA ORD. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
References
- Asarnow JR, Porta G, Spirito A, Emslie G, Clarke G, Wagner KD, et al. Suicide attempts and nonsuicidal self-injury in the treatment of resistant depression in adolescents: Findings from the TORDIA study. J Am Acad Child Adolesc Psychiatry. 2011;50:772–781. doi: 10.1016/j.jaac.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentley KH, Cassiello-Robbins CF, Vittorio L, Sauer-Zavala S, Barlow DH. The association between nonsuicidal self-injury and the emotional disorders: A meta-analytic review. Clin Psychol Rev. 2015;37:72–88. doi: 10.1016/j.cpr.2015.02.006. [DOI] [PubMed] [Google Scholar]
- Blake D, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a Clinician-Administered PTSD Scale. J Trauma Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Blosnich JR, Bossarte RM, Silenzio VM. Suicidal ideation among sexual minority veterans: Results from the 2005–2010 Massachusetts Behavioral Risk Factor Surveillance Survey. Am J Public Health. 2012;102:S44–S47. doi: 10.2105/AJPH.2011.300565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briere J, Gil E. Self-mutilation in clinical and general population samples: Prevalence, correlates, and functions. Am J Orthopsychiatry. 1998;68:609–620. doi: 10.1037/h0080369. [DOI] [PubMed] [Google Scholar]
- Bryan C, Bryan A. Nonsuicidal self-injury among a sample of United States Military Personnel and Veterans enrolled in college classes. J Clin Psychol. 2014:1–12. doi: 10.1002/jclp.22075. [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Cukrowicz KC, West CL, et al. Combat experience and the acquired capability for suicide. J Clin Psychol. 2010;66:1044–1056. doi: 10.1002/jclp.20703. [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Hernandez AM, Allison S, Clemans T. Combat exposure and suicide risk in two samples of military personnel. J Clin Psychol. 2013;69:64–77. doi: 10.1002/jclp.21932. [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Rudd MD, Wertenberger E, Peterson AL, Young-McCaughan S, Mintz J, et al. Nonsuicidal self-injury as a prospective predictor of suicide attempts in a clinical sample of military personnel. Compr Psychiat. 2015;59:1–7. doi: 10.1016/j.comppsych.2014.07.009. [DOI] [PubMed] [Google Scholar]
- Bullman TA, Kang HK. Posttraumatic stress disorder and the risk of traumatic deaths among Vietnam veterans. J Nerv Ment Dis. 1994;182:604–610. doi: 10.1097/00005053-199411000-00002. [DOI] [PubMed] [Google Scholar]
- Chapman AL, Gratz KL, Brown MZ. Solving the puzzle of deliberate self-harm: The experiential avoidance model. Behav Res Ther. 2006;44:371–394. doi: 10.1016/j.brat.2005.03.005. [DOI] [PubMed] [Google Scholar]
- Crosby AE, Ortega L, Melanson C. Self-directed Violence Surveillance: Uniform Definitions and Recommended Data Elements. 2011 Retrieved from: http://www.cdc.gov/violenceprevention/pdf/Self-Directed-Violence-a.pdf.
- DeBeer BB, Kimbrel NA, Meyer EC, Gulliver SB, Morissette SB. Combined posttraumatic stress (PTSD) and depressive symptoms interact with social support to predict suicidal ideation in Operation Enduring Freedom and Operation Iraqi Freedom (OEF/OIF) veterans. Psychiat Res. 2014;216:357–362. doi: 10.1016/j.psychres.2014.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structural Clinical Interview for Axis I DSM-IV Disorders (Version 2nd) New York, NY: Biometrics Research Department; 1994. [Google Scholar]
- Gerberding JL, Binder S. Report to Congress on mild traumatic brain injury in the United States: Steps to prevent a serious public health problem National Center for Inquiry Prevention and Control. Atlanta, GA: Centers for Disease Control and Prevention; 2003. [Google Scholar]
- Gratz KL, Tull MT, Levy R. Randomized controlled trial and uncontrolled 9-month follow-up of an adjunctive emotion regulation group therapy for deliberate self-harm among women with borderline personality disorder. Psychol Med. 2014;44:2099–2112. doi: 10.1017/S0033291713002134. [DOI] [PubMed] [Google Scholar]
- Hamza CA, Stewart SL, Willoughby T. Examining the link between nonsuicidal self-injury and suicidal behavior: A review of the literature and an integrated model. Clin Psychol Rev. 2012;32:482–495. doi: 10.1016/j.cpr.2012.05.003. [DOI] [PubMed] [Google Scholar]
- Joiner TE. Why people die by suicide. Harvard University Press; Cambridge: 2005. [Google Scholar]
- Kang HK, Bullman TA. Risk of suicide among US veterans after returning from the Iraq or Afghanistan war zones. JAMA. 2008;300:652–653. doi: 10.1001/jama.300.6.652. [DOI] [PubMed] [Google Scholar]
- Kaplan MS, Huguet N, McFarland BH, Newsom JT. Suicide among male veterans: A prospective population-based study. J Epidemiol Commun H. 2007;61:619–624. doi: 10.1136/jech.2006.054346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiat. 1999;56:617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- Kimbrel NA, Calhoun P, Elbogen E, Brancu M, VA Mid-Atlantic MIRECC Registry Workgroup. Beckham JC. The factor structure of psychiatric comorbidity among Iraq/Afghanistan-ear veterans and its relationship to violence, incarceration, suicide attempts, and suicidality. Psychiat Res. 2014b;220:397–403. doi: 10.1016/j.psychres.2014.07.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, Evans LD, Patel AB, Wilson LC, Meyer EC, Gulliver SB, et al. The Critical Warzone Experiences (CWE) Scale: Initial Psychometric properties and association with PTSD, anxiety, and depression. Psychiat Res. 2014c;220:1118–1124. doi: 10.1016/j.psychres.2014.08.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, Johnson ME, Clancy C, Hertzberg M, Collie C, Van Voorhees EE, et al. Deliberate self-harm in male Iraq/Afghanistan veterans seeking treatment for posttraumatic stress disorder. J Trauma Stress. 2014a;27:474–477. doi: 10.1002/jts.21932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, DeBeer BB, Meyer EC, Silvia PJ, Beckham JC, Young KA, et al. An examination of the broader effects of warzone experiences on returning Iraq/Afghanistan veterans’ psychiatric health. Psychiat Res. 2015;226:78–83. doi: 10.1016/j.psychres.2014.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, Gratz KL, Tull MT, Morissette SB, Meyer EC, DeBeer BB, et al. Non-suicidal self-injury as a predictor of active and passive suicidal ideation among Iraq/Afghanistan veterans. Psychiat Res. 2015a;227:360–362. doi: 10.1016/j.psychres.2015.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonsky ED. Non-suicidal self-injury in United States adults: prevalence, sociodemographics, topography and functions. Psychol Med. 2011;41:1981–1986. doi: 10.1017/S0033291710002497. [DOI] [PubMed] [Google Scholar]
- Klonsky ED, May AM, Glenn CR. The relationship between nonsuicidal self-injury and attempted suicide: Converging evidence from four samples. J Abnorm Psychol. 2013;122:231–237. doi: 10.1037/a0030278. [DOI] [PubMed] [Google Scholar]
- Linehan M. Cognitive-behavioral treatment of borderline personality disorder. Guilford; New York: 1993. [Google Scholar]
- Maguen S, Metzler TJ, Bosch J, Marmar CR, Knight SJ, Neylan TC. Killing in combat may be independently associated with suicidal ideation. Depress Anxiety. 2012;29:918–923. doi: 10.1002/da.21954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller D. Women Who Hurt Themselves. New York: Basic Books; 1994. [Google Scholar]
- Morissette SB, Woodward M, Kimbrel NA, Meyer EC, Kruse MI, Dolan S, et al. Deployment-related TBI, persistent post-concussive symptoms, PTSD, and depression in OEF/OIF Veterans. Rehabil Psychol. 2011;56:340–350. doi: 10.1037/a0025462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Hwang I, Sampson NA, Kessler RC. Mental disorders, comorbidity, and suicidal behavior: Results from the National Comorbidity Survey Replication. Mol Psychiatr. 2010;15:868–876. doi: 10.1038/mp.2009.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Joiner TE, Jr, Gordon KH, Lloyd-Richardson E, Pinstein MJ. Non-suicidal self-injury among adolescents: Diagnostic correlates and relation to suicide attempts. Psychiat Res. 2006;144(1):65–72. doi: 10.1016/j.psychres.2006.05.010. [DOI] [PubMed] [Google Scholar]
- Nock MK, Kessler RC. Prevalence of and risk factors for suicide attempts versus suicide gestures: Analysis of the National Comorbidity Survey. J Abnorm Psychol. 2006;115:616–623. doi: 10.1037/0021-843X.115.3.616. [DOI] [PubMed] [Google Scholar]
- Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, et al. The Columbia-Suicide Severity Rating Scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiat. 2011;168(12):1266–1277. doi: 10.1176/appi.ajp.2011.10111704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remafedi G, French S, Story M, Resnick MD, Blum R. The relationship between suicide risk and sexual orientation: Results of a population-based study. Am J Public Health. 1998;88:57–60. doi: 10.2105/ajph.88.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacks M, Flood A, Dennis MF, Hertzberg MA, Beckham JC. Self-mutilative behaviors in male veterans with posttraumatic stress disorder. J Psychiat Res. 2008;42:487–494. doi: 10.1016/j.jpsychires.2007.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selby EA, Anestis MD, Bender TW, et al. Overcoming the fear of lethal injury: Evaluating suicidal behavior in the military through the lens of the Interpersonal–Psychological Theory of Suicide. Clin Psychol Rev. 2010;30:298–307. doi: 10.1016/j.cpr.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman MM, Berman AL, Sanddal ND, O’Carroll PW, Joiner TE. Rebuilding the Tower of Babel: A revised nomenclature for the study of suicide and suicidal behaviors part 1: Background, rationale, and methodology. Suicide Life Threat. 2007;27:248–263. doi: 10.1521/suli.2007.37.3.248. [DOI] [PubMed] [Google Scholar]
- Suyemoto KL. The functions of self-mutilation. Clin Psychol Rev. 1998;18:531–554. doi: 10.1016/s0272-7358(97)00105-0. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Veterans Affair. Mental health services, suicide prevention program. Suicide Data Report. 2013 Retrieved from: http://www.va.gov/opa/docs/Suicide-Data-Report-2012-final.pdf.
- Vasterling JJ. TBI screening interview [Unpublished measure] Boston, MA: VA Boston Healthcare System; 2008. [Google Scholar]


