Abstract
Japan’s prototype of depression was traditionally a melancholic depression based on the premorbid personality known as shūchaku-kishitsu proposed by Mitsuzo Shimoda in the 1930s. However, since around 2000, a novel form of depression has emerged among Japanese youth. Called ‘modern type depression (MTD)’ by the mass media, the term has quickly gained popularity among the general public, though it has not been regarded as an official medical term. Likewise, lack of consensus guidelines for its diagnosis and treatment, and a dearth of scientific literature on MTD has led to confusion when dealing with it in clinical practice in Japan. In this review article, we summarize and discuss the present situation and issues regarding MTD by focusing on historical, diagnostic, psychosocial, and cultural perspectives. We also draw on international perspectives that begin to suggest that MTD is a phenomenon that may exist not only in Japan but also in many other countries with different sociocultural and historical backgrounds. It is therefore of interest to establish whether MTD is a culture-specific phenomenon in Japan or a syndrome that can be classified using international diagnostic criteria as contained in the ICD or the DSM. We propose a novel diagnostic approach for depression that addresses MTD in order to combat the current confusion about depression under the present diagnostic systems.
Keywords: atypical depression, depression, DSM-5, dysthymia, major depressive disorder, shūchaku-kishitsu
CLINICAL PICTURE
Case: male, 24 years old
Chief complaint: No desire to do anything
Medical history: No previous psychiatric disorder
Family history: Nothing of note
Developmental and social history: He is the first son, with an older sister. His father is a company employee, his mother a full-time homemaker. There was nothing particularly problematic during junior or senior high school, although apparently he sometimes deliberately did not apply himself to the subjects of teachers that he disliked. At university he took part in group activities and had a part-time job, just like other students. He was not terribly enthusiastic about searching for a job and aimed to become a civil servant. After graduation, he attended a vocational college for a year to prepare for the entrance exam to the civil service, and at the age of 23 started to work in the municipal government of a provincial city – he says he just happened to sit the exam and pass it.
History of present illness: He did not particularly dislike the work in the place he was assigned to after being hired, though he was not greatly interested in it either. However, he would occasionally be absent from work; he says this was because he had an annoying boss who he couldn’t stand the sight of. Nonetheless, it was not a case of being unable to go to work because he was depressed, and when he was absent from work he would play slot machines, go to the movies, or go shopping.
In June 2010, a year after starting work, he married a female colleague from the same work-place with whom he had fallen in love. In May 2011, his first child was born. He was still halfhearted about his job, but also finding it hard to be at home, he would play slot machines or go to the movies. Raising the child proved to be very difficult, but his wife had stopped working and, together with both his mother and her own mother, managed the household very well.
In December 2011, his boss reprimanded him for his attitude toward his work. He had previously been given warnings on a number of occasions, but apparently this time the reprimand he received was very severe. He subsequently left work early, complaining of feeling unwell. He says that from that day on he was unable to sleep at night. He became easily irritated and tended to have feelings of desperation. Even though, he went to work properly every day. Whilst at work, he had no motivation to do anything and had no energy. He would become angry and did not feel like attending work social events, such as the year-end party or the New Year party. He would tend to stay out of his boss’s sight. He would feel a little more cheerful only when he played slot machines and when spending time in an Internet cafe, but when he went home he would again slip into gloom because, he says, he found it boring. His anger was not toward himself but others, such as his boss and his wife. He sometimes would feel valueless himself; however, he could alleviate such unpleasant feelings by his devotion toward his hobbies. His sleep was constantly mildly disturbed but not severely, and sometimes he would have trouble getting to sleep and fail to get up in the morning. Therefore, from around the middle of January he started to fail to go into his office once/twice a week and during this absence he would surf the net to relax or go out to play slot machines.
In March of 2012, he found a site on the Internet called ‘Mind medicine cures your Depression!!’ which contained a checklist for depression, and he quickly came to believe that he himself must have ‘depression.’ The following day, he decided to go to a local psychiatric clinic for a prescription of antidepressants. He entered the examination room, greeting the doctor politely, then he voluntarily read out his life history and medical history from a memo he had prepared. When he finished, he handed the psychiatrist in charge a depression checklist, which he had found on the Internet, and requested a particular medicine by himself: ‘Doctor, as I have just mentioned, these diagnostic criteria apply to me. I heard that selective serotonin re-uptake inhibitors are effective.’ Based on his examination, his score on the Hamilton Rating Scale for Depression1,2 was 17 (mild depressive level); he met the DSM-IV criteria for a major depressive episode (based on the handbook, entitled Quick Reference to the Diagnostic Criteria from DSM-IV-TR3) and was diagnosed as suffering from depression. He requested a medical certificate then and there. Additional clinical history revealed that he did not meet the diagnostic criteria for avoidant personality disorder, schizoid personality disorder, or narcissistic personality disorder. Also, according to information supplied by his wife, who was present when he was examined, there was nothing particular in the symptoms to suggest that the illness was feigned.
This clinical picture was originally used for the symposium during the 109th annual meeting of The Japanese Society of Psychiatry and Neurology in Fukuoka, 2013.
INTRODUCTION
Cases like the above have emerged in Japan since around 2000, and these cases have been called ‘modern type depression (MTD)’ – a novel form of depression. This catchy ‘modern’ name has quickly and widely spread to the public via Japan’s mass-media and Internet-related media, while the name itself has not been regarded as an official medical term, and there is no consensus guideline for its diagnosis and treatments, which has led to confusion when dealing with MTD in clinical practice. Scientific literature about MTD remains very limited. In this review paper, we summarize and discuss the present situation and issues regarding MTD – focusing on historical, diagnostic, sociocultural and international perspectives, by referring to our recent international survey.4 Is MTD a phenomenon limited to Japan? The pilot survey has indicated that MTD may exist not only in Japan but also in many other countries with different sociocultural and historical backgrounds. It is therefore of interest to establish whether MTD is a cultural phenomenon specific to Japan or a syndrome that can be classified using the present international diagnostic criteria of the ICD/DSM. Finally, we propose a novel diagnostic system of depression including MTD in order to combat current confusion regarding the diagnosis of depression under the present ICD/DSM diagnostic systems.
HISTORICAL BACKGROUND
Just since the beginning of the 21st century, Japanese psychiatrists have increasingly reported patients with a type of depression that does not seem to fit the criteria of the ICD-10 and the DSM-IV, and which is widely denoted as MTD among Japanese psychiatrists. The Japanese psychiatrist/psychopathologist Shin Tarumi reported the increasing occurrence of MTD and he labeled MTD as Dysthymia-gata utsu-byo (dysthymic type of depression) in the Japanese literature.5,6 Tarumi described the associated premorbid personality as Typus dysthymicus (TD) and compared it with Japan’s traditional type of depression.5,6 Tarumi defined the characteristics of MTD with TD as follows: (i) younger generation; (ii) attachment to oneself with less loyalty for social structures; (iii) feeling distressed about rules/order; (iv) negative feelings about social order/models; (v) vague sense of omnipotence; and (vi) not hard-working by nature (Table 1).6–17 MTD is also characterized by (a) distress and reluctance to accept prevailing social norms; and (b) avoidance of effort and any strenuous work.4,18 Most sufferers of MTD are born after 1970, that is, the generation growing up with home video games in the era of Japan’s high economic growth. Youths with MTD tend to feel depressed only when they are at work; otherwise, they can enjoy the virtual world of the Internet, video games, and pachinko (Japanese pinball). Therefore, sufferers of MTD have difficulties in adapting to work/school and participating in the labor market.
Table 1.
Comparison between Japan’s traditional type depression, Tarumi’s Japan’s modern type depression and atypical depression
| Japan’s traditional type depression (Originally proposed by Tarumi, 20056) | Japan’s modern type depression (Originally proposed by Tarumi, 20056) | Atypical depression | |
|---|---|---|---|
| Age-group/Sex | Middle and older generation | Younger generation (especially 20s and 30s) | Younger generation, female (Benazzi, 2005;7; Blanco et al., 20128) |
| Symptoms | Agitation and/or retardation Exhaustion and guilt Well prepared suicide, No mood reactivity Continuous depressive symptoms |
Fatigue and not feeling good enough Avoidant behaviors Blaming others (extrapunitive) Impulsive suicidal action Occasional depressive symptoms mainly during work/school |
Mood reactivity Hyperphagia, hypersomnia, leaden paralysis Interpersonal rejection sensitivity (resembles personality disorders) Lifetime psychiatric diseases comorbidity (Blanco et al., 20128) Affinity with bipolar disorder (Akiskal et al., 20069) |
| Severity of depression | Mild to severe | Mild to moderate (occasionally, minor depressive episode) | Mild to severe |
| Characteristics (temperament, behavior and interpersonal relationships) | Obsessive Honest/cooperative A preference to exist with social roles Love for order, models A hard worker A preference for hierarchy-based social relations |
A vague sense of omnipotence Avoidant/withdrawal tendency A preference to exist without social roles Avoidance and hatred of social order Not naturally a hard worker An avoidance/hatred of hierarchical social relations |
Sharpening of premorbid character (mild depression, emotional instability, impulsivity, anger attack, sentimentalism, aggressiveness, regression) |
| Cognition and attitudes during clinical settings | Resistance to being labeled/diagnosed with ‘depression’ Learning from experience of depression after recovery |
Accepts being labeled/diagnosed with ‘depression’ Tends to check his/her own depressive symptoms Strong belief that ‘I have “depression” ’ Struggles to depart from ‘depressive’ condition (prefers to be continuously diagnosed with ‘depression’) |
Has insight into disease, but cannot control behavior |
| Drug response/therapeutic intervention | Usually good response to antidepressants Complete remission |
Partial response solely to antidepressants Antidepressants may worsen the situation Good response to psychotherapy, especially group psychotherapy |
Refractory to treatment Deteriorated by ECT |
| Prognosis | Good response to rest and antidepressants Ambivalent about environmental change |
Tends to recur and become chronic by just rest and antidepressants Environmental change (such as quitting a job) rapidly improves symptoms on a superficial level |
Chronic clinical course and severe social distress |
| Previous concepts |
Shūchaku-kishitsu (Shimoda 193210) Typus melancholicus (Tellenbach 196111) |
Student apathy (Walters, 196112) Withdrawal neurosis (Kasahara and Kimura, 197513) Avoidant type depression (Hirose, 197714) modern type depression (Matsunami and Yamashita, 199115) Immature type depression (Abe, 199516) |
Hysteroid dysphoria (Klein, 198017) |
This table is a proposed comparison between Japan’s traditional type depression, Japan’s modern type depression and atypical depression according to Tarumi 2005,6 Tarumi & Kanba 2005,5 and Kato et al. 2011.4 Data, especially the section on ‘Drug response/Therapeutic intervention,’ has not yet been validated. ECT, electroconvulsive therapy.
Formerly, the melancholic type of depression had been regarded as a typical form of depression amongst the Japanese population, whose premorbid personality was defined as shūchaku-kishitsu (SK) by the Japanese psychiatrist Mitsuzo Shimoda.10,19 Shimoda characterized SK as: (i) middle aged; (ii) strong loyalty to society and community and one’s role within these structures; (iii) a preference for rules and order; (iv) positive feelings about social order/models; (v) attentive and diligent; and (vi) fundamentally hardworking.10,19,20 SK has been discussed in a similar context to Tellenbach’s Typus melancholicus (TM), which was identified amongst Germans after World War II.11 Tellenbach described the premorbid personality of patients with unipolar endogenous depression as orderly, devoted to duty and to family members, and scrupulous.11 Such types of depression based on SK and TM are considerably different from MTD. On the other hand, since the 1970s, different types of depression have been reported by Japanese psychiatrists and psychopathologists, such as taikyaku shinkei-sho (withdrawal neurosis);13 tohi-gata utsu-byo (avoidant type of depression);14 gendai-gata utsu-byo (modern type of depression);15 and mizyuku-gata utsu-byo (immature type of depression).16 Commonalities between the above types of depression and the currently emerging MTD have been pointed out. The former (taikyaku shinkei-sho, tohi-gata utsu-byo, gendai-gata utsu-byo and mizyuku-gata utsu-byo) was limited to highly educated youth, but MTD has been known to affect youth regardless of educational backgrounds.4
The 24-year-old man presented in the above clinical picture expressed moderate depressive symptoms just after a stressful event at his workplace. He came to regard himself as having severe depression, and finally he asked a doctor for sick leave in order to take a rest. His depressive symptoms mainly emerged during working time, and his symptoms were relieved in other situations. His characteristics, including behaviors and interpersonal relationships, contained the following features: not naturally a hard worker; an avoidance/hatred of hierarchical social relations; a preference to exist without social roles; extrapunitive type; and a vague sense of omnipotence. These features are exactly matched with MTD proposed by Tarumi.5,6
DIAGNOSTIC ISSUES OF MTD
MTD has not been regarded as an official medical term, and various diagnoses have been applied based on ICD-10 and DSM-IV criteria. Our case vignette survey among Japanese psychiatrists suggests that MTD tends to be diagnosed as a variety of psychiatric disorders, such as mood disorder (296, code of DSM-IV; the same shall apply hereafter), dysthymic disorder (300.4), adjustment disorder (309) and adjustment disorder with depressed mood (309.0) by Japanese psychiatrists.4 Interestingly, some Japanese psychiatrists reported that categorical diagnostic systems, such as the ICD-10 and the DSM-IV, are not applicable to MTD. The case vignette survey was also administered to foreign psychiatrists at the same time, which revealed that they tend to diagnose the MTD case as mood disorder (296), dysthymic disorder (300.4), adjustment disorder (309), adjustment disorder with depressed mood (309.0) and adjustment disorder with mixed anxiety and depressed mood (309.28). Based on the reports and our clinical experiences in Japan, it is challenging to differentiate between MTD and other types of depression, such as atypical depression (AD) and dysthymia.
Atypical depression
It is often difficult to differentiate MTD from AD due to some overlap of their clinical features, including young onset, impulsivity, aggression toward others, behavioral symptoms similar to personality disorders, being refractory to treatment, and severe social disability caused by a chronic clinical course.7,8,21
Patients with MTD tend to have specific features of personality or characteristics, while patients with AD have no such features. However, it is also well known that the characteristics of AD patients would alter dramatically around the onset of AD, showing its aggressive and impulsive aspects. Around the onset of AD, the characteristics in patients with AD often sharpen, and their emotions become unstable. The features and alterations of characteristics in patients with both AD and MTD often lead to interpersonal rejection sensitivity and social disability. Formerly, Klein suggested the concept of ‘hysteroid dysphoria’ in regards to the disease concept related to AD,17 and recently, AD has been suggested to have the affinity of characteristics or symptoms with bipolar II disorder.9 In the present stage, there exists no specific markers to differentiate MTD from AD, but specific symptoms of AD (hyperphagia, hypersomnia, leaden paralysis, and mood reactivity) seem to be useful for the differentiation.
Dysthymia
Dysthymia is also on the differential diagnosis for MTD, because both show a chronic clinical course and less severe depressive symptoms. In regards to this differentiation, the Japanese psychiatrist Shin Tarumi did not refer to the distinct difference between the two diseases and just stated ‘MTD has not completely become dysthymia yet.’5,6
In DSM-5, dysthymia (dysthymic disorder) was combined with chronic major depressive disorder under the name of persistent depressive disorder.22 The DSM-5 diagnostic criteria for persistent depressive disorder still characteristically include subjective superior symptoms, but not some objective depressive symptoms, such as psychomotor agitation/inhibition and suicidal ideation. These would be common features of MTD. Needless to say, the concept of dysthymia itself has not been clearly defined, which makes the differentiation between MTD and dysthymia more difficult.
Previously, Akiskal developed a framework of soft bipolar from subaffective dysthymia to character-spectrum disorders by therapeutic reactions.23 Similar to soft bipolar, the present situation has suggested that MTD might be heterogeneous. Therefore, further studies are needed to clarify the syndrome of MTD, which has important implications for the selection of appropriate interventions.
Personality disorder
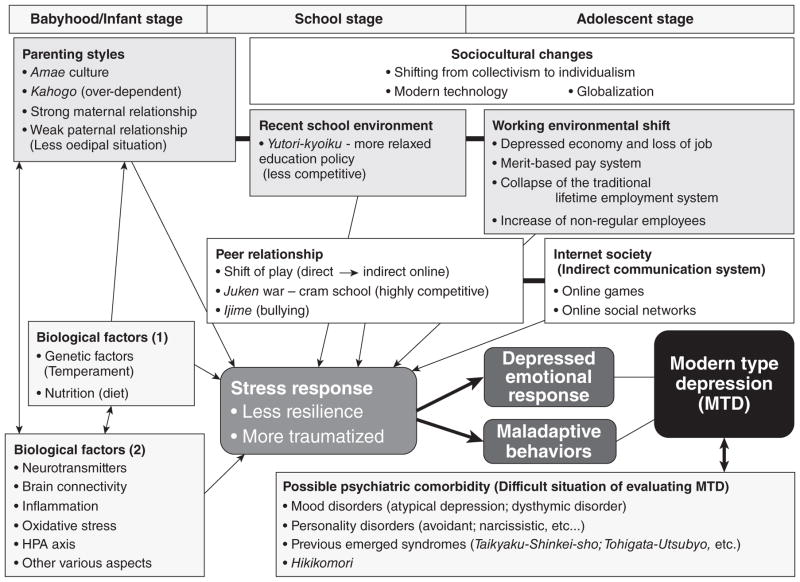
Tarumi did not include the comorbidity of personality disorders (avoidant personality disorder, schizoid personality disorder, or narcissistic personality disorder) in clinical case descriptions of MTD in his original paper.5 However, the international case vignette survey by Kato et al. in 2011 has suggested that personality problem is the most highly influential factor for MTD, and a variety of personality disorders are suggested to be comorbid with MTD.4 The underlying features of personality have yet to been clarified, while psychopathologists have highlighted the temperamental features of MTD syndrome as narcissism (omnipotence) and avoidance.5,6,24 In addition, immaturity may be an important factor.25 People who originally have a tendency toward an immature and narcissistic personality may easily develop depression and evasive behaviors when confronted with stressful situations at school and in the work-place (Fig. 1).
Figure 1.
Multidimensional understandings of Japan’s modern type depression (MTD). A variety of psychosocial factors, from the early stages of life through to adolescence, have been suggested to contribute to the onset of MTD. Especially important are childrearing, school and later workplace environments. Within this, parent–child relationships, and how/whether good-enough relationships between peers and friends have been established is vital. The establishment of these bonds can facilitate smooth relationships with workplace colleagues and superiors later in life. However, in MTD, the establishment of such fundamental interpersonal skills during the early stages of life may be insufficient, which can induce vulnerability to stress, meaning that mental dysfunctions are more likely to develop. In other words, lower resilience and the greater possibility of experiencing stress traumatically. Regarding the sociocultural impact in Japan, along with modernization and globalization, there has been a continuing shift away from the hitherto respected and venerated ‘group mentality’ to an ‘individualism’ in which individual achievements are pursued and this shift has resulted in rapid changes in school and work environments. In addition, we suppose that such sociocultural factors are occurring along with an interrelated biological basis, and it is important not to ignore underlying biological factors. With regards to diagnosis and evaluation of MTD, we are in a transitional period and a differential method to distinguish from existing psychiatric diagnoses is warranted. HPA, hypothalamic–pituitary–adrenal.
On the other hand, in the case vignette survey, only Japanese psychiatrists disregarded the factor of personality – SK, that is, immodithymia – as a component cause of Japan’s traditional type of depression, while many psychiatrists in other countries believed that the SK personality strongly affects the onset of depression as a pathological factor. Generally speaking, the Japanese are regarded to be a diligent, scrupulous and hard-working people, and such personality traits have been positively accepted and moreover encouraged in Japanese society over a long period of history since the Samurai era.26 However, these personality traits are not always considered to be positive but as a cause of illness, such as obsessional personality, by experts, including psychiatrists, anthropologists and sociologists in Japan and other countries.27,28 Therefore, Japanese psychiatrists’ opinions in the case vignette survey indicate that not only lay people but also psychiatrists in Japan have been influenced by such Japanese cultural contexts.4
Interestingly, a Japanese clinical study, published in 1997, suggested that TM, which is similar to SK, is not the premorbid personality trait of unipolar (endogenous) depression in Japan.29 This result might have predicted the recently suggested prototype shift of depression in Japan from TM to TD.30
On the other hand, Kotov et al. performed a meta-analysis regarding the association between the personality traits in the Big Three model (negative emotionality, positive emotionality, and disinhibition vs constraint) and Big Five model (neuroticism, extraversion, conscientiousness, agreeableness, and openness), and common psychiatric disorders, such as depression, anxiety and substance abuse disorders.31 The meta-analysis revealed that these common psychiatric disorders are strongly connected to personality. Both major depressive disorder (MDD) and dysthymic disorder showed a similar tendency for high neuroticism and low conscientiousness. Dysthymic disorder showed the most pathological profile. Actually, more than other ailments, dysthymic disorder showed extremely negative extraversion, negative conscientiousness, and positive disinhibition. There is a fairly small number of studies but this outcome is consistent with the argument that dysthymic disorder may be best seen as a form of personality disorder.32 Indeed, dysthymic disorder tends to be chronic and is often lifelong.33 Hence, prominent personality disturbance can be expected to manifest in dysthymic disorder. Surprisingly, the connection between MDD and extraversion was unexpectedly weak. On the other hand, low extraversion was revealed to play an important role in dysthymic disorder. Prospective studies are extremely rare in this field and a causal relationship is yet to be elucidated. Moreover, there are only a few longitudinal studies, the problem of comorbidity, and other limitations (Japanese clinical data seem not to be included in this meta-analysis). In spite of these limitations, this meta-analysis is an important resource when considering the relationship between MTD and personality.
Further clinical, psychopathological and epidemiological studies are needed to clarify underlying personalities, temperaments and characteristics of depression and MTD among particular cultural groups.
SOCIOCULTURAL ASPECTS
Psychiatric disorders are strongly influenced by culture, society, history and region.34,35 In any case, much attention should be paid to any medical culture that allows for an immediate diagnosis and the dispensation of medicines in such cases. Japan’s rapid socioeconomic and cultural changes have affected the lifestyle, behavior and mentality of people of all ages in Japan,36 and new types of psychiatric disorders or behavioral disorders have recently appeared in Japan. Tarumi suggested that MTD is caused by the unique Japanese cultural background and sociocultural changes in Japan.5,6 Tarumi regarded MTD as the byproduct of Japan’s historical socioeconomical shifts; beginning with World War II, the following period of high and rapid economic growth (1960–1980s), the economic crisis (1990s), and the diversity and complexity of modern society in the 21st century.5,6 Traditionally, Japanese society has greatly encouraged immodithymia, but modernization, globalization and the introduction of Western culture have led to a mixture of cultures and the celebration of individualism in Japan. The effects of changes in the education system and a move from its traditional disciplinarian base to Yutori education, a system that emphasizes the individual and freedom, may have been great. In the corporate world, the collapse of the traditional nenkō joretsu or seniority-based promotion system will also have had an effect. With the disintegration of the seniority system, there has been an evolution to an intensely competitive society and a distancing from the traditionally harmonious Japanese sense of group belonging.37 It has been suggested that a lack of a sense of belonging could be behind the increase in middle–older-age suicide.38,39 With regards to MTD, the problem of such a sense of belonging may be another major consideration. In the corporate world, younger employees who do not have such a sense of belonging and exhibit aspects of depression at work are often able to function normally and happily with such a sense on weekends, at places of leisure and/or online (Facebook, etc.), and this may reflect that very lack of a sense of belonging within the traditional Japanese organizations. According to the analysis by Takahashi et al.,40 the Japanese corporate organization gave a sense of belonging and community to workers because of its long-term-based relationship under the systems of seniority and permanent employment. After the burst of the bubble economy in the 1990s, however, these traditional systems collapsed and this organization no longer provides a sense of community or belonging.
Unfortunately, Japanese society had not prepared for the effects of this transition. Thus, patients with symptoms of MTD may have often been judged as lazy or ‘sloths’ because one of the most highlighted characteristics of MTD is the tendency to feel depressed only during work or at school.4,18
MTD and hikikomori based on amae
While the psychopathology of MTD is not well understood, it has been suggested that it is related to amae and other Japanese forms of mentality, a suggestion that raises the possibility of MTD as a cultural syndrome or form of psychopathology that predominates in Japan.28
Takeo Doi, a psychiatrist and psychoanalyst, described Japanese dependent behaviors with the word amae.28 The person who is acting amae may beg or plead, or alternatively act selfishly and indulgently, while secure in the knowledge that the caregiver will forgive this. The behavior of children towards their parents is the most typical example of amae. Doi argued that child-rearing practices in Western society seek to stop this kind of dependence in children, whereas in Japan it persists into adulthood in all kinds of social relationships.28 Even now, compared to Western societies, in Asian societies, including Japan, Korea and Taiwan, young people tend to be more economically dependent on their parents, and this phenomenon seems to be one of the expressed forms of amae.41 Hikikomori, a form of social withdrawal characterized by persistent isolation in one’s home for more than 6 months, may be indirectly promoted by amae to the extent that parents accept their child staying at home for prolonged periods of time.41 Even though the concept of amae was originally considered to be uniquely Japanese, contemporary opinions suggest that amae is actually more universal in nature.42 Thus, there is an interesting parallel to hikikomori that has been thought of as unique to Japan but, as our preliminary results show, is perceived by psychiatrists as occurring in a variety of other countries.41 In addition, our international clinical investigations have revealed real hikikomori persons in different countries, including the USA.43,44 These facts suggest that hikikomori and/or MTD could also be a universally observed psychiatric problem.
Cultural/social psychological understandings of MTD and hikikomori
The sociocultural background and tradition of amae is related to hikikomori and MTD. On the other hand, as another research stream, cultural psychologists and social psychologists have focused on the cultural uniqueness of inter-dependence with experiment and quantitative methods.45–49 A common argument being that East Asians are more collectivistic and/or more inter-dependent than Westerners.50–52 In a collectivist culture, inter-dependence is emphasized and in an individualist culture, independence has more value than inter-dependence. A common traditional assumption of these concepts is that collectivistic people tend to prefer harmonious inter-dependence to individual motivation or self-interest. This means that collectivists are ‘harmony seekers.’ On the other hand, Hashimoto and Yamagishi have claimed that the above assumption is not necessarily true, and have recently proposed a novel dimension, namely ‘dis-engaging inter-dependence.’53 They have claimed that the conventional distinction has focused only on dis-engaging independence and engaging interdependence, and relatively ignored the opposite (engaging independence and dis-engaging interdependence). Engaging independence is characterized as voluntary formation of interaction relationships with others to find desirable interaction partners and to prove to others that one is a desirable interaction partner. Hence, individualistic and harmonious. On the other hand, dis-engaging interdependence is characterized as ‘rejection avoidance’ to try to confirm qualification of informal membership in a given social group by following the group norm and informal rules. It is not voluntary adaptation for the group, but motivated to avoid being ostracized by other group members. Hence, collectivistic but not harmonious.
Of these categories, dis-engaging inter-dependence may be deeply related to MTD and also hikikomori. Patients with MTD tend to avoid many interpersonal relationships because they are so afraid of being hurt and humiliated by others. They are always scared of potential psychological attack from others. In particular, hikikomori persons do not want to leave their homes. For them, their family is the only group that they are convinced will not hurt them. This is consistent with the characteristics of dis-engaging interdependence. Although an empirical demonstration has yet to be carried out, it would be plausible to consider MTD patients as having much higher levels of dis-engaging inter-dependence than normal and healthy people. According to Hashimoto and Yamagishi,53,54 comparing student samples from the USA and Japan, the Japanese showed significantly higher scores on dis-engaging inter-dependence than Americans. This may be indirect evidence that it can be related to MTD because currently MTD is frequently observed among youth in Japan. Interestingly, a recent review article by Li and Wong has indicated the interaction between hikikomori and inter-dependence.55 It is necessary to conduct systematic empirical research to investigate the relationship (and/or causality) between MTD and dis-engaging inter-dependence.
BIOLOGICAL FACTORS
While the biological foundation of MTD is unknown, some specific biological mechanisms are worth speculation. The frequently observed clinical viewpoint that treatment with only the standard pharmacological therapies for depression is not successful for patients with MTD has strongly suggested that a different biological mechanism from traditional depression may exist in the biological features of MTD.
Abnormal function of the hypothalamic–pituitary–adrenal (HPA) axis has long been proposed as a candidate biological foundation of depression.56 A number of studies using the dexamethasone (DEX)/corticotrophin-releasing hormone (CRH) test have been conducted for the assessment of HPA axis function in patients with depression, while these outcomes have been inconsistent.57 The inconsistency may result from the heterogeneity of depression. Hori et al. have reported key findings in elucidating the heterogeneity of depression using the DEX/CRH test and the Temperament and Character Inventory in patients with MDD.58 MDD patients with high cooperativeness showed exaggerated cortisol reactivity; on the contrary, patients with low cooperativeness and high reward dependence showed blunted cortisol reactivity.58 In addition, Hori et al. revealed that MDD patients with escape-avoidance coping showed blunted cortisol reactivity.59 On the other hand, schizotypal personality traits60 and low novelty-seeking with harm avoidance61 in healthy adults are reported to be correlated with exaggerated cortisol reactivity, which proposes the possibility that functions of the HPA axis differ with character and temperament. Low cooperativeness and escape-avoidance coping coincide with the features of MTD, thus the biological foundation of MTD may, at least to some extent, result from abnormal functions of the HPA axis. While not MTD, abnormal function of the HPA axis (abnormal cortisol reactivity in DEX/CRH test) has also been observed in patients with borderline personality disorder62 and atypical depression.63 Based on the above data, Kunugi et al. has recently proposed a classification of depression focusing on the HPA axis functions.64
Interestingly, a recent clinical research regarding atypical depression has suggested a significantly higher comorbidity with metabolic syndrome.65 Metabolic syndrome has recently been suggested to be related to oxidative stress and inflammation.66 Our pilot study has indicated a correlation between serum proinflammatory cytokines and depressive symptoms/personality traits in Japanese university students (unpub. data). We propose an inflammation hypothesis of psychiatric diseases, including depression, via microglia, brain immune cells.67–71 These data may suggest that inflammation and oxidative stress may link to MTD. Further translational studies are needed to clarify the biological foundation of MTD.
THERAPEUTIC APPROACH
No systematic data have been reported regarding therapeutic interventions of MTD. While our previous case vignette survey has suggested that both psychotherapy and pharmacotherapy were recommended to treat MTD, psychotherapy was especially preferred by psychiatrists in all countries.4 Interestingly, Japanese psychiatrists seemed to hesitate to recommend pharmacotherapy for MTD. In addition, some Japanese psychiatrists hesitated to treat MTD at all. These data have indicated that Japanese psychiatrists, at least to some extent, regard MTD as a non-medical condition. This was in contrast to most psychiatrists in other countries endorsing the need for active treatments to MTD.4 Why is there a discrepancy in psychiatrists’ attitudes toward MTD? These findings may suggest that Japanese psychiatrists themselves are bound to their own socio-cultural and historical contexts.4
The arrival of new antidepressants to Japan in 1999 has also been suggested to have influenced the public view toward depression,72 and may have led to a similar phenomenon occurring in Western countries.73 Previously, depressed persons had tended to hesitate to visit psychiatrists, and Japanese psychiatrists had tended to equate depression only with the traditional melancholic type. Perhaps with the introduction of public awareness campaigns for depression and antidepressants, people who considered themselves depressed began to feel less self-conscious about visiting psychiatrists. This may have been a contributing factor leading to increasing numbers of visits of depressed persons to psychiatrists in Japan.4 However, as the case vignette survey implies, this popular shift has not been accompanied by similar changes in the perception of Japanese psychiatrists, who have very much remained deeply bound to earlier, more traditional conceptions of depression. On the other hand, the results of the case vignette survey indicate that psychotherapy was regarded to be of importance for MTD patients with Japanese psychiatrists who did not see a role for pharmacotherapy.4 Therefore, public education about depression and psychotherapy as a treatment should also be considered as one of the possible solutions to alleviate this discrepancy between the general population and psychiatrists in Japan.
Therapeutic strategies regarding MTD based on pathophysiological understandings should be established. We hypothesize that child and adolescent development has been impacted by rapid environmental changes, which may cause the novel phenomenon. The ways of ‘playing’ among children and adolescents have dramatically shifted from ‘direct playing’ (direct communication in a physical space, such as outdoors or in parks) to ‘indirect playing’ (indirect virtual communication via video games and Internet-related materials) within the past decades.36 People who have grown up in such new environments may become confused and depressed when they enter the traditional workforce and encounter the need for real direct communication. Therefore, psychoeducation and (group) psychotherapy may be the recommended approaches in order to develop skills of direct communication, which may lead to a smoother adjustment to adult communication environments. In addition, pharmacological and social approaches may also be effective. Clinical research to measure therapeutic responses should be performed to dig up the appropriate intervention.
HOW TO SOLVE THE ISSUES ASSOCIATED WITH MTD
Blind-spots of the DSM system
Recently, early-career psychiatrists in Japan have considered that it is possible to make diagnoses based solely on the abbreviated pocket-sized DSM-IV-TR. This book, entitled the Quick Reference to the Diagnostic Criteria from DSM-IV-TR,3 states that it is intended to be used in combination with the unabridged version of the DSM-IV-TR (which is 900+ pages in length).74 In fact, the DSM-IV-TR also states in an introductory section entitled ‘Cautionary Statement’ that ‘the proper use of these criteria requires specialized clinical training that provides both body of knowledge and clinical skills.’ Many early-career psychiatrists seem to be unaware of these facts. The DSM-IV-TR includes detailed explanations of diagnostic criteria, diagnostic features, and differential diagnoses for each disorder. However, even in the unabridged version, there is no mention of which examinations should be performed in the garnering of information for each disorder. This can only be achieved through not only reading of psychiatric textbooks but also the accumulation of real clinical experiences with supervisory psychiatrists involving the joint examination of patients in a hospital/clinic setting. However, in reality, early-career psychiatrists who are actually willing to accumulate such valuable experiences are on the decline. In addition, there are some problems based on the nature of operational diagnosis in DSM. Parker indicated that operational criteria of the depression dimensional model in DSM has made it easy to diagnose depression, and also resulted in loose diagnostic practice blunting clarification of causes and treatment specificity of depression.75
On the other hand, the Structured Clinical Interview for DSM-IV (SCID) is considered the best available method for diagnosis of psychiatric disorders, but in reality there are limitations to its applicability. When applying the systematic diagnostic criteria for MDD based on the DSM-IV (and also DSM-5), whilst being relevant, a difficulty arises when strictly applying the criteria. In particular, within the definition of MDD, a continuous depressed mood of more than 2 weeks is one of the criteria for diagnosis, and in reality it is difficult to judge whether this criteria has been met for this continuous period for almost every day for 2 weeks. Furthermore, ambiguity exists regarding the extent at which ‘continuous’ may be defined. In MTD, depressive symptoms are exhibited at work or at school but during weekend rest times or when at home these symptoms are not exhibited. In such cases, are the DSM criteria of ‘for more than 2 weeks’ met? Depending on the psychiatrist, there are those who would diagnose MDD and others who would not. In Japanese clinical settings, for such cases and similar cases where symptoms are even less frequent, there is still a high probability that a diagnosis of MDD will eventuate.
Proposing a novel diagnostic approach to depression
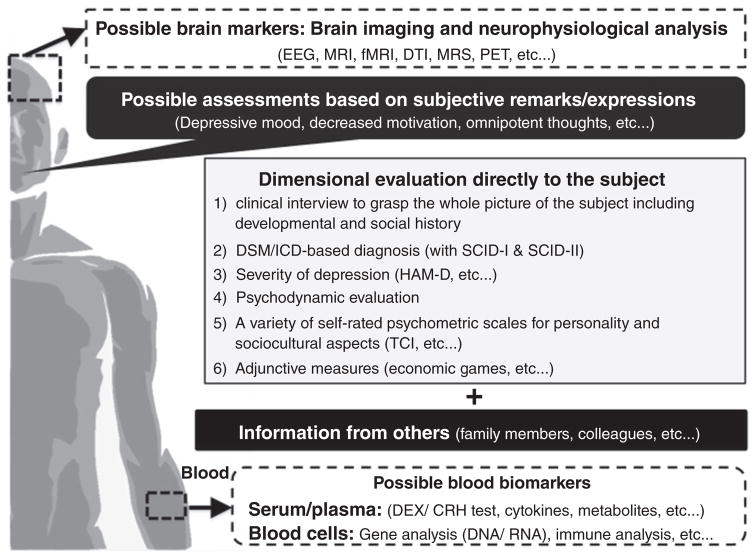
The greatest difficulty in the evaluation and diagnosis of depression is the gap between subjective patient symptoms and objective realities. It is a well-known given among experienced psychiatrists that information garnered from the individual only is not enough in the diagnosis of depression. Information regarding psychiatric symptoms from an individual is no more than ‘subjective symptoms’ and in many cases differs from objective realities. It is particularly difficult for inexperienced psychiatrists to reach a diagnosis for depression based on information garnered solely from the individual but it is also often the case that treatment is commenced without understanding this reality. Moreover, it is important to note that recently not only psychiatrists but also physicians are diagnosing depression and tend to prescribe antidepressants. In order to improve this situation, changes must be made to allow for a more detailed assessment of the individual’s situation. Along with the individual, the collection of information from family members and other third parties is incredibly important (Fig. 2). When an individual claims to be depressed, an objective assessment is required that cannot be limited to the individual. Because of this, when the only obtainable information is from the individual, a diagnosis of ‘possible’ depression may be preferable. This aspect has not been included in many guidelines of depression; however, it must be of great importance, especially in diagnosing MTD.
Figure 2.
Multi-axial assessments of modern type depression (MTD). In order to evaluate MTD, we recommend utilizing the 1–6 assessment methods directly to depressed persons. In addition, information from others is essential to evaluate such persons. Objective biomarkers of MTD have not been developed until now. Some biomarkers of MTD may overlap with major depressive disorder and other psychiatric diagnosis/syndromes, while some data from brain imaging/neurophysiological analysis and peripheral blood analysis may help to distinguish MTD from other psychiatric conditions. Further investigations should be developed to dig up such biomarkers. CRH, corticotrophin-releasing hormone; DEX, dexamethasone; DTI, diffusion tensor imaging; EEG, electroencephalography; HAM-D, Hamilton Rating Scale for Depression; fMRI, functional magnetic resonance imaging; MRI, magnetic resonance imaging; MRS, magnetic resonance spectroscopy; PET, positron emission tomography; SCID, Structured Clinical Interview for DSM-IV; TCI, Temperament and Character Inventory.
Using a three-tier diagnostic system (possible/probable/definite)
Here, we propose a novel criteria that can make evaluation/diagnosis of depression understandable even for less experienced psychiatrists.76 Along the lines of a diagnostic system for many physical illnesses (cancer, etc ) and dementia, we propose that diagnosis of depression should be divided into the three tiers of ‘possible,’ ‘probable’ and ‘definite.’ The first tier (possible) would be ‘diagnosis based on information from the subject only,’ the second tier (probable) would be ‘diagnosis based on the information from the subject and other sources (family or colleagues, etc.),’ and the third tier (definite) would be ‘diagnosis based on information from the subject + (family, colleagues, etc.) + (intensive clinical examination during outpatient clinic and/or hospitalization).’ Furthermore, we believe that each tier should have a different treatment guideline.77 By utilizing this novel diagnostic system, we can avoid the tendency to overdiagnose depression in persons with MTD tendencies (Fig. 2).
Investigating research into adjunctive measures, such as economic games
In addition, economic games, such as the trust game, have been utilized to evaluate real-world interpersonal relationships as a novel candidate for psychiatric evaluations. Economic games have been developed in the field of social psychology and economics, and have been proposed as a novel tool for evaluating interpersonal psychiatric problems. Clinical studies using economic games (prisoner’s dilemma, the public goods game, the ultimatum game and the trust game) have revealed some difficulties of social decision-making in individuals with MDD and personality disorders.77–80 The trust game, an economic game, has been widely used to evaluate a person’s trust toward others.81 In this two-person game, the first player has to make a risky financial decision depending on how much s/he would trust the second player (partner). Recent studies have examined whether other factors, such as personality and psychiatric conditions, influence trusting behaviors and cooperation.79,80,82–84 As a pilot study, we recently conducted a trust game experiment with 81 Japanese university students.85 Clinical case reports have indicated that people with MTD and hikikomori have difficulties in developing trust among family members, and colleagues in schools and working places.86–88 Therefore, a common feature of modern psychiatric syndromes may be induced through difficulty in trusting others, and these features may not be limited to patients but also to the wider contemporary populations, especially the young. In the economic experiment, participants made a risky financial decision about whether to trust each of 40 photographed partners.85 Participants then answered a set of questionnaires, including the Patient Health Questionnaire (PHQ)-9. Regression analysis revealed that item 8 of the PHQ-9 (subjective agitation and/or retardation) for female participants was associated with participants’ trusting behaviors. Women with higher subjective agitation (and/or retardation) gave less money to men and highly attractive women, but more to less attractive women in interpersonal relationships. This indicates that women with high subjective agitation may tend to make more defensive and cautious decisions in daily life, which may cause difficulties in various social interactions. These data indicate the possible impact of economic games in psychiatric research and clinical practice, including MTD, and further validation should be investigated.
CONCLUSION
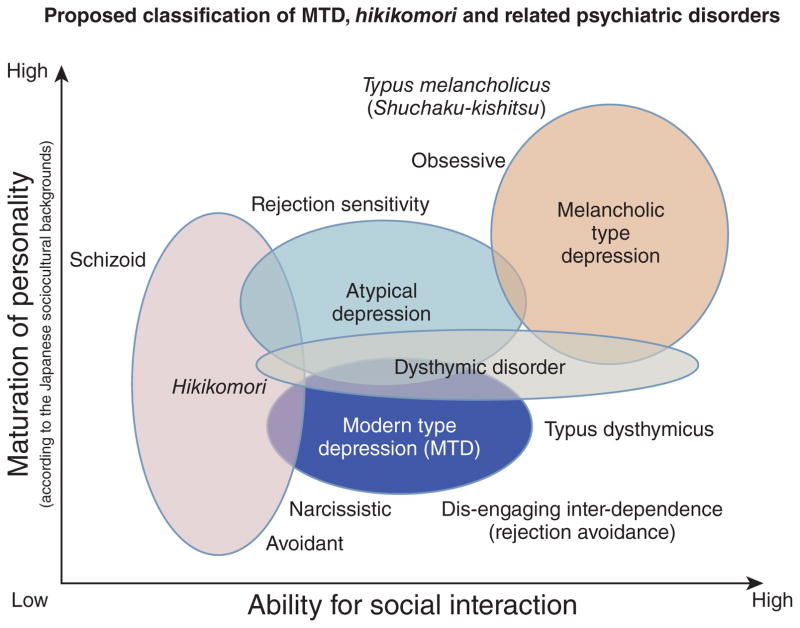
In this review paper, we introduced MTD, citing the few scientific reports available and offered our collective experiences and perspectives on its diagnosis and treatment. In Japan, MTD refers to a syndrome with predominant symptoms of depression and withdrawal that has rapidly increased among youth since around 2000. It is worth recalling that the phenotype of mental illness – be it the appearance of late-19th century hysteria, the appearance of post-1950 eating disorders, or post-1970 borderline personality disorders – is transforming along with society. Despite the lack of agreement upon diagnostic criteria of MTD, it may be considered that cultural, social, and biological factors are all involved in its development and Japanese cultural and social influences may be creating MTD (Fig. 1). In Japan, along with MTD, social withdrawal syndrome (i.e. hikikomori) is concurrently prevalent amongst youth and is considered a great social problem. We hypothesize that the onset of MTD and a prolonged maladaptive social situation may be one of the causal factors of hikikomori. As we may consider ‘withdrawal/avoidance’ to be a common factor in both syndromes, further research regarding shared psychopathology and risk factors in modern society is necessary. We believe that combating MTD may also rescue hikikomori. Differentiation of MTD from other psychiatric disorders has not been established under the present situation, while we have newly classified MTD and related psychiatric disorders (syndromes) from the following two aspects: maturation of personality and ability for social interaction (Fig. 3).
Figure 3.
Proposed classification of modern type depression (MTD), hikikomori and related psychiatric disorders. Based on the maturation of personality and ability of social interaction, we have classified the five psychiatric disorders (syndromes), including MTD and hikikomori. The level of personality maturation in this figure is based on the Japanese sociocultural contexts. In Japan, melancholic personality (Typus melancholicus or Shūchaku-kishitsu) has long been regarded as matured personality, while this perspective may not be applied in other countries with different sociocultural backgrounds.
We have suggested the necessity for the introduction of novel methods of evaluation, not only limited to the diagnosis of MTD but to depressive disorders in general, as we consider the modern usage of psychiatric tools that rely on subjective claims by patients to be insufficient. In particular, we recommend the addition of: third-party evaluations to the diagnostic criteria; the usage of economic game experiments and the like; and the evaluation of actual behavioral characteristics. It is hoped that through the introduction of these tools, a more accurate diagnosis of depressive disorders will become possible. The development of a new multi-axial evaluation and diagnostic tool that incorporates such new tools is required (Fig. 2). As the nosology of MTD has not been validated, we need to keep in mind that the presented data shown in the ‘biological factors’ and ‘therapeutic approach’ sections does not directly provide the findings of MTD (mixed with issues regarding major depression in general). In order to advance MTD research, we have proposed research-based draft operational criteria for MTD (Table 2). The draft operational criteria are limited to research use at the present stage. We hope that in the near future, a breakthrough diagnostic and treatment methodology for MTD will be developed based on these draft criteria.
Table 2.
Proposed research-based operational criteria and intervention for ‘modern type depression (MTD)’: Provisional –recommended only for research use
|
| Specify whether: |
| Typical case of MTD: Full criteria not met for MDD. |
| Severe Case of MTD: Full criteria met for MDD. |
| Diagnostic Features |
| Many cases of MTD are considered to be mildly to moderately depressed when evaluated for the level of depressive state (e.g. according to HAM-D etc.); severely depressed cases of MTD are uncommon. |
| Development and course |
| In case of a typical case of MTD, psychosocial interventions (e.g. environmental regulation, group psychotherapy) should be primarily considered, as unwarranted medication can prolong or worsen the condition and therefore requires caution. In case of a severe case of MTD, psychosocial interventions (e.g. environmental regulation, group psychotherapy) should be considered first, and depending on the severity of the depressive condition, pharmacological intervention (e.g. antidepressants) should be considered. |
| Comorbidity |
| MTD is often comorbid with other mood disorders or personality disorders (including subthreshold cases). |
In order to advance MTD research, MTD should be defined with more systematic methodology. Thus, we herein propose operational criteria for MTD based on the present knowledge of MTD. The draft operational criteria are for research use at the present stage. Based on research with the draft criteria, clinically useful operational criteria should be developed in the near future. Of note, five components are listed as representative of MTD in Item C. In order to evaluate the temperament of MTD, the person must be comprehensively assessed, including personality, development, life history and present status. In order to help conduct the assessment more efficiently, a self-report questionnaire (‘MTD-trait scale’) for evaluation of MTD temperament is being developed (Kato et al. unpub. material). HAM-D, Hamilton Rating Scale for Depression; MDD, major depressive disorder; MTD, modern type depression.
Acknowledgments
A series of MTD studies in Kyushu University has been conducted with the cherished desire of the late Shin Tarumi (1971–2005). This work was supported in part by the Japanese Ministry of Education, Culture, Sports, Science, and Technology KAKENHI (Grant-in-Aid 26713039 for Young Scientists [A] to T.A.K., Grant-in-Aid 24650227 & 15K15431 for Challenging Exploratory Research to T.A.K., and Grant-in-Aid 25117011 for Scientific Research on Innovative Areas [Glia Assembly] to S.K.); JSPS Bilateral Joint Research Project between USA–Japan (to T.A.K.); Japan Agency for Medical Research and Development (AMED) – The Japanese Ministry of Health, Labour and Welfare (H27 – Seishin-Syogai Taisaku-Jigyo to S.K.); and SENSHIN Medical Research Foundation (to T.A.K. and S.K.). All the authors report no financial relationships with commercial interests.
References
- 1.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Furukawa TA, Streiner DL, Azuma H, et al. Cross-cultural equivalence in depression assessment: Japan-Europe-North American study. Acta Psychiatr Scand. 2005;112:279–285. doi: 10.1111/j.1600-0447.2005.00587.x. [DOI] [PubMed] [Google Scholar]
- 3.American Psychiatric Publishing. Quick Reference to the Diagnostic Criteria from DSM-IV-TR. American Psychiatric Publishing, Inc; Arlington, VA: 2000. [Google Scholar]
- 4.Kato TA, Shinfuku N, Fujisawa D, et al. Introducing the concept of modern depression in Japan: An international case vignette survey. J Affect Disord. 2011;135:66–76. doi: 10.1016/j.jad.2011.06.030. [DOI] [PubMed] [Google Scholar]
- 5.Tarumi S, Kanba S. Sociocultural approach toward depression – Dysthymic type depression. Jpn Bull Soc Psychiatr. 2005;13:129–136. (in Japanese) [Google Scholar]
- 6.Tarumi S. The ‘new’ variant of depression: The dysthymic type. Jpn J Clin Psychiatr. 2005;34:687–694. (in Japanese) [Google Scholar]
- 7.Benazzi F. Testing atypical depression definitions. Int J Methods Psychiatr Res. 2005;14:82–91. doi: 10.1002/mpr.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blanco C, Vesga-Lopez O, Stewart JW, Liu SM, Grant BF, Hasin DS. Epidemiology of major depression with atypical features: Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) J Clin Psychiatry. 2012;73:224–232. doi: 10.4088/JCP.10m06227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Akiskal HS, Akiskal KK, Perugi G, Toni C, Ruffolo G, Tusini G. Bipolar II and anxious reactive ‘comorbidity’: Toward better phenotypic characterization suitable for genotyping. J Affect Disord. 2006;96:239–247. doi: 10.1016/j.jad.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 10.Shimoda M. On the treatment of involutional depression in my department. Taiwan Igaku Zasshi. 1932;31:113–115. (in Japanese) [Google Scholar]
- 11.Tellenbach H. Melancholie. Springer; Berlin: 1961. [Google Scholar]
- 12.Walters PA., Jr . Student apathy. In: Blame GB Jr, McArthur CC, editors. Emotional problems of the student. Appleton-Century-Crofts; New York: 1961. pp. 129–147. [Google Scholar]
- 13.Kasahara Y, Kimura B. Utsu-byo no rinshoteki-bunrui ni kansuru kenkyu. Seishin Shinkeigaku Zasshi. 1975;77:715–735. (in Japanese) [PubMed] [Google Scholar]
- 14.Hirose T. Tohi-gata utsu-byo ni tsuite. In: Miyamoto T, editor. Sou-utsu-byo no seishin-byori 2 [Psychopathology of Manic-Depressive Illness 2] Kobundo, Tokyo: 1977. pp. 61–86. [Google Scholar]
- 15.Matsunami K, Yamashita Y. Syakai-hendo to utsu-byo [Social changes and depression] Jpn Bull Soc Psychiatr. 1991;14:193–200. (in Japanese) [Google Scholar]
- 16.Abe T, Otsuka K, Nagano M, Kato S, Miyamoto T. A consideration on ‘Immature Type of Depression’: Premorbid personalities and clinical pictures of depression from the structural-dynamic viewpoint (W. Janzarik) Jpn Clin Psychopathol. 1995;16:239–248. (in Japanese) [Google Scholar]
- 17.Klein DF, Liebowitz MR. Hysteroid dysphoria. Am J Psychiatry. 1982;139:1520–1521. doi: 10.1176/ajp.139.11.1520. [DOI] [PubMed] [Google Scholar]
- 18.Kato TA, Shinfuku N, Sartorius N, Kanba S. Are Japan’s hikikomori and depression in young people spreading abroad? Lancet. 2011;378:1070. doi: 10.1016/S0140-6736(11)61475-X. [DOI] [PubMed] [Google Scholar]
- 19.Shimoda M. Shuchaku-kishitsu ni tsuite. Yonago Igaku Zasshi. 1950;2:1–2. (in Japanese) [Google Scholar]
- 20.Kanba S. Modern interpretation of Shimoda’s shuchaku-kishitsu. Kyushu Neuro-Psychiatry. 2006;52:79–88. (in Japanese) [Google Scholar]
- 21.Ohmae S. The modern concept of atypical depression: Four definitions. Seishin Shinkeigaku Zasshi. 2010;112:3–22. (in Japanese) [PubMed] [Google Scholar]
- 22.American Psychiatric Publishing. Diagnostic and Statistical Manual of Mental Disorders. 5. American Psychiatric Publishing; Arlington, VA: 2013. [Google Scholar]
- 23.Akiskal HS. Dysthymic disorder: Psychopathology of proposed chronic depressive subtypes. Am J Psychiatry. 1983;140:11–20. doi: 10.1176/ajp.140.1.11. [DOI] [PubMed] [Google Scholar]
- 24.Hirose T. Depression of avoidant type compared with depression of dysthymic type. Jpn J Clin Psychiatr. 2008;37:1179–1182. (in Japanese) [Google Scholar]
- 25.Abe T. Depression from the viewpoint of life stage: Diagnosis and treatment. Jpn J Psychosom Med. 2009;49:987–993. (in Japanese) [Google Scholar]
- 26.Nitobe I. Bushido: The Soul of Japan. G. P. Putnam’s Sons; New York: 1906. [Google Scholar]
- 27.Benedict RF. The Chrysanthemum and the Sword: Patterns of Japanese Culture. Houghton Mifflin; Boston, MA: 1946. [Google Scholar]
- 28.Doi T. The Anatomy of Dependence. Kodensha International; Tokyo: 1973. [Google Scholar]
- 29.Furukawa T, Nakanishi M, Hamanaka T. Typus melancholicus is not the premorbid personality trait of unipolar (endogenous) depression. Psychiatry Clin Neurosci. 1997;51:197–202. doi: 10.1111/j.1440-1819.1997.tb02582.x. [DOI] [PubMed] [Google Scholar]
- 30.Kanba S, Kano R, Eguchi S, Utsumi T, Abe T. Has the prototype of depression been shifted? Jpn J Clin Psychiatr. 2008;37:1091–1109. (in Japanese) [Google Scholar]
- 31.Kotov R, Gamez W, Schmidt F, Watson D. Linking ‘big’ personality traits to anxiety, depressive, and substance use disorders: A meta-analysis. Psychol Bull. 2010;136:768–821. doi: 10.1037/a0020327. [DOI] [PubMed] [Google Scholar]
- 32.Watson D, Clark LA. Depression and the melancholic temperament. Eur J Pers. 1995;9:351–366. [Google Scholar]
- 33.Klein DN, Shankman SA, Rose S. Ten-year prospective follow-up study of the naturalistic course of dysthymic disorder and double depression. Am J Psychiatry. 2006;163:872–880. doi: 10.1176/ajp.2006.163.5.872. [DOI] [PubMed] [Google Scholar]
- 34.Tseng WS. Handbook of Cultural Psychiatry. Academic Press; San Diego, CA: 2001. [Google Scholar]
- 35.Alarcon RD. Culture, cultural factors and psychiatric diagnosis: Review and projections. World Psychiatry. 2009;8:131–139. doi: 10.1002/j.2051-5545.2009.tb00233.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ogata Y, Izumi Y, Kitaike T. Mobile-phone e-mail use, social networks, and loneliness among Japanese high school students. Nippon Koshu Eisei Zasshi. 2006;53:480–492. (in Japanese) [PubMed] [Google Scholar]
- 37.Watabe M. Social exchange; transition from ‘embedded long-term relationships’ to ‘voluntary short-term relationships’. In: Hibino A, Watabe M, Ishii K, editors. Disconnected Society (Tsunagarenai Shakai) Nakanishiya, Kyoto: 2014. [Google Scholar]
- 38.Hatcher S, Stubbersfield O. Sense of belonging and suicide: A systematic review. Can J Psychiatry. 2013;58:432–436. doi: 10.1177/070674371305800709. [DOI] [PubMed] [Google Scholar]
- 39.Kim SY, Kim MH, Kawachi I, Cho Y. Comparative epidemiology of suicide sin South Korea and Japan: Effects of age, gender and suicide methods. Crisis. 2011;32:5–14. doi: 10.1027/0227-5910/a000046. [DOI] [PubMed] [Google Scholar]
- 40.Takahashi K, Kawai D, Nagata M, Watabe M. Fukigen na shokuba [Unpleasant Workplace] Kodansha, Tokyo: 2008. [Google Scholar]
- 41.Kato TA, Tateno M, Shinfuku N, et al. Does the ‘hikikomori’ syndrome of social withdrawal exist outside Japan? A preliminary international investigation. Soc Psychiatry Psychiatr Epidemiol. 2012;47:1061–1075. doi: 10.1007/s00127-011-0411-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Niiya Y, Ellsworth PC, Yamaguchi S. Amae in Japan and the United States: An exploration of a ‘culturally unique’ emotion. Emotion. 2006;6:279–295. doi: 10.1037/1528-3542.6.2.279. [DOI] [PubMed] [Google Scholar]
- 43.Teo AR, Stufflebam K, Saha S, et al. Psychopathology associated with social withdrawal: Idiopathic and comorbid presentations. Psychiatry Res. 2015;228:182–183. doi: 10.1016/j.psychres.2015.04.033. [DOI] [PubMed] [Google Scholar]
- 44.Teo AR, Fetters MD, Stufflebam K, et al. Identification of the hikikomori syndrome of social withdrawal: Psychosocial features and treatment preferences in four countries. Int J Soc Psychiatry. 2015;61:64–72. doi: 10.1177/0020764014535758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Heine SJ. Cultural Psychology. W. W. Norton & Company; New York: 2011. [Google Scholar]
- 46.Yamagishi T. Trust – The Evolutionary Game of Mind and Society. Springer Tokyo; Tokyo: 2011. [Google Scholar]
- 47.Yamagishi T, Cook KS, Watabe M. Uncertainty, trust, and commitment formation in the United States and Japan. Am J Sociol. 1998;104:165–194. [Google Scholar]
- 48.Cross SE, Hardin EE, Gercek-Swing B. The what, how, why, and where of self-construal. Pers Soc Psychol Rev. 2011;15:142–179. doi: 10.1177/1088868310373752. [DOI] [PubMed] [Google Scholar]
- 49.Markus HR, Kitayama S. Culture and the self: Implications for cognition, emotion, and motivation. Psychol Rev. 1991;98:224–253. [Google Scholar]
- 50.Oyserman D, Coon HM, Kemmelmeier M. Rethinking individualism and collectivism: Evaluation of theoretical assumptions and meta-analyses. Psychol Bull. 2002;128:3–72. [PubMed] [Google Scholar]
- 51.Matsumoto D. Culture and self: An empirical assessment of Markus and Kitayama’s theory of independent and interdependent self-construals. Asian J Soc Psychol. 1999;2:289–310. [Google Scholar]
- 52.Levine TR, Bresnahan MJ, Park HS, et al. Self-construal scales lack validity. Hum Commun Res. 2003;29:210–252. [Google Scholar]
- 53.Hashimoto H, Yamagishi T. Center for the Study of Cultural and Ecological Foundations of the Mind Working Paper Series. 141. Hokkaido University; 2014. Engaging and disengaging aspects of independence and interdependence: An adaptationist perspective. [Google Scholar]
- 54.Hashimoto H, Yamagishi T. Two faces of interdependence: Harmony seeking and rejection avoidance. Asian J Soc Psychol. 2013;16:142–151. [Google Scholar]
- 55.Li TM, Wong PW. Youth social withdrawal behavior (hikikomori): A systematic review of qualitative and quantitative studies. Aust N Z J Psychiatry. 2015;49:595–609. doi: 10.1177/0004867415581179. [DOI] [PubMed] [Google Scholar]
- 56.Holsboer F. The corticosteroid receptor hypothesis of depression. Neuropsychopharmacology. 2000;23:477–501. doi: 10.1016/S0893-133X(00)00159-7. [DOI] [PubMed] [Google Scholar]
- 57.Holsboer F, von Bardeleben U, Wiedemann K, Muller OA, Stalla GK. Serial assessment of corticotropin-releasing hormone response after dexamethasone in depression. Implications for pathophysiology of DST nonsuppression. Biol Psychiatry. 1987;22:228–234. doi: 10.1016/0006-3223(87)90237-x. [DOI] [PubMed] [Google Scholar]
- 58.Hori H, Teraishi T, Sasayama D, et al. Relationship of temperament and character with cortisol reactivity to the combined dexamethasone/CRH test in depressed outpatients. J Affect Disord. 2013;147:128–136. doi: 10.1016/j.jad.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 59.Hori H, Teraishi T, Ota M, et al. Psychological coping in depressed outpatients: Association with cortisol response to the combined dexamethasone/CRH test. J Affect Disord. 2014;152–154:441–447. doi: 10.1016/j.jad.2013.10.013. [DOI] [PubMed] [Google Scholar]
- 60.Hori H, Teraishi T, Ozeki Y, et al. Schizotypal personality in healthy adults is related to blunted cortisol responses to the combined dexamethasone/corticotropin-releasing hormone test. Neuropsychobiology. 2011;63:232–241. doi: 10.1159/000322146. [DOI] [PubMed] [Google Scholar]
- 61.Tyrka AR, Wier LM, Price LH, et al. Cortisol and ACTH responses to the Dex/CRH test: Influence of temperament. Horm Behav. 2008;53:518–525. doi: 10.1016/j.yhbeh.2007.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rinne T, de Kloet ER, Wouters L, Goekoop JG, DeRijk RH, van den Brink W. Hyperresponsiveness of hypothalamic-pituitary-adrenal axis to combined dexamethasone/corticotropin-releasing hormone challenge in female borderline personality disorder subjects with a history of sustained childhood abuse. Biol Psychiatry. 2002;52:1102–1112. doi: 10.1016/s0006-3223(02)01395-1. [DOI] [PubMed] [Google Scholar]
- 63.Gold PW, Chrousos GP. The endocrinology of melancholic and atypical depression: Relation to neurocircuitry and somatic consequences. Proc Assoc Am Physicians. 1999;111:22–34. doi: 10.1046/j.1525-1381.1999.09423.x. [DOI] [PubMed] [Google Scholar]
- 64.Kunugi H, Hori H, Ogawa S. Biochemical markers subtyping major depressive disorder. Psychiatry Clin Neurosci. 2015;69:597–608. doi: 10.1111/pcn.12299. [DOI] [PubMed] [Google Scholar]
- 65.Takeuchi T, Nakao M, Kachi Y, Yano E. Association of metabolic syndrome with atypical features of depression in Japanese people. Psychiatry Clin Neurosci. 2013;67:532–539. doi: 10.1111/pcn.12104. [DOI] [PubMed] [Google Scholar]
- 66.Hotamisligil GS. Inflammation and metabolic disorders. Nature. 2006;444:860–867. doi: 10.1038/nature05485. [DOI] [PubMed] [Google Scholar]
- 67.Horikawa H, Kato TA, Mizoguchi Y, et al. Inhibitory effects of SSRIs on IFN-gamma induced microglial activation through the regulation of intracellular calcium. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34:1306–1316. doi: 10.1016/j.pnpbp.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 68.Kato TA, Monji A, Mizoguchi Y, et al. Anti-inflammatory properties of antipsychotics via microglia modulations: Are antipsychotics a ‘fire extinguisher’ in the brain of schizophrenia? Mini Rev Med Chem. 2011;11:565–574. doi: 10.2174/138955711795906941. [DOI] [PubMed] [Google Scholar]
- 69.Kato TA, Yamauchi Y, Horikawa H, et al. Neurotransmitters, psychotropic drugs and microglia: Clinical implications for psychiatry. Curr Med Chem. 2013;20:331–344. doi: 10.2174/0929867311320030003. [DOI] [PubMed] [Google Scholar]
- 70.Mizoguchi Y, Kato TA, Seki Y, et al. Brain-derived neurotrophic factor (BDNF) induces sustained intracellular Ca2+ elevation through the up-regulation of surface transient receptor potential 3 (TRPC3) channels in rodent microglia. J Biol Chem. 2014;289:18549–18555. doi: 10.1074/jbc.M114.555334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Monji A, Kato T, Kanba S. Cytokines and schizophrenia: Microglia hypothesis of schizophrenia. Psychiatry Clin Neurosci. 2009;63:257–265. doi: 10.1111/j.1440-1819.2009.01945.x. [DOI] [PubMed] [Google Scholar]
- 72.Schulz K. New York Times. 2004. Did antidepressants depress Japan? [Google Scholar]
- 73.Healy D. The Antidepressant Era. Harvard University Press; Cambridge, MA: 1997. [Google Scholar]
- 74.American Psychiatric Publishing. Diagnostic and Statistical Manual of Mental Disorders. 4. American Psychiatric Publishing; Arlington, VA: 2000. text rev. [Google Scholar]
- 75.Parker G. Is depression overdiagnosed? Yes. BMJ. 2007;335:328. doi: 10.1136/bmj.39268.475799.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hashimoto R, Yasuda Y, Yamamori H, et al. Is it possible to make a diagnosis of major depression based solely on the medical interview of the patient? Seishinka. 2013;22:243–249. [Google Scholar]
- 77.Wang Y, Zhou Y, Li S, Wang P, Wu GW, Liu ZN. Impaired social decision making in patients with major depressive disorder. BMC Psychiatry. 2014;14:18. doi: 10.1186/1471-244X-14-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zhang HJ, Sun D, Lee TM. Impaired social decision making in patients with major depressive disorder. Brain Behav. 2012;2:415–423. doi: 10.1002/brb3.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Brendan Clark C, Thorne CB, Hardy S, Cropsey KL. Cooperation and depressive symptoms. J Affect Disord. 2013;150:1184–1187. doi: 10.1016/j.jad.2013.05.011. [DOI] [PubMed] [Google Scholar]
- 80.King-Casas B, Sharp C, Lomax-Bream L, Lohrenz T, Fonagy P, Montague PR. The rupture and repair of cooperation in borderline personality disorder. Science. 2008;321:806–810. doi: 10.1126/science.1156902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Berg J, Dickhaut J, McCabe K. Trust, reciprocity, and social history. Games Econ Behav. 1995;10:122–142. [Google Scholar]
- 82.Chiu PH, Kayali MA, Kishida KT, et al. Self responses along cingulate cortex reveal quantitative neural phenotype for high-functioning autism. Neuron. 2008;57:463–473. doi: 10.1016/j.neuron.2007.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kato TA, Watabe M, Tsuboi S, et al. Minocycline modulates human social decision-making: Possible impact of microglia on personality-oriented social behaviors. PLoS ONE. 2012;7:e40461. doi: 10.1371/journal.pone.0040461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Watabe M, Kato TA, Monji A, Horikawa H, Kanba S. Does minocycline, an antibiotic with inhibitory effects on microglial activation, sharpen a sense of trust in social interaction? Psychopharmacology. 2012;220:551–557. doi: 10.1007/s00213-011-2509-8. [DOI] [PubMed] [Google Scholar]
- 85.Watabe M, Kato TA, Teo AR, et al. Relationship between trusting behaviors and psychometrics associated with social network and depression among young generation: A pilot study. PLoS ONE. 2015;10:e0120183. doi: 10.1371/journal.pone.0120183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Nakano M. How supervisors deal with subordinates who have characteristics of ‘new-type depression’. Rinsho-Shinrigaku. 2014;14:235–243. [Google Scholar]
- 87.Tsujii H, Natsuhori K, Uozumi E. Nursing care for an adolescent hikikomori case with domestic violence: A case report. Nihon Seishinka Kangogaku Kaishi. 2010;52:72–76. [Google Scholar]
- 88.Nakagama H. Integration of individual and family conjoint interview: A case study of a social withdrawal adolescent and his family members. Kazoku-Shinrigaku-Kenkyu. 2008;22:28–41. [Google Scholar]