Summary
Mesenchymal stem cells (MSC) are of major interest to regenerative medicine, because of the ease of harvesting from a variety of sources (including bone marrow and fat aspirates) and ability to form a range of mesenchymal tissues, in vitro and in vivo. We focus here on the use of MSCs for engineering of cartilage, bone, and complex osteochondral tissue constructs, using protocols that replicate some aspects of the natural mesodermal development. For engineering of human bone, we discuss some of the current advances, and highlight the use of perfusion bioreactors for supporting anatomically exact human bone grafts. For engineering of human cartilage, we discuss limitations of current approaches, and highlight engineering of stratified, mechanically functional human cartilage interfaced with bone by mesenchymal condensation of MSCs. Taken together, the current advances enable engineering physiologically relevant bone, cartilage and osteochondral composites, and physiologically relevant studies of osteochondral development and disease.
Keywords: Cartilage, bone, regenerative medicine, bioreactor, anatomically shaped grafts
Introduction
Bone, cartilage, and their interface are each unique and complex tissues, but together they provide the structure and support systems necessary for load-bearing and movement. Damage to any of these tissues, caused by trauma or diseases such as osteoarthritis, can cause pain, inhibit functionality and restrict mobility of the patient. In the United States alone, there are over 1.7 million osteochondral surgical procedures performed each year (1). Such invasive surgeries were previously limited to elderly patients suffering from extensive osteoarthritis or brittle bones caused by osteoporosis. However, the last 20 years has seen a substantial increase in the number of corrective procedures performed in younger age groups (2). Characteristically, this younger age group is more active, and demands higher performance from treatment options (3).
Currently, surgical treatments include manufactured, natural, and autologous options. Manufactured options mostly use a combination of metal and plastic. These solutions provide excellent mechanical properties that restore structure and mobility, factors especially important for joint replacements (4). However, despite extensive research on bio-integration into native tissue, a high percentage of implants still do not fully integrate with the host tissue and eventually experience failure (5). Currently, the average lifetime of a manufactured implant is 10–15 years (6), meaning younger generations will undergo multiple replacement surgeries during their lifetime. In addition, inert solutions lack the ability to grow and adapt with the native tissue, and in some cases induce negative adaptation, which in turn requires surgical intervention (5).
Natural treatment solutions are based on the use of tissues that are xenogenic (from animals) and allogenic (from other patients). With advancements in removing cellular material, decellularized allografts and xenografts have become a frequent treatment option (7). Decellularized grafts maintain the original structure, composition and mechanical properties of the extracellular matrix, while the removal of the cellular components prevents the activation of immune responses and graft rejection (5). In principle, decellularized tissue grafts provide a natural, non-inflammatory framework for cell infiltration, graft incorporation, and regeneration of the tissue structure. However, in clinical practice these grafts have limited osteogenicity and clinical outcomes are not predictable. Recent research has focused on the use of growth factors doped into these scaffolds to elicit more predictable and robust outcomes (5, 8).
Autologous solutions (tissues harvested from another region in the same patient) are the current gold standard for bone and cartilage repair. Autologous grafts have the advantage of being from the patient’s own body, thereby preventing rejection events. In addition, the presence of native cells and vasculature within the tissue should result in predictable regeneration and recovery of the treated tissue (9). A major disadvantage of the autologous solution is the need to harvest donor tissue, which is always in limited supply (5). Besides requiring additional time for the patient on the operating table, the harvest site experiences donor-site morbidity (7, 8). Also, the harvested tissue is not in the correct anatomical shape, so the surgeon must shape the graft.
These limitations in the use of tissue autografts have heightened interest in the fast-developing field of tissue engineering. Tissue engineering proposes to combine the benefits from each of the current solutions to produce an autologous, integrative solution with adequate mechanical properties, thereby providing a customized graft for the osteochondral surgical intervention that does not require tissue harvest. Tissue engineers strive to construct patient-tailored tissue grafts utilizing a combination of three elements: scaffolds, bioreactors and cells (10). Scaffolds provide the main framework of the tissue, and have been created from both synthetic and natural sources (11). With synthetic scaffolds, engineers are able to control the chemical make-up, degradation rate, isotropy, and mechanical properties of the tissue (11). Scaffolds derived from natural tissues, such as decellularized allografts, have fantastic biocompatibility and usually contain important factors that aid in the regeneration process (11).
Bioreactors allow engineers to recreate on the benchtop, key aspects of the in vivo environment (10). Common osteochondral bioreactors include perfusion bioreactors, to replicate vasculature by providing adequate nutrient transport and waste removal, and bioreactors with mechanical stimulation, to replicate the physiological stresses placed on tissues (12–14). These bioreactors can be used to develop and mature tissue before implantation, and also as highly controllable tools for investigating normal and diseased tissue states (15).
The cells, incorporated in vitro, modify the tissue engineered construct in preparation for implantation, and can have a critical impact on regeneration after placement in vivo. Initially in tissue engineering strategies, primary cells were utilized. These cells had the capacity to create and maintain a desired tissue and have produced exciting results (16–19). However, sources of these cells can be a problem. Allogeneic sources are readily available and the cells can be easily harvested, but cause tissue rejection when implanted, while autologous cells can only be obtained by sacrificing tissue at another location in the body, similar to tissue harvest for autografts.
In response to problems with the use of primary cells, mesenchymal stem cells (MSC) have been actively explored as a source of cells with a major clinical interest. Residing in the mesoderm that drives the formation of the entire osteochondral tissue, mesenchymal stem cells have been harvested from a variety of tissues (see Table 1 for an overview of tissue sources for isolation of MSC), with evidence suggesting that stem cells can be isolated from any vascularized construct (20, 21). The mesenchymal nature of MSCs provides an ideal solution for engineering osteochondral grafts. These cells enable replication of the natural mesodermal development, leading to the formation of entire ostepchondral constructs comprising multiple tissue types from a single batch of easily harvested autologous cells (20, 22, 23).
Table 1.
Tissue sources for deriving mesenchymal stem cells for osteochondral tissue engineering
In this chapter, we focus on the use of MSC for tissue engineering of osteochondral tissues. We also discuss recent developments in engineering of cartilage and bone from human MSCs, and describe potential strategies to unify multiple tissue types into a single, complete osteochondral graft.
MSC for Engineering Bone
Over the last two decades, advancements have been made in determining the appropriate scaffold to influence MSC differentiation. Mechanically stiff substrates (29), the application of mechanical forces (30) and the inclusion of minerals into the scaffold (31) all stimulate osteogenic differentiation and bone formation. A majority of studies have shown satisfactory bone formation in vitro, and many have even shown the ability of engineered bone to regenerate and integrate into the native skeleton (32–35). The in vivo studies were most commonly performed in the mouse subcutaneous pouch or a rat calvarial defect.
The small size of the animals necessitated the use of similarly small constructs. During cultivation of these small constructs, passive diffusion was sufficient to ensure adequate nutrient delivery and waste removal. However, increasing the complexity and size of the constructs has proven difficult, primarily due to passive diffusion no longer being sufficient for cell cultivation. The lack of nutrition and waste management causes cell death and necrosis in the interior, destroying the scaffold. Current research is focused on resolving this problem, by designing strategies to enhance transport throughout the bone interior, allowing eventually the production of complex, anatomical constructs.
One important strategy enables pre-vascularization of bone grafts facilitating communication with the vasculature of the host. Current research initiatives are pursuing smart scaffold designs, providing structural pathways and growth factors to attract vascular formation (36, 37). Another research direction utilizes co-culture of MSC/MSC-derived osteoblasts with vascular cells (38–40). These studies aim to facilitate interactions between the cells and promote the construction of natural vascular pathways. Therefore, upon implantation, the host will integrate with the pre-formed structures, establishing circulation more readily.
In parallel studies, media compositions were developed to differentiate MSC into hypertrophic chondrocytes (41, 42). Triggering of chondrogenic maturation in vitro resulted, following implantation in vivo, in the formation of bone and bone marrow, replicating the endochondral ossification pathway that is associated with bone development and fracture repair (42, 43). Hypertrophic chondrocytes are essential for endochondral ossification as they initiate transition from the soft callus to provisional bone by provoking vascular invasion and depositing the bone template (44). Hypertrophic chondrocytes are an attractive tool for tissue engineering because of their survival in the hypoxic environment of cartilage, thereby withstanding the time delay necessary for vascular development in vivo (42).
A promising route for growing bone grafts in vitro, and maintaining their viability for an extended period of time to allow differentiation and maturation, is with perfusion bioreactors (45–47). Perfusion bioreactors provide nutrients and – most critically – oxygen to the entire construct, permitting cell growth and maturation regardless of the complexity of the scaffold shape. Perfusion is critically important for engineering bone and other metabolically active, vascularized tissues, as the diffusional depth of oxygen supply is only a fraction of a millimeter.
In the following section, the highlighted paper details the advancement of perfusion bioreactors from those supporting generic, small-size constructs to those designed to engineer anatomically exact human bone grafts. To create these complex grafts, Grayson, et al. approached the problem in three separate steps: generation of the anatomically exact scaffold, construction and validation of a unique bioreactor, and integration of the two during cultivation (48).
Highlight: “Engineering Anatomically Shaped Human Bone Grafts” Grayson et al. (48)
The exact anatomical dimensions of the mandibular condyle, selected as a model due to its complex shape and need for bone grafting solutions for the temporomandibular joint, were determined by computed tomography scans. Using specialized, commercially available computer software, the 2D slices of the scan were reconstructed into a 3D file that could be imported into computer-aided manufacturing (CAM) software to produce the necessary fabrication steps for the computer-numerical-control (CNC) milling machine. Decellularized trabecular bone was chosen as the scaffold for its structural, biochemical, osteoinductive and mechanical properties, and micromilled to the exact anatomical shape.
Control of perfusion through the bone scaffold was dictated by the design of a specific anatomically shaped perfusion chamber, also created using the converted computed tomography scans. The perfusion chamber - a PDMS negative mold of the scaffold - was compressed by two manifolds to direct the medium flow through the cell-seeded scaffold. Clamps on the flow tubing allowed control of the flow rate. Computational modeling was conducted to verify that the chosen flow rates produced satisfactory perfusion to all areas of the scaffold. The method is shown in Figure 1.
Figure 1. Tissue engineering of anatomically shaped bone grafts.
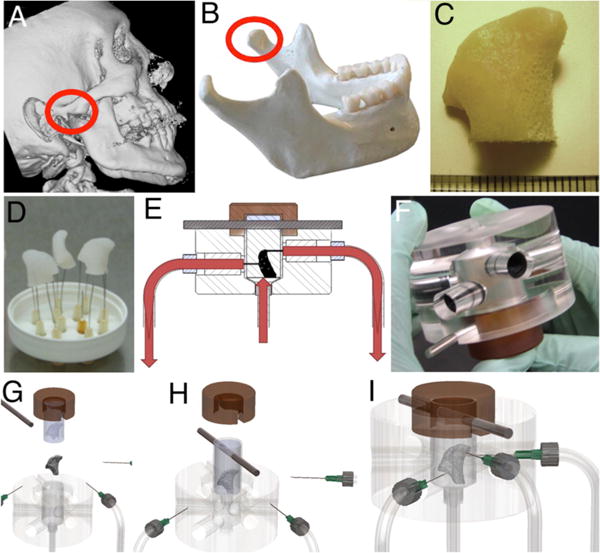
(A–C) Scaffold preparation. (A, B) Clinical CT images were used to obtain high-resolution digital data for the reconstruction of the exact geometry of human temporomandibular joint (TMJ) condyles. (C) These data were incorporated into the MasterCAM software to machine TMJ-shaped scaffolds from fully decellularized trabecular bone. (D) A photograph illustrating the complex geometry of the final scaffolds that appear markedly different in each projection. (E) The scaffolds were seeded in a stirred suspension of hMSC, using 3 million cells per scaffold (~1 cm3 volume), pre-cultured for 1 week to allow cell attachment, and cultured with perfusion through the cell-seeded scaffold for an additional 4 weeks. (F) A photograph of the perfusion bioreactor used to cultivate anatomically shaped grafts in vitro. (G–I) Key steps in the bioreactor assembly. Images are reproduced with permission from reference (48).
Human bone marrow stem cells were expanded and seeded into the anatomically shaped scaffolds using the spinner flask method. After loading into the bioreactor, the scaffolds were cultured for five weeks in osteogenic medium. After cultivation, constructs under perfusion had a 7.5 fold increase in DNA compared with statically cultured constructs, with histological analysis showing significant cell viability and bone deposition in all parts of the scaffold. In the static controls, the interior of the complex scaffolds was devoid of cells and showed only minimal bone deposition. Temporal evaluation of the constructs using μCT demonstrated a significant increase in bone volume over five weeks, and displayed significantly more bone volume than the statically cultivated constructs. Differences in the development and matrix deposition between the two groups are shown in Figure 2.
Figure 2. Effects of perfusion on bone formation in vitro.
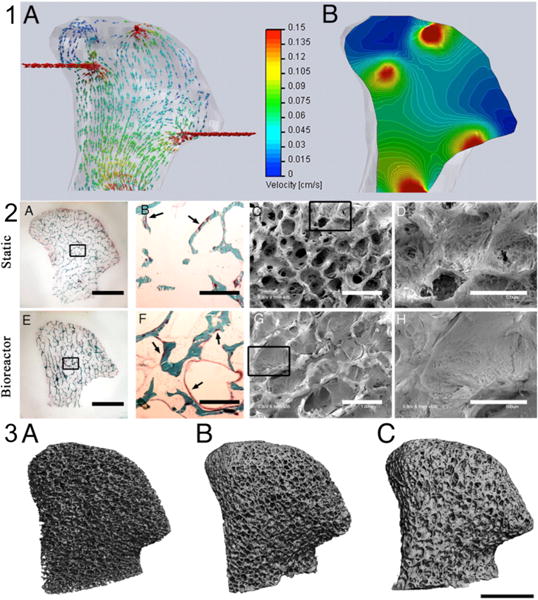
(1) Computational models of medium flow through TMJ constructs during bioreactor cultivation. (1A) Color-coded velocity vectors indicate the magnitude and direction of flow through the entire construct based on experimentally measured parameters. (1B) Construct is digitally sectioned, and the color-coded contours are used to indicate the magnitude of flow in the inner regions. (2A–H) Bone formation was markedly enhanced by perfusion, in a manner dependent on the fluid flow pattern. (2A–D) Constructs cultured under static conditions. (2E–H) Constructs cultured with medium perfusion. (2A, E) Trichrome staining of the entire cross-section of scaffolds showing differences in the new matrix distribution (red) compared with the original scaffold (green) for the static (2A) and perfused (2E) culture groups. (2B, F) Major differences in osteoid formation (arrows) in the central regions of constructs cultured statically (2B) and in perfusion (2F). (2C, D, G, H) SEM images of the central construct regions. (2C, D) Statically cultured constructs exhibit empty pore spaces and loosely packed cells. (2G, H) Constructs cultured in perfusion demonstrate the formation of dense and confluent lamellae of bone tissue that fill entire pore spaces. (Scale bars - 2A, E: 5 mm; 2B, C, F, G: 1 mm; 2D, H: 500 μm.) (3A–C) Architecture of the mineralized bone matrix developed over time and in a manner dependent on culture conditions. The reconstructions of 3D μCT images demonstrate the changes in pore structure (relative to the initial state) that were evident at the end of the 5th week of cultivation. (Scale bar: 5 mm.) Images reproduced with permission from reference (48)
In summary, the use of a custom-designed perfusion system allowed successful, development of viable, anatomically shaped engineered tissues, proving their validity and advancing tissue engineered bone grafts towards clinical translation.
Engineering Cartilage using MSCs
Early studies demonstrated the efficacy of synthetic materials, such as polyglycolic acid (PGA) and poly-L-lactic acid (PLLA), as scaffolds for primary chondrocytes both in vitro and in vivo (49, 50). In addition to the scaffold-based cell carriers, hydrogels such as agarose and alginate, consisting of water-swollen networks, were also widely used as carriers to maintain chondrocyte phenotype and provide local microenvironmental control (51). While trophic factors such as TGF-β are essential for chondrogenesis, biophysical stimulation such as deformational loading has also been used to modulate cartilage development in vitro (18, 52). These studies contributed to an overall tissue-engineering paradigm involving three-dimensional environments with tissue-specific biochemical and biophysical stimulation.
Despite their well-established ability to form cartilage in vitro, chondrocytes have limited proliferative ability and are prone to de-differentiation in vitro. Investigators attempted to extend methods successfully used with chondrocytes to the engineering of cartilage from MSC, but only with limited success. In particular, studies comparing the use of agarose to engineer cartilage from chondrocytes and from MSCs revealed that MSCs formed cartilaginous tissues with subnormal biochemical and mechanical properties (19, 53). Still, several studies showed that long-term culture with the application of TGF-β, mechanical stimulation, osmotic loading and enzymatic treatment all improved the properties of cartilage grown from agarose seeded with MSCs (19, 53–55).
Multiple labs have shown that incorporation of glycosaminoglycans such as hyaluronic acid and chondroitin sulfate by polymerization into hydrogels recreated a biomimetic microenvironment for chondrogenesis (56–58). Furthermore, scaffold architecture can also be designed to mimic that of native cartilage matrix, as studies showed that interlocking woven polycaprolactone (PCL) supported the formation of cartilaginous tissue (59). Interestingly, investigators adapted these techniques for making cell-instructive and bioactive scaffolds to further enhance cartilage formation by controlling differentiation of hMSC. For example, Bian et al showed that neo-cartilage formation by hMSC in vivo could be enhanced by incorporating N-cadherin, an intercellular cell binding protein implicated in cell condensation that precedes cartilage formation, into methacrylated HA (60). Similarly, Brunger et al showed that a viral vector immobilized on a woven PCL scaffold could mediate transduction of hMSC and drive TGF-β3 expression, thus leading to potent chondrogenic differentiation (61).
Highlight: self-assembly of hMSC into functional and stratified cartilage (71)
While it is evident that biomimetic methods enhance tissue formation by simulating the native microenvironment, the formation of physiologic tissue by progenitor cells ultimately required lessons taken from native tissue morphogenesis. Self-assembly has been proposed as an in vitro method for recapitulating mesenchymal condensation that precedes chondrogenesis.(62)
Scaffold-free cartilage formation by self-assembly of hMSC was first introduced as the pellet culture, whereby cells centrifuged into high-density aggregates were cultured in chondrogenic medium. This method was shown to recapitulate the progression of chondrogenesis (63, 64). Still, the proponents of scaffold-based cartilage tissue engineering criticized the use of pellets for their physiologically irrelevant size, geometry and mechanical properties. Similar to earlier studies with chondrocytes, studies also showed that MSC self-assembled on scaffold formed cartilaginous tissues that resembled hyaline cartilage with dense ECM and zonal organization (65–70).
Our lab recently showed that fusion of condensed mesenchymal bodies (CMBs) on decellularized bone (DCB) can lead to the formation of large, functional and well organized cartilage grafts (71). To overcome the limitations in size and geometry of the pellets, numerous CMBs were packed, within a mold, onto the surface of decellularized bone and cultured for up to 5 weeks (Figure 3). For the first time, centimeter-sized cartilage with physiologic stratification, mechanical and tribological properties comparable to native cartilage was successfully grown in vitro from hMSC (Table 2).
Figure 3. In vitro formation of physiologically stratified, stiff and frictionless human cartilage interfaced with a bone substrate.
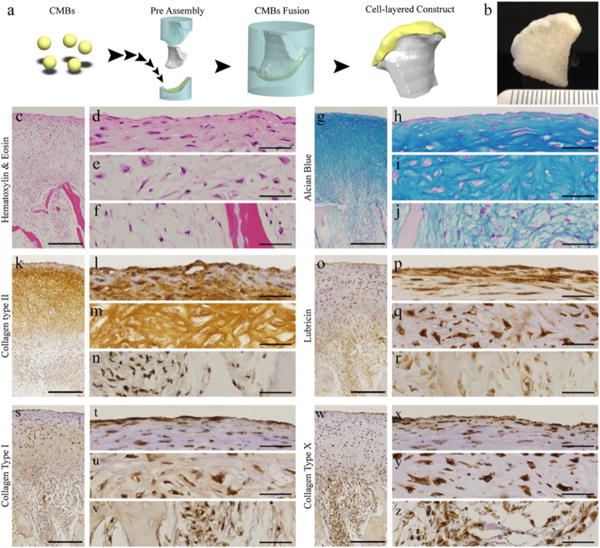
Cartilage was formed from condensed mesenchymal bodies (CMBs) press fit onto a bone substrate, and cultured in vitro, as reported by Bhumiratana et al (71). (A–B) CMBs were press-fitted within molds on a decellularized bone scaffold (DCB), forming cartilage after 5 weeks of chondrogenic induction. Histological and immunohistochemical analysis showing representative stains of (C–F) H&E, (G–J) Alcian Blue for GAG, (K–N) collagen type II, (O–R) lubricin, (S–V) collagen type I, and (W–Z) collagen type X. (Scale bar: 500 μm in low-magnification images, 50 μm in high-magnification images.)
Table 2.
Mechanical properties of human cartilage engineered by CMB fusion
| Articular cartilage constructs | Young’s modulus, kPa | Minimum friction coefficient, μmin | Equilibrium friction coefficient, μmax |
|---|---|---|---|
| Day 3 CMBs | 788 ± 200 | 0.049 ± 0.008 | 0.276 ± 0.033 |
| Day 5 CMBs | 825 ± 197 | 0.046 ± 0.010 | 0.283 ± 0.042 |
| Day 7 CMBs | 457 ± 46* | 0.064 ± 0.013 | 0.334 ± 0.053 |
Interestingly, we also observed that the formation of boundaries around CMBs, indicated by the presence of tenascin-C, limits integration of CMBs that must be fused within 3 to 5 days following chondrogenic induction to achieve successful integration. The boundaries between CMBs that were fused after one week of condensation persisted for a long time in culture, hindered integration and resulted in formation of cartilage with subnormal mechanical and tribological properties. Other early chondrogenic markers characteristic of mesenchymal condensation were also increasingly expressed during the first week of culture prior to the onset of ECM production. This study showed the feasibility of engineering cartilage by self-assembly of hMSC pellets, using a method that mimics mesenchymal condensation.
Engineering Osteochondral Composites using MSCs
The osteochondral composite consists of a cartilage layer above a bone layer, with a functional interface between the two tissue layers. Engineering such a complex tissue presents significant challenges, as the articular cartilage and the subchondral bone comprise different cell types and different microenvironments. Also, the subchondral bone has a much higher mechanical stiffness than articular cartilage.
The strategies proposed and evaluated for fabrication of osteochondral composites have been summarized in two excellent recent reviews (72, 73). Broadly, the strategies can be classified according to their selection of the scaffold and cell source for cartilage and bone layers (Figure 4). Some investigators formed the cartilage layer using chondrocytes, while others chose to form both the cartilage layer and the bone phase using MSCs in order to overcome the limitations of chondrocytes.
Figure 4. Approach to assembling osteochondral composites.

The schematic shows one of the scaffolds and cell based strategies for engineering osteochondral composites discussed here, proposed by Martin et al (72).
Most commonly, investigators used bi-layered scaffolds whereby the cartilage layer comprises a synthetic or natural polymer and the bone layer comprises polymers, ceramics or metals. The cartilage and bone layers were combined using sutures and adhesives, such as fibrin. Interestingly, several groups used a scaffold-free approach similar to self-assembly methods for culturing cells at high density on top of the bone layer. In these various approaches, desirable outcomes of the in vitro culture and in vivo implantation were generally associated with strong integration between the cartilaginous and bone layer, sometimes with the formation of a calcified transition zone.
In a functional osteochondral unit, the interface needs to recapitulate the transition between bone and cartilage with strong integration between the layers. In the articular cartilage, deep zone collagen fibrils extend into the calcified layer that inter-digitates with the subchondral bone. In addition to integrating the cartilage and bone, the calcified cartilage distributes load across the interface between the biomechanically incompatible non-mineralized cartilage and mineralized subchondral bone.
Depending on the method of seeding and the choice of scaffold for the bone layer, the production of cartilaginous ECM and the transition of this matrix into calcified cartilage at the interface can be enhanced using various methods. For example, Schaefer and colleagues reported that a chondrocyte-seeded PGA mesh sutured with a collagen-hydroxyapatite (Col-HA) sponge had the ability to integrate following long term implantation (74). Similarly, Wang and colleagues showed that the scaffold free, high density seeding of chondrocytes atop of a porous osteoconductive scaffold resulted in neo-cartilage integration with the collagen-hydroxyapatite (Col-HA) scaffold (75). Kandel and colleagues showed the formation of mechanically strong cartilage by self-assembly of chondrocytes on calcium polyphosphate (CPP) in a long-term orthotopic sheep model. Finally, Allan and colleagues subsequently showed enhanced cartilage-bone integration with deep zone mineralization of chondrocytes cultured on CPP in the presence of β-glycerophosphate (β-GP) (76, 77). Thus, it is evident that ECM integration and calcified layer formation are important determinants of the composite outcome.
Highlight: Osteochondral composites and the calcified cartilage
Several groups have reported that high-density scaffold-free cultures of chondrocytes on polymer-ceramic bone scaffolds could result in the formation of well-integrated osteochondral composites. Our lab introduced the fusion of scaffold-free mesenchymal bodies with the bone substrate, followed with bioreactor culture of the composite tissue.
This new method resulted in the formation of a physiologically stratified cartilage layer that resembled the stiffness and frictionless properties of native cartilage and was well integrated with the underlying bone matrix (71). RemTuli et al also showed in an earlier study, the formation of an organized osteochondral composite with distinct cartilage-bone transition by press coating a PLA scaffold with a chondrogenically induced hMSC pellet (78). Both investigations reported scaffold free formation of an organized cartilage layer that was well integrated with the bone substrate. Of note, our use of DCB as the bone layer scaffold is similar to the successful use of Col-HA scaffolds in earlier investigations. Also, we optimized the approach to scaffold free cartilage formation on an anatomical scale from hMSC by fusion of numerous CMBs.
In our study, we did not observe the formation of calcified cartilage and our bone layer consisted of native bone matrix permeated with cells from the cartilage layer without osteogenic induction. Tuli et al showed the concomitant formation of a bone layer by separately seeding the bone scaffold with ostegenically induced MSC. The studies in the Kandel lab and Allan lab observed deep zone hypertrophy and the formation of a calcified layer at the cartilage-bone interface when scaffold free chondrocytes were cultured on a ceramic scaffold in the presence of a phosphate source (β-GP). Interestingly, Khanarian et al recently reported enhanced mineralization and matrix deposition by hypertrophic chondrocytes in a hydrogel-ceramic composite containing micro-HA particles that recapitulated the aggregate size and content of the native mineral (79).
Taken together, these studies show that a suitable biomimetic approach to engineering osteochondral composites from hMSC could involve a scaffold-free formation of the cartilage layer by high density culture of hMSC atop an osteoinductive scaffold seeded with osteogenically induced hMSC. Further, formation of a calcified layer at the interface could be enhanced with a soluble phosphate source and the incorporation of ceramic at the interface as well as in the osteoinductive scaffold.
Future Directions
The use of MSC in osteochondral tissue engineering is a highly attractive proposition, as autologous MSC are easily accessible and readily form bone and cartilage. For the purpose of personalized regenerative medicine, it is evident that cartilage and bone grafts as well as their composites can be entirely derived from MSC taken from each subject, with the application of tissue engineering methods that are inspired by cartilage and bone development. As highlighted above, the pursuit of engineering bone, cartilage and osteochondral composites from MSC have taken interesting directions, and the progress made is gratifying. Still, there are numerous problems that need to be addressed, as investigators search for biologically inspired regenerative approaches.
For MSC based bone tissue engineering, concerns remain about the long-term viability of grafts following implantation. It is believed that after implantation, cells in the interior will die before the host vasculature can penetrate the graft, triggering necrosis and graft failure. To address this issue, investigators are using two complementary approaches: promoting pre-vascularization of bioengineered grafts and directing maturation of MSC to recapitulate endochondral ossification. Pre-vascularization of the bone graft is expected to facilitate rapid vascularization following implantation. Current initiatives are pursuing smart scaffold designs to provide structural pathways and growth factors for connecting the graft to the host vasculature (37, 80), and co-cultures of MSC/MSC-derived osteoblasts with vascular cells (81, 82).
Another fascinating direction emerged from the studies of Mueller et al and Scotti et al who developed media for differentiating MSCs toward hypertrophic chondrocytes (42, 83). Triggering chondrogenic maturation resulted in the formation of bone and bone marrow in vivo, by replicating the endochondral ossification pathway utilized in bone development and long bone fracture repair (42, 43). Hypertrophic chondrocytes are essential in endochondral ossification as they trigger transition from the soft callus to preliminary bone by provoking vascular invasion and deposition of the initial bone template (44). Hypertrophic chondrocytes are an attractive tissue engineering tool due to their survival in the hypoxic environment of cartilage, thereby withstanding the time delay necessary for the vascular development they help orchestrate (42). Tissue engineered bone grafts are on the verge of clinical translation, and the relentless progression of the field will hopefully produce the most clinically appropriate grafts for treating numerous patients requiring bone grafts. The rapid advancement in bone tissue engineering is likely to convert this exciting bone technology into routine practice.
Similarly, MSC based cartilage tissue engineering has its unique problems, even though the functional properties of in vitro grown cartilage are increasingly approaching the functional properties of native cartilage. Of note, hMSC derived cartilage is prone to hypertrophy and mineralization not seen with chondrocyte based cartilage. Recent investigations have shown that hypertrophy correlates with the tendency to mineralize ectopically in vivo and that cartilage formed by MSC was unstable and could spontaneously mineralize in long term in vitro cultures (83–86).
Interestingly, the mineralization of cartilage formed by MSC is usually localized, which suggests that MSC could have different chondrogenic fates. Whether the organization and differentiation fate of MSC can be controlled during in vitro cartilage formation is still very much a work in progress. Still, some recent studies have shed light on how we might be able to better control chondrogenic differentiation of hMSC. With the availability of compound libraries and high throughput screening technology, potent small molecules for chondrogenic differentiation of hMSC are being discovered. Recent studies have shown that these small molecules can enhance the in vitro and in vivo cartilage formation by association with a key transcription factor, RUNX1 (87, 88).
The role of oxygen tension during in vitro chondrogenesis has also been clarified as investigators have shown that sustained hypoxia promoted the formation of cartilage by hMSC with denser ECM and this construct is less prone to mineralize (89). Further, the requirements of cartilage homeostasis have also been elucidated as investigators have shown, using in vivo models, that the depletion of either superficial zone progenitors or superficial zone proteins resulted in articular cartilage degradation (90, 91). These studies have advanced our collective understanding of what drives cartilage formation, maturation and homeostasis. For tissue engineers, the problem remains to specify cartilage formation effectively and accurately so that cartilage grown in vitro can be used to treat cartilage injuries and diseases as well as restore joint homeostasis.
Osteochondral composites have been proposed as an in vitro model for understanding the pathogenesis of degenerative joint diseases with cartilage and bone etiologies such as osteoarthritis. To recreate osteochondral composites from MSC, accurate spatiotemporal control of trophic factors is essential as the articular cartilage and the subchondral bone consist of different cell types in different microenvironments. We are now moving towards developing bioreactors for optimizing simultaneous chondrogenic and osteogenic differentiation of MSC within a biphasic osteochondral composite. Biophysical cues such as compressive loading and interstitial shear, which have been shown to benefit chondrogenic and osteogenic differentiation, should be made compatible with bioreactor designs (92–95).
Moving forward, the methods for engineering physiologically relevant bone, cartilage and osteochondral composites from MSC need to be inspired by a keen understanding of the development, maturation and homeostasis of native cartilage and bone. The interactions between multiple signaling pathways and multiple cell types governing joint morphogenesis and endochondral ossification are just a few aspects of the complexities that are the focus of current undertakings by biologists and clinicians (62, 96–99). These investigations should provide critical insights into strategies for engineering osteochondral grafts from MSC, and aid development of models for studying osteochondral development and disease.
Figure 5. Osteochondral composites obtained by combining pre-grown cartilage and bone.
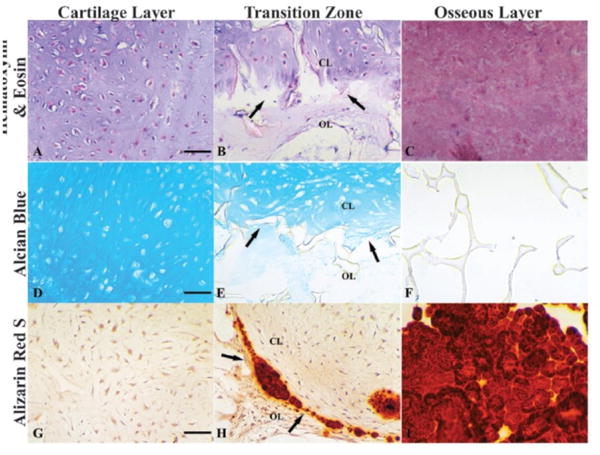
The panel shows osteochondral constructs cultured for 10 weeks following the assembly of cartilage and bone regions. (A–C) H&E for the cells and matrix of the cartilage layer (A), sharply demarcated transition zone (B, arrows), and an osseous layer (C); (D–F) alcian blue, for proteoglycan that is strongly positive in the cartilage layer (D), diminishingly positive in the transition zone (E, arrows), and negative in the osseous layer (F); (G–I) alizarin red staining, for mineralization that was negative in the cartilage layer (G), and strongly positive in the transition zone (H, arrows) and the osseous layer (I). CL: cartilage layer; OL: osseous layer. Scale bars: 80 μm. Reproduced with permission from Tuli et al (78).
Acknowledgments
Funding of the work described in this chapter has been provided by the NIH (grants DE016525, EB002520, AR061988 to GVN), A*STAR Graduate Academy in Singapore (grant S8725508E to JN), NSF (graduate fellowship to JB), Whitaker Foundation (fellowship to JB) and Columbia University (Presidential Fellowship to JB).
References
- 1.Inpatient Surgery: National Center for Health Statistics. 2013 [cited 2014 November 20]. Available from: http://www.cdc.gov/nchs/fastats/inpatient-surgery.htm.
- 2.Orthopedic Instrumentation BioMed Trends. 2010 http://www.biomedtrends.com/GetDetails.asp?CatName=Orthopedics.
- 3.Minzlaff P, Feucht MJ, Saier T, et al. Can young and active patients participate in sports after osteochondral autologous transfer combined with valgus high tibial osteotomy? Knee surgery, sports traumatology, arthroscopy. 2014 doi: 10.1007/s00167-014-3447-x. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 4.Hayes JS, Richards RG. The use of titanium and stainless steel in fracture fixation. Expert Rev Med Devices. 2010;7:843–853. doi: 10.1586/erd.10.53. [DOI] [PubMed] [Google Scholar]
- 5.Barone DTJ, Raquez JM, Dubois P. Bone-guided regeneration: from inert biomaterials to bioactive polymer (nano) composites. Polym Adv Technol. 2011;22:463–745. [Google Scholar]
- 6.Hip Fracture: Cleveland Clinic. 2014 [cited 2014 November 20]. Available from: https://my.clevelandclinic.org/services/orthopaedics-rheumatology/diseases-conditions/hip-fracture.
- 7.Giannoudis PV, Dinopoulos H, Tsiridis E. Bone substitutes: An update. Injury-Int J Care Inj. 2005;36:20–27. doi: 10.1016/j.injury.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 8.Calori GM, Mazza E, Colombo M, et al. The use of bone-graft substitutes in large bone defects: Any specific needs? Injury-Int J Care Inj. 2011;42:S56–S63. doi: 10.1016/j.injury.2011.06.011. [DOI] [PubMed] [Google Scholar]
- 9.Salgado AJ, Coutinho OP, Reis RL. Bone tissue engineering: State of the art and future trends. Macromol Biosci. 2004;4:743–765. doi: 10.1002/mabi.200400026. [DOI] [PubMed] [Google Scholar]
- 10.Langer R, Vacanti JP. Tissue Engineering. Science. 1993;260:920–926. doi: 10.1126/science.8493529. [DOI] [PubMed] [Google Scholar]
- 11.Hutmacher DW. Scaffolds in tissue engineering bone and cartilage. Biomaterials. 2000;21:2529–2543. doi: 10.1016/s0142-9612(00)00121-6. [DOI] [PubMed] [Google Scholar]
- 12.Griffith LG, Naughton G. Tissue engineering - Current challenges and expanding opportunities. Science. 2002;295:1009–1014. doi: 10.1126/science.1069210. [DOI] [PubMed] [Google Scholar]
- 13.Hansmann J, Groeber F, Kahlig A, et al. Bioreactors in tissue engineering - principles, applications and commercial constraints. Biotechnol J. 2013;8:298–307. doi: 10.1002/biot.201200162. [DOI] [PubMed] [Google Scholar]
- 14.Martin I, Wendt D, Heberer M. The role of bioreactors in tissue engineering. Trends in Biotechnology. 2004;22:80–86. doi: 10.1016/j.tibtech.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 15.Vunjak-Novakovic G, Tandon N, Godier A, et al. Challenges in Cardiac Tissue Engineering. Tissue Eng Part B-Rev. 2010;16:169–187. doi: 10.1089/ten.teb.2009.0352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hutmacher DW, Schantz T, Zein I, et al. Mechanical properties and cell cultural response of polycaprolactone scaffolds designed and fabricated via fused deposition modeling. J Biomed Mater Res. 2001;55:203–216. doi: 10.1002/1097-4636(200105)55:2<203::aid-jbm1007>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 17.Wang YZ, Blasioli DJ, Kim HJ, et al. Cartilage tissue engineering with silk scaffolds and human articular chondrocytes. Biomaterials. 2006;27:4434–4442. doi: 10.1016/j.biomaterials.2006.03.050. [DOI] [PubMed] [Google Scholar]
- 18.Mauck RL, Nicoll SB, Seyhan SL, et al. Synergistic action of growth factors and dynamic loading for articular cartilage tissue engineering. Tissue Engineering. 9:597–611. doi: 10.1089/107632703768247304. [DOI] [PubMed] [Google Scholar]
- 19.Mauck RL, Yuan X, Tuan RS. Chondrogenic differentiation and functional maturation of bovine mesenchymal stem cells in long-term agarose culture. Osteoarthritis and Cartilage. 2006;14:179–189. doi: 10.1016/j.joca.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 20.Caplan AI. Mesenchymal Stem-Cells. J Orthop Res. 1991;9:641–650. doi: 10.1002/jor.1100090504. [DOI] [PubMed] [Google Scholar]
- 21.Crisan M, Yap S, Casteilla L, et al. A perivascular origin for mesenchymal stem cells in multiple human organs. Cell Stem Cell. 2008;3:301–313. doi: 10.1016/j.stem.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 22.Mauney JR, Volloch V, Kaplan DL. Role of adult mesenchymal stem cells in bone tissue-engineering applications: Current status and future prospects. Tissue Eng. 2005;11:787–802. doi: 10.1089/ten.2005.11.787. [DOI] [PubMed] [Google Scholar]
- 23.Pittenger MF, Mackay AM, Beck SC, et al. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284:143–147. doi: 10.1126/science.284.5411.143. [DOI] [PubMed] [Google Scholar]
- 24.Zuk PA, Zhu M, Mizuno H, et al. Multilineage cells from human adipose tissue: Implications for cell-based therapies. Tissue Eng. 2001;7:211–228. doi: 10.1089/107632701300062859. [DOI] [PubMed] [Google Scholar]
- 25.Seo BM, Miura M, Gronthos S, et al. Investigation of multipotent postnatal stem cells from human periodontal ligament. Lancet. 2004;364:149–155. doi: 10.1016/S0140-6736(04)16627-0. [DOI] [PubMed] [Google Scholar]
- 26.Yoshimura H, Muneta T, Nimura A, et al. Comparison of rat mesenchymal stem cells derived from bone marrow, synovium, periosteum, adipose tissue, and muscle. Cell Tissue Res. 2007;327:449–462. doi: 10.1007/s00441-006-0308-z. [DOI] [PubMed] [Google Scholar]
- 27.in’t Anker PS, Scherjon SA, Kleijburg-van der Keur C, et al. Isolation of mesenchymal stem cells of fetal or maternal origin from human placenta. Stem Cells. 2004;22:1338–1445. doi: 10.1634/stemcells.2004-0058. [DOI] [PubMed] [Google Scholar]
- 28.Erices A, Conget P, Minguell JJ. Mesenchymal progenitor cells in human umbilical cord blood. Br J Haematol. 2000;109:235–242. doi: 10.1046/j.1365-2141.2000.01986.x. [DOI] [PubMed] [Google Scholar]
- 29.Engler AJ, Sen S, Sweeney HL, et al. Matrix elasticity directs stem cell lineage specification. Cell. 2006;126:677–689. doi: 10.1016/j.cell.2006.06.044. [DOI] [PubMed] [Google Scholar]
- 30.Kreke MR, Huckle WR, Goldstein AS. Fluid flow stimulates expression of osteopontin and bone sialoprotein by bone marrow stromal cells in a temporally dependent manner. Bone. 2005;36:1047–1055. doi: 10.1016/j.bone.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 31.Bhumiratana S, Grayson WL, Castaneda A, et al. Nucleation and growth of mineralized bone matrix on silk-hydroxyapatite composite scaffolds. Biomaterials. 2011;32:2812–2820. doi: 10.1016/j.biomaterials.2010.12.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cui L, Liu B, Liu G, et al. Repair of cranial bone defects with adipose derived stem cells and coral scaffold in a canine model. Biomaterials. 2007;28:5477–5486. doi: 10.1016/j.biomaterials.2007.08.042. [DOI] [PubMed] [Google Scholar]
- 33.Jukes JM, Both SK, Leusink A, et al. Endochondral bone tissue engineering using embryonic stem cells. Proc Natl Acad Sci U S A. 2008;105:6840–6845. doi: 10.1073/pnas.0711662105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu HH, Peng HJ, Wu Y, et al. The promotion of bone regeneration by nanofibrous hydroxyapatite/chitosan scaffolds by effects on integrin-BMP/Smad signaling pathway in BMSCs. Biomaterials. 2013;34:4404–4417. doi: 10.1016/j.biomaterials.2013.02.048. [DOI] [PubMed] [Google Scholar]
- 35.Yuan J, Cui L, Zhang WJ, et al. Repair of canine mandibular bone defects with bone marrow stromal cells and porous beta-tricalcium phosphate. Biomaterials. 2007;28:1005–1013. doi: 10.1016/j.biomaterials.2006.10.015. [DOI] [PubMed] [Google Scholar]
- 36.Kneser U, Polykandriotis E, Ohnolz J, et al. Engineering of vascularized transplantable bone tissues: Induction of axial vascularization in an osteoconductive matrix using an arteriovenous loop. Tissue Eng. 2006;12:1721–1731. doi: 10.1089/ten.2006.12.1721. [DOI] [PubMed] [Google Scholar]
- 37.Santos MI, Reis RL. Vascularization in Bone Tissue Engineering: Physiology, Current Strategies, Major Hurdles and Future Challenges. Macromol Biosci. 2010;10:12–27. doi: 10.1002/mabi.200900107. [DOI] [PubMed] [Google Scholar]
- 38.Tsigkou O, Pomerantseva I, Spencer JA, et al. Engineered vascularized bone grafts. Proc Natl Acad Sci U S A. 2010;107:3311–3316. doi: 10.1073/pnas.0905445107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang L, Fan HB, Zhang ZY, et al. Osteogenesis and angiogenesis of tissue-engineered bone constructed by prevascularized beta-tricalcium phosphate scaffold and mesenchymal stem cells. Biomaterials. 2010;31:9452–9461. doi: 10.1016/j.biomaterials.2010.08.036. [DOI] [PubMed] [Google Scholar]
- 40.Correia C, Grayson WL, Park M, et al. In Vitro Model of Vascularized Bone: Synergizing Vascular Development and Osteogenesis. PLoS One. 2011;6:9. doi: 10.1371/journal.pone.0028352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mueller MB, Tuan RS. Functional characterization of hypertrophy in chondrogenesis of human mesenchymal stem cells. Arthritis Rheum. 2008;58:1377–1388. doi: 10.1002/art.23370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Scotti C, Tonnarelli B, Papadimitropoulos A, et al. Recapitulation of endochondral bone formation using human adult mesenchymal stem cells as a paradigm for developmental engineering. Proc Natl Acad Sci U S A. 2010;107:7251–7256. doi: 10.1073/pnas.1000302107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Scotti C, Piccinini E, Takizawa H, et al. Engineering of a functional bone organ through endochondral ossification. Proc Natl Acad Sci U S A. 2013;110:3997–4002. doi: 10.1073/pnas.1220108110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Olsen BR, Reginato AM, Wang WF. Bone development. Annual Review of Cell and Developmental Biology. 2000;16:191–220. doi: 10.1146/annurev.cellbio.16.1.191. [DOI] [PubMed] [Google Scholar]
- 45.Cartmell SH, Porter BD, Garcia AJ, et al. Effects of medium perfusion rate on cell-seeded three-dimensional bone constructs in vitro. Tissue Eng. 2003;9:1197–1203. doi: 10.1089/10763270360728107. [DOI] [PubMed] [Google Scholar]
- 46.Grayson WL, Bhumiratana S, Cannizzaro C, et al. Effects of Initial Seeding Density and Fluid Perfusion Rate on Formation of Tissue-Engineered Bone. Tissue Eng Part A. 2008;14:1809–1820. doi: 10.1089/ten.tea.2007.0255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sikavitsas VI, Bancroft GN, Holtorf HL, et al. Mineralized matrix deposition by marrow stromal osteoblasts in 3D perfusion culture increases with increasing fluid shear forces. Proc Natl Acad Sci U S A. 2003;100:14683–14688. doi: 10.1073/pnas.2434367100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Grayson WL, Frohlich M, Yeager K, et al. Engineering anatomically shaped human bone grafts. Proc Natl Acad Sci U S A. 2010;107:3299–3304. doi: 10.1073/pnas.0905439106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Freed LE, Marquis JC, Nohria A, et al. Neocartilage formation in vitro and in vivo using cells cultured on synthetic biodegradable polymers. Journal of Biomedical Materials Research. 1993;27:11–23. doi: 10.1002/jbm.820270104. [DOI] [PubMed] [Google Scholar]
- 50.Vunjak-Novakovic G, Martin I, Obradovic B, et al. Bioreactor cultivation conditions modulate the composition and mechanical properties of tissue-engineered cartilage. Journal of Orthopaedic Research. 1999;17:130–1308. doi: 10.1002/jor.1100170119. [DOI] [PubMed] [Google Scholar]
- 51.Benya PD, Shaffer JD. Dedifferentiated chondrocytes reexpress the differentiated collagen phenotype when cultured in agarose gels. Cell. 1982;30:215–224. doi: 10.1016/0092-8674(82)90027-7. [DOI] [PubMed] [Google Scholar]
- 52.Mauck RL, Soltz MA, Wang CCB, et al. Functional tissue engineering of articular cartilage through dynamic loading of chondrocyte-seeded agarose gels. Journal of Biomechanical Engineering-Transactions of the Asme. 2000;122:252–260. doi: 10.1115/1.429656. [DOI] [PubMed] [Google Scholar]
- 53.Huang AH, Stein A, Tuan RS, et al. Transient Exposure to Transforming Growth Factor Beta 3 Improves the Mechanical Properties of Mesenchymal Stem Cell-Laden Cartilage Constructs in a Density-Dependent Manner. Tissue Engineering Part A. 2009;15:3461–3472. doi: 10.1089/ten.tea.2009.0198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sampat SR, Dermksian MV, Oungoulian SR, et al. Applied osmotic loading for promoting development of engineered cartilage. Journal of Biomechanics. 2013;46:2674–2681. doi: 10.1016/j.jbiomech.2013.07.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.O’Connell GD, Nims RJ, Green J, et al. Time and dose-dependent effects of chondroitinase ABC on growth of engineered cartilage. European Cells & Materials. 2014;27:312–320. doi: 10.22203/ecm.v027a22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Suh JKF, Matthew HWT. Application of chitosan-based polysaccharide biomaterials in cartilage tissue engineering: a review. Biomaterials. 2000;21:2589–2598. doi: 10.1016/s0142-9612(00)00126-5. [DOI] [PubMed] [Google Scholar]
- 57.Varghese S, Hwang NS, Canver AC, et al. Chondroitin sulfate based niches for chondrogenic differentiation of mesenchymal stem cells. Matrix Biology. 2008;27:12–21. doi: 10.1016/j.matbio.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 58.Kim IL, Mauck RL, Burdick JA. Hydrogel design for cartilage tissue engineering: A case study with hyaluronic acid. Biomaterials. 2011;32:8771–8782. doi: 10.1016/j.biomaterials.2011.08.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Moutos FT, Freed LE, Guilak F. A biomimetic three-dimensional woven composite scaffold for functional tissue engineering of cartilage. Nature Materials. 2007;6:162–167. doi: 10.1038/nmat1822. [DOI] [PubMed] [Google Scholar]
- 60.Bian L, Guvendiren M, Mauck RL, et al. Hydrogels that mimic developmentally relevant matrix and N-cadherin interactions enhance MSC chondrogenesis. Proc Natl Acad Sci U S A. 2013;110:10117–10122. doi: 10.1073/pnas.1214100110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Brunger JM, Huynh NPT, Guenther CM, et al. Scaffold-mediated lentiviral transduction for functional tissue engineering of cartilage. Proc Natl Acad Sci U S A. 2014;111:E798–E806. doi: 10.1073/pnas.1321744111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pacifici M, Koyama E, Shibukawa Y, et al. Cellular and molecular mechanisms of synovial joint and articular cartilage formation. In: Zaidi M, editor. Skeletal Development and Remodeling in Health, Disease, and Aging. Annals of the New York Academy of Sciences. 2006;1068:74–86. doi: 10.1196/annals.1346.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Johnstone B, Hering TM, Caplan AI, et al. In vitro chondrogenesis of bone marrow-derived mesenchymal progenitor cells. Experimental Cell Research. 1998;238:265–272. doi: 10.1006/excr.1997.3858. [DOI] [PubMed] [Google Scholar]
- 64.Sekiya I, Vuoristo JT, Larson BL, et al. In vitro cartilage formation by human adult stem cells from bone marrow stroma defines the sequence of cellular and molecular events during chondrogenesis. Proc Natl Acad Sci U S A. 2002;99:4397–4402. doi: 10.1073/pnas.052716199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Elder SH, Cooley AJ, Jr, Borazjani A, et al. Production of Hyaline-like Cartilage by Bone Marrow Mesenchymal Stem Cells in a Self-Assembly Model. Tissue Engineering Part A. 2009;15:3025–3036. doi: 10.1089/ten.TEA.2008.0617. [DOI] [PubMed] [Google Scholar]
- 66.Kandel RA, Boyle J, Gibson G, et al. In vitro formation of mineralized cartilagenous tissue by articular chondrocytes. In vitro cellular & developmental biology Animal. 1997;33:174–181. doi: 10.1007/s11626-997-0138-7. [DOI] [PubMed] [Google Scholar]
- 67.Lee WD, Hurtig MB, Kandel RA, et al. Membrane Culture of Bone Marrow Stromal Cells Yields Better Tissue Than Pellet Culture for Engineering Cartilage-Bone Substitute Biphasic Constructs in a Two-Step Process. Tissue Engineering Part C-Methods. 2011;17:939–948. doi: 10.1089/ten.TEC.2011.0147. [DOI] [PubMed] [Google Scholar]
- 68.Murdoch AD, Grady LM, Ablett MP, et al. Chondrogenic differentiation of human bone marrow stem cells in transwell cultures: Generation of Scaffold-free cartilage. Stem Cells. 2007;25:2786–2796. doi: 10.1634/stemcells.2007-0374. [DOI] [PubMed] [Google Scholar]
- 69.Ofek G, Revell CM, Hu JC, et al. Matrix Development in Self-Assembly of Articular Cartilage. Plos One. 2008;3:e2795. doi: 10.1371/journal.pone.0002795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Yu HS, Grynpas M, Kandel RA. Composition of cartilagenous tissue with mineralized and non-mineralized zones formed in vitro. Biomaterials. 1997;18:1425–1431. doi: 10.1016/s0142-9612(97)00071-9. [DOI] [PubMed] [Google Scholar]
- 71.Ratana S, Eton RE, Oungoulian SR, et al. Large, stratified, and mechanically functional human cartilage grown in vitro by mesenchymal condensation. Proc Natl Acad Sci U S A. 2014;111:6940–6945. doi: 10.1073/pnas.1324050111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Martin I, Miot S, Barbero A, et al. Osteochondral tissue engineering. Journal of Biomechanics. 2007;40:750–765. doi: 10.1016/j.jbiomech.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 73.Nooeaid P, Salih V, Beier JP, et al. Osteochondral tissue engineering: scaffolds, stem cells and applications. Journal of Cellular and Molecular Medicine. 2012;16:2247–2270. doi: 10.1111/j.1582-4934.2012.01571.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Schaefer D, Martin I, Jundt G, et al. Tissue-engineered composites for the repair of large osteochondral defects. Arthritis and Rheumatism. 2002;46:2524–2534. doi: 10.1002/art.10493. [DOI] [PubMed] [Google Scholar]
- 75.Wang YZ, Kim UJ, Blasioli DJ, et al. In vitro cartilage tissue engineering with 3D porous aqueous-derived silk scaffolds and mesenchymal stem cells. Biomaterials. 2005;26:7082–7094. doi: 10.1016/j.biomaterials.2005.05.022. [DOI] [PubMed] [Google Scholar]
- 76.Allan KS, Pilliar RM, Wang J, et al. Formation of biphasic constructs containing cartilage with a calcified zone interface. Tissue Engineering. 2007;13:167–177. doi: 10.1089/ten.2006.0081. [DOI] [PubMed] [Google Scholar]
- 77.Kandel RA, Grynpas M, Pilliar R, et al. Repair of osteochondral defects with biphasic cartilage-calcium polyphosphate constructs in a Sheep model. Biomaterials. 2006;27:4120–4131. doi: 10.1016/j.biomaterials.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 78.Tuli R, Nandi S, Li WJ, et al. Human mesenchymal progenitor cell-based tissue engineering of a single-unit osteochondral construct. Tissue Engineering. 2004;10:1169–1179. doi: 10.1089/ten.2004.10.1169. [DOI] [PubMed] [Google Scholar]
- 79.Khanarian NT, Haney NM, Burga RA, et al. A functional agarose-hydroxyapatite scaffold for osteochondral interface regeneration. Biomaterials. 2012;33:5247–5258. doi: 10.1016/j.biomaterials.2012.03.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kneser U, Polykandriotis E, Ohnolz J, et al. Engineering of vascularized transplantable bone tissues: Induction of axial vascularization in an osteoconductive matrix using an arteriovenous loop. Tissue Engineering. 2006;12:1721–1731. doi: 10.1089/ten.2006.12.1721. [DOI] [PubMed] [Google Scholar]
- 81.Tsigkou O, Pomerantseva I, Spencer JA, et al. Engineered vascularized bone grafts. Proc Natl Acad Sci U S A. 2010;107:3311–3316. doi: 10.1073/pnas.0905445107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wang L, Fan H, Zhang ZY, et al. Osteogenesis and angiogenesis of tissue-engineered bone constructed by prevascularized beta-tricalcium phosphate scaffold and mesenchymal stem cells. Biomaterials. 2010;31:9452–9461. doi: 10.1016/j.biomaterials.2010.08.036. [DOI] [PubMed] [Google Scholar]
- 83.Mueller MB, Fischer M, Zellner J, et al. Hypertrophy in Mesenchymal Stem Cell Chondrogenesis: Effect of TGF-beta Isoforms and Chondrogenic Conditioning. Cells Tissues Organs. 2010;192:158–166. doi: 10.1159/000313399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Dickhut A, Pelttari K, Janicki P, et al. Calcification or Dedifferentiation: Requirement to Lock Mesenchymal Stem Cells in a Desired Differentiation Stage. Journal of Cellular Physiology. 2009;219:219–226. doi: 10.1002/jcp.21673. [DOI] [PubMed] [Google Scholar]
- 85.Farrell MJ, Fisher MB, Huang AH, et al. Functional properties of bone marrow-derived MSC-based engineered cartilage are unstable with very long-term in vitro culture. Journal of Biomechanics. 2014;47:2173–2182. doi: 10.1016/j.jbiomech.2013.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Pelttari K, Winter A, Steck E, et al. Premature induction of hypertrophy during in vitro chondrogenesis of human mesenchymal stem cells correlates with calcification and vascular invasion after ectopic transplantation in SCID mice. Arthritis and Rheumatism. 2006;54:3254–3266. doi: 10.1002/art.22136. [DOI] [PubMed] [Google Scholar]
- 87.Johnson K, Zhu S, Tremblay MS, et al. A Stem Cell-Based Approach to Cartilage Repair. Science. 2012;336:717–721. doi: 10.1126/science.1215157. [DOI] [PubMed] [Google Scholar]
- 88.Yano F, Hojo H, Ohba S, et al. A novel disease-modifying osteoarthritis drug candidate targeting Runx1. Annals of the Rheumatic Diseases. 2013;72:748–53. doi: 10.1136/annrheumdis-2012-201745. [DOI] [PubMed] [Google Scholar]
- 89.Leijten J, Georgi N, Teixeira LM, et al. Metabolic programming of mesenchymal stromal cells by oxygen tension directs chondrogenic cell fate. Proc Natl Acad Sci U S A. 2014;111:13954–13959. doi: 10.1073/pnas.1410977111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ruan MZ, Erez A, Guse K, et al. Proteoglycan 4 Expression Protects Against the Development of Osteoarthritis. Science Translational Medicine. 2013;5:176ra34. doi: 10.1126/scitranslmed.3005409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Taniguchi N, Carames B, Kawakami Y, et al. Chromatin protein HMGB2 regulates articular cartilage surface maintenance via beta-catenin pathway. Proc Natl Acad Sci U S A. 2009;106:16817–16822. doi: 10.1073/pnas.0904414106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Alexander PG, Gottardi R, Lin H, et al. Three-dimensional osteogenic and chondrogenic systems to model osteochondral physiology and degenerative joint diseases. Experimental Biology and Medicine. 2014;239:1080–1095. doi: 10.1177/1535370214539232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Grayson WL, Bhumiratana S, Chao PHG, et al. Spatial regulation of human mesenchymal stem cell differentiation in engineered osteochondral constructs: effects of pre-differentiation, soluble factors and medium perfusion. Osteoarthritis and Cartilage. 2010;18:714–723. doi: 10.1016/j.joca.2010.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Liu XG, Jiang HK. Preparation of an osteochondral composite with mesenchymal stem cells as the single-cell source in a double-chamber bioreactor. Biotechnology Letters. 2013;35:1645–1553. doi: 10.1007/s10529-013-1248-9. [DOI] [PubMed] [Google Scholar]
- 95.Vunjak-Novakovic G, Meinel L, Altman G, et al. Bioreactor cultivation of osteochondral grafts. Orthodontics & craniofacial research. 2005;8:209–218. doi: 10.1111/j.1601-6343.2005.00334.x. [DOI] [PubMed] [Google Scholar]
- 96.Goldring MB, Tsuchimochi K, Ijiri K. The control of chondrogenesis. Journal of Cellular Biochemistry. 2006;97:33–44. doi: 10.1002/jcb.20652. [DOI] [PubMed] [Google Scholar]
- 97.Kusumbe AP, Ramasamy SK, Adams RH. Coupling of angiogenesis and osteogenesis by a specific vessel subtype in bone. Nature. 2014;507:323–328. doi: 10.1038/nature13145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Xie H, Cui Z, Wang L, et al. PDGF-BB secreted by preosteoclasts induces angiogenesis during coupling with osteogenesis. Nature Medicine. 2014;20:1270–1278. doi: 10.1038/nm.3668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Zaidi M. Skeletal remodeling in health and disease. Nature Medicine. 2007;13:791–801. doi: 10.1038/nm1593. [DOI] [PubMed] [Google Scholar]


