Abstract
Science and technology have always been the vitals of human’s struggle, utilized exclusively for the development of novel tools and products, ranging from micro- to nanosize. Nanotechnology has gained significant attention due to its extensive applications in biomedicine, particularly related to bio imaging and drug delivery. Various nanodevices and nanomaterials have been developed for the diagnosis and treatment of different diseases. Herein, we have described two primary aspects of the nanomedicine, i.e., in vivo imaging and drug delivery, highlighting the recent advancements and future explorations. Tremendous advancements in the nanotechnology tools for the imaging, particularly of the cancer cells, have recently been observed. Nanoparticles offer a suitable medium to carryout molecular level modifications including the site-specific imaging and targeting. Invention of radionuclides, quantum dots, magnetic nanoparticles, and carbon nanotubes and use of gold nanoparticles in biosensors have revolutionized the field of imaging, resulting in easy understanding of the pathophysiology of disease, improved ability to diagnose and enhanced therapeutic delivery. This high specificity and selectivity of the nanomedicine is important, and thus, the recent advancements in this field need to be understood for a better today and a more prosperous future.
Keywords: Nanotechnology, Nanocomposites, In vivo imaging, Drug delivery and pharmaceutical nanosystems
Review
Introduction
As a matter of fact, nanotechnology is making progress through all imperative fields of engineering and science, and scientists are revolutionizing all the industries and human lives by designing things capable of working on the smallest scale length, atom by atom [1]. Nanotechnology involves the study of eminently small structures. Nanotechnology can be defined comprehensively as the study, creation, design, synthesis, and implementation of functional materials, systems, and devices through controlling matter within the size range of 1–100 nm at the nanometer scale. Moreover, the manipulation of innovative phenomena and improved properties of matter at this nanometer scale, also referred as molecular nanotechnology, is a magical point on scale length where smallest man-made appliances encounter the molecules and atoms of the universe [2–4].
The early inception of the concept of nanotechnology and nanomedicine sprang from the discerning idea of Feynman that tiny nanorobots and related devices could be developed, fabricated, and introduced into the human body to repair cells at molecular level. Although later in the 1980s and 1990s, this innovative concept was advocated in the famous writings of Drexler [5, 6], and in 1990s and 2000s in the popular writings of Freitas [7, 8]. Feynman offered the first known proposal for a nanomedical procedure to cure heart disease. In general, miniaturization of medical tools will provide more accurate, controllable, reliable, versatile, cost-effective, and quick approaches for improved quality of human life [9]. In 2000, for the very first time, National Nanotechnology Initiative was launched; then from onwards, modeling of electronics and molecular structures of new materials, establishment of nanoscale photonic and electronic devices [10, 11], development of 3D networking, nanorobotics [12], and advent of multi-frequency force microscopy [13] have paved the way for emergence of molecular nanotechnology.
Nanoparticles are considered as the essential building blocks of nanotechnology. Presence of strong chemical bonds, extensive delocalization of valence electrons varying with size, and structural modifications in nanoparticles lead to different physical and chemical properties including melting points, optical properties, magnetic properties, specific heats, and surface reactivity. These ultrafine nanoparticles exhibit completely new and improved properties as compared to their bulk counterpart due to variation in specific characteristics such as size, distribution, and of the particles which give rise to larger surface area to volume ratio [14–16]. As the field of nanostructured materials has been evolved, many different labels and terminologies are being used including 3D nanoparticle, nanocrystals, nanofilms, nanotubes, nanowires, and quantum dots with promising potential of infinite number of properties [17]. Because of the variety of potential applications (including industrial and military), governments have invested billions of dollars in nanotechnology research. The USA has invested 3.7 billion dollars through its National Nanotechnology Initiative, and European Union has also subsidized 1.2 billion, and 750 million dollars were invested by Japan [18].
Today, nanotechnology is one of the most innovative, vanguard areas of scientific study, and it continues to progress at staggering rates [19]. Through advancement in nanotechnology, many state-of-the-art technologies became available for the drug delivery. Researchers have extensively investigated the potential of nanodevices for target specific and controlled delivery of various micro- and macromolecules including drugs, proteins, monoclonal antibodies, and DNA (deoxyribonucleic acid) in multifarious biomedical applications like cancer [20, 21], vaccination [22], dental [23], inflammatory [24], and other health disorders. It is therefore a need of the day to demonstrate efficient use of nanotechnology applications ranging from in-vivo imaging system to controlled drug delivery, to mark the current progress and get directions for impending research in medical fields.
Pharmaceutical Nanosystems
Pharmaceutical nanotechnology can be classified into two main categories of nanotools, i.e., nanomaterials and nanodevices. Nanomaterials can be further categorized on the basis of three basic parameters including structure, dimension, and phase composition. Nanostructures are further classified into polymeric and non-polymeric structures including nanoparticles, micelles, dendrimers, drug conjugates, metallic nanoparticles, and quantum dots [25]. On the basis of their dimensions, nanomaterials are classified in four groups, i.e., zero, one, two, and three nanodimension materials. According to phase composition, these nanomaterials can be categorized in three groups. Nanodevices are subdivided in three groups, including microelectromechanical systems/nanoelectromechanical system (MEMS/NEMS), microarrays, and respirocytes. These structures and devices can be fabricated with a high degree of functional property for use in medicine to interact with cells at a molecular level, thus allowing an extent of integration between biological systems and latest technology that was not achievable previously [26]. Detailed classification of pharmaceutical nanotools is described with their examples in Table 1.
Table 1.
Pharmaceutical nanosystems (classification of nanotools)
| Classification | Sub types | Examples | Structures | Applications | References | ||
|---|---|---|---|---|---|---|---|
| Pharmaceutical nanosystems | Nanomaterials | On basis of structure | Polymeric | Drug conjugates |

|
• Deliver cytotoxic agents • Provide controlled release • Increase potency, tolerability and activity of drugs |
[130] |
| Micelles |

|
• Amphiphilic block copolymers • Extremely small structure • Increase aqueous solubility of drugs |
[131] | ||||
| Dendrimers |
|
• Photodynamic therapy, boron neutron capture therapy • Potent anticancer agents |
[132, 133] | ||||
| Nonpolymeric | Quantum dots |
|
• Luminescent nanoprobes • Improved efficacy and bioavailability • Reduced side effects |
[134] | |||
| Carbon nanotubes |

|
• Increase drug solubility and stability • Targeted drug delivery • Combination therapy |
[135] | ||||
| Metallic nanoparticles |

|
• Contrast agents • Provide controlled, targeted delivery |
[136] | ||||
| Silica nanoparticles |

|
• Improved pharmacokinetic profile • Enhanced bioavailability • Cornell dots |
[137] | ||||
| Dimension wise | Zero-nanodimension | Spheres, clusters (fullerene) |

|
• Production of nanoparticles • Functionalization of nanoparticles by dendritic structures |
[138] | ||
| One-nanodimension | Fibers, wires, rods |
|
• Increase stability • Use in nanodevices, fibrils of nanodimensions, fabrication of polymer nanocomposites |
[139, 140] | |||
| Two-nanodimension | Films, plates, networks |

|
• Used in sensing, electronics and optoelectronics | [141] | |||
| Three-nanodimension | Tri and tetra pods, nanocombs |

|
• Used in separation, catalytic, biomedical and heat transfer | [142] | |||
| Phase composition wise | Single phase solids | Amorphous particles and layers |

|
• Increase drug solubility • Increase the shelf life of drugs |
[143] | ||
| Multi-phase solids | Matrix composites |

|
• Long term, repeated, on demand delivery of drugs for pain, chemotherapy, and insulin | [144] | |||
| Multi-phase system | Colloids, ferro fluids |
|
• Diagnosis and drug targeting • Deliver vaccines, toxoids, anticancer, gene and anti HIV drugs |
[145] | |||
| Nanodevices | NEMS/MEMS |
|
• Microscopic devices with length more than 100 nm but less than 1 mm, possess combined electrical and mechanical components • Used for optical activities, electronic or biological applications and micro machines |
[146] | |||
| Microarrays |
|
• Mapping of biological pathways, analysis of bio molecular interactions, assay development for compound screening, delivery of protein and peptides | [147] | ||||
| Respirocytes |
|
• Artificial nanospherical robotic erythrocytes with internal pressure 1000 atm of combined oxygen and carbon dioxide • Preserve living tissues, treat anemia, asphyxia, and other respiratory problems |
[148] | ||||
Manufacturing Approaches
Nanosizing technologies have achieved great importance for the formulation of poorly water soluble drugs. By reducing the particle size to nanoscale range, the dissolution rate and bioavailability increase because of the increase in surface area, according to the Noyes-Whitney equation [27]. Approaches used for the manufacturing materials are categorized into bottom up techniques, top down techniques, and the combination of bottom up and top down techniques. Bottom up techniques involve built up of molecules. Some of the techniques that follow bottom up approach for manufacturing of nanoscale materials include liquid phase techniques based on inverse micelles, chemical vapor deposition (CVD), sol-gel processing, and molecular self-assembly. The components produced by bottom up are significantly stronger than the macroscale components because of the covalent forces that hold them together. In top down techniques, materials are micronized by cutting, carving, and molding for manufacturing of nanomaterials. Examples include milling, physical vapor deposition, hydrodermal technique electroplating, and nanolithography [28]. Different manufacturing approaches with their respective types are described in Table 2.
Table 2.
Different approaches for manufacturing of various nanomaterials with their respective types
| Approach | Subtypes | Principle | Example of drug | Nanostructure/nanodevice | References |
|---|---|---|---|---|---|
| Nanoprecipitation-dependent techniques | Anti-solvent precipitation | Supersaturation in which dissolution of a lipophilic drug in organic solvent followed by in anti-solvent (water). It leads to the nucleation of drug followed by precipitation of particles. |
Itraconazole | Amorphous nanoparticles (<250 nm) | [149] [150] |
| Curcumin | Nanoparticles | [151] | |||
| Flash nanoprecipitation | Dissolution of a hydrophobic drug and amphiphilic copolymers in a water miscible organic solvent. Then, the organic solvent is mixed with an anti-solvent (water). High supersaturation level is achieved that triggers nanoprecipitaion. | Curcumin | Nanoparticles (40 nm) | [152] | |
| AIE (aggregation-induced emission) active dye of EDP | Fluorescent nanoparticles (20–60 nm) | [153] | |||
| Doxorubicin | Nanoparticles (<100 nm) | [154] | |||
| Sono precipitation | Crystallization by ultrasonic waves | Fenofibrate | Nanocrystals | [155] | |
| Felodipine | Nanosuspension | [156]. | |||
| Herceptin (HCT)-functionalized paclitaxel | Nanocrystals | [157] | |||
| Lovastatin | Rod shaped nanocrystals | [158] | |||
| High gravity controlled precipitation | High gravity conditions are maintained for precipitation by passing solution across rotating bed packing. | Hydroxyapatite (nHAP) | Nanoparticles (1.9–14.2 nm) | [159] | |
| Milling-dependent techniques | Wet milling technique | Attrition is involved in which microsized particles are commuted by milling beads in a milling chamber to obtain nanosized particles (usually smaller than 400 nm). | Griseofulvin and Indomethacin | Nanoparticles (<100 nm) | [160] |
| Itraconazole adipic acid | Nanocrystals | [161] | |||
| Repaglinide | Nanocrystals | [162] | |||
| Salt-assisted milling | Milling along with salts like NaCl with steel balls to produce nanosized particles. NaCl is incorporated in milling medium to prevent degradation and aggregation of nanoparticles [28]. |
Nanodiamond aggregates (50–1000 nm) | Nanodiamond colloids (5–10 nm) | [163] | |
| Co-grinding | Grinding of APIs with specific additives to produce nanosized particles [164]. |
Ibuprofen–glucosamine HCl | Co-ground particles | [165] | |
| Piroxicam | Cryogenic co-ground solid dispersions | [166] | |||
| High-pressure homogenization | Milling of suspended drug particles under high pressure by using homogenizer. | Myricetin | Nanosuspension | [167] | |
| α-chitin | Nanofibers (<100 nm) | [168] | |||
| Spraying-dependent techniques | Spray drying | Dispersion or liquids are transformed into solid powdered form upon spraying into drying medium at high temperature [169]. | Cyclosporine A | Nanoparticles (317 to 681 nm) | [170] |
| Electrospraying | Strong electric field is applied to atomize a liquid into fine dispersed particles at normal pressure and ambient temperature and without use of surfactants. | Piroxicam | Nanospheres | [171] | |
| Supercritical fluid technology | RESS (Rapid expansion in supercritical solution) | Drug is solubilized in a supercritical fluid and the solution is then expanded in a low-pressure area through a nozzle. The drug becomes insoluble in low pressure gas and then supersaturation occurs and this leads to the production of micro and nanosized particles. |
Olanzapine | Nanoparticles (150–350 nm) | [172] |
| RESS-SC (Rapid expansion of supercritical solution with solid co-solvent) | In this technique, supercritical fluid, i.e., CO2, is saturated with several solid co solvents [173]. | Theophylline | Nanoparticles (mean size: 85 nm) | [173] | |
| SAS (supercritical anti-solvent) | In this technique, precipitation of drug occurs upon its dissolution in an organic solvent, due to antisolvent effect. | Polyvinylpyrrolidone (PVP)–folic acid (FA) | Microspheres | [174] | |
| BSA (bovine serum albumin) | Nanoparticles (60 nm ± 10 nm) | [174] | |||
| SAA (supercritical-assisted atomization) | The organic solution and supercritical carbon dioxide (SC-CO2) are mixed; they form an expanded liquid in a saturator. It is then atomized under some specific conditions results in the formation of nanodroplets which produce NPs by drying [175]. |
Rifampicin | PLLA nanoparticles (123 to 148 nm) | [176] | |
| Gentamycin sulfate | Microparticles (<2 μm) | [177] |
Biomedical Applications of Advanced Nanotechnology
Imaging
Tremendous advancements were reported during the last decade, using the nanotechnology tools for the imaging and therapy in research particularly targeting the cancer cells. Nanoparticles, with size 10–100 nm, offer a very suitable medium to carry out molecular level modifications such as the site-specific imaging and targeting in cancer cells [29]. The following section summarizes some recent advancement in the imaging techniques.
Radionuclide Imaging
Because of the inability of small molecules to be viewed with the noninvasive technique, the site-targeted contrast agents are employed to identify a selected biomarker that is impossible to be separated from the normal surrounding tissues [30]. The radionuclide imaging has been developed with the concept that the expressed protein is probed with a radiopharmaceutical or isotope-labeled agent or cell and is tracked further in vivo [31]. The positron emission tomography (PET) imaging is used in the cancer patients successfully to image the multidrug resistance through P-glycoprotein transport using 99 m tetrofosmin and sestamibi as the radiolabeled substrates for the P-glycoprotein [32, 33]. The mechanism of imaging is determined by the type of modality used for the imaging such as nanocarriers including liposomes [34], dendrimers [35], Bucky balls [36], and numerous polymers and copolymers [37]. They can be filled with the large number of imaging particles such as optically active compounds and radionuclides for the detection with imaging equipment. The BODIPY (boron dipyrromethane)-labeled jasplakinolide analogs have been used to visualize the long lived actin filaments inside the living cells [38, 39].
The enormous growth of nanotechnology is leading the research in the molecular imaging with many contrast agents. To obtain an appropriate imaging, the contrast agent selected should have longer half-life, low background signal, specific epitope binding, and enhanced contrast to noise enhancement. Large number of carrier availability is able to define more advancements in imaging with particular focus on the molecular and cellular mechanisms of the disease; this will create more opportunities for the rational development of imaging and drug delivery systems [30].
Quantum Dots
Semiconductor quantum dots are now used as a new class of fluorescent labels. These semiconductor nanocrystals are a promising tool for visualization of the biological cells owing to their easy surface chemistry, allowing biocompatibility and hereto conjugation with elongation of fluorescence time [29, 40]. The visualization properties of quantum dots (fluorescence wavelength) are strongly size dependent. The optical properties of quantum dots depend upon their structure as they are composed of an outer shell and a metallic core. For instance, grapheme quantum dots (GQD), a type of green fluorescence carbon nanomaterials, are made by cutting grapheme oxide solvothermally and are found to be dominating the visualization properties [41].
Quantum dot core is usually made up of cadmium selenide, cadmium sulfide, or cadmium telluride. The outer shell is fabricated on the core with high band gap energy in order to provide electrical insulation with preservation of fluorescence properties of quantum dots. The fine-tuned core and shells with different sizes and compositions with visualization properties of specific wavelength provide a large number of biomarkers [40]. Quantum dots are conjugated with different ligands in order to obtain specific binding to biological receptors. The tumor-targeting ligands are linked with amphiphilic polymer quantum dots and used to carry out the imaging studies of prostate cancer in mice [42]. Similarly, quantum dots offer significant advantages over the conventional dyes such as narrow bandwidth emission, higher photo stability, and extended absorption spectrum for the single excitation source. Moreover, the challenge of hydrophobicity in quantum dots has been overcome by making them water soluble. An example of the aqueous quantum dots with long retention time in biological fluids is the development of highly fluorescent metal sulfide (MS) quantum dots fabricated with thiol-containing charged groups [43]. Furthermore, the unique fluorescence properties of quantum dots made them suitable imaging tools for the cancer cells [42]. Quantum dots linked with A10 RNA aptamer conjugated with doxorubicin (QD-Apt-Dox) is the example of targeted cancer cell imaging [44]. However, increased toxicity of quantum dots has been observed due to the incorporation of heavy metals, resulting in their limited use for the in vivo imaging. Nevertheless, recent approaches focus on the reduction in toxicity and the enhancement of biocompatibility of quantum dots to the body cells. It is also worth to mention that quantum dots with the diameter less than 5.5 nm are rapidly and efficiently excreted from the urine resulting in reduced toxicity. This phenomenon was exhibited by the synthesis of cadmium free, CulnS2/ZnS (copper indium sulfide/ zinc sulfide) as the core and shell of the quantum dots, which resulted in enhanced stability in the living cells for lymph node imaging with a clear reduction in acute local toxicity [45, 46].
Biosensors
One of the greatest achievements in nanomaterials since last few years is the development of biosensors. Biosensors are the devices that contain the biological sensing element that is either connected or integrated in the transducer. Biosensor exhibits their action by recognition of specific molecules in the body on the basis of their structure including antibody antigen, enzyme substrate, and receptor hormone. The two major properties of biosensor including their specificity and selectivity are dependent upon this recognition system. These basic properties of the biosensors are most importantly used for the concentration that is proportional to the signals [47–49].
In order to produce the biosensor with high efficiency, the substrate selected for the sensing material dispersion is prerequisite. Different types of nanomaterial including quantum dots [50], magnetic nanoparticles [51], carbon nanotubes (CNTs) [52], and gold nanoparticles (GNPs) [53] are applied to the biosensors. The distinctive chemical, physical, magnetic, optical, and mechanical properties of nanomaterial lead to their increased specificity and sensitivity for detection. Biosensors containing GNPs have offered a compatible environment for the biomolecules that has increased the immobilized biomolecules concentration on the surface of electrode. It has resulted in enhanced sensitivity of the biosensors [54, 55]. The most widely used electrode surfaces within the biosensors are the glassy carbon electrode (GCE), which are modified from GNPs. Moreover, they have shown best sensitivity as well as electrochemical stability. In this regards, methylene blue (MB) and GNPs are easily assembled and modified through layer by layer (LBL) technique in the form of films on GCE, in order to detect the concentration of human chorionic gonadotrophin (HCG) [56]. Owing to the large surface area contained by the nanoparticles in order to load anti-HCG, these immunosensors have their potential to be used for detecting the concentrations of HCG in the human blood or urine samples. Similarly, CNTs have found great applications in biomedical engineering, bio-analysis, bio-sensing, and nanoelectronics [57–59]. Moreover, multi-walled carbon nanotubes (MWNT) in the form of bio-nanocomposite layers of polymers have the potential to be used for the DNA detection [60]. Furthermore, magnetic nanoparticles have also found wide applications because of their magnetic properties, including magnetic resonance imaging (MRI) contrast agent [61], hyperthermia [62], immunoassay [63], tissue repair [64], cell separation [65], GMR-sensor [66], and drug or gene delivery [67].
Likewise, a new type of magnetic chitosan microspheres (MCMS) has also been produced by simply using chitosan and carbon-coated magnetic nanoparticles [68]. In this study, hemoglobin was also immobilized successfully on the MCMS modified GCE surface by using glutaraldehyde as the crosslinking agent. Another important application of biosensors is in the optical technology, which includes the detection of various kinds of DNA oligonucleotides by using SsDNA–CNT probes as the biosensors [69]. Similarly, liposome-based biosensors have also gained considerable attention as they have been used in the monitoring of the organophosphorus pesticides, including paraoxon and dichlorvos on the minimum levels [70].
Magnetic Nanoparticles
Magnetic nanoparticles (MNPs) provide exclusive magnetic properties as they have the ability to work at the molecular or cellular level of the biological interactions, which make them the best compounds as contrast agents in MRI and as carriers in drug delivery. The recent advancements in nanotechnology have gained attention as it helped in the modification of the properties and features of MNPs for the biomedical applications. In this respect, the liver tumor and metastasis imaging via RES-mediated uptake of superparamagnetic iron oxides (SPIOs) has been shown to be capable of the differentiation of the lesions that are as small as only 2–3 mm [70, 71]. Moreover, these ultra-small supermagnetic iron oxides (USPIOs) are also very effective in the imaging of the metastasis of the lymph nodes with only 5 to 10 mm of diameter [72]. Furthermore, importance of this noninvasive approach has also been shown in the detection of the lymphatic dissemination as it is considered an important part in the staging as well as in identifying the treatment approaches for the breast colon and prostate cancers [73].
Drug Delivery
Nanotechnology is an attractive tool for disciplines ranging from materials science to biomedicine because of their different physical, optical, and electronic characteristics. The most effective research areas of nanotechnology are nanomedicine that applies nanotechnology principles for the treatment, prevention, and diagnosis of diseases. Moreover, many products of nanomedicine have been marketed due to the surge in nanomedicine research during the past few decades, around the globe. Currently, nanomedicine is influenced by drug delivery systems, accounting for more than 75% of the total sales [74]. In this regards, nanoparticle-based drug delivery platforms have gain the trust of scientists for being the most appropriate vehicles in addressing the pharmacokinetic drawbacks associated with conventional drug formulations [75]. Hence, various nanoforms have been attempted as drug delivery systems such as liposomes, solid lipid nanoparticles, dendrimers, and solid metal-containing NPs, to enhance the therapeutic efficacy of drugs [76, 77]. Some of the major fields of interest are discussed below.
Ophthalmology
Drug delivery through the ophthalmic route is highly attractive yet challenging for the pharmaceutical scientists. The eye is a tiny intricate organ with multi-compartments. Its biochemistry, physiology, and anatomy have made it most impermeable to the xenobiotic. Common conditions that demand ocular administration contain the eye infections such as, conjunctivitis along with the corneal disorders like glaucoma. The most common drug classes used in the ocular delivery include mydriatics or cycloplegics miotics, anti-infective, anti-inflammatory, diagnostics, and surgical adjuvants. For the small ocular irregularity, gene therapy is required too, and a large amount of work is being conducted within this area. Nanocarrier supported approaches have got attention of the scientists for their suitability and specificity. It has been reported that particulate delivery system such as microspheres and nanoparticles and vesicular carriers like liposomes, niosomes, pharmacosomes, and discomes improved the pharmacokinetic and pharmacodynamics properties of various types of drug molecules [76]. Many novel controlled drug delivery systems have been emerged including hydrogels, muco-adhesive polymers, microemulsions, dendrimers, iontophoretic drug delivery, siRNA-based approaches, stem cells technology, non-viral gene therapy, and laser therapy with the sclera plugs [78]. Different systems for drug delivery are costumed for the delivery of drug through the ocular route. The chief goal of all the drug delivery systems is to improve the residence period, enhance the corneal permeability, and liberate the drug at posterior chamber of eye, leading to increased bioavailability and improved patient compliance [79].
Abrego et al. prepared PLGA (poly lactic co-glycolic acid) nanoparticles of pranoprofen for ophthalmic delivery in the form of hydrogel. This hydrogel formulation have suitable rheological and physicochemical properties for the ocular delivery of pranoprofen with improved biopharmaceutical outline of the drug. Moreover, it intensified the local anti-inflammatory and analgesic results of the drug, resulting in improved patient’s compliance [80]. In another study, cefuroxim loaded nanoparticles of chitosan were developed using a double crosslinking in double emulsion technique. The inference point out chitosan-gelatin particles as potently practical candidates for DD at intraocular level [81]. Moreover, diclofenac loaded N-trimethyl chitosan nanoparticles (DC-TMCNs) were developed for ophthalmic use to improve ocular bioavailability of the drug [82]. Furthermore, nanosized supramolecular assemblies of chitosan-based dexamethasone phosphate have been developed for improved pre-corneal drug residence time due to its muco-adhesive characteristics. These nanoparticles interact strongly with both ocular surface and drug and protect the drug from metabolic degradation leading to extended pre-corneal residence [83]. Glaucoma, an ophthalmic disease, was treated with brimonidine-based loaded sustained release solid lipid nanoparticles using glyceryl monostearate as solid lipid [84, 85]. Similarly, daptomycin-loaded chitosan-coated alginate (CS-ALG) nanoparticles were developed with a suitable size for ocular applications and high encapsulation efficiency (up to 92%). This study revealed that daptomycin nanocarrier system could be used in future to deliver this antibiotic directly into the eye, in order to act as a prospective therapy against bacterial endophthalmitis and as an efficient alternative to chitosan nanoparticles [86].
One of the major causes of short- and long-term failure of grafts in the corneal transplantation is the immunologic graft rejection. For this purpose, PLGA-based biodegradable nanoparticle system of dexamethasone sodium phosphate (DSP) was prepared, resulting in the sustained release of the corticosteroids in order to prevent the rejection of corneal graft [87]. Moreover, MePEG-PCL (polyethylene glycol-poly caprolactone) nanoparticles of curcumin were reported, and they showed increased efficiency, enhanced retention of curcumin in the cornea, and significant improvement in prevention of the corneal neovascularization over free curcumin [88]. Likewise, silver nanoparticle-infused tissue adhesive (2-octyl cyanoacrylate) were developed with enhanced mechanical strength and antibacterial efficacy. These doped adhesive (silver nanoparticles) supported the use of tissue adhesives as a viable supplement or alternative to sutures [89].
Pulmonology
Lung diseases probably asthma, chronic obstructive pulmonary disease (COPD), and lung cancer have a high occurrence and are often life threatening. For instance, it is described that COPD is the fourth major cause of death, and lung carcinoma is the most prevailing cause of cancer deaths worldwide. Nanoparticles are scrutinized as a choice to improve therapy of these severe diseases [90]. Various drug-laden nanoparticles have been utilized for their local and systemic effects in the treatment of lung diseases. Delivery of curative agents to the place of action for lung diseases may permit for effective treatment of chronic lung infections, lung cancers, tuberculosis, and other respiratory pathologies [91]. The nanocarriers used for this purpose include liposomes, lipid- or polymer-based micelles, dendrimers, and polymeric NPs [92]. Polymeric NPs are of prenominal interest, as the polymers can be co-polymerized, surface modified, or bio-conjugated for ameliorate targeting capacity and distribution of the encapsulated agents. The generally used nanocarriers in pulmonary drug delivery contain natural polymers such as gelatin, chitosan, and alginate and synthetic polymers like poloxamer, PLGA, and PEG [93].
It was observed that PLGA NPs exhibit the most convenient set of characteristics as carriers for pulmonary protein/DNA delivery while gelatin NPs are an agreeable reciprocal choice [94]. Similarly, anisotropic or Janus particles of doxorubicin and curcumin were formulated to cargo the anticancer drugs for the treatment of lung cancer through inhalation. The particles were formulated by using the biocompatible and biodegradable materials binary mixtures. These particles did not exhibit geno- and cytotoxic consequence. The cancer cells internalize these Janus particles and massed them in the nucleus and cytoplasm leading to prolonged retention. Moreover, polyamidoamine (PAMAM) dendrimers were evaluated as nanocarriers for pulmonary delivery of the model weakly soluble anti-asthma pharmaceutical beclometasone dipropionate (BDP) using G3, G4 and G4 [12] dendrimers. This study showed that BDP-dendrimers have potential for pulmonary inhalation using air-jet and vibrating-mesh nebulizers. Furthermore, it was observed that the aerosol characteristics were influenced by nebulizer design rather than dendrimers generation [95]. Additionally, engineered nanoparticles (ENP), composed of inorganic metals, metal oxides, metalloids, organic biodegradable, and inorganic biocompatible polymers were used efficiently as carriers for the vaccine and drug delivery and for the management of a variety of lung diseases. Properties and efficacious effects of ENPs on lungs are represented in Fig. 1. Inorganic ENP (silver, gold, and carbon ENP), metal oxides ENP (iron oxide, zinc oxides, and titanium dioxide), and organic ENP (Lipid-based, polysaccharide-based, polymer matrix-based) were developed and evaluated for pulmonary immune hemostasis. As well as being relatively secure carriers, modern studies indicated ENP cable of supervening beneficial outcomes with anti-inflammatory properties (e.g., silver and polystyrene) and imprinting of the lung which present the maintenance of immune homeostasis (e.g., polystyrene). Further knowing of the mechanisms may help in better understanding the useful effects of ENP on pulmonary immune homeostasis and/or management of inflammatory lung disease [96].
Fig. 1.
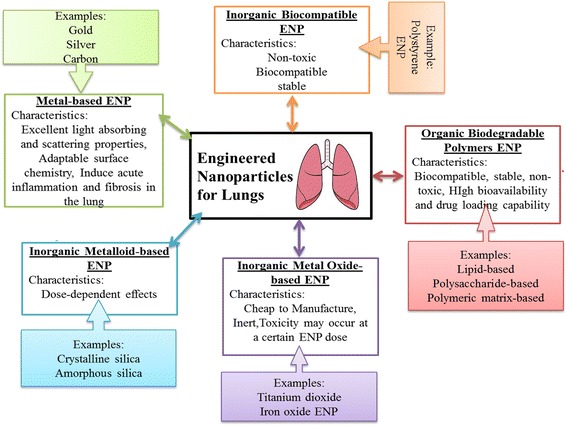
Properties and efficacious effects of ENPs on lungs
It is important to state that functionalized cationic lipo-polyamine (Star: Star-mPEG-550) have been recently developed for the siRNA (short interference RNA) in vivo delivery to the pulmonary vascular cells. This balanced lipid formulation intensify the siRNA retention in the lungs of mouse and accomplished significant disassemble of the target gene. The results were found useful and with reduced toxicity of miRNA-145 inhibitor delivery to the lung by using the functionalized cationic lipopolyamine nanoparticles to recruit the pulmonary arteriopathy and rectify function of heart within rats with intense pulmonary arterial hypertension (PAH) [97].
Cardiovascular System
Cardiovascular disease is the ailment that affects the cardiovascular system, vascular diseases of the brain and kidney, and peripheral arterial disorder. Despite of all advances in pharmacological and clinical management, heart failure is a foremost reason of morbidity worldwide. Many novel therapeutic strategies, embody cell transplantation, gene delivery or therapy, and cytokines or other small molecules, have been studied to treat heart failure [98]. An inadequate number of people are affected in developing countries; over 80% of deaths due to cardiovascular disorder take place in underdeveloped countries and occur almost evenly in male and females [99]. Mathers et al. in 2008 estimated that there are 9.4 million deaths each year [100]. This concludes 45% of deaths caused by coronary heart disease and 51% of deaths due to heart strokes [101]. There are many distinct types of drug delivery vehicles, like polymeric micelles, liposomes, dendrimers, lipoprotein-supported pharmaceutical carriers, and nanoparticle drug carriers.
Chitosan-based liposomes of sirolimus having ≥83% entrapment efficiency were developed for the treatment of restenosis and have been proved a novel platform for efficient targeted delivery [102]. Similarly, bile salt-enriched niosomes of carvedilol with 85% entrapment efficiency have resulted in enhanced bioavailability of drug, and thus, better therapeutic effect [103] was obtained. Inhibition of restenosis in balloon-injured carotid artery is achieved in rats by developing PLGA-based nanoparticles encapsulating AGL 2043 and AG1295, selective blockers of platelet-derived growth factors (PDGF) receptors [104]. Angiogenic therapy of myocardial ischemia with vascular endothelial growth factor (VEGF) is a favorable approach to overcome hypoxia and its sequel effects. Polymeric particles loaded with VEGF have been proved a promising system for delivery of cytokines to rat myocardial ischemic model. This approach could be further explored for clinical studies [105]. Coenzyme Q10 (CoQ10) owing to its role in mitochondrial electron transport chain appears to be a reliable candidate to treat myocardial ischemia (MI) but its poor biopharmaceutical characteristics needed to be addressed by developing promising delivery approaches. Polymeric nanoparticles were developed to encapsulate CoQ10 to overcome its poor pharmaceutical properties and administered to MI-induced rats. Cardiac function was analyzed by determining ejection fraction before and after 3 months of therapy. Results showed significant betterment in the ejection fraction after 3 months [106].
Oncology
Cancer is a prime cause of mortality around the globe. The World Health Organization determines that 84 million people die of cancer between 2005 and 2015. The eventual target of cancer therapeutics is to increase the life span and the quality of life of the patient by minimizing the systemic toxicity of chemotherapy [107]. Chemotherapeutic agents have widely been studied in oncology for the past 25 years, but their tumor specificity is unsatisfactory and therefore exhibit dose-dependent toxicity. To overcome this limitation, recent interest has been centered on developing nanoscale delivery carriers that can be targeted directly to the cancer cell, deliver the drug at a controlled rate, and optimize the therapeutic efficacy [108, 109]. Passive and active targeting is used to deliver the drug at its tumor site. The passive phenomenon called the “enhanced permeability and retention (EPR) effect,” discovered by Matsumura and Maeda, is the dominated pathway used for chemotherapeutics [110, 111]. Active targeting is achieved by grafting ligand at the surface of nanocarriers that bind to receptors or stimuli-based carriers, e.g., dual reverse thermosensitive [112], photo-responsive [113], magnetic nanoparticles [114], and enzymatically activated pro-drugs [115]. Nanoparticles (NPs) can be conjugated with various smart therapeutic carriers like polymeric nanoparticles [116], micelles [117], liposomes [118], solid lipid nanoparticles (SLNs) [119], protein nanoparticles [120], viral nanoparticles [121], metallic nanoparticles [122], aptamers [123], dendrimers [124], and monoclonal antibody [125] to improve their efficacy and decrease the systemic toxicity. Table 3 summarizes the different approaches for drug deliveries which are widely studied to target the tumor with maximize therapeutic response and minimum toxicity.
Table 3.
Nanomaterials and drug delivery approaches for tumor treatment
| Nanomaterials | Delivery approaches | Advantages | References |
|---|---|---|---|
| Aptamer functionalized silica gold nanorods (60 nm) | Near-infrared light responsive drug delivery system | Biocompatibility, cancer cell recognition ability, and efficient intracellular drug release | [178] |
| Doxorubicin-loaded PEG diacrylate -Chitosan derivative-single-wall carbon nanotubes (CNT) (240 nm) | Near-infrared (NIR) light triggered drug delivery system | Enhanced cellular uptake and the faster drug release | [179] |
| (DOX)-loaded hollow mesoporous copper sulfide nanoparticles (HMCuS NPs) with iron oxide nanoparticles (IONPs) (124.5 ± 3.8 nm) |
Near-infrared (NIR) light triggered drug delivery system | Minimized the adverse effects, enhanced photo thermal therapy effect |
[180] |
| DOX-(HMCuSNPs) with hyaluronic acid (HA) (113.8 ± 6.9 nm) |
Near infrared (NIR) light triggered drug delivery system | Facilitate intracellular tunable drug release, enhanced targeting and accumulation capacity in tumor site | [181] |
| α-Cyclodextrin and poly (ethylene glycol)-platinum dendrimer (1.9 ± 0.3 nm) |
Near infrared (NIR) light-responsive supramolecular hydrogel | Enhanced release of drug, low toxicity | [182] |
| End-capped mesoporous silica nanoparticles (MSNs) (130 nm) |
Redox-responsive nanoreservoirs | Excellent biocompatibility, cell-specific intracellular drug delivery, and cellular uptake properties | [183] |
| Transferrin (Tf)-(MSNs)-DOX (280 nm) |
Redox-responsive drug delivery system | Biocompatible, enhanced intracellular accumulation, targeting capability | [184] |
| Amino- β –cyclodextrin- MSNs (203.3 nm) |
Folate mediated and pH targeting | High intercellular release | [185] |
| DOX-thiolated poly(ethylene glycol)-biotin-DNA conjugated gold nanorod (GNR) (length of 50 ± 5 nm diameter of 14 ± 3 nm) |
pH-and near infrared (NIR) radiation dual-stimuli triggered drug delivery | Increased potency (~67-fold), increased cell uptake, low drug efflux | [186] |
| Cytochrome C conjugated lactobionic acid (CytC–LA)- Doxorubicin (DOX)- MSNs (115.8 nm) |
pH and redox dual-responsive drug delivery | Good biocompatibility, high efficiency, inhibits tumor growth with minimal toxic side effect. | [187] |
| Poly (propylene sulfide)-polyethylene glycol-serine-folic acid (PPS-mPEG-Ser-FA)- zinc phthalocyanine-doxurubicin micelle (80 nm) |
Reactive oxygen species (ROS) sensitive drug delivery system | Minimal toxic side effects | [188] |
| Rituximab-conjugated doxorubicin- MSNs (40.7 ± 19.1 nm) |
pH-sensitive controlled drug release system | Reduce systemic toxicity, improve the therapeutic efficacy | [189] |
| PEGylated-MoS 2 nanosheets (diameter 50 nm, thickness ∼2 nm) |
Combined photothermal and chemotherapy targeting | Highly efficient loading | [190] |
| DOX-Gold nanorod-1-tetradecanol-MSNs (thickness 35 nm) | Photothermalablation and chemotherapy | Precise control over drug release, localized delivery with enhanced targeting | [191] |
| Fe3O4–azobis [N-(2-carboxyethyl)-2-methylpropionamidine](Azo)-Doxorubicin | Combined photothermal therapy and chemotherapy | Enhanced cell-killing effects, increased stability, low toxicity | [192] |
Biodegradable poly (o-caprolactone) nanocarriers loaded with tamoxifen were developed for the management of estrogen receptor-specific breast cancer [126]. This study suggested that the nanoparticle preparations of selective estrogen receptor modulators deliver the drug in the specific estrogen receptor zone resulting in enhanced therapeutic efficacy. Similarly, a nanoconjugation of doxorubicin and cisplatin was developed by Chohen et al. [127], which have exhibited enhanced efficiency and reduced side effects of the loaded drugs in the treatment of localized progressive breast cancer. Likewise, chemotherapeutic drug oxaliplatin-loaded nanoparticulate micelles were prepared by Cabral et al. [128], with sustained release of loaded drug in the tumor microenvironment, resulted in enhanced antitumor effect [128]. Furthermore, SLN loaded-5-FU resulted in enhanced bioavailability and sustained release of the encapsulated anticancer drug, leading to enhanced antitumor effect [129].
Conclusions
Nanotechnology is subjected to inordinate progress in various fronts especially to make innovations in healthcare. Target-selective drug delivery and approaches for molecular imaging are the areas of prime importance for research where nanotechnology is playing a progressive role. This review provides readers with a wide vision on novel ongoing potentialities of various nanotechnology-based approaches for imaging and delivery of therapeutics. In order to obtain effective drug delivery, nanotechnology-based imaging has enabled us to apprehend the interactions of nanomaterials with biological environment, targeting receptors, molecular mechanisms involved in pathophysiology of diseases, and has made the real time monitoring of therapeutic response possible. Development of analytical technologies to measure the size of particles in nanometer ranges, and advent of latest manufacturing approaches for nanomaterials, has resulted in establishment of more effective methods for delivery of therapeutics for the treatment of ophthalmological, pulmonary, cardiovascular diseases, and more importantly cancer therapy. These new drug therapies have already been shown to cause fewer side effects and be more effective than traditional therapies. Furthermore, the imaging techniques have enhanced the determination of tumor location in human bodies and their selective targeting. Altogether, this comparatively new and thriving data suggest that additional clinical and toxicity studies are required further on the “proof-of-concept” phase. Nanomedicine cost and manufacturing at larger scale is also a matter of concern that needs to be addressed. Notwithstanding, future of nanomedicines is propitious.
Acknowledgments
Funding
There was no funding available for this work.
Availability of Data and Materials
Presented in the main paper.
Authors’ Contributions
FuD and AuR presented the idea; MM and SR did the literature review; MM, SI, and AZ write the manuscript. MK, FuD, GMK, and AuR critically review the manuscript. All authors read and approved the final manuscript.
Abbreviations
- AIE
Aggregation-induced emission
- BDP
Beclometasone dipropionate
- BODIPY
Boron dipyrromethane
- CNTs
Carbon nanotubes
- COPD
Chronic obstructive pulmonary disease
- CulnS2/ZnS
Copper indium sulfide/zinc sulfide quantum dots
- CVD
Chemical vapor deposition
- DNA
Deoxyribonucleic acid
- ENPs
Engineered nanoparticles
- EPR
Enhanced permeability and retention
- GCE
Glassy carbon electrode
- GNPs
Gold nanoparticles
- GQD
Grapheme quantum dots
- HCG
Human chorionic gonadotrophin
- MEMS
Microelectromechanical systems
- MI
Myocardial ischemia
- MNPs
Magnetic nanoparticles
- MSNs
Mesoporous silica nanoparticles
- MWNT
Multi-walled carbon nanotubes
- NEMS
Nanoelectromechanical system
- PAH
Pulmonary arterial hypertension
- PCL
Poly caprolactone
- PDGF
Platelet-derived growth factors
- PEG
Poly ethylene glycol
- PET
Positron emission tomography
- PLGA
Poly lactic-co-glycolic acid
- ROS
Reactive oxygen species
- SiRNA
Short interference RNA
- SLNS
Solid lipid nanoparticles
- SPIOs
Superparamagnetic iron oxides
- VEGF
Vascular endothelial growth factor
Ethics approval and consent to participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors declare that they have no competing interests.
Contributor Information
Asim ur Rehman, Phone: +92-51-90644144, Email: arehman@qau.edu.pk.
Fakhar ud Din, Phone: +92-51-90644056, Email: fudin@qau.edu.pk.
References
- 1.Arora S, Rajwade JM, Paknikar KM. Nanotoxicology and in vitro studies: the need of the hour. Toxicol Appl Pharm. 2012;258(2):151–165. doi: 10.1016/j.taap.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 2.Saini R, Saini S, Sharma S. Nanotechnology: the future medicine. J Cutan Aesthet Surg. 2010;3(1):32. doi: 10.4103/0974-2077.63301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Holdren J. The national nanotechnology initiative strategic plan report at subcommittee on nanoscale science, engineering and technology of committee on technology. 2011. [Google Scholar]
- 4.Fakruddin M, Hossain Z, Afroz H. Prospects and applications of nanobiotechnology: a medical perspective. J Nanobiotechnol. 2012;10(1):31. doi: 10.1186/1477-3155-10-31. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 5.Drexler E. Reprint. Engines of Creation. The Coming Era of Nanotechnology. New York: Anchor Books. Original edition, NY: Anchor Books; 1986
- 6.Drexler KE, Peterson C, Pergamit G. Unbounding the future. New York: William Morrow; 1991. [Google Scholar]
- 7.Freitas RA. Nanomedicine, volume I: basic capabilities: Landes Bioscience. TX: Georgetown; 1999. [Google Scholar]
- 8.Freitas RA., Jr . Nanomedicine, Vol. IIA: Biocompatibility. Landes Bioscience. USA: Georgetown; 2003. [Google Scholar]
- 9.Freitas RA. What is nanomedicine? Nanomed Nanotech Biol Med. 2005;1(1):2–9. doi: 10.1016/j.nano.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 10.Parviz BA, Ryan D, Whitesides GM. Using self-assembly for the fabrication of nano-scale electronic and photonic devices. IEEE Trans Adv Packag. 2003;26(3):233–241. doi: 10.1109/TADVP.2003.817971. [DOI] [Google Scholar]
- 11.Nakano T, Moore MJ, Wei F, Vasilakos AV, Shuai J. Molecular communication and networking: opportunities and challenges. IEEE Trans Nanobioscience. 2012;11(2):135–148. doi: 10.1109/TNB.2012.2191570. [DOI] [PubMed] [Google Scholar]
- 12.Cavalcanti A, Shirinzadeh B, Fukuda T, Ikeda S, editors. Hardware architecture for nanorobot application in cerebral aneurysm. Nanotechnology, 2007 IEEE-NANO 2007 7th IEEE Conference on; 2007: IEEE
- 13.Garcia R, Herruzo ET. The emergence of multifrequency force microscopy. Nat Nanotechnol. 2012;7(4):217–226. doi: 10.1038/nnano.2012.38. [DOI] [PubMed] [Google Scholar]
- 14.Sun Q, Cai X, Li J, Zheng M, Chen Z, Yu C-P. Green synthesis of silver nanoparticles using tea leaf extract and evaluation of their stability and antibacterial activity. Colloids Surf A Physicochem Eng Asp. 2014;444:226–231. doi: 10.1016/j.colsurfa.2013.12.065. [DOI] [Google Scholar]
- 15.Ferrari M. Cancer nanotechnology: opportunities and challenges. Nat Rev Cancer. 2005;5(3):161–171. doi: 10.1038/nrc1566. [DOI] [PubMed] [Google Scholar]
- 16.Vasir JK, Reddy MK, Labhasetwar VD. Nanosystems in drug targeting: opportunities and challenges. Curr Nanosci. 2005;1(1):47–64. doi: 10.2174/1573413052953110. [DOI] [Google Scholar]
- 17.Klaessig F, Marrapese M, Abe S (2011) Current perspectives in nanotechnology terminology and nomenclature. Nanotechnology standards. Springer, pp 21–52
- 18.Yadav T, Mungray AA, Mungray AK. Fabricated nanoparticles: current status and potential phytotoxic threats. Rev Environ Contam Toxicol. volume: Springer; 2014. p. 83–110 [DOI] [PubMed]
- 19.Scott N, Chen H. Nanoscale science and engineering for agriculture and food systems. Ind Biotechnol. 2013;9(1):17–18. doi: 10.1089/ind.2013.1555. [DOI] [Google Scholar]
- 20.Ebrahimi E, Akbarzadeh A, Abbasi E, Khandaghi AA, Abasalizadeh F, Davaran S. Novel drug delivery system based on doxorubicin-encapsulated magnetic nanoparticles modified with PLGA-PEG1000 copolymer. Artif Cells Nanomed Biotechnol. 2016;44(1):290–297. doi: 10.3109/21691401.2014.944646. [DOI] [PubMed] [Google Scholar]
- 21.Cosco D, Cilurzo F, Maiuolo J, Federico C, Di Martino MT, Cristiano MC et al (2015) Delivery of miR-34a by chitosan/PLGA nanoplexes for the anticancer treatment of multiple myeloma. Sci Rep 5 [DOI] [PMC free article] [PubMed]
- 22.Vartak A, Sucheck SJ. Recent advances in subunit vaccine carriers. Vaccine. 2016;4(2):12. doi: 10.3390/vaccines4020012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Virlan MJR, Miricescu D, Totan A, Greabu M, Tanase C, Sabliov CM et al (2015) Current uses of poly (lactic-co-glycolic acid) in the dental field: a comprehensive review. J Chem 2015
- 24.Hua S, Marks E, Schneider JJ, Keely S. Advances in oral nano-delivery systems for colon targeted drug delivery in inflammatory bowel disease: selective targeting to diseased versus healthy tissue. Nanomed Nanotech Biol Med. 2015;11(5):1117–1132. doi: 10.1016/j.nano.2015.02.018. [DOI] [PubMed] [Google Scholar]
- 25.Bhatia S (2016) Nanoparticles types, classification, characterization, fabrication methods and drug delivery applications. In: Natural polymer drug delivery systems. Springer, pp 33–93
- 26.Silva GA. Introduction to nanotechnology and its applications to medicine. Surg Neurol. 2004;61(3):216–220. doi: 10.1016/j.surneu.2003.09.036. [DOI] [PubMed] [Google Scholar]
- 27.Sinha B, Müller RH, Möschwitzer JP. Bottom-up approaches for preparing drug nanocrystals: formulations and factors affecting particle size. Int J Pharm. 2013;453(1):126–141. doi: 10.1016/j.ijpharm.2013.01.019. [DOI] [PubMed] [Google Scholar]
- 28.Kaialy W, Al SM. Recent advances in the engineering of nanosized active pharmaceutical ingredients: promises and challenges. Adv Colloid Interf Sci. 2016;228:71–91. doi: 10.1016/j.cis.2015.11.010. [DOI] [PubMed] [Google Scholar]
- 29.Portney NG, Ozkan M. Nano-oncology: drug delivery, imaging, and sensing. Anal Bioanal Chem. 2006;384(3):620–630. doi: 10.1007/s00216-005-0247-7. [DOI] [PubMed] [Google Scholar]
- 30.Wickline SA, Lanza GM. Nanotechnology for molecular imaging and targeted therapy. 2003. [DOI] [PubMed] [Google Scholar]
- 31.Allport JR, Weissleder R. In vivo imaging of gene and cell therapies. Exp Hematol. 2001;29(11):1237–1246. doi: 10.1016/S0301-472X(01)00739-1. [DOI] [PubMed] [Google Scholar]
- 32.Ballinger JR (2001) 99mTc-Tetrofosmin for functional imaging of P-glycoprotein modulation in vivo. J Clin Pharmacol 41(S7) [PubMed]
- 33.Kao CH, Hsieh JF, Tsai SC, Ho YJ, ChangLai SP, Lee JK. Paclitaxel-based chemotherapy for non–small cell lung cancer: predicting the response with 99mTc-tetrofosmin chest imaging. J Nucl Med. 2001;42(1):17–20. [PubMed] [Google Scholar]
- 34.Martina M-S, Fortin J-P, Ménager C, Clément O, Barratt G, Grabielle-Madelmont C, et al. Generation of superparamagnetic liposomes revealed as highly efficient MRI contrast agents for in vivo imaging. J Am Chem Soc. 2005;127(30):10676–10685. doi: 10.1021/ja0516460. [DOI] [PubMed] [Google Scholar]
- 35.Kuil J, Buckle T, Oldenburg J, Yuan H, Borowsky AD, Josephson L, et al. Hybrid peptide dendrimers for imaging of chemokine receptor 4 (CXCR4) expression. Mol Pharm. 2011;8(6):2444–2453. doi: 10.1021/mp200401p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Noon WH, Kong Y, Ma J. Molecular dynamics analysis of a buckyball–antibody complex. Proc Natl Acad Sci. 2002;99(suppl 2):6466–6470. doi: 10.1073/pnas.022532599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Torchilin VP. Polymeric contrast agents for medical imaging. Curr Pharm Biotechnol. 2000;1(2):183–215. doi: 10.2174/1389201003378960. [DOI] [PubMed] [Google Scholar]
- 38.Milroy LG, Rizzo S, Calderon A, Ellinger B, Erdmann S, Mondry J, et al. Selective chemical imaging of static actin in live cells. J Am Chem Soc. 2012;134(20):8480–8486. doi: 10.1021/ja211708z. [DOI] [PubMed] [Google Scholar]
- 39.Kowada T, Maeda H, Kikuchi K. BODIPY-based probes for the fluorescence imaging of biomolecules in living cells. Chem Soc Rev. 2015;44(14):4953–4972. doi: 10.1039/C5CS00030K. [DOI] [PubMed] [Google Scholar]
- 40.Mohs AM, Provenzale JM. Applications of nanotechnology to imaging and therapy of brain tumors. Neuroimaging Clin N Am. 2010;20(3):283–292. doi: 10.1016/j.nic.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 41.Wang L, Zhu SJ, Wang HY, Qu SN, Zhang YL, Zhang JH, et al. Common origin of green luminescence in carbon nanodots and graphene quantum dots. ACS Nano. 2014;8(3):2541–2547. doi: 10.1021/nn500368m. [DOI] [PubMed] [Google Scholar]
- 42.Gao X, Cui Y, Levenson RM, Chung LW, Nie S. In vivo cancer targeting and imaging with semiconductor quantum dots. Nat Biotechnol. 2004;22(8):969–976. doi: 10.1038/nbt994. [DOI] [PubMed] [Google Scholar]
- 43.Shih WH, Shih WY, Li H, Schillo MC. Water soluble quantum dots. 2009. [Google Scholar]
- 44.Bagalkot V, Zhang L, Levy-Nissenbaum E, Jon S, Kantoff PW, Langer R, et al. Quantum dot− aptamer conjugates for synchronous cancer imaging, therapy, and sensing of drug delivery based on bi-fluorescence resonance energy transfer. Nano Lett. 2007;7(10):3065–3070. doi: 10.1021/nl071546n. [DOI] [PubMed] [Google Scholar]
- 45.Choi HS, Liu W, Misra P, Tanaka E, Zimmer JP, Ipe BI, et al. Renal clearance of quantum dots. Nat Biotechnol. 2007;25(10):1165–1170. doi: 10.1038/nbt1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pons T, Pic E, Lequeux N, Cassette E, Bezdetnaya L, Guillemin F, et al. Cadmium-free CuInS2/ZnS quantum dots for sentinel lymph node imaging with reduced toxicity. ACS Nano. 2010;4(5):2531–2538. doi: 10.1021/nn901421v. [DOI] [PubMed] [Google Scholar]
- 47.Buch RM, Rechnitz G. Intact chemoreceptor-based biosensors: responses and analytical limits. Biosensors. 1989;4(4):215–230. doi: 10.1016/0265-928X(89)80036-7. [DOI] [Google Scholar]
- 48.Kricka L (1988) Molecular and ionic recognition by biological systems, Chemical sensors. Springer, pp 3–14
- 49.Zhang X, Guo Q, Cui D. Recent advances in nanotechnology applied to biosensors. Sensors. 2009;9(2):1033–1053. doi: 10.3390/s90201033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.You X, He R, Gao F, Shao J, Pan B, Cui D. Hydrophilic high-luminescent magnetic nanocomposites. Nanotechnology. 2007;18(3):035701. doi: 10.1088/0957-4484/18/3/035701. [DOI] [PubMed] [Google Scholar]
- 51.Pan B, Cui D, Sheng Y, Ozkan C, Gao F, He R, et al. Dendrimer-modified magnetic nanoparticles enhance efficiency of gene delivery system. Cancer Res. 2007;67(17):8156–8163. doi: 10.1158/0008-5472.CAN-06-4762. [DOI] [PubMed] [Google Scholar]
- 52.Cui D, Tian F, Coyer SR, Wang J, Pan B, Gao F, et al. Effects of antisense-Myc-conjugated single-walled carbon Nanotubes on HL-60Cells. J Nanosci Nanotechnol. 2007;7(4–1):1639–1646. doi: 10.1166/jnn.2007.348. [DOI] [PubMed] [Google Scholar]
- 53.Pan B, Cui D, Xu P, Li Q, Huang T, He R, et al. Study on interaction between gold nanorod and bovine serum albumin. Colloids Surf A Physicochem Eng Asp. 2007;295(1):217–222. doi: 10.1016/j.colsurfa.2006.09.002. [DOI] [Google Scholar]
- 54.Liang KZ, Qi JS, Mu WJ, Chen ZG. Biomolecules/gold nanowires-doped sol–gel film for label-free electrochemical immunoassay of testosterone. J Biochem Biophys Methods. 2008;70(6):1156–1162. doi: 10.1016/j.jprot.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 55.He X, Yuan R, Chai Y, Shi Y. A sensitive amperometric immunosensor for carcinoembryonic antigen detection with porous nanogold film and nano-au/chitosan composite as immobilization matrix. J Biochem Biophys Methods. 2008;70(6):823–829. doi: 10.1016/j.jbbm.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 56.Chai R, Yuan R, Chai Y, Ou C, Cao S, Li X. Amperometric immunosensors based on layer-by-layer assembly of gold nanoparticles and methylene blue on thiourea modified glassy carbon electrode for determination of human chorionic gonadotrophin. Talanta. 2008;74(5):1330–1336. doi: 10.1016/j.talanta.2007.08.046. [DOI] [PubMed] [Google Scholar]
- 57.Pan B, Cui D, He R, Gao F, Zhang Y. Covalent attachment of quantum dot on carbon nanotubes. Chem Phys Lett. 2006;417(4):419–424. doi: 10.1016/j.cplett.2005.10.044. [DOI] [Google Scholar]
- 58.Cui D, Tian F, Kong Y, Titushikin I, Gao H. Effects of single-walled carbon nanotubes on the polymerase chain reaction. Nanotechnology. 2003;15(1):154. doi: 10.1088/0957-4484/15/1/030. [DOI] [Google Scholar]
- 59.Cui D. Advances and prospects on biomolecules functionalized carbon nanotubes. J Nanosci Nanotechnol. 2007;7(4–1):1298–1314. doi: 10.1166/jnn.2007.654. [DOI] [PubMed] [Google Scholar]
- 60.Li G, Xu H, Huang W, Wang Y, Wu Y, Parajuli R. A pyrrole quinoline quinone glucose dehydrogenase biosensor based on screen-printed carbon paste electrodes modified by carbon nanotubes. Meas SciTechnol. 2008;19(6):065203. doi: 10.1088/0957-0233/19/6/065203. [DOI] [Google Scholar]
- 61.Lee H, Lee E, Kim DK, Jang NK, Jeong YY, Jon S. Antibiofouling polymer-coated superparamagnetic iron oxide nanoparticles as potential magnetic resonance contrast agents for in vivo cancer imaging. J Am Chem Soc. 2006;128(22):7383–7389. doi: 10.1021/ja061529k. [DOI] [PubMed] [Google Scholar]
- 62.Kim DH, Lee SH, Kim KN, Kim KM, Shim IB, Lee YK. Cytotoxicity of ferrite particles by MTT and agar diffusion methods for hyperthermic application. J Magn Magn Mater. 2005;293(1):287–292. doi: 10.1016/j.jmmm.2005.02.078. [DOI] [Google Scholar]
- 63.Sincai M, Ganga D, Ganga M, Argherie D, Bica D. Antitumor effect of magnetite nanoparticles in cat mammary adenocarcinoma. J Magn Magn Mater. 2005;293(1):438–441. doi: 10.1016/j.jmmm.2005.02.074. [DOI] [Google Scholar]
- 64.Ito A, Ino K, Kobayashi T, Honda H. The effect of RGD peptide-conjugated magnetite cationic liposomes on cell growth and cell sheet harvesting. Biomaterials. 2005;26(31):6185–6193. doi: 10.1016/j.biomaterials.2005.03.039. [DOI] [PubMed] [Google Scholar]
- 65.Guedes MHA, Sadeghiani N, Peixoto DLG, Coelho JP, Barbosa LS, Azevedo RB, et al. Effects of AC magnetic field and carboxymethyldextran-coated magnetite nanoparticles on mice peritoneal cells. J Magn Magn Mater. 2005;293(1):283–286. doi: 10.1016/j.jmmm.2005.02.052. [DOI] [Google Scholar]
- 66.Rife J, Miller M, Sheehan P, Tamanaha C, Tondra M, Whitman L. Design and performance of GMR sensors for the detection of magnetic microbeads in biosensors. Sens Actuators A-Phys. 2003;107(3):209–218. doi: 10.1016/S0924-4247(03)00380-7. [DOI] [Google Scholar]
- 67.Morishita N, Nakagami H, Morishita R. Takeda S-i, Mishima F, Nishijima S, et al. magnetic nanoparticles with surface modification enhanced gene delivery of HVJ-E vector. Biochem. Biophys. Res. Commun. 2005;334(4):1121–1126. doi: 10.1016/j.bbrc.2005.06.204. [DOI] [PubMed] [Google Scholar]
- 68.Lai GS, Zhang HL, Han DY. A novel hydrogen peroxide biosensor based on hemoglobin immobilized on magnetic chitosan microspheres modified electrode. Sens and Actuators B: Chem. 2008;129(2):497–503. doi: 10.1016/j.snb.2007.08.041. [DOI] [Google Scholar]
- 69.Cao C, Kim JH, Yoon D, Hwang ES, Kim YJ, Baik S. Optical detection of DNA hybridization using absorption spectra of single-walled carbon nanotubes. Mater Chem Phys. 2008;112(3):738–741. doi: 10.1016/j.matchemphys.2008.07.129. [DOI] [Google Scholar]
- 70.Corot C, Robert P, Idée JM, Port M. Recent advances in iron oxide nanocrystal technology for medical imaging. Adv Drug Deliv Rev. 2006;58(14):1471–1504. doi: 10.1016/j.addr.2006.09.013. [DOI] [PubMed] [Google Scholar]
- 71.Semelka RC, Helmberger TK. Contrast agents for MR imaging of the liver 1. Radiology. 2001;218(1):27–38. doi: 10.1148/radiology.218.1.r01ja2427. [DOI] [PubMed] [Google Scholar]
- 72.Harisinghani MG, Barentsz J, Hahn PF, Deserno WM, Tabatabaei S, van de Kaa CH, et al. Noninvasive detection of clinically occult lymph-node metastases in prostate cancer. N Engl J Med. 2003;348:2491–2499. doi: 10.1056/NEJMoa022749. [DOI] [PubMed] [Google Scholar]
- 73.Harisinghani MG, Weissleder R. Sensitive, noninvasive detection of lymph node metastases. PLoS Med. 2004;1(3):e66. doi: 10.1371/journal.pmed.0010066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wagner V, Dullaart A, Bock AK, Zweck A. The emerging nanomedicine landscape. Nat Biotechnol. 2006;24(10):1211–1217. doi: 10.1038/nbt1006-1211. [DOI] [PubMed] [Google Scholar]
- 75.Blanco E, Shen H, Ferrari M. Principles of nanoparticle design for overcoming biological barriers to drug delivery. Nat Biotechnol. 2015;33(9):941–951. doi: 10.1038/nbt.3330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wadhwa S, Paliwal R, Paliwal SR, Vyas S. Nanocarriers in ocular drug delivery: an update review. Curr Pharm Des. 2009;15(23):2724–2750. doi: 10.2174/138161209788923886. [DOI] [PubMed] [Google Scholar]
- 77.ud Din F, Rashid R, Mustapha O, Kim DW, Park JH, Ku SK, et al. Development of a novel solid lipid nanoparticles-loaded dual-reverse thermosensitive nanomicelle for intramuscular administration with sustained release and reduced toxicity. RSC Adv. 2015;5(54):43687–43694. doi: 10.1039/C5RA05656J. [DOI] [Google Scholar]
- 78.Patel A, Cholker K, Agrahari V, Mitra AK. Occular drug delivery systems: an overview. World J Pharmacol 2013;2(2): 47–64 [DOI] [PMC free article] [PubMed]
- 79.Puglia C, Offerta A, Carbone C, Bonina F, Pignatello R, Puglisi G. Lipid nanocarriers (LNC) and their applications in ocular drug delivery. Curr Med Chem. 2015;22(13):1589–1602. doi: 10.2174/0929867322666150209152259. [DOI] [PubMed] [Google Scholar]
- 80.Abrego G, Alvarado H, Souto EB, Guevara B, Bellowa LH, Parra A, et al. Biopharmaceutical profile of pranoprofen-loaded PLGA nanoparticles containing hydrogels for ocular administration. Eur J Pharm Biopharm. 2015;95:261–270. doi: 10.1016/j.ejpb.2015.01.026. [DOI] [PubMed] [Google Scholar]
- 81.Andrei G, Peptu CA, Popa M, Desbrieres J, Peptu C, Gardikiotis F, et al. Formulation and evaluation of cefuroxim loaded submicron particles for ophthalmic delivery. Int J Pharm. 2015;493(1):16–29. doi: 10.1016/j.ijpharm.2015.07.053. [DOI] [PubMed] [Google Scholar]
- 82.Asasutjarit R, Theerachayanan T, Kewsuwan P, Veeranodha S, Fuongfuchat A, Ritthidej GC. Development and evaluation of diclofenac sodium loaded-N-Trimethyl chitosan nanoparticles for ophthalmic use. AAPS PharmSciTech. 2015;16(5):1013–1024. doi: 10.1208/s12249-015-0290-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Fabiano A, Chetoni P, Zambito Y. Mucoadhesive nano-sized supramolecular assemblies for improved pre-corneal drug residence time. Drug Dev Ind Pharm. 2015;41(12):2069–2076. doi: 10.3109/03639045.2015.1066798. [DOI] [PubMed] [Google Scholar]
- 84.El-Salamouni NS, Farid RM, El-Kamel AH, El-Gamal SS. Effect of sterilization on the physical stability of brimonidine-loaded solid lipid nanoparticles and nanostructured lipid carriers. Int J Pharm. 2015;496(2):976–983. doi: 10.1016/j.ijpharm.2015.10.043. [DOI] [PubMed] [Google Scholar]
- 85.Ibrahim MM, Abd-Elgawad A-EH, Soliman OA-E, Jablonski MM. Natural bioadhesive biodegradable nanoparticle-based topical ophthalmic formulations for management of glaucoma. Transl Vis Sci Technol. 2015;4(3):12. doi: 10.1167/tvst.4.3.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Costa J, Silva N, Sarmento B, Pintado M. Potential chitosan-coated alginate nanoparticles for ocular delivery of daptomycin. Eur J Clin Microbiol Infect Dis. 2015;34(6):1255–1262. doi: 10.1007/s10096-015-2344-7. [DOI] [PubMed] [Google Scholar]
- 87.Pan Q, Xu Q, Boylan NJ, Lamb NW, Emmert DG, Yang J-C, et al. Corticosteroid-loaded biodegradable nanoparticles for prevention of corneal allograft rejection in rats. J Control Release. 2015;201:32–40. doi: 10.1016/j.jconrel.2015.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Pradhan N, Guha R, Chowdhury S, Nandi S, Konar A, Hazra S. Curcumin nanoparticles inhibit corneal neovascularization. J Mol Medic. 2015;93(10):1095–1106. doi: 10.1007/s00109-015-1277-z. [DOI] [PubMed] [Google Scholar]
- 89.Yee W, Selvaduray G, Hawkins B. Characterization of silver nanoparticle-infused tissue adhesive for ophthalmic use. J Mech Behav Biomed Mater. 2016;55:67–74. doi: 10.1016/j.jmbbm.2015.10.011. [DOI] [PubMed] [Google Scholar]
- 90.Weber S, Zimmer A, Pardeike J. Solid lipid Nanoparticles (SLN) and Nanostructured lipid carriers (NLC) for pulmonary application: a review of the state of the art. Eur J Pharm Biopharm. 2014;86(1):7–22. doi: 10.1016/j.ejpb.2013.08.013. [DOI] [PubMed] [Google Scholar]
- 91.Yang W, Peters JI, Williams RO., III. Inhaled nanoparticles--a current review. Int J Pharm. 2008;356(1–2):239–247. doi: 10.1016/j.ijpharm.2008.02.011. [DOI] [PubMed] [Google Scholar]
- 92.Smola M, Vandamme T, Sokolowski A. Nanocarriers as pulmonary drug delivery systems to treat and to diagnose respiratory and nonrespiratory diseases. Int J Nanomedicine. 2008;3(1):1. doi: 10.2217/17435889.3.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sung JC, Pulliam BL, Edwards DA. Nanoparticles for drug delivery to the lungs. Trends Biotechnol. 2007;25(12):563–570. doi: 10.1016/j.tibtech.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 94.Menon JU, Ravikumar P, Pise A, Gyawali D, Hsia CC, Nguyen KT. Polymeric nanoparticles for pulmonary protein and DNA delivery. Acta Biomater. 2014;10(6):2643–2652. doi: 10.1016/j.actbio.2014.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Nasr M, Najlah M, D’Emanuele A, Elhissi A. PAMAM dendrimers as aerosol drug nanocarriers for pulmonary delivery via nebulization. Int J Pharm. 2014;461(1):242–250. doi: 10.1016/j.ijpharm.2013.11.023. [DOI] [PubMed] [Google Scholar]
- 96.Mohamud R, Xiang SD, Selomulya C, Rolland JM, O’Hehir RE, Hardy CL, et al. The effects of engineered nanoparticles on pulmonary immune homeostasis. Drug Metab Rev. 2014;46(2):176–190. doi: 10.3109/03602532.2013.859688. [DOI] [PubMed] [Google Scholar]
- 97.McLendon JM, Joshi SR, Sparks J, Matar M, Fewell JG, Abe K, et al. Lipid nanoparticle delivery of a microRNA-145 inhibitor improves experimental pulmonary hypertension. J Control Release. 2015;210:67–75. doi: 10.1016/j.jconrel.2015.05.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Arora N, Singh K, Garg T. Areas of nanomedicine applications. Int J Univ Pharm Life Sci. 2012;2:216–227. [Google Scholar]
- 99.Singh B, Garg T, Goyal AK, Rath G. Recent advancements in the cardiovascular drug carriers. Artif Cells Nanomed Biotechnol. 2016;44(1):216–225. doi: 10.3109/21691401.2014.937868. [DOI] [PubMed] [Google Scholar]
- 100.Mathers C, Fat DM, Boerma JT. The global burden of disease: 2004 update: World Health Organization. 2008. [Google Scholar]
- 101.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2013;380(9859):2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Haeri A, Sadeghian S, Rabbani S, Anvari MS, Ghassemi S, Radfar F, et al. Effective attenuation of vascular restenosis following local delivery of chitosan decorated sirolimus liposomes. Carbohydr Polymer. 2017;157:1461–1469. doi: 10.1016/j.carbpol.2016.11.021. [DOI] [PubMed] [Google Scholar]
- 103.Arzani G, Haeri A, Daeihamed M, Bakhtiari-Kaboutaraki H, Dadashzadeh S. Niosomal carriers enhance oral bioavailability of carvedilol: effects of bile salt-enriched vesicles and carrier surface charge. Int J Nanomedicine. 2015;10:4797. doi: 10.2147/IJN.S84703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Godin B, Sakamoto JH, Serda RE, Grattoni A, Bouamrani A, Ferrari M. Emerging applications of nanomedicine for the diagnosis and treatment of cardiovascular diseases. Trends Pharmacol Sci. 2010;31(5):199–205. doi: 10.1016/j.tips.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Formiga FR, Pelacho B, Garbayo E, Abizanda G, Gavira JJ, Simon-Yarza T, et al. Sustained release of VEGF through PLGA microparticles improves vasculogenesis and tissue remodeling in an acute myocardial ischemia–reperfusion model. J Control Release. 2010;147(1):30–37. doi: 10.1016/j.jconrel.2010.07.097. [DOI] [PubMed] [Google Scholar]
- 106.Simón-Yarza T, Tamayo E, Benavides C, Lana H, Formiga FR, Grama CN, et al. Functional benefits of PLGA particulates carrying VEGF and CoQ 10 in an animal of myocardial ischemia. Int J Pharm. 2013;454(2):784–790. doi: 10.1016/j.ijpharm.2013.04.015. [DOI] [PubMed] [Google Scholar]
- 107.Danhier F, Feron O, Preat V. To exploit the tumor microenvironment: passive and active tumor targeting of nanocarriers for anti-cancer drug delivery. J Control Release. 2010;148(2):135–146. doi: 10.1016/j.jconrel.2010.08.027. [DOI] [PubMed] [Google Scholar]
- 108.Mishra B, Patel BB, Tiwari S. Colloidal nanocarriers: a review on formulation technology, types and applications toward targeted drug delivery. Nanomed Nanotechnol Biol Med. 2010;6(1):9–24. doi: 10.1016/j.nano.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 109.Din FU, Kim DW, Choi JY, Thapa RK, Mustapha O, Kim DS, et al. Irinotecan-loaded double-reversible thermogel with improved antitumor efficacy without initial burst effect and toxicity for intramuscular administration. Acta Biomater. 2017;54:239–248. doi: 10.1016/j.actbio.2017.03.007. [DOI] [PubMed] [Google Scholar]
- 110.Maeda H, Bharate G, Daruwalla J. Polymeric drugs for efficient tumor-targeted drug delivery based on EPR-effect. Eur J Pharma Biopharm. 2009;71(3):409–419. doi: 10.1016/j.ejpb.2008.11.010. [DOI] [PubMed] [Google Scholar]
- 111.Matsumura Y, Maeda H. A new concept for macromolecular therapeutics in cancer chemotherapy: mechanism of tumoritropic accumulation of proteins and the antitumor agent smancs. Cancer Res. 1986;46(12 Part 1):6387–6392. [PubMed] [Google Scholar]
- 112.Din FU, Choi JY, Kim DW, Mustapha O, Kim DS, Thapa RK, et al. Irinotecan-encapsulated double-reverse thermosensitive nanocarrier system for rectal administration. Drug Deliv. 2017;24(1):502–510. doi: 10.1080/10717544.2016.1272651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Tong R, Hemmati HD, Langer R, Kohane DS. Photoswitchable nanoparticles for triggered tissue penetration and drug delivery. J Am Chem Soc. 2012;134(21):8848–8855. doi: 10.1021/ja211888a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Arias JL, Reddy LH, Othman M, Gillet B, Desmaele D, Zouhiri F, et al. Squalene based nanocomposites: a new platform for the design of multifunctional pharmaceutical theragnostics. ACS Nano. 2011;5(2):1513–1521. doi: 10.1021/nn1034197. [DOI] [PubMed] [Google Scholar]
- 115.Brown JM, Wilson WR. Exploiting tumour hypoxia in cancer treatment. Nat Rev Cancer. 2004;4(6):437–447. doi: 10.1038/nrc1367. [DOI] [PubMed] [Google Scholar]
- 116.Cao J, Deng X, Su T, He B. Fabrication of polymeric nanoparticles for cancer therapy and intracellular tracing. Nanomed Nanotechnol Biol Med. 2016;12(2):459. doi: 10.1016/j.nano.2015.12.036. [DOI] [Google Scholar]
- 117.Xie J, Zhang X, Teng M, Yu B, Yang S, Lee RJ, et al. Synthesis, characterization, and evaluation of mPeg–sN38 and mPeg–Pla–sN38 micelles for cancer therapy.Int J Nanomedicine. 2016;11:1677 [DOI] [PMC free article] [PubMed]
- 118.Eloy JO, Petrilli R, Topan JF, Antonio HMR, Barcellos JPA, Chesca DL, et al. Co-loaded paclitaxel/rapamycin liposomes: development, characterization and in vitro and in vivo evaluation for breast cancer therapy. Colloids Surf B Biointerfaces. 2016;141:74–82. doi: 10.1016/j.colsurfb.2016.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Din FU, Mustapha O, Kim DW, Rashid R, Park JH, Choi JY, et al. Novel dual-reverse thermosensitive solid lipid nanoparticle-loaded hydrogel for rectal administration of flurbiprofen with improved bioavailability and reduced initial burst effect. Eur J Pharm Biopharm. 2015;94:64–72. doi: 10.1016/j.ejpb.2015.04.019. [DOI] [PubMed] [Google Scholar]
- 120.Lee J, Kang JA, Ryu Y, Han S-S, Nam YR, Rho JK, et al. Genetically engineered and self-assembled oncolytic protein nanoparticles for targeted cancer therapy. Biomaterials. 2017;120:22–31. doi: 10.1016/j.biomaterials.2016.12.014. [DOI] [PubMed] [Google Scholar]
- 121.Le DH, Lee KL, Shukla S, Commandeur U, Steinmetz NF. Potato virus X, a filamentous plant viral nanoparticle for doxorubicin delivery in cancer therapy. Nano. 2017;9(6):2348–2357. doi: 10.1039/c6nr09099k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Volsi AL, de Aberasturi DJ, Henriksen-Lacey M, Giammona G, Licciardi M, Liz-Marzán LM. Inulin coated plasmonic gold nanoparticles as a tumor-selective tool for cancer therapy. J Mater Chem B. 2016;4(6):1150–1155. doi: 10.1039/C5TB01810B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Zhuang Y, Deng H, Su Y, He L, Wang R, Tong G, et al. Aptamer-functionalized and backbone redox-responsive hyperbranched polymer for targeted drug delivery in cancer therapy. Biomacromolecules. 2016;17(6):2050–2062. doi: 10.1021/acs.biomac.6b00262. [DOI] [PubMed] [Google Scholar]
- 124.Wang X, Wang H, Wang Y, Yu X, Zhang S, Zhang Q et al (2016) A facile strategy to prepare Dendrimer-stabilized gold Nanorods with sub-10-nm size for efficient Photothermal cancer therapy. Sci Rep 6 [DOI] [PMC free article] [PubMed]
- 125.Gray MJ, Gong J, Nguyen V, Schuler-Hatch M, Hughes C, Hutchins J, et al. Abstract B27: targeting of phosphatidylserine by monoclonal antibody ch1N11 enhances the antitumor activity of immune checkpoint inhibitor PD-1/PD-L1 therapy in orthotopic murine breast cancer models. 2016. [Google Scholar]
- 126.Chawla JS, Amiji MM. Biodegradable poly (ε-caprolactone) nanoparticles for tumor-targeted delivery of tamoxifen. Int J Pharm. 2002;249(1):127–138. doi: 10.1016/S0378-5173(02)00483-0. [DOI] [PubMed] [Google Scholar]
- 127.Cohen SM, Mukerji R, Cai S, Damjanov I, Forrest ML, Cohen MS. Subcutaneous delivery of nanoconjugated doxorubicin and cisplatin for locally advanced breast cancer demonstrates improved efficacy and decreased toxicity at lower doses than standard systemic combination therapy in vivo. Am J Surg. 2011;202(6):646–653. doi: 10.1016/j.amjsurg.2011.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Cabral H, Murakami M, Hojo H, Terada Y, Kano MR. Chung Ui, et al. targeted therapy of spontaneous murine pancreatic tumors by polymeric micelles prolongs survival and prevents peritoneal metastasis. Proc Natl Acad Sci. 2013;110(28):11397–11402. doi: 10.1073/pnas.1301348110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Yassin A, Anwer MK, Mowafy HA, El-Bagory IM, Bayomi MA, Alsarra IA. Optimization of 5-fluorouracil solid-lipid nanoparticles: a preliminary study to treat colon cancer. Int J Med Sci. 2010;7(6):398–408. doi: 10.7150/ijms.7.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Alley SC, Okeley NM, Senter PD. Antibody–drug conjugates: targeted drug delivery for cancer. Curr opinion Chem Biol. 2010;14(4):529–537. doi: 10.1016/j.cbpa.2010.06.170. [DOI] [PubMed] [Google Scholar]
- 131.Reddy B, Yadav HK, Nagesha DK, Raizaday A, Karim A. Polymeric micelles as novel carriers for poorly soluble drugs—review. J Nanosci Nanotechnol. 2015;15(6):4009–4018. doi: 10.1166/jnn.2015.9713. [DOI] [PubMed] [Google Scholar]
- 132.Gillies ER, Frechet JM. Dendrimers and dendritic polymers in drug delivery. Drug Discov Today. 2005;10(1):35–43. doi: 10.1016/S1359-6446(04)03276-3. [DOI] [PubMed] [Google Scholar]
- 133.Anupa R. Menjoge rangaramanujam, M.; Kannan Donald, a,; Tomalia. Dendrimer–based drug and imaging conjugates: desingn considerations for nanomedical application. Drug Discov Today. 2010;15:171–185. doi: 10.1016/j.drudis.2010.01.009. [DOI] [PubMed] [Google Scholar]
- 134.Zhao M-X, Zhu B-J. The research and applications of quantum dots as nano-carriers for targeted drug delivery and cancer therapy. Nanoscale Res Lett. 2016;11(1):207. doi: 10.1186/s11671-016-1394-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Martincic M, Tobias G. Filled carbon nanotubes in biomedical imaging and drug delivery. Expert Opin Drug Deliv. 2015;12(4):563–581. doi: 10.1517/17425247.2015.971751. [DOI] [PubMed] [Google Scholar]
- 136.Ahmad MZ, Akhter S, Jain GK, Rahman M, Pathan SA, Ahmad FJ, et al. Metallic nanoparticles: technology overview & drug delivery applications in oncology. Expert Opin Drug Deliv. 2010;7(8):927–942. doi: 10.1517/17425247.2010.498473. [DOI] [PubMed] [Google Scholar]
- 137.Wang Y, Zhao Q, Han N, Bai L, Li J, Liu J, et al. Mesoporous silica nanoparticles in drug delivery and biomedical applications. Nanomed Nanotech Biol Med. 2015;11(2):313–327. doi: 10.1016/j.nano.2014.09.014. [DOI] [PubMed] [Google Scholar]
- 138.Nazemi A, Gillies ER. Dendritic surface functionalization of nanomaterials: controlling properties and functions for biomedical applications. Braz J Pharm Sci. 2013;49(SPE):15–32. doi: 10.1590/S1984-82502013000700003. [DOI] [Google Scholar]
- 139.Bottari G, Urbani M, Torres T. Organic Nanomaterials: synthesis, characterization, and device applications. 2013. Covalent, donor–acceptor ensembles based ON Phthalocyanines AND CARBON nanostructures; pp. 163–186. [Google Scholar]
- 140.Siró I, Plackett D. Microfibrillated cellulose and new nanocomposite materials: a review. Cellulose. 2010;17(3):459–494. doi: 10.1007/s10570-010-9405-y. [DOI] [Google Scholar]
- 141.Jariwala D, Sangwan VK, Lauhon LJ, Marks TJ, Hersam MC. Carbon nanomaterials for electronics, optoelectronics, photovoltaics, and sensing. Chem Soc Rev. 2013;42(7):2824–2860. doi: 10.1039/C2CS35335K. [DOI] [PubMed] [Google Scholar]
- 142.Duran H, Steinhart M. Butt H-Jr, Floudas G. From heterogeneous to homogeneous nucleation of isotactic poly (propylene) confined to nanoporous alumina. Nano Lett. 2011;11(4):1671–1675. doi: 10.1021/nl200153c. [DOI] [PubMed] [Google Scholar]
- 143.Kumari A, Yadav SK, Yadav SC. Biodegradable polymeric nanoparticles based drug delivery systems. Colloids Surf B Biointerfaces. 2010;75(1):1–18. doi: 10.1016/j.colsurfb.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 144.Hoare T, Santamaria J, Goya GF, Irusta S, Lin D, Lau S, et al. A magnetically-triggered composite membrane for on-demand drug delivery. Nano Lett. 2009;9(10):3651. doi: 10.1021/nl9018935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Mishra B, Patel BB, Tiwari S. Colloidal nanocarriers: a review on formulation technology, types and applications toward targeted drug delivery. Nanomed Nanotech Biol Med. 2010;6(1):9–24. doi: 10.1016/j.nano.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 146.Rabl P, Kolkowitz S, Koppens F, Harris J, Zoller P, Lukin M. A quantum spin transducer based on nanoelectromechanical resonator arrays. Nat Phys. 2010;6(8):602–608. doi: 10.1038/nphys1679. [DOI] [Google Scholar]
- 147.Chandrasekhar S, Iyer LK, Panchal JP, Topp EM, Cannon JB, Ranade VV. Microarrays and microneedle arrays for delivery of peptides, proteins, vaccines and other applications. Expert Opin Drug Deliv. 2013;10(8):1155–1170. doi: 10.1517/17425247.2013.797405. [DOI] [PubMed] [Google Scholar]
- 148.Shabnashmi PS. NKS, Vithya V., Vijaya Lakshmi B. And jasmine R. Therapeutic applications of Nanorobots- Respirocytes and Microbivores. J Chem Pharm Res. 2016;8(5):605–609. [Google Scholar]
- 149.Homayouni A, Sadeghi F, Varshosaz J, Garekani HA, Nokhodchi A. Promising dissolution enhancement effect of soluplus on crystallized celecoxib obtained through antisolvent precipitation and high pressure homogenization techniques. Colloid Surf B Biointerfaces. 2014;122:591–600. doi: 10.1016/j.colsurfb.2014.07.037. [DOI] [PubMed] [Google Scholar]
- 150.Mugheirbi NA, Paluch KJ, Tajber L. Heat induced evaporative antisolvent nanoprecipitation (HIEAN) of itraconazole. Int J Pharm. 2014;471(1):400–411. doi: 10.1016/j.ijpharm.2014.05.045. [DOI] [PubMed] [Google Scholar]
- 151.Sadeghi F, Ashofteh M, Homayouni A, Abbaspour M, Nokhodchi A, Garekani HA. Antisolvent precipitation technique: a very promising approach to crystallize curcumin in presence of polyvinyl pyrrolidon for solubility and dissolution enhancement. Colloids Surf B Biointerfaces. 2016;147:258–264. doi: 10.1016/j.colsurfb.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 152.Margulis K, Magdassi S, Lee HS, Macosko CW. Formation of curcumin nanoparticles by flash nanoprecipitation from emulsions. J Colloid Interface Sci. 2014;434:65–70. doi: 10.1016/j.jcis.2014.07.040. [DOI] [PubMed] [Google Scholar]
- 153.Wang M, Yang N, Guo Z, Gu K, Shao A, Zhu W, et al. Facile preparation of AIE-active fluorescent Nanoparticles through flash Nanoprecipitation. Ind Eng Chem Res. 2015;54(17):4683–4688. doi: 10.1021/acs.iecr.5b00501. [DOI] [Google Scholar]
- 154.Tam YT, To KKW. Chow AHL. Fabrication of doxorubicin nanoparticles by controlled antisolvent precipitation for enhanced intracellular delivery. Colloid Surf B Biointerfaces. 2016;139:249–258. doi: 10.1016/j.colsurfb.2015.12.026. [DOI] [PubMed] [Google Scholar]
- 155.Ige PP, Baria RK, Gattani SG. Fabrication of fenofibrate nanocrystals by probe sonication method for enhancement of dissolution rate and oral bioavailability. Colloid Surf B Biointerfaces. 2013;108:366–373. doi: 10.1016/j.colsurfb.2013.02.043. [DOI] [PubMed] [Google Scholar]
- 156.Sahu BP, Das MK. Preparation and in vitro/in vivo evaluation of felodipine nanosuspension. Eur J Drug Metab Pharmacokinet. 2014;39(3):183–193. doi: 10.1007/s13318-013-0158-5. [DOI] [PubMed] [Google Scholar]
- 157.Noh J-K, Naeem M, Cao J, Lee EH, Kim M-S, Jung Y, et al. Herceptin-functionalized pure paclitaxel nanocrystals for enhanced delivery to HER2-postive breast cancer cells. Int J Pharm. 2016;513(1):543–553. doi: 10.1016/j.ijpharm.2016.09.067. [DOI] [PubMed] [Google Scholar]
- 158.Guo M, Fu Q, Wu C, Guo Z, Li M, Sun J, et al. Rod shaped nanocrystals exhibit superior in vitro dissolution and in vivo bioavailability over spherical like nanocrystals: a case study of lovastatin. Colloid Surf B Biointerfaces. 2015;128:410–418. doi: 10.1016/j.colsurfb.2015.02.039. [DOI] [PubMed] [Google Scholar]
- 159.Peng H, Wang J, Lv S, Wen J, Chen JF. Synthesis and characterization of hydroxyapatite nanoparticles prepared by a high-gravity precipitation method. Ceram Int. 2015;41(10):14340–14349. doi: 10.1016/j.ceramint.2015.07.067. [DOI] [Google Scholar]
- 160.Li M, Yaragudi N, Afolabi A, Dave R, Bilgili E. Sub-100nm drug particle suspensions prepared via wet milling with low bead contamination through novel process intensification. Chem Eng Sci. 2015;130:207–220. doi: 10.1016/j.ces.2015.03.020. [DOI] [Google Scholar]
- 161.De Smet L, Saerens L, De Beer T, Carleer R, Adriaensens P, Van Bocxlaer J, et al. Formulation of itraconazole nanococrystals and evaluation of their bioavailability in dogs. Eur J Pharm Biopharm. 2014;87(1):107–113. doi: 10.1016/j.ejpb.2013.12.016. [DOI] [PubMed] [Google Scholar]
- 162.Gadadare R, Mandpe L, Pokharkar V. Ultra rapidly dissolving repaglinide nanosized crystals prepared via bottom-up and top-down approach: influence of food on pharmacokinetics behavior. AAPS PharmSciTech. 2015;16(4):787–99. Int J Pharm. 2014;477(1):251–260. doi: 10.1208/s12249-014-0267-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Turcheniuk K, Trecazzi C, Deeleepojananan C, Mochalin VN. Salt-assisted ultrasonic deaggregation of nanodiamond. ACS Appl Mater Interfaces. 2016;8(38):25461–25468. doi: 10.1021/acsami.6b08311. [DOI] [PubMed] [Google Scholar]
- 164.Adebisi AO, Kaialy W, Hussain T, Al-Hamidi H, Nokhodchi A, Conway BR, et al. An assessment of triboelectrification effects on co-ground solid dispersions of carbamazepine. Powder Technol. 2016;292:342–350. doi: 10.1016/j.powtec.2016.02.008. [DOI] [Google Scholar]
- 165.Al-Hamidi H, Asare-Addo K, Desai S, Kitson M, Nokhodchi A. The dissolution and solid-state behaviours of coground ibuprofen–glucosamine HCl. Drug Dev Ind Pharm. 2015;41(10):1682–1692. doi: 10.3109/03639045.2014.991401. [DOI] [PubMed] [Google Scholar]
- 166.Penkina A, Semjonov K, Hakola M, Vuorinen S, Repo T, Yliruusi J, et al. Towards improved solubility of poorly water-soluble drugs: cryogenic co-grinding of piroxicam with carrier polymers. Drug Dev Ind Pharm. 2016;42(3):378–388. doi: 10.3109/03639045.2015.1054400. [DOI] [PubMed] [Google Scholar]
- 167.Hong C, Dang Y, Lin G, Yao Y, Li G, Ji G, et al. Effects of stabilizing agents on the development of myricetin nanosuspension and its characterization: an in vitro and in vivo evaluation. Int J Pharm. 2014;477(1):251–260. doi: 10.1016/j.ijpharm.2014.10.044. [DOI] [PubMed] [Google Scholar]
- 168.Salaberria AM, Fernandes SC, Diaz RH, Labidi J. Processing of α-chitin nanofibers by dynamic high pressure homogenization: characterization and antifungal activity against a. Niger. Carbohydr Polym. 2015;116:286–291. doi: 10.1016/j.carbpol.2014.04.047. [DOI] [PubMed] [Google Scholar]
- 169.Sosnik A, Seremeta KP. Advantages and challenges of the spray-drying technology for the production of pure drug particles and drug-loaded polymeric carriers. Adv Colloid Interf Sci. 2015;223:40–54. doi: 10.1016/j.cis.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 170.Başaran E, Yenilmez E, Berkman MS, Büyükköroğlu G, Yazan Y. Chitosan nanoparticles for ocular delivery of cyclosporine a. J Microencapsul. 2014;31(1):49–57. doi: 10.3109/02652048.2013.805839. [DOI] [PubMed] [Google Scholar]
- 171.Mustapha O, Din F, Kim DW, Park JH, Woo KB, Lim S-J, et al. Novel piroxicam-loaded nanospheres generated by the electrospraying technique: physicochemical characterisation and oral bioavailability evaluation. J Microencapsul. 2016;33(4):323–330. doi: 10.1080/02652048.2016.1185475. [DOI] [PubMed] [Google Scholar]
- 172.Paisana MC, Müllers KC, Wahl MA, Pinto JF. Production and stabilization of olanzapine nanoparticles by rapid expansion of supercritical solutions (RESS) J Supercrit Fluids. 2016;109:124–133. doi: 10.1016/j.supflu.2015.11.012. [DOI] [Google Scholar]
- 173.Uchida H, Nishijima M, Sano K, Demoto K, Sakabe J, Shimoyama Y. Production of theophylline nanoparticles using rapid expansion of supercritical solutions with a solid cosolvent (RESS-SC) technique. J Supercrit Fluids. 2015;105:128–135. doi: 10.1016/j.supflu.2015.05.005. [DOI] [Google Scholar]
- 174.Prosapio V, Reverchon E, De Marco I. Antisolvent micronization of BSA using supercritical mixtures carbon dioxide+ organic solvent. J Supercrit Fluids. 2014;94:189–197. doi: 10.1016/j.supflu.2014.07.012. [DOI] [Google Scholar]
- 175.Campardelli R, Baldino L, Reverchon E. Supercritical fluids applications in nanomedicine. J Supercrit Fluids. 2015;101:193–214. doi: 10.1016/j.supflu.2015.01.030. [DOI] [Google Scholar]
- 176.Labuschagne P, Adami R, Liparoti S, Naidoo S, Swai H, Reverchon E. Preparation of rifampicin/poly (d, l-lactice) nanoparticles for sustained release by supercritical assisted atomization technique. J Supercrit Fluids. 2014;95:106–117. doi: 10.1016/j.supflu.2014.08.004. [DOI] [Google Scholar]
- 177.De Cicco F, Reverchon E, Adami R, Auriemma G, Russo P, Calabrese EC, et al. In situ forming antibacterial dextran blend hydrogel for wound dressing: SAA technology vs. spray drying. Carbohydr Polym. 2014;101:1216–1224. doi: 10.1016/j.carbpol.2013.10.067. [DOI] [PubMed] [Google Scholar]
- 178.Yang X, Liu X, Liu Z, Pu F, Ren J, Qu X. Near-infrared light-triggered, targeted drug delivery to cancer cells by Aptamer gated Nanovehicles. Adv Mater. 2012;24(21):2890–2895. doi: 10.1002/adma.201104797. [DOI] [PubMed] [Google Scholar]
- 179.Qin Y, Chen J, Bi Y, Xu X, Zhou H, Gao J, et al. Near-infrared light remote-controlled intracellular anti-cancer drug delivery using thermo/pH sensitive nanovehicle. Acta Biomater. 2015;17:201–209. doi: 10.1016/j.actbio.2015.01.026. [DOI] [PubMed] [Google Scholar]
- 180.Feng Q, Zhang Y, Zhang W, Hao Y, Wang Y, Zhang H, et al. Programmed near-infrared light-responsive drug delivery system for combined magnetic tumor-targeting magnetic resonance imaging and chemo-phototherapy. Acta Biomater. 2016;49:402–413. doi: 10.1016/j.actbio.2016.11.035. [DOI] [PubMed] [Google Scholar]
- 181.Feng Q, Zhang Y, Zhang W, Shan X, Yuan Y, Zhang H, et al. Tumor-targeted and multi-stimuli responsive drug delivery system for near-infrared light induced chemo-phototherapy and photoacoustic tomography. Acta Biomater. 2016;38:129–142. doi: 10.1016/j.actbio.2016.04.024. [DOI] [PubMed] [Google Scholar]
- 182.Wang X, Wang C, Zhang Q, Cheng Y. Near infrared light-responsive and injectable supramolecular hydrogels for on-demand drug delivery. Chem Commun. 2016;52(5):978–981. doi: 10.1039/C5CC08391E. [DOI] [PubMed] [Google Scholar]
- 183.Luo Z, Cai K, Hu Y, Zhao L, Liu P, Duan L, et al. Mesoporous silica nanoparticles end-capped with collagen: redox-responsive nanoreservoirs for targeted drug delivery. Angew Chem Int Ed. 2011;50(3):640–643. doi: 10.1002/anie.201005061. [DOI] [PubMed] [Google Scholar]
- 184.Chen X, Sun H, Hu J, Han X, Liu H, Hu Y. Transferrin gated Mesoporous silica Nanoparticles for Redox-responsive and targeted drug delivery. 2017. [DOI] [PubMed] [Google Scholar]
- 185.Zhang Q, Liu F, Nguyen KT, Ma X, Wang X, Xing B, et al. Multifunctional Mesoporous silica Nanoparticles for cancer-targeted and controlled drug delivery. Adv Funct Mater. 2012;22(24):5144–5156. doi: 10.1002/adfm.201201316. [DOI] [Google Scholar]
- 186.Zhang W, Wang F, Wang Y, Wang J, Yu Y, Guo S, et al. pH and near-infrared light dual-stimuli responsive drug delivery using DNA-conjugated gold nanorods for effective treatment of multidrug resistant cancer cells. J Control Release. 2016;232:9–19. doi: 10.1016/j.jconrel.2016.04.001. [DOI] [PubMed] [Google Scholar]
- 187.Huang L, Zhang Q, Dai L, Shen X, Chen W, Cai K (2017) Phenylboronic acid-modified hollow silica nanoparticles for dual-responsive delivery of doxorubicin for targeted tumor therapy. Regenerative Biomaterials:rbw045 [DOI] [PMC free article] [PubMed]
- 188.Dai L, Yu Y, Luo Z, Li M, Chen W, Shen X, et al. Photosensitizer enhanced disassembly of amphiphilic micelle for ROS-response targeted tumor therapy in vivo. Biomaterials. 2016;104:1–17. doi: 10.1016/j.biomaterials.2016.07.002. [DOI] [PubMed] [Google Scholar]
- 189.Zhou S, Wu D, Yin X, Jin X, Zhang X, Zheng S, et al. Intracellular pH-responsive and rituximab-conjugated mesoporous silica nanoparticles for targeted drug delivery to lymphoma B cells. J Exp Clin Cancer Res. 2017;36(1):24. doi: 10.1186/s13046-017-0492-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Liu T, Wang C, Gu X, Gong H, Cheng L, Shi X, et al. Drug delivery with PEGylated MoS2 Nano-sheets for combined Photothermal and chemotherapy of cancer. Adv Mater. 2014;26(21):3433–3440. doi: 10.1002/adma.201305256. [DOI] [PubMed] [Google Scholar]
- 191.Liu J, Detrembleur C, Pauw-Gillet D, Mornet S, Jérôme C, Duguet E. Gold Nanorods coated with Mesoporous silica Shell as drug delivery system for remote near infrared light-activated release and potential phototherapy. Small. 2015;11(19):2323–2332. doi: 10.1002/smll.201402145. [DOI] [PubMed] [Google Scholar]
- 192.Chen L, Wu L, Liu F, Qi X, Ge Y, Shen S. Azo-functionalized Fe 3 O 4 nanoparticles: a near-infrared light triggered drug delivery system for combined therapy of cancer with low toxicity. J Mater Chem B. 2016;4(21):3660–3669. doi: 10.1039/C5TB02704G. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Presented in the main paper.


