Abstract
Background
Illicit fentanyl use has become wide spread in the US, causing high rates of overdose deaths among people who use drugs. This study describes patterns and perceptions of fentanyl exposure among opioid users in Rhode Island.
Methods
A mixed methods study was conducted via questionnaire with a convenience sample of 149 individuals using illicit opioids or misusing prescription opioids in Rhode Island between January and November 2016. Of these, 121 knew of fentanyl and reported known or suspected exposure to fentanyl in the past year. Semi-structured interviews were conducted with the first 47 participants.
Results
Study participants were predominantly male (64%) and white (61%). Demographic variables were similar across sample strata. Heroin was the most frequently reported drug of choice (72%). Self-reported exposure to illicit fentanyl in the past year was common (50.4%, n=61). In multivariate models, regular (at least weekly) heroin use was independently associated with known or suspected fentanyl exposure in the past year (adjusted prevalence ratio (APR)=4.07, 95% CI: 1.24-13.3, p=0.020). In interviews, users described fentanyl as unpleasant, potentially deadly, and to be avoided. Participants reporting fentanyl exposure routinely experienced or encountered non-fatal overdose. Heroin users reported limited ability to identify fentanyl in their drugs. Harm reduction strategies used to protect themselves from fentanyl exposure and overdose, included test hits, seeking prescription opioids in lieu of heroin, and seeking treatment with combination buprenorphine/naloxone. Participants were often unsuccessful in accessing structured treatment programs.
Conclusion
Among illicit opioid users in Rhode Island, known or suspected fentanyl exposure is common, yet demand for fentanyl is low. Fentanyl-contaminated drugs are generating user interest in effective risk mitigation strategies, including treatment. Responses to the fentanyl epidemic should be informed by the perceptions and experiences of local users. The rapid scale-up of buprenorphine/naloxone provision may slow the rate of fentanyl-involved overdose deaths.
Keywords: fentanyl, mediation assisted treatment, overdose, heroin, drug use, qualitative methods
1. Background
“Well, I don't really know what it looks like.” David shifted awkwardly in his chair. He hedged his answers a few times, making an effort to separate what he knew firsthand and what he knew through rumor. He continued:
David: I've done, um, a couple of times I've done heroin, supposing it was heroin, where somebody said to me, ‘it's got fentanyl in it.’ The times I did those two, I did like that twice, and they told me, the people that sold it to me, it was like, I did it once and like six months later again, but it was the same deal, White, greyish, silky. And they said “be careful. It's got a lotta bodies on it.”
JC: A lot of bodies on it?
David: Meaning, like, yea, but when I did it I was like, “Whoa! What the heck kinda dope1 is this?” I never. I mean, it was like really potent. And from what I had been told through other people was like, “well, that's fentanyl.”
JC: What does “a lot of bodies on it” mean?
David: Oh. It's so strong it's killing people.
The use of illicit fentanyl, a synthetic opioid many times stronger than morphine (Volpe et al., 2011), among people who use drugs has become wide-spread in the last two years (United States Drug Enforcement Administration, 2016). As David describes, fentanyl has also become a significant factor in heroin-involved deaths (Rudd, Aleshire, Zibbell, & Gladden, 2016).
In the state of Rhode Island, located in the New England region of the United States, the rate of fentanyl-related overdose deaths more than doubled between 2013 and 2014, rising from 2.5 to 8.0 per 100,000 population (Mercado-Crespo, Sumner, Spelke, Sugerman, & Stanley, 2014; Rhode Island Governor's Overdose Prevention and Intervention Task Force, 2016). In 2015, Fentanyl was implicated in 122 of the 258 fatal overdoses—approximately 50% of all overdose deaths in the state (Rhode Island Governor's Overdose Prevention and Intervention Task Force, 2016). In response to this trend, the Rhode Island Governor's Overdose Prevention Task Force was formed in 2015 and tasked with identifying strategies for decreasing the rate of fatal overdose (Rhode Island Governor's Overdose Prevention and Intervention Task Force, 2015). A key element of the strategy recommended by the Task Force is increased access to buprenorphine/naloxone, partial opioid antagonist used in medication-assisted therapy (MAT), an effective treatment for opioid use disorder (Mauger, Fraser, & Gill, 2014) that effectively reduces drug-related harm and risk of overdose death (Otiashvili et al., 2013).
Despite fentanyl's significant impact on rates of overdose in Rhode Island, the effects of fentanyl exposure on perceptions of drug use-related risk and the variety of risk reduction strategies used by consumers of illicit or diverted opioids are not well understood. A recent study among young adults in the state who use prescription opioids non-medically found that 11% reported known or suspected fentanyl exposure through contaminated drugs in the past six months (Macmadu, Carroll, Hadland, Green, & Marshall, 2017), indicating that fentanyl is reaching a wide spectrum of opioid users in the region. However, without more knowledge about the local drug market and drug use behaviors in the context of pervasive fentanyl exposure, policy-makers are limited in their ability to identify andtarget the individuals at the greatest risk of overdose. To quell the current overdose epidemic, it is essential to identify those most at risk of fentanyl exposure and fentanyl-related overdose, as well as to identify effective points of intervention to increase access to and uptake of potentially life-saving tools likebuprenorphine/naloxone. In the present mixed methods study, we used convergent exploratory and explanatory methods (Fetters, Curry, & Creswell, 2013) to describe patterns of illicit fentanyl use and the characteristics, perspectives, and experiences of individuals exposed to fentanyl in Rhode Island.
2. Methods
2.1 Subject recruitment
Subject recruitment and data collection for this study took place between January and November 2016. Eligible participants met the following criteria: at least 18 years of age; current resident of Rhode Island; able to provide verbal consent; and self-reported misuse of opioids (this includes the use of illicit opioids; the use of diverted prescription opioids; or the deliberate misuse of opioids received through a prescription, often called self-diversion) in the previous 30 days. Participants were recruited through targeted canvassing at local needle exchange programs, harm reduction outreach programs, emergency departments, and community-based health clinics.
Recruitment took place with the assistance of medical and counseling staff at these partnering community organizations. Staff would reach out to clients they believed to qualify for this study either by phone or as those clients presented at their respective organizations for support and services. Clients would be invited to visit the organization or were recruited from organization grounds on a day when a researcher was present and available (and situated in a private space, like an exam room, away from contact with clients seeking direct services). Staff members would then personally introduce interested participants, at which point the staff would return to their post and the researcher would invite the potential participant to undergo the informed consent process in a private space temporarily allocated for this purpose. Consent was obtained verbally. The first 47 subjects were offered $20 for completing a written survey and participating in a semi-structured interview immediately following. The subsequently recruited participants in this study were offered $10 compensation for completing the written survey only.
2.2 Data Collection
All consenting participants completed an anonymous written survey designed to capture demographic information as well as information pertaining to substance use, prescription drug diversion, experience with overdose, access to naloxone, and access to treatment. The use of any substance more than once per week was considered “regular” use. Most items were derived from prior cross sectional studies (Bazazi, Yokell, Fu, Rich, & Zaller, 2011; Yokell, Green, Bowman, McKenzie, & Rich, 2011; Yokell, Zaller, Green, McKenzie, & Rich, 2012). Known or suspected exposure to fentanyl in the past year was measured according to self-report. Specifically, we asked participants whether they had (in the past year) knowingly or intentionally consumed fentanyl or if they held a strong belief that they had consumed fentanyl-contaminated drugs based on the physical sensation of the drugs or on information obtained from their supplier after the fact. A positive response to either of question was considered known or suspected fentanyl exposure. Additionally, participants were asked whether they had ever experienced a non-fatal overdose and, if yes, when their most recent overdose experience occurred. Using these measures, participants who reported experiencing a non-fatal overdose in the past year were identified and this binary variable used in our statistical analyses. All participants were given the option of completing the survey independently or having the survey administered verbally by the researcher.
The first 47 participants who completed this written survey also participated in a qualitative interview. A semi-structured interview guide was used to elicit personal histories with substance use, drug treatment, and overdose, as well as perceptions of and recent encounters with fentanyl and fentanyl-contaminated drugs. Interviews, which ranged from approximately fifteen minutes to fifty minutes in length, were audio-recorded and transcribed for analysis. Participants were encouraged to share personal experiences and offer their own insights into their choices related to opioid use and treatment seeking. All surveys and interviews were conducted in English [by J.C.]. Instruments are available by request from the first author.
2.3 Statistical Analysis
Descriptive statistics were generated for all demographic factors as well as patterns of substance use, incarceration, overdose, and treatment seeking. We calculated prevalence ratios (PRs) of demographic and behavioral variables to identify factors associated with known or suspected exposure to fentanyl in the past year. Due to the high prevalence of this outcome, a modified Poisson regression with robust standard errors was built to model correlates of exposure and adjust for potential confounders. Variables considered for inclusion in multivariate models were those associated at p<0.05 in univariate analysis. We included measures of recent rather than lifetime self-reported experiences when time-dependent data was available (i.e., in the case of non-fatal overdose or witnessing overdose). The age range and gender of participants were included as variables in all models. Statistical analysis was conducted with STATA® Data Analysis and Statistical Software version 14 software (College Station, TX).
2.4 Qualitative Data Analysis
Qualitative data was used to triangulate survey findings, clarify discrepancies, and generate a greater understanding of emerging trends and themes. Interview transcripts were analyzed [by J.C.] using a modified version of grounded analysis for generating social theory (Glaser & Strauss, 1967). Transcripts were read and free-coded in order to identify broad themes and narratives across interviews while those interviews were still being conducted. Qualitative analysis, therefore, began before quantitative data analysis was begun. This process also allowed for the generation, testing, and refinement of hypotheses regarding behavior patterns, social relationships, and shared risk perceptions throughout the data collection process. Identified themes were further explored after interviews had concluded through recursive coding exercises, which identified shared norms and values related to illicit fentanyl and other and patterns of substance use. The findings presented here were isolated in these final stages of analysis.
2.5 Human Subjects Approval
This research protocol was approved by the Institutional Review Board at the Miriam Hospital.
3. Results
3.1 Study population
A total of 149 participants were recruited into this study. Of these, 121 (81%) were aware of fentanyl as a potential contaminant in illegal drug supplies and were able to report whether they knew or strongly believed they had been exposed to fentanyl through illicit drugs in the past year. Demographic and behavioral characteristics for these 121 participants, according to reported fentanyl exposure, are described in Table 1. Fentanyl exposure was reported by 61 (50.4%) of these 121 participants. More than one-third of this subset were female (34% among those reporting exposure to fentanyl, 35% among those reporting no exposure), and more than two thirds were White (73% and 64% among those exposed and not exposed, respectively). Participants tended to be unemployed or on disability, with a minority employed part-time. Most study participants (79% of those exposed, 80% of those not exposed) had been previously incarcerated. Heroin was the most common drug of choice, used at least weekly by 75% of this subset. The rate of regular (at least weekly) heroin use was significantly higher (93%) among those with known or suspected fentanyl exposure in the past year than those who reported no exposure (56%).
Table 1. Characteristics of adult opioid users in Rhode Island, according to known or suspected fentanyl exposure, with unadjusted prevalence ratios (PR) for significant differences.
| Those with no known or suspected fentanyl use in the past year (N=60) | Those with known or suspected fentanyl use in the past year (N=61) | Unadjusted PR | 95% CI | |
|---|---|---|---|---|
|
| ||||
| n (%) | n (%) | |||
| Gender | (n=60) | (n=61) | ||
| Female | 21 (35) | 21 (34) | 0.99 | 0.68-1.43 |
| Age | (n=60) | (n=57) | ||
|
| ||||
| 18-30 yrs | 19 (32) | 12 (21) | Comparison group | -- |
| 31-45 yrs | 21 (35) | 29 (51) | 1.50 | 0.91-2.47 |
| 46 yrs or more | 20 (33) | 16 (29) | 1.15 | 0.65-2.04 |
| Race (participants could select more than one race) | (n=42) | (n=51) | ||
|
| ||||
| White or Caucasian | 27 (64) | 37 (73) | 1.37 | 0.95-1.99 |
| Black, African American, Haitian, or Cape Verdean | 3 (7) | 3 (6) | 0.89 | 0.39-2.01 |
| Other (includes First Nations, Asian, Asian American, Native Hawaiian, and Pacific Islander) | 15 (36) | 15 (29) | 0.85 | 0.56-1.30 |
| Ethnicity | (n=44) | (n=49) | ||
|
| ||||
| Hispanic | 12 (27) | 11 (22) | 0.88 | 0.55-1.42 |
| Employment Status | (n=58) | (n=61) | ||
|
| ||||
| Full-time | 2 (3) | 6 (10) | Comparison group | -- |
| Part-time | 8 (14) | 8 (13) | 0.67 | 0.35-1.25 |
| Disability | 14 (24) | 18 (30) | 0.75 | 0.45-1.24 |
| Unemployed | 34 (59) | 29 (48) | 0.61 | 0.38-0.99 |
| Education | (n=58) | (n=59) | ||
|
| ||||
| Did not complete high school | 21 (36) | 20 (34) | Comparison group | -- |
| High school graduate | 23 (40) | 22 (37) | 1.00 | 0.65-1.55 |
| Some college or college graduate | 14 (24) | 17 (29) | 1.10 | 0.46-2.60 |
| Incarceration | (n=60) | (n=61) | ||
|
| ||||
| Previously incarcerated | 48 (80) | 48 (79) | 0.96 | 0.63-1.47 |
| Drugs used regularly* | (n varies due to missing data) | (n varies due to missing data) | ||
|
| ||||
| Heroin | 32 (56) | 54 (93) | 4.55 | 1.81-11.47‡ |
| Prescription opioids | 30 (56) | 10 (17) | 0.38 | 0.21-0.66‡ |
| Cocaine | 17 (30) | 21 (34) | 1.11 | 0.77-1.58 |
| Benzodiazepines | 18 (32) | 12 (20) | 0.72 | 0.45-1.16 |
| Amphetamines | 1 (2) | 2 (3) | 1.30 | 0.57-2.95 |
| Alcohol | 8 (14) | 7 (11) | 0.89 | 0.50-1.58 |
| Buprenorphine | 7 (15) | 10 (19) | 1.14 | 0.73-1.78 |
| Methadone | 8 (17) | 8 (15) | 0.94 | 0.56-1.60 |
| Frequency of opioid use | (n=59) | (n=57) | ||
|
| ||||
| Daily | 38 (63) | 38 (67) | Comparison group | -- |
| 5-6 times/wk | 6 (10) | 6 (11) | 0.90 | 0.51-1.61 |
| 3-4 times/wk | 5 (8) | 5 (9) | 0.64 | 0.31-1.31 |
| 1-2 times/wk | 5 (8) | 5 (9) | 0.43 | 0.20-0.95‡ |
| Less than weekly | 3 (5) | 3 (5) | 0.50 | 0.19-1.31 |
| Medication-assisted Treatment | (n varies due to missing data) | (n varies due to missing data) | ||
|
| ||||
| Past or current experience with MAT | 30 (50) | 46 (75) | 1.82 | 1.16-2.85‡ |
| Is currently receiving methadone maintenance treatment (MMT) | 1 (18) | 15 (25) | 0.94 | 0.63-1.38 |
| Is currently receiving buprenorphine/naloxone by prescription | 3 (5) | 3 (5) | 0.81 | 0.36-1.85 |
| Has sought a buprenorphine/naloxone prescriber in the past year | 11 (18) | 20 (33) | 1.44 | 1.01-2.03 |
| Overdose | (n varies due to missing data) | (n varies due to missing data) | ||
|
| ||||
| Has ever experienced (and survived) an overdose | 20 (39) | 39 (70) | 1.87 | 1.22-2.85‡ |
| Has experienced (and survived) an overdose in the past year | 8 (17) | 26 (51) | 1.99 | 1.39-2.85‡ |
| Has ever witnessed someone else overdose | 48 (84) | 55 (93) | 1.74 | 0.75-4.00 |
| Has witnessed someone else overdose in the past year | 23 (49) | 38 (73) | 1.69 | 1.07-2.68† |
| Has administered naloxone to reverse someone else's overdose | 16 (28) | 23 (40) | 1.30 | 0.91-1.86 |
| Average number of overdoses witnessed | 4.0 (IQR**=4) | 4.2 (IQR=4) | -- | -- |
Participants were asked to report substances they used at least weekly.
Interquartile range
p<0.05
p<0.01
Many participants in this study had personally experienced at least one non-fatal overdose. Lifetime history of non-fatal overdose was significantly higher in those reporting fentanyl exposure (70%) than those reporting no exposure (39%), as was non-fatal overdose within the past 12 months (51% and 17%, respectively). Participants reported having been a bystander during an overdose with similar frequency regardless of their history of fentanyl exposure. Those exposed to fentanyl and not exposed to fentanyl reported witnessing a lifetime average of 4.2 and 4.0 unintentional overdoses, respectively (interquartile range for both groups=4). Treatment seeking was also relatively common among our study population, 33% of those exposed and 18% of those not exposed to fentanyl reported that they actively sought a licensed buprenorphine/naloxone prescriber in the past year.
3.3 Statistical Analyses: Correlates and Predictors of Known or Suspected Fentanyl Exposure
In bivariate analyses (Table 1), exposure to fentanyl was positively associated with regular heroin use (PR=4.55, 95% CI: 1.81-11.5) and lifetime experience with MAT (PR=1.82, 95% CI: 1.16-2.85). Recent overdose experience was also significantly associated with fentanyl exposure. Those exposed to fentanyl in the past year were more likely to have witnessed an overdose in the past year (PR=1.69, 95% CI: 1.07-2.68) and more likely to have experienced a non-fatal overdose (PR=1.99, 95% CI: 1.39-2.85) in the past year. Fentanyl exposure was negatively associated with regular use of diverted or self-diverted prescription opioids (PR=0.38, 95% CI: 0.21-0.66).
In the multivariable regression analysis (Table 2), we included the following variables based on their significance in unadjusted bivariate analyses: past or current experience with MAT; regular heroin use; regular prescription opioid use; experiencing non-fatal overdose within the past year; witnessing an overdose in the past year. Lifetime overdose experience was not included, as recent overdose experience was already included in the model. We expected to find collinearity between experiencing a recent overdose and witnessing a recent overdose and, therefore, subjected these variables to a chi-squared test. These variables were not found to be significantly correlated in our dataset (p=0.69). We also completed additional regression analyses, in which we included excluded one or the other of these variables. In each analysis, our findings were consistent. In the final model, adjusted for age and gender, only regular heroin use was independently associated with known or suspected exposure to fentanyl in the past year (adjusted prevalence ratio (APR)=4.07, 95% CI: 1.24-13.3, p=0.020).
Table 2.
Adjusted prevalence ratios (APR) for factors associated with known or suspected fentanyl exposure, adjusted for age and gender.
| Known or suspected exposure to fentanyl in past year (n=121) | |||
|---|---|---|---|
|
| |||
| Behavior or Experience | APR | 95% CI | p |
| Regular heroin use | 4.07 | 1.24-13.3 | 0.020 |
| Regular painkiller use | 0.73 | 0.37-1.49 | 0.372 |
| Current or past experience with MAT | 1.13 | 0.70-1.84 | 0.612 |
| Experiencing an overdose in the past 12mo | 1.29 | 0.87-1.92 | 0.208 |
| Witnessing someone else overdose in the past 12mo | 1.11 | 0.69-1.90 | 0.692 |
MAT = medication assisted treatment
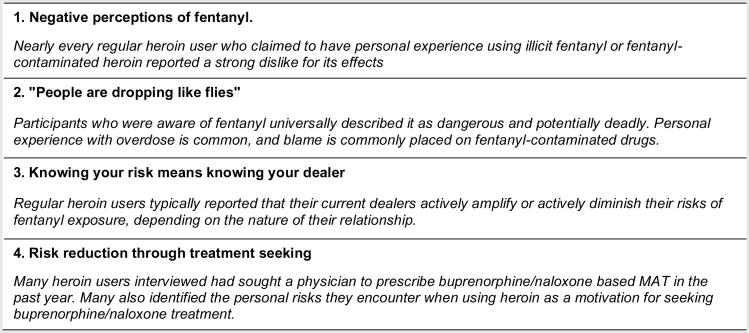
3.4 Qualitative Finding: Negative Perceptions of Fentanyl
In interviews, nearly every regular heroin user who claimed to have personal experience using illicit fentanyl or fentanyl-contaminated heroin reported a strong dislike for its effects (see Figure 1 for a summary of all qualitative findings presented here). Rather than the soft, droopy “nod” that they have come to expect from pure heroin, users described uncomfortable “tingling” and “pins and needles” sensations in their faces and extremities when injecting heroin they knew or believed to contain fentanyl. Users also characterized fentanyl as much stronger in effect than heroin—stronger but not necessarily better. Many theatrically expressed the speed of onset and severity of its physical and neurological effects. Sheryl, a middle aged woman who is financially supported by her partner, described the effects in these words:
I could tell, uh, I could tell it was different…It just went like, whoa, right to the head, like, whoa, like, I need to grab something and hold on you know? So that's how we suspected the fentanyl and it was like, she [another person who buys from our dealer] had gone out also.
Figure 1.
A summary of major findings from qualitative interviews.
Others mimed desperate lurches for the coffee table, pretending to knock over furniture, and falling to the floor with booms, whooshes, and other illustrative sound effects that often defied transcription.
Opinions among regular users varied as to whether fentanyl-contaminated heroin is sufficient to keep withdrawal symptoms at bay, but a general consensus emerged that the effects of fentanyl are distinctly uncomfortable or distressing, even when it is simply being used to relieve the discomfort of withdrawal. Dan, a daily heroin user in his sixties, described his most recent encounter with what he suspects is fentanyl-contaminated heroin as frightening and very unexpected:
I don't do a lot first of all, and I did, you know like, my normal. I did half a bag. And I went out [lost consciousness]. I was out, I, like I said, I came through, the needle was in my arm, my head was inside my drawer, and I didn't know where I was. I was inside my apartment but I didn't know where I was for like five minutes after I came out. It had to be the dope. It had to be the heroin.
After this incident, Charlie only buys heroin from the dealer he trusts and never considers buying from anyone else. “If he doesn't take care of me,” he said, “I go through the sickness. I go through the sickness. I don't want to die. I don't want to die, you know. I don't want to die.”
Some participants reported that it may be possible to identify fentanyl-contaminated heroin by sight or by smell. Sheryl said she often suspects heroin to be fentanyl-contaminated when it looks white. “The dope's a different color than—heroin's tan usually,” she said. “When it's a little more white that's the cut they put in it. Or it's got some fentanyl in it.” Other participants described fentanyl-contaminated heroin as white, grey, pink, clear, silvery, or of an a-typical appearance when cooked and drawn into the needle. A few reported that fentanyl-contaminated heroin lacked the distinct, acidic odor of pure heroin, providing instead a neutral, powdery smell. Carl, a man in his thirties from a suburb of Providence, described this feature as key to identifying pure heroin. “I try to smell the vinegar—the vinegary smell,” he said. “If there's a vinegary smell you know that's dope. Fentanyl doesn't have a smell when you sniff it. It tastes like you're sniffing Tylenol. But then you're destroyed afterwards.”
Even though many heroin users often relied on this informal system to identify fentanyl in their drugs, the avoidance of fentanyl-contaminated heroin was consistently described as difficult or impossible to achieve. This point was made spontaneously by Jeff, a young man in his mid twenties, as he explained his preference for pure black tar heroin, which he maintains is less likely to be fentanyl-contaminated, and his belief in the inevitability of fentanyl contamination in powder heroin:
Black tar heroin I feel safer doing, It's harder to cut. It's not powder. Powder you can add anything to…Black tar heroin, in order to cut it, you have to do all this stuff to it, cook it, and it's a lot harder to cut, so I feel safer doing that. But as far as fentanyl? There's no way to know until you [use] it. Like I said, I avoid the grey dope, but there's nothing you can really do [to avoid it].
Even Sheryl, who claimed a particular skill for spotting fentanyl-contaminated heroin by its color, admitted that she, too, was often hard pressed to tell what she was injecting. “No. No. You can't tell,” she said. “When you draw it up into the needle—nope. Can't even tell.”
Some participants reported that they typically choose to inject heroin they suspected to contain fentanyl, but that they would do so in a more controlled and systematic manner. Daniel, a man well past retirement age living with family in central Providence, described his approach:
If I don't know the guy, and I don't know the material, know what I'm saying, I would take it—I would test it with my finger. You know. Taste it. I put the water in, I put the heat to it, I see how it reacts, know what I'm sayin'? Then I would taste [inject] a little bit again, know what I'm sayin', and see if it's got a strong taste to it, you know. And then I wouldn't do the whole bag. I would do half a bag, know what I'm sayin'? Just to see how I felt when I shoot it, and I see what my reaction is, you know?
This sentiment was echoed by Jason, a regular heroin user from the north end of the state, when he was asked how he decided whether to use fentanyl-contaminated heroin:
[It depends on] the availability of other batches and how sick I am. If I'm sick, I gotta do it, you know? I won't do half a gram. You know, I'll do a little pinch and I'll figure it out from there, but I won't start big. I'll start a little and figure it out. It's scary. I've watched overdoses. And I've had one in front of my girl.
As Jason's statement illustrates, when users find themselves deciding whether or not to use fentanyl-contaminated heroin, risking an overdose becomes easier to accept or to narrativize as a reasonable choice when the alternative scenario—experiencing physical withdrawal symptoms— is all but guaranteed. Yet, many do make conscious changes in their use patterns when their suspicions of fentanyl-contamination are piqued.
3.5 Qualitative Finding: “People are Dropping Like Flies”
Participants who were aware of fentanyl universally described it as dangerous and potentially deadly. Chris, a parolee in his late thirties, was familiar with the dangers of fentanyl despite being released from jail and back in his community for less than two months. He said, “I know that people are dying off it. That people who shoot, who do injections, are ODing.” Chris was not alone in his recognition that heroin users are at higher risk of encountering fentanyl. Elise, a young woman who works part-time at a fast food restaurant, believed that she had never encountered fentanyl herself and was confident that her choice to use prescription opioids in lieu of heroin had lowered her risk of fentanyl exposure:
I used to take just the pills, and then I started doing dope, the heroin, only when I could get it, when it was cheaper. But I don't prefer it because you never know what you're getting. It's scary, so I'm more into pills.
It was also commonly accepted that heroin injectors were at greater risk of fentanyl-related injury or overdose than those who consume heroin by smoking or snorting. Matt, a young man in his twenties from western Rhode Island, said he prefers to snort heroin instead of injecting. He believes that this form of heroin consumption carries minimal risk of fentanyl-related overdose, especially compared to intravenous use:
Like, I've seen people OD in front of me from shooting the stuff [fentanyl]. I sniff it…I'm afraid, I have a very addictive personality so I'm afraid to shoot it. I'm afraid I'll like it. I know based on the people that I know what I know about fentanyl. It's mostly affecting the shooters because they're used to getting certain bags and [instead] they're getting fentanyl and they're shooting the same amount and just dying instantly. It's scary.
These avoidance strategies were mentioned by a minority of interviewed participants; the logic that participants gave for using alternatives to heroin or heroin injection was consistently linked to reducing individual risk of overdose.
A number of participants in this study reported recent incidents in which friends and significant others collapsed or stopped breathing within minutes of injection—an unusual occurrence when injecting pure heroin. Especially sobering was how frequently regular heroin users interviewed could name someone close to them who had recently died from an overdose. Many younger interviewees had cultivated their heroin use over time in the context of a tight-knit social group—often childhood friends. In such intimate cohorts, the impact of fentanyl overdose was felt very personally. In Matt's words, “People are dropping like flies. I've had three friends I grew up with since I was ten, they're all dead from [heroin cut with fentanyl].” Elise, the young woman who tries to avoid fentanyl by sticking to pills, had lost five close friends to fentanyl by the time of our interview in January 2016.
Many heroin users also appeared to have internalized the blame for deaths of friends and loved ones. This self-blame was powerfully demonstrated by Maggie, a woman in her early forties, as she recounted the events leading up to her boyfriend's recent death from a fentanyl-related overdose:
Maggie: Somebody that I was seeing overdosed and died on me, and I found him in the back of a restaurant over here on Howard St. And I think I might be allergic to it because I get really itchy, and I get blotches everywhere, and I get all swollen up. I don't know if it's that or if it—I think it's the fentanyl. It's definitely the fentanyl….We got into an argument. I was fifteen feet away from him. There was four of us. We each did half a gram. I walked over and he was in the same position. And I sat down on a bucket. I flipped it over and sat down. I called him a pain in the ass, or an asshole. And I kicked him in his ass and he rolled over. That's how I knew he was dead. I wouldn't have even known if I hadn't done that.
JC: About how long ago was that?
Maggie: January
JC: And how are they now?
Maggie: He's dead. He must have OD'd in that 15 minutes. I tried giving him mouth to mouth and all that stuff, and it didn't work.
JC: Was 911 called?
Maggie: They came. They tried to bring him back and they couldn't…The four of us used together. And we got into an argument and I walked away from him. He was perfectly fine. He showed no signs. But you can overdose five minutes after. After five minutes, you're basically cool. You know, but up to five—I always watch everybody for at least five minutes. I usually watch everybody for at least ten, because I don't trust the five-minute rule. After ten to fifteen minutes, you're probably alright. If you're gonna go, you'll go pretty fast.
JC: Is that a popular rule, the five-minute rule?
Maggie: For me. I'm anal like that. I have to watch everybody now. I get nervous about everybody. Usually I won't buy for anybody. Cause I don't want anything to happen. I feel like a douchebag.
JC: Why does that make you a douchebag?
Maggie: If they die? Because I bought it for them?
JC: Wouldn't they have gotten it from somewhere else?
Maggie: I don't care where else they get it from. As long as it didn't come from me.
Despite her stated confidence that fentanyl, cut into the heroin they were using without their knowledge, is what killed her boyfriend, and despite the fact that her boyfriend chose freely to use the heroin they had purchased, Maggie's words and demeanor during her interview indicated that she assigns much the blame for his death to herself and her alleged carelessness in walking away from her boyfriend rather than staying near and watching him closely. Maggie seemed to be admonishing herself for previously lacking the discipline or responsibility that she now champions.
3.6 Qualitative Finding: Knowing Your Risk Means Knowing Your Dealer
In interviews, regular heroin users were divided as to whether their current dealers actively amplified or actively diminished their risks of fentanyl exposure. Some reported very positive and sometimes long-standing relationships with a single dealer, which was often described as a source of protection against fentanyl. Tracy, a professional in her early thirties who uses heroin daily, offered a typical explanation:
My guys, they don't really want to mess with anybody like that, like, their main guy—if they have it, they don't want it. We deal with two people and they want nothing to do with it…you know, they don't want people dropping on them, to get involved in something like that…And I'm not, like, out on the street buying it from random people either. I know what I'm buying. So, that's kinda how. I don't go through any new people. I don't like chancing that.
Matt also reported that he was typically informed as to the presence of fentanyl in the heroin he purchased to snort, a privilege he attributed to his long-standing friendship with the people who sell to him. “Not every dealer will [tell you]. I know a couple of dealers I've been friends with [since before we started using] and they let me know if it's heroin or not …But most of the time people don't want fentanyl, so if they have it, they're not gonna tell you.” Sheryl reported that her primary dealer discovered he was selling fentanyl-contaminated heroin when one of his clients suffered a fentanyl overdose. Her death made the nightly news, and Sheryl's dealer called her right away to tell her that his heroin apparently contained fentanyl and she should throw out any heroin she hadn't already used.
Others felt their dealers directly contributed to their risk of fentanyl exposure. These interviewees described the economic motivations for selling heroin as able to outweigh any ethical concern dealers might have for customer safety. As Aaron, an experienced user in his sixties, put it: “A lot of people like to say they don't have [fentanyl] in [their heroin]. And you can't go by what they say, cause they'll sell rat poison if they can make their money. They're liable to tell you anything.” Some also argued that dealers are incentivized to lie by the fact that demand for heroin grossly exceeds the supply. “Why should they care [if you overdose on fentanyl]?” complained Eric, a man in his late fifties. “There's more [customers] coming. One passes away, two more comes.” Maggie, the woman who had witnessed her boyfriend's fatal overdose just a few weeks before her interview, shared especially pointed words on this topic:
Maggie: I don't think [dealers] give a fuck.
JC: What makes you say that?
Maggie: Cause it's not really about that. It's about the money.
JC: What else would it be about?
Maggie: That's it. Money.
JC: No one's afraid of their clients dying off?
Maggie: Not really. When it all boils down to it, no.
3.7 Qualitative Finding: Risk Reduction Through Treatment Seeking
Many of the heroin users interviewed for this study had sought a physician to prescribe bupernorphone/naloxone-based MAT in the past year. Often, participants chose to seek this form of treatment either they have experience this combination buprenorphine/naloxone therapy and had positive views of its effect or because they prefer the freedom of prescription, primary care-based buprenorphine/naloxone to the supervised consumption protocols that define methadone-based MAT programs. Derek, a young man in his 20s who lives with family, said:
[Staff at the methadone clinic I used to go to] asked me if I wanted to come back when I left [prison, a few months ago]. I said no. Cause it's liquid. It can't go anywhere. I can't go to Foxwoods [a local casino] for the night, get a hotel room. I have to go to the clinic in the morning. Now that I've been using I've actually been considering Suboxone [a brand-name buprenorphine/naloxone formulation], because it's a prescription, and I've taken Suboxone illegally, and I've found that I've done very, very well on it. So, I'm looking for a Suboxone provider.
Many participants identified the personal risks they encounter when using heroin as a motivation for seeking buprenorphine/naloxone treatment. At the time of his interview, Daniel felt ready to enter a treatment program, and his thinking was typical of many interviewees:
The danger of it, the money, you know what I'm sayin', the chasin'…I wanted to stop doin' it. I want to stop doin' it now, but I need to get on a program. I'm tryin' to find a Suboxone provider. You know any?
Some explicitly described a frightening encounter with fentanyl as directly responsible for their treatment seeking behaviors. Sam, a self-described “transient” in his late fifties, experienced a near-fatal overdose from fentanyl-contaminated heroin in the past year, which inspired him to give treatment a try:
I overdosed. If my friend didn't have the [naloxone], I'd have died…it was the fentanyl in it, you know? It's dangerous. So after that I went to detox, I went to [a clinic] to try to get clean. And I did it. I was on Suboxones. That lasted about, oh, almost five weeks.
Though he experienced a relapse shortly after beginning treatment, Sam continues to contemplate returning for another treatment attempt.
Many participants who sought buprenorphine/naloxone treatment in the past year experienced significant barriers to this form of care. Some were unable to find a buprenorphine/naloxone prescriber with the capacity to prescribe to new patients. Joshua, who is in his late twenties, had experienced repeated failures in his attempts to access treatment:
I've been calling around and getting “we're not taking new patients right now, we're not taking new patients: at every office I'm calling. So any leads I can get I'm calling every doctor as soon as I can, because it's exhausting buying [buprenorphine/naloxone] off the street, because they are like five dollars a piece on the street, and then some people want to charge eight dollars, and when you're taking two or three of those a day it adds up and, you know, let's just face it, when you're not making good money at the time or if you've got too many bills, you know, it's like being a junkie all over again. It's difficult. I would like for that burden to be lifted off my chest.
Others encountered difficulties with their health insurance, such as prior authorization requirements or poor treatment coverage, which caused substantial delays in their entry into care. Carlos, a middle-aged man from the south side of Providence, experienced such delays. “I talked to my doctor,” he said, “and I told him I want Suboxone, but [he said] I have to wait a month because my insurance, they don't cover it, you know?” Carlos eventually became frustrated and quit trying to access treatment. He continues to inject heroin. He, too, has experienced a fentanyl-related overdose in the past year.
4. Discussion
This mixed methods study explored patterns and perceptions of fentanyl exposure among users of illicit opioids in Rhode Island. Our quantitative analysis found that fentanyl is prevalent in the local drug supply and that regular heroin use was independently associated with known or suspected fentanyl exposure in the past year, suggesting that the risk of fentanyl exposure is determined by the nature of the product supplies that are available for users to purchase, not by any influence rooted in age, race, gender, or other socio-cultural associations that may influence consumer preference. Qualitative data from interviews indicate that fentanyl exposure has led to frequent, often fatal overdose within the heroin using community and has spurred heightened levels of perceived risk. High perceived risk of fentanyl is, in turn, motivating active users to develop novel strategies for minimizing the individual risks of fentanyl-contaminated heroin. Purported risk minimization strategies identified in this study that are worthy of examination in future studies include: (1) learning the visual and olfactory characteristics of contaminated heroin; (2) taking test hits to determine the strength of suspicious products; (3) taking turns or having one person observe others use the drug and wait 5 to 10 minutes to enable a response; (4) continuing to or reverting back to misuse prescription opioid products in lieu of heroin; (5) consciously deciding to snort instead of inject drugs; (5) maintaining long-term relationships with trusted dealers, who may test their product prior to sale; and (6) seeking medication-assisted treatment with buprenorphine/naloxone. Despite very good access to naloxone through pharmacies, community based programs, prison and emergency department based programs in the state, we note that none of the interviewees spontaneously or mentioned getting, carrying, stockpiling, or using naloxone as a risk reduction technique to protect against fentanyl.
Qualitative results from this study indicate that the majority of interviewees consider fentanyl highly undesirable. Awareness of high rates of fentanyl-related fatal overdose appear to be altering behaviors related to drug use, as people become accustomed to the new lethal drug supply. Interview data support a behavior change hypothesis, with many having expressed great fear of overdose and voicing their preference to avoid fentanyl whenever possible. This finding differs from those of a 2007 study conducted in Toronto, which found fentanyl to be highly desired among illicit drug users (Firestone, Goldman, & Fischer, 2009). However, opioid users surveyed in the Toronto study were consuming diverted, prescription-grade fentanyl. Heroin users in Rhode Island are encountering illicitly made fentanyl and fentanyl analogs produced in clandestine labs, not the medical-grade drug (Mercado-Crespo et al., 2014). There is some evidence that chronic users of illicit or diverted opioids may prefer the physical effects of fentanyl to those of pure heroin (Comer, Sullivan, Whittington, Vosburg, & Kowalczyk, 2008; Greenwald, 2008), and may seek it out (Macmadu et al., 2017); however, with no drug quality information available to opioid consumers and a high local prevalence of fentanyl-related overdose, perceived desirability of fentanyl in Rhode Island currently appears low.
This finding is especially important in light of recent trends that have characterized official statements and, subsequently, media coverage of the fentanyl-related overdose crisis across New England (the region of the US to the north and east of New York state). Such statements have increasingly supported the narrative that the prevalence of fentanyl in the illicit drug market and the high rates of fentanyl-related overdose are caused by high user demand for this drug. Below is a representative sample of direct quotes taken from local law enforcement officers and federal agents in New England, printed in local media:
“The users know they could die…They're chasing the dragon. They're looking for the ultimate high.” Worchester Telegram, 2014 (Petrishen, 2014)
“Heroin cut with fentanyl gives the user a more intense high. In an addict's world they want that ultimate high, taking them right to the edge,” EastBayRI.com, 2016 (Rego, 2016)
“The users know that they could die from taking this heroin, but yet they want the ultimate high.” New Haven Register, 2016 (Flynn, 2016)
“I think they're thinking they have a chance to get the ultimate high,” WTNH Connecticut News, 2016 (Slater, 2016)
Our findings directly contradict this narrative on multiple fronts. First, our quantitative analysis found regular heroin use to be an independent predictor of fentanyl-exposure, which suggests a special vulnerability to illicit fentanyl among those who inject or snort heroin independent of consumer preference; second, most interviewed heroin users overwhelmingly indicated that they prefer to avoid fentanyl-contaminated heroin whenever possible; and, third, when they do encounter fentanyl-contaminated heroin, many users report greatly disliking and often fearing the unpredictability of its effects. Importantly, these findings mirror those of other studies conducted in urban centers across North America, which found supply-side forces to be responsible for waves of fentanyl-related overdose in New Jersey, US (Hempstead & Yildirim, 2014) and that nearly three out of four illicit opioid users exposed to fentanyl in Vancouver, Canada, were unaware of their own exposure (Amlani et al., 2015).
Acknowledging the fentanyl-related overdose crisis in Rhode Island as a largely (if not exclusively) supply-side phenomenon bears significant local policy implications. Primary among these is the conclusion that user education about the presence of fentanyl in the drug supply and the potentially lethal effects of consumption will be insufficient to reduce users' risk of overdose so long as they are unable to control whether fentanyl is in the drugs they purchase. In light of significant evidence that fentanyl-associated overdose is characterized by sudden onset, rapid progression to death, and atypical presentation (Somerville et al., 2017), a more effective overdose prevention strategy might be the integration of fentanyl-specific content into standard trainings for overdose response and reversal with naloxone. Second, while increased policing of drug retailers (a standard strategy for supply reduction) may result in the seizure of certain batches of fentanyl-contaminated drugs from circulation, detailed knowledge of the social networks that make up the local heroin market would likely be needed to assess how effectively police operations are able to target the multiple sources that place fentanyl into circulation. Furthermore, some heroin users stated that their dealers actively protect them from fentanyl exposure. If these statements are accurate, placing those dealers under arrest may put their clients directly at risk of fentanyl exposure, as they are now forced to purchase drugs from a new, less familiar, less trusted seller. This indicates that it may well be time for new approaches to reducing the risk in the drug supply, including supplier-based risk reduction (as opposed to public safety) interventions (Greenfield & Paoli, 2017; Latkin, Yang, Tobin, & German, 2013), drug checking services (Quintana et al., 2017), or the adaptation of anonymous notification services for those connected by dealer networks (Huffam et al., 2013; Tan et al., 2016), as current practices aimed at supply reduction may exacerbate opioid-related risks to public health and public safety at the local level.
Though people exposed to fentanyl are at extremely high risk for fatal overdose, this study has evidenced that demand for treatment in Rhode Island's opioid using and fentanyl-exposed population is high. This finding is of central importance for overdose prevention efforts, as growth in the number of opioid users enrolled in buprenorphine-based MAT programs has been associated with significantly reduced rates of heroin overdose in the city of Baltimore (Schwartz et al., 2013) and in France (Auriacombe, Fatséas, Dubernet, Daulouède, & Tignol, 2004). Given the demonstrated life-saving effects of buprenorphine/naloxone treatment, the frequency of reports made by participants in this study of difficulty locating a buprenorphine/naloxone prescriber is distressing. Unfortunately, this finding mirrors nation-wide discrepancies between need for and availability of MAT, as reported by others (Jones, Campopiano, Baldwin, & McCance-Katz, 2015). Therefore, significant local investments in increasing the availability of and ease of access to MAT—and especially to buprenorphine/naloxone—is essential for maximizing the life-saving benefits of these treatment options and lowering the burden of fatal opioid overdose among opioid users. Effective emergency-department based (D'Onofrio et al., 2015) and prison-based models (Lee & Rich, 2012; Nunn et al., 2009; Rich et al., 2015) of MAT induction are emerging from the research literature, and could be optimized to address unmet needs of extremely high risk populations at times of high relapse and overdose risk.
Several limitations should be taken into account when interpreting these results. Broader application of these findings to illicit or diverted opioid users beyond Rhode Island may not be appropriate. Fewer than 150 illicit or diverted opioid users participated in this study; as well, the true prevalence of fentanyl in Rhode Island's heroin supply is not known. Future research should test identified correlations in larger study populations and augment those findings with forensic lab or other test data from street-obtained samples of the local drug supply. Additionally, this study did not capture the outcomes of participants' reported treatment seeking behaviors. As with all cross-sectional studies, the chronology of exposure and outcome development is not entirely clear, although qualitative interviews help to clarify some of the motivations for patterns of opioid use, treatment seeking, and other observed behaviors. Further research is needed to validate the hypotheses for causality identified in our data. We note that participants from this study were recruited from direct-service points or by recommendation from staff at those organizations and that participants were overwhelmingly unemployed or underemployed. Thus, findings may not be generalizable to illicit or diverted opioid users who are not interfacing with community organizations or those who are of a higher socio-economic status.
5. Conclusions
This study indicates that fentanyl is pervasive in the local drug supply. At the same time, user demand for fentanyl appears remarkably low. Local drug users are keenly aware of fentanyl's presence in local heroin and are aware that fentanyl poses a high risk of fatal overdose. Overdose reduction strategies implemented at the state and community levels will have the greatest impact if they take the perceptions and behaviors of local drug users into account and develop interventions that capitalize on the individual risk reduction strategies with which users already engage. Demand for treatment in Rhode Island's opioid using population is high, yet access to MAT and other forms of potentially life-saving care is inadequate. Increasing the availability of and ease of access to MAT—and especially to buprenorphine/naloxone—is an essential step for lowering the burden of fatal opioid overdose in Rhode Island and elsewhere.
Acknowledgments
Funding for this study was provided by CVS Health for the Rhode Island Governors Task Force on Overdose and Addiction. This research has been facilitated in part by the infrastructure and resources provided by the Lifespan/Tufts/Brown Center for AIDS research, an NIH funded program, grant number P30-AI-42853, from the National Institutes of Health, Center for AIDS Research. This research was supported by the National Institute on Drug Abuse (Award Numbers T32 DA013911 and K24 DA022112), the Agency for Healthcare Research and Quality (Award Number R18 HS024021), and a Henry Merrit Wriston Fellowship from Brown University.
We would like to acknowledge and thank Mariya Bachmaha, Alexandra Macmadu, and Cassandra Sutten-Coates for their research assistance.
Footnotes
“Dope” is a slang term used in Rhode Island (and elsewhere) to refer to heroin.
Declarations of interests: We have no conflicts of interest to declare.
Conflict of Interest Statement: We have no competing interests to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Amlani A, McKee G, Khamis N, Raghukumar G, Tsang E, Buxton JA. Why the FUSS (Fentanyl Urine Screen Study)? A cross-sectional survey to characterize an emerging threat to people who use drugs in British Columbia, Canada. Harm Reduction Journal. 2015;12:54. doi: 10.1186/s12954-015-0088-4. https://doi.org/10.1186/s12954-015-0088-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auriacombe M, Fatséas M, Dubernet J, Daulouède JP, Tignol J. French field experience with buprenorphine. The American Journal on Addictions. 2004;13 Suppl 1:S17–28. doi: 10.1080/10550490490440780. https://doi.org/10.1080/10550490490440780. [DOI] [PubMed] [Google Scholar]
- Bazazi AR, Yokell M, Fu JJ, Rich JD, Zaller ND. Illicit use of buprenorphine/naloxone among injecting and noninjecting opioid users. Journal of Addiction Medicine. 2011;5;3:175–180. doi: 10.1097/ADM.0b013e3182034e31. https://doi.org/10.1097/ADM.0b013e3182034e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer SD, Sullivan MA, Whittington RA, Vosburg SK, Kowalczyk WJ. Relative abuse liability of prescription opioids compared to heroin in morphine-maintained heroin abusers. Neuropsychopharmacology: Official Publication of the American College of Neuropsychopharmacology. 2008;335:1179–1191. doi: 10.1038/sj.npp.1301479. https://doi.org/10.1038/sj.npp.1301479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Onofrio G, O'Connor PG, Pantalon MV, Chawarski MC, Busch SH, Owens PH, et al. Fiellin DA. Emergency department-initiated buprenorphine/naloxone treatment for opioid dependence: a randomized clinical trial. JAMA. 2015;313(16):1636–1644. doi: 10.1001/jama.2015.3474. https://doi.org/10.1001/jama.2015.3474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fetters MD, Curry LA, Creswell JW. Achieving Integration in Mixed Methods Designs—Principles and Practices. Health Services Research. 2013;48(6pt2):2134–2156. doi: 10.1111/1475-6773.12117. https://doi.org/10.1111/1475-6773.12117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firestone M, Goldman B, Fischer B. Fentanyl use among street drug users in Toronto, Canada: behavioural dynamics and public health implications. The International Journal on Drug Policy. 2009;20(1):90–92. doi: 10.1016/j.drugpo.2008.02.016. https://doi.org/10.1016/j.drugpo.2008.02.016. [DOI] [PubMed] [Google Scholar]
- Flynn R. Connecticut, federal law enforcement officials team up to target opioid distributors. 2016 Apr 13; Retrieved October 6, 2016, from http://www.nhregister.com/general-news/20160413/connecticut-federal-law-enforcement-officials-team-up-to-target-opioid-distributors.
- Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. Aldine; 1967. [Google Scholar]
- Greenfield VA, Paoli L. Research as due diligence: What can supply-side interventions accomplish and at what cost? The International Journal on Drug Policy. 2017;41:162–163. doi: 10.1016/j.drugpo.2017.01.010. https://doi.org/10.1016/j.drugpo.2017.01.010. [DOI] [PubMed] [Google Scholar]
- Greenwald MK. Behavioral economic analysis of drug preference using multiple choice procedure data. Drug and Alcohol Dependence. 2008;93:1–2. 103–110. doi: 10.1016/j.drugalcdep.2007.09.002. https://doi.org/10.1016/j.drugalcdep.2007.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hempstead K, Yildirim EO. Supply-side response to declining heroin purity: fentanyl overdose episode in New Jersey. Health Economics. 2014;23(6):688–705. doi: 10.1002/hec.2937. https://doi.org/10.1002/hec.2937. [DOI] [PubMed] [Google Scholar]
- Huffam S, Fairley CK, Chung M, Sze JK, Bilardi J, Chen MY. Facilitating partner notification through an online messaging service: Let Them Know. Sexual Health. 2013;10(4):377–379. doi: 10.1071/SH13007. https://doi.org/10.1071/SH13007. [DOI] [PubMed] [Google Scholar]
- Jones CM, Campopiano M, Baldwin G, McCance-Katz E. National and State Treatment Need and Capacity for Opioid Agonist Medication-Assisted Treatment. American Journal of Public Health. 2015;105(8):e55–63. doi: 10.2105/AJPH.2015.302664. https://doi.org/10.2105/AJPH.2015.302664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin CA, Yang C, Tobin KE, German D. Injection drug users' and their risk networks' experiences of and attitudes towards drug dealer violence in Baltimore, Maryland. The International Journal on Drug Policy. 2013;24(2):135–141. doi: 10.1016/j.drugpo.2012.07.007. https://doi.org/10.1016/j.drugpo.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JD, Rich JD. Opioid pharmacotherapy in criminal justice settings: now is the time. Substance Abuse. 2012;33(1):1–4. doi: 10.1080/08897077.2011.616797. https://doi.org/10.1080/08897077.2011.616797. [DOI] [PubMed] [Google Scholar]
- Macmadu A, Carroll JJ, Hadland SE, Green TC, Marshall BDL. Prevalence and correlates of fentanyl-contaminated heroin exposure among young adults who use prescription opioids non-medically. Addictive Behaviors. 2017;68:35–38. doi: 10.1016/j.addbeh.2017.01.014. https://doi.org/10.1016/j.addbeh.2017.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauger S, Fraser R, Gill K. Utilizing buprenorphine-naloxone to treat illicit and prescription-opioid dependence. Neuropsychiatric Disease and Treatment. 2014;10:587–598. doi: 10.2147/NDT.S39692. https://doi.org/10.2147/NDT.S39692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercado-Crespo MC, Sumner SA, Spelke MB, Sugerman DE, Stanley C. Notes from the Field: Increase in Fentanyl-Related Overdose Deaths - Rhode Island, November 2013-March 2014. Morbidity and Mortality Weekly Report. 2014;63(24):531. [PMC free article] [PubMed] [Google Scholar]
- Nunn A, Zaller N, Dickman S, Trimbur C, Nijhawan A, Rich JD. Methadone and buprenorphine prescribing and referral practices in US prison systems: results from a nationwide survey. Drug and Alcohol Dependence. 2009;105:1–2. 83–88. doi: 10.1016/j.drugalcdep.2009.06.015. https://doi.org/10.1016/j.drugalcdep.2009.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otiashvili D, Piralishvili G, Sikharulidze Z, Kamkamidze G, Poole S, Woody GE. Methadone and buprenorphine-naloxone are effective in reducing illicit buprenorphine and other opioid use, and reducing HIV risk behavior--outcomes of a randomized trial. Drug and Alcohol Dependence. 2013;133(2):376–382. doi: 10.1016/j.drugalcdep.2013.06.024. https://doi.org/10.1016/j.drugalcdep.2013.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrishen B. Confronting the opiate. 2014 Dec 12; Retrieved October 6, 2016, from http://www.telegram.com/article/20141212/NEWS/312129821.
- Quintana P, Ventura M, Grifell M, Palma A, Galindo L, Fornís I, et al. Torrens M. The hidden web and the fentanyl problem: Detection of ocfentanil as an adulterant in heroin. The International Journal on Drug Policy. 2017;40:78–83. doi: 10.1016/j.drugpo.2016.10.006. https://doi.org/10.1016/j.drugpo.2016.10.006. [DOI] [PubMed] [Google Scholar]
- Rego M. East Providence Police intensify heroin interdiction. 2016 Jan 8; Retrieved October 6, 2016, from http://www.eastbayri.com/stories/east-providence-police-intensifyheroin-interdiction,17962.
- Rhode Island Governor's Overdose Prevention and Intervention Task Force. Rhode Island's Strategic Plan on Addiction and Overdose: Four Strategies to Alter the Course of an Epidemic. 2015 Retrieved from http://www.strategicplanri.org/s/Task-Force-Strategic-Plan.pdf.
- Rhode Island Governor's Overdose Prevention and Intervention Task Force. See the Data – Prevent Overdose RI. 2016 Retrieved from http://preventoverdoseri.org/see-the-data/
- Rich JD, McKenzie M, Larney S, Wong JB, Tran L, Clarke J, et al. Zaller N. Methadone continuation versus forced withdrawal on incarceration in a combined US prison and jail: a randomised, open-label trial. Lancet (London, England) 2015;386(9991):350–359. doi: 10.1016/S0140-6736(14)62338-2. https://doi.org/10.1016/S0140-6736(14)62338-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in Drug and Opioid Overdose Deaths--United States, 2000-2014. MMWR Morbidity and Mortality Weekly Report. 2016;64(50–51):1378–1382. doi: 10.15585/mmwr.mm6450a3. https://doi.org/10.15585/mmwr.mm6450a3. [DOI] [PubMed] [Google Scholar]
- Schwartz RP, Gryczynski J, O'Grady KE, Sharfstein JM, Warren G, Olsen Y, et al. Jaffe JH. Opioid agonist treatments and heroin overdose deaths in Baltimore, Maryland, 1995-2009. American Journal of Public Health. 2013;103(5):917–922. doi: 10.2105/AJPH.2012.301049. https://doi.org/10.2105/AJPH.2012.301049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slater J. Heroin crisis continues to grow in Connecticut. 2016 Sep 14; Retrieved from http://wtnh.com/2016/09/14/heroin-crisis-continues-to-grow-in-connecticut/
- Somerville NJ, O'Donnell J, Gladden RM, Zibbell JE, Green TC, Younkin M, et al. Walley AY. Characteristics of Fentanyl Overdose — Massachusetts, 2014–2016. MMWR Morbidity and Mortality Weekly Report. 2017;66(14):382–386. doi: 10.15585/mmwr.mm6614a2. https://doi.org/10.15585/mmwr.mm6614a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan WS, Chen M, Ivan M, Stone K, Rane V, Fairley CK, Ong JJ. Partner Notification Outcomes for Men Who Have Sex With Men Diagnosed With Syphilis Referred to Partner Notification Officers, Melbourne, Australia. Sexually Transmitted Diseases. 2016;43(11):685–689. doi: 10.1097/OLQ.0000000000000512. https://doi.org/10.1097/OLQ.0000000000000512. [DOI] [PubMed] [Google Scholar]
- United States Drug Enforcement Administration. National Heroin Threat Assessment Summary - Updated (DEA Intelligence Report No. DEA-DCT-DIR-031-16) US Drug Enforcement Agency. 2016 Retrieved from https://www.dea.gov/divisions/hq/2016/hq062716_attach.pdf.
- Volpe DA, Tobin GAM, Mellon RD, Katki AG, Parker RJ, Colatsky T, et al. Verbois SL. Uniform assessment and ranking of opioid Mu receptor binding constants for selected opioid drugs. Regulatory Toxicology and Pharmacology. 2011;59(3):385–390. doi: 10.1016/j.yrtph.2010.12.007. https://doi.org/10.1016/j.yrtph.2010.12.007. [DOI] [PubMed] [Google Scholar]
- Yokell MA, Green TC, Bowman S, McKenzie M, Rich JD. Opioid Overdose Prevention and Naloxone Distribution in Rhode Island. Medicine and Health, Rhode Island. 2011;94(8):240–242. [PMC free article] [PubMed] [Google Scholar]
- Yokell MA, Zaller ND, Green TC, McKenzie M, Rich JD. Intravenous use of illicit buprenorphine/naloxone to reverse an acute heroin overdose. Journal of Opioid Management. 2012;8(1):63–66. doi: 10.5055/jom.2012.0098. [DOI] [PMC free article] [PubMed] [Google Scholar]