Abstract
The purpose of this study was to investigate the morphological and mechanical properties of the transverse carpal ligament (TCL) in patients with carpal tunnel syndrome (CTS). Thickness and stiffness of the TCL in eight female CTS patients and eight female control subjects were examined using ultrasound imaging modalities. CTS patients had a 30.9% thicker TCL than control subjects. There was no overall difference in TCL stiffness between the two groups, but the radial TCL region was significantly stiffer than the ulnar region within the CTS group and such a regional difference was not found for the controls. The increased thickness and localized stiffness of the TCL for CTS patients may contribute to CTS symptoms due to reduction in carpal tunnel space and compliance. Advancements in ultrasound technology provide a means of understanding CTS mechanisms and quantifying the morphological and mechanical properties of the TCL in vivo.
Keywords: Transverse carpal ligament, carpal tunnel syndrome, ultrasound imaging, acoustic radiation force impulse
INTRODUCTION
The transverse carpal ligament (TCL) is a band of collagenous tissue that forms the volar boundary of the carpal tunnel. The TCL has many biomechanical functions, including serving as an origin site for the thenar and hypothenar muscles [6, 8, 17, 39], stabilizing the carpal tunnel structure [4, 44, 48], acting as a pulley for the flexor tendons [14, 16], and contributing to carpal tunnel compliance [13, 19, 36]. Clinically, the TCL is closely associated with carpal tunnel syndrome (CTS) which is demonstrated by the ligament’s surgical transection as a common treatment to relieve median nerve compression within the carpal tunnel.
Despite the high prevalence of CTS, its etiological mechanisms remain unclear. Multiple disease mechanisms have been proposed for idiopathic CTS, including those that involve changes to tunnel tissues. For example, microtears and fibrosis of the subsynovial connective tissue have been suggested to cause median nerve neuropathy [45]. Aside from the carpal tunnel contents, the morphological and mechanical changes (e.g. hypertrophying and stiffening) of the TCL may be a causative factor in CTS [11, 26, 30, 37, 42]. Such pathological changes of the TCL may reduce the amount of space available to the carpal tunnel contents or compromise the inherent compliance of the carpal tunnel structure, both of which may negatively implicate the median nerve. There are inconsistencies regarding whether or not thickening of the TCL occurs in CTS patients with some studies noting evident thickening [7, 11, 26] and others indicating no change in ligament thickness [35, 43]. Additionally, examinations of TCL samples from CTS patients have shown that some patients exhibit fibrosis [34] or cellular changes [1] within the ligament, but these findings have not been consistently confirmed [20, 31]. The current study is motivated, in large part, by such observations of TCL changes being anecdotal in nature and requiring invasive methodologies, with few studies quantitatively examining morphological and mechanical differences of the TCL among CTS patients and controls.
Due to the relatively superficial location of the TCL, deep only to other soft tissues at the palmar aspect of the wrist (e.g. skin, fat, muscle), ultrasound imaging is an ideal tool to noninvasively examine the ligament. B-mode ultrasound imaging has been shown to provide a reliable means of measuring the thickness of the TCL at the distal level of the carpal tunnel [38]. Morphological characteristics of the TCL in CTS patients have also been examined using B-mode ultrasound, noting increased ligament bowing or curvature [5, 21], as well as pathological variations of TCL thickness [26]. Furthermore, advancements in ultrasonography have provided a means to non-invasively quantify the mechanical properties of tissues in terms of elasticity. For example, acoustic radiation force impulse (ARFI) imaging is a type of sonoelastography that mechanically excites tissues via localized impulsive radiation forces that result in measurable shear wave propagation in terms of shear wave velocity (SWV). SWV has been demonstrated to correlate with tissue stiffness [32]. Sonoelastography imaging has been used to quantify the stiffness of the TCL in healthy controls [40], patients with CTS [26], and a repetitive hand use population [24]. In the repetitive hand use population, a localized stiffness increase in the radial aspect of the TCL was found in comparison to the ulnar aspect [24]. These localized changes were attributed to the radial aspect of the TCL serving as an origin site for the thenar muscles. To date, it is unknown if similar localized changes occur in the TCL for CTS patients, and if such potential changes are detectable using ultrasound imaging.
The purpose of this study was to investigate the morphological and mechanical properties of the TCL, specifically its thickness and stiffness, associated with CTS using B-mode and sonoelastography ultrasound imaging, respectively. It was hypothesized that CTS patients, in comparison to healthy controls, would demonstrate increased thickness and stiffness of the TCL. Furthermore, the differences between the radial and ulnar portions of the TCL were investigated, and it was hypothesized that for CTS patients the radial aspect of the TCL would have an increased thickness and stiffness in comparison to the ulnar aspect.
METHODS
Human Subjects
Sixteen female subjects voluntarily participated in this study; eight of the subjects were patients clinically diagnosed with CTS (57.5 ± 7.5 years old) and the remaining eight participants were healthy control subjects (50.9 ± 11.4 years old). For each group, the right hand was imaged for six subjects and the left hand was imaged for two subjects. The inclusion criteria for the CTS group included confirmation of CTS according to clinical discretion [12] and required satisfying at least three of the following criteria: (1) history of pain and/or numbness in the median-innervated territory of the right hand for at least 3 months; (2) positive provocative tests (e.g. Tinel’s sign, Phalen’s maneuver, and/or median nerve compression); (3) abnormal electrodiagnostic test results consistent with median neuropathy at/or distal to the wrist; and (4) an overall Boston Carpal Tunnel Syndrome Questionnaire [18] score greater than 1.5. Exclusion criteria for both groups included any history of systemic disease associated with increased incidence of CTS (e.g. diabetes or rheumatoid arthritis), surgical intervention or trauma to the hand or wrist, or current pregnancy. Additionally, for the CTS group, subjects were excluded if they had received a steroid injection for CTS treatment within 3 months of the experiment. Prior to study participation, each subject provided written, informed consent in accordance with the local institutional review board.
Subject Positioning
Each participant placed the hand/forearm into a thermoplastic splint with the forearm supinated and the wrist stabilized in a neutral position. The fingers were placed in full extension and the thumb was abducted 45° within the plane of the palm; Velcro® straps were used to secure the forearm and digits (Figure 1).
Figure 1.
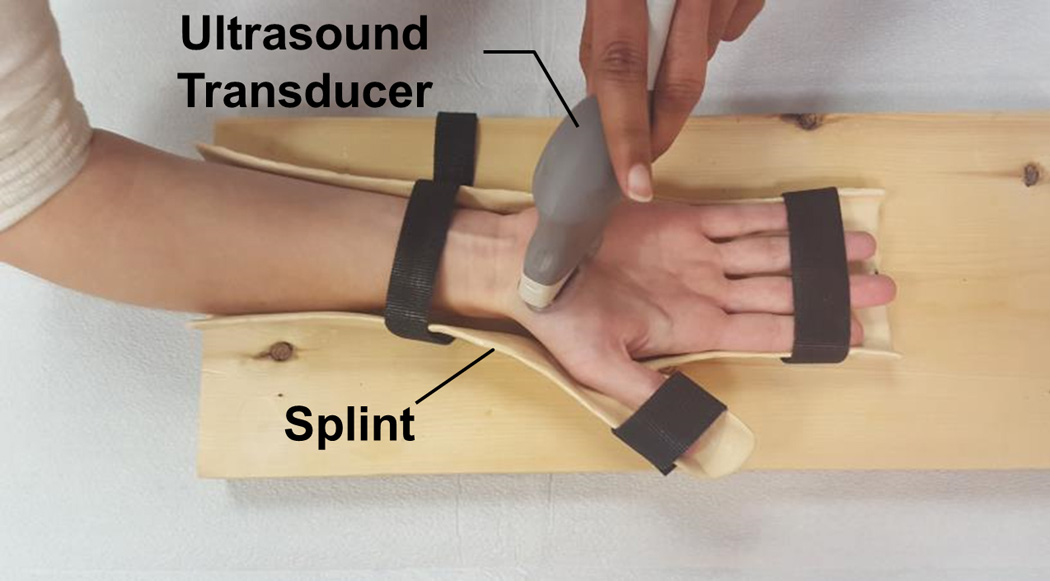
Experimental setup for ultrasound imaging of the TCL at the distal carpal tunnel level.
Experimental Protocol
Ultrasound images of the TCL at the distal level of the carpal tunnel were captured using two types of ultrasonography: 1) B-mode imaging and 2) acoustic radiation force impulse (ARFI) imaging, a type of sonoelastography. A single operator (TLM) conducted ultrasound examinations on all subjects using an Acuson S2000 ultrasound system (Siemens Medical Solutions USA, Mountain View, CA) equipped with Virtual Touch Tissue IQ™ software. Two linear array ultrasound transducers (Siemens Medical Solutions USA, Mountain View, CA) were used for image acquisition, specifically the 18L6 HD transducer for B-mode imaging with an imaging frequency of 12MHz and the 9L4 transducer for ARFI imaging at a frequency of 8MHz. The image depth was set to 3.0 cm for B-mode and 4.0–4.5 cm for ARFI imaging.
Axial images of the TCL at the distal carpal tunnel were obtained with the ultrasound transducers oriented perpendicularly to the surface of the palm. This imaging location provided visualization of the TCL, ridge of the trapezium, hook of the hamate, and the thenar muscles’ ulnar point (TUP). The TUP is a readily identifiable landmark on ultrasound images at the distal level of the carpal tunnel and represents the most ulnar origin point of the thenar muscles into the TCL [38]. A total of 10 images were acquired for each type of ultrasonography, with the order of ultrasonography type randomized for each subject. Care was taken to minimize the amount of force applied on the palm of the subject by the transducer during imaging. Prior to each image capture, a layer of ultrasound gel (~ 1 cm thick) was applied to the transducer and the transducer was gently placed in contact with the palm to identify the imaging plane, after which the transducer was slowly lowered towards the palm until the point that the gel layer was no longer visible on the ultrasound image.
Data Processing
The thickness of the TCL was obtained from the acquired B-mode images (Figure 2A) according to a procedure similar to that previously validated by Shen and Li [38]; the procedure is briefly described as follows. First, the coordinates of the volar and dorsal boundaries of the TCL were determined by manually selecting the ligament’s boundaries using the ImageJ segmented line tool (U.S. National Institutes of Health, Bethesda, MD, USA). Additionally, the coordinates of the hook of the hamate, the ridge of the trapezium, and the TUP were found using the ImageJ point tool. Then, all of the obtained coordinates were input into a custom MATLAB program (The MathWorks, Natick, MA, USA). The program was used to establish an anatomically relevant coordinate system with its origin at the ridge of the trapezium point, x-axis along the line pointing from the ridge of the trapezium to the hook of the hamate, and y-axis perpendicular to the x-axis pointing in the volar direction. Next, the MATLAB program transformed the coordinates obtained in ImageJ to the defined anatomical coordinate system. Then, linear interpolation was performed for the volar and dorsal boundaries of the TCL at each pixel, and the mid-line between the volar and dorsal boundaries of the TCL was determined. The volar, dorsal, and mid-line points were then fit with a fourth-order polynomial. Next, a line perpendicular to the mid-line at each pixel was established and the intersection of this line with the volar and dorsal curves was found. The thickness of the TCL was calculated as the distance between the intersection points of the volar and dorsal curves at each pixel. The average TCL thickness was determined for the following three regions that were defined along the x-axis: 1) the 10 mm portion centered at the TUP (central region), 2) the radial region defined as the 5 mm portion radial to the TUP, and 3) the ulnar region defined as the 5 mm portion ulnar to the TUP (Figure 2A).
Figure 2.
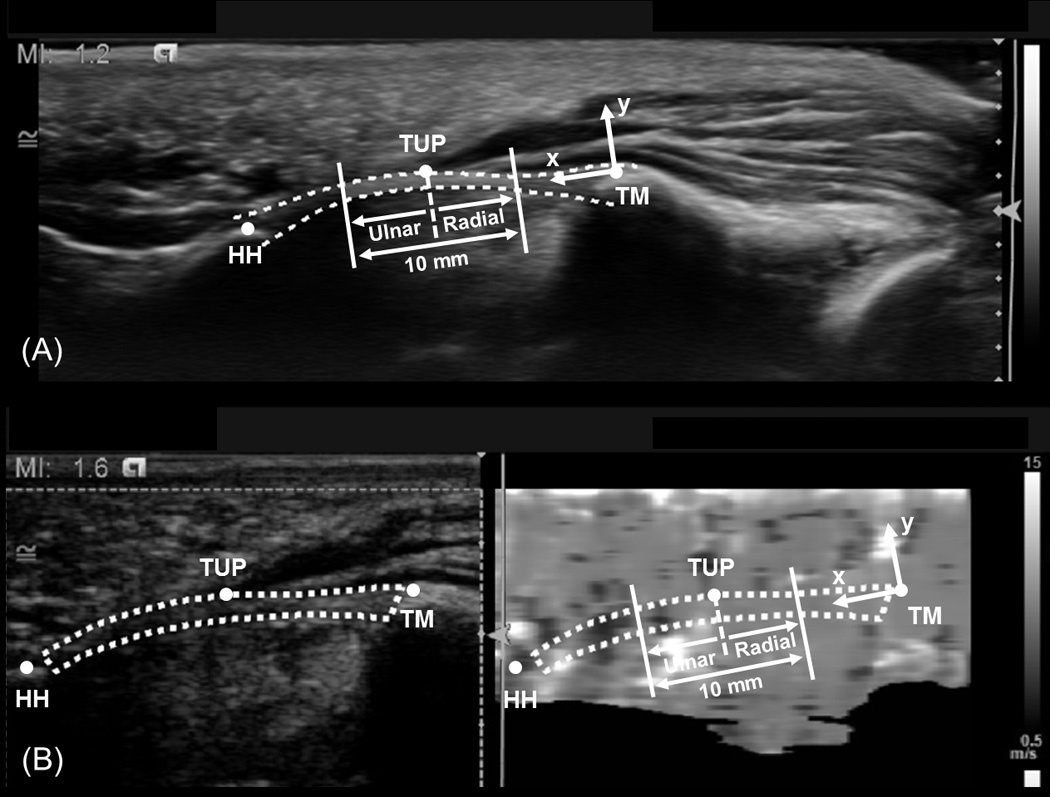
Representative B-mode (A) and ARFI-mode (B) ultrasound images that indicate the anatomically defined coordinate system, TCL (dotted line), hook of the hamate (HH), thenar muscles ulnar point (TUP), and ridge of the trapezium (TM). Additionally, the central 10 mm region of the TCL is identified in each image, along with the radial and ulnar regions used for analysis.
The SWV of the TCL was determined from the ARFI images as a means of quantifying the ligament’s stiffness. The SWV is the speed at which a propagation wave travels through a tissue and provides a means of quantifying the elasticity of tissues in vivo [32]. Each AFRI image consisted of two parts, namely a B-mode portion on the left side and an ARFI portion on the right side of the image (Figure 2B). Using a custom MATLAB program, the boundary of the TCL was manually selected on the B-mode portion of the ARFI image. Additionally, the hook of the hamate, ridge of the trapezium, and TUP points were identified on the B-mode portion of the image. Then, the identified region and points were translated to the ARFI side of the image. An anatomically relevant coordinate system was determined on the ARFI image side according to the procedures described for the TCL thickness analysis; the selected TCL region and points were transformed to the established coordinate system. The ARFI image side was comprised of a grayscale map in which the grayscale intensity of each pixel (0–255) corresponds to a SWV value of up to 15.0 m/s. Given this relationship, the SWV value at each pixel within the TCL section was found. Then, the median SWV within the same three regions analyzed for TCL thickness were determined, specifically the 1) central, 2) radial, and 3) ulnar regions (Figure 2B).
Statistical Analysis
For each of the three regions (central, radial, and ulnar), average TCL thickness and median SWV were determined from each trial and subject specific means were determined from five trials of each type of ultrasonography. The remaining 5 trials of each imaging type served as backup. Student’s t-tests were used to compare the thickness, as well as the SWV, of the central TCL region between the CTS and control groups. Additionally, two-way repeated measures ANOVAs were performed with factors of group (CTS and control) and region (radial and ulnar) to investigate localized differences in the TCL thickness and SWV values. Post-hoc Tukey’s tests were used for all pairwise comparisons. All statistical analyses were completed using SigmaStat 3.5 (Systat Software Inc., San Jose, CA, USA) with an alpha level of 0.05.
RESULTS
B-mode and ARFI ultrasound imaging were used to investigate the thickness and stiffness of the TCL among CTS patients and control subjects. Analyses revealed that there were significant differences in the thickness of the central region of the TCL between the two groups (p < 0.001); however, there were no significant difference in the ligament’s SWV for this TCL region (p = 0.406). Specifically, the TCL thickness for the CTS group was 1.31 (SD 0.17) mm which was 30.9% greater than the thickness of the control group (1.00 (SD 0.09) mm). For TCL stiffness, the SWV of the ligament’s central region was 7.39 (SD 0.41) m/s for CTS patients and 7.14 (SD 0.72) m/s for the control subjects.
When the TCL thickness was further examined by dividing the ligament into radial and ulnar portions, each spanning 5 mm, it was found that there was a significant group effect (p < 0.001), but there were neither effects of region (p = 0.839) nor a group × region interaction (p= 0.787, Figure 3).
Figure 3.
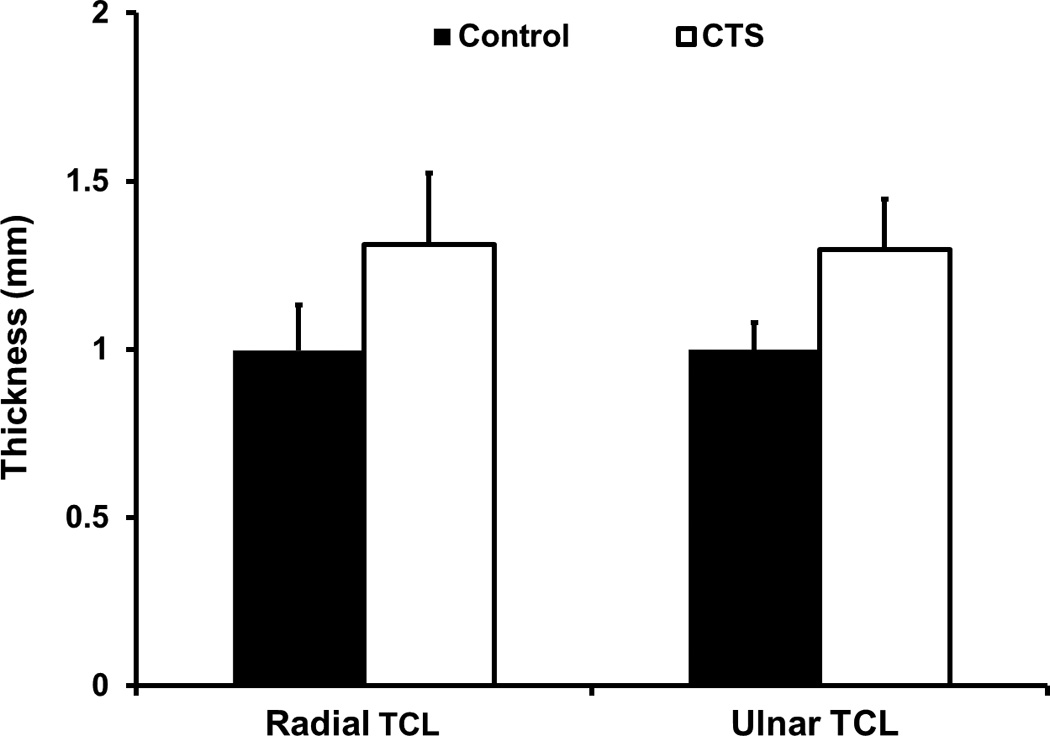
The thickness of the radial and ulnar regions of the TCL for CTS patients and control subjects.
Although there was no difference in the SWV of the central TCL region between the CTS and control groups, when the ligament was divided into radial and ulnar aspects it was revealed that there was a significant group × region interaction (p < 0.01) for SWV. The main effect of group was not found to be significant (p = 0.595), whereas the effect of region was significant (p < 0.001). Post-hoc analysis showed that within the CTS group, the SWV of the radial region of the TCL (7.71 (SD 0.47) m/s) was significantly greater than the ulnar region of the TCL (6.91 (SD 0.48) m/s, p < 0.001). A significant difference was not found between the SWV of the radial and ulnar regions of the TCL within the control group, 7.20 (SD 0.83) m/s and 7.09 (SD 0.68) m/s, respectively (p = 0.436).
DISCUSSION
In this study, in vivo quantifications of the thickness and stiffness of the TCL were performed for CTS patients and control subjects using non-invasive ultrasound imaging techniques. The hypothesis that CTS patients have a thicker TCL was confirmed. Although the central region of the TCL was not found to be stiffer for CTS patients, when the TCL was divided into radial and ulnar regions, an interaction effect was found for ligament stiffness revealing that localized, regional stiffness changes existed for CTS patients that were not found for control subjects.
The limitations of this study should be considered while interpreting its results. First, only female subjects were included in this study as a means to investigate the phenomenon of TCL changes associated with CTS without introducing additional variables such as gender. Future studies can explore if the findings in the current study are applicable to male patients with CTS. Second, CTS severity and disease duration were not considered as factors in this study. Inclusion criteria for the CTS group required a clinical diagnosis of CTS, however patients within the group had varying degrees of CTS severity (mild to moderate) and disease duration (range: less than1 year to greater than 15 years). It is possible that severity and duration of CTS may affect the morphological and mechanical properties of the TCL and this warrants future investigation involving a larger sample size with more stratified subgroups. Finally, the TCL was examined at the distal level of the carpal tunnel, and as such conclusions regarding changes of the ligament at other carpal tunnel levels (e.g. proximal and middle) cannot be drawn from this study. The distal level of the carpal tunnel was selected because this is a common location of median nerve compression for CTS patients [5, 23].
As a soft tissue with many biomechanical functions, the TCL is vulnerable to adaptations that may negatively affect the carpal tunnel structure and mechanical properties, potentially causing CTS. During normal hand use, the TCL biomechanically interacts with the thenar muscles at its volar aspect, and with the flexor tendons at its dorsal aspect. For example during thumb-index finger pinching, it has been shown that the thenar muscles are contracted and the TCL is pulled volarly [39]. Similarly, the TCL has been shown to be displaced volarly when the flexor tendons are tensioned with finger loading [9]. Such mechanical stimulations of the TCL at its volar and dorsal boundaries, if repetitive in nature, may induce maladaptation of the ligament and may help to explain the increased ligament thickness found in the current study for CTS patients. CTS is commonly associated with repetitive hand use [41] and soft, connective tissues (e.g. ligaments) have been shown to remodel from repetitive, mechanical stimulations [47]. The increased ligament thickness for CTS patients may reduce the amount of space available to the carpal tunnel contents thereby inducing or exacerbating CTS symptoms. The difference in TCL thickness between CTS patients and control subjects in this study were similar to those previously reported using ultrasound [26] and computed tomography [22] imaging methods.
Although an increase in thickness of the central region of the TCL was identified for CTS patients, this thickness increase was not accompanied by increased ligament stiffness in the central region. However, further analysis into the radial and ulnar regions of the TCL revealed regional differences in the stiffness for CTS patients. The mechanical properties of the TCL have been shown to vary with location. For example, cadaveric studies have found differences in the compliance of the proximal and distal TCL regions [36, 48], as well as differences in the elastic modulus [10] and amount of strain [3] between radial and ulnar ligament portions. Shear wave elastography methods, such as ARFI, provide a means to non-invasively quantify the elasticity of tissues in vivo, including those of the TCL. In a recent study by Mhanna et al. [24], the SWV of the radial and ulnar TCL at the distal carpal tunnel level were investigated in a repetitive hand use model (i.e. pianists) and it was shown that the TCL was stiffer in its radial segment in comparison to its ulnar segment for the pianists. The results of the current study agree well with this previous finding. One explanation for this regional difference may be related to the thenar muscles being attached to the radial portion of the TCL [6, 17]. In the case of repetitive hand use, particularly involving the thenar muscles of the thumb, an interaction between the muscles and the radial TCL region may result in a localized increase in the tissue’s mechanical properties. Additionally, localized interactions among the tensioned flexor tendons of the index finger, for example, and the TCL may also contribute to regional stiffness changes in the ligament [9]. This localized change in the TCL stiffness may decrease the compliance of the carpal tunnel structure, potentially leading to and/or contributing to median nerve compression.
There has been increased popularity of using ultrasound imaging as a diagnostic and assessment tool for CTS. Most commonly, B-mode imaging has been used to examine the size and shape of the median nerve in CTS patients according to established cut-off criteria [2, 15, 27, 29, 46, 49]. More recently, sonoelastography techniques have also been applied to the assess CTS-associated changes in the elasticity of the median nerve [25, 27, 33] and additional carpal tunnel contents [28]. The current study provides insight into the structural and mechanical maladaptations of the TCL using ultrasound imaging, which may provide valuable, complimentary assessment in addition to current clinical strategies for diagnosing or of evaluating CTS. More studies with large sample sizes are needed to establish the sensitivity and specificity of TCL morphological and mechanical properties as a diagnostic tool for CTS. This study further demonstrates that the TCL adapts its tissue properties in a location-dependent manner corresponding to the local biomechanical environment. Future studies are needed to determine the implications of CTS severity and disease duration, as well as to establish standardized imaging protocols, prior to determining the efficacy of applying such imaging techniques of the TCL for CTS diagnosis and evaluation.
Figure 4.
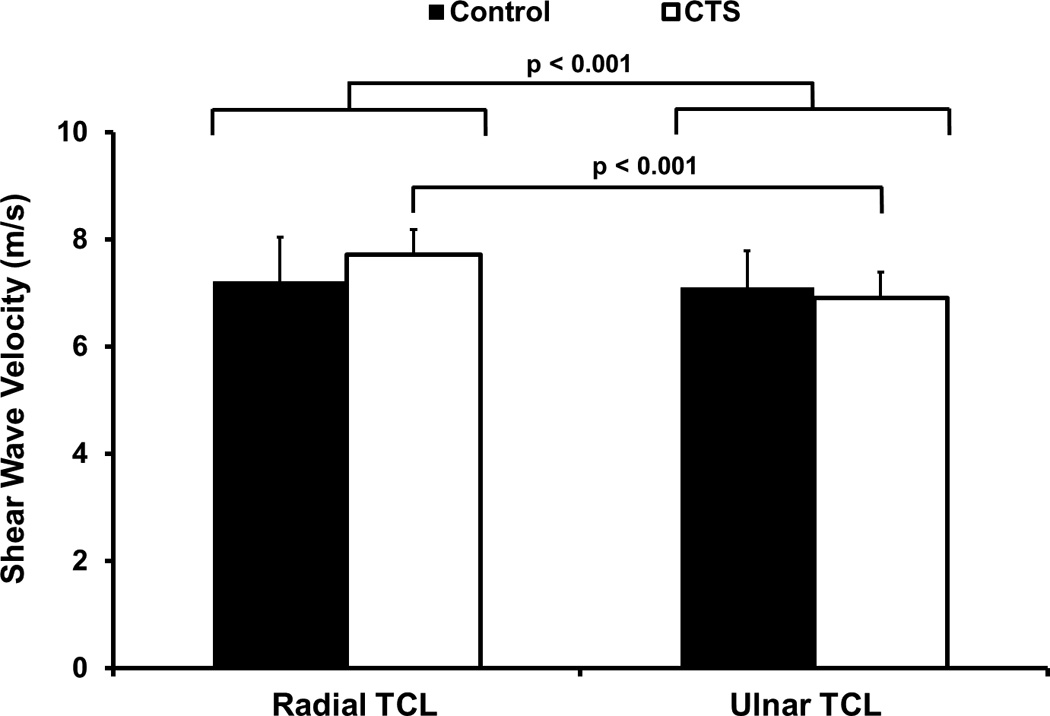
The shear wave velocity (SWV) of the radial and ulnar regions of the TCL for CTS patients and control subjects.
Acknowledgments
Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number R21AR064957 (ZML). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest Statement
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
SUBMISSION STATEMENT
We represent that this submission is original work, and is not under consideration for publication with any other journal.
REFERENCES
- 1.Allampallam K, Chakraborty J, Bose KK, Robinson J. Explant culture, immunofluorescence and electron-microscopic study of flexor retinaculum in carpal tunnel syndrome. J Occup Environ Med. 1996;38(3):264–271. doi: 10.1097/00043764-199603000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Altinok T, Baysal O, Karakas HM, Sigirci A, Alkan A, Kayhan A, Yologlu S. Ultrasonographic assessment of mild and moderate idiopathic carpal tunnel syndrome. Clin Radiol. 2004;59(10):916–925. doi: 10.1016/j.crad.2004.03.019. [DOI] [PubMed] [Google Scholar]
- 3.Brett AW, Oliver ML, Agur AM, Edwards AM, Gordon KD. Quantification of the transverse carpal ligament elastic properties by sex and region. Clin Biomech (Bristol, Avon) 2014;29(6):601–606. doi: 10.1016/j.clinbiomech.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 4.Brooks JJ, Schiller JR, Allen SD, Akelman E. Biomechanical and anatomical consequences of carpal tunnel release. Clin Biomech (Bristol, Avon) 2003;18(8):685–693. doi: 10.1016/s0268-0033(03)00052-4. [DOI] [PubMed] [Google Scholar]
- 5.Buchberger W, Schon G, Strasser K, Jungwirth W. High-resolution ultrasonography of the carpal tunnel. J Ultrasound Med. 1991;10(10):531–537. doi: 10.7863/jum.1991.10.10.531. [DOI] [PubMed] [Google Scholar]
- 6.Cobb TK, Dalley BK, Posteraro RH, Lewis RC. Anatomy of the flexor retinaculum. J Hand Surg Am. 1993;18(1):91–99. doi: 10.1016/0363-5023(93)90251-W. [DOI] [PubMed] [Google Scholar]
- 7.Ferrari FS, Della Sala L, Cozza S, Guazzi G, Belcapo L, Mariottini A, Bolognini A, Stefani P. High-resolution ultrasonography in the study of carpal tunnel syndrome. Radiol Med. 1997;93(4):336–341. [PubMed] [Google Scholar]
- 8.Fuss FK, Wagner TF. Biomechanical alterations in the carpal arch and hand muscles after carpal tunnel release: a further approach toward understanding the function of the flexor retinaculum and the cause of postoperative grip weakness. Clin Anat. 1996;9(2):100–108. doi: 10.1002/(SICI)1098-2353(1996)9:2<100::AID-CA2>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 9.Gabra JN, Gordon JL, Marquardt TL, Seitz WH, Evans PJ, Li ZM. In vivo tissue interaction between the transverse carpal ligament and finger flexor tendons associated with wrist posture and tendon tension. Medical Engineering and Physics. 2016;38(10):1055–1062. doi: 10.1016/j.medengphy.2016.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holmes MW, Howarth SJ, Callaghan JP, Keir PJ. Biomechanical properties of the transverse carpal ligament under biaxial strain. J Orthop Res. 2012;30(5):757–763. doi: 10.1002/jor.21583. [DOI] [PubMed] [Google Scholar]
- 11.John V, Nau HE, Nahser HC, Reinhardt V, Venjakob K. CT of carpal tunnel syndrome. AJNR Am J Neuroradiol. 1983;4(3):770–772. [PMC free article] [PubMed] [Google Scholar]
- 12.Keith MW, Masear V, Chung KC, Maupin K, Andary M, Amadio PC, Watters WC, 3rd, Goldberg MJ, Haralson RH, 3rd, Turkelson CM, Wies JL, McGowan R. American Academy of Orthopaedic Surgeons Clinical Practice Guideline on diagnosis of carpal tunnel syndrome. J Bone Joint Surg Am. 2009;91(10):2478–2479. doi: 10.2106/JBJS.I.00643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim DH, Marquardt TL, Gabra JN, Shen ZL, Evans PJ, Seitz WH, Li ZM. Pressure-morphology relationship of a released carpal tunnel. J Orthop Res. 2013;31(4):616–620. doi: 10.1002/jor.22271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kiritsis PG, Kline SC. Biomechanical changes after carpal tunnel release: a cadaveric model for comparing open, endoscopic, and step-cut lengthening techniques. J Hand Surg Am. 1995;20(2):173–180. doi: 10.1016/S0363-5023(05)80003-6. [DOI] [PubMed] [Google Scholar]
- 15.Klauser AS, Halpern EJ, De Zordo T, Feuchtner GM, Arora R, Gruber J, Martinoli C, Loscher WN. Carpal tunnel syndrome assessment with US: value of additional cross-sectional area measurements of the median nerve in patients versus healthy volunteers. Radiology. 2009;250(1):171–177. doi: 10.1148/radiol.2501080397. [DOI] [PubMed] [Google Scholar]
- 16.Kline SC, Moore JR. The transverse carpal ligament. An important component of the digital flexor pulley system. J Bone Joint Surg Am. 1992;74(10):1478–1485. [PubMed] [Google Scholar]
- 17.Kung J, Budoff JE, Wei ML, Gharbaoui I, Luo ZP. The origins of the thenar and hypothenar muscles. J Hand Surg Br. 2005;30(5):475–476. doi: 10.1016/j.jhsb.2005.04.019. [DOI] [PubMed] [Google Scholar]
- 18.Levine DW, Simmons BP, Koris MJ, Daltroy LH, Hohl GG, Fossel AH, Katz JN. A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. J Bone Joint Surg Am. 1993;75(11):1585–1592. doi: 10.2106/00004623-199311000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Li ZM, Marquardt TL, Evans PJ, Seitz WH., Jr Biomechanical role of the transverse carpal ligament in carpal tunnel compliance. J Wrist Surg. 2014;3(4):227–232. doi: 10.1055/s-0034-1394136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lin R, Lin E, Engel J, Bubis JJ. Histo-mechanical aspects of carpal tunnel syndrome. Hand. 1983;15(3):305–309. [PubMed] [Google Scholar]
- 21.Marquardt TL, Evans PJ, Seitz WH, Li ZM. Carpal arch and median nerve changes during radioulnar wrist compression in carpal tunnel syndrome patients. J Orthop Res. 2016 doi: 10.1002/jor.23126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Merhar GL, Clark RA, Schneider HJ, Stern PJ. High-resolution computed tomography of the wrist in patients with carpal tunnel syndrome. Skeletal Radiol. 1986;15(7):549–552. doi: 10.1007/BF00361053. [DOI] [PubMed] [Google Scholar]
- 23.Mesgarzadeh M, Schneck CD, Bonakdarpour A, Mitra A, Conaway D. Carpal tunnel: MR imaging. Part II. Carpal tunnel syndrome. Radiology. 1989;171(3):749–754. doi: 10.1148/radiology.171.3.2541464. [DOI] [PubMed] [Google Scholar]
- 24.Mhanna C, Marquardt TL, Li ZM. Adaptation of the Transverse Carpal Ligament Associated with Repetitive Hand Use in Pianists. PLoS One. 2016;11(3):e0150174. doi: 10.1371/journal.pone.0150174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miyamoto H, Halpern EJ, Kastlunger M, Gabl M, Arora R, Bellmann-Weiler R, Feuchtner GM, Jaschke WR, Klauser AS. Carpal tunnel syndrome: diagnosis by means of median nerve elasticity--improved diagnostic accuracy of US with sonoelastography. Radiology. 2014;270(2):481–486. doi: 10.1148/radiol.13122901. [DOI] [PubMed] [Google Scholar]
- 26.Miyamoto H, Miura T, Morizaki Y, Uehara K, Ohe T, Tanaka S. Comparative study on the stiffness of transverse carpal ligament between normal subjects and carpal tunnel syndrome patients. Hand Surg. 2013;18(2):209–214. doi: 10.1142/S0218810413500251. [DOI] [PubMed] [Google Scholar]
- 27.Miyamoto H, Morizaki Y, Kashiyama T, Tanaka S. Grey-scale sonography and sonoelastography for diagnosing carpal tunnel syndrome. World J Radiol. 2016;8(3):281–287. doi: 10.4329/wjr.v8.i3.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miyamoto H, Siedentopf C, Kastlunger M, Martinoli C, Gabl M, Jaschke WR, Klauser AS. Intracarpal tunnel contents: evaluation of the effects of corticosteroid injection with sonoelastography. Radiology. 2014;270(3):809–815. doi: 10.1148/radiol.13131083. [DOI] [PubMed] [Google Scholar]
- 29.Mohammadi A, Afshar A, Etemadi A, Masoudi S, Baghizadeh A. Diagnostic value of cross-sectional area of median nerve in grading severity of carpal tunnel syndrome. Arch Iran Med. 2010;13(6):516–521. [PubMed] [Google Scholar]
- 30.Moore JS. Biomechanical models for the pathogenesis of specific distal upper extremity disorders. Am J Ind Med. 2002;41(5):353–369. doi: 10.1002/ajim.10037. [DOI] [PubMed] [Google Scholar]
- 31.Nakamichi K, Tachibana S. Histology of the transverse carpal ligament and flexor tenosynovium in idiopathic carpal tunnel syndrome. J Hand Surg Am. 1998;23(6):1015–1024. doi: 10.1016/s0363-5023(98)80009-9. [DOI] [PubMed] [Google Scholar]
- 32.Nightingale K, Soo MS, Nightingale R, Trahey G. Acoustic radiation force impulse imaging: in vivo demonstration of clinical feasibility. Ultrasound Med Biol. 2002;28(2):227–235. doi: 10.1016/s0301-5629(01)00499-9. [DOI] [PubMed] [Google Scholar]
- 33.Orman G, Ozben S, Huseyinoglu N, Duymus M, Orman KG. Ultrasound elastographic evaluation in the diagnosis of carpal tunnel syndrome: initial findings. Ultrasound Med Biol. 2013;39(7):1184–1189. doi: 10.1016/j.ultrasmedbio.2013.02.016. [DOI] [PubMed] [Google Scholar]
- 34.Patiala H, Rokkanen P, Kruuna O, Taponen E, Toivola M, Hakkinen V. Carpal tunnel syndrome. Anatomical and clinical investigation. Arch Orthop Trauma Surg. 1985;104(2):69–73. doi: 10.1007/BF00454239. [DOI] [PubMed] [Google Scholar]
- 35.Phalen GS. The carpal-tunnel syndrome. Seventeen years' experience in diagnosis and treatment of six hundred fifty-four hands. J Bone Joint Surg Am. 1966;48(2):211–228. [PubMed] [Google Scholar]
- 36.Ratnaparkhi R, Xiu KH, Guo X, Li ZM. Changes in Carpal Tunnel Compliance with Incremental Flexor Retinaculum Release. Journal of Orthopaedic Surgery and Research. 2016 doi: 10.1186/s13018-016-0380-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Richman JA, Gelberman RH, Rydevik BL, Hajek PC, Braun RM, Gylys-Morin VM, Berthoty D. Carpal tunnel syndrome: morphologic changes after release of the transverse carpal ligament. J Hand Surg Am. 1989;14(5):852–857. doi: 10.1016/s0363-5023(89)80089-9. [DOI] [PubMed] [Google Scholar]
- 38.Shen ZL, Li ZM. Ultrasound assessment of transverse carpal ligament thickness: a validity and reliability study. Ultrasound Med Biol. 2012;38(6):982–988. doi: 10.1016/j.ultrasmedbio.2012.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shen ZL, Li ZM. Biomechanical interaction between the transverse carpal ligament and the thenar muscles. J Appl Physiol. 2013;114:225–229. doi: 10.1152/japplphysiol.01273.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shen ZL, Vince DG, Li ZM. In vivo study of transverse carpal ligament stiffness using acoustic radiation force impulse (ARFI) imaging. PLoS One. 2013;8(7):e68569. doi: 10.1371/journal.pone.0068569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Silverstein BA, Fine LJ, Armstrong TJ. Occupational factors and carpal tunnel syndrome. Am J Ind Med. 1987;11(3):343–358. doi: 10.1002/ajim.4700110310. [DOI] [PubMed] [Google Scholar]
- 42.Sucher BM. Carpal tunnel syndrome: ultrasonographic imaging and pathologic mechanisms of median nerve compression. J Am Osteopath Assoc. 2009;109(12):641–647. doi: 10.7556/jaoa.2009.109.12.641. [DOI] [PubMed] [Google Scholar]
- 43.Tanzer RC. The carpal-tunnel syndrome; a clinical and anatomical study. J Bone Joint Surg Am. 1959;41-A:626–634. [PubMed] [Google Scholar]
- 44.Tengrootenhuysen M, van Riet R, Pimontel P, Bortier H, Van Glabbeek F. The role of the transverse carpal ligament in carpal stability: an in vitro study. Acta Orthop Belg. 2009;75(4):467–471. [PubMed] [Google Scholar]
- 45.Werthel JD, Zhao C, An KN, Amadio PC. Carpal tunnel syndrome pathophysiology: role of subsynovial connective tissue. J Wrist Surg. 2014;3(4):220–226. doi: 10.1055/s-0034-1394133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wong SM, Griffith JF, Hui AC, Tang A, Wong KS. Discriminatory sonographic criteria for the diagnosis of carpal tunnel syndrome. Arthritis Rheum. 2002;46(7):1914–1921. doi: 10.1002/art.10385. [DOI] [PubMed] [Google Scholar]
- 47.Woo SL, Gomez MA, Woo YK, Akeson WH. Mechanical properties of tendons and ligaments. II. The relationships of immobilization and exercise on tissue remodeling. Biorheology. 1982;19(3):397–408. doi: 10.3233/bir-1982-19302. [DOI] [PubMed] [Google Scholar]
- 48.Xiu KH, Kim JH, Li ZM. Biomechanics of the transverse carpal arch under carpal bone loading. Clin Biomech (Bristol, Avon) 2010;25(8):776–780. doi: 10.1016/j.clinbiomech.2010.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ziswiler HR, Reichenbach S, Vogelin E, Bachmann LM, Villiger PM, Juni P. Diagnostic value of sonography in patients with suspected carpal tunnel syndrome: a prospective study. Arthritis Rheum. 2005;52(1):304–311. doi: 10.1002/art.20723. [DOI] [PubMed] [Google Scholar]


