Abstract
Objectives
Increasing prevalence of asthma in developing countries has been a significant challenge for public health in recent decades. A number of studies have suggested that ambient air pollution can trigger asthma attacks. Biomass and solid fuels are a major source of indoor air pollution, but in developing countries the health effects of indoor air pollution are poorly understood. In this study we examined the effect of cooking smoke produced by biomass and solid fuel combustion on the reported prevalence of asthma among adult men and women in India.
Methods
The analysis is based on 99,574 women and 56,742 men aged between 20 and 49 years included in India’s third National Family Health Survey conducted in 2005–2006. Effects of exposure to cooking smoke, determined by the type of fuel used for cooking such as biomass and solid fuels versus cleaner fuels, on the reported prevalence of asthma were estimated using multivariate logistic regression. Since the effects of cooking smoke are likely to be confounded with effects of tobacco smoking, age, and other such factors, the analysis was carried out after statistically controlling for such factors.
Results
The results indicate that adult women living in households using biomass and solid fuels have a significantly higher risk of asthma than those living in households using cleaner fuels (OR: 1.26; 95%CI: 1.06–1.49; p = .010), even after controlling for the effects of a number of potentially confounding factors. Interestingly, this effect was not found among men (OR: 0.98; 95%CI: 0.77–1.24; p = .846). However, tobacco smoking was associated with higher asthma prevalence among both women (OR: 1.72; 95%CI: 1.34–2.21; p < .0001) and men (OR: 1.35; 95%CI: 1.49–2.25; p < .0001). Combined effects of biomass and solid fuel use and tobacco smoke on the risk of asthma were greater and more significant in women (OR: 2.16; 95%CI: 1.58–2.94; p < .0001) than they were in men (OR: 1.34; 95%CI: 1.04–1.72; p = .024).
Conclusions
The findings have important program and policy implications for countries such as India, where large proportions of the population still rely on polluting biomass fuels for cooking and heating. Decreasing household biomass and solid fuel use and increasing use of improved stove technology may decrease the health effects of indoor air pollution. More epidemiological research with better measures of smoke exposure and clinical measures of asthma is needed to validate the findings.
Keywords: asthma, biomassfuels and solid fuels, tobacco smoking, indoor air pollution, women, men, NFHS-3, India
Introduction
The increase in incidence, prevalence, morbidity, and economic burden of noncommunicable respiratory diseases such as asthma over recent decades presents a significant challenge to public health (1–8). Approximately 300 million people worldwide currently have asthma (8). Asthma is a chronic respiratory disease characterized by sudden attacks of labored breathing, chest tightness, and coughing, particularly at night or in the early morning (9). It is a complex multifactorial disease with both genetic and environmental components (10). However, the rapid increase in asthma in recent decades cannot be ascribed to changes in genetic factors. Rather, the focus of interventions for combating the increased prevalence of asthma should be on environmental factors. International variations in asthma prevalence (11), together with recent increases in many countries, have focused the attention on the role of air pollution. Asthma in poor rural communities in less-developed countries has been little studied, and the relationship between asthma and environment is still less.
Much of the research on factors affecting asthma has been conducted in urban areas of developed countries where a number of studies have suggested that ambient air pollution can trigger asthma attacks (12, 13). Also exposure to several specific air pollutants, such as respirable particulate matter such as PM10 (inhalable material <10 mm in aerodynamic diameter), CO, O3, SO2, and NO2, has been related with increased asthma symptoms (14–19). In many homes in rural areas and urban slums in developing countries, a major source of indoor air pollution is cooking smoke, when people rely on unprocessed biomass fuels such as wood, crop residues, and dung cakes for cooking and space heating even where cleaner and more sophisticated fuels are available (20). Although the proportion of global energy derived from biomass fuels fell from 50% in 1900 to around 13% in 2000, there is evidence that their use is now increasing among the poor (21). According to some estimates, more than half of the world’s population still relies on unprocessed biomass fuels for cooking and heating (22). In the developing countries of South Asia and sub-Saharan Africa, this proportion is as high as 80% or more (23).
Indoor air pollution emanating from traditional fuels and cooking stoves and high exposure to the air pollutants in biomass smoke are a potentially large health threat. The burning of solid fuels indoors in open fires or traditional cooking stoves (chulhas) results in high levels of toxic pollutants in the kitchen area (20, 24). As such, the use of these fuels is considered to be a major risk factor for lung cancer as well as for cardiovascular and noncommunicable respiratory diseases such as chronic obstructive pulmonary disease and asthma (9, 24–28) and other respiratory diseases such as acute respiratory infections (20), chronic bronchitis (21, 29–30), chronic obstructive pulmonary disease (31, 32), and tuberculosis (33, 34). Poor ventilation in kitchens may worsen the adverse health effects of asthma (35–40). Findings from India’s third National Family Health Survey (NFHS-3, 2005–2006) showed that 90% of rural and 32% of urban households (all India total is 71%) in India use biomass and solid cooking fuels that generate smoke and unhealthy conditions when inhaled (41). Smith reported between 410,000 and 570,000 premature deaths among adult women and children aged less than 5 years arising from exposure to indoor air pollution on the basis of the data on risk and exposure derived principally from studies carried out in India (26).
The biomass fuels are typically burned indoors in simple household cooking stoves, such as a pit (a hole in the ground), three pieces of brick, or a U-shaped construction made from mud, which burn these fuels inefficiently and are often not vented with flues or hoods to take the pollutants to the outside (10). Even when the cooking stoves are vented to the outside, combustion of unprocessed solid fuels produces enough pollution to significantly affect the local “neighborhood” pollution levels, with implications for total exposures (25). Under such conditions, high volumes of a number of health-damaging airborne pollutants are generated indoors. Because cooking stoves are usually used for several hours each day and at times when people are present indoors, their exposure effectiveness is high; that is, the percentage of their emissions that reaches people’s breathing zones is much higher than for outdoor sources. The individual peak and mean exposures experienced in such settings are often much greater than the safe levels recommended by the World Health Organization (42). In biomass-burning households, PM10 or PM2.5 often exceeds guideline levels of mean 24 h concentration and severely more so during cooking (30, 43, 44). The mean CO concentrations in homes that use biomass fuel are typically in the range of 2–50 ppm but can be as high as 500 ppm during cooking (45), which is significantly higher than the EPA 8-h safety standard for CO (<9 ppm).
The poorest and the most vulnerable populations in developing countries are the most exposed to indoor air pollution from biomass and solid fuel combustion for cooking and heating. Often households cannot afford alternative fuels or energy-efficient fuels such as kerosene, liquefied petroleum gas (LPG), and electricity (46) because of poverty, which is one of the main barriers to the adoption of cleaner fuels (47). Besides poverty, population growth and the rising price of alternative fuels increase the use of biomass fuels in developing countries (48). The slow pace of development in many countries suggests that biomass fuels will continue to be used by the poor for many decades (22). Exposure levels are usually much higher among women, who tend to do most of the cooking (49), and among young children, who are often held on their mother’s back or lap during cooking times (21).
High exposures to the air pollutants in biomass smoke have been associated with a host of respiratory diseases (20, 21, 30–34) but the evidence on the effect of cooking smoke on asthma is mixed (22, 50–53), even though it contains some of the same pollutants that are found in ambient air pollution or tobacco smoke, both of which have been associated with asthma. Anecdotal association of asthma with cooking smoke is common, but few epidemiologic studies seem to have been done (25). Of the limited research that does exist on this issue, some studies have found a positive association between biomass fuel exposure and asthma (10, 54–58), whereas others found no significant relationship (48, 59, 60–61) or found a protective effect (62, 63).
Various studies have suggested that exposure to tobacco smoke can also increase the risk of developing asthma (56, 59, 64–68). Several studies have found that exposure to tobacco smoke can increase the frequency and severity of asthmatic attacks (69–71), but some fail to link tobacco smoking to onset of asthma in adults (72, 73). Smoking has been associated with airway hyperresponsiveness in a number of surveys as well as in clinical studies (27, 73–76). Exposures to tobacco smoke lead to an increase in severity of asthma, decreased response to treatment, and accelerated decline in lung functions (77, 78).
It is seen from the above discussion that biomass and solid fuels are a major source of indoor air pollution, but in less-developed countries the health effects of indoor air pollution are poorly understood. In this article, the effect of exposure to cooking smoke from biomass and solid fuel combustion on the prevalence of self-reported asthma has been examined using data from a large-scale cross-sectional nationally representative sample of adult men and women in India.
Materials and Methods
Study Population
Data from NFHS-3 conducted in 2005–2006 were used for this article. Briefly, NFHS-3 collected demographic, socioeconomic, and health information from a nationally representative probability sample of 124,385 women aged 15–49 years and 74,369 men aged 15–54 years residing in 109,041 households. All states of India are represented in the sample (except the small Union Territories), covering more than 99% of the country’s population. The sample is a multistage cluster sample with an overall response rate of 98%. All eligible respondents were geo-coded to the primary sampling unit, district, and state to which they belong (79). The primary sampling units were villages or groups of villages in rural areas, and wards or municipal localities in urban areas. Details of sample design, including sampling frame and sample implementation, are provided in the basic all India survey report (41). The analysis presented in this study is based on 99,574 women and 56,742 men aged 20–49 years who lived in the sample households.
Response Variable
Several questions were asked in the survey relating to the current health status of the respondents, including whether the respondent suffered from asthma. The question was, “Do you currently have Asthma?” The survey was conducted using an interviewer-administered questionnaire in the native language of the respondent using a local, commonly understood term for asthma. A total of 18 languages were used in the survey with back translation to English to ensure accuracy and comparability. However, no effort was made to clinically test for the disease. In our analysis, this reported prevalence of asthma is the response variable.
Predictor Variables
Exposure to cooking smoke is determined indirectly by the type of fuel used for cooking in the household. The survey used a 10-item classification of cooking fuel: electricity, LPG/natural gas, biogas, kerosene, coal/lignite, charcoal, wood, straw/shrubs/grass, agricultural crop waste, dung cakes, and a residual category of other fuels (unknown). The question asked was, “What type of fuel does your household mainly use for cooking?,” followed by the above list of fuels. We used information from the above questions to group households into two categories representing the extent of exposure to cooking smoke: high- and medium-exposure group (households using either biomass fuels—such as, wood, straw/shrubs/grass, agricultural crop waste, dung cakes, or others—or solid fuels—such as coal/lignite and charcoal); and low-exposure group (households using only cleaner fuels—such as kerosene, LPG/natural gas, biogas, or electricity). This two-category classification of fuels—that is, cleaner fuel and biomass and solid fuel—is the principal predictor variable in this study.
The survey also collected information on use of tobacco directly by asking respondents to report on their own tobacco use. Four specific questions (“Do you currently smoke cigarettes or bidis?,” “In the last 24 h how many cigarettes or bidis did you smoke?,” “Do you currently smoke or use tobacco in any other form?,” and “In what other form do you currently smoke or use tobacco?”) on current use of tobacco (smoke and nonsmoke variants) were asked to all eligible men and women who were interviewed. The information from these four questions was used to ascertain exposure to tobacco smoke—active smoking (person currently smokes) and no smoking (the person does not smoke). However, question on past smoking is not ascertained in the data.
Because the effects of exposure to cooking smoke as well as tobacco smoke on the prevalence of asthma are likely to be confounded with the effects of other risk factors, it is necessary to statistically control, or adjust, for such factors. Control variables included in this study were age, marital status, education, religion, caste/tribe status, house type, place for cooking, crowding, wealth status of the household, urban/rural residence, and geographic regions. For definition of variables, see Table 1.
Table 1.
Percentage distribution of sample aged 20–49 years by selected characteristics in India, 2005–2006.
| Characteristics | Women | Men |
|---|---|---|
| Cooking smokea | ||
| Cleaner fuels | 29.8 | 31.8 |
| Biomass and solid fuels | 70.2 | 68.2 |
| Tobacco smoke | ||
| No smoking | 98.2 | 62.4 |
| Currently smoking | 1.8 | 37.6 |
| Age (years) | ||
| 20–29 | 43.4 | 40.3 |
| 30–39 | 33.7 | 33.6 |
| 40–49 | 23.0 | 26.2 |
| Marital status | ||
| Currently married | 86.7 | 76.0 |
| Widowed/divorced/separated/deserted | 5.7 | 1.7 |
| Not married | 7.5 | 22.3 |
| Educationb | ||
| Illiterate | 45.3 | 20.5 |
| Below middle school | 14.5 | 17.7 |
| Middle school complete | 31.8 | 47.2 |
| High school complete or above | 8.4 | 14.7 |
| Religion | ||
| Hindu | 81.1 | 82.4 |
| Muslim | 13.0 | 12.1 |
| Othersc | 5.9 | 5.6 |
| Caste/tribesd | ||
| Scheduled castes | 19.0 | 19.5 |
| Scheduled tribes | 8.2 | 8.6 |
| Other backward class | 40.6 | 40.1 |
| Others | 32.1 | 31.8 |
| House typee | ||
| Pucca | 48.6 | 50.2 |
| Semi-pucca/Kachcha | 51.4 | 49.8 |
| Place for cooking | ||
| In the house, separate room | 45.9 | 30.1 |
| In the house, no separate room | 28.5 | 45.3 |
| In a separate building | 8.7 | 8.7 |
| Outdoor/other | 16.7 | 15.9 |
| Crowding | ||
| <2 persons per room | 21.5 | 22.5 |
| 2–4 persons per room | 48.1 | 47.9 |
| 4 or more persons per room | 30.3 | 29.6 |
| Household structure | ||
| Nuclear | 52.8 | 48.5 |
| Joint | 47.2 | 48.3 |
| Wealth indexf | ||
| Lowest | 17.4 | 16.0 |
| Second | 18.6 | 18.0 |
| Middle | 19.8 | 20.3 |
| Fourth | 21.0 | 22.3 |
| Highest | 23.2 | 23.4 |
| Residence | ||
| Urban | 33.5 | 36.6 |
| Rural | 66.5 | 63.4 |
| Regiong | ||
| North | 13.3 | 22.2 |
| Northeast | 4.0 | 4.1 |
| Central | 22.3 | 22.9 |
| East | 22.0 | 20.8 |
| West | 15.1 | 16.4 |
| South | 23.2 | 13.7 |
| Numberh | 99,574 | 56,742 |
Biomass fuels: wood, straw/shrubs/grass, agricultural crop waste, dung cakes, and others; solid fuels: coal/lignite or charcoal; and cleaner fuels: kerosene, liquefied petroleum gas/natural gas, biogas, or electricity.
Education: illiterate (0 years of education), below middle school complete (1–5 years of education), middle school complete (6–8 years of education), and high school complete or above (9+ years of education).
Others include Sikh, Buddhist, Christian, Jain, Jewish, and Zoroastrian.
Scheduled castes and scheduled tribes are identified by the Government of India as socially and economically backward and needing protection from social injustice and exploitation. Other backward class is a diverse collection of intermediate castes that were considered low in the traditional caste hierarchy but are clearly above scheduled castes. “Others” is thus a default residual group that enjoys a higher status in the caste hierarchy.
Pucca houses are made from high-quality materials (bricks, tiles, cement, and concrete) throughout, including roof, walls, and floor; kachcha houses are made from mud, thatch, or other low-quality materials. Semi-pucca houses are made from a combination of high- and low-quality materials.
The wealth index is based on the following assets in the household: household electrification, type of windows, drinking water source, type of toilet facility, type of flooring, material of exterior walls, type of roofing, house ownership, ownership of a bank or post office account, and ownership of a mattress, a pressure cooker, a chair, a cot/bed, a table, an electric fan, a radio/transistor, a black and white television, a color television, a sewing machine, a mobile telephone, any other telephone, a computer, a refrigerator, a watch or clock, a bicycle, a motorcycle or scooter, an animal-drawn cart, a car, a water pump, a thresher, and a tractor.
Region: North: Delhi, Haryana, Himachal Pradesh, Jammu and Kashmir, Punjab, Rajasthan, Uttaranchal; Northeast: Assam, Arunachal Pradesh, Manipur, Meghalaya, Mizoram, Nagaland, Sikkim, Tripura; Central: Chhattisgarh, Madhya Pradesh, Uttar Pradesh; East: Bihar, Jharkhand, West Bengal, Orissa; West: Maharashtra, Goa, Gujarat; South: Andhra Pradesh, Karnataka, Kerala, Tamil Nadu.
Number of men and women varies slightly for individual variables depending on the number of missing values.
Statistical Analysis
Because our response variable, that is, prevalence of self-reported asthma, is dichotomous, we use logistic regression to estimate the effects of cooking smoke (biomass and solid fuel use vs. cleaner fuel use) and tobacco smoke (current smoking vs. not smoking) on asthma prevalence, with the other 12 socioeconomic and demographic variables mentioned above as controls. Because of large sex differentials in the exposure to cooking smoke and tobacco smoke, the analysis is carried out separately for women and men. Results are presented in the form of odds ratios (ORs) with 95% confidence intervals (95%CI). The estimation of confidence intervals takes into account design effects due to clustering at the level of the primary sampling unit. All analyses including the logistic regression models were done using the SPSS statistical software package Version 16.
Before carrying out the multivariate models, we tested for the possibility of multicollinearity between the predictor variables. In the correlation matrix of predictor variables, all pairwise Pearson correlation coefficients were <0.5, suggesting that multicollinearity is not a problem. In the survey, certain states and certain categories of households were oversampled. In all our analysis, weights are used to restore the representativeness of the sample (41).
Ethical Consideration
The survey got ethical clearance from the International Institute for Population Science’s Ethical Review Board. The analysis presented in this study is secondary analysis of existing survey data with all identifying information removed. The survey personnel had obtained informed consent from each respondent before asking questions.
Results
Profile of the Sample Population
Table 1 shows the sample distribution by selected characteristics. Women and men populations are almost equally distributed in most of the parameters. Almost 70% of the sample population lives in households which use biomass and solid fuels, and only about 30% lives in households using cleaner fuels. As expected, the proportion of women and men declines by age. Of the sample, 87% of women and 76% of men were currently married, and almost one-fourth of the men were not married or were single at the time of the survey. Two out of three of the sample population lives in rural areas. More than two-fifth of the women and more than one-fifth of the men are illiterate, and only 15% of men have high school complete or above education. Religion and caste/tribe distribution shows that over four out of five of the sample population belong to Hindu religion and one out of four belongs to a scheduled caste or scheduled tribe. Two out of five of the sample population live in households with the lowest wealth quintile, and one out of four lives in a household with the highest wealth quintile. About half of the sample population lives in pucca (higher-quality) houses, and 29% of women and 45% men live in houses where the place for cooking is inside the house, without a separate room.
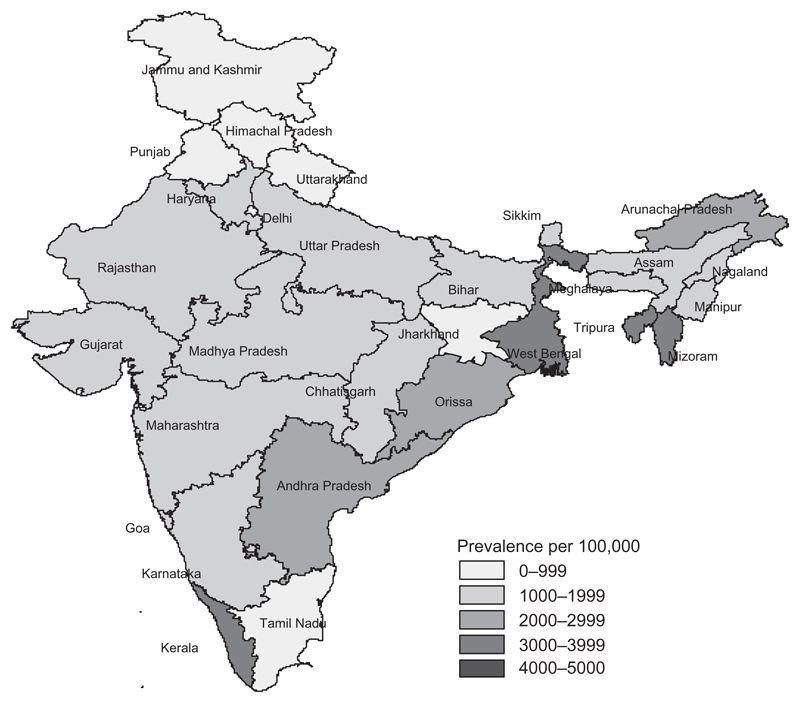
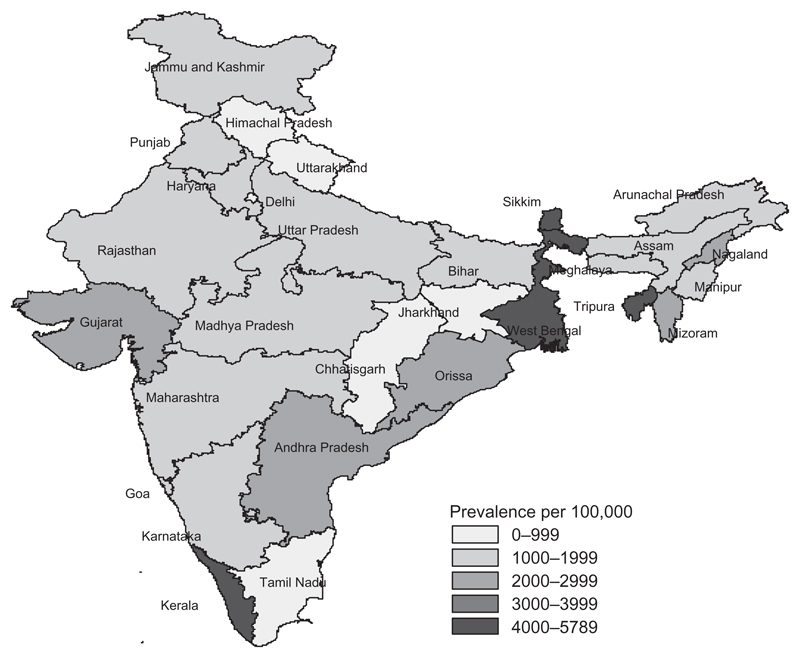
Prevalence of Self-Reported Asthma among Adult Women and Men
Table 2 shows that the prevalence of asthma is higher among women (1.9%) than among men (1.8%) and higher in rural areas (2.0%) than in urban areas (1.8%). Prevalence of asthma in urban and rural India is depicted in Figures 1 and 2, respectively. Prevalence of asthma increases with increasing age both among women and men. By type of cooking fuel, women and men living in households using biomass and solid fuels are more likely to suffer from asthma (2.0% each) than are those living in households using cleaner fuels. Women (3.9%) and men (2.3%) who currently smoke are also much more likely to suffer from asthma than are those who currently does not smoke. The prevalence of asthma is somewhat higher among women who live in houses with fewer than two persons per room (2.3%) and who live in a nuclear family (2.0%). Women (2.9%) and men (5.0%) who are widowed/divorced/separated or deserted are more likely to suffer from asthma than are those who are not married or are currently married. Illiterate women and men are more likely to suffer from asthma than those with high school complete or above education. The prevalence of self-reported asthma is considerably higher among women and men living in households where cooking is done in a separate building and the highest among men belonging to households with a lowest wealth quintile. The prevalence of asthma among women/men is also higher among those living in semi-pucca/kachcha houses. Region wise, the prevalence of self-reported asthma is the highest in the eastern region and the lowest in the central region of India among both women and men.
Table 2.
Self-reported asthma prevalence among adult women and men aged 20–49 years by selected characteristics in India, 2005–2006.
| Woman |
Man |
|||
|---|---|---|---|---|
| Characteristics | Asthma prevalence (%) | λ2 p-value | Asthma prevalence (%) | λ2 p-value |
| Cooking smoke | .002 | <.0001 | ||
| Cleaner fuels | 1.7 | 1.4 | ||
| Biomass and solid fuels | 2.0 | 2.0 | ||
| Tobacco smoke | <.0001 | <.0001 | ||
| No smoking | 1.9 | 1.4 | ||
| Currently smoking | 3.9 | 2.3 | ||
| Age | <.0001 | <.0001 | ||
| 20–29 | 1.1 | 1.0 | ||
| 30–39 | 2.1 | 1.8 | ||
| 40–49 | 3.1 | 3.1 | ||
| Marital status | <.0001 | <.0001 | ||
| Currently married | 1.9 | 1.9 | ||
| Widowed/divorced/separated/deserted | 2.9 | 5.5 | ||
| Not married | 1.1 | 1.1 | ||
| Education | <.0001 | <.0001 | ||
| Illiterate | 2.1 | 2.6 | ||
| Below middle school | 2.1 | 2.3 | ||
| Middle school complete | 1.7 | 1.5 | ||
| High school complete or above | 1.4 | 0.9 | ||
| Religion | .012 | .002 | ||
| Hindu | 1.9 | 1.7 | ||
| Muslim | 2.2 | 2.3 | ||
| Others | 2.0 | 1.6 | ||
| Caste/tribe | .0001 | <.0001 | ||
| Scheduled castes | 1.7 | 1.9 | ||
| Scheduled tribes | 1.9 | 2.3 | ||
| Other backward class | 1.7 | 1.4 | ||
| Others | 2.2 | 1.9 | ||
| House type | .131 | <.0001 | ||
| Pucca | 1.9 | 1.5 | ||
| Semi-pucca/Kachcha | 2.0 | 2.0 | ||
| Place for cooking | <.0001 | <.0001 | ||
| In the house, separate room | 1.7 | 1.8 | ||
| In the house, no separate room | 1.9 | 1.6 | ||
| In a separate building | 2.5 | 2.5 | ||
| Outdoor/other | 1.9 | 1.9 | ||
| Crowding | <.0001 | .731 | ||
| <2 persons per room | 2.3 | 1.7 | ||
| 2–4 persons per room | 1.9 | 1.8 | ||
| 4 or more persons per room | 1.7 | 1.8 | ||
| Household structure | .033 | <.0001 | ||
| Nuclear | 2.0 | 2.0 | ||
| Joint | 1.8 | 1.5 | ||
| Wealth index | .256 | <.0001 | ||
| Lowest | 1.9 | 2.7 | ||
| Second | 2.1 | 1.9 | ||
| Middle | 1.9 | 1.6 | ||
| Fourth | 1.9 | 1.7 | ||
| Highest | 1.8 | 1.3 | ||
| Residence | .083 | <.0001 | ||
| Urban | 1.8 | 1.4 | ||
| Rural | 2.0 | 2.0 | ||
| Region | <.0001 | <.0001 | ||
| North | 1.4 | 1.5 | ||
| Northeast | 2.1 | 1.8 | ||
| Central | 1.3 | 1.3 | ||
| East | 2.6 | 2.5 | ||
| West | 1.9 | 2.1 | ||
| South | 2.1 | 1.5 | ||
| Total prevalence | 1.9 | 1.8 | ||
| Number | 99,574 | 56,742 | ||
For definition of variables see Table 1.
Figure 1.
Urban prevalence of asthma in India, 2005–2006.
Figure 2.
Rural prevalence of asthma in India, 2005–2006.
Effects of Cooking Smoke, Tobacco Smoke, and Control Variables on Self-Reported Asthma among Women
Table 3 shows the estimated effects of cooking smoke, tobacco smoke, and selected socioeconomic and demographic factors on the prevalence of asthma among women in alternative models. Model 1 in Table 3 shows that unadjusted odds of suffering from asthma are almost 1.2 times higher among women living in households using biomass and solid fuels for cooking than among those living in households using cleaner fuels for cooking (OR: 1.17; 95%CI: 1.05–1.29). Controlling for exposure to tobacco smoke (in Model 2) reduces the effect of biomass fuel use on asthma prevalence slightly (OR: 1.14; 95%CI: 1.03–1.27). The effect of biomass fuel use remains virtually unchanged (OR: 1.17; 95%CI: 1.05–1.29) when age is additionally controlled in Model 3. Even when the 12 socioeconomic control variables are included in Model 4, cooking with biomass and solid fuels still has a large and statistically significant effect (OR: 1.26; 95%CI: 1.06–1.49) on the risk of asthma among women.
Table 3.
Unadjusted and adjusted effects (odds ratio (OR) and 95% confidence interval (CI)) of cooking smoke, tobacco smoke, and other factors on asthma among adult women in India, 2005–2006.
| Characteristics | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|
| Cooking smoke | ||||
| Cleaner fuelsR | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] |
| Biomass and solid fuels | 1.17 [1.05–1.29] | 1.14 [1.03–1.27] | 1.17 [1.06–1.30] | 1.26 [1.06–1.49] |
| Tobacco smoke | ||||
| No smokingR | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] |
| Currently smoking | 2.10 [1.65–2.68] | 2.03 [1.59–2.59] | 1.61 [1.26–2.05] | 1.72 [1.34–2.21] |
| Age | ||||
| 20–29R | 1.00 [reference] | 1.00 [reference] | ||
| 30–39 | 1.90 [1.69–2.14] | 1.77 [1.56–2.01] | ||
| 40–49 | 2.76 [2.45–3.10] | 2.55 [2.24–2.91] | ||
| Place for cooking | ||||
| In the house, separate roomR | 1.00 [reference] | |||
| In the house, no separate room | 1.15 [1.01–1.30] | |||
| In a separate building | 1.18 [0.98–1.41] | |||
| Outdoor/other | 1.01 [0.87–1.17] | |||
| Wealth index | ||||
| LowestR | 1.00 [reference] | |||
| Second | 1.05 [0.89–1.23] | |||
| Middle | 0.97 [0.82–1.16] | |||
| Fourth | 1.06 [0.85–1.31] | |||
| Highest | 1.08 [0.81–1.42] | |||
| Region | ||||
| North | 0.61 [0.51–0.73] | |||
| Northeast | 0.94 [0.72–1.23] | |||
| Central | 0.62 [0.53–0.73] | |||
| East | 1.15 [1.00–1.32] | |||
| West | 0.86 [0.73–1.01] | |||
| SouthR | 1.00 [reference] | |||
| Number of women | 100,382 | 100,382 | 100,382 | 95,501 |
Notes: Model 1 unadjusted. Model 2 adjusted for tobacco smoke only. Model 3 adjusted for tobacco smoke and age. Model 4 adjusted for variables in Model 3 and other characteristics: marital status, education, religion, caste/tribe, house type, crowding, household structure, and residence. For definition of variables see Table 1.
Reference category.
Women who currently smoke tobacco are at a considerably higher risk of suffering from asthma (OR: 2.10; 95%CI: 1.65–2.68) than are those who currently does not smoke in the unadjusted Model 1 (Table 3). This effect is reduced somewhat when the effect of cooking smoke is controlled (OR: 2.03; 95%CI: 1.59–2.59) and reduced further when women’s age is additionally controlled in Model 3 (OR: 1.61; 95%CI: 1.26–2.05). In the full model (Model 4), when the effects of cooking fuel type and 12 other variables are controlled, the odds of suffering from asthma are 1.7 times (95%CI: 1.34–2.21) higher among women who are current smokers than among the nonsmoking women.
The discussion of the adjusted effects of the control variables focuses on the full model (Model 4) in Table 3. With other variables controlled, age has a positive and statistically significant effect on the prevalence of asthma among women. Women living in households where the place for cooking is in the house with no separate kitchen have a higher prevalence of asthma than do those living in households with a separate kitchen. Women living in households belonging to the highest wealth quintile have higher risk of asthma than those living in households belonging to the lowest wealth quintile, but the effect is not statistically significant. By geographic region, women residing in the eastern region have higher risk of asthma than do those in other regions. The likelihood of asthma among women does not vary significantly by other characteristics.
Effects of Cooking Smoke, Tobacco Smoke, and Control Variables on Self-Reported Asthma among Men
Table 4 shows the estimated effects of cooking smoke, tobacco smoke, and selected socioeconomic and demographic variables on the prevalence of asthma among men in alternative models. Model 1 in Table 4 shows that unadjusted odds of suffering from asthma are almost 1.4 times higher among men living in households using biomass and solid fuels for cooking than among those living in households using cleaner fuels for cooking (OR: 1.39; 95%CI: 1.21–1.61). Controlling for exposure to tobacco smoke (in Model 2) reduces the effect of biomass fuel use on asthma prevalence slightly (OR: 1.30; 95%CI: 1.13–1.51). The effect of biomass fuel use remains virtually unchanged (OR: 1.32; 95%CI: 1.14–1.51) when age is additionally controlled in Model 3. However, when the 12 socioeconomic control variables are included in Model 4, cooking with biomass and solid fuels does not have a statistically significant effect (OR: 0.98; 95%CI: 0.77–1.24) on the prevalence of asthma among men.
Table 4.
Unadjusted and adjusted effects (OR and 95% CI) of cooking smoke, tobacco smoke, and other factors on asthma among adult men in India, 2005–2006.
| Characteristics | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|
| Cooking smoke | ||||
| Cleaner fuelR | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] |
| Biomass and solid fuels | 1.39 [1.21–1.61] | 1.30 [1.13–1.51] | 1.32 [1.14–1.51] | 0.98 [0.77–1.24] |
| Tobacco smoke | ||||
| No smokingR | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] |
| Currently smoking | 1.64 [1.45–1.86] | 1.59 [1.40–1.80] | 1.42 [1.25–1.61] | 1.35 [1.19–2.25] |
| Age | ||||
| 20–29R | 1.00 [reference] | 1.00 [reference] | ||
| 30–39 | 1.41 [1.52–2.15] | 1.83 [1.49–2.25] | ||
| 40–49 | 3.13 [2.65–3.68] | 3.13 [2.55–3.84] | ||
| Place for cooking | ||||
| In the house, separate roomR | 1.00 [reference] | |||
| In the house, no separate room | 1.04 [0.88–1.23] | |||
| In a separate building | 1.13 [0.89–1.45] | |||
| Outdoor/other | 1.03 [0.84–1.25] | |||
| Wealth index | ||||
| LowestR | 1.00 [reference] | |||
| Second | 0.69 [0.56–0.85] | |||
| Middle | 0.67 [0.52–0.84] | |||
| Fourth | 0.72 [0.53–0.96] | |||
| Highest | 0.57 [0.39–0.84] | |||
| Region | ||||
| North | 0.97 [0.76–1.24] | |||
| Northeast | 1.21 [0.82–1.78] | |||
| Central | 0.75 [0.59–0.97] | |||
| East | 1.23 [0.98–0.56] | |||
| West | 1.45 [1.14–1.84] | |||
| SouthR | 1.00 [reference] | |||
| Number of men | 56,739 | 56,739 | 56,739 | 54,476 |
Notes: Model 1 unadjusted. Model 2 adjusted for tobacco smoke. Model 3 adjusted for tobacco smoke and age. Model 4 adjusted for variables in Model 3 and other characteristics: marital status, education, religion and caste/tribe, house type, crowding, household structure, and residence. For definition of variables see Table 1.
Reference category.
Men who currently smoke tobacco are at a considerably higher risk of suffering from asthma (OR: 1.64; 95%CI: 1.45–1.86) than are those who currently does not smoke, in unadjusted Model 1. This effect is somewhat reduced when the effect of cooking smoke is controlled (OR: 1.59; 95%CI: 1.40–1.80) in Model 2 and reduced further when respondent’s age is additionally controlled (OR: 1.42; 95%CI: 1.25–1.61) in Model 3. In the full model (Model 4), when the effects of cooking fuel type and the 12 other variables are controlled, the odds of suffering from asthma are 1.4 times (95%CI: 1.49–2.25) higher among the men who are current smokers with reference to men who do not smoke.
The discussion of the adjusted effects of the control variables focuses on the full model (Model 4) in Table 4. With other variables controlled, age has a positive and statistically significant effect on the prevalence of asthma among men. A higher wealth status of the household was associated with lower asthma risk among men. By geographic region, men residing in the western region have significantly higher prevalence of asthma than do those in other regions. The likelihood of the risk of asthma among men does not vary significantly by other characteristics.
Combined Effect of Cooking Smoke and Tobacco Smoke on Self-Reported Asthma
The combined effect of cooking smoke and tobacco smoke on the risk of asthma among both women and men was found more profound even after controlling for socioeconomic and demographic characteristics (Tables 5 and 6). The odds of suffering from asthma is more than 2 times higher among women (OR: 2.16; 95%CI: 1.58–2.94; p < .0001) and 1.3 times higher among men (OR: 1.34; 95%CI: 1.04–1.72; p = .024) when they are exposed to biomass and solid fuel use and tobacco smoke combined, with reference to those women and men who are not exposed to biomass and solid fuel and do not smoke.
Table 5.
Adjusted effect (OR and 95% CI) of combination of cooking smoke and tobacco smoke on asthma among adult women in India, 2005–2006.
| Predictors | Number of cases | Distribution (%) | Asthma prevalence (%) | Adjusted ORa (95% CI) |
|---|---|---|---|---|
| Biomass and solid fuel use and tobacco smoke combined | 1752 | 1.8 | 3.9 | 2.16 [1.58–2.94] p < .0001 |
| Either biomass and solid fuel use or tobacco smoke | 68,246 | 68.5 | 1.9 | 1.26 [1.06–1.50] p < .0001 |
| Neither biomass and solid fuel use nor tobacco smokeR | 29,563 | 29.7 | 1.7 | 1.00 [reference] |
Reference category.
Adjusted for all background characteristics: age, marital status, education, religion, caste/tribe, house type, place for cooking, crowding, household structure, wealth index, residence, and regions.
Table 6.
Adjusted effect (OR and 95% CI) of combination of cooking smoke and tobacco smoke on asthma among adult men in India, 2005–2006.
| Predictors | Number of cases | Distribution (%) | Asthma prevalence (%) | Adjusted ORa (95% CI) |
|---|---|---|---|---|
| Biomass and solid fuel use and currently smoking combined | 16,254 | 28.7 | 2.6 | 1.34 [1.04–1.72] p = .024 |
| Either biomass and solid fuel use or currently smoking | 27,521 | 48.5 | 1.5 | 0.93 [0.75–1.17] p = .554 |
| Neither biomass and solid fuel use nor tobacco smokeR | 12,955 | 22.8 | 1.3 | 1.00 [reference] |
Reference category.
Adjusted for all background characteristics: age, marital status, education, religion, caste/tribe, house type, place for cooking, crowding, household structure, wealth index, residence, and regions.
Discussion
Findings from this study suggest that exposure to cooking smoke is strongly associated with the prevalence of self-reported asthma among adult women in India but not among men, and this association is significant and is independent of exposure to tobacco smoke, age, and other factors. Current tobacco smoking also has a substantial effect. However, the combined effects of both cooking smoke and tobacco smoke on self-reported asthma are greater and more significant for women than for men.
The finding that the effect of cooking smoke is greater for women and nonexistent for men is consistent with expectation, because women are more exposed than men to cooking smoke. The magnitude of association between exposure and asthma in women is consistent with that found in other studies (10, 49, 80–82). Because of women’s customary involvement in cooking, their exposure is much higher than men’s; and also due to sex differences in nutritional status, women’s compromised respiratory system from cooking smoke, and access to treatment and care, the effects of cooking smoke and tobacco smoking on asthma are likely to be higher among women (10).
The estimate of asthma prevalence in this study may be somewhat biased because of the fact that the effect of cooking smoke on asthma is collective over time and people might have shifted their cooking fuel use from biomass and solid fuels to cleaner fuels (10). There could be another reason for the estimate being biased, as asthma seemed more likely to be underreported by persons from households that use biomass and solid fuels. Conversely, the estimated effect of asthma may be again biased because households that use biomass and solid fuels are more likely to report some other disease condition such as chronic bronchitis or chronic obstructive pulmonary disease with similar symptoms as asthma. In cases where asthma might have been confused with some other chronic respiratory disorder, it is not possible from our data to separate the effect of asthma from the effect of some other condition with similar symptoms. Moreover, we could not control for the extent of use of medical services in connection with asthma directly in this study, although our set of control variables includes several measures of socioeconomic status correlated with access to and use of medical services.
It is also important to recognize here that self-report of asthma is not as accurate as clinical measures of asthma, but as there is no such golden standard in asthma diagnosis, validated questions perhaps are more accurate than the clinical measures of asthma. There is a risk of under-reporting of mild asthma in self-reporting as well. Hence, though respiratory health can be assessed through standardized questionnaires—a simple and relatively inexpensive method for collecting data—it should be complemented whenever and wherever possible with objective measurements (e.g. spirometry) (47). Smoking behavior of the respondents in this study was also assessed by self-report obtained during personal interview. It may be possible that the use of self-reported smoking histories and lack of information on past smoking have resulted in nondifferential misclassification of smoking status, which might have produced an underestimate of the association of smoking with self-reported asthma in this study.
Nevertheless, in India, where clinical data on asthma are mostly unavailable or very weak, this reported prevalence of asthma in a nationally representative sample of adult women and men provided an important estimate of the effect of biomass and solid fuel exposure on asthma risk. However, well-designed epidemiologic studies with better measures of smoke exposure and clinical measures of asthma are needed to validate these findings and to better understand the pathogenesis of asthma among adult women and men in India.
Conclusions
The findings from this study suggest that there is an urgent need for public information campaigns designed to inform people about the risks of exposure to cooking smoke and programs to promote improved cooking stoves designed to reduce exposure to smoke by means of improved combustion and improved venting (10). Interventions that reduce the burden of biomass smoke exposure also are urgently required in India (31). Feasible low-cost measures that could reduce the devastating health outcomes of exposure to indoor biomass smoke include cooking outdoors, cooking for shorter periods, improving ventilation by adding more windows around cooking areas or by building chimneys above stoves, improving stove construction and technology, and using cleaner or energy-efficient fuels such as LPG, ethanol, or biogas (32). Substitution of traditional open fires with locally produced improved stoves has been shown to have significant health benefits (83–85). For making community development programs effective, local needs and community participation should be given high priority (10). Also, programs to reduce exposure to tobacco smoke should be promoted, in addition to strengthening asthma prevention and treatment programs. Further, it is also important to increase awareness about the health effects of solid fuel smoke inhalation among physicians and health administrators as well (31), which may improve diagnosis and treatment of affected patients and trigger preventive actions through education, research, and policy change. A focus on community education on the harmful effect of biomass fuel smoke exposure may mobilize demand for improved stove installations and better household ventilation. These findings may also motivate more community development programs and, specifically, strategies for poverty reduction, which are currently underway in India.
Acknowledgments
I would like to acknowledge the support of Macro International (Calverton, MD, USA) and International Institute for Population Sciences (Mumbai, India) for providing access to the 2005–2006 Indian National Family Health Survey 3 data. Further, valuable comments and suggestions from two anonymous referees are also acknowledged.
Footnotes
Declaration of Interest
The author reports no conflicts of interest. The author alone is responsible for the content and writing of this article.
References
- 1.Anderson HR. Air pollution and trends in asthma. Ciba Found Symp. 1997;206:190–202. 203–207. [PubMed] [Google Scholar]
- 2.Platts-Mills TAE, Woodfolk J. Rise in asthma cases. Science. 1997;278:1001. doi: 10.1126/science.278.5340.997c. [DOI] [PubMed] [Google Scholar]
- 3.World Resources Institute. World Resources 1998–1999: A Guide to the Global Environment. Oxford: Oxford University Press; 1998. [Google Scholar]
- 4.Pearce N, Douwes J, Beasley R. The rise and rise of asthma: a new paradigm for the new millennium? J Epidemiol Biostat. 2000;5:5–16. [PubMed] [Google Scholar]
- 5.Bach J-F. The effect of infections on susceptibility to autoimmune and allergic diseases. N Engl J Med. 2002;347:911–920. doi: 10.1056/NEJMra020100. [DOI] [PubMed] [Google Scholar]
- 6.Isolauri E, Huurre A, Salminen S, Impivaara O. The allergy epidemic extends beyond the past few decades. Clin Exp Allergy. 2004;34:1007–1010. doi: 10.1111/j.1365-2222.2004.01999.x. [DOI] [PubMed] [Google Scholar]
- 7.Beggs PJ, Bambrick HJ. Is the global rise of asthma an early impact of anthropogenic climate change? Environ Health Perspect. 2005;113:915–919. doi: 10.1289/ehp.7724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Braman SS. The global burden of asthma. Chest. 2006;130:4S–12S. doi: 10.1378/chest.130.1_suppl.4S. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organisation. Chronic respiratory diseases and arthritis prevention of allergy and allergic asthma. Based on the WHO/WAO meeting on the prevention of allergy and allergic asthma; 8–9 January 2002; Geneva. Management of Noncommunicable Diseases Department; 2002. WHO/NMH/MNC/CRA/03.2. [Google Scholar]
- 10.Mishra V. Effect of indoor air pollution from biomass combustion on prevalence of asthma in the elderly. Environ Health Perspect. 2003;111:71–77. doi: 10.1289/ehp.5559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee. Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema. Lancet. 1998;351:1225–1232. [PubMed] [Google Scholar]
- 12.Bjorksten B. The environmental influence on childhood asthma. Allergy. 1999;54:17–23. doi: 10.1111/j.1398-9995.1999.tb04383.x. [DOI] [PubMed] [Google Scholar]
- 13.Koren HS, Utell MJ. Asthma and the environment. Environ Health Perspect. 1997;105:534–537. doi: 10.1289/ehp.97105534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baldi I, Tessier JF, Kauffmann F, Jacqmin-Gadda H, Nejjari C, Salamon R. Prevalence of asthma and mean levels of air pollution: results from the French PAARC survey. Eur Respir J. 1999;14:132–138. doi: 10.1034/j.1399-3003.1999.14a22.x. [DOI] [PubMed] [Google Scholar]
- 15.Bates DV. Observations on asthma. Environ Health Perspect. 1995;103(Suppl. 6):243–247. doi: 10.1289/ehp.95103s6243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Castellsague J, Sunyer J, Saez M, Anto JM. Short-term association between air pollution and emergency room visits for asthma in Barcelona. Thorax. 1995;50:1051–1056. doi: 10.1136/thx.50.10.1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.de Diego Damia A, Leon Fabregas M, Perpina Tordera M, Compte Torrero L. Effects of air pollution and weather conditions on asthma exacerbation. Respiration. 1999;66:52–58. doi: 10.1159/000029337. [DOI] [PubMed] [Google Scholar]
- 18.Greer JR, Abbey DE, Burchette RJ. Asthma related to occupational and ambient air pollutants in nonsmokers. J Occup Med. 1993;35:909–915. doi: 10.1097/00043764-199309000-00014. [DOI] [PubMed] [Google Scholar]
- 19.Zhang J, Qian Z, Kong L, Zhou L, Yan L, Chapman RS. Effects of air pollution on respiratory health of adults in three Chinese cities. Arch Environ Health. 1999;54:373–381. doi: 10.1080/00039899909603368. [DOI] [PubMed] [Google Scholar]
- 20.Smith KR, Samet JM, Romieu I, Bruce N. Indoor air pollution in developing countries and acute lower respiratory infections in children. Thorax. 2000;55:518–532. doi: 10.1136/thorax.55.6.518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Albalak R, Frisancho AR, Keeler GJ. Domestic biomass fuel combustion and chronic bronchitis in two rural Bolivian villages. Thorax. 1999;54:1004–1008. doi: 10.1136/thx.54.11.1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bruce N, Neufeld L, Boy E, West C. Indoor biofuel air pollution and respiratory health: the role of confounding factors among women in highland Guatemala. Int J Epidemiol. 1998;27:454–458. doi: 10.1093/ije/27.3.454. [DOI] [PubMed] [Google Scholar]
- 23.Holdren JP, Smith KR. Energy, the environment, and health. In: Goldemberg J, editor. The World Energy Assessment: Energy and the Challenge of Sustainability. New York, NY: United National Development Programme; 2000. pp. 61–110. [Google Scholar]
- 24.Duflo E, Greenstone M, Hanna R. Cooking stoves, indoor air pollution and respiratory health in rural Orissa. Econ Pol Wkly. 2008;43(32):71–76. [Google Scholar]
- 25.Smith KR. Indoor air pollution in developing countries: recommendations for research. Int J Indoor Environ Health. 2002;3:1–7. doi: 10.1034/j.1600-0668.2002.01137.x. [DOI] [PubMed] [Google Scholar]
- 26.Smith KR. The national burden of disease from indoor air pollution in India. In: Raw G, Aizlewood C, Warren P, editors. Indoor Air 99, the 8th International Conference on Indoor Air Quality and Climate; 1999, August; Edinburgh. London: Construction Research Ltd; 1999. pp. 13–18. [Google Scholar]
- 27.Aggarwal AN, Chaudhry K, Chhabra SK, D’Souza GA, Gupta D, Jindal SK, Katiyar SK, Kumar R, Shah B, Vijayan VK. Prevalence and risk factors for bronchial asthma in Indian adults: a multicentre study. Indian J Chest Dis Allied Sci. 2006;48:13–22. [PubMed] [Google Scholar]
- 28.Saxena S, Dayal V. Total exposure as a basis for the economic valuation of air pollution in India. Energy Environment Monitor. 1997;13(2):93–102. [Google Scholar]
- 29.Akhtar T, Ullah Z, Khan MH, Nazli R. Chronic bronchitis in women using solid biomass fuel in rural Peshawar, Pakistan. Chest. 2007;132:1472–1475. doi: 10.1378/chest.06-2529. [DOI] [PubMed] [Google Scholar]
- 30.Bruce N, Perez-Padilla R, Albalak R. Indoor air pollution in developing countries: a major environmental and public health challenge. Bull WHO. 2000;78:1080–1092. [PMC free article] [PubMed] [Google Scholar]
- 31.Salvi S, Barnes PJ. Is exposure to biomass smoke the biggest risk factor for COPD globally. Chest. 2010;138:3–6. doi: 10.1378/chest.10-0645. [DOI] [PubMed] [Google Scholar]
- 32.Salvi S, Barnes PJ. Chronic obstructive pulmonary disease in non-smokers. Lancet. 2009;374:733–743. doi: 10.1016/S0140-6736(09)61303-9. [DOI] [PubMed] [Google Scholar]
- 33.Mishra VK, Retherford RD, Smith KR. Biomass cooking fuels and prevalence of tuberculosis in India. Int J Infect Dis. 1999;3:119–129. doi: 10.1016/s1201-9712(99)90032-2. [DOI] [PubMed] [Google Scholar]
- 34.Perez-Padilla R, Perez-Guzman C, Baez-Saldana R, Torres-Cruz A. Cooking with biomass stoves and tuberculosis: a case-control study. Int J Tuberc Lung Dis. 2001;5:1–7. [PubMed] [Google Scholar]
- 35.Reddy TS, Guleria R, Sinha S, Sharma SK, Pande JN. Domestic cooking fuel and lung functions in healthy non-smoking women. Indian J Chest Dis Allied Sci. 2004;46:85–90. [PubMed] [Google Scholar]
- 36.Pokharel PK, Kabra SK, Kapoor SK, Pandey RM. Risk factors associated with bronchial asthma in school going children of rural Haryana. Indian J Pediatr. 2001;68:103–106. doi: 10.1007/BF02722022. [DOI] [PubMed] [Google Scholar]
- 37.Behera D, Chakrabarti T, Khanduja KL. Effect of exposure to domestic cooking fuels in bronchial asthma. Indian J Chest Dis Allied Sci. 2001;43:27–31. [PubMed] [Google Scholar]
- 38.Gupta D, Aggarwal AN, Chaudhary J, Jindal SK. Domestic fuel combustion and morbidity from asthma amongst nonsmoking women. Lung India. 1999;17:10–14. [Google Scholar]
- 39.Jindal SK, Jha LK, Gupta D. Bronchial hyper-responsiveness of women with asthma exposed to environmental tobacco smoke. Indian J Chest Dis Allied Sci. 1999;41:75–82. [PubMed] [Google Scholar]
- 40.Singh H, Soni RK, Gill PJS. Epidemiological and risk factors in childhood bronchial asthma. Indian J Community Med. 1998;23:42–44. [Google Scholar]
- 41.IIPS and Macro International. National Family Health Survey (NFHS-3), 2005–2006: India. Mumbai: International Institute for Population Sciences; 2007. [Google Scholar]
- 42.WHO. Health and Environment for Sustainable Development: Five Years after the Earth Summit. Geneva: World Health Organization; 1997. [Google Scholar]
- 43.Ezzati M, Kammen D. Indoor air pollution from biomass combustion and acute respiratory infections in Kenya: an exposure-response study. Lancet. 2001;358:619–624. doi: 10.1016/s0140-6736(01)05777-4. [DOI] [PubMed] [Google Scholar]
- 44.Regalado J, Perez-Padilla R, Sansores R, Ramirez JIP, Brauer M, Paré P, Vedal S. The effect of biomass burning on respiratory symptoms and lung function in rural Mexican women. Am J Respir Crit Care Med. 2006;174:901–905. doi: 10.1164/rccm.200503-479OC. [DOI] [PubMed] [Google Scholar]
- 45.Boy E, Bruce N, Delgado H. Birth weight and exposure to kitchen wood smoke during pregnancy in rural Guatemala. Environ Health Perspect. 2002;110(1):109–114. doi: 10.1289/ehp.02110109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Masera O, Saatkamp BD, Kammen D. From linear fuel switching to multiple cooking strategies: a critique and alternative to the energy ladder model. World Dev. 2000;28:2083–2103. [Google Scholar]
- 47.Torres-Duque C, Maldonado D, Perez-Padilla R, Ezzati M, Viegi G, On behalf of the Forum of International Respiratory Societies (FIRS) Task Force on Health Effects of Biomass Exposure Biomass fuels and respiratory diseases: a review of the evidence. Proc Am Thorac Soc. 2008;5:577–590. doi: 10.1513/pats.200707-100RP. [DOI] [PubMed] [Google Scholar]
- 48.Po JYT, FitzGerald JM, Carlsten C. Respiratory disease associated with solid biomass fuel exposure in rural women and children: systematic review and meta analysis. Thorax. 2011;66:232–239. doi: 10.1136/thx.2010.147884. [DOI] [PubMed] [Google Scholar]
- 49.Behera D, Dash S, Malik S. Blood carboxyhaemoglobin levels following acute exposure to smoke of biomass fuel. Indian J Med Res. 1988;88:522–542. [PubMed] [Google Scholar]
- 50.Behera D, Sood P, Singh S. Passive smoking, domestic fuels and lung function in north Indian children. Indian J Chest Dis Allied Sci. 1998;40:89–98. [PubMed] [Google Scholar]
- 51.Fagbule D, Ekanem EE. Some environmental risk factors for childhood asthma: a case control study. Ann Trop Paediatr. 1994;14:15–19. doi: 10.1080/02724936.1994.11747686. [DOI] [PubMed] [Google Scholar]
- 52.Noorhassim I, Rampal KG, Hashim JH. The relationship between prevalence of asthma and environmental factors in rural households. Med J Malaysia. 1995;50:263–267. [PubMed] [Google Scholar]
- 53.Qureshi KA. Domestic smoke pollution and prevalence of chronic bronchitis/asthma in a rural area of Kashmir. Indian J Chest Dis Allied Sci. 1994;36:61–72. [PubMed] [Google Scholar]
- 54.Mohammed N, Ng’ang’a L, Odhiambo J, Nyamwaya J, Menzies R. Home environment and asthma in Kenyan school children: a case-control study. Thorax. 1995;50:74–78. doi: 10.1136/thx.50.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pistelly R. Wood smoke and asthma: a controversial issue. Am J Respir Crit Care Med. 1997;155:A941. [Google Scholar]
- 56.Thorn J, Brisman J, Toren K. Adult-onset asthma is associated with self-reported mold or environmental tobacco smoke exposures in the home. Allergy. 2001;56:287–292. doi: 10.1034/j.1398-9995.2001.00805.x. [DOI] [PubMed] [Google Scholar]
- 57.Xu X, Niu T, Christiani DC, Weiss ST, Chen C, Zhou Y, Fang Z, Jiang Z, Liang W, Zhang F. Occupational and environmental risk factors for asthma in rural communities in China. Int J Occup Environ Health. 1996;2:172–176. doi: 10.1179/oeh.1996.2.3.172. [DOI] [PubMed] [Google Scholar]
- 58.Barry AC, Mannino DM, Hopenhayn C, Bush H. Exposure to indoor biomass fuel pollutants and asthma prevalence in Southeastern Kentucky: results from the Burden of Lung Disease (BOLD) study. J Asthma. 2010;47(7):735–741. doi: 10.3109/02770903.2010.485661. [DOI] [PubMed] [Google Scholar]
- 59.Azizi BH, Henry RL. The effects of indoor environmental factors on respiratory illness in primary school children in Kuala Lumpur. Int J Epidemiol. 1991;20:144–150. doi: 10.1093/ije/20.1.144. [DOI] [PubMed] [Google Scholar]
- 60.Maier WC, Arrighi HM, Morray B, Llewellyn C, Redding GJ. Indoor risk factors for asthma wheezing among Seattle school children. Environ Health Perspect. 1997;105:208–214. doi: 10.1289/ehp.97105208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wafula EM, Onyango FE, Thairu H, Boleji JSM, Hoek F, Ruigewaard P, Kagwanja S, de Koning H, Pio A, Kimani E, Ombui P, et al. Indoor Air Pollution in a Kenyan Village. East Afr Med J. 1990;67:24–32. [PubMed] [Google Scholar]
- 62.Volkmer RE, Ruffin RE, Wigg NR, Davies N. The prevalence of respiratory symptoms in South Australian preschool children. II. Factors associated with indoor air quality. J Paediatr Child Health. 1995;31:116–120. doi: 10.1111/j.1440-1754.1995.tb00758.x. [DOI] [PubMed] [Google Scholar]
- 63.von Mutius E, Illi S, Nicolai T, Martinez FD. Relation of indoor heating with asthma, allergic sensitization, and bronchial responsiveness: survey of children in south Bavaria. Br Med J. 1996;312:1448–1450. doi: 10.1136/bmj.312.7044.1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Azizi BH, Zulkifli HI, Kasim S. Indoor air pollution and asthma in hospitalized children in a tropical environment. J Asthma. 1995;32:413–418. doi: 10.3109/02770909409077752. [DOI] [PubMed] [Google Scholar]
- 65.Flodin U, Jonsson P, Ziegler J, Axelson O. An epidemiologic study of bronchial asthma and smoking. Epidemiology. 1995;6:503–505. doi: 10.1097/00001648-199509000-00007. [DOI] [PubMed] [Google Scholar]
- 66.Strachan DP, Cook DG. Parental smoking and childhood asthma: longitudinal and case-control studies. Thorax. 1998;53:204–212. doi: 10.1136/thx.53.3.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Piipari R, Jaakkola JJK, Jaakkola N, Jaakkola MS. Smoking and asthma in adults. Eur Respir J. 2004;24:734–739. doi: 10.1183/09031936.04.00116903. [DOI] [PubMed] [Google Scholar]
- 68.Gilliland FD, Islam T, Berhane K, Gauderman WJ, McConnell R, Avol E, Peters JM. Regular smoking and asthma incidence in adolescents. Am J Respir Crit Care Med. 2006;174:1094–1100. doi: 10.1164/rccm.200605-722OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Althuis MD, Sexton M, Prybylski D. Cigarette smoking and asthma symptom severity among adult asthmatics. J Asthma. 1999;36:257–264. doi: 10.3109/02770909909075409. [DOI] [PubMed] [Google Scholar]
- 70.Beeh KM, Micke P, Ksoll M, Buhl R. Cigarette smoking, but not sensitization to Alternaria, is associated with severe asthma in urban patients. J Asthma. 2001;38:41–49. doi: 10.1081/jas-100000020. [DOI] [PubMed] [Google Scholar]
- 71.Siroux V, Pin I, Oryszczyn MP, Le Moual N, Kauffmann F. Relationships of active smoking to asthma and asthma severity in the EGEA study. Epidemiological Study on the Genetics and Environment of Asthma. Eur Respir J. 2000;15:470–477. doi: 10.1034/j.1399-3003.2000.15.08.x. [DOI] [PubMed] [Google Scholar]
- 72.Ben-Noun L. Is there a relationship between smoking and asthma in adults? J Int Med Res. 1999;27:15–21. doi: 10.1177/030006059902700102. [DOI] [PubMed] [Google Scholar]
- 73.Jindal SK, Gupta D. The relationship between tobacco smoke and bronchial asthma. Indian J Med Res. 2004;120:443–453. [PubMed] [Google Scholar]
- 74.Singh D, Sobti PC, Arora V, Soni RK. Epidemiological study of asthma in rural children. Indian J Community Med. 2002;27:167–170. [Google Scholar]
- 75.Gupta D, Aggarwal AN, Kumar R, Jindal SK. Prevalence of bronchial asthma and association with environmental tobacco smoke exposure in adolescent school children in Chandigarh, North India. J Asthma. 2001;38:501–507. doi: 10.1081/jas-100105871. [DOI] [PubMed] [Google Scholar]
- 76.Chhabra SK, Gupta CK, Chhabra P, Rajpal S. Prevalence of bronchial asthma in school children in Delhi. J Asthma. 1998;35:291–296. doi: 10.3109/02770909809068220. [DOI] [PubMed] [Google Scholar]
- 77.Global Initiative for Asthma. GINA workshop report: global strategy for asthma management and prevention. [Accessed 19 Aug 2011];2011 Available at: http://www.ginasthma.com/wr_clean.pdf.
- 78.Boulet L-P, Lemière C, Archambault F, Carrier G, Descary MC, Deschesnes F. Smoking and asthma: clinical and radiologic features, lung function, and airway inflammation. Chest. 2006;129:661–668. doi: 10.1378/chest.129.3.661. [DOI] [PubMed] [Google Scholar]
- 79.Subramanian SV, Ackerson LK, Subramanyam MA, Wright RJ. Domestic violence is associated with adult and childhood asthma prevalence in India. Int J Epidemiol. 2007;36:569–579. doi: 10.1093/ije/dym007. [DOI] [PubMed] [Google Scholar]
- 80.Hu G, Zhou Y, Tian J, Yao W, Li J, Li B, Ran P. Risk of COPD from exposure to biomass smoke: a meta analysis. Chest. 2010;138:20–31. doi: 10.1378/chest.08-2114. [DOI] [PubMed] [Google Scholar]
- 81.Kurmi OP, Semple S, Simkhada P, Smith WCS, Ayres JG. COPD and chronic bronchitis risk of indoor air pollution from solid fuel: a systematic review and meta-analysis. Thorax. 2010;65:221–228. doi: 10.1136/thx.2009.124644. [DOI] [PubMed] [Google Scholar]
- 82.Behera D, Jindal SK. Respiratory symptoms in Indian women using domestic cooking fuels. Chest. 1991;100:385–388. doi: 10.1378/chest.100.2.385. [DOI] [PubMed] [Google Scholar]
- 83.Smith-Sivertsen T, Díaz E, Pope D, Lie RT, Díaz A, McCracken J, Bakke P, Arana B, Smith KR, Bruce N. Effect of reducing indoor air pollution on women’s respiratory symptoms and lung function: the RESPIRE Randomized Trial, Guatemala. Am J Epidemiol. 2009;170(2):211–220. doi: 10.1093/aje/kwp100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Chapman RS, He X, Blair AE, Lan Q. Improvement in household stoves and risk of chronic obstructive pulmonary disease in Xuanwei, China: retrospective cohort study. BMJ. 2005;331(7524):1050–1056. doi: 10.1136/bmj.38628.676088.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Romieu I, Riojas-Rodríguez H, Marrón-Mares AT, Schilmann A, Perez-Padilla R, Masera O. Improved biomass stove intervention in rural Mexico: impact on the respiratory health of women. Am J Respir Crit Care Med. 2009;180(7):649–656. doi: 10.1164/rccm.200810-1556OC. [DOI] [PubMed] [Google Scholar]