Abstract
Successful propagation of HIV in the human host requires entry into a permissive cell, reverse transcription of viral RNA, integration into the human genome, transcription of the integrated provirus, and assembly/release of new virus particles. Currently, there are antiretrovirals against each of these viral steps, except for provirus transcription. An inhibitor of HIV transcription could both increase potency of treatment and suppress drug-resistant strains. Cellular cyclin-dependent kinase 9 (CDK9) serves as a cofactor for the HIV Tat protein and is required for effective transcription of the provirus. Previous studies have shown that the CDK9 inhibitor Indirubin 3’-monoxime (IM) inhibits HIV transcription in vitro and in short-term in vivo studies of HIV acute infection in humanized mice (PBMC-NSG model), suggesting a therapeutic potential. The objective of this study is to evaluate the toxicity, pharmacokinetics and long-term antiviral activity of IM during chronic HIV infection in humanized mice (HSC-NSG model). We show that IM concentrations above EC50 values are rapidly achieved and sustained for > 3 h in plasma, and that non-toxic concentrations durably reduce HIV RNA levels. In addition, IM enhanced the antiviral activity of antiretrovirals from the reverse transcriptase, protease and integrase inhibitor classes in in vitro infectivity assays. In summary, IM may enhance current antiretroviral treatments and could help achieve a “functional cure” in HIV patients by preventing expression of proviruses.
Introduction
Cellular human positive transcription elongation factor (P-TEFb), composed of cyclin-dependent kinase 9 (CDK9) and cyclin T1, regulates RNA Polymerase II dependent transcription of cellular and integrated HIV genes [1–6]. CDK9, unlike most other CDKs, controls gene transcription and has little effect on cell cycle regulation [7]. Approaches targeting CDK9 in vitro with catalytic inhibitors [8–10], RNAi [11], and direct inhibition using a dominant negative form [12], have all suggested that inhibition of HIV transcription without toxicity might be possible.
Because CDK9 inhibition suppresses transcription of antiapoptotic proteins [13, 14], several CDK9 inhibitors are currently in clinical development for the treatment of cancer [15–24]. However, these inhibitors may have off-target toxicities [18–20, 25–27], suggesting safer CDK9 inhibitors are needed. Indirubin and its derivatives have been used successfully in China for the treatment of chronic myelogenous leukemia [28]. They act by competitively inhibiting ATP binding to the catalytic domain of several CDKs [29]. The indirubin derivative indirubin 3’-monoxime (IM) inhibits CDK9 more potently than other CDKs [30], it is not cytotoxic to primary lymphocytes and macrophages [30, 31], and it is more soluble than indirubin [29]. We [30], and others [31, 32], have previously shown that IM inhibits Tat-mediated elongation of HIV transcripts, and virus replication in primary lymphocytes and macrophages (IM EC50 values of 1 and 0.5 μM, respectively). We have also shown that IM suppresses HIV viremia and preserves CD4/CD8 ratios in NSG mice transplanted with human PBMCs (PBMC-NSG mice) [33]. However, these studies could only evaluate the antiviral activity of IM in the short-term (18 days) because of inherent limitations of the PBMC-NSG mouse model, namely, animal deterioration due to graft-versus-host disease (GVHD). In addition, HIV replication in PBMC-NSG mice resembles acute, rather than chronic, infection in humans because depleted lymphocytes are not replenished and HIV viremia cannot be sustained [34, 35].
The potential use of CDK9 inhibitors, such as IM, in HIV patients will likely involve treatment during chronic infection and for prolonged periods of time. In the present study, we report IM toxicity and pharmacokinetics for the first time. We also report the antiviral activity of IM during chronic HIV infection using NSG mice transplanted with human CD34+ cells (HSC-NSG mice), a model that allows continuous production of lymphocytes and supports HIV replication for extended periods of time as in humans [35–40]. Together, the data demonstrate that IM has favorable pharmacokinetics, and that IM can safely and durably reduce viremia in humanized mice with chronic HIV infection, suggesting it could help control HIV in patients.
Materials and methods
Ethics statement
All research with human samples and mice was performed in compliance with the institutional guidelines and the US Department of Health and Human Services Guide for the Care and Use of Laboratory Animals. The Committee on Animal Care at the University of Maryland School of Medicine reviewed and approved the described studies. Mice were monitored daily for morbidity and mortality, and euthanized immediately if any of the alternative endpoints was met. The alternative endpoints included a weight loss exceeding 20% as compared to day 0, signs of sluggishness, diarrhea (debilitating or prolonged for 2–3 days), postural hunching, fur ruffling, alopecia (covering at least 25% of body surface area), loss of appetite, GVHD, and ocular trauma. The euthanization method for mice of age 7 days or older was CO2 asphyxiation followed by cervival dislocation. For mice younger than 7 days, the euthanization method was decapitation with sharp scissors.
Toxicity studies
IM (Cayman Chemicals, Ann Arbor, MI) was dissolved in 10% Cremophor EL (Sigma, St. Louis, MO). Adult, female BALB/c mice were treated with IM (2.5, 5, and 20 mg/kg; n = 5 per dose) or its vehicle (10% Cremophor EL; n = 5) daily, via intraperitoneal (i.p.) injections, for 14 days. We used mice from a single sex to reduce potential variability of the data, although gender is not expected to have an effect on the toxicity of IM. On day 14, animals were anesthesized with ketamine-xylazine (100-150mg/kg Ketamine + 10-16mg/kg Xylazine) and, after confirming (via toe pinch) that a deep surgical plane of anesthesia had been reached, blood was collected by cardiac puncture. Blood samples were submitted for measurements of blood chemistry profiles and of blood counts.
Generation and infection of humanized mice
NSG mice were humanized at the age of 2–3 days, following whole body irradiation (10cGy) and hepatic injection of 1.2x105 human cord blood-derived CD34+ cells (Lonza, Walkersville, MD). At week 12, mice were checked for human cell reconstitution by double staining with FITC-conjugated antihuman CD45 antibody (BD Pharmingen) and APC-conjugated antimouse CD45 antibody (BD Pharmingen). Mice were considered successfully transplanted if they had ≥ 5% of human CD45+ cells in peripheral blood. Successfully transplanted mice were infected, via i.p. injection, with 15,000 TCID50 units of the CCR5-tropic HIV reference strain BaL.
Pharmacokinetic data analysis
Fasting, female NSG mice (n = 16) were injected with 40 mg/kg IM via i.p. Blood samples were obtained pre-dose (30 minutes before compound injection) and at 5, 15, 30, 60, 120, 180, 240 and 300 minutes after injection using a sparse sampling design (n = 2 samples per mouse, n = 4 samples per time point). Separated plasma was further extracted and processed for analysis, and IM concentrations determined using HPLC analysis. In brief, sample processing involved extraction of plasma (30 μL) with 400 μL acetonitrile and 2 μg/mL internal standard (estrone sulfate). The sample was briefly vortexed and centrifuged (12 minutes, 6°C), with transfer of 400 μL of supernatant to a clean test tube. The sample was evaporated to dryness under nitrogen, reconstituted in 50 μL of methanol:water (75:25), and 20 μL was injected onto the column. The concentration of primary analyte (IM) and internal standard (IS) d4-estrone were determined using a Shimadzu Nexera X2 liquid chromatography system coupled with a SPD-M30A UV-VIS diode array detector. The liquid chromatography separation was performed on a Prodigy ODS-3V C18 column, 250 × 4.6 mm, 5 μm. The mobile phase consisted of 35% water and 65% Methanol (Optima LC-MS grade) delivered at a flow rate of 0.85 mL/min. Retention times for IM and IS were 13 and 15 minutes, respectively, with detection at 280 nm. The IM peak identity was confirmed using the complete 240–600 nm absorbance spectra. The standard concentration curve was linear over the range of 0.025 μg/mL– 4.0 μg/mL using regression plots of IM to internal standard peak area ratios versus drug concentrations derived with 1/x2 weighting. The bias of the analytical method did not exceed 20% (judged by percent deviation from nominal value) for at least two of three concentrations from quality control samples, and the intra-assay precision error was <15% (expressed as coefficient of variation). Non-compartmental pharmacokinetic parameters were determined from pooled average data at each time point using Phoenix WinNonlin v6.4 (Certara, St. Louis, MO).
Quantification of HIV RNA levels and CD4/CD8 ratios in humanized mice
Plasma HIV RNA levels were quantified by an in-house real-time RT PCR using HIV Gag primers SK38/SK39 and SYBR green dyes, as in our previous studies [33, 41]. The assay has a sensitivity of 150 copies HIV RNA/40μL plasma. Percentages of human CD4+ and CD8+ T cells were determined by flow cytometry analysis using fluorochrome labeled antibodies against human CD4 (clone SK3), CD8 (SK1), CD3 (clone SK7), and CD45 (clone 2D1) (BD Biosciences). Data were acquired in a BD FACSCalibur flow cytometer and analyzed using FLowJo software (v. 9.7.7). CD4/CD8 ratios were calculated and plotted using GraphPad Prism 5.0 software.
Drug susceptibility assays
The ARTs tenofovir, raltegravir and indinavir were obtained from the NIH AIDS Research and Reference Reagent Program (Gaithersburg, MD). Drug susceptibility assays were performed in PBMCs as previously [42, 43]. Briefly, donor PBMCs were activated by culture with phytohemagglutinin (PHA) for 3 days. Activated PBMCs were infected with HIV (M.O.I of 0.001) for 2 hours in the absence of IM or ARTs, washed to remove non-adsorbed virus, and plated in culture medium containing IL-2 and various dilutions of IM and ARTs alone and in combination. On day 3, fresh medium with fresh drug was added to the cultures. On day 7, cultures were evaluated for HIV production by measuring HIV p24 levels in the culture supernatants by ELISA (PerkinElmer Life Sciences, Inc., Boston, Massachusetts). Data were normalized to p24 levels in drug untreated controls (100%) and EC50 values determined by fitting the data to sigmoidal dose-response (variable slope) curves using GraphPad Prism 5.0 software.
Results
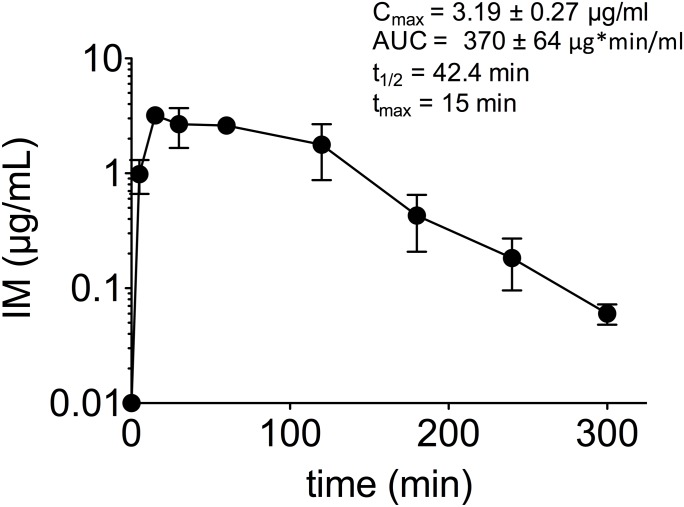
Pharmacokinetics of IM
We evaluated the pharmacokinetics of IM in NSG mice following a single i.p. injection of 40 mg/kg, a dose that inhibited plasma HIV RNA levels by 2 log 10 units in our previous study [33]. Data (S1 Table) were plotted on concentration-time curves and pharmacokinetic parameter values determined (Fig 1). The maximum concentration of IM in plasma (Cmax) was 3.19 ± 0.27 μg/mL. The time to Cmax (Tmax) was 15 min; the AUC was 370 ± 64 μg*min/mL; and the elimination t1/2 was 42.4 min. These data are consistent with IM antiviral activity because the Cmax values, which correspond to 11.5 ± 0.97 μM, are above the drug EC50 values for inhibition of HIV in vitro (EC50 values of 1 μM in lymphocytes and 0.5 μM in macrophages, [30]). Thus, IM concentrations above HIV EC50 values are rapidly achieved and maintained for > 3 h following i.p. injection of 40 mg/kg IM.
Fig 1. Pharmacokinetics of IM in mice.
NSG mice (n = 16) were i.p. injected with 40 mg/kg IM. Blood samples were obtained pre-dose and at 5, 15, 30, 60, 120, 180, 240 and 300 minutes after injection using a sparse sampling design (n = 2 samples per mouse, n = 4 samples per time point). Separated plasma was further extracted and processed for analysis, and IM concentrations were determined using HPLC analysis.
Toxicity of IM
There is currently limited information on IM toxicity [44–46]. In our previous studies in NSG mice, daily IM treatment at doses ranging between 2.5 and 40 mg/kg reduced plasma HIV RNA in a dose dependent manner and increased CD4/CD8 ratios, in the absence of general toxicity [33]. To better evaluate the toxicity of IM we conducted toxicity studies following standard protocols [47]. We used BALB/c mice because, unlike NSG mice, are fully immunocompetent and thus more suitable for assessing hematological toxicities. BALB/c mice were treated with IM (2.5, 5 and 20 mg/kg; n = 5 per dose) or its vehicle (n = 5) daily, via i.p. injections, for 14 days. The highest IM dose evaluated was 20 mg/kg because previous results suggested that the 40 mg/kg dose could interfere with lymphocyte proliferation [33]. Mice were monitored daily for morbidity and mortality. One mouse in the vehicle-treatment control group died in the first week of the experiment, but death did not appear to be related to treatment. The other 19 mice remained healthy and had no evidence of morbidity. Blood tests performed at the end of the study showed values within normal ranges for blood counts and for all chemistry profiles except for creatinine, which were lower in all animals (both IM and vehicle treated) (Table 1). Creatinine levels below reference ranges may be due to sample hemolysis [48, 49]. There were no statistical differences in blood counts or chemistry levels between any of the IM doses and vehicle controls. Thus, these data show that daily IM doses of up to 20 mg/kg do not cause: i) anemia, neutropenia, lymphopenia or thrombocytopenia suggestive of hematologic toxicity; ii) increases on blood urea nitrogen or creatinine suggestive of renal toxicity; or iii) increases on alanine aminotransferase, aspartate aminotransferase, alkaline phosphatase, or bilirubin suggestive of liver toxicity. Together, these data suggest that IM doses of up to 20 mg/kg are not associated with hematologic, renal or liver toxicity.
Table 1. Toxicity of IMa.
| Test | Vehicle (n = 4) |
IM (2.5 mg/kg) (n = 5) |
IM (5 mg/kg) (n = 5) |
IM (20 mg/kg) (n = 5) |
Reference values |
|---|---|---|---|---|---|
| Hematology | |||||
| WBC (109/L) | 8.9 ± 1.3 (6–12) | 6.5 ± 0.6 (5.4–9) | 6.8 ± 0.6 (4.9–8.5) | 7.1 ± 0.6 (5.5–8.7) | 5.7–14.8 |
| ANC (109/L) | 0.8 ± 0.2 (0.4–1.3) | 1.0 ± 0.1 (0.8–1.5) | 1.1 ± 0.1 (0.8–1.4) | 1.1 ± 0.1 (0.7–1.4) | 0.7–3 |
| ALC (109/L) | 7.7 ± 1.4 (5–12) | 5.2 ± 0.5 (4.1–7.1) | 5.3 ± 0.5 (3.6–6.8) | 5.7 ± 0.5 (4.4–7.2) | 3.6–11.5 |
| RBC (1012/L) | 10 ± 0.2 (9.7–10) | 9.8 ± 0.1 (9.3–10) | 9.6 ± 0.1 (9.3–9.8) | 9.4 ± 0.2 (8.7–9.8) | 8.2–11.7 |
| Renal Function or metabolism | |||||
| BUN (mg/dL) | 23 ± 2.9 (17–31) | 21 ± 1.1 (17–24) | 20 ± 0.7 (18–21) | 17 ± 0.9 (16–21) | 7–31 |
| Creatinine (mg/dL) | 0.07 ± 0.02 (0–0.1) | 0.16 ± 0.02 (0.1–0.2) | 0.14 ± 0.04 (0–0.2) | 0.16 ± 0.02 (0.1–0.2) | 0.2–0.5 |
| Albumin (g/dL) | 2.9 ± 0.07 (2.7–3) | 3.0 ± 0.05 (2.8–3.1) | 2.8 ± 0.02 (2.8–2.9) | 3.0 ± 0.05 (2.8–3.1) | 3.0–5.3 |
| Total protein (g/dL) | 4.8 ± 0.1 (4.5–5) | 4.8 ± 0.05 (4.7–5) | 4.8 ± 0.02 (4.7–4.8) | 4.8 ± 0.1 (4.6–5.1) | 4.9–7.3 |
| Calcium (mg/dL) | 8.9 ± 0.6 (7.1–9.6) | 7.7 ± 1.8 (0.4–10) | 9.5 ± 0.2 (9.1–10) | 9.7 ± 0.2 (9.3–10) | 8.4–12.7 |
| Phosphate (mg/dL) | 9.8 ± 0.8 (7.7–11) | 10 ± 0.6 (9.1–12) | 9.1 ± 0.7 (7.1–11) | 9.1 ± 1.1 (6.3–12) | 7.8–13.5 |
| Liver Function | |||||
| ALT (IU/L) | 64 ± 16.6 (34–99) | 77 ± 22 (44–161) | 131 ± 41 (13–250) | 43 ± 8 (23–70) | 40–170 |
| AST (IU/L) | 327 ± 135 (103–712) | 423 ± 84 (283–731) | 680±219(216–1451) | 324 ± 58 (192–515) | 67–381 |
| ALK (IU/L) | 154 ± 12 (124–182) | 152 ± 35 (13–205) | 170 ± 15 (137–220) | 177 ± 9 (150–205) | 108–367 |
| Total bilirubin (mg/dL) | 0.23 ± 0.02 (0.2–0.3) | 0.16 ± 0.02 (0.1–0.2) | 0.16 ± 0.04(0.1–0.3) | 0.24 ± 0.02 (0.2–0.3) | 0.2–0.7 |
a Data are means ± SEM, and range (parenthesis values). BALB/c mice received daily intraperitoneal (ip) injections of vehicle or the indicated doses of IM for 14 days. On day 15, whole blood and serum samples were collected and submitted for hematology and chemistries, respectively.
Abbreviations: WBC, white blood count; ANC, absolute neutrophil count; ALC, absolute lymphocyte count; RBC, red blood count; BUN, blood urea nitrogen; ALT, alanine aminotransferase; AST, aspartate aminotransferase; ALK, alkaline phosphatase.
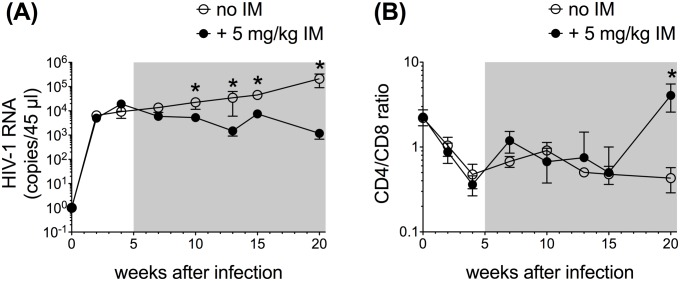
Antiviral activity of IM during chronic HIV infection
We next evaluated the antiviral activity of IM in HSC-NSG mice chronically infected with HIV. For this, 12-week old HSC-NSG mice were infected with HIV BaL. Five weeks after infection, animals initiated daily i.p. treatment with IM (5 and 20 mg/kg/day) or vehicle control for 15 weeks. Each experimental and control group had 5 mice. Viral replication was monitored by measuring HIV RNA in plasma by RT-PCR. Blood CD4/CD8 ratios were measured by Flow Cytometry. Mice treated with 5 mg/kg dose had modest, but significant, declines in plasma HIV RNA during the 15-week treatment period (Fig 2a). By the end of the study, plasma HIV RNA levels were 2.1 log10 units lower in mice treated with 5 mg/kg IM compared to controls. The CD4/CD8 ratios increased to similar levels in IM (5 mg/kg) and control groups for most of the study duration. By the end of the study, however, CD4/CD8 ratios were significantly higher in mice treated with 5 mg/kg IM (Fig 2b). Mice treated with 20 mg/kg IM had progressive losses in human T cells in blood and were euthanized after 5 weeks of treatment. The limited available data from the 20 mg/kg IM dose showed no consistent inhibition of plasma HIV RNA or increases in CD4/CD8 ratios (S1 Fig). Together, these data demonstrate that 5 mg/kg IM reduces HIV viremia and increases CD4/CD8 ratios during chronic HIV infection of humanized mice.
Fig 2. IM reduces HIV viremia in HSC-NSG chronically infected with HIV.
Twelve-week old HSC-NSG mice were infected with HIV BaL. Five weeks after infection, treatment was initiated at IM doses of 0 (vehicle alone) and 5 mg/kg/day. Each group had 5 mice. Treatment was continued for 15 weeks. Blood samples collected at the indicated time points were evaluated for plasma HIV RNA levels by quantitative RT-PCR (A), and for CD4/CD8 ratios by Flow Cytometry Analysis (B). At each time point, data were tested for statistical significant differences by Mann-Whitney U tests (GraphPad Prism Software, La Jolla, CA); P < 0.05 was considered significant. Shaded boxes indicate duration of treatment.
Antiviral interactions of IM and antiretrovirals
A potential use of CDK9 inhibitor for the treatment of HIV will probably be in combination with ARTs from other classes. We thus evaluated the antiviral interaction between IM and ARTs from the NRTI, integrase and protease inhibitor classes in PBMCs infectivity assays in vitro. We used the virus strain HIV-1 NL4-3 to ensure a robust viral replication in the assays. Although HIV-1 NL4-3 differs from HIV-1 BaL in usage of coreceptor for cell entry, it is expected to have similar sensitivity to the tested ARTs. At 1 μM IM the EC50 values of tenofovir, raltegravir and indinavir were decreased by 3-, 3.3- and 2.2-fold, respectively (Table 2 and S2 Table). These enhancements of ART potencies by IM are consistent with targeting of different steps of the HIV cycle by IM and the tested ARTs.
Table 2. IM enhances inhibition of HIVNL4-3 by tenofovir (TDF), raltegravir (RAL) and indinavir (IND) in PBMCs1.
| Geometric mean ART EC50, (95% CI)2 | ||
|---|---|---|
| ART | No IM | + 1μM IM |
| TDF | 0.60 μM (0.28–1.28) | 0.19 μM (0.17–0.22) |
| RAL | 6.98 nM (4.93–9.9) | 2.12 nM (0.99–4.5) |
| IND | 7.74 nM (4.56–13.14) | 3.55 nM (1.25–10) |
1 PHA-activated donor PBMCs were infected with virus, in the absence of drug, for 3 h. Infected cells were cultured in IL-2 medium containing drugs.
2 HIV p24 values on day 7 after infection were normalized to p24 values in the absence of IM. EC50 values were determined by variable slope non-linear regression analysis using GraphPad Prism software.
Discussion
We propose to improve HIV treatment in patients by inhibiting a step in the virus life cycle that is not targeted with current ARTs, namely, transcription of the provirus. Previous in vitro work, including ours, has suggested CDK9 as a potential target for inhibition of HIV transcription [8, 9, 11, 12, 30, 31]. Two previous studies, including one from our group, targeted CDK9 in PBMC-NSG mice, but only for short duration (2–3 weeks) and in the setting of acute infection [33, 50], which is relevant for pre- and post-exposure prophylaxis of HIV. Because HIV therapy is life-long and because CDK9 is required for transcription of host genes, there is a need to test the validity of targeting CDK9 in vivo under conditions that resemble treatment of chronic HIV infection in humans.
In the present study, we have evaluated for the first time IM pharmacokinetics and toxicities, and IM control of chronic HIV infection (HSC-NSG mice) during 15-week treatment. We show that IM pharmacokinetics are consistent with IM antiviral activity, demonstrating that therapeutic concentrations of IM are rapidly achieved and maintained in plasma for > 3 h. We also show that daily IM doses of up to 20 mg/kg for 14 days have no hematologic, liver or renal toxicity in immunocompetent BALB/c mice. A 15-week IM treatment (5 mg/kg/day) of HIV chronic infection in HSC-NSG mice progressively decreased viral loads, achieving ~ 2 log10 unit inhibition by the end of the study. Decreased HIV viral loads were associated with recovery of CD4/CD8 ratios, but this effect was only evident at the latest time point. That CD4/CD8 ratios did not recover until late in the study, when viral suppression was highest, suggests that inhibition of HIV replication by a certain threshold might be necessary to achieve cell recovery in this animal model. A higher IM dose of 20 mg/kg/day in HSC-NSG mice was discontinued after 5 weeks of treatment because human lymphocytes declined in blood. This decline on human lymphocytes by 20 mg/kg/day IM was unexpected because the same dose was not immunosuppressive in BALB/c mice. It is possible that the irradiation step performed in NSG mice prior to injection of human HSC cells may increase the sensitivity of cell replenishment to IM. This is consistent with irradiation induced systemic toxicities in many cell types (including HSC cells) and interference with stromal cell function [51].
The present study evaluating IM in established HIV infection of HSC-NSG mice shows some apparent differences with our previous study evaluating IM in acute HIV infection of PBMC-NSG mice [33]. Whereas IM demonstrates similar magnitude of HIV inhibition (~ 2 log10 units) in both acute and chronic infection, the antiviral activity and CD4/CD8 ratio recovery were delayed in the current study of chronic infection compared to the previous study of acute infection [33]. However, a direct comparison of both studies is not possible because the former study used drug-resistant CXCR4-tropic viruses whereas the latter study used wild-type CCR5-tropic HIV. An appropriate comparison of IM activity during acute and chronic infection will require additional animal experiments using same virus strains.
Our study has several limitations. First, the PK studies were conducted at a single dose and over a short period (5 rather than 24 hours), precluding precise estimates on optimal dosing and frequency. Second, toxicity studies conducted in BALB/c mice, which were chosen because of their immunocompetent status, may not be fully relevant to humanized NSG mice and cannot evaluate toxicity on immune cells of human origen. Third, the antiviral activity of IM in mice was evaluated at doses of 5 and 20 mg/kg only. We did not evaluate higher doses (e.g., 40 mg/kg) because previous studies suggested inhibition of human PBMC proliferation in humanized mice [33]. The IM dose of 5 mg/kg IM inhibited HIV viral loads by ~ 2 log10 units, whereas the 20 mg/kg dose was discontinued because it inhibited cell proliferation. It is possible that IM doses in the range of 5–20 mg/kg may have even stronger antiviral effects without compromising cell proliferation. Fourth, although IM enhanced the anti-HIV activities of NRTI, integrase and protease inhibitors in tissue culture experiments, the potential clinical relevance of these observations will require assessment in in vivo studies. Despite these limitations, the data demonstrate that targeting CDK9 with IM, which interferes with HIV transcription [30–32], reduces HIV viremia during chronic HIV infection of humanized mice. The antiviral IM dose of 5 mg/kg in mice would translate into an equivalent human dose of 0.4 mg/kg after dividing by an interspecies scaling factor of 12.3 [52]. Targeting HIV transcription may complement the antiviral activity of available inhibitors of reverse transcriptase, integrase and protease if, as suggested by in vitro experiments, enhanced ART potency is also seen in future animal studies. IM, and other CDK9 inhibitors, may also potentiate inhibition of HIV transcription by Tat inhibitors [53]. Moreover, IM, unlike some ARTs [54], has favorable penetration in brain [44, 55], suggesting it could help control HIV in long-lived brain macrophages and reduce HIV-associated CNS complications [56, 57]. Addition of IM, or other CDK9 inhibitors, to existing ART regimens may also help control replication of emerging viral variants resistant to ARTs (21, 22). Finally, targeting of HIV transcription may also prevent reactivation of HIV in resting CD4+ T cells, helping to achieve a “functional” cure [58].
Supporting information
Twelve-week old HSC-NSG mice were infected with HIV BaL. Five weeks after infection, treatment was initiated at IM doses of 0 (vehicle alone) and 20 mg/kg/day. Each group had 5 mice. Treatment was discontinued after 5 weeks of IM treatment. Blood samples collected at the indicated time points were evaluated for plasma HIV RNA levels by quantitative RT-PCR (A), and for CD4/CD8 ratios by Flow Cytometry Analysis (B). Shaded boxes indicate duration of treatment.
(TIFF)
NSG mice were given a single i.p. injection of 40 mg/kg. Blood samples collected at the indicated time points were processed and subjected to HPLC analysis as described in the Methods section.
(DOCX)
PHA-activated donor PBMCs were infected with NL4-3 in the absence of drugs. Infected cells were cultured in IL-2 medium containing various dilutions of TDF, RAL and IND in the absence and presence of IM. Virus production was measured by p24 ELISA on day 7 after infection.
(DOCX)
Acknowledgments
We thank Roberto Speck and Audigé Annette (University Hospital of Zurich, University of Zurich, Zurich, Switzerland) for sharing protocols on humanization of mice, and Dr. Sean McCormick (FSU-Shimadzu Core Laboratory) for assistance in developing the PK method for detection of IM.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by NIH-1R21AI114288. The role of the funding agent was funding of salaries and experimental approaches; no direct role in this research.
References
- 1.Kao SY, Calman AF, Luciw PA, Peterlin BM. Anti-termination of transcription within the long terminal repeat of HIV-1 by tat gene product. Nature. 1987;330(6147):489–93. Epub 1987/12/03. doi: 10.1038/330489a0 . [DOI] [PubMed] [Google Scholar]
- 2.Dingwall C, Ernberg I, Gait MJ, Green SM, Heaphy S, Karn J, et al. HIV-1 tat protein stimulates transcription by binding to a U-rich bulge in the stem of the TAR RNA structure. Embo J. 1990;9(12):4145–53. Epub 1990/12/01. ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marciniak RA, Sharp PA. HIV-1 Tat protein promotes formation of more-processive elongation complexes. Embo J. 1991;10(13):4189–96. Epub 1991/12/01. ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang X, Gold MO, Tang DN, Lewis DE, Aguilar-Cordova E, Rice AP, et al. TAK, an HIV Tat-associated kinase, is a member of the cyclin-dependent family of protein kinases and is induced by activation of peripheral blood lymphocytes and differentiation of promonocytic cell lines. Proc Natl Acad Sci U S A. 1997;94(23):12331–6. Epub 1997/11/14. ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhu Y, Pe'ery T, Peng J, Ramanathan Y, Marshall N, Marshall T, et al. Transcription elongation factor P-TEFb is required for HIV-1 tat transactivation in vitro. Genes Dev. 1997;11(20):2622–32. Epub 1997/10/23. ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wei P, Garber ME, Fang SM, Fischer WH, Jones KA. A novel CDK9-associated C-type cyclin interacts directly with HIV-1 Tat and mediates its high-affinity, loop-specific binding to TAR RNA. Cell. 1998;92(4):451–62. Epub 1998/03/10. . [DOI] [PubMed] [Google Scholar]
- 7.Garriga J, Bhattacharya S, Calbo J, Marshall RM, Truongcao M, Haines DS, et al. CDK9 is constitutively expressed throughout the cell cycle, and its steady-state expression is independent of SKP2. Mol Cell Biol. 2003;23(15):5165–73. doi: 10.1128/MCB.23.15.5165-5173.2003 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chao SH, Fujinaga K, Marion JE, Taube R, Sausville EA, Senderowicz AM, et al. Flavopiridol inhibits P-TEFb and blocks HIV-1 replication. J Biol Chem. 2000;275(37):28345–8. Epub 2000/07/25. doi: 10.1074/jbc.C000446200 . [DOI] [PubMed] [Google Scholar]
- 9.Flores O, Lee G, Kessler J, Miller M, Schlief W, Tomassini J, et al. Host-cell positive transcription elongation factor b kinase activity is essential and limiting for HIV type 1 replication. Proc Natl Acad Sci U S A. 1999;96(13):7208–13. ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Okamoto M, Hidaka A, Toyama M, Hosoya T, Yamamoto M, Hagiwara M, et al. Selective inhibition of HIV-1 replication by the CDK9 inhibitor FIT-039. Antiviral research. 2015;123:1–4. doi: 10.1016/j.antiviral.2015.08.012 . [DOI] [PubMed] [Google Scholar]
- 11.Chiu YL, Cao H, Jacque JM, Stevenson M, Rana TM. Inhibition of human immunodeficiency virus type 1 replication by RNA interference directed against human transcription elongation factor P-TEFb (CDK9/CyclinT1). J Virol. 2004;78(5):2517–29. doi: 10.1128/JVI.78.5.2517-2529.2004 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Salerno D, Hasham MG, Marshall R, Garriga J, Tsygankov AY, Grana X. Direct inhibition of CDK9 blocks HIV-1 replication without preventing T-cell activation in primary human peripheral blood lymphocytes. Gene. 2007;405(1–2):65–78. Epub 2007/10/24. doi: 10.1016/j.gene.2007.09.010 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen R, Keating MJ, Gandhi V, Plunkett W. Transcription inhibition by flavopiridol: mechanism of chronic lymphocytic leukemia cell death. Blood. 2005;106(7):2513–9. doi: 10.1182/blood-2005-04-1678 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krystof V, Baumli S, Furst R. Perspective of cyclin-dependent kinase 9 (CDK9) as a drug target. Current pharmaceutical design. 2012;18(20):2883–90. doi: 10.2174/138161212800672750 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Byrd JC, Lin TS, Dalton JT, Wu D, Phelps MA, Fischer B, et al. Flavopiridol administered using a pharmacologically derived schedule is associated with marked clinical efficacy in refractory, genetically high-risk chronic lymphocytic leukemia. Blood. 2007;109(2):399–404. doi: 10.1182/blood-2006-05-020735 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Christian BA, Grever MR, Byrd JC, Lin TS. Flavopiridol in chronic lymphocytic leukemia: a concise review. Clinical lymphoma & myeloma. 2009;9 Suppl 3:S179–85. doi: 10.3816/CLM.2009.s.009 . [DOI] [PubMed] [Google Scholar]
- 17.McClue SJ, Blake D, Clarke R, Cowan A, Cummings L, Fischer PM, et al. In vitro and in vivo antitumor properties of the cyclin dependent kinase inhibitor CYC202 (R-roscovitine). Int J Cancer. 2002;102(5):463–8. doi: 10.1002/ijc.10738 . [DOI] [PubMed] [Google Scholar]
- 18.Gojo I, Sadowska M, Walker A, Feldman EJ, Iyer SP, Baer MR, et al. Clinical and laboratory studies of the novel cyclin-dependent kinase inhibitor dinaciclib (SCH 727965) in acute leukemias. Cancer chemotherapy and pharmacology. 2013;72(4):897–908. Epub 2013/08/21. doi: 10.1007/s00280-013-2249-z ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mita MM, Joy AA, Mita A, Sankhala K, Jou YM, Zhang D, et al. Randomized phase II trial of the cyclin-dependent kinase inhibitor dinaciclib (MK-7965) versus capecitabine in patients with advanced breast cancer. Clinical breast cancer. 2014;14(3):169–76. Epub 2014/01/08. doi: 10.1016/j.clbc.2013.10.016 . [DOI] [PubMed] [Google Scholar]
- 20.Stephenson JJ, Nemunaitis J, Joy AA, Martin JC, Jou YM, Zhang D, et al. Randomized phase 2 study of the cyclin-dependent kinase inhibitor dinaciclib (MK-7965) versus erlotinib in patients with non-small cell lung cancer. Lung cancer. 2014;83(2):219–23. Epub 2014/01/07. doi: 10.1016/j.lungcan.2013.11.020 . [DOI] [PubMed] [Google Scholar]
- 21.Bible KC, Peethambaram PP, Oberg AL, Maples W, Groteluschen DL, Boente M, et al. A phase 2 trial of flavopiridol (Alvocidib) and cisplatin in platin-resistant ovarian and primary peritoneal carcinoma: MC0261. Gynecologic oncology. 2012;127(1):55–62. Epub 2012/06/06. doi: 10.1016/j.ygyno.2012.05.030 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Karp JE, Garrett-Mayer E, Estey EH, Rudek MA, Smith BD, Greer JM, et al. Randomized phase II study of two schedules of flavopiridol given as timed sequential therapy with cytosine arabinoside and mitoxantrone for adults with newly diagnosed, poor-risk acute myelogenous leukemia. Haematologica. 2012;97(11):1736–42. Epub 2012/06/27. doi: 10.3324/haematol.2012.062539 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lanasa MC, Andritsos L, Brown JR, Gabrilove J, Caligaris-Cappio F, Ghia P, et al. Final results of EFC6663: a multicenter, international, phase 2 study of alvocidib for patients with fludarabine-refractory chronic lymphocytic leukemia. Leukemia research. 2015;39(5):495–500. Epub 2015/03/26. doi: 10.1016/j.leukres.2015.02.001 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rahaman MH, Kumarasiri M, Mekonnen LB, Yu M, Diab S, Albrecht H, et al. Targeting CDK9: a promising therapeutic opportunity in prostate cancer. Endocrine-related cancer. 2016;23(12):T211–T26. Epub 2016/09/02. doi: 10.1530/ERC-16-0299 . [DOI] [PubMed] [Google Scholar]
- 25.Maddocks K, Wei L, Rozewski D, Jiang Y, Zhao Y, Adusumilli M, et al. Reduced occurrence of tumor flare with flavopiridol followed by combined flavopiridol and lenalidomide in patients with relapsed chronic lymphocytic leukemia (CLL). American journal of hematology. 2015;90(4):327–33. Epub 2015/02/03. doi: 10.1002/ajh.23946 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hofmeister CC, Poi M, Bowers MA, Zhao W, Phelps MA, Benson DM, et al. A phase I trial of flavopiridol in relapsed multiple myeloma. Cancer chemotherapy and pharmacology. 2014;73(2):249–57. Epub 2013/11/19. doi: 10.1007/s00280-013-2347-y ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jones JA, Rupert AS, Poi M, Phelps MA, Andritsos L, Baiocchi R, et al. Flavopiridol can be safely administered using a pharmacologically derived schedule and demonstrates activity in relapsed and refractory non-Hodgkin's lymphoma. American journal of hematology. 2014;89(1):19–24. Epub 2013/08/21. doi: 10.1002/ajh.23568 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Xiao Z, Hao Y, Liu B, Qian L. Indirubin and meisoindigo in the treatment of chronic myelogenous leukemia in China. Leuk Lymphoma. 2002;43(9):1763–8. Epub 2003/04/11. doi: 10.1080/1042819021000006295 . [DOI] [PubMed] [Google Scholar]
- 29.Hoessel R, Leclerc S, Endicott JA, Nobel ME, Lawrie A, Tunnah P, et al. Indirubin, the active constituent of a Chinese antileukaemia medicine, inhibits cyclin-dependent kinases. Nat Cell Biol. 1999;1(1):60–7. Epub 1999/11/13. doi: 10.1038/9035 . [DOI] [PubMed] [Google Scholar]
- 30.Heredia A, Davis C, Bamba D, Le N, Gwarzo MY, Sadowska M, et al. Indirubin-3'-monoxime, a derivative of a Chinese antileukemia medicine, inhibits P-TEFb function and HIV-1 replication. Aids. 2005;19(18):2087–95. . [DOI] [PubMed] [Google Scholar]
- 31.Toossi Z, Wu M, Hirsch CS, Mayanja-Kizza H, Baseke J, Aung H, et al. Activation of P-TEFb at sites of dual HIV/TB infection, and inhibition of MTB-induced HIV transcriptional activation by the inhibitor of CDK9, Indirubin-3'-monoxime. AIDS research and human retroviruses. 2012;28(2):182–7. Epub 2011/04/02. doi: 10.1089/AID.2010.0211 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guendel I, Agbottah ET, Kehn-Hall K, Kashanchi F. Inhibition of human immunodeficiency virus type-1 by cdk inhibitors. AIDS research and therapy. 2010;7(1):7 doi: 10.1186/1742-6405-7-7 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Heredia A, Natesan S, Le NM, Medina-Moreno S, Zapata JC, Reitz M, et al. Indirubin 3'-monoxime, from a Chinese traditional herbal formula, suppresses viremia in humanized mice infected with multidrug-resistant HIV. AIDS Res Hum Retroviruses. 2014;30(5):403–6. doi: 10.1089/AID.2013.0249 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brehm MA, Jouvet N, Greiner DL, Shultz LD. Humanized mice for the study of infectious diseases. Curr Opin Immunol. 2013;25(4):428–35. doi: 10.1016/j.coi.2013.05.012 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kumar P, Ban HS, Kim SS, Wu H, Pearson T, Greiner DL, et al. T cell-specific siRNA delivery suppresses HIV-1 infection in humanized mice. Cell. 2008;134(4):577–86. Epub 2008/08/12. doi: 10.1016/j.cell.2008.06.034 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brehm MA, Wiles MV, Greiner DL, Shultz LD. Generation of improved humanized mouse models for human infectious diseases. Journal of immunological methods. 2014;410:3–17. Epub 2014/03/13. doi: 10.1016/j.jim.2014.02.011 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Akkina R, Allam A, Balazs AB, Blankson JN, Burnett JC, Casares S, et al. Improvements and Limitations of Humanized Mouse Models for HIV Research: NIH/NIAID "Meet the Experts" 2015 Workshop Summary. AIDS Res Hum Retroviruses. 2016;32(2):109–19. doi: 10.1089/AID.2015.0258 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Choudhary SK, Rezk NL, Ince WL, Cheema M, Zhang L, Su L, et al. Suppression of human immunodeficiency virus type 1 (HIV-1) viremia with reverse transcriptase and integrase inhibitors, CD4+ T-cell recovery, and viral rebound upon interruption of therapy in a new model for HIV treatment in the humanized Rag2-/-{gamma}c-/- mouse. J Virol. 2009;83(16):8254–8. Epub 2009/06/06. doi: 10.1128/JVI.00580-09 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nischang M, Sutmuller R, Gers-Huber G, Audige A, Li D, Rochat MA, et al. Humanized mice recapitulate key features of HIV-1 infection: a novel concept using long-acting anti-retroviral drugs for treating HIV-1. PloS one. 2012;7(6):e38853 doi: 10.1371/journal.pone.0038853 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Halper-Stromberg A, Lu CL, Klein F, Horwitz JA, Bournazos S, Nogueira L, et al. Broadly neutralizing antibodies and viral inducers decrease rebound from HIV-1 latent reservoirs in humanized mice. Cell. 2014;158(5):989–99. doi: 10.1016/j.cell.2014.07.043 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Heredia A, Le N, Gartenhaus RB, Sausville E, Medina-Moreno S, Zapata JC, et al. Targeting of mTOR catalytic site inhibits multiple steps of the HIV-1 lifecycle and suppresses HIV-1 viremia in humanized mice. Proc Natl Acad Sci U S A. 2015;112(30):9412–7. doi: 10.1073/pnas.1511144112 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Heredia A, Davis C, Amin MN, Le NM, Wainberg MA, Oliveira M, et al. Targeting host nucleotide biosynthesis with resveratrol inhibits emtricitabine-resistant HIV-1. Aids. 2014;28(3):317–23. doi: 10.1097/QAD.0000000000000168 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Heredia A, Davis CE, Reitz MS, Le NM, Wainberg MA, Foulke JS, et al. Targeting of the Purine Biosynthesis Host Cell Pathway Enhances the Activity of Tenofovir Against Sensitive and Drug-Resistant HIV-1. J Infect Dis. 2013;208(12):2085–94. doi: 10.1093/infdis/jit395 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Selenica ML, Jensen HS, Larsen AK, Pedersen ML, Helboe L, Leist M, et al. Efficacy of small-molecule glycogen synthase kinase-3 inhibitors in the postnatal rat model of tau hyperphosphorylation. Br J Pharmacol. 2007;152(6):959–79. Epub 2007/10/02. doi: 10.1038/sj.bjp.0707471 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sugihara K, Okayama T, Kitamura S, Yamashita K, Yasuda M, Miyairi S, et al. Comparative study of aryl hydrocarbon receptor ligand activities of six chemicals in vitro and in vivo. Arch Toxicol. 2008;82(1):5–11. Epub 2007/09/28. doi: 10.1007/s00204-007-0232-3 . [DOI] [PubMed] [Google Scholar]
- 46.Ding Y, Qiao A, Fan GH. Indirubin-3'-monoxime rescues spatial memory deficits and attenuates beta-amyloid-associated neuropathology in a mouse model of Alzheimer's disease. Neurobiol Dis. 2010;39(2):156–68. Epub 2010/04/13. doi: 10.1016/j.nbd.2010.03.022 . [DOI] [PubMed] [Google Scholar]
- 47.Parasuraman S. Toxicological screening. Journal of pharmacology & pharmacotherapeutics. 2011;2(2):74–9. Epub 2011/07/21. doi: 10.4103/0976-500X.81895 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fernandez I, Pena A, Del Teso N, Perez V, Rodriguez-Cuesta J. Clinical biochemistry parameters in C57BL/6J mice after blood collection from the submandibular vein and retroorbital plexus. J Am Assoc Lab Anim Sci. 2010;49(2):202–6. ;. [PMC free article] [PubMed] [Google Scholar]
- 49.Matsuzawa T, Hayashi Y, Nomura M, Unno T, Igarashi T, Furuya T, et al. A survey of the values of clinical chemistry parameters obtained for a common rat blood sample in ninety-eight Japanese laboratories. J Toxicol Sci. 1997;22(1):25–44. . [DOI] [PubMed] [Google Scholar]
- 50.Van Duyne R, Guendel I, Jaworski E, Sampey G, Klase Z, Chen H, et al. Effect of mimetic CDK9 inhibitors on HIV-1-activated transcription. J Mol Biol. 2013;425(4):812–29. Epub 2012/12/19. doi: 10.1016/j.jmb.2012.12.005 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Stoddart CA, Galkina SA, Joshi P, Kosikova G, Moreno ME, Rivera JM, et al. Oral administration of the nucleoside EFdA (4'-ethynyl-2-fluoro-2'-deoxyadenosine) provides rapid suppression of HIV viremia in humanized mice and favorable pharmacokinetic properties in mice and the rhesus macaque. Antimicrob Agents Chemother. 2015;59(7):4190–8. doi: 10.1128/AAC.05036-14 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stoddart CA, Bales CA, Bare JC, Chkhenkeli G, Galkina SA, Kinkade AN, et al. Validation of the SCID-hu Thy/Liv mouse model with four classes of licensed antiretrovirals. PloS one. 2007;2(7):e655 doi: 10.1371/journal.pone.0000655 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mousseau G, Kessing CF, Fromentin R, Trautmann L, Chomont N, Valente ST. The Tat Inhibitor Didehydro-Cortistatin A Prevents HIV-1 Reactivation from Latency. MBio. 2015;6(4):e00465 doi: 10.1128/mBio.00465-15 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Varatharajan L, Thomas SA. The transport of anti-HIV drugs across blood-CNS interfaces: summary of current knowledge and recommendations for further research. Antiviral research. 2009;82(2):A99–109. doi: 10.1016/j.antiviral.2008.12.013 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhang SG, Wang XS, Zhang YD, Di Q, Shi JP, Qian M, et al. Indirubin-3'-monoxime suppresses amyloid-beta-induced apoptosis by inhibiting tau hyperphosphorylation. Neural Regen Res. 2016;11(6):988–93. doi: 10.4103/1673-5374.184500 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Vivithanaporn P, Heo G, Gamble J, Krentz HB, Hoke A, Gill MJ, et al. Neurologic disease burden in treated HIV/AIDS predicts survival: a population-based study. Neurology. 2010;75(13):1150–8. doi: 10.1212/WNL.0b013e3181f4d5bb ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Robertson KR, Smurzynski M, Parsons TD, Wu K, Bosch RJ, Wu J, et al. The prevalence and incidence of neurocognitive impairment in the HAART era. Aids. 2007;21(14):1915–21. doi: 10.1097/QAD.0b013e32828e4e27 . [DOI] [PubMed] [Google Scholar]
- 58.Mousseau G, Mediouni S, Valente ST. Targeting HIV Transcription: The Quest for a Functional Cure. Current topics in microbiology and immunology. 2015;389:121–45. doi: 10.1007/82_2015_435 ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Twelve-week old HSC-NSG mice were infected with HIV BaL. Five weeks after infection, treatment was initiated at IM doses of 0 (vehicle alone) and 20 mg/kg/day. Each group had 5 mice. Treatment was discontinued after 5 weeks of IM treatment. Blood samples collected at the indicated time points were evaluated for plasma HIV RNA levels by quantitative RT-PCR (A), and for CD4/CD8 ratios by Flow Cytometry Analysis (B). Shaded boxes indicate duration of treatment.
(TIFF)
NSG mice were given a single i.p. injection of 40 mg/kg. Blood samples collected at the indicated time points were processed and subjected to HPLC analysis as described in the Methods section.
(DOCX)
PHA-activated donor PBMCs were infected with NL4-3 in the absence of drugs. Infected cells were cultured in IL-2 medium containing various dilutions of TDF, RAL and IND in the absence and presence of IM. Virus production was measured by p24 ELISA on day 7 after infection.
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.