Abstract
Whereas most of studies investigating relationship between oral health and atherosclerosis have focused on periodontitis, very few of them were examined about occlusal status of natural teeth which possibly influence dietary habit. The primary aim of this cross-sectional study was to investigate the association between the occlusal support of posterior teeth and the prevalence of atherosclerosis in community-dwelling septuagenarians. Also, the second aim was to test the hypothesis that the intake of key nutrients for atherosclerosis prevention would have a mediating effect on the relationship between the occlusal status and atherosclerosis. The study population included 468 community-dwelling dentate persons aged 69–71 years recruited from the local residential registration in Japan. Participants were divided into three groups, according to the number of occlusal support zones (OSZ) in the posterior area: Complete (four OSZ), Moderate (three or two OSZ), and Collapsed (one or no OSZ). Dietary intakes were assessed using a brief-type self-administered diet history questionnaire. Atherosclerosis was defined as carotid intima-media thickness ≧1.10 mm by using carotid ultrasonography test. The logistic or linear regression model was used in multivariate analysis to assess relationship between occlusal status and atherosclerosis, and the mediating effect of key nutrients within the relationship. Multivariable analysis showed a significant association between occlusal status and atherosclerosis (odds ratio for Collapsed group to Complete group: 1.87; 95% CI: 1.45–2.41), independent of periodontal status (odds ratio: 2.01, 95%CI: 1.46–2.78). Fish and shellfish, vitamin B6 and n-3PUFAs were significantly related to both of occlusal status and atherosclerosis, and also was indicated a mediating effect on the association between occlusal status and atherosclerosis. This study implied that, within the limitation of the cross-sectional study design, the reduced posterior occlusion was related to the increased prevalence of atherosclerosis via the decline of key dietary intakes among Japanese community-dwelling dentate individuals.
Introduction
In older adults, oral health has a high impact on diet and nutrition, which can affect systemic health. In particular, a decline in masticatory function resulting from loss of natural occlusion in the posterior region is reported to make chewing difficult for older adults and to lead to avoidance of hard-to-chew foods such as vegetables, fruits, fish and shellfish [1–5]. On the other hand, there is increasing evidence that a higher intake of vegetables, fruits, fish and shellfish can reduce the risk of cardiovascular or cerebrovascular disease via favorable effects on disease contributors [6–12]. Thus, maintaining good occlusal support of natural teeth could possibly help prevent cardiovascular and cerebrovascular accidents, which are the most common causes of sudden death and disability in older adults worldwide.
Since the beginning of the 21st century, the relationship between atherosclerosis, which contributes to cardiovascular and cerebrovascular accidents, and periodontal disease has been the subject of growing research [13]. Recent literature reviews report a potential link between atherosclerosis and oral health through the inflammatory effects of periodontal disease [14,15].
Therefore, two pathways connecting oral health with atherosclerosis can be hypothesized: (a) the effect of bad dietary habits resulting from poor occlusal condition [1–12] and (b) the effect of inflammation associated with chronic periodontal infection on the circulatory system [13–15]. However, no previous studies have investigated the association between occlusal condition and atherosclerosis adjusting periodontal disease in same population.
The aim of this cross-sectional study was to investigate the relationship between the prevalence of atherosclerosis and both of occlusal and periodontal status in a community-dwelling septuagenarian. And secondly, it was also aimed to test a mediating effect of the intake of atheroprotective nutrients within the relation between the occlusal status and atherosclerosis. The null hypothesis of this study was that poor occlusal condition was not significantly associated with neither atherosclerosis nor atheroprotective nutrient intakes.
Materials and methods
Study population
This cross-sectional study was conducted as a baseline assessment for the prospective study of health and longevity called the SONIC (Septuagenarians, Octogenarians, Nonagenarians Investigation with Centenarians) Study. Participants were 495 community-dwelling septuagenarians aged 69–71 years who were recruited from the Basic Resident Registration of Itami (urban area) and Asago (rural area) in Hyogo Prefecture, Japan. Data collection was conducted in 2010 and 2011 at each local community hall.
For this study, 23 edentulous participants were excluded. In addition, four participants who did not attend the medical examination were excluded. Thus, 468 participants (Group A) were included in the multivariable assessment between occlusal status and atherosclerosis. Additionally, in analyzing of nutrient intakes, we excluded participants who reported either an extremely high energy intake (≥ 4000 kcal/d) or an extremely low energy intake (<600 kcal/d), who were receiving dietary counseling from a doctor or dietician at enrollment, or those with intentional dietary change during the preceding year. The final pool of participants for the analysis of nutrients numbered 371 (Group B).
The study protocol was approved by the Institutional Review Board of Osaka University Graduate Schools of Dentistry (approval number H22-E9) and Medicine (approval number 266). All participants gave written informed consent to participate.
Dental examination
Oral examinations, including periodontal and dental examinations, were performed by registered dental clinicians. Occlusal support condition was categorized into one of three groups, based on the number of occlusal support zones (OSZ) which consist of occlusal contacts of natural teeth or fixed prosthesis on both side of the premolar and molar regions, which is basically from the concept of Eichner’s Index [16]: Complete (four OSZ: Eichner A1, A2 and A3), Moderate (three or two OSZ: Eichner B1 and B2), and Collapsed (one or no OSZ: Eichner B3, B4, C1 and C2). Periodontal condition was assessed by measuring periodontal pocket depth (PPD). All remaining teeth of participants were measured. If the probing depths varied within a site, the deepest reading obtained at that site was recorded; only one reading was recorded per site measurement. Periodontal condition was categorized into one of three groups, according to the participant’s deepest PPD: Healthy (PPD 3 mm or less), Moderate (PPD 4 or 5 mm), and Severe (PPD 6 mm or more).
Evaluation of carotid atherosclerosis
Atherosclerosis was diagnosed with carotid ultrasonography. The left and right common carotid arteries were examined with a high-resolution duplex scanner (GE LOGIQ book XP; GE Healthcare, Tokyo, Japan), using a probe at a frequency of 7.5 MHz for the B-scan. Participants were examined in the supine position, with the head slightly turned away from the side being scanned. Following the same methodology as a previous study [17], the thickness of the carotid intima-media (IMT) and plaque were measured; the maximum was defined as the maximum IMT (max-IMT). In this study, atherosclerosis was defined as max-IMT ≥ 1.10, which is the value generally used for individuals in their seventies.
Other medical examinations and diagnostic criteria
Blood samples were collected after overnight fasting. Levels of total cholesterol, high-density lipoprotein cholesterol (HDL-C), triglycerides (TG), and fasting plasma glucose were determined with biochemical testing. Low-density lipoprotein cholesterol (LDL-C) was calculated with the Friedwald formula. Dyslipidemia was defined as LDL-C ≥ 140 mg/dL, TG ≥ 150 mg/dL, HDL-C < 40 mg/dL, and/or medications for dyslipidemia [18]. Diabetes mellitus was defined as fasting plasma glucose ≥ 126 mg/dL and/or hemoglobin A1c ≥ 6.5% and/or current medications for diabetes mellitus [19]. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured twice in a sitting position at the venue, using a calibrated standard mercury sphygmomanometer. Two measured BP levels were averaged. Hypertension was defined as SBP ≥ 140 mm Hg and/or DBP ≥ 90 mm Hg and/or current medications for hypertension [18,20].
Questionnaire assessment
Socioeconomic and other factors were assessed based on answers to a questionnaire. Residential region was categorized as urban (Itami, population 7875/km2) or rural (Asago, population 81/km2). Education level was categorized into one of three groups, according to the number of years of education: <10 years, 10 to 12 years, and >12 years. Financial status was scaled with self-reported subjective assessment as follows: dissatisfied, moderately satisfied, and satisfied. Research staff questioned participants on their history of smoking and alcohol intake; responses were classified as never, past, or current.
Nutrient intakes
Nutrient intakes during the preceding month were assessed using a brief-type self-administered diet history questionnaire (BDHQ) that measures consumption frequencies of selected food commonly consumed and calculates energy-adjusted dietary intakes. The methods used to calculate dietary intake and the validity of the BDHQ have been detailed in previous reports [21–23]. Values were indicated as a mean amount per 1000 kcal of energy to minimize the influence of dietary misreporting. Key nutrients for preventing atherosclerotic disease such as green and yellow vegetables, other vegetables, fruits, and fish and shellfish, and specifically dietary fiber, vitamin A, C, E, B6, B12, folic acid, n-3 polyunsaturated fatty acid (n-3PUFAs) were determined in this present study [24–29].
Statistical methods
In assessing the association between the prevalence of atherosclerosis and each variable in the group A (n = 468), the outcome assessed in this study was set as the prevalence of atherosclerosis, and two predictors were defined as occlusal status and periodontal status. The other potential confounders were region of residence, education level, financial status, and risk factors for atherosclerosis, including gender, smoking habits, drinking habits, obesity (body mass index [BMI] ≥ 25), hypertension, diabetes mellitus, dyslipidemia, and hyperuricemia. The chi-square test was used in bivariate analysis to assess the association between the prevalence of atherosclerosis and each variable. Multiple logistic regression analysis was performed to examine the association between the prevalence of atherosclerosis and occlusal support and periodontal condition, adjusted for gender, region of residence, smoking habits, drinking habits, education level, diabetes mellitus, hypertension, dyslipidemia, and hyperuricemia. P-values less than 0.05 were considered to be statistically significant.
Secondly, among group B (n = 371), to determine between the occlusal status and the difference of means of each key dietary intake, the one-way ANOVA test was used. For the post hoc test, Tukey’s HSD test was used. To examine the relationship between each key dietary intake and both of atherosclerosis and occlusal status, multivariable linear regression model was used, adjusted for periodontal condition, gender, region of residence, smoking habits, drinking habits, education level, diabetes mellitus, hypertension, dyslipidemia, and hyperuricemia. P-values less than 0.10 were considered to be statistically significant.
And finally, to test the mediating effect of dietary intakes within the relation between occlusal status and atherosclerosis, multivariable logistic regression analysis was also performed.
Multiple imputations were conducted for missing data in multivariate analysis. Data were analyzed with PASW Statistics 18 software (formerly SPSS; IBM Company, Tokyo, Japan) and R software, Version 3.1.1 (10 July 2014, R Core Team, http://www.r-project.org/).
Results
Overall of group A (n = 468), 217 participants (46%) were diagnosed as having carotid atherosclerosis. In terms of posterior occlusal support, 57% (n = 265) of participants had complete occlusion (four OSZ), 17% (n = 79) had moderate occlusion (three or two OSZ), and 26% (n = 117) had collapsed occlusion (one or no OSZ). Sixteen percent (n = 73) of all participants had healthy periodontal status, 40% (n = 185) had moderate periodontal disease, and 44% (n = 206) had severe periodontal disease. The statistical correlation between occlusal support and periodontal condition was very weak (Cramer’s V = .114, p = .017).
Bivariate analysis showed that occlusal support as well as periodontal condition was significantly associated with the prevalence of atherosclerosis. The associations between atherosclerosis and other potential confounders are shown in Table 1.
Table 1. Demographic and clinical characteristics of the group A by prevalence of atherosclerosis.
| Variable a | N | Atherosclerosis |
p-value (χ2 test) |
|
|---|---|---|---|---|
| Absence (n = 251) |
Prevalence (n = 217) |
|||
| Occlusal support | 0.002 | |||
| Complete | 265 | 155 (58%) | 110 (42%) | |
| Moderate | 79 | 46 (58%) | 33 (42%) | |
| Collapsed | 121 | 48 (40%) | 73 (60%) | |
| Periodontal condition | 0.006 | |||
| Healthy | 73 | 50 (68%) | 23 (32%) | |
| Moderate | 185 | 102 (55%) | 83 (45%) | |
| Severe | 206 | 97 (47%) | 109 (53%) | |
| Gender | <0.001 | |||
| Female | 251 | 169 (67%) | 82 (33%) | |
| Male | 217 | 82 (38%) | 135 (62%) | |
| Living region | 0.091 | |||
| Urban | 237 | 118 (50%) | 119 (50%) | |
| Country | 231 | 133 (58%) | 98 (42%) | |
| Self-rated financial status | 0.816 | |||
| Dissatisfied | 130 | 67 (52%) | 63 (48%) | |
| Moderate | 233 | 128 (55%) | 108 (45%) | |
| Satisfied | 102 | 54 (53%) | 48 (47%) | |
| Education level | 0.021 | |||
| ≤9 years | 110 | 51 (46%) | 59 (54%) | |
| 10–12 years | 235 | 141 (60%) | 94 (40%) | |
| ≥13 years | 121 | 58 (48%) | 63 (52%) | |
| Smoking | <0.001 | |||
| Never | 274 | 176 (64%) | 98 (36%) | |
| Past | 131 | 49 (37%) | 82 (63%) | |
| Current | 39 | 8 (21%) | 31 (79%) | |
| Alcohol exposure | <0.001 | |||
| No | 244 | 151 (62%) | 93 (38%) | |
| Yes | 203 | 86 (45%) | 117 (55%) | |
| Hypertension | 0.483 | |||
| No | 144 | 81 (56%) | 63 (44%) | |
| Yes | 323 | 169 (52%) | 154 (48%) | |
| Diabetes mellitus | <0.001 | |||
| No | 313 | 185 (59%) | 128 (41%) | |
| Yes | 71 | 24 (34%) | 47 (66%) | |
| Dyslipidemia | 0.315 | |||
| No | 168 | 85 (51%) | 83 (49%) | |
| Yes | 263 | 146 (56%) | 117 (44%) | |
| Hyperuricemia | 0.016 | |||
| No | 375 | 209 (56%) | 166 (44%) | |
| Yes | 37 | 13 (35%) | 24 (65%) | |
| Obesity | 0.417 | |||
| BMI<25 | 349 | 191 (55%) | 158 (45%) | |
| BMI≥25 | 119 | 60 (50%) | 59 (50%) | |
a: Data are shown with counts and column percentages, i.e., N (%).
BMI: Body mass index
Table 2 shows the results of multivariable logistic regression analysis to examine the association between the prevalence of atherosclerosis and both occlusal status and periodontal condition, after adjustment for potential confounders, including gender, region of residence, smoking habits, drinking habits, education level, diabetes mellitus, hypertension, dyslipidemia, and hyperuricemia. Global testing indicated that this model predicts the prevalence of carotid atherosclerosis based on a group of independent variables (p < .001). The Collapsed group had significantly a higher risk of atherosclerosis (odds ratio (OR): 1.87, p = .013), compared with the Complete group; a reduction in the number of OSZ was significantly associated with the prevalence of atherosclerosis (p = .035). Individuals with severe periodontal disease were also at significantly higher risk of atherosclerosis than those with healthy periodontal tissues (OR: 2.01, p = .032).
Table 2. Odds ratios of main variables with adjustment for periodontal disease.
| Variable | Odds ratio | 95% CI | p-value |
|---|---|---|---|
| Occlusal support | |||
| Complete | 1.00 | ||
| Moderate | 0.99 | 0.56, 1.75 | 0.958 |
| Collapsed | 1.87 | 1.14, 3.07 | 0.013 |
| Periodontal condition | |||
| Healthy | 1.00 | ||
| Moderate | 1.83 | 0.98, 3.44 | 0.059 |
| Severe | 2.01 | 1.06, 3.79 | 0.032 |
| Gender | |||
| Male | 1.00 | ||
| Female | 0.45 | 0.24, 0.83 | 0.011 |
| Living region | |||
| Urban | 1.00 | ||
| Country | 0.69 | 0.45, 1.07 | 0.100 |
| Smoking | |||
| Never | 1.00 | ||
| Past | 1.80 | 0.97, 3.36 | 0.063 |
| Current | 3.22 | 1.28, 8.11 | 0.013 |
| Alcohol exposure | |||
| No | 1.00 | ||
| Yes | 0.84 | 0.49, 1.44 | 0.520 |
| Education level | |||
| ≤9 years | 1.00 | ||
| 10–12 years | 0.57 | 0.34, 0.98 | 0.041 |
| ≥13 years | 0.83 | 0.45, 1.51 | 0.533 |
| Diabetes mellitus | |||
| No | 1.00 | ||
| Yes | 2.45 | 1.42, 4.21 | 0.001 |
| Hypertension | |||
| No | 1.00 | ||
| Yes | 0.92 | 0.59, 1.43 | 0.703 |
| Hyperuricemia | |||
| No | 1.00 | ||
| Yes | 1.43 | 0.64, 3.20 | 0.385 |
| Dyslipidemia | |||
| No | 1.00 | ||
| Yes | 0.95 | 0.61, 1.48 | 0.817 |
As characteristics of the group B was indicated almost the same as the group A (Table 3), the group B was treated as a representative cohort of the group A in this study.
Table 3. Demographic and clinical characteristics of the group B by prevalence of atherosclerosis.
| Variable a | N | Atherosclerosis |
p-value (χ2 test) |
|
|---|---|---|---|---|
| Absence (n = 202) |
Prevalence (n = 169) |
|||
| Occlusal support | 0.051 | |||
| Complete | 223 | 129 (58%) | 94 (42%) | |
| Moderate | 56 | 33 (59%) | 23 (41%) | |
| Collapsed | 92 | 40 (43%) | 52 (57%) | |
| Periodontal condition | 0.053 | |||
| Healthy | 61 | 41 (67%) | 20 (33%) | |
| Moderate | 151 | 83 (55%) | 68 (45%) | |
| Severe | 159 | 78 (49%) | 81 (51%) | |
| Gender | <0.001 | |||
| Female | 201 | 138 (69%) | 63 (31%) | |
| Male | 170 | 64 (38%) | 106 (62%) | |
| Living region | 0.218 | |||
| Urban | 189 | 97 (51%) | 92 (49%) | |
| Country | 182 | 105 (58%) | 77 (42%) | |
| Self-rated financial status | 0.758 | |||
| Dissatisfied | 108 | 56 (52%) | 52 (48%) | |
| Moderate | 176 | 99 (56%) | 77 (44%) | |
| Satisfied | 86 | 46 (53%) | 40 (47%) | |
| Education level | 0.234 | |||
| ≤9 years | 86 | 43 (50%) | 43 (50%) | |
| 10–12 years | 193 | 113 (59%) | 80 (41%) | |
| ≥13 years | 91 | 45 (49%) | 46 (51%) | |
| Smoking | <0.001 | |||
| Never | 227 | 146 (64%) | 81 (36%) | |
| Past | 96 | 37 (39%) | 59 (61%) | |
| Current | 33 | 6 (18%) | 27 (82%) | |
| Alcohol exposure | <0.001 | |||
| No | 198 | 124 (63%) | 74 (37%) | |
| Yes | 162 | 69 (43%) | 93 (57%) | |
| Hypertension | 0.915 | |||
| No | 115 | 62 (54%) | 53 (46%) | |
| Yes | 255 | 139 (55%) | 116 (45%) | |
| Diabetes mellitus | 0.001 | |||
| No | 253 | 150 (59%) | 103 (41%) | |
| Yes | 46 | 15 (33%) | 31 (67%) | |
| Dyslipidemia | 0.399 | |||
| No | 139 | 71 (51%) | 68 (49%) | |
| Yes | 201 | 112 (56%) | 89 (44%) | |
| Hyperuricemia | 0.024 | |||
| No | 298 | 168 (56%) | 130 (44%) | |
| Yes | 29 | 10 (34%) | 19 (66%) | |
| Obesity | 0.186 | |||
| BMI<25 | 284 | 160 (56%) | 124 (44%) | |
| BMI≥25 | 87 | 42 (48%) | 45 (52%) | |
a: Data are shown with counts and column percentages, i.e., N (%)
The association between the occlusal status and the key dietary intakes was shown in Tables 4 and 5. From bivariate analysis (Table 4), all of key dietary intakes declined in Collapsed group. Although no significant differences of any key dietary intakes between Complete and Moderate groups were found, of Collapsed group, intakes of green and yellow vegetables, fish and shellfish, vitamin E, B6 and n-3PUFAs were significantly lower than those of Complete group.
Table 4. Unadjusted association between key food or nutrient intakes and occlusal support.
| Food Intakes | Occlusal Support | Mean | 95% CI | p-value |
| Green and Yellow Vegetables (g/1000kcal) | Complete | 71.5 | 66.6, 76.4 | (Ref.) |
| Moderate | 68.5 | 57.7, 79.3 | 0.849 | |
| Collapsed | 59.4 | 64.2, 71.8 | 0.023 | |
| Other Vegetables (g/1000kcal) | Complete | 106.8 | 100.0, 113.5 | (Ref.) |
| Moderate | 101.4 | 89.1, 113.6 | 0.746 | |
| Collapsed | 97.6 | 87.7, 107.5 | 0.294 | |
| Fruits (g/1000kcal) | Complete | 81.5 | 73.4, 89.5 | (Ref.) |
| Moderate | 90.9 | 72.8, 108.9 | 0.575 | |
| Collapsed | 78.7 | 65.3, 92.1 | 0.933 | |
| Fish and Shellfish (g/1000kcal) | Complete | 57.7 | 53.4, 62.0 | (Ref.) |
| Moderate | 56.2 | 46.9, 65.6 | 0.945 | |
| Collapsed | 46.5 | 42.0, 51.0 | 0.009 | |
| Nutrient Intakes | ||||
| Vitamin A (μg retinol equivalent/ 1000kcal) | Complete | 2.62 | 2.45, 2.79 | (Ref.) |
| Moderate | 2.44 | 2.07, 2.81 | 0.621 | |
| Collapsed | 2.30 | 2.03, 2.55 | 0.095 | |
| Vitamin C (mg/1000kcal) | Complete | 76.8 | 72.6, 81.1 | (Ref.) |
| Moderate | 76.7 | 67.3, 86.0 | 1.000 | |
| Collapsed | 71.9 | 65.5, 78.3 | 0.438 | |
| Vitamin E (mg/1000kcal) | Complete | 4.32 | 4.18, 4.47 | (Ref.) |
| Moderate | 4.21 | 3.91, 4.50 | 0.743 | |
| Collapsed | 3.97 | 3.75, 4.20 | 0.025 | |
| Vitamin B6 (mg/1000kcal) | Complete | 0.76 | 0.73, 0.78 | (Ref.) |
| Moderate | 0.75 | 0.70, 0.80 | 0.970 | |
| Collapsed | 0.70 | 0.67, 0.74 | 0.048 | |
| Vitamin B12 (mg/1000kcal) | Complete | 6.47 | 6.03, 6.92 | (Ref.) |
| Moderate | 6.56 | 5.59, 7.54 | 0.983 | |
| Collapsed | 5.62 | 5.12, 6.12 | 0.078 | |
| Dietary Fibre (g/1000kcal) | Complete | 7.24 | 6.98, 7.50 | (Ref.) |
| Moderate | 7.27 | 6.65, 7.88 | 0.996 | |
| Collapsed | 6.94 | 6.49, 7.39 | 0.478 | |
| Follic Acid (μg/1000kcal) | Complete | 221.9 | 209.6, 228.5 | (Ref.) |
| Moderate | 208.4 | 188.4, 228.5 | 0.574 | |
| Collapsed | 203.1 | 189.6, 216.5 | 0.160 | |
| n-3PUFAs (g/1000kcal) | Complete | 1.60 | 1.53, 1.67 | (Ref.) |
| Moderate | 1.57 | 1.42, 1.72 | 0.919 | |
| Collapsed | 1.42 | 1.33, 1.51 | 0.013 |
CI: confidence interval, n-3PUFAs: n-3 polyunsaturated fatty acid
Table 5. Relationship of each key food or nutrient to atherosclerosis and to occlusal support, adjusted for covariates.
| Food or Nutrients | < Atherosclerosis> | < Occlusal Support > | ||
|---|---|---|---|---|
| β1 (95% CI) | P-value | β2 (95% CI) | P-value | |
| Green and Yellow Vegetables (g/1000kcal) | -5.02 (-13.1, -3.06) | 0.223 | -7.36 (-16.0, 1.30) | 0.096 |
| Other Vegetables (g/1000kcal) | -2.10 (-12.4, 8.22) | 0.690 | -5.54 (-16.65, 5.57) | 0.328 |
| Fruits (g/1000kcal) | -1.88 (-15.1, 11.3) | 0.779 | 2.67 (-11.75, 17.10) | 0.716 |
| Fish and Shellfish (g/1000kcal) | -5.93 (-12.7, 0.83) | 0.085 | -9.57 (-16.86, -2.27) | 0.010 |
| Dietary Fiber (g/1000kcal) | -0.29 (-0.78, 0.19) | 0.322 | -0.09 (-0.53, 0.36) | 0.706 |
| Vitamin A (μg retinol equivalent/ 1000kcal) | -285.8 (-590.2, 18.6) | 0.442 | -191.7 (-487.7, 104.3) | 0.204 |
| Vitamin C (mg/1000kcal) | -4.77 (-12.3, 2.80) | 0.770 | -1.69 (-8.79, 5.42) | 0.640 |
| Vitamin E (mg/1000kcal) | -0.33 (-0.58, -0.07) | 0.028 | -0.20 (-0.45, 0.04) | 0.107 |
| Vitamin B6 (mg/1000kcal) | -0.05 (-0.09, -0.01) | 0.033 | -0.04 (-0.08, 0.004) | 0.074 |
| Vitamin B12 (mg/1000kcal) | -0.90 (-1.65, -0.15) | 0.119 | -0.82(-1.59, -0.05) | 0.037 |
| Folic Acid (μg/1000kcal) | -13.5 (-30.0, 3.02) | 0.330 | -7.37 (-23.0, 8.26) | 0.355 |
| N-3PUFAs (g/1000kcal) | -0.18 (-0.30, -0.06) | 0.014 | -0.16 (-0.28, -0.04) | 0.012 |
β1 and β2: regression coefficient, CI: confidence interval, n-3PUFAs: n-3 polyunsaturated fatty acid. All models were adjusted for periodontal disease, gender, region of residence, smoking habits, drinking habits, education level, diabetes mellitus, hypertension, dyslipidemia, and hyperuricemia.
After adjusting confounders, green and yellow vegetables (p = .096), fish and shellfish (p = .010), vitamin B6 (p = .074), vitamin B12 (p = .037) and n-3PUFAs (p = .012) were significantly related to occlusal status (Complete & Moderate groups vs. Severe group) (Table 5). In terms of atherosclerosis, fish and shellfish (p = .085), vitamin E (p = .028), vitamin B6 (p = .033) and n-3PUFAs (p = .014) were significantly related (Table 5). Therefore, fish and shellfish, vitamin B6 and n-3PUFAs were the commonly related factors between occlusal status and atherosclerosis.
To assess whether these common related dietary factors have a mediating effect on the relationship between occlusal status and atherosclerosis, changes of odds ratio of occlusal status (Complete & Moderate groups vs. Severe group) on the prevalence of Atherosclerosis when adding the commonly related dietary factors were shown in Fig 1.
Fig 1. Odds ratio of occlusal status towards atherosclerosis assessing the effect of fish and shellfish, vitamin B6 and n-3PUFAs.
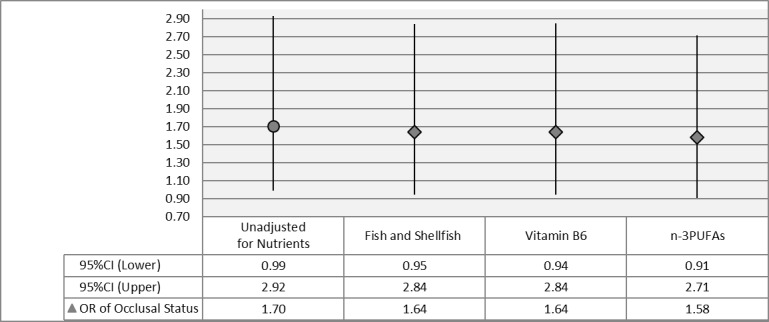
CI: Confidence Interval, OR: Odds Ratio, n-3PUFAs: n-3 polyunsaturated fatty acid, Model*: adjusting for periodontal disease, gender, region of residence, smoking habits, drinking habits, education level, diabetes mellitus, hypertension, dyslipidemia, and hyperuricemia., Model**: Model* + (Fish & Shellfish), Model***: Model* + (Vitamin B6), Model****: Model* + (n-3PUFAs).
Odd ratio of occlusal status from the multiple logistic regression model with no adjustment for any dietary factor was 1.70 (95%CI: 0.99–2.92). However, odd ratio with adjustment for intake of fish and shellfish was reduced into 1.64 (95%CI: 0.95–2.84). Similarly, odds ratio with adjustment for vitamin B6 and n-3PUFAs were declined into 1.64 (95%CI: 0.94–2.84) and 1.58 (95%CI: 0.91–2.71), respectively. This means a statistical mediating effect of Fish and shellfish, vitamin B6 and n-3PUFAs within the relation between occlusal status and atherosclerosis.
Discussion
This cross-sectional study showed an association between occlusal status and atherosclerosis, independent of periodontal condition. Collapsed occlusion in the posterior region was significantly related to the prevalence of atherosclerosis, as was severe periodontal disease. Besides, collapsed occlusion group tended to consume less of all key nutrients, and multivariable assessment showed intakes of green and yellow vegetables, fish and shellfish, vitamin B6, vitamin B12 and n-3 PUFAs were significantly declined in collapsed occlusion group, comparting to complete and moderate groups. Furthermore, fish and shellfish, vitamin B6 and n-3 PUFAs had the mediating effect within the relationship between occlusal status and atherosclerosis. Therefore, the null hypothesis was rejected. Within the limitation of a cross-sectional design, our findings may help to support the hypothesis of one pathway that poor intakes of specific nutrients resulting from decline in the occlusal support of posterior teeth could cause atherosclerosis, apart from periodontitis. This is the first report assessing the two pathways in the same population.
The relationship between periodontal disease and atherosclerosis has been the subject of growing research in recent decades [13], and a literature review reported a potential link between periodontal disease and atherosclerosis through the inflammatory effect of oral bacteria [15]. Another review concluded that there was consistent and strong epidemiologic evidence that periodontitis increases the risk of future cardiovascular disease [14]. We also found that severe periodontal disease was related to the prevalence of atherosclerosis. Therefore, the link between periodontitis and atherosclerosis very possibly exists.
A national diet and nutrition survey in the UK towards 955 older adults reported that the number of posterior tooth occlusion affected perceived chewing ability and food selection [1]. Japanese research groups also reported that loss of occlusion in the posterior region was related to lower consumption of vegetables or fish and shellfish [2,5], and our cohort had also a similar outcomes. The intakes of vegetables, fruits, fish and shellfish are regarded as the key for the prevention of cardiovascular disease, as is mentioned in the Japan Atherosclerosis Society (JAS) guidelines [25]. Vegetables and fruits are a primary dietary source of antioxidant vitamins such as vitamin A, E and C, dietary fiber and folic acid which reported on associations with reduced mortality from cardiovascular disease [6,7,27,30–32]. And fish and shellfish are rich in B-complex vitamins such as vitamin B6 and vitamin B12, and n-3PUFAs which were also reported to have a preventive efficacy of cardiovascular disease in several cohort studies [33–36]. In our cohort study, intake of fish and shellfish, and specifically consumption of vitamin B6 and n-3PUNFAs were significantly related to both of atherosclerosis and occlusal condition. Moreover, these indicated a mediating effect on the relationship between occlusal status and atherosclerosis (Fig 1). So that implies decreasing occlusal support of natural teeth might avoid eating fish and shellfish, and this lower intake of fish and shellfish containing of vitamin B6 and n-3PUNFAs would contribute to atherosclerotic plaque formation. As for vegetables and fruits, no significant relationship with the prevalence of atherosclerosis was observed in our study. And, although collapsed occlusal support group showed lower intake of green and yellow vegetable, intakes of other vegetable and fruit seemed to complement intakes of dietary fiber, vitamin A, vitamin C and folic acid.
As for other conventional risk factors in our study, the multivariable analysis showed that hypertension, dyslipidemia, and hyperuricemia were not significantly related to the prevalence of carotid atherosclerosis, whereas gender, smoking, educational level, and diabetes mellitus were related. The detailed mechanisms underlying the prevalence or absence of a significant relationship with these conventional risk factors cannot be explained based on this study. However, medications for hypertension, dyslipidemia, and hyperuricemia, which would indicate early detection and treatment at a routine medical check-up, could have influenced results. Furthermore, although the prevalence of hypertension and dyslipidemia was high in this study cohort compared with the general population, which would be expected to influence our results, the treatment status was not considered in the present study. In contrast, unmodifiable factors such as gender and smoking habits were shown to have a strong impact. Diabetes mellitus is generally hard to control, which explains why it is one of the main risk factors for atherosclerosis [37].
Because of this observational community-based study design, it cannot be denied that there might still be other hidden confounders’ effect or some sampling bias. However, our study was conducted by a complete enumeration survey method and participants were all of the septuagenarians (69–71 years old) recruited from both urban and rural regions and their dental and medical status was similar to the national data of Japan, indicating that our samples could be a representative of older adults in Japan. Since the general common risk factors of atherosclerosis were comprehensively covered to adjust those influence in this model and also the model was proved well fitted by global testing (p<0.001), it could be optimally designed. Nevertheless, to prove the causal association of our hypothetic pathways, the longitudinal data from our following survey are definitely required.
Conclusions
In conclusion, within the limitations of the cross-sectional study design, which cannot prove causality, this study implied that poorer occlusal support of natural teeth was associated with the prevalence of carotid atherosclerosis. Keeping a good posterior occlusion of natural teeth would possibly be a supportive driving force to prevent cardiovascular or cerebrovascular accidents which are the most common causes of sudden death or disability of older adults worldwide. To establish affirmative evidence of the complex pathway between occlusal status and atherosclerosis via dietary intake, a prospective study is required.
Supporting information
(XLSX)
Acknowledgments
We greatly appreciate our colleagues at Osaka University Graduate School of Dentistry, in particular, Dr. Kaori Enoki, Dr. Yusuke Mihara, Dr. Kodai Hatta who greatly support the SONIC study. We also appreciate the great support of the Japan Cardiovascular Research Foundation.
Data Availability
According to the approval by the Institutional Review Board of Osaka University Graduate Schools of Dentistry (approval number H22-E9) and Medicine (approval number 266) our data set is nor allowed to provide to others. Data can be made available upon request by contacting the data access committee at: sonic@hus.osaka-u.ac.jp.
Funding Statement
This research was supported by a Grant-in-Aid for Scientific Research (Nos. 23390440 and 25293394) from the Japan Society for the Promotion of Science (http://www.jsps.go.jp/english/index.html) and Health Labour Sciences and Research Grant (H26AK002) (http://www.mhlw.go.jp/stf/seisakunitsuite/bunya/hokabunya/kenkyujigyou/index.html).
References
- 1.Sheiham A, Steele JG, Marcenes W, Finch S, Walls AW. The impact of oral health on stated ability to eat certain foods; findings from the National Diet and Nutrition Survey of Older People in Great Britain. Gerodontology. 1999; 16: 11–20. [DOI] [PubMed] [Google Scholar]
- 2.Yoshida M, Kikutani T, Yoshikawa M, Tsuga K, Kimura M, Akagawa Y. Correlation between dental and nutritional status in community-dwelling elderly Japanese. Geriatr Gerontol Int. 2011; 11: 315–319. doi: 10.1111/j.1447-0594.2010.00688.x [DOI] [PubMed] [Google Scholar]
- 3.Sahyoun NR, Lin CL, Krall E. Nutritional status of the older adult is associated with dentition status. J Am Diet Assoc. 2003; 103: 61–66. doi: 10.1053/jada.2003.50003 [DOI] [PubMed] [Google Scholar]
- 4.Sheiham A, Steele JG, Marcenes W, Lowe C, Finch S, Bates CJ, et al. The relationship among dental status, nutrient intake, and nutritional status in older people. J Dent Res. 2001; 80: 408–413. doi: 10.1177/00220345010800020201 [DOI] [PubMed] [Google Scholar]
- 5.Iwasaki M, Taylor GW, Manz MC, Yoshihara A, Sato M, Muramatsu K, et al. Oral health status: relationship to nutrient and food intake among 80-year-old Japanese adults. Community Dent Oral Epidemiol. 2014; 42: 441–450. [DOI] [PubMed] [Google Scholar]
- 6.He FJ, Nowson CA, Lucas M, MacGregor GA. Increased consumption of fruit and vegetables is related to a reduced risk of coronary heart disease: meta-analysis of cohort studies. J Hum Hypertens. 2007; 21: 717–728. doi: 10.1038/sj.jhh.1002212 [DOI] [PubMed] [Google Scholar]
- 7.Joshipura KJ, Hung HC, Li TY, Hu FB, Rimm EB, Stampfer MJ, et al. Intakes of fruits, vegetables and carbohydrate and the risk of CVD. Public Health Nutr. 2009; 12: 115–121. doi: 10.1017/S1368980008002036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nakamura K, Nagata C, Oba S, Takatsuka N, Shimizu H. Fruit and vegetable intake and mortality from cardiovascular disease are inversely associated in Japanese women but not in men. J Nutr. 2008; 138: 1129–1134. [DOI] [PubMed] [Google Scholar]
- 9.Buscemi S, Nicolucci A, Lucisano G, Galvano F, Grosso G, Belmonte S, et al. Habitual fish intake and clinically silent carotid atherosclerosis. Nutr J. 2014; 13: 2 doi: 10.1186/1475-2891-13-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hino A, Adachi H, Toyomasu K, Yoshida N, Enomoto M, Hiratsuka A, et al. Very long chain N-3 fatty acids intake and carotid atherosclerosis: an epidemiological study evaluated by ultrasonography. Atherosclerosis. 2004; 176: 145–149. doi: 10.1016/j.atherosclerosis.2004.04.020 [DOI] [PubMed] [Google Scholar]
- 11.Nanri H, Nakamura K, Hara M, Higaki Y, Imaizumi T, Taguchi N, et al. Association between dietary pattern and serum C-reactive protein in Japanese men and women. J Epidemiol. 2011; 21: 122–131. doi: 10.2188/jea.JE20100110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matheson EM, Mainous AG, Hill EG, Carnemolla MA. Shellfish consumption and risk of coronary heart disease. J Am Diet Assoc. 2009; 109: 1422–1426. doi: 10.1016/j.jada.2009.05.007 [DOI] [PubMed] [Google Scholar]
- 13.Lockhart PB, Bolger AF, Papapanou PN, Osinbowale O, Trevisan M, Levison ME, et al. Periodontal disease and atherosclerotic vascular disease: does the evidence support an independent association?: a scientific statement from the American Heart Association. Circulation. 2012; 125: 2520–2544. doi: 10.1161/CIR.0b013e31825719f3 [DOI] [PubMed] [Google Scholar]
- 14.Aarabi G, Eberhard J, Reissmann DR, Heydecke G, Seedorf U. Interaction between periodontal disease and atherosclerotic vascular disease—Fact or fiction? Atherosclerosis. 2015; 241: 555–560. doi: 10.1016/j.atherosclerosis.2015.04.819 [DOI] [PubMed] [Google Scholar]
- 15.Ahmed U, Tanwir F. Association of periodontal pathogenesis and cardiovascular diseases: a literature review. Oral Health Prev Dent. 2015; 13: 21–27. doi: 10.3290/j.ohpd.a32823 [DOI] [PubMed] [Google Scholar]
- 16.Ikebe K, Matsuda K, Kagawa R, Enoki K, Okada T, Yoshida M, et al. Masticatory performance in older subjects with varying degrees of tooth loss. J Dent. 2012; 40: 71–76. doi: 10.1016/j.jdent.2011.10.007 [DOI] [PubMed] [Google Scholar]
- 17.Takiuchi S, Kamide K, Miwa Y, Tomiyama M, Yoshii M, Matayoshi T, et al. Diagnostic value of carotid intima-media thickness and plaque score for predicting target organ damage in patients with essential hypertension. J Hum Hypertens. 2004; 18: 17–23. doi: 10.1038/sj.jhh.1001628 [DOI] [PubMed] [Google Scholar]
- 18.Teramoto T, Sasaki J, Ueshima H, Egusa G, Kinoshita M, Shimamoto K, et al. Risk factors of atherosclerotic diseases. Executive summary of Japan Atherosclerosis Society (JAS) guideline for diagnosis and prevention of atherosclerosis cardiovascular diseases for Japanese. J Atheroscler Thromb. 2007; 14: 267–277. [DOI] [PubMed] [Google Scholar]
- 19.Kuzuya T, Nakagawa S, Satoh J, Kanazawa Y, Iwamoto Y, Kobayashi M, et al. Report of the Committee on the classification and diagnostic criteria of diabetes mellitus. Diabetes Res Clin Pract. 2002; 55: 65–85. [DOI] [PubMed] [Google Scholar]
- 20.Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res. 2014; 37: 253–390. doi: 10.1038/hr.2014.20 [DOI] [PubMed] [Google Scholar]
- 21.Kobayashi S, Murakami K, Sasaki S, Okubo H, Hirota N, Notsu A, et al. Comparison of relative validity of food group intakes estimated by comprehensive and brief-type self-administered diet history questionnaires against 16 d dietary records in Japanese adults. Public Health Nutr. 2011; 14: 1200–1211. doi: 10.1017/S1368980011000504 [DOI] [PubMed] [Google Scholar]
- 22.Kobayashi S, Honda S, Murakami K, Sasaki S, Okubo H, Hirota N, et al. Both comprehensive and brief self-administered diet history questionnaires satisfactorily rank nutrient intakes in Japanese adults. J Epidemiol. 2012; 22: 151–159. doi: 10.2188/jea.JE20110075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Inomata C, Ikebe K, Kagawa R, Okubo H, Sasaki S, Okada T, et al. Significance of occlusal force for dietary fibre and vitamin intakes in independently living 70-year-old Japanese: from SONIC Study. J Dent. 2014; 42: 556–564. doi: 10.1016/j.jdent.2014.02.015 [DOI] [PubMed] [Google Scholar]
- 24.Teramoto T, Sasaki J, Ishibashi S, Birou S, Daida H, Dohi S, et al. Comprehensive risk management for the prevention of cardiovascular disease: executive summary of the Japan Atherosclerosis Society (JAS) guidelines for the diagnosis and prevention of atherosclerotic cardiovascular diseases in Japan—2012. J Atheroscler Thromb. 2013; 20: 603–615. [DOI] [PubMed] [Google Scholar]
- 25.Teramoto T, Sasaki J, Ishibashi S, Birou S, Daida H, Dohi S, et al. Treatment A) lifestyle modification: executive summary of the Japan Atherosclerosis Society(JAS) guidelines for the diagnosis and prevention of atherosclerotic cardiovascular diseases in Japan—2012 version. J Atheroscler Thromb. 2013; 20: 835–849. [DOI] [PubMed] [Google Scholar]
- 26.Shimazu T, Kuriyama S, Hozawa A, Ohmori K, Sato Y, Nakaya N, et al. Dietary patterns and cardiovascular disease mortality in Japan: a prospective cohort study. Int J Epidemiol. 2007; 36: 600–609. doi: 10.1093/ije/dym005 [DOI] [PubMed] [Google Scholar]
- 27.Kubota Y, Iso H, Date C, Kikuchi S, Watanabe Y, Wada Y, et al. Dietary intakes of antioxidant vitamins and mortality from cardiovascular disease: the Japan Collaborative Cohort Study (JACC) study. Stroke. 2011; 42: 1665–1672. doi: 10.1161/STROKEAHA.110.601526 [DOI] [PubMed] [Google Scholar]
- 28.Choe H, Hwang JY, Yun JA, Kim JM, Song TJ, Chang N, et al. Intake of antioxidants and B vitamins is inversely associated with ischemic stroke and cerebral atherosclerosis. Nutr Res Pract. 2016; 10: 516–523. doi: 10.4162/nrp.2016.10.5.516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cui R, Iso H, Date C, Kikuchi S, Tamakoshi A. Dietary folate and vitamin b6 and B12 intake in relation to mortality from cardiovascular diseases: Japan collaborative cohort study. Stroke. 2010; 41: 1285–1289. doi: 10.1161/STROKEAHA.110.578906 [DOI] [PubMed] [Google Scholar]
- 30.Asplund K. Antioxidant vitamins in the prevention of cardiovascular disease: a systematic review. J Intern Med. 2002; 251: 372–392. [DOI] [PubMed] [Google Scholar]
- 31.Willcox BJ, Curb JD, Rodriguez BL. Antioxidants in cardiovascular health and disease: key lessons from epidemiologic studies. Am J Cardiol. 2008; 101: 75D–86D. doi: 10.1016/j.amjcard.2008.02.012 [DOI] [PubMed] [Google Scholar]
- 32.Kato Y, Ikehara S, Maruyama K, Inagawa M, Oshima M, Yokota K, et al. Trends in dietary intakes of vitamins A, C and E among Japanese men and women from 1974 to 2001. Public Health Nutr. 2009; 12: 1343–1350. doi: 10.1017/S1368980008003960 [DOI] [PubMed] [Google Scholar]
- 33.Cui R, Iso H, Date C, Kikuchi S, Tamakoshi A, Japan Collaborative Cohort Study G. Dietary folate and vitamin b6 and B12 intake in relation to mortality from cardiovascular diseases: Japan collaborative cohort study. Stroke. 2010; 41: 1285–1289. doi: 10.1161/STROKEAHA.110.578906 [DOI] [PubMed] [Google Scholar]
- 34.Dong H, Pi F, Ding Z, Chen W, Pang S, Dong W, et al. Efficacy of Supplementation with B Vitamins for Stroke Prevention: A Network Meta-Analysis of Randomized Controlled Trials. PLoS One. 2015;10(9):e0137533 doi: 10.1371/journal.pone.0137533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ishihara J, Iso H, Inoue M, Iwasaki M, Okada K, Kita Y, et al. Intake of folate, vitamin B6 and vitamin B12 and the risk of CHD: the Japan Public Health Center-Based Prospective Study Cohort I. J Am Coll Nutr. 2008; 27: 127–136. [DOI] [PubMed] [Google Scholar]
- 36.Iso H, Kobayashi M, Ishihara J, Sasaki S, Okada K, Kita Y, et al. Intake of fish and n3 fatty acids and risk of coronary heart disease among Japanese: the Japan Public Health Center-Based (JPHC) Study Cohort I. Circulation. 2006; 113: 195–202. doi: 10.1161/CIRCULATIONAHA.105.581355 [DOI] [PubMed] [Google Scholar]
- 37.Fox CS, Golden SH, Anderson C, Bray GA, Burke LE, de Boer IH, et al. Update on Prevention of Cardiovascular Disease in Adults With Type 2 Diabetes Mellitus in Light of Recent Evidence: A Scientific Statement From the American Heart Association and the American Diabetes Association. Diabetes Care. 2015. August 5 pii: dci150012. doi: 10.2337/dci15-0012 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
Data Availability Statement
According to the approval by the Institutional Review Board of Osaka University Graduate Schools of Dentistry (approval number H22-E9) and Medicine (approval number 266) our data set is nor allowed to provide to others. Data can be made available upon request by contacting the data access committee at: sonic@hus.osaka-u.ac.jp.


