Abstract
Chronic pain disorders represent a significant public health concern, particularly for children and adolescents. High rates of comorbid anxiety and unipolar mood disorders often complicate psychological interventions for chronic pain. Unified treatment approaches, based on emotion regulation skills, are applicable to a broad range of emotional disorders and suggest the possibility of extending these interventions to chronic pain and pain-related dysfunction. This case report describes the use of a unified protocol for treatment of an adolescent boy with chronic daily headache and social anxiety and an adolescent girl with whole body pain and depression. Following weekly, 50-minute individual treatment sessions, the boy demonstrated notable improvement in emotional symptoms, emotion regulation skills, somatization, and functional disability. The girl showed some improvement on measures of anxiety and depression, although there appeared to be a worsening of pain symptoms and somatization. However, both patients demonstrated improvement over follow-up. This case study illustrates the potential utility of a unified treatment approach targeting pain and emotional symptoms from an emotion regulation perspective in an adolescent population.
Keywords: chronic pain, anxiety, depression, adolescents, unified treatment
Chronic intractable nonmalignant pain, including such disorders as complex regional pain syndrome type 1 (CRPS-1), chronic daily headache, fibromyalgia, myofascial pain, and recurrent abdominal pain, is now recognized as a significant problem among children and adolescents, with potential long-term impact on the child's physical, social, and academic functioning, as well as on the family as a whole (Kashikar-Zuck et al., 2010; Smith & Smith, 2010; Walker, Dengler-Crish, Rippel, & Bruehl, 2010). A significant concern for children and adolescents with chronic pain is the high rate of comorbid anxiety and depression in this patient population (Campo, Bridge, et al., 2004; Campo, Comer, Jansen-Mcwilliams, Gardner, & Kelleher, 2002; Dorn et al., 2003; Ghanizadeh et al., 2007; Lipsitz et al., 2005; Ramchandani, Fazel, Stein, Wiles, & Hotopf, 2007). Generally, results across these studies indicate a greater risk of comorbid anxiety and/or unipolar mood disorders, as well as increased levels of anxiety and depression symptoms in individuals with chronic pain. These data highlight the significant overlap between physical and psychological disorders.
Possible Mechanisms Underlying Pain and Emotions
The biopsychosocial model of pain purports that chronic pain represents a complex interaction of biological, psychological, and social factors (Gatchel, Peng, Peters, Fuchs, & Turk, 2007). Pain itself is a multidimensional construct incorporating both sensory (e.g., intensity, duration) and affective (emotional) aspects. Recognition of the affective dimension of pain has focused attention on the ways in which mood states influence the pain experience. For example, higher levels of anticipatory anxiety about an upcoming pain task have been shown to predict increased pain responses to that pain task in children and adolescents (Tsao et al., 2004).
Neurobiological
Although the mechanism(s) by which emotions influence pain is unclear, it is possible that pain and emotions share similar neurobiological pathways. A recent study explored the neural correlates of pain anticipation in a sample of participants with and without major depressive disorder (MDD) (Strigo, Simmons, Matthews, Craig, & Paulus, 2008). Results suggested that anticipation of the pain task led to increased activity in brain areas associated with emotional reactivity only for subjects with MDD. Furthermore, in subjects with MDD only, greater activation in the right amygdala during anticipation of pain was associated with greater levels of perceived helplessness. The authors suggest that the presence of MDD may lead to an impaired ability to modulate painful experiences due to activation of these emotional centers of the brain (Strigo et al., 2008). Others have highlighted the role of the endogenous opioid system in the modulation of both pain and stress (anxiety; Ribeiro, Kennedy, Smith, Stohler, & Zubieta, 2005).
Emotion Regulation
Given the prominent role of mood in modulating the pain experience, it follows that difficulties in regulating emotions may have an adverse impact on pain. Emotion regulation (ER) refers to attempts to change subjective experiential, cognitive, behavioral, or physiological emotional responses in oneself or others. While some approaches are adaptive, growing evidence suggests that excessive and rigid attempts to control, suppress, or hide emotional experiences results in increased levels, intensity, and duration of the very emotion attempting to be regulated (Barrett, Rapee, Dadds, & Ryan, 1996; Gross, 2002; Keefe et al., 2001; Zeman, Cassano, Perry-Parrish, & Stegall, 2006).
Although evidence now supports the concept of emotion dysregulation as both a contributing and maintaining factor for emotional disorders, more recently this concept has been extended to physical health and pain. Initial findings highlight a potentially important role of ER in pain responses, with evidence pointing especially to problems with emotion identification and expression (Lumley, Beyer, & Radcliffe, 2008; Mattila et al., 2008; Tuzer et al., 2010). Similarly, the tendency to inhibit or suppress feelings appears to have deleterious consequences with regard to pain. In laboratory studies, students instructed to suppress thoughts of pain demonstrated poorer recovery following a cold pressor pain task, as compared to students who were asked to monitor pain responses. In addition, recall of pain intensity was significantly higher in the suppression group (Cioffi & Holloway, 1993). In a separate investigation, when individuals were asked to suppress thoughts about pain prior to a pain task, they reported significantly more intrusive thoughts about the pain and greater pain severity, as compared to those who were not asked to suppress (Sullivan, Rouse, Bishop, & Johnston, 1997). In chronic pain patients (women with fibromyalgia), intensity of affect was related to more severe pain, only for those individuals who also had difficulty identifying and expressing feelings (van Middendorp et al., 2008). These findings suggest that interventions aimed at improving ER and psychological flexibility (i.e., flexibility in behavioral responding to various emotional states) may assist in the amelioration of chronic pain.
Psychological Treatments for Chronic Pain
Psychologically based therapies are commonly used to assist individuals with chronic pain to improve function and reduce disability (Jensen, Nielson, & Kerns, 2003). In a recent review, Eccleston and colleagues (2009) found that psychological therapies (such as cognitive behavior therapy [CBT], biofeedback, hypnosis, and relaxation) were effective for treating pain in children with headache, abdominal pain, and musculoskeletal pain. Similar results were obtained in a meta-analysis of psychological therapies for children with pain (Palermo, Eccleston, Lewandowski, Williams, & Morley, 2010). More recently, a treatment that uses exposures in combination with an acceptance-based approach rooted in Acceptance and Commitment Therapy (ACT; Hayes, Strosahl, & Wilson, 1999) has been applied to adolescents with chronic pain with demonstrated success as compared to a multidisciplinary treatment approach that included amitriptyline (Wicksell, Melin, Lekander, & Olsson, 2009).
Despite these encouraging data on the efficacy of psychological interventions for pain, there are still a number of patients who remain impaired following treatment or who do not improve at all (Eccleston, Morley, Williams, Yorke, & Mastroyannopoulou, 2002; Merlijn et al., 2005). Eccleston and colleagues (2002) note that the major limitations of available studies to this point have focused on pain relief as the primary outcome variable, when there are other critical factors that may be necessary to address. An even more recent review highlighted the need for data on the effect of therapies on disability and mood (Eccleston et al., 2009). Given the high rate of anxiety and depressive symptoms in chronic pain, these potentially “complicating” comorbidities (which appear to increase the risk for and possibly exacerbate pain disorders) may be a specific target of change in future interventions.
In fact, both pharmacological and psychological interventions have begun to be applied specifically to individuals with chronic pain and anxiety/mood disorders. A recent single arm pilot study explored citalopram for recurrent abdominal pain and internalizing disorders in children ages 7 to 18 years. After 12 weeks of treatment, 84% of participants were classified as treatment responders, with evidence of improvement in ratings of pain, anxiety, depression, functional impairment, and somatic symptoms (Campo, Perel, et al., 2004). However, results must be interpreted with caution, given the nature of the study design.
Another promising approach is the Treatment for Anxiety and Physical Symptoms (TAPS), specifically for adolescents with chronic pain and comorbid separation, social, or generalized anxiety disorders (Reigada, Fisher, Cutler, & Masia Warner, 2008). This protocol, based on the Coping Cat Workbook (Kendall, 1992), uses a standard cognitive behavioral approach including psychoeducation, relaxation, cognitive restructuring, and exposures. In a pilot, single arm study, seven children (ages 8 to 15) with abdominal pain and anxiety received 12 weekly sessions of individual TAPS treatment with all participants classified as treatment responders (reductions in diagnostic severity, anxiety, and pain; Masia Warner, Reigada, Fisher, Saborsky, & Benkov, 2009). Although these data are encouraging, small sample, single pain condition, and lack of follow-up limit strength of conclusions.
Unified Protocol for the Treatment of Emotions in Youth With Pain (UP-YP)
Ehrenreich-May and Bilek (2012) provide a review of the research and background supporting a unified approach to treating emotional disorders in adults and adolescents, a review that will not be repeated here. In short, a unified, or transdiagnostic, approach may represent a more efficient, and possibly more efficacious, way to ameliorate overlapping emotional disorder symptomatology (comorbidity), in addition to facilitating effective dissemination of empirically supported treatments to practicing clinicians (Allen, Ehrenreich, & Barlow, 2005). We believe that chronic pain disorders naturally fit within this transdiagnostic paradigm, given the high rates of psychological comorbidity in chronic pain populations, common neurobiological underpinnings, evidence of emotion dysregulation associated with chronic pain, and the efficacy of cognitive-behavioral strategies for managing chronic pain. The treatment presented here is an adaptation of the Unified Protocol for the Treatment of Emotional Disorders in Youth (UP-Y; Ehrenreich-May et al., 2008) for use with adolescents (ages 12 to 17) with a chronic pain disorder and self-reported symptoms of anxiety and/or depression. Our adaptation of the protocol differs substantially from the UP-Y by emphasizing emotional reactions to discomfort and pain—an area that is only minimally addressed in the UP-Y in the context of interoceptive exposure and panic attacks.
The UP-YP (Allen, Tsao, Zeltzer, Ehrenreich-May, & Barlow, 2010) is a transdiagnostic treatment that uses cognitive-behavioral principles to address both pain-related and emotional dysfunction. This unified approach differs from the transdiagnostic approaches described earlier (e.g., Masia Warner et al., 2009; Reigada et al., 2008) in a number of important ways. First, from a theoretical perspective, the UP-YP goes beyond the application of general cognitive-behavioral strategies to pain and anxiety and instead focuses on identifying and modifying maladaptive emotion regulation and response strategies associated with the experience of pain. Although the techniques may be similar to traditional CBT, the function is different. In the UP-YP, the therapist aims to implement more adaptive emotion regulation skills using a variety of situations and contexts, and this theoretical shift allows the UP-YP to be applied to any emotional experience, regardless of whether it stems from pain or is related to anxiety, depression, anger, etc. Second, as this theoretical perspective implies, therapists will not be limited to working with only certain types of pain disorders or emotional comorbidity (including depressive disorders). Even though the particular situations and contexts may be different given different symptom presentation, the function of the treatment strategies in the UP-YP is similar.
Treatment Approach
The UP-YP is a flexible, modular-based individual treatment protocol. A full course of treatment can consist of between 8 and 21 50-minute sessions, all occurring within a 6-month time frame. It is recommended that, at least initially, sessions occur on a weekly basis. However, as termination approaches, sessions may be spaced out to every 2 weeks. Therapists using the UP-YP are expected to have some level of familiarity with traditional CBT protocols; however, initial research has shown that even junior-level therapists are able to successfully use the protocol in adults (Ellard, Fairholme, Boisseau, Farchione, & Barlow, 2010) and adolescents (Ehrenreich, Goldstein, Wright, & Barlow, 2009) with emotional disorders.
The UP-YP modules are as follows and are described in more detail in the context of the case presentations below: (a) psychoeducation about emotions and pain, (b) awareness of emotions and pain, (c) flexibility in thinking, (d) modifying emotion-driven behaviors through exposures, and (e) treatment review and relapse prevention. In addition, several optional modules are available for therapists, which include (a) building and keeping motivation, (b) keeping safe (for adolescents with suicidal ideation or intent), and (c) parenting the emotional adolescent with pain. Regarding delivery of the UP-YP, it is important to note that some of the basic procedures described in the protocol are not necessarily different from the procedures a therapist might employ using a traditional CBT protocol. In fact, it is the theoretical underpinnings and conceptualization that makes the UP-YP unique and different from traditional CBT. Whereas CBT aims to improve emotional reactions through modification of maladaptive cognitions and elimination of conditioned associations with environmental cues, the UP-YP aims to modify both pain and emotions based on emotion theory using an emotion regulation framework: creating emotional change through reduced emotional avoidance and modification of action tendencies. Therefore, although the techniques may appear similar for clients with similar diagnoses or symptoms, the potential value of the UP-YP is in teaching therapists the necessary targets of emotional change so that strategies can be applied flexibly and individually across clients with various presenting complaints.
Case Examples
Case 1: Kevin
Kevin1 was a 14-year-old Caucasian/Hispanic boy in the eighth grade referred to the Pediatric Pain Program for management of chronic daily headache. Kevin was aggressively tackled while playing football approximately 2 weeks prior to the onset of his symptoms 1 year earlier and reported experiencing constant, disabling headaches since then. Kevin also stated that, prior to his football injury, he had been experiencing mild but increasingly symptomatic headaches in the previous year. He missed a large majority of the school year due to headaches and was being home-schooled. At the time of admission to the Pediatric Pain Program, no treatment (including a hospitalization) had resulted in any substantial reduction in his headaches. He had also participated in an integrative pain management program that included acupuncture, craniosacral massage, self-hypnosis/relaxations skills, but Kevin continued to have daily headaches.
Kevin also described experiencing some anxiety about schoolwork and social relationships. Upon further questioning, it appeared that anxiety in a variety of social situations was causing some impairment in his ability to make and maintain friendships. Although Kevin reported having a “best friend,” it was later discovered that this friend lived over an hour away and he saw him only two to three times per year. Kevin had some additional friends at school, although he denied having a close relationship with any of them. When encountering others, Kevin reported that he usually enjoyed making his peers laugh but he would often remain silent if he could not think of anything to say. He also experienced significant anxiety while talking to his friends on the phone. In school, Kevin worried that he would say the “wrong thing” or ask a “stupid question” so he was often very quiet in class.
One additional factor contributing to Kevin's difficulty with peer relationships was his apparent lack of desire to have close friends—a symptom that did not appear related to social anxiety. In fact, despite his anxiety around others, he reported that it was “fine” with him if he did not have any close friends and he was not particularly interested in meeting and having a wide social circle. He reported difficulty connecting with peers and did not share similar interests, instead preferring to be by himself and communicate with peers via the Internet.
Integrative Assessment
Kevin's medical history was reviewed extensively by a pediatric pain physician (L. Zeltzer). Prior evaluations by two child neurologists, including brain imaging studies, were negative and he had failed multiple trials of typical migraine-focused medications. Pain clinic biopsychosocial assessment including the nature of the headaches and physical examination findings of multiple neck muscular tender points with lack of other structural (e.g., spinal) reasons for pain provided criteria for diagnoses of chronic daily headaches (central and myofascial). Kevin was also referred for neuropsychological testing to explore the possibility of a diagnosis of high-functioning autism spectrum disorder (ASD) to capture his apparent indifference to spending time alone, perseveration on small details associated with tasks, and extreme sensitivity to light and sound. The diagnosis of a high-functioning ASD was confirmed, and it was hypothesized that his ASD neurobiology could be exacerbating Kevin's headaches by creating a low tolerance for headache pain as well as perseveration on his pain. His ASD also may have created challenges for Kevin to filter sensory stimuli and caused him to perseverate on his pain without developing other coping strategies. Assessment of Kevin's psychological symptoms through self-report questionnaires and unstructured clinical interview also suggested a diagnosis of social anxiety disorder, with symptoms of generalized anxiety disorder present at a subclinical level.
Transdiagnostic Case Conceptualization
Kevin's symptom presentation fit well within the transdiagnostic conceptualization of pain and emotional disorders. His symptoms of headache and social anxiety were related in that Kevin's worry and avoidance of situations related to both pain and anxiety were identified as maladaptive emotion regulation strategies that were maintaining his symptoms. The UP-YP aimed to address this emotion dysregulation by teaching Kevin to learn to tolerate his emotions associated with both social anxiety and pain, and to modify behavioral responses to situations he would typically escape or avoid.
Case 2: Marla
Marla was a 17-year-old Caucasian girl in the eleventh grade, who presented to the Pediatric Pain Program with pain in many parts of her body. For example, Marla reported that her stomach hurt when eating or drinking anything before 1:00 P.M. and she would get sick to the point where she “couldn't think.” She stated that the pain was “constant,” with no vomiting, constipation, diarrhea, or bloating, and she was unable to get any relief from the stomach pain. In addition, she reported that her neck hurt “most of the time,” and her joints felt “frozen [when] trying to move them,” although they were never red or swollen. Marla also felt pain in her chest, which she described as “blinding, searing, hot pain.” She said the pain felt worse when breathing in and out, but she did not feel out of breath.
Marla also reported experiencing symptoms of depression and anxiety that began when the pain initially started. She described feeling “negative” on many days, in combination with a general lack of interest in activities other than playing in the school band, trouble falling asleep and also difficulty waking up, irritability, difficulty concentrating, and psychomotor retardation. Marla also described having some passive suicidal ideation (i.e., thoughts that she would be better off dead), but denied any current or past history of suicidal intent, plan, or attempts. She also described herself as a worrier, with worries focused on her schoolwork and where she will attend college.
Integrative Assessment
Marla's medical history and all past related laboratory and radiographic studies were reviewed by a pediatric pain physician (L. Zeltzer), who concluded, after a biopsychosocial assessment and the only positive findings on physical examination of widespread numerous muscle tender points, that she met criteria for fibromyalgia and functional abdominal pain with nausea and constipation. Marla was also presenting with symptoms of depression and anxiety as evidenced by self-report questionnaires and responses during the unstructured clinical interview with the physician, and she reported that her low mood, irritability, and thoughts of death were most problematic for her. As a result, Marla was diagnosed with fibromyalgia, irritable bowel syndrome (IBS), and MDD.
Transdiagnostic Case Conceptualization
From the perspective of the UP-YP, Marla's symptoms of depression, fibromyalgia, and IBS were connected both behaviorally and emotionally. Depression and pain share common neurobiological pathways, and also Marla's emotional responses to pain (i.e., feelings of hopelessness) were clearly associated with her symptoms of depression. The UP-YP aimed to address Marla's dysregulated emotional responses to pain by encouraging her to acknowledge and not avoid or control her emotions related to pain and her feelings of hopelessness.
Measures
Both Kevin and Marla and their respective parents participated in intake interviews and general medical exams with a pediatrician. Upon study enrollment, Kevin and Marla (and their parents) also participated in brief, semistructured interviews about current and past history of pain, and Kevin and Marla each completed self-report questionnaires throughout the treatment.
Pain Interview
This interview was created using items derived from Schanberg et al. (2001) and McGrath et al. (2000) to determine current and past pain experience, the presence of pain models, and pain-related health care utilization.
Children's Somatization Inventory (CSI; Walker & Garber, 2003)
The CSI measures perceptions of nonspecific somatic symptoms. Children rate how much they were bothered by each of 35 symptoms (e.g., headaches) during the last 2 weeks using a 4-point scale (0=not at all to 3=a whole lot). Adequate reliability and validity have been established (Walker & Garber; Walker, Garber, & Greene, 1993; Walker, Garber, Van Slyke, & Greene, 1995). School and clinical samples suggest normative means of 19.02 (SD=17.06; range 0–120) and 22.69 (SD=14.45, range 3–81), respectively (Walker & Garber).
Emotion Expression Scale for Children (EESC; Penza-Clyve & Zeman, 2002)
The EESC examines two aspects of deficient emotion expression: lack of emotion awareness and reluctance to express negative emotion. It consists of 16 items that are ranked using a five-point Likert scale from 1 (not at all) to 5 (extremely true). Scores for the Poor Awareness and Expressive Reluctance subscales range from 8 to 40, with higher scores pointing towards a deficiency in these two areas. Internal consistency for the EESC based on a community sample of 208 children is .83 for the Poor Awareness factor and .81 for the Expressive Reluctance factor. Test-retest reliabilities for the EESC are low but adequate, at .59 and .56, respectively. Community sample normative estimates report mean scores of 15.61 (SD=6.40) for the Poor Awareness subscale and 17.33 (SD=6.46) for the Expressive Reluctance subscale.
Faces Pain Scale–Revised (FPS-R; Hicks, von Baeyer, Spafford, van Korlaar, & Goodenough, 2001)
The FPS-R is a self-report measure to assess the intensity of children's pain. Children rate their current level of pain as represented in one of six drawings of facial expressions ranging from no pain (0) to very severe pain (10).
Functional Disability Inventory (FDI; Walker & Greene, 1991)
The FDI is a 15-item measure assessing perceived difficulty in physical and psychosocial functioning in the past 2 weeks due to physical health. Items are rated on a 5-point scale (0=no trouble to 5=impossible). Walker and Greene reported high internal consistency (alphas=.85 – .92) and a 2-week test-retest reliability of .80 for pediatric patients with recurrent abdominal pain. The mean score on this measure was 11.25 (SD=9.84; range 0–53) in a sample of children with recurrent abdominal pain (Claar & Walker, 2006).
Revised Child Anxiety and Depression Scale (Chorpita, Yim, Moffitt, Umemoto, & Francis, 2000)
This 47-item adaptation of the Spence Children's Anxiety Scale (SCAS; Spence, 1997; SCAS; Spence, 1998) assesses children's report of symptoms corresponding to selected DSM-IV anxiety disorders and depression. Children rate how often each item applies to them. Items are scored 0 to 3 corresponding to “never, “sometimes,” “often,” and “always.” This measure has acceptable reliability and validity (Chorpita, Moffitt, & Gray, 2005; Chorpita et al., 2000).
Procedure
Treatment Overview
Kevin
Kevin's treatment took place over the course of seventeen 50-minute weekly sessions with an individual therapist (L. Allen). The first module of the UP-YP consists primarily of psychoeducation about emotions and pain responses. Treatment began with a review of the functional/adaptive nature of emotions and pain, describing how both are signals that can give important information about the environment. Kevin initially struggled with understanding the function of emotions and had difficulty identifying his own emotions. Because the UP-YP is heavily focused on emotions and (eventual) modification of subsequent responses, emotional awareness is a particularly important skill that is taught at the beginning of treatment. Due to Kevin's difficulty recognizing and identifying his emotions, a number of initial sessions were spent discussing various emotional states and how Kevin could better identify how he was feeling by describing how he or others might appear (body language, facial expression) when experiencing different emotions. Kevin was also asked to monitor his emotions and pain levels at various times during the day and notice if there was a connection between his mood and pain. Through this practice, Kevin was able to acknowledge that when he experienced “stress,” his head pain became worse; however, he also reported that feeling relaxed did not make his pain better. Kevin was encouraged to consider the possibility that the exercises and skills he would learn would not necessarily reduce his pain immediately, although he could begin to learn ways to stop the cycle of pain and emotions.
The second module of the UP-YP focused specifically on awareness of emotions through the use of specific practices designed to elicit different emotions. The first awareness skill involved using diaphragmatic breathing as an opportunity to become more aware of what Kevin was feeling, both physically and emotionally. Consistent with an emotional acceptance-based approach, the UP-YP does not emphasize breathing as way to “relax,” as this may have the unintended effect of creating increased levels of anxiety/stress because of the implied goal of suppressing any “nonrelaxing” experiences. In this sense, breathing is only used as a tool to increase awareness. He also engaged in some exposures designed to trigger at least mild pain symptoms, such as specifically attending to his head pain. During these exposures, the goal was not to create or exacerbate this pain, per se; rather, he was told to practice being aware of his emotional responses to the pain. In this sense, the UP-YP was targeting the emotional dysregulation (affective component) related to pain, rather than the sensory experience of pain. Although Kevin did report an improvement in his level of awareness of both pain and stress as a result of this module, he found the concepts somewhat abstract and difficult to grasp. As a result, the therapist only chose to spend a single session on this module.
Next, the importance of flexibility in thinking (Module 3) was introduced. Kevin had never considered that his own interpretations may be subject to his personal experience; he had always considered his thoughts as “facts.” He was able to generate alternative interpretations of various ambiguous pictures, a process that helped illustrate the importance of flexibility in thinking. Next, the therapist reviewed specific skills for responding to automatic interpretations, including identification of “thinking traps” (i.e., negative or unhelpful ways of thinking that are easy to get “stuck” in) and “detective questioning” (i.e., using evidence from past experience to consider whether automatic interpretations are accurate). In this module, Kevin first chose to focus on automatic interpretations that were present when calling friends on the phone. He identified one automatic interpretation as “I'll say the wrong thing and then my friend won't like me anymore.” This interpretation was first identified as the “jumping to conclusions” thinking trap. Then, the therapist helped Kevin use detective questioning skills to examine the likelihood of saying the wrong thing and the likelihood that his friend would not like him anymore. Kevin was also able to identify how he would cope if his friend actually did not like him anymore.
Kevin also identified that he would engage in “thinking the worst” (i.e., catastrophizing) when he would anticipate experiencing head pain. These interpretations were often triggered when Kevin was asked to go to school or on a field trip for school. Kevin reported he was afraid of doing these activities because he believed that his head pain would get worse and would not get better. Detective questioning skills helped Kevin reevaluate the likelihood that his head pain would never get any better by looking at the fluctuations in his pain levels over the course of several days or a week. He was also able to consider that he could cope with higher levels of head pain by looking at how often he rated his pain as a “10” (on a 0–10 scale). Being flexible in his interpretations of the pain helped Kevin experience less anxiety when confronted with these situations.
Another situation where Kevin noticed the “jumping to conclusions” thinking trap was related to his concern about getting into a particular high school. Even though this situation was not related to the target disorder (social anxiety disorder), the flexibility of the UP-YP allowed the therapist to apply the same skills to the emotion of anxiety related to general worry, as opposed to the particular situation associated with the target disorder. Kevin's automatic interpretation was that if he did not get into a particular high school, he would not be able to attend the college of his choice. Through detective questioning skills, he was able to identify that many other aspects of his application would be relevant to college admission other than just the high school he attended.
The fourth module of the UP-YP involved specifically designing and executing situational exposures that triggered uncomfortable emotions so that behaviors that occurred during the experience of emotion (i.e., “emotion-driven behaviors”—usually escape during the experience of fear) could be modified, and emotional avoidance and safety behaviors would be reduced or eliminated. In this module, the triggers can vary from interoceptive (e.g., pain) to situational (e.g., in vivo), so that the therapist has a large amount of flexibility to design effective emotion exposures. For Kevin, emotion exposures initially began in a social context. He chose various passages and poems to read aloud in front of the therapist and confederates. Kevin struggled with reading aloud in class and church, and if he did read aloud, he would often engage in avoidance behaviors such as speaking quietly and/or refraining from expressing emotion while speaking. If he was asked to read aloud, he would also escape from the situation by leaving the room. These avoidance and emotion-driven behaviors were specifically identified and Kevin was asked to both speak loudly and with expression. He initially reported high levels of anxiety when conducting in-session exposures, although over the course of this module, Kevin became significantly less anxious about his anxiety in a public speaking context. In-session interoceptive exposures began with conducting a symptom induction test, where Kevin was asked to engage in three exercises: spinning while standing, hyperventilating, and breathing through a thin straw. He completed these exercises and noted that hyperventilating triggered anxiety about his head pain becoming worse, so Kevin was asked to practice hyperventilating daily at home. Even though his physiological reaction to the hyperventilating did not change, his anxiety about his physiological reaction decreased over the course of his practice, which was the primary aim of the exposure. Kevin also practiced not wearing his sunglasses during session, which constituted an exposure to the anxiety about his head pain getting worse. Similarly, he still experienced discomfort during the exercise even after repeated practice, but his anxiety about the practice decreased.
Out-of-session practices typically focused on interacting with peers and engaging in activities that Kevin had previously avoided due to anxiety about his head pain. Near the end of treatment, Kevin even agreed to perform in a lip synching performance for his church, which he reported went very well. Treatment strategies also focused on Kevin's avoidance of situations due to fears of triggering and exacerbating his head pain, so he began attending school more regularly, even when he would be in noisy and bright situations. He would have avoided these activities in the past because he worried that the noises increased his head pain. Kevin also spent more time with his family and made an effort to be more active in his daily life. Even though Kevin was fearful that these activities would increase his head pain, he noticed that although his pain levels generally stayed at the same level, his overall mood improved substantially.
The final module (Module 5) consisted of one session reviewing Kevin's progress and anticipating future difficulties. At this session, Kevin was back at school nearly full-time and regularly engaging in social activities. He was able to better identify how he was feeling and notice if he was experiencing stress. Kevin was regularly applying the flexible thinking skills and practicing exposures outside of session. His eye contact had improved and he was able to smile and laugh in session. Both Kevin and his parents reported significant improvement in his anxiety and disability, even though his head pain levels were similar to when he began treatment.
The UP-YP allows for several parenting sessions as part of the optional parenting module. Kevin's parents were both actively involved in the treatment process and understood the role of avoidance and negative reinforcement. Both Kevin and his therapist agreed that scheduling additional sessions with his parents was not necessary for treatment. Instead, the therapist, Kevin, and his parents met as a group for approximately 10 minutes at the end of every session to review session content, discuss homework practice, and answer questions. However, it is conceivable that other more complex cases may require a more substantial parent component.
Kevin's course of treatment was distinctively transdiagnostic in that he was taught specific skills that were then flexibly applied to his emotional disorder and pain responses. In particular, the skills of emotional identification and awareness, as well as flexibility in thinking, proved to be relevant and helpful to Kevin across the diagnostic categories of his presenting symptoms. Although the specific techniques (i.e., social anxiety exposures) may be similar to those found in traditional CBT protocols, it is the conceptualization of the mechanisms of treatment that makes the UP-YP unique. The value of this transdiagnostic conceptualization of mechanisms is that it allows the therapist to more efficiently, and perhaps more effectively, address a variety of presenting complaints, as in the case of Kevin.
Marla
Marla participated in a total of twelve 50-minute weekly sessions with an individual therapist (L. Allen). After providing basic psychoeducation about emotions and pain responses, as with Kevin, Marla was encouraged to consider in what situations her emotions and pain were functional. She quickly identified how a foot injury triggered an appropriate pain and emotional response in that the pain sensations and anxiety about experiencing more pain helped her stay off her foot until the tissue healed. After discussing the functional nature of that response, treatment focused on identifying the negative (i.e., dysfunctional) cycle of pain and mood that had developed in response to Marla's initial back pain. Marla was able to acknowledge how whenever she experienced pain, she would experience a very “negative” emotional response in that she would feel hopeless and want to “give up” trying to improve her functioning. As a result, she became less active, spent less time with friends, and her symptoms of irritability began to interfere in her relationship with her parents. Marla struggled with the concept of being aware of her emotions, as she would often react to the experience of any negative mood (i.e., anger, frustration, hopelessness) by withdrawing and disengaging from the conversation (which were conceptualized in session as emotion-driven behaviors). However, she was able to monitor her moods over the course of the week and reported that her mood was lower when she was experiencing more pain, and negative moods also triggered pain.
In the second module of the UP-YP, Marla was taught the skills of emotional awareness, so that she could continue to become more aware of her emotional responses to pain and other triggers. In session, she was asked to notice sensations in her body as she moved her extremities (which triggered pain sensations). She was also asked to notice her emotional response to the sensations of pain, and not avoid her emotions by stopping the activity. Marla had difficulty completing these exercises and reported that she would typically stop an exercise as soon as she experienced any discomfort in her body. Although encouraging activities is a part of traditional CBT protocols for pain, the UP-YP emphasized the role of emotional avoidance and its relationship to pain responses. Marla was asked to continue to practice awareness of her emotions in other situations, such as during arguments with her parents and friends. Over the course of this module, it became clear that Marla was very reluctant to acknowledge or express her emotions, particularly feelings of frustration to her parents. This pattern was identified as an emotional avoidance strategy and she was asked to become more aware of her feelings related to the conflict with her parents. This skill seemed to be particularly important for Marla, as she was able to identify that her whole body pain became worse when she had an argument with her parents. The conceptualization of emotional avoidance and its contribution to pain is a unique and specific goal of the transdiagnostic approach inherent in the UP-YP. Whereas traditional CBT protocols, or protocols addressing pain and anxiety, may identify specific behavioral targets of change (i.e., exposures), the UP-YP focuses on identifying and modifying potentially any situation where the individual is attempting to control, avoid, or escape from emotions.
The skills of the third module (Flexibility in Thinking) were less helpful for Marla. She identified a core thought related to her experience of pain (i.e., “I'll never be allowed to leave my parents’ house if I have chronic pain”), as well as a core depressive thought (e.g., “No one understands me”). Both these thoughts were identified as “thinking traps.” Treatment sessions in this module aimed to address her core beliefs by considering alternative interpretations. For example, Marla's parents had become quite anxious about the possibility of her experiencing significant pain when she was not at home; however, they had already agreed that she could attend band camp, as well as a summer program away from home. Yet, Marla found it difficult to integrate these examples into her belief about her parents’ desire to keep her at home.
Over the course of treatment, it became clear that a number of issues were contributing to the pain-mood relationship, and these included: (a) Marla's difficulty expressing her feelings, especially those of frustration, (b) her difficulty tolerating frustration and anger and responding appropriately, and (c) feelings of sadness and hopelessness triggered by pain that she attempted to avoid by withdrawing from social situations and activities. Contrary to what may be typically addressed in traditional CBT protocols for pain, the UP-YP identified these three issues as primary targets of change because they directly stemmed from Marla's attempts to avoid uncomfortable emotions. As a result, emotion exposures during the fourth module were focused on having Marla acknowledge and express her feelings to others, not avoid situations when she felt angry, and allowing herself to feel sad when she was in pain without withdrawing. Because Marla very much enjoyed writing poetry, this was identified as an exposure to help her begin to approach uncomfortable feelings. She was asked to write poetry every week, and she would bring in her poetry and writing samples to read aloud during session. As a result, Marla was also confronting her fears of expressing her emotions to others. She reported that she very much enjoyed these exposures afterward, and she felt more connected to the therapist.
At this point, Marla was able to disclose that she did not fully trust any of her treatment providers, and she acknowledged that she was not willing to openly disclose her more private thoughts and feelings in session. Even though this was identified as an emotional avoidance strategy, Marla was unwavering in her decision not to reveal certain aspects of herself in session. Despite repeatedly connecting these patterns to Marla's overall emotional difficulties with depression and loneliness, Marla stated that she was only willing to address certain topics in session, such as the relationship with her parents and activities with friends. Sessions then focused on exposing Marla to the emotion of frustration, often triggered by her parents, and not immediately “blowing up” and leaving an argument. Marla reported on several occasions that she was able to “talk things through” with her parents, which improved their relationship to some degree. Finally, Marla was encouraged to become more involved in the activities that she was avoiding because of feeling sad about her pain. She initially spent more time with friends and practicing for band; however, she found it difficult to maintain her commitment to these activities if her pain level was high. The rationale for emotion exposure was revisited, but Marla reported that feelings of hopelessness became very strong and she did not continue to engage in these activities when she did not feel well physically.
Near the end of treatment, Marla was diagnosed with pneumonia and her pain levels, as well as depression, increased dramatically. She reported that she wanted to terminate therapy at that time, although she did agree to attend a total of 12 treatment sessions, including a termination session. During the termination session, her progress was reviewed and the relationship between her mood, activity level, and pain was discussed. Despite the relatively clear evidence that her ability to tolerate and experience uncomfortable emotions was associated with better mood and improved functioning, Marla was not able to use this information to motivate a change in her behavior.
Even though it was expected that Marla's parents would participate in treatment, Marla expressed at the outset of the sessions that she did not want her parents involved at all. However, she was willing to compromise to some degree and agreed to have her parents meet with the therapist and herself for 5 minutes at the end of each session.
Marla's case clearly illustrates the potential value of the transdiagnostic conceptualization in the UP-YP. Her physical complaints and experience of pain was correlated with her tendency to experience strong emotions (i.e., frustration, sadness) and attempts to avoid them by withdrawing from friends and family. Marla's pain symptoms were initially being addressed as she began to explore and become more aware of her emotions, although her physical illness toward the end of treatment precluded her from the potential benefits of this continued practice.
Results
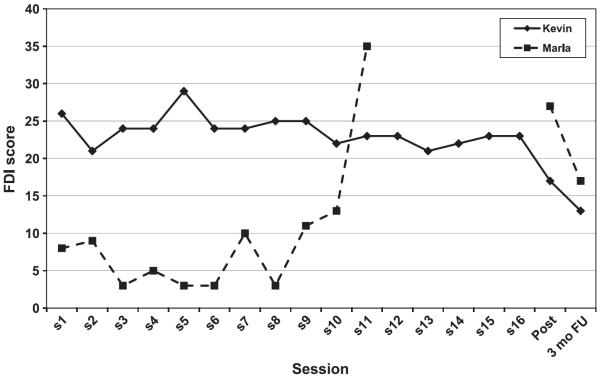
Over the course of treatment, Kevin demonstrated improvement in various domains of functioning. As shown in Fig. 1, levels of functional disability fluctuated somewhat, although showed a decline on average across treatment. Kevin's self-reported symptoms of anxiety, as measured by the RCADS total anxiety and depression subscale and social anxiety subscale also improved from pretreatment to posttreatment. Emotional awareness and expression increased, while somatization decreased. Notably, these changes were made while Kevin's current levels of pain remained identical to pretreatment (see Table 1).
Figure 1.
Levels of functional disability for Kevin and Marla across treatment and follow-up, as measured by the Functional Disability Inventory (higher scores indicating greater disability).
Table 1.
Kevin and Marla's Self-Report Measures of Anxiety and Depression, Emotion Regulation, Somatization, and Pain at Pretreatment, Posttreatment, and 3-Month Follow-up
| Measure | Pre | Post | Follow-up | |
|---|---|---|---|---|
| Kevin | RCADS (total anxiety and depression) | 34 (t=49) | 31 (t=47) | 17 (t=38) |
| RCADS (social anxiety subscale) | 19 (t=67) | 17 (t=63) | 14 (t=56) | |
| EESC (poor awareness) | 23 | 18 | 14 | |
| EESC (expressive reluctance) | 26 | 22 | 18 | |
| CSI (total) | 18 | 12 | 9 | |
| FPS-R (current pain) | 8 | 8 | 6 | |
| Marla | RCADS (total anxiety and depression) | 55 (t=56) | 44 (t=50) | 37 (t=46) |
| RCADS (depression subscale) | 16 (t=65) | 16 (t=65) | 13 (t=58) | |
| EESC (poor awareness) | 16 | 22 | 14 | |
| EESC (expressive reluctance) | 31 | 36 | 28 | |
| CSI (total) | 16 | 32 | 18 | |
| FPS-R (current pain) | 0 | 6 | 2 |
Note: RCADS = Revised Child Anxiety and Depression Scale (t scores of 65 and above suggest clinically significant symptoms); EESC = Emotion Expression Scale for Children (higher scores indicate greater emotion regulation deficits); CSI = Children's Somatization Inventory (higher scores indicate increased somatization); FPS-R = Faces Pain Scale – Revised (higher scores indicate greater pain).
Perhaps the most significant improvements occurred for Kevin over the course of the 3-month follow-up. During this time, there was clearly a dramatic improvement in anxiety, emotional awareness and expression, and somatization. At follow-up, Kevin rated his current pain level at a 6 on the FPS-R (see Table 1), which is the lowest he had ever rated his pain at any point during the study.
For Marla, improvement in functional disability, pain, and depression was less clear. Although she initially appeared to show reduced disability, by the end of treatment her levels of functional disability were at their highest (Fig. 1)—likely due to her physical illness and increased pain levels at the time. Other measures of emotion regulation, somatization, and pain also increased from pre- to posttreatment, although levels of depression remained the same. However, Marla also demonstrated improvement on all measures across follow-up, suggesting that she may have been able to implement some of the skills she learned after treatment ended. Her parents also reported a notable change in her overall mood and irritability at follow-up; however, this may have not been captured by the self-report measures.
Discussion
These cases illustrate the use of a single, transdiagnostic cognitive-behavioral treatment protocol that targets both emotion- and pain-related dysfunction in adolescents. Based on a transdiagnostic protocol for adolescents with emotional disorders (Ehrenreich-May et al., 2008), the UP-YP extends the principles of emotion regulation and behavior change to chronic pain—a complex biopsychosocial condition that is highly comorbid with emotional disorders. Treatment strategies in the UP-YP addressed Kevin's chronic daily head pain and symptoms of social anxiety and Marla's fibromyalgia, IBS, and depression through psychoeducation, training in emotional awareness, increasing cognitive flexibility, and emotion and pain exposures. Although some of the actual strategies used in session are similar or even identical to those seen in traditional CBT protocols, the value of the UP-YP is in its conceptualization of the mechanisms of successful treatment. Kevin's improvement across the measures of anxiety, emotion regulation, somatization, pain, and functional disability suggest the potential utility of an emotion regulation-based intervention that specifically includes emotion identification and awareness for chronic pain and emotional symptoms. Marla's symptoms of pain and depression also support the transdiagnostic conceptualization as it became clear that the primary difficulties she experienced were identifying and expressing her uncomfortable emotions. Even though her symptoms worsened at posttreatment, this may be explained by the physical illness she had at that time, or it may suggest that the UP-YP is less helpful for whole body pain (fibromyalgia) or depression or both. Although results cannot be generalized to the larger population of adolescents with chronic pain and emotional disorders based on these data, future randomized controlled trials can explore the efficacy of the UP-YP in larger and more diagnostically diverse samples.
There may be several potential mechanisms by which the UP-YP is able to address a broad range of symptoms. It is possible that the strategies used target common, underlying processes contributing to both pain and emotional dysfunction. Another possibility is that teaching a core set of skills allows a client to apply those skills to each disorder individually. However, regardless of the mechanism, these cases suggest that broadening the scope of applicability of emotion regulation skills and cognitive-behavioral treatment strategies may be both feasible and helpful for individuals with complex medical and psychological conditions.
Acknowledgments
This study was supported by 1F32MH084424 awarded by the National Institute of Mental Health (PI: Laura B. Allen), 2R01DE012754, awarded by the National Institute of Dental and Craniofacial Research (PI: Lonnie K. Zeltzer), and 1R01MH063779, awarded by the National Institute of Mental Health (PI: Margaret C. Jacob).
Footnotes
Details about the cases in this article have been modified to protect the identities of the clients.
Contributor Information
Laura B. Allen, Pediatric Pain Program, David Geffen School of Medicine at UCLA
Jennie C.I. Tsao, Pediatric Pain Program, David Geffen School of Medicine at UCLA
Laura C. Seidman, Pediatric Pain Program, David Geffen School of Medicine at UCLA
Jill Ehrenreich-May, University of Miami.
Lonnie K. Zeltzer, Pediatric Pain Program, David Geffen School of Medicine at UCLA
References
- Allen LB, Ehrenreich JT, Barlow DH. A unified treatment for emotional disorders: Applications with adults and adolescents. Japanese Journal of Behavior Therapy. 2005;31:3–31. [Google Scholar]
- Allen LB, Tsao JCI, Zeltzer LK, Ehrenreich-May JT, Barlow DH. Unified Protocol for Treatment of Emotions in Youth with Pain (UP-YP) Pediatric Pain Program, UCLA; 2010. [Google Scholar]
- Barrett PM, Rapee RM, Dadds MM, Ryan SM. Family enhancement of cognitive style in anxious and aggressive children. Journal of Abnormal Child Psychology. 1996;24:187–203. doi: 10.1007/BF01441484. [DOI] [PubMed] [Google Scholar]
- Campo JV, Bridge J, Ehmann M, Altman S, Lucas A, Birmaher B, et al. Recurrent abdominal pain, anxiety, and depression in primary care. Pediatrics. 2004;113(4):817–824. doi: 10.1542/peds.113.4.817. [DOI] [PubMed] [Google Scholar]
- Campo JV, Comer DM, Jansen-Mcwilliams L, Gardner W, Kelleher KJ. Recurrent pain, emotional distress, and health service use in childhood. Journal of Pediatrics. 2002;141(1):76–83. doi: 10.1067/mpd.2002.125491. [DOI] [PubMed] [Google Scholar]
- Campo JV, Perel J, Lucas A, Bridge J, Ehmann M, Kalas C, et al. Citalopram treatment of pediatric recurrent abdominal pain and comorbid internalizing disorders: An exploratory study. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:1234–1242. doi: 10.1097/01.chi.0000136563.31709.b0. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Moffitt CE, Gray J. Psychometric properties of the Revised Child Anxiety and Depression Scale in a clinical sample. Behaviour Research and Therapy. 2005;43:309–322. doi: 10.1016/j.brat.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Yim L, Moffitt C, Umemoto LA, Francis SE. Assessment of symptoms of DSM-IV anxiety and depression in children: A Revised Child Anxiety and Depression Scale. Behaviour Research and Therapy. 2000;38:835–855. doi: 10.1016/s0005-7967(99)00130-8. [DOI] [PubMed] [Google Scholar]
- Cioffi D, Holloway J. Delayed costs of suppressed pain. Journal of Personality and Social Psychology. 1993;64:274–282. doi: 10.1037//0022-3514.64.2.274. [DOI] [PubMed] [Google Scholar]
- Claar RL, Walker LS. Functional assessment of pediatric pain patients: Psychometric properties of the functional disability inventory. Pain. 2006;121(1–2):77–84. doi: 10.1016/j.pain.2005.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorn LD, Campo JC, Thato S, Dahl RE, Lewin D, Chandra R, Di Lorenzo C. Psychological comorbidity and stress reactivity in children and adolescents with recurrent abdominal pain and anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:66–75. doi: 10.1097/00004583-200301000-00012. [DOI] [PubMed] [Google Scholar]
- Eccleston C, Morley S, Williams A, Yorke L, Mastroyannopoulou K. Systematic review of randomised controlled trials of psychological therapy for chronic pain in children and adolescents, with a subset meta-analysis of pain relief. Pain. 2002;99(1–2):157–165. doi: 10.1016/s0304-3959(02)00072-6. [DOI] [PubMed] [Google Scholar]
- Eccleston C, Palermo TM, Williams AC, Lewandowski A, Morley S. Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Systematic Reviews. 2009;(2) doi: 10.1002/14651858.CD003968.pub2. CD003968. [DOI] [PubMed] [Google Scholar]
- Ehrenreich-May J, Bilek EL. The development of a transdiagnostic, cognitive behavioral group intervention for childhood anxiety disorders and co-occurring depression symptoms. Cognitive and Behavioral Practice. 2012;19:41–55. (this issue) [Google Scholar]
- Ehrenreich-May JT, Buzzella BA, Trosper SE, Bennett SM, Wright LR, Barlow DH. Unpublished treatment manual. Boston University; 2008. Unified Protocol for the Treatment of Emotional Disorders in Youth (UP-Y) [Google Scholar]
- Ehrenreich JT, Goldstein CM, Wright LR, Barlow DH. Development of a Unified Protocol for the Treatment of Emotional Disorders in Youth. Child and Family Behavior Therapy. 2009;31:20–37. doi: 10.1080/07317100802701228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellard KK, Fairholme CP, Boisseau CL, Farchione TJ, Barlow DH. Unified Protocol for the Transdiagnostic Treatment of Emotional Disorders: Protocol development and initial outcome data. Cognitive and Behavioral Practice. 2010;17:88–101. doi: 10.1016/j.cbpra.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gatchel R, Peng Y, Peters M, Fuchs P, Turk D. The biopsychosocial approach to chronic pain: Scientific advances and future directions. Psychological Bulletin. 2007;133:581–624. doi: 10.1037/0033-2909.133.4.581. [DOI] [PubMed] [Google Scholar]
- Ghanizadeh A, Moaiedy F, Imanieh MH, Askani H, Haghighat M, Dehbozorgi G, et al. Psychiatric disorders and family functioning in children and adolescents with functional abdominal pain syndrome. Journal of Gastroenterology and Hepatology. 2007 doi: 10.1111/j.1440-1746.2007.05224.x. [DOI] [PubMed] [Google Scholar]
- Gross JJ. Emotion regulation: Affective, cognitive, and social consequences. Psychophysiology. 2002;39:281–291. doi: 10.1017/s0048577201393198. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and Commitment Therapy: An experiential approach to behavior change. Guilford Press; New York: 1999. [Google Scholar]
- Hicks CL, von Baeyer CL, Spafford PA, van Korlaar I, Goodenough B. The Faces Pain Scale-Revised: Toward a common metric in pediatric pain measurement. Pain. 2001;93:173–183. doi: 10.1016/S0304-3959(01)00314-1. [DOI] [PubMed] [Google Scholar]
- Jensen MP, Nielson WR, Kerns RD. Toward the development of a motivational model of pain self-management. Journal of Pain. 2003;4:477–492. doi: 10.1016/s1526-5900(03)00779-x. [DOI] [PubMed] [Google Scholar]
- Kashikar-Zuck S, Parkins IS, Ting TV, Verkamp E, Lynch-Jordan A, Passo M, Graham TB. Controlled follow-up study of physical and psychosocial functioning of adolescents with juvenile primary fibromyalgia syndrome. Rheumatology. 2010;49:2204–2209. doi: 10.1093/rheumatology/keq254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keefe FJ, Lumley M, Anderson T, Lynch T, Studts JL, Carson KL. Pain and emotion: New research directions. Journal of Clinical Psychology. 2001;57:587–607. doi: 10.1002/jclp.1030. [DOI] [PubMed] [Google Scholar]
- Kendall PC. Coping cat workbook. Workbook Publishing; Ardmore, PA: 1992. [Google Scholar]
- Lipsitz JD, Masia C, Apfel H, Marans Z, Gur M, Dent H, et al. Noncardiac chest pain and psychopathology in children and adolescents. Journal of Psychosomatic Research. 2005;59:185–188. doi: 10.1016/j.jpsychores.2005.05.004. [DOI] [PubMed] [Google Scholar]
- Lumley MA, Beyer J, Radcliffe A. Alexithymia and physical health problems: A critique of potential pathways and a research agenda. In: Vingerhoets A, Nyklicek I, Denollet J, editors. Emotion regulation: Conceptual and clinical issues. Springer; New York: 2008. pp. 43–68. [Google Scholar]
- Masia Warner C, Reigada LC, Fisher PH, Saborsky AL, Benkov KJ. CBT for anxiety and associated somatic complaints in pediatric medical settings: An open pilot study. Journal of Clinical Psychology in Medical Settings. 2009;16:169–177. doi: 10.1007/s10880-008-9143-6. [DOI] [PubMed] [Google Scholar]
- Mattila AK, Kronholm E, Jula A, Salminen JK, Koivisto AM, Mielonen RL, Joukamaa M. Alexithymia and somatization in general population. Psychosomatic Medicine. 2008;70:716–722. doi: 10.1097/PSY.0b013e31816ffc39. [DOI] [PubMed] [Google Scholar]
- McGrath PA, Speechley KN, Seifert CE, Biehn JT, Cairney AE, Gorodzinsky FP, Morrissy JR. A survey of children's acute, recurrent, and chronic pain: Validation of the pain experience interview. Pain. 2000;87:59–73. doi: 10.1016/S0304-3959(00)00273-6. [DOI] [PubMed] [Google Scholar]
- Merlijn VP, Hunfeld JA, van der Wouden JC, Hazebroek-Kampschreur AA, van Suijlekom-Smit LW, Koes BW, Passchier J. A cognitive-behavioural program for adolescents with chronic pain: A pilot study. Patient Education and Counseling. 2005;59:126–134. doi: 10.1016/j.pec.2004.10.010. [DOI] [PubMed] [Google Scholar]
- Palermo TM, Eccleston C, Lewandowski AS, Williams AC, Morley S. Randomized controlled trials of psychological therapies for management of chronic pain in children and adolescents: An updated meta-analytic review. Pain. 2010;148:387–397. doi: 10.1016/j.pain.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penza-Clyve S, Zeman J. Initial validation of the Emotion Expression Scale for Children (EESC) Journal of Clinical Child and Adolescent Psychology. 2002;31:540–547. doi: 10.1207/S15374424JCCP3104_12. [DOI] [PubMed] [Google Scholar]
- Ramchandani PG, Fazel M, Stein A, Wiles N, Hotopf M. The impact of recurrent abdominal pain: Predictors of outcome in a large population cohort. Acta Paediatrica. 2007;96:697–701. doi: 10.1111/j.1651-2227.2007.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reigada LC, Fisher PH, Cutler C, Masia Warner C. An innovative treatment approach for children With anxiety disorders and medically unexplained somatic complaints. Cognitive and Behavioral Practice. 2008;15:140–147. doi: 10.1016/j.cbpra.2007.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribeiro SC, Kennedy SE, Smith YR, Stohler CS, Zubieta JK. Interface of physical and emotional stress regulation through the endogenous opioid system and mu-opioid receptors. Progress in Neuro-psychopharmacology and Biological Psychiatry. 2005;29:1264–1280. doi: 10.1016/j.pnpbp.2005.08.011. [DOI] [PubMed] [Google Scholar]
- Schanberg LE, Anthony KK, Gil KM, Lefebvre JC, Kredich DW, Macharoni LM. Family pain history predicts child health status in children with chronic rheumatic disease. Pediatrics. 2001;108:E47. doi: 10.1542/peds.108.3.e47. [DOI] [PubMed] [Google Scholar]
- Smith JP, Smith GC. Long-term economic costs of psychological problems during childhood. Social Science & Medicine. 2010;71:110–115. doi: 10.1016/j.socscimed.2010.02.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spence SH. Structure of anxiety symptoms among children: A confirmatory factor-analytic study. Journal of Abnormal Psychology. 1997;106:280–297. doi: 10.1037//0021-843x.106.2.280. [DOI] [PubMed] [Google Scholar]
- Spence SH. A measure of anxiety symptoms among children. Behaviour Research and Therapy. 1998;36:545–566. doi: 10.1016/s0005-7967(98)00034-5. [DOI] [PubMed] [Google Scholar]
- Strigo IA, Simmons AN, Matthews SC, Craig AD, Paulus MP. Major depressive disorder is associated with altered functional brain response during anticipation and processing of heat pain. Archives of General Psychiatry. 2008;65:1275–1284. doi: 10.1001/archpsyc.65.11.1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan MJL, Rouse D, Bishop S, Johnston S. Thought suppression, catastrophizing, and pain. Cognitive Therapy and Research. 1997;21:555–568. [Google Scholar]
- Tsao JC, Myers CD, Craske MG, Bursch B, Kim SC, Zeltzer LK. Role of anticipatory anxiety and anxiety sensitivity in children's and adolescents' laboratory pain responses. Journal of Pediatric Psychology. 2004;29:379–388. doi: 10.1093/jpepsy/jsh041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuzer V, Dogan Bulut S, Bastug B, Kayalar G, Göka E, Bestepe E. Causal attributions and alexithymia in female patients with fibromyalgia or chronic low back pain. Nordic Journal of Psychiatry. 2010;65 doi: 10.3109/08039488.2010.522596. [DOI] [PubMed] [Google Scholar]
- van Middendorp H, Lumley MA, Jacobs JW, van Doornen LJ, Bijlsma JW, Geenen R. Emotions and emotional approach and avoidance strategies in fibromyalgia. Journal of Psychosomatic Research. 2008;64:159–167. doi: 10.1016/j.jpsychores.2007.08.009. [DOI] [PubMed] [Google Scholar]
- Walker LS, Dengler-Crish CM, Rippel S, Bruehl S. Functional abdominal pain in childhood and adolescence increases risk for chronic pain in adulthood. Pain. 2010;150:568–572. doi: 10.1016/j.pain.2010.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker LS, Garber J. Manual for the Children's Somatization Inventory. Department of Pediatrics, Vanderbilt University School of Medicine; Nashville: 2003. [Google Scholar]
- Walker LS, Garber J, Greene JW. Psychosocial correlates of recurrent childhood pain: A comparison of pediatric patients with recurrent abdominal pain, organic illness, and psychiatric disorders. Journal of Abnormal Psychology. 1993;102:248–258. doi: 10.1037//0021-843x.102.2.248. [DOI] [PubMed] [Google Scholar]
- Walker LS, Garber J, Van Slyke DA, Greene JW. Long-term health outcomes in patients with recurrent abdominal pain. Journal of Pediatric Psychology. 1995;20:233–245. doi: 10.1093/jpepsy/20.2.233. [DOI] [PubMed] [Google Scholar]
- Walker LS, Greene JW. The Functional Disability Inventory: Measuring a neglected dimension of child health status. Journal of Pediatric Psychology. 1991;16:39–58. doi: 10.1093/jpepsy/16.1.39. [DOI] [PubMed] [Google Scholar]
- Wicksell RK, Melin L, Lekander M, Olsson GL. Evaluating the effectiveness of exposure and acceptance strategies to improve functioning and quality of life in longstanding pediatric pain - A randomized controlled trial. Pain. 2009;141:248–257. doi: 10.1016/j.pain.2008.11.006. [DOI] [PubMed] [Google Scholar]
- Zeman J, Cassano M, Perry-Parrish C, Stegall S. Emotion regulation in children and adolescents. Journal of Developmental and Behavioral Pediatrics. 2006;27:155–168. doi: 10.1097/00004703-200604000-00014. [DOI] [PubMed] [Google Scholar]