Abstract
Introduction
Low-income populations have elevated exposure to early life risk factors for obesity, but are understudied in longitudinal research. Our objective was to assess the utility of a cohort derived from electronic health record data from safety net clinics for investigation of obesity emerging in early life.
Methods
We examined data from the PCORNet ADVANCE Clinical Data Research Network, a national network of Federally-Qualified Health Centers serving >1.7 million safety net patients across the US. This cohort includes patients who, in 2012–2014, had ≥1 valid Body Mass Index measure when they were 0–5 years of age. We characterized the cohort with respect to factors required for early life obesity research in vulnerable subgroups: sociodemographic diversity, weight status based on World Health Organization (<2 years) or Centers for Disease Control (≥2 years) growth curves, and data longitudinality.
Results
The cohort includes 216,473 children and is racially/ethnically diverse (e.g., 17.9% Black, 45.4% Hispanic). A majority (56.9%) had family incomes below the Federal Poverty Level (FPL); 32% were <50% of FPL. Among children <2 years, 7.6% and 5.3% had high and low weight-for-length, respectively. Among children 2–5 years, 15.0%, 12.7%, and 2.4% were overweight, obese, and severely obese, respectively; 5.3% were underweight. In the study period, 79.1% of children had ≥2 BMI measures. Among 4–5 year olds, 21.9% had >1 BMI measure when they were <2 years.
Discussion
The ADVANCE Early Life cohort offers unique opportunities to investigate early life determinants of obesity in the understudied population of low income and minority children.
Keywords: Obesity, Socioeconomic factors, infant, child, longitudinal
INTRODUCTION
Early life is a critical period in the etiology of obesity and chronic disease (Perez-Escamilla & Kac, 2013). Low-income and racial/ethnic minority children have a high prevalence of adverse prenatal exposures (Taveras, Gillman, Kleinman, Rich-Edwards, & Rifas-Shiman, 2013) and elevated risk of obesity and disease later in life (Rossen & Schoendorf, 2012). Socioeconomically disadvantaged children are among the most vulnerable, yet most understudied populations.
Studying prenatal and early childhood influences on obesity-related health in vulnerable populations presents several challenges. First, recruitment of large numbers of low-income and racial/ethnic minority participants is challenging due to social and economic barriers to study participation (Yancey, Ortega, & Kumanyika, 2006). Second, obesity research requires objectively measured body weight, stature, and clinical outcomes. Third, extensive follow-up is needed to study impacts of early life on health outcomes that develop over long periods.
Electronic health records (EHRs) address these barriers by providing longitudinal clinical data on large populations. Yet the handful of existing EHR-based perinatal and pediatric research datasets (Hillier et al., 2008; Koebnick et al., 2012; Vesco et al., 2011) are comprised predominately of insured health system members, and thus underrepresent socioeconomically disadvantaged populations. The growth of EHR data from community health centers serving safety net (publicly insured and uninsured) patients (DeVoe et al., 2014) thus has great potential for enhancing early life obesity research in socially vulnerable children.
Using retrospective EHR data from safety net clinics, we constructed the Accelerating Data Value Across a National Community Health Center Network (ADVANCE) Early Life Cohort, a cohort of >200,000 low-income children 0–5 years of age from all regions of the U.S. The objective of this paper is to evaluate the utility of our cohort for studying early life determinants of obesity in vulnerable children. Specifically, we characterized the cohort with respect to key factors required for early life obesity research: sociodemographic diversity, obesity burden, and availability of longitudinal data.
METHODS
Study population
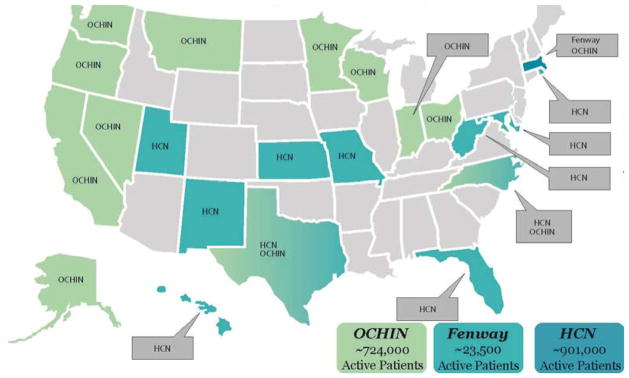
ADVANCE is a multi-center collaborative led by the OCHIN, Inc. (not an acronym) health information network in partnership with Health Choice Network (HCN) and Fenway Health. The ADVANCE data warehouse has been described previously (DeVoe et al., 2014). Briefly, these systems have outpatient clinical data from >100 Federally-Qualified Health Center (FQHC) health systems with 974 clinics serving >2 million safety net patients in 22 states (Figure 1). OCHIN and HCN networks provide EHR data infrastructure and technical support that is not typically feasible for a single community health center. ADVANCE includes pediatric and adult OCHIN, HCN, and Fenway patients with at least 1 office visit on or after 1/1/2012. Patients are added to the study population as the ADVANCE data warehouse is refreshed with EHR data on a quarterly basis.
Figure 1.
Geographic distribution of ADVANCE clinics
As of September 2013
The ADVANCE Early Life Cohort contains ADVANCE patients who, between 1/1/2012 and 12/31/2014 (at the time of data analysis in 2015), had at least one valid BMI measure when they were 0–5 years of age. Fenway Health’s pediatric population is small (<1% are <18 years) and therefore excluded. This research was approved by the Western Institutional Review Board.
Data source
We examined outpatient EHR data from the OCHIN and HCN networks. The OCHIN EHR database contains information from the Epic practice management system (e.g., billing and appointments) as well as demographic, utilization, and clinical data from the full Epic EHR (DeVoe et al., 2014). The HCN EHR database contains information from a hosted and centralized EHR platform (Intergy by Greenway Health) and supported by network-wide clinical informatics and analytic tools. Among patients in the ADVANCE Early Life cohort, we extracted EHR data collected at clinical encounters from as early as 1/1/2005 through 12/31/2014. Availability of historical data reflects the dates of EHR implementation by each clinic, which began as early as 2003, although in general EHR implementation occurred earlier for OCHIN clinics than HCN clinics.
Study variables
Body Mass Index (BMI) and weight-for-length percentiles
Body weight and concurrently measured length or height were ascertained from clinical encounter records. Length and height are recorded in a single field and assumed to represent length for children <24 months, and height for children ≥24 months.
Among encounters at which the child was <24 months of age, weight-for-length (WFL) was calculated and converted to age- and sex-specific WFL percentiles relative to the World Health Organization (WHO) standard growth curve (WHO, 2006). Low and high WFL were defined as <2.3rd and >97.7th percentiles, respectively, which are comparable to the CDC 5th and 95th percentiles (Grummer-Strawn, Reinold, & Krebs, 2010).
Among encounters at which the child was ≥24 months of age, BMI was calculated and converted to age- and sex-specific BMI percentiles using the CDC 2000 growth curves (Kuczmarski et al., 2002). BMI percentiles were classified into underweight (<5th percentile), normal weight (5th to <85th), overweight (85th to <95th), obese (95th to <20% higher than the 95th percentile), and severe obese (≥20% higher than the 95th percentile) (Flegal et al., 2009).
Valid WFL and BMI measures were limited to biologically plausible measures (CDC or WHO growth curve z-score <−4 or >5) (Centers for Disease Control and Prevention, 2015). We used each child’s most recent valid WFL or BMI measure within the 2012–2014 study period; hereafter, the “index encounter.”
Sociodemographic characteristics
Patient-level sociodemographics were ascertained from the patient table: sex (male, female), date of birth, race/ethnicity (non-Hispanic white, African American, Asian, Native Hawaiian/Pacific Islander, other/unknown; or Hispanic of any race), and primary language spoken at home (English, Spanish, other) are reported by the patient and recorded by clinical staff. Date of birth was used to calculate age at each encounter.
Standard workflows stipulate that payer (uninsured, Medicaid, commercial, other public non-portable coverage), income as a percent of the Federal Poverty Level (FPL; calculated from household income and household size) and residential address are confirmed with the patient and updated routinely (approximately semi-annually) by clinic staff. We report the most recently reported payer and FPL among encounters in 2012–2014 and U.S. Census-defined regions (Northeast, Midwest, South, West) based on the most recently reported state of residence.
Statistical analysis
To evaluate key factors required for early life obesity research, we conducted descriptive analysis on availability of BMI measures, sociodemographic characteristics, weight status, and longitudinal follow-up of the cohort. Given the large sample size, we focused on the magnitude of group differences rather than statistical significance. We calculated prevalence of each weight status category, stratified by age group (<2 and 2–5 years) to account for the differences in reference curves and weight status definitions. To evaluate potential bias resulting from the transient nature of the safety net population, we assessed the degree to which those with longer follow-up differed with respect to sociodemographic characteristics and BMI.
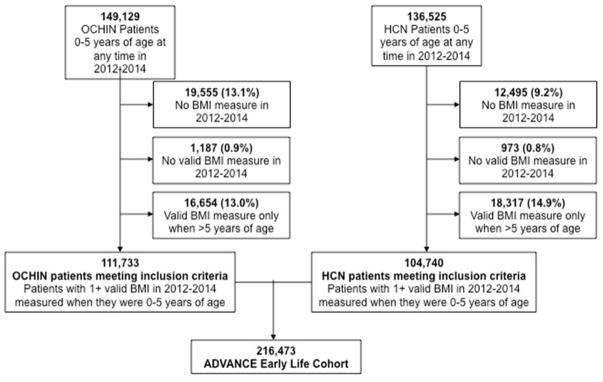
RESULTS
The ADVANCE Early Life Cohort had 216,473 children who had at least one valid BMI recorded at encounters between 1/1/2012 and 12/31/2014 when they were 0–5 years of age (Figure 2). Among the 149,129 OCHIN patients who met the age criterion, 19,555 (13.1%) were excluded because they did not have a BMI measure during this period. Among those remaining, 1,187 (0.9%) had invalid BMI measures, and an additional 16,654 had valid BMI measures only when they were >5 years of age. Similar exclusions were observed in HCN patients.
Figure 2.
Identification of the ADVANCE Early Life Cohort
Among patients who met the age criterion (n=285,654), those excluded from the cohort due to missing (n=32,050) or invalid (n=2,160) BMI measures in 2012–2014 (n=34,971; versus included, n=216,473) have a higher prevalence of uninsurance and missing data on other variables (race/ethnicity, income) (Appendix, Table S1). Those excluded due to age restrictions are similar to the final cohort, except for characteristics linked to age, including Medicaid eligibility and BMI z-score and classification.
Sociodemographic and geographic diversity
The cohort is 49.1% female and 33.3% are <2 years of age (Table 1). Hispanics are the largest racial/ethnic group (45.4%), followed by non-Hispanic white (29.2%) and Black (17.9%). Only 7.6% of cohort families have incomes >200% of FPL, with 56.9% <100% of FPL (compared to 24% nationally (CDC, 2014)) and 32.0% <50% of FPL. Another 23% have missing or invalid income data. Most children (67.8%) had primary Medicaid coverage at their most recent encounter. About one-fourth (26.5%) have EHR documentation that Spanish is the primary language spoken at home. Children reside predominantly in the West and South regions, corresponding to the central locations of OCHIN and HCN, respectively.
Table 1.
Sociodemographic characteristics of the ADVANCE Early Life Cohort (n=216,473)a
| Count | Percent | |
|---|---|---|
| Sex | ||
| Male | 110,154 | 50.9 |
| Female | 106,319 | 49.1 |
| Age | ||
| 0–<6 months | 24,282 | 11.2 |
| 6 to <12 months | 16,061 | 7.4 |
| 12 to <24 months | 31,873 | 14.7 |
| 2 to <4 years | 53,269 | 24.6 |
| 4 to <6 years | 90,988 | 42.0 |
| Race-Ethnicity | ||
| Asian | 5,451 | 2.5 |
| Native Hawaiian/Pacific Islander | 1,347 | 0.6 |
| Black or African American | 38,838 | 17.9 |
| White | 63,287 | 29.2 |
| Other/Unknown | 9,347 | 4.3 |
| Hispanic | 98,203 | 45.4 |
| Income as percent of FPLb | ||
| 0–50% | 69,345 | 32.0 |
| >50–100% | 53,969 | 24.9 |
| >100–138% | 17,398 | 8.0 |
| >138–200% | 9,628 | 4.4 |
| >200% | 16,368 | 7.6 |
| Missing or invalid | 49,765 | 23.0 |
| Insurance statusc | ||
| Uninsured | 25,040 | 11.6 |
| Medicaid | 146,810 | 67.8 |
| Commercial | 27,710 | 12.8 |
| Other public non-portable coverage | 16,913 | 7.8 |
| Missing | 401 | 0.2 |
| Language | ||
| English | 150,747 | 69.6 |
| Spanish | 57,280 | 26.5 |
| Other | 7,171 | 3.3 |
| Missing | 1,275 | 0.6 |
| Region | ||
| Northeast | 10,642 | 4.9 |
| Midwest | 21,457 | 9.9 |
| South | 82,792 | 38.2 |
| West | 101,424 | 46.9 |
| Missing | 158 | 0.1 |
OCHIN and HCN patients who, between 1/1/2012 and 12/31/2014, had at least one valid BMI measure when they were 0–5 years of age, regardless of weight status
Last known FPL.
At most recent visit
HCN, Health Choice Network; FPL, Federal Poverty Level
Weight status
Among children <2 years, 7.6% had high WFL (Table 2a). Among children 2–5 years, 15.0%, 12.7%, and 2.4% were overweight, obese, and severely obese, respectively (Table 2b). Prevalence of high WFL and overweight/obesity was slightly higher in boys than in girls; and higher in Blacks and Native Hawaiian/Pacific Islanders, older children, and those with lower income (Tables 2a–b). Overweight/obesity prevalence was higher in the Northeast region, and higher in OCHIN (32.0%) than HCN (28.1%) (Table 2b). Severe obesity was highest in 4–5 year old children (3.1%), Hispanics (3.2%), and Native Hawaiian/Pacific Islanders (3.0%). Subgroup differences in obesity prevalence were generally reflected in higher mean WFL and BMI z-scores (Tables 2a–b).
Table 2a.
Weight for length (WFL) classification and z-score, by sociodemographic subgroups of interest: 0 to <24 months of age [count (%)]:ADVANCE Early Life Cohorta
| WFL classification [count (%)] | WFL z-score [mean (SD)] | |||
|---|---|---|---|---|
|
| ||||
| Low weight for length | Normal weight for length | High weight for length | ||
| Total | 3,807 (5.3) | 62,916 (87.1) | 5,493 (7.6) | 0.19 (1.31) |
| Sex | ||||
| Girls | 1,804 (5.1) | 30,990 (88.0) | 2,428 (6.9) | 0.21 (1.34) |
| Boys | 2,003 (5.4) | 31,926 (86.3) | 3,065 (8.3) | 0.17 (1.28) |
| Age | ||||
| 0–<6 months | 2,860 (11.8) | 20,544 (84.6) | 878 (3.6) | −0.37 (1.36) |
| 6 to <12 months | 496 (3.1) | 14,483 (90.2) | 1,082 (6.7) | 0.25 (1.19) |
| 12 to <24 months | 451 (1.4) | 27,889 (87.5) | 3,533 (11.1) | 0.59 (1.18) |
| Race/ethnicity | ||||
| Asian | 104 (5.4) | 1,703 (89.0) | 107 (5.6) | 0.03 (1.25) |
| Native Haw/Pacific Isl | 33 (6.5) | 431 (84.5) | 46 (9.0) | 0.27 (1.37) |
| Black or African Am | 788 (6.1) | 11,082 (86.1) | 995 (7.7) | 0.15 (1.35) |
| White | 1,311 (6.0) | 19,163 (87.4) | 1,459 (6.7) | 0.08 (1.32) |
| Other/Unknown | 270 (6.9) | 3,362 (85.9) | 280 (7.2) | 0.06 (1.36) |
| Hispanic | 1,301 (4.2) | 27,175 (87.4) | 2,606 (8.4) | 0.31 (1.28) |
| Income as percent of FPLb | ||||
| 0–50% | 1,401 (5.8) | 20,994 (86.5) | 1,888 (7.8) | 0.18 (1.34) |
| >50–100% | 924 (5.4) | 14,953 (87.2) | 1,273 (7.4) | 0.18 (1.31) |
| >100–138% | 234 (4.3) | 4,846 (88.5) | 393 (7.2) | 0.20 (1.28) |
| >138–200% | 157 (5.2) | 2,653 (87.4) | 227 (7.5) | 0.16 (1.29) |
| >200% | 274 (6.3) | 3,819 (87.6) | 265 (6.1) | 0.05 (1.30) |
| Missing or invalid | 817 (4.6) | 15,651 (87.4) | 1,447 (8.1) | 0.25 (1.30) |
| Region | ||||
| Northeast | 196 (5.8) | 2,906 (86.7) | 251 (7.5) | 0.17 (1.32) |
| Midwest | 326 (4.6) | 6,026 (85.7) | 676 (9.6) | 0.34 (1.33) |
| South | 1,861 (6.9) | 23,338 (86.9) | 1,655 (6.2) | 0.02 (1.33) |
| West | 1,420 (4.1) | 30,593 (87.6) | 2,904 (8.3) | 0.29 (1.28) |
| Health system | ||||
| OCHIN | 1,335 (3.4) | 34,141 (87.8) | 3,406 (8.8) | 0.00 (1.35) |
| HCN | 2,472 (7.4) | 28,775 (86.3) | 2,087 (6.3) | 0.35 (1.25) |
Weight for length classified according to World Health Organization sex-specific growth curves. Low and high weight-for-length were defined as <2.3rd and > 97.7th percentiles, respectively
Last known FPL.
HCN, Health Choice Network; FPL, Federal Poverty Level
Table 2b.
Body Mass Index (BMI) classification and z-score (2–5 years), by sociodemographic subgroups of interest [count (%)]: ADVANCE Early Life Cohorta
| BMI classification [count (%)] | BMI z-score [mean (SD)] | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Under-weight | Normal BMI | Overweight | Obese | Severe obese | ||
| Total | 7,607 (5.3) | 93,309 (64.7) | 21,674 (15.0) | 18,270 (12.7) | 3,397 (2.4) | 0.41 (1.23) |
| Sex | ||||||
| Girls | 3,697 (5.2) | 46,315 (65.1) | 10,923 (15.4) | 8,460 (11.9) | 1,702 (2.4) | 0.39 (1.20) |
| Boys | 3,910 (5.3) | 46,994 (64.2) | 10,751 (14.7) | 9,810 (13.4) | 1,695 (2.3) | 0.42 (1.26) |
| Age | ||||||
| 2 to <4 years | 3,655 (6.9) | 35,849 (67.3) | 7,148 (13.4) | 6,038 (11.3) | 579 (1.1) | 0.25 (1.26) |
| 4 to <6 years | 3,952 (4.3) | 57,460 (63.2) | 14,526 (16.0) | 12,232 (13.4) | 2,818 (3.1) | 0.50 (1.20) |
| Race/ethnicity | ||||||
| Asian | 340 (9.6) | 2,434 (68.8) | 374 (10.6) | 331 (9.4) | 58 (1.6) | 0.08 (1.32) |
| Native Haw/Pacific Isl | 41 (4.9) | 537 (64.2) | 127 (15.2) | 107 (12.8) | 25 (3.0) | 0.45 (1.26) |
| Black or African Am | 1,837 (7.1) | 17,509 (67.4) | 3,555 (13.7) | 2,629 (10.1) | 443 (1.7) | 0.23 (1.25) |
| White | 2,468 (6.0) | 28,347 (68.5) | 5,882 (14.2) | 4,045 (9.8) | 612 (1.5) | 0.27 (1.20) |
| Other/Unknown | 325 (6.0) | 3,634 (66.9) | 746 (13.7) | 635 (11.7) | 95 (1.7) | 0.31 (1.23) |
| Hispanic | 2,596 (3.9) | 40,848 (60.9) | 10,990 (16.4) | 10,523 (15.7) | 2,164 (3.2) | 0.58 (1.22) |
| Income as percent of FPLb | ||||||
| 0–50% | 2,511 (5.6) | 29,106 (64.6) | 6,682 (14.8) | 5,695 (12.6) | 1,068 (2.4) | 0.39 (1.25) |
| >50–100% | 1,847 (5.0) | 23,389 (63.5) | 5,748 (15.6) | 4,880 (13.3) | 955 (2.6) | 0.44 (1.24) |
| >100–138% | 619 (5.2) | 7,697 (64.5) | 1,794 (15.0) | 1,528 (12.8) | 287 (2.4) | 0.42 (1.24) |
| >138–200% | 370 (5.6) | 4,293 (65.1) | 987 (15.0) | 793 (12.0) | 148 (2.2) | 0.37 (1.22) |
| >200% | 687 (5.7) | 7,962 (66.3) | 1,751 (14.6) | 1,362 (11.3) | 248 (2.1) | 0.34 (1.22) |
| Missing or invalid | 1,573 (4.9) | 20,862 (65.5) | 4,712 (14.8) | 4,012 (12.6) | 691 (2.2) | 0.41 (1.21) |
| Region | ||||||
| Northeast | 298 (4.1) | 4,382 (60.1) | 1,230 (16.9) | 1,142 (15.7) | 237 (3.3) | 0.59 (1.25) |
| Midwest | 886 (6.1) | 9,358 (64.9) | 2,173 (15.1) | 1,698 (11.8) | 314 (2.2) | 0.36 (1.24) |
| South | 3,545 (6.3) | 36,826 (65.8) | 7,745 (13.8) | 6,583 (11.8) | 1,239 (2.2) | 0.31 (1.26) |
| West | 2,874 (4.3) | 42,681 (64.2) | 10,508 (15.8) | 8,837 (13.3) | 1,607 (2.4) | 0.47 (1.20) |
| Health system | ||||||
| OCHIN | 3,038 (4.2) | 46,472 (63.8) | 11,776 (16.2) | 9,791 (13.4) | 1,774 (2.4) | 0.32 (1.27) |
| HCN | 4,569 (6.4) | 46,837 (65.6) | 9,898 (13.9) | 8,479 (11.9) | 1,623 (2.3) | 0.49 (1.19) |
BMI percentiles were classified according to Centers for Disease Control 2000 growth curves: underweight (<5th percentile), normal weight (5th to <85th), overweight (85th to <95th), obese (95th to <20% higher than the 95th percentile), and severe obese (≥20% higher than the 95th percentile).
Last known FPL.
HCN, Health Choice Network; FPL, Federal Poverty Level
Prevalence of low WFL (<2 years) and underweight (2–5 years) were both 5.3%. Low WFL and underweight prevalence varied by sociodemographic characteristics; in particular, prevalences were highest in the Southern region and within HCN.
Longitudinality of BMI data
Children in the cohort had an average of 9.7 encounters, providing an average of 4.7 valid BMI measures per child in the 2012–2014 period (Table 3). The number of valid BMI measures varied from 1 to 10 (90th percentile) or more measures per child. 79.2% of children had ≥2 valid BMI measures between 2006 and 2014, and 47.2% had ≥5 BMI measures. A higher percentage of OCHIN children had historical BMI measures prior to 2011 than HCN children (24.0% vs. 10.9; data not shown); longitudinality was otherwise similar for OCHIN and HCN.
Table 3.
Longitudinal data availability of the ADVANCE Early Life Cohorta
| Number of encounters in 2012–2014 mean number (SD) per child | 9.7 (10.1) |
| Number of valid BMI measures in 2012–2014 | |
| Mean number (SD) per child | 4.7 (4.5) |
| Median number (10%, 90%) per child | 3 (1, 10) |
| Children with 1, 2, 3–4, or ≥5 valid BMI measures per child from 2006–2014 (#/%) | |
| 1 | 45,226 (20.9%) |
| 2 | 28,519 (13.2%) |
| 3–4 | 40,601 (18.8%) |
| ≥5 | 102,127 (47.2%) |
| Children with a valid BMI measures observed in calendar year (#/%): | |
| 2011 | 54,820 (25.3%) |
| 2010 | 24,843 (11.5%) |
| 2009 | 10,215 (4.7%) |
| 2006–2008 | 3,030 (1.4%) |
OCHIN and HCN patients who, between 1/1/2012 and 12/31/2014, had at least one valid BMI measure when they were 0–5 years of age, regardless of weight status.
HCN, Health Choice Network
Availability of BMI measures collected through the child’s life span are reported in Table 4. 74.7% of infants had ≥2 valid BMI measures. Among children with a BMI measure when they were 4–5 years of age, 21.9% had ≥1 BMI measure when they were younger than 2 years; 9.8% had a BMI measure in the first six months of life.
Table 4.
BMI availability over the life spans of children in the ADVANCE Early Life Cohorta
| Age at index visitb | ||||
|---|---|---|---|---|
|
| ||||
| 0 to <12 months | 12 to <24 months | 2 to <4 years | 4 to <6 years | |
| Number of children | 40,171 | 31,901 | 53,413 | 90,988 |
| Number of valid BMI measures per child | ||||
| 1 | 10,148 (25.3%) | 5,336 (16.7%) | 11,844 (22.2%) | 17,898 (19.7%) |
| 2 | 7,284 (18.1%) | 2,869 (9.0%) | 5,822 (10.9%) | 12,544 (13.8%) |
| 3 | 6,136 (15.3%) | 2,067 (6.5%) | 3,774 (7.1%) | 10,319 (11.3%) |
| 4 | 5,186 (12.9%) | 1,869 (5.8%) | 3,019 (5.7%) | 8,231 (9.1%) |
| 5+ | 11,417 (28.4%) | 19,760 (62.0%) | 28,954 (54.2%) | 41,996 (46.2%) |
| Age at first BMI | ||||
| 0 to <6 months | 36,378 (90.6%) | 19,939 (62.5%) | 21,916 (41.0%) | 8,885 (9.8%) |
| 6 to <12 months | 3,793 (9.4%) | 3,354 (10.5%) | 3,855 (7.2%) | 2,959 (3.3%) |
| 12 to <24 months | -NA- | 8,608 (27.0%) | 7,784 (14.6%) | 8,045 (8.8%) |
| 2 to <4 years | -NA- | -NA- | 19,858 (37.2%) | 25,176 (27.7%) |
| 4 to <6 years | NA- | -NA- | -NA- | 45,923 (50.5%) |
| Children who had at least 1 valid BMI measure when child was: | ||||
| 0 to <6 months | 36,378 (90.6%) | 19,939 (62.5%) | 21,916 (41.0%) | 8,885 (9.8%) |
| 6 to <12 months | 15,872 (39.5%) | 21,849 (68.5%) | 24,058 (45.0%) | 11,056 (12.2%) |
| 12 to <24 months | -NA- | 31,901 (100.0%) | 32,063 (60.0%) | 18,989 (20.9%) |
OCHIN and HCN patients who, between 1/1/2012 and 12/31/2014, had at least one valid BMI measure when they were 0–5 years of age, regardless of weight status.
Index visit is the last visit in 2012–2014 with a valid BMI.
HCN, Health Choice Network
Among 4–5 year old children, those with available BMI measures as early as infancy, 12 to <24 months, or >2 years, were similar with respect to sex and mean BMI z-score (Table 5). Those with (vs. without) BMI measures in infancy were less likely to be Black or African American; and more likely to be Hispanic, have Medicaid, have incomes below 200% of FPL, and to be overweight at ages 4–5.
Table 5.
Comparison of children with weight status measures across key life stages, among children in the ADVANCE Early Life Cohort with BMI measured when they were 4 to <6 years of age (n=90,988)
| Earliest period with weight status measures | |||
|---|---|---|---|
|
| |||
| Infancy (0 to <12 months) | Early childhood (12 to <24 months) | 24+ months | |
| Sex | |||
| Male | 5,976 (50.5) | 4,122 (51.2) | 36,006 (50.6) |
| Female | 5,868 (49.5) | 3,923 (28.8) | 35,093 (49.4) |
| Race-Ethnicity | |||
| Asian | 277 (2.3) | 179 (2.2) | 1,695 (2.4) |
| Native Hawaiian/Pacific Islander | 106 (0.9) | 43 (0.5) | 341 (0.5) |
| Black or African American | 1,500 (12.7) | 1,409 (17.5) | 13,460 (18.9) |
| White | 2,967 (25.1) | 2,035 (25.3) | 20,484 (28.8) |
| Other/Unknown | 308 (2.6) | 201 (2.5) | 2,700 (3.8) |
| Hispanic | 6,686 (56.5) | 4,178 (51.9) | 32,419 (45.6) |
| Income as percent of FPLb | |||
| 0–50% | 3,583 (30.3) | 2,352 (29.2) | 21,814 (30.7) |
| >50–100% | 3,789 (32.0) | 2,475 (30.8) | 17,202 (24.2) |
| >100–138% | 1,567 (13.2) | 844 (10.5) | 6,446 (9.1) |
| >138%–200% | 492 (4.2) | 279 (3.5) | 2,303 (3.2) |
| >200% | 875 (7.4) | 637 (7.9) | 7,106 (10.0) |
| Missing or invalid | 1,538 (13.0) | 1,458 (18.1) | 16,228 (22.8) |
| Insurance statusc | |||
| Uninsured | 690 (5.8) | 622 (7.7) | 8,565 (12.1) |
| Medicaid | 9,335 (78.8) | 5,786 (71.9) | 45,321 (63.7) |
| Commercial | 1,025 (8.7) | 961 (12.0) | 10,053 (14.1) |
| Other public non-portable coverage | 794 (6.7) | 676 (8.4) | 7,160 (10.1) |
| BMI z-score (mean)d | 0.6 (1.2) | 0.5 (1.2) | 0.5 (1.2) |
| BMI classificationd | |||
| Underweight | 441 (3.7) | 338 (4.2) | 3,173 (4.5) |
| Normal weight | 7,261 (61.3) | 5,047 (62.7) | 45,152 (63.5) |
| Overweight | 2,026 (17.1) | 1,254 (15.6) | 11,246 (15.8) |
| Obeseb | 1,742 (14.7) | 1,148 (14.3) | 9,342 (13.1) |
| Severe obese | 374 (3.2) | 258 (3.2) | 2,186 (3.1) |
OCHIN and HCN patients who, between 1/1/2012 and 12/31/2014, had at least one valid BMI measure when they were 4–5 years of age, regardless of weight status.
Last known FPL.
At most recent visit
At index visit (latest observed well child visit with a valid BMI within 2012–2014)
HCN, Health Choice Network; FPL, Federal Poverty Level
DISCUSSION
The ADVANCE Early Life Cohort provides an exceptionally large, racially and ethnically diverse population of low-income children who are typically under-represented in research on early life determinants of health. We present evidence that the cohort addresses critical research challenges of studying early life processes through which obesity develops in socially vulnerable children.
First, our cohort represents an understudied, vulnerable population, with 32% in extreme poverty (<50% FPL). Our cohort will enable investigation of gradations of poverty and interactions between racial/ethnic groups and modifiable factors such as socioeconomic status or access to care, which is often infeasible due to insufficient sample size. The national scope of the population will support research on environmental exposures such as food policy, chemical exposures, or health care access that vary geographically. It will also provide a foundation for research on transforming clinical care to incorporate family-based behavioral interventions (Willis et al., 2014) and strategies for linking patients to community-based resources (Garg, Toy, Tripodis, Silverstein, & Freeman, 2015).
Second, our cohort spans the full spectrum of weight status, based on objectively measured weight and stature. Obesity prevalence in our cohort (7.1% high WFL in children <2 years; 12.7% obese, 2.4% severely obese in children 2–5years) was similar to a nationally representative samples: 7.1% in children <2 years (Ogden, Carroll, Kit, & Flegal, 2014), 11.1% obese and 2.6% severely obese in children 2–5 years (Skinner & Skelton, 2014)) and 14.7 % obese in a national sample of low-income children ages 2–4 years. comprised predominantly of Special Supplemental Nutrition Program for Women, Infants, and Children participants (Pan, McGuire, Blanck, May-Murriel, & Grummer-Strawn, 2015). Yet disparities in obesity prevalence become more pronounced later in childhood (Skinner & Skelton, 2014); that is, children with lower socioeconomic status tend to be born smaller, then experience faster growth in infancy and early childhood, which can continue throughout childhood (Boone-Heinonen, Messer, Andrade, & Takemoto, 2016). Therefore, research is needed on clinical and community supports that can prevent the socioeconomic divergence in obesity as children grow into adolescents. Furthermore, underweight was common in our cohort (5.3%, compared to 3.4% nationally)(Fryar & Ogden, 2012), potentially reflecting the challenges of hunger or lack of access to basic needs facing low-income populations, or greater prevalence of underlying health conditions that restrict growth.
Third, our cohort provides longitudinal measures needed to study early life determinants of obesity in low-income populations. While segments of the safety net population are transient, we observed substantial follow-up for a large proportion of our population. For example, >10,000 children 4–5 years of age had historical BMI measures spanning into infancy, which can support investigation of early life growth patterns and obesity later in life. Children with and without BMI measures spanning from infancy through 4–5 years were similar with respect to sex, income, and BMI. Because differences in race/ethnicity and region in part reflects later onboarding of HCN to the EHR (typically 2011 or after), which is located in the Southeastern U.S., we expect these differences to decrease as children age. Longitudinal research will require more detailed examination of systematic differences in children with varying durations of follow-up and application and development of appropriate adjustment strategies.
Collectively, our findings suggest that our cohort and similar EHR-based cohorts are promising for longitudinal research on obesity development in early life. Important next steps are to apply the data for hypothesis-based research about early origins of obesity and disparities, and to extend this work to other health outcomes, including obesity sequela (e.g., diabetes) and other conditions such as asthma or infectious disease.
Limitations
A critical limitation of our cohort is that, like other EHR-based data sources, data on key factors such as breastfeeding are not typically available. We are positioned to integrate these variables, consistent with Institute of Medicine’s recommendations to integrate social determinants of health into EHRs (IOM, 2014). Ongoing advancements in natural language processing methods used to extract information from clinician notes (Pivovarov & Elhadad, 2015) can further enhance EHR databases. Yet specialized data, such as detailed infant feeding or diet, is outside the scope of routine clinical interaction and will require ancillary data collection.
The cohort represents children who obtained clinical care for well child visits or other visits at OCHIN or HCN clinics; systematic differences in those included versus excluded from safety net clinics can result in overestimation of disease prevalence and bias in exposure-disease associations and requires appropriate adjustment strategies and interpretation. Other limitations include mobility in and out of the safety net population and error in and lack of validation of anthropometric and sociodemographic measures. For example, we assumed that stature measures reflect length in children under two years of age. We included BMI measures recorded at encounters other than well-child visits; in our safety net population, preliminary analysis suggested that differential exclusion of uninsured children was of greater concern than underestimation of BMI due to illness. Validation of measures in the EHR needs to be assessed overall, and across provider, clinic, or health network.
Conclusions
Early childhood obesity and severe obesity are critical problems in the safety net population, with clear racial/ethnic disparities. The ADVANCE Early Life cohort offers unique opportunities to identify and mitigate early life determinants of obesity in this large, diverse population of low-income children.
Supplementary Material
SIGNIFICANCE.
What is known
Early life determinants of health are understudied in low-income populations. Electronic health records provide longitudinal clinical data on large U.S. populations, but typically omit uninsured and socially vulnerable children.
What this article adds
The ADVANCE Early Life Cohort is the first national low-income study population that leverages electronic health record data from two networks of Federally-Qualified Health Centers. This cohort of >200,000 low-income children provides the sociodemographic diversity, full spectrum of weight status, and substantial longitudinality required to conduct future research on early life determinants of obesity in low-income children.
Acknowledgments
This publication was funded through a Patient-Centered Outcomes Research Institute (PCORI) Award (1306-04716) for development of the National Patient-Centered Clinical Research Network, known as PCORnet. The statements presented in this publication are solely the responsibility of the author(s) and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors or Methodology Committee or other participants in PCORnet. The project described was also supported by the Office of Research in Women’s Health and the National Institute of Child Health and Human Development, Oregon BIRCWH Award Number K12HD043488-01. We thank the ADVANCE research team: Vance Bauer (governance and collaboration), Melissa Laurie, Jill Arkind, Katie Dambrun, and Elizabeth Hooker (research coordination), Nathan Warren (patient engagement), and Jon Puro and Pedro Rivera (data systems). ADVANCE data are accessible to outside investigators through approval by the ADVANCE Research Leadership Committee and, subsequently, research collaboration and agreement with ADVANCE investigators.
Footnotes
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
References
- Boone-Heinonen J, Messer L, Andrade K, Takemoto E. Connecting the Dots in Childhood Obesity Disparities: a Review of Growth Patterns from Birth to Pre-Adolescence. Current Epidemiology Reports. 2016;3(1):113–124. doi: 10.1007/s40471-016-0065-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. Age and Sex of All People, Family Members and Unrelated Individuals Iterated by Income-to-Poverty Ratio and Race. 2014 Retrieved from http://www.census.gov/hhes/www/cpstables/032015/pov/pov01_100.htm.
- Centers for Disease Control and Prevention. A SAS Program for the 2000 CDC Growth Charts (ages 0 to <20 years) 2015 Available at: http://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm.
- DeVoe JE, Gold R, Cottrell E, Bauer V, Brickman A, Puro J, … Fields S. The ADVANCE network: accelerating data value across a national community health center network. Journal of the American Medical Informatics Association. 2014;21(4):591–595. doi: 10.1136/amiajnl-2014-002744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal KM, Wei R, Ogden CL, Freedman DS, Johnson CL, Curtin LR. Characterizing extreme values of body mass index-for-age by using the 2000 Centers for Disease Control and Prevention growth charts. American Journal of Clinical Nutrition. 2009;90(5):1314–1320. doi: 10.3945/ajcn.2009.28335. [DOI] [PubMed] [Google Scholar]
- Fryar CD, Ogden CL. Prevalence of Underweight Among Children and Adolescents Aged 2–19 Years: United States, 1963–1965 Through 2007–2010. 2012 Available at: http://www.cdc.gov/nchs/data/hestat/underweight_child_07_10/underweight_child_07_10.htm.
- Garg A, Toy S, Tripodis Y, Silverstein M, Freeman E. Addressing social determinants of health at well child care visits: a cluster RCT. Pediatrics. 2015;135(2):e296–304. doi: 10.1542/peds.2014-2888peds.2014-2888. [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grummer-Strawn LM, Reinold C, Krebs NF. Use of World Health Organization and CDC growth charts for children aged 0–59 months in the United States. MMWR: Recommendations and Reports. 2010;59(RR-9):1–15rr5909a1. [pii] [PubMed] [Google Scholar]
- Hillier TA, Pedula KL, Vesco KK, Schmidt MM, Mullen JA, LeBlanc ES, Pettitt DJ. Excess gestational weight gain: modifying fetal macrosomia risk associated with maternal glucose. Obstetrics and Gynecology. 2008;112(5):1007–1014. doi: 10.1097/AOG.0b013e31818a9779112/5/1007. [pii] [DOI] [PubMed] [Google Scholar]
- IOM. Capturing social and behavioral domains and measures in electronic health records: Phase 2. 2014 Retrieved from Washington, DC: http://www.nationalacademies.org/hmd/Reports/2014/EHRdomains2.aspx. [PubMed]
- Koebnick C, Coleman KJ, Black MH, Smith N, Der-Sarkissian JK, Jacobsen SJ, Porter AH. Cohort profile: the KPSC Children’s Health Study, a population-based study of 920 000 children and adolescents in southern California. International Journal of Epidemiology. 2012;41(3):627–633. doi: 10.1093/ije/dyq252dyq252. [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, … Johnson CL. 2000 CDC Growth Charts for the United States: methods and development. Vital and Health Statistics. Series 11: Data from the National Health Survey. 2002;(246):1–190. [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan L, McGuire LC, Blanck HM, May-Murriel AL, Grummer-Strawn LM. Racial/ethnic differences in obesity trends among young low-income children. American Journal of Preventive Medicine. 2015;48(5):570–574. doi: 10.1016/j.amepre.2014.11.009S0749-3797(14)00665-5. [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez-Escamilla R, Kac G. Childhood obesity prevention: a life-course framework. International journal of obesity supplements. 2013;3(Suppl 1):S3–s5. doi: 10.1038/ijosup.2013.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pivovarov R, Elhadad N. Automated methods for the summarization of electronic health records. Journal of the American Medical Informatics Association. 2015;22(5):938–947. doi: 10.1093/jamia/ocv032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossen LM, Schoendorf KC. Measuring health disparities: trends in racial-ethnic and socioeconomic disparities in obesity among 2- to 18-year old youth in the United States, 2001–2010. Annals of Epidemiology. 2012;22(10):698–704. doi: 10.1016/j.annepidem.2012.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner AC, Skelton JA. Prevalence and trends in obesity and severe obesity among children in the United States, 1999–2012. JAMA Pediatrics. 2014;168(6):561–566. doi: 10.1001/jamapediatrics.2014.21. [DOI] [PubMed] [Google Scholar]
- Taveras EM, Gillman MW, Kleinman KP, Rich-Edwards JW, Rifas-Shiman SL. Reducing racial/ethnic disparities in childhood obesity: the role of early life risk factors. JAMA Pediatrics. 2013;167(8):731–738. doi: 10.1001/jamapediatrics.2013.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vesco KK, Sharma AJ, Dietz PM, Rizzo JH, Callaghan WM, England L, … Hornbrook MC. Newborn size among obese women with weight gain outside the 2009 Institute of Medicine recommendation. Obstetrics and Gynecology. 2011;117(4):812–818. doi: 10.1097/AOG.0b013e3182113ae400006250-201104000-00008. [pii] [DOI] [PubMed] [Google Scholar]
- WHO. Weight-for-length/height. Child Growth Standards. 2006 Retrieved from http://www.who.int/childgrowth/standards/weight_for_length_height/en/
- Willis TA, George J, Hunt C, Roberts KP, Evans CE, Brown RE, Rudolf MC. Combating child obesity: impact of HENRY on parenting and family lifestyle. Pediatric Obesity. 2014;9(5):339–350. doi: 10.1111/j.2047-6310.2013.00183.x. [DOI] [PubMed] [Google Scholar]
- Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annual Review of Public Health. 2006;27:1–28. doi: 10.1146/annurev.publhealth.27.021405.102113. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.