Abstract
Objectives
We describe the clinical characteristics, prevalence and control of coronary artery disease (CAD) risk factors of the Indian cohort enrolled in the CLARIFY registry and compare them with data from rest of the world (ROW).
Methods
CLARIFY is an international, prospective, observational, longitudinal cohort study in stable CAD outpatients. The baseline data of Indian cohort (n = 709) were compared to ROW (n = 31994).
Results
The CLARIFY India patients were significantly younger than the ROW (59.6 ± 10.9 vs 64.3 ± 10.4). Indian patients were more likely than those in ROW to have diabetes (42.9% vs 28.8%) and angina (27.8% vs 21.9%). Mean heart rate was significantly greater in Indians measured by either palpatory method (76.1 ± 10.4 vs 68.0 ± 10.5) or ECG (74.9 ± 12.9 vs 67.0 ± 11.3). The use of aspirin (85.6% vs 87.8%), β-blockers (69.4% vs 75.4%), and lipid-lowering agents (90% vs 92.4%) was lower in India. A significantly greater proportion of patients in India exhibited low HDL cholesterol (41.6% vs 31.2%), and heart rate ≥70 bpm (82.2% vs 48.5%). The risk factors control was poor in India with heart rate goal of ≤60 bpm achieved in 2.5%; HbA1c <7% in 9.9%; and HbA1c <6.5% in 4.6% patients.
Conclusion
The CLARIFY registry demonstrates a high prevalence and poor control of cardiovascular risk factors in Indian patients. Systematic efforts to improve risk factor control are required.
Keywords: Coronary artery disease, Heart rate, Risk factors, India, Registries, Secondary prevention
1. Introduction
Coronary artery disease (CAD) is the leading cause of cardiovascular morbidity and mortality worldwide, contributing to over 7 million deaths annually.1 Regardless of a recent decline in CAD mortality in the developed countries,2 the burden of CAD in India is rising remarkably. The national commission on macroeconomics and health estimated about 359 lakh CAD cases in 2005 that has been projected to rise up to 615 lakhs in 2015,3 with the corresponding loss of the national income of approximately 237 billion USD in India.4 These estimates draw special attention to the urgent need of aggressive strategies for the prevention and control of CAD in India.
A line of evidence indicates that the Indians are more susceptible to CAD and manifest higher mortality rate than their western counterparts.5, 6, 7, 8 The fact may be attributed to diverse risk factors distribution and control across various geographical locations in India.9 Therefore, one of the crucial strategies in the primary prevention of CAD could be achieving the risk factors control, which has been emphasised even in recent clinical practice guidelines.10, 11 Although, there are enormous advances in the secondary prevention of CAD as witnessed by numerous clinical trials of antiplatelet therapy, statins, and angiotensin-converting enzyme inhibitors, the data on contemporary clinical practice management of CAD and its impact on clinical outcomes are scarce in India. Moreover, the available epidemiological data are not derived from well-designed high-quality studies, and majorly included patients with acute coronary syndrome with limited information on outpatients with stable CAD.12, 13 Bridging this gap, the Prospective Observational Longitudinal Registry of patients with stable coronary artery disease (CLARIFY) registry was carried out across 45 geographical regions of the world with the objectives to gain information on their demographic characteristics, clinical presentation, and management of CAD. The registry also intends to study clinical outcomes of these patients and identify the long-term prognostic factors determining the clinical outcomes.
This communication describes the clinical characteristics, prevalence and control of risk factors for CAD in India and compares them with the rest of the world (ROW) by analysing data from global CLARIFY registry.
2. Methods
2.1. Study design
CLARIFY is an international, prospective, observational, longitudinal cohort study in stable CAD outpatients with 5 years of follow-up. Detailed methods have been published previously.14, 15, 16
2.2. Patient selection
Stable CAD patients with at least one of the following: coronary stenosis >50% on coronary angiography; documented myocardial infarction (MI, >3months ago); chest pain with myocardial ischemia proven using stress electrocardiogram stress echocardiography, or myocardial imaging; history of coronary artery bypass graft surgery (CABG) or percutaneous coronary intervention (PCI; performed >3 months ago), were enrolled in the registry. Patients with planned revascularisation, patients hospitalised for cardiovascular disease (CVD) (included revascularisation) 3 months prior to enrolment, patients with conditions anticipated to impede 5-year follow-up (e.g. serious non-cardiovascular disease, conditions limiting life expectancy, limited cooperation or legal capacity, or severe CVD [advanced heart failure, severe valve disease, history of valve repair/replacement, etc]), were excluded from the study.
2.3. Data collection and selection of patients for India sub-study
The information collected included demographic characteristics; risk factors and lifestyle; medical history included present symptoms; physical examination; cardiac evaluation included measuring the heart rate (HR) by pulse palpation and the resting electrocardiogram within the previous 6 months. Blood pressure both systolic and diastolic was recorded. All patients had an ECG taken and a record of rhythm documented. Blood tests recorded included haemoglobin, fasting blood glucose, HbA1c, serum triglycerides and cholesterol, and serum creatinine, if available. A note was made of current medications taken regularly by the patient for ≥7 days before entry in the registry.
In the current paper, only the patients recruited from India (709) were compared with rest of the world.
2.4. Ethics
The registry was conducted in line with the principles outlined in the Declaration of Helsinki and was approved by the National Research Ethics Service, Isle of Wight, Portsmouth, and Southeast Hampshire Research Ethics Committee, UK. Approval was also obtained in all participating centres in accordance with local regulations. All patients provided written informed consent. The ISRCTN registration number of CLARIFY is ISRCTN43070564.
2.5. Statistical analysis
Data are summarised as mean with standard deviation or median with interquartile range. Categorical data are presented as counts and percentages. Data were analysed by χ2 tests or Fisher’s exact test for categorical and t-test or Mann–Whitney U test for continuous variables using 2-sided tests at a significance level of 5% using Statistical Analysis Software (version 9.2).
3. Results
The global CLARIFY registry included a total of 32703 analysable patients, of these, Indian cohort comprised of 709 (2.2%) stable CAD patients.
3.1. Patient characteristics
A majority of baseline characteristics and lifestyle practices of CLARIFY India cohort were similar to the ROW population (Table 1). The CLARIFY India patients were significantly younger than the ROW (59.6 ± 10.9 vs 64.3 ± 10.4). Indian patients were more likely than those in the ROW to have diabetes (42.9% vs 28.8%), but less likely to have a family history of premature CAD (21.3% vs 28.7%), dyslipidaemia (63% vs 75.2%), peripheral arterial disease (4.8% vs 10%), aortic abdominal aneurysm (0.1% vs 1.6%), and carotid disease (1.8% vs 7.7%) (Table 2). Indian participants had less frequent history of MI (55.3% vs 60%), PCI (42.5% vs 59%) and CABG (20.7% vs 23.6%) than the ROW patients. The mean HR (bpm) of CLARIFY Indian cohort was significantly higher when compared to the ROW; measured by both palpation (76.1 ± 10.4 vs 68.0 ± 10.5) and ECG (74.9 ± 12.9 vs 67.0 ± 11.3). Angina was significantly more prevalent in India (27.8% vs 21.9%).
Table 1.
Baseline demographic characteristics and lifestyle of patients.
| Clinical characteristics | India (N = 709) | Rest of the world (N = 31994) | p value |
|---|---|---|---|
| Demographic characteristics | |||
| Age (years), mean(SD) | 59.6 (10.9) | 64.3 (10.4) | <0.0001 |
| Male | 564 (79.5) | 24801 (77.5) | 0.2223 |
| BMI (kg/m2), mean(SD) | 25.7 (4) | 27.9 (4.6) | <0.0001 |
| Ethnicity | <0.00001 | ||
| Caucasian | 13 (1.8) | 21099 (65.9) | |
| South Asian | 696 (98.2) | 1748 (5.5) | |
| Lifestyle | |||
| Living Alone | 21 (3) | 3665 (11.5) | <0.0001 |
| Smoking status | <0.00001 | ||
| Current | 62 (8.7) | 4015 (12.6) | |
| Former | 171 (24.1) | 14938 (46.7) | |
| Never | 476 (67.1) | 13037 (40.8) | |
| Alcohol Intake | 124 (17.4) | 16955 (53) | <0.0001 |
| Weekly Physical Activity | <0.00001 | ||
| None | 88 (12.4) | 5199 (16.3) | |
| Only Light | 449 (63.3) | 16361 (51.2) | |
| Vigorous at least once or twice | 98 (13.8) | 5372 (16.8) | |
| Vigorous 3 or more times | 74 (10.4) | 5047 (15.8) | |
| Value represents n (%) unless specified | |||
Table 2.
Medical history of patients.
| Clinical characteristics | India (N = 709) | Rest of the world (N = 31994) | p value |
|---|---|---|---|
| Medical history | |||
| Family history of premature CAD | 151 (21.3) | 9175 (28.7) | <0.0001 |
| Treated Hypertension | 493 (69.5) | 22717 (71) | 0.2050 |
| Diabetes | 304 (42.9) | 9198 (28.8) | <0.0001 |
| Dyslipidemia | 447 (63) | 24057 (75.2) | <0.0001 |
| Peripheral Arterial Disease | 34 (4.8) | 3205 (10) | <0.0001 |
| Myocardial Infarction | 392 (55.3) | 19203 (60) | 0.0060 |
| PCI | 301 (42.5) | 18861 (59) | <0.0001 |
| CABG | 147 (20.7) | 7556 (23.6) | 0.0402 |
| Aortic abdominal aneurysm | 1 (0.1) | 503 (1.6) | 0.0018 |
| Carotid Disease | 13 (1.8) | 2461 (7.7) | <0.0001 |
| Internal Cardiac Defibrillator, | 2 (0.3) | 416 (1.3) | 0.0133 |
| Pacemaker | 7 (1) | 781 (2.4) | 0.0088 |
| Stroke | 11 (1.6) | 1303 (4.1) | 0.0005 |
| TIA | 17 (2.4) | 984 (3.1) | 0.1770 |
| Hospitalization for CHF | 17 (2.4) | 1514 (4.7) | 0.0024 |
| Atrial fibrillation/Flutter | 9 (1.3) | 2304 (7.2) | <0.0001 |
| Asthma/COPD | 46 (6.5) | 2373 (7.4) | 0.1940 |
| Current or previous trial participation | 5 (0.7) | 1130 (3.5) | <0.0001 |
| Current symptoms and measurements | |||
| Angina | 197 (27.8) | 7015 (21.9) | 0.0002 |
| CHF | 63 (8.9) | 4862 (15.2) | <0.0001 |
| SBP (mmHg), mean(SD) | 131.6 (18.6) | 131.0 (16.6) | 0.3425 |
| DBP (mmHg), mean(SD) | 80.8 (9.3) | 77.2 (10) | <0.0001 |
| HR by pulse palpation (bpm), mean (SD) | 76.1 (10.4) | 68.0 (10.5) | <0.0001 |
| HR on ECG (bpm), mean (SD) | 74.9 (12.9) | 67.0 (11.3) | <0.0001 |
| LBBB if ECG available | 23 (5.4) | 1178 (4.9) | 0.7512 |
| Value represents n (%) unless specified |
3.2. Medical therapies
The use of selected chronic cardiovascular medications at enrolment is presented in Table 3. Overall, a major proportion of the India and the ROW cohorts were taking guideline-recommended therapy. The use of anti-platelets was high with aspirin being the most commonly used (85.6% vs 87.8%) in India vs ROW. Thienopyridine (54.9% vs 26.6%) and dual anti-platelets (53.3% vs 27.4%) were prescribed to significantly higher proportion of patients in India than the ROW. The use of β-blockers (69.4% vs 75.4%) and ivabradine (5.4% vs 9.9%) was significantly lower in India compared to the ROW. Though a total of 90% and 92.4% patients in India and the ROW, respectively, used lipid lowering agents, there was less frequent use of statin in India (77.9% vs 90%).
Table 3.
Medical therapy at baseline.
| Medication | India (N = 709) | Rest of the world (N = 31994) | p value |
|---|---|---|---|
| Aspirin | 607 (85.6) | 28080 (87.8) | 0.0443 |
| Thienopyridine | 389 (54.9) | 8492 (26.6) | <0.0001 |
| Other antiplatelet agents | 69 (9.7) | 2954 (9.2) | 0.3534 |
| Aspirin and another antiplatelet agent | 378 (53.3) | 8767 (27.4) | <0.0001 |
| Oral anticoagulant | 65 (9.2) | 2605 (8.2) | 0.1820 |
| Antiplatelet agent and anticoagulant | 53 (7.5) | 1641 (5.1) | 0.0035 |
| β-Blockers | 492 (69.4) | 24119 (75.4) | <0.0001 |
| Ivabradine | 38 (5.4) | 3180 (9.9) | <0.0001 |
| Calcium antagonists | 183 (25.8) | 8726 (27.3) | 0.2032 |
| Verapamil or Dilitiazem | 41 (5.8) | 1855 (5.8) | 0.4920 |
| ACE Inhibitors | 280 (39.5) | 16615 (52) | <0.0001 |
| Angiotensin II receptor blockers | 211 (29.8) | 8463 (26.5) | 0.0274 |
| Lipid-lowering drugs | 638 (90) | 29553 (92.4) | 0.0101 |
| Statins if on lipid lowering agents | 497 (77.9) | 26602 (90) | 0.0001 |
| Other antianginal agents | 140 (19.7) | 4401 (13.8) | <0.0001 |
| Trimetazidine | 68 (9.6) | 3388 (10.6) | 0.2120 |
| Ranolazine | 38 (5.4) | 98 (0.3) | <0.0001 |
| Diuretics | 214 (30.2) | 9371 (29.3) | 0.3204 |
| Other antihypertensive agents | 72 (10.2) | 2179 (6.8) | 0.0003 |
| Digoxin and derivatives | 28 (3.9) | 800 (2.5) | 0.0106 |
| Amiodarone/Dronedarone | 17 (2.4) | 945 (3) | 0.2245 |
| Other Antiarrhythmics | 2 (0.3) | 304 (1) | 0.0514 |
| Anti-diabetes agents | 254 (35.8) | 7762 (24.3) | <0.0001 |
| Value represents n (%) unless specified |
3.3. Risk factors and their control
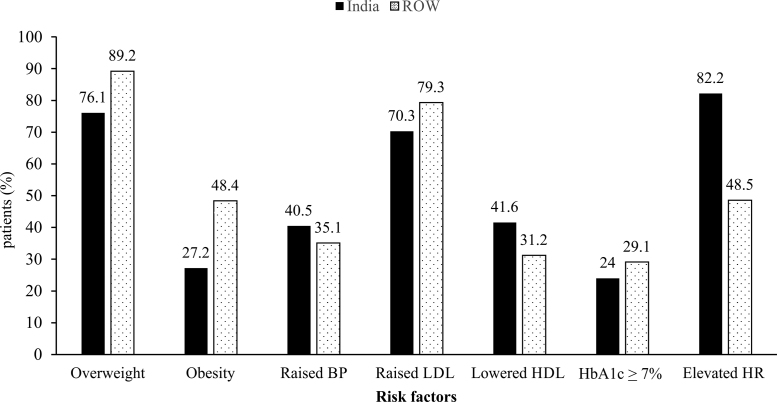
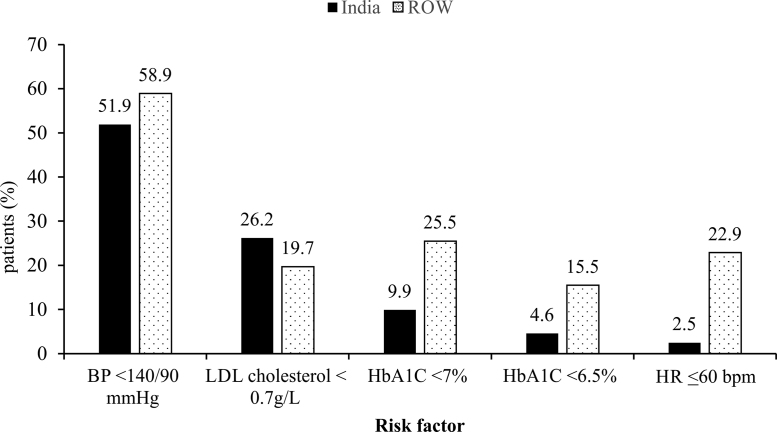
In general, the prevalence of cardiovascular risk factors was very high in CLARIFY India cohort compared to the ROW (Fig. 1, Fig. 2). The Indian cohort was less likely to be overweight (76.1% vs 89.2%) and obese (27.2% vs 48.4%) than the ROW. A significantly greater proportion of patients in India displayed dyslipidaemia, notably raised LDL cholesterol (70.3% vs 79.3%) and low HDL cholesterol (41.6% vs 31.2%). The remarkably high proportion of Indian patients exhibited elevated HR (≥70 bpm) than the ROW (82.2% vs 48.5, p < 0.0001), and only 2.5% in India vs 22.9% in the ROW achieved the HR goal of ≤60 bpm when presented with symptoms of angina. About 9.9% and 4.6% patients achieved HbA1c <7% and HbA1c <6.5%, respectively, in India.
Fig. 1.
Distribution of risk factors in India and the rest of the world (all p < 0.05). Overweight: BMI ≥23 kg/m2; Obesity: BMI of ≥27.0 kg/m2; Raised BP: SBP ≥140 mmHg and/or DBP ≥90 mmHg; Raised LDL (≥0.7 g/L, 1.8 mmol/L); Lowered HDL (≤40 mg/dL, 1.0 mmol/L); HbA1c ≥ 7% in diabetic patients; Elevated HR on palpation ≥70 in angina patients BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; LDL, low density lipoprotein; HDL, high density lipoprotein; HR, heart rate; ROW, rest of the world.
Fig. 2.
Control of risk factors in India and the rest of the world (all p < 0.05). BP <140/90 mm Hg in patients with hypertension; LDL cholesterol <0.7 g/L in patients with dyslipidaemia; HbA1c <7% in patients with diabetes; HbA1c <6.5% in patients with diabetes; Heart rate ≤60 bpm in patients with symptoms of angina BP, blood pressure; LDL, low density lipoprotein; HDL, high density lipoprotein; HR, heart rate; ROW, rest of the world.
4. Discussion
The CLARIFY registry is an international, prospective, observational longitudinal registry focused on outpatients with stable CAD.
Similar to the previous epidemiological studies,17, 18 the prevalence of cardiovascular risk factors was higher in CLARIFY India cohort. CLARIFY India results witnessed lower prevalence of overweight and obesity than the ROW. These findings are consistent with the WHO estimates that show a relatively low rate of overweight and obesity in India.19 However, there is a strong evidence that the metabolic consequences of obesity, dyslipidaemia (particularly hypertriglyceridemia, low HDL and increased numbers of small dense LDL particles) and dysglycaemia (insulin resistance and type 2 diabetes), are apparent at lower absolute levels of total body fat in South Asians than in whites. In agreement with these facts, the proportion of patients with raised LDL-C, reduced HDL-C, and diabetes (with poor glycaemic control) were greater in CLARIFY India cohort. Moreover, one of the remarkable characteristics was younger age of the Indian cohort than the ROW. The results are in agreement with the results of the INTERHEART study, an international case-control study carried out in 52 countries, including India, involving 15152 cases of acute MI.20 The study has shown a high prevalence of cardiovascular risk factors even among controls who were less than sixty years of age.
One of the crucial strategies for prevention of CAD universally recommended by evidence-based guidelines includes comprehensive management of modifiable risk factors, which includes weekly physical activity, weight management, smoking/tobacco cessation, and dietary modification.21 The findings from this sub-set analysis (Table 1) show that the majority of patients in the CLARIFY Indian cohort were not practicing healthy lifestyle for managing modifiable risk factors. Therefore, the current pattern of CAD characterised by the high prevalence of inadequately controlled risk factors, as revealed by CLARIFY registry, suggest that the increased cardiovascular risk in India may be preventable through lifestyle interventions and the judicious use of drugs to attain optimal levels of blood pressure, lipids and glucose.
Medical therapy is an important component of secondary prevention that includes aspirin, statins, and β-blockers. In addition, angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers are recommended for concomitant heart failure, hypertension, or diabetes. Several prospective registries such as WHO-PREMISE and PURE studies report underutilization of evidence-based medicine in India22, 23; however, it is noteworthy that the majority of CLARIFY India patients received the recommended medical care. Like ROW CLARIFY cohort (92.4%), the majority of CLARIFY India patients (90%) received lipid lowering agents with a noticeable difference in the proportion of patients receiving a statin. Although the majority of patients received recommended therapy, yet there are significant gaps in secondary prevention of CVD in urban and rural communities despite the availability of medications at an affordable cost as demonstrated in Andhra Pradesh Rural Health Initiative (APRHI) in India.24 Moreover, underused treatments, lack of awareness among patients and the physician, and non-adherence to medications are some of the factors responsible for poor management, despite the sheer scale of CVD prevalence in India.25, 26, 27 All these factors mandate systematic interventions to improve the long-term use of basic, inexpensive, and effective drugs.
Determining the long-term prognostic value of HR remains the imperative objective of the CLARIFY. The data on clinical outcomes after 5 year follow-up of these Indian CAD patients is intended to be published separately. Taking into account the increased cardiovascular risk with elevated HR,28 several recent clinical practice guidelines have emphasised HR reduction as a substantial cardiovascular risk management strategy.11 In the similar context, the mean HR and proportion of patients having HR ≥70 bpm of CLARIFY India cohort were higher than ROW. In addition, only 2.5% and 22.9% patients in the present cohort of CLARIFY India and the ROW, respectively, achieved goal HR ≤60 bpm. Similar results were revealed in BEAUTIFUL trial enrolling stable CAD patients; more than half of patients demonstrated a baseline resting HR ≥70 bpm, which was associated with significantly higher risk of myocardial infarction, coronary revascularization, and death, even with ß-blockers.29 An important finding of the trial was that ivabradine added to optimal preventive therapy further reduced the risk of coronary events such as MI by −36% and revascularization by −30%.29 Ivabradine is a pure HR-lowering agent having a selective action on the sinus node and is thus devoid of the usual side effects of β-blockers. In light of the above data, taking a step forward in the management of coronary patients, recent guidelines now recommend ivabradine for heart rate reduction as a second line treatment in the management of coronary patients.11
Voluntary enrolment of patients by physicians contributed inherent selection bias. In particular, the CLARIFY India cohort included patients attending outpatient clinics/hospitals only in major city areas indicating urban bias. Despite these limitations, the registry has several strengths, including a large number of participating countries, making the results more generalizable.
5. Conclusion
The baseline results of the Indian cohort from CLARIFY registry indicate that there is a high prevalence and poor control of cardiovascular risk factors. Systematic approaches to improve control of modifiable risk factors and increase the long-term use of essential primary and secondary prevention medications are required to fulfil the lacuna in the management of stable CAD in current clinical practice.
Disclosure
The authors have no conflict of interest
Acknowledgement
This study was supported by a research grant from Servier, France, manufacturers of original ivabradine (Coralan®). Servier did not participate in study design, data collection and analysis, decision to publish and preparation of the manuscript. Authors would like to thank all CLARIFY investigators.
Appendix A.
List of the CLARIFY India Investigators (other than authors)
J. P. S. Sawhney (Delhi), M.S. Hiremath (Pune), K. Kunhali (Calicut), P. Khera (Lucknow), A. K. Trivedi (Kanpur), G. Vijayaraghavan (Thiruvanathapuram), I. A. Khan (Indore), D. K. Kumbla (Mumbai), N. S. Chonkar (Mumbai), R. Karnik (Mumbai), Dr Dayasagar Rao V (Secunderabad), K. Srinivasa Reddy(Guntur), Thillai Vallal (Chennai), D. Shukla (Lucknow), R. Ahuja (Lucknow), S. Modi (Delhi), A. Mehta (Delhi), T. Ghose (Delhi), S. Chandra (Delhi), T. Roy (Delhi), M. S. Chenniappan (Trichy), L. Sreenivasa Murthy (Bangalore), S. S. Ramesh (Bangalore), A. Vadavi (Bangalore), M. M. Singh (Patiala), B. Prasad (Kolkata), B.K. Goyal (Mumbai), M. P. Samal (Bilaspur), J. Rawal (Ahmedabad), S. R. Shetty (Mumbai), Late M. Juneja (Mumbai).
References
- 1.World Health Organization . 2004. The Top Ten Causes of Death Fact Sheet. Available at: http://www.who.int/mediacentre/factsheets/fs310/en/index.html. (Accessed 2 July 2016) [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) Prevalence of coronary heart disease-United States, 2006–2010. MMWR Morb Mortal Wkly Rep. 2011;60:1377–1381. [PubMed] [Google Scholar]
- 3.National Commission on Macroeconomics and Health, Ministry of Health & Family Welfare, Government of India; 2005. Report of the National Commission on Macroeconomics and Health. Available at: http://www.who.int/macrohealth/action/Report%20of%20the%20National%20Commission.pdf. (Accessed 2 July 2016) [Google Scholar]
- 4.World Health Organization . 2005. WHO Global Report. Preventing Chronic Diseases-A Vital Investment. Available at: http://www.who.int/chp/chronic_disease_report/en/. (Accessed 2 July 2016) [Google Scholar]
- 5.Prabhakaran D., Yusuf S. Cardiovascular disease in India: lessons learnt & challenges ahead. Indian J Med Res. 2010;132:529–530. [PMC free article] [PubMed] [Google Scholar]
- 6.Nag T., Ghosh A. Cardiovascular disease risk factors in Asian Indian population: a systematic review. J Cardiovasc Dis Res. 2013;4:222–228. doi: 10.1016/j.jcdr.2014.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Balarajan R. Ethnic differences in mortality from ischaemic heart disease and cerebrovascular disease in England and Wales. BMJ. 1991;302:560–564. doi: 10.1136/bmj.302.6776.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Enas E., Garg A., Davidson M. Coronary heart disease and its risk factors in first-generation immigrant Asian Indians to the United States of America. Indian Heart J. 1995;48:343–353. [PubMed] [Google Scholar]
- 9.Krishnan M.N. Coronary heart disease and risk factors in India − on the brink of an epidemic? Indian Heart J. 2012;64:364–367. doi: 10.1016/j.ihj.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fihn S.D., Gardin J.M., Abrams J. ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2012;60:e44–e164. doi: 10.1016/j.jacc.2012.07.013. [DOI] [PubMed] [Google Scholar]
- 11.Montalescot G., Sechtem U., Achenbach S. ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. 2013;34:2949–3003. doi: 10.1093/eurheartj/eht296. [DOI] [PubMed] [Google Scholar]
- 12.Xavier D., Pais P., Devereaux P. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371:1435–1442. doi: 10.1016/S0140-6736(08)60623-6. [DOI] [PubMed] [Google Scholar]
- 13.Ahmad N., Bhopal R. Is coronary heart disease rising in India? A systematic review based on ECG defined coronary heart disease. Heart. 2005;91:719–725. doi: 10.1136/hrt.2003.031047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Steg P.G. Heart rate management in coronary artery disease: the CLARIFY registry. Eur Heart J Suppl. 2009;1:D13–18. [Google Scholar]
- 15.Steg P.G., Ferrari R., Ford I. Heart rate and use of beta-blockers in stable outpatients with coronary artery disease. PLoS One. 2012;7:e36284. doi: 10.1371/journal.pone.0036284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Steg P.G., Greenlaw N., Tardif J.C. Women and men with stable coronary artery disease have similar clinical outcomes: insights from the international prospective CLARIFY registry. Eur Heart J. 2012;33:2831–2840. doi: 10.1093/eurheartj/ehs289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.James C. Risk factors for coronary artery diseases: a study among patients with ischemic heart disease in Kerala. Heart India. 2013;1:7–11. [Google Scholar]
- 18.Rao M., Xavier D., Devi P. Prevalence, treatments and outcomes of coronary artery disease in Indians: a systematic review. Indian Heart J. 2015;67:302–310. doi: 10.1016/j.ihj.2015.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yatsuya H., Li Y., Hilawe E.H. Global trend in overweight and obesity and its association with cardiovascular disease incidence. Circ J. 2014;78:2807–2818. doi: 10.1253/circj.cj-14-0850. [DOI] [PubMed] [Google Scholar]
- 20.Vamadevan A.S., Prabhakaran D. Coronary heart disease in Indians: implications of the INTERHEART study. Indian J Med Res. 2010;132:561–566. doi: 10.4103/0971-5916.73396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hall S.L., Lorenc T. Secondary prevention of coronary artery disease. Am Fam Phys. 2010;81:289–296. [PubMed] [Google Scholar]
- 22.Sharma K.K., Gupta R., Agrawal A. Low use of statins and other coronary secondary prevention therapies in primary and secondary care in India. Vasc Health Risk Manag. 2009;5:1007–1014. doi: 10.2147/vhrm.s8017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sharma K.K., Guptha S., Gupta R. Secondary prevention therapies for coronary heart disease in patients with type 2 diabetes: an audit. J Assoc Phys India. 2012;60:28–30. [PubMed] [Google Scholar]
- 24.Joshi R., Chow C.K., Raju P.K. Fatal and nonfatal cardiovascular disease and the use of therapies for secondary prevention in a rural region of India. Circulation. 2009;119:1950–1955. doi: 10.1161/CIRCULATIONAHA.108.819201. [DOI] [PubMed] [Google Scholar]
- 25.Mendis S., Abegunde D., Yusuf S. WHO study on prevention of REcurrences of myocardial infarction and StrokE (WHO-PREMISE) Bull World Health Organ. 2005;83:820–829. [PMC free article] [PubMed] [Google Scholar]
- 26.Gupta R., Guptha S., Sharma K.K. Regional variations in cardiovascular risk factors in India: India heart watch. World J Cardiol. 2012;4:112–120. doi: 10.4330/wjc.v4.i4.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.George C.E., Ramadas D., Norman G. Barriers to cardiovascular disease risk reduction: does physicians' perspective matter? Indian Heart J. 2016;68:278–285. doi: 10.1016/j.ihj.2015.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fox K., Ford I., Steg P.G. Heart rate as a prognostic risk factor in patients with coronary artery disease and left-ventricular systolic dysfunction (BEAUTIFUL): a subgroup analysis of a randomised controlled trial. Lancet. 2008;372:817–821. doi: 10.1016/S0140-6736(08)61171-X. [DOI] [PubMed] [Google Scholar]
- 29.Fox K., Ford I., Steg P.G. Ivabradine for patients with stable coronary artery disease and left-ventricular systolic dysfunction (BEAUTIFUL): a randomised, double-blind, placebo-controlled trial. Lancet. 2008;372:807–816. doi: 10.1016/S0140-6736(08)61170-8. [DOI] [PubMed] [Google Scholar]