Abstract
Objective
Cardiac surgery intensive care unit (ICU) characteristics and clinician staffing patterns have not been well characterized. We sought to describe Pennsylvania cardiac ICUs and to determine whether ICU characteristics are associated with mortality in the 30 days after cardiac surgery.
Design
From 2012–2013, we conducted a survey of cardiac surgery ICUs in Pennsylvania to assess ICU structure, care practices, and clinician staffing patterns. ICU data were linked to an administrative database of cardiac surgery patient discharges. We used logistic regression to measure the association between ICU variables and death in 30 days.
Setting
Cardiac surgery ICUs in Pennsylvania.
Patients
Patients having coronary artery bypass grafting (CABG) and/or cardiac valve repair or replacement from 2009 to 2011.
Interventions
None
Measurements and Main Results
Out of 57 cardiac surgical ICUs in Pennsylvania, 43 (75.4%) responded to the facility survey. Rounds included respiratory therapists in 26/43 (60.5%) and pharmacists in 23/43 (53.5%). 26.8% (11/41) reported that at least 2/3 of their nurses had a BSN degree. Advanced practice providers were present in most of the ICUs (37/43, 86.0%), but residents (8/42, 18.6%) and fellows (7/43, 16.3%) were not. Daytime intensivists were present in 48.8% (21/43) of responding ICUs; 18.6% (8/43) had nighttime intensivists. Among 29,449 patients, there was no relationship between mortality and nurse ICU experience, presence of any intensivist, or absence of residents after risk adjustment. To exclude patients who may have undergone transcatheter aortic valve replacement, we conducted a subgroup analysis of patients undergoing only CABG, and results were similar.
Conclusions
Pennsylvania cardiac surgery ICUs have variable structures, care practices, and clinician staffing, although none of these are statistically significantly associated with mortality in the 30 days following surgery after adjustment.
Keywords: intensive care staffing, cardiac surgery, outcomes, administrative data
Introduction
Intensive care unit (ICU) organizational features, such as clinician staffing, constitute modifiable risk factors for adverse outcomes that may potentially affect both organizational resource allocation and patients’ choices about healthcare providers and facilities. Intensive care staffing schemes have been linked to process measures of care quality(1, 2) and to short-term outcomes such as intensive care unit (ICU) mortality(3) and length of stay.(4) Given the apparent association between ICU organizational practices and patient outcomes, payers and other stakeholders have set standards about how many and what kinds of providers are needed to optimally care for critically ill patients.(5–8)
Nonetheless, the evidence supporting specific ICU care paradigms remains heterogeneous and conflicting, and has limited generalizability. In addition, most ICU staffing studies focus on medical or mixed medical-surgical ICUs, with relative underrepresentation of ICUs focusing on surgical care. Cardiac surgery is one important surgical subgroup characterized by high elective surgical volume and highly protocolized care,(9) which might attenuate the impact of specific organizational practices. Additionally, almost all patients undergoing open cardiac surgical procedures are admitted to ICUs for post-surgical care, so understanding the impact of ICU organizational practices is broadly relevant to this patient population.
The objective of this study was to characterize ICU organizational characteristics in cardiac surgical ICUs in Pennsylvania, a large state with urban and rural, community and academic hospitals performing cardiac surgery. Given the multidisciplinary nature of critical care, we conducted a detailed facility survey to collect staffing data about clinicians (nurses, advanced practice providers, respiratory therapists, pharmacists, and physicians) currently working in Pennsylvania ICUs. Linking facility survey responses to discharge data on patients treated in responding hospitals, we examined associations between ICU organizational characteristics and mortality in the 30 days after cardiac surgery.
Materials and Methods
This is a retrospective cohort study of all intensive care units in Pennsylvania that care for adult patients who have undergone cardiac surgery. We merged data from four sources: (1) survey data (collected from 2012 to 2013) describing ICU care practices and clinician staffing patterns, (2) administrative discharge data from Pennsylvania hospitals (2009 to 2011) obtained from the Pennsylvania Health Care Cost Containment Council (PHC4), (3) vital status information from the Pennsylvania Department of Health, and (4) information on hospital characteristics and hospital safety made publicly available by the American Hospital Association Healthcare Data Viewer,(10) the Leapfrog Group, and the American Nurses Credentialing Center (Supplemental Digital Content 1). This project was deemed exempt from IRB review by the Perelman School of Medicine of the University of Pennsylvania IRB.
Study population
For the facility survey, we identified Pennsylvania hospitals performing cardiac surgery, excluding children’s hospitals, from the Pennsylvania Health Care Cost Containment Council (PHC4) state cardiac surgery report from 2008 to 2009,18 the most recent year for which data was publicly available at the start of this project.
Our patient sample included all patients aged 18 or older discharged from a Pennsylvania hospital between January 1, 2009 and December 31, 2011 with a principal or secondary International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) procedure code for coronary artery bypass grafting (CABG, ICD-9-CM procedure codes: 36.10 – 36.17, 36.19) or cardiac valvular repair or replacement surgery (ICD-9-CM procedure code: 35.10 – 35.14, 35.20 – 35.28, 35.33, 35.99).
Questionnaire
We designed an instrument for this project (Supplemental Digital Content 2) based on prior ICU facility surveys,(3) and adapted through consultation with physicians and nurses with expertise in ICU staffing models. The study questionnaire included questions about: (A) use of common ICU protocols; (B) access to resources to support ICU care, including computerized physician order entry and telemedicine consultation, and (C) ICU physician and nurse staffing characteristics, including training and shift structure. For nurse staffing, we asked about ICU experience, the proportion of the ICU nurses who had obtained a bachelor’s degree in nursing (BSN), and the maximum duration of a nursing shift. For experience and education, nurse managers divided their staff into thirds, indicating that “less than 1/3”, “between 1/3 and 2/3”, or “greater than 2/3” of their nurses had a given characteristic. Given our intention to link survey responses to administrative data, we also asked whether clinician staffing characteristics changed between 2009 and 2012. We pilot tested the instrument for comprehension and construct validity with respondents from eight cardiac surgical intensive care units in Delaware, New Jersey, and Ohio.
Recruitment
From September 2012 to May 2013, publicly available directory information was used to contact each hospital’s telephone operator, who then connected research staff to the cardiac surgery ICU, after which we attempted to reach the nurse manager. The nurse manager of each ICU was invited to complete the survey via telephone. When nurse managers were not available, we left call-back information with ICU staff. If contact was unsuccessful after several attempts, a letter of invitation was sent by postal mail and telephone contact was attempted again. Non-responders were mailed an additional letter, along with a paper copy of the survey, a stamped return envelope, and a US $10 bill.
Outcomes
Our primary study outcome was mortality at 30 days after hospital admission, as recorded in Pennsylvania Department of Health vital statistics files.
Independent variables
The survey-derived organizational exposures of interest for the primary analysis were (1) physician staffing (including presence of “intensivists” (physicians with critical care fellowship training), presence of residents and interns, physician coverage during weekdays, weeknights, and weekends), (2) nurse staffing (registered nurse (RN) training, RN ICU experience, RN shift length, and (3) access to resources (multidisciplinary rounds, telemedicine access, computerized physician order entry). To compare survey responders to non-responders, we obtained hospital level variables from the American Hospital Association Healthcare Data Viewer (http://www.ahadataviewer.com/quickreport/accessed May 2013), the Leapfrog Group (http://www.hospitalsafetyscore.org/accessed May 2013), and the American Nurses Credential Center (http://www.nursecredentialing.org/Magnet/FindaMagnetFacilityaccessed May 2013); these variables were: teaching status, locality (urban vs. rural), Magnet® status (a nursing excellence designation), number of beds, and Hospital Safety ScoreSM (a score that tracks complications and safety practices.
Severity adjustment
We obtained information from PHC4 on patient demographics information (e.g. age, race, sex, residence ZIP code), and admission diagnosis, admission source, discharge disposition. We calculated the Charlson comorbidity index(11) for each patient in the sample based on secondary ICD-9-CM diagnosis codes for the index hospital admission. In secondary analyses, we used the Elixhauser modification of Charlson co-morbidity scores as well as the MediQual predicted risk of death, a proprietary score available for PHC4 discharges before 2011.
Statistical analysis
We used nonparametric univariate hypothesis tests to compare survey responders and non-responders with respect to available facility-level characteristics. We used descriptive statistics to characterize the distribution of responses to questionnaire items across ICUs in our sample, and of patient-level characteristics among all patients in our final, linked dataset. We measured the association of selected ICU organizational characteristics with the study primary outcome using univariate hypothesis tests and via multivariable regression analysis to adjust for potential patient-level confounders. As an exploratory aim, we stratified the patient data by urgency of admission into emergent versus non-emergent cardiac surgical procedures as defined by PHC4. This secondary analysis was performed in order to assess if staffing characteristics differentially affected patient outcomes when patients were stratified by acuity of admission. Models utilized robust standard errors to account for clustering of patients withins ICUs.(12) The hospital was used as the level of clustering.
All data analyses were conducted with Stata IC, version 13 (StataCorp LLC, College Station, TX). We used p=0.05 as a cutoff for statistical significance.
Results
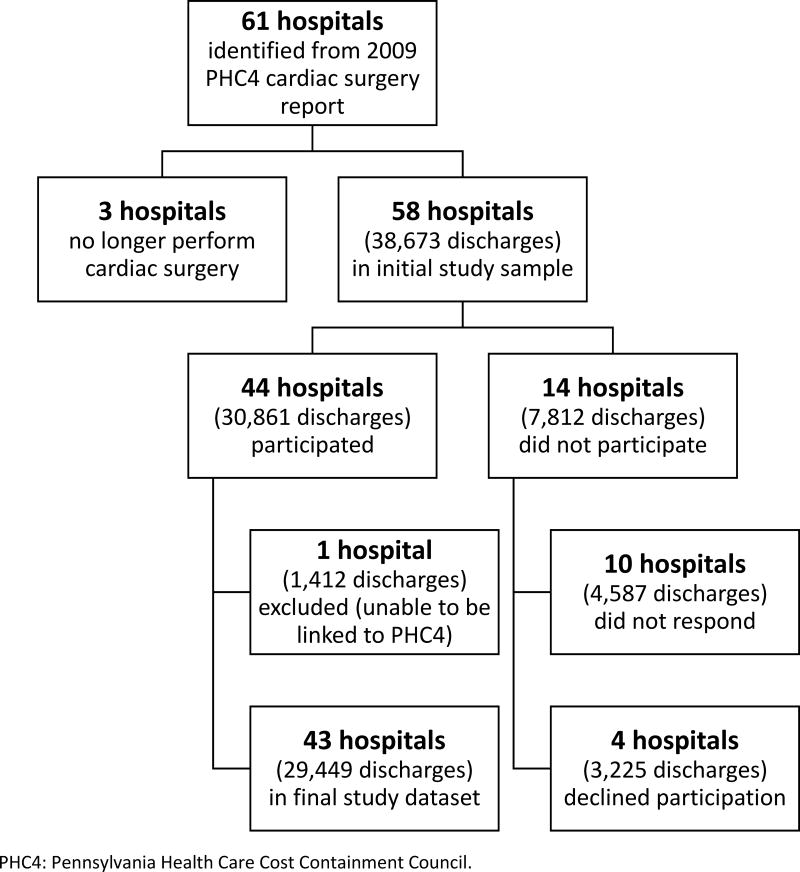
Based on information in PHC4 hospital performance reports, we identified 61 Pennsylvania hospitals that reported data on cardiac surgery outcomes; of these, three were excluded because the nurse managers of these ICUs indicated that their hospitals no longer performed cardiac surgery and one was excluded because it did not have a unique facility identifier in the PHC4 database. This left 57 potential participating hospitals for the facility survey. Of these, 43 (75.4%) provided responses to the facility survey (Figure 1). Responding and non-responding hospitals did not have statistically significant differences with respect to facility-level characteristics (Table 1). 27/43 (62.8%) of ICUs were located in teaching hospitals (Table 1), but only 8/27 of these ICUs (29.6% of those in teaching hospitals, or 18.6% of the total) had residents or fellows staffing the cardiac surgery ICU (Table 2). 16/43 ICUs exclusively admitted cardiac surgery patients, while the others admitted mixed surgical and medical-surgical populations. More than 75% of the ICUs reported using protocols for each one of the following indications: liberation from mechanical ventilation, management of sedation, therapeutic hypothermia after cardiac arrest, and central venous catheter insertion. Fewer than 50% of the ICUs, however, used protocols for low tidal volume ventilation in the setting of acute lung injury (Table 2).
Figure 1.
Table 1.
Facility-level and patient-level characteristics of Pennsylvania hospitals with cardiac surgery ICUs, grouped by survey response.
| Attribute | Value | Total | Responders | Non-responders | p-value | |
|---|---|---|---|---|---|---|
|
| ||||||
| Hospital characteristics | N=57 | N=43 (75.4%)* | N=14 (24.6%) | |||
|
| ||||||
| Hospital Safety ScoreSM | A | 20 (35.1%) | 17 (39.5%) | 3 (21.4%) | 0.561 | |
|
| ||||||
| B | 15 (26.3%) | 10 (23.3%) | 5 (35.7%) | |||
|
| ||||||
| C | 18 (31.6%) | 13 (30.2%) | 5 (35.7%) | |||
|
| ||||||
| D | 1 (1.8%) | 1 (2.3%) | 0 (0%) | |||
|
| ||||||
| missing | 3 (5.3%) | 2 (4.7%) | 1 (7.1%) | |||
|
| ||||||
| Teaching status | Major | 18 (31.6%) | 14 (32.6%) | 4 (28.6%) | 0.928 | |
|
| ||||||
| Minor | 17 (29.8%) | 13 (30.2%) | 4 (28.6%) | |||
|
| ||||||
| Non | 22 (38.6%) | 16 (37.2%) | 6 (42.9%) | |||
|
| ||||||
| Locality | Urban | 53 (93.0%) | 39 (90.7%) | 14 (100%) | 0.237 | |
|
| ||||||
| Rural | 4 (7.0%) | 4 (9.3%) | 0 (0%) | |||
|
| ||||||
| Magnet® status | Yes | 15 (26.3%) | 14 (32.6%) | 1 (7.1%) | 0.061 | |
|
| ||||||
| No | 42 (73.7%) | 29 (67.4%) | 13 (92.9%) | |||
|
| ||||||
| Number of beds | <250 | 17 (29.8%) | 14 (32.6%) | 3 (21.4%) | 0.727 | |
|
| ||||||
| 250–500 | 26 (45.6%) | 19 (44.2%) | 7 (50.0%) | |||
|
| ||||||
| >500 | 14 (24.6%) | 10 (23.3%) | 4 (28.6%) | |||
|
| ||||||
| Patient characteristics | N=37,261 | N=29,449 (79.0%) | N=7,812 (21.0%) | |||
|
| ||||||
| Age in years, median (IQR) | 68 (59–76) | 68 (59–76) | 67 (60–76) | 0.0158 | ||
|
| ||||||
| Race | White | 33,119 (88.9%) | 25,992 (88.3%) | 7,127 (91.2%) | 0.000 | |
|
| ||||||
| Black | 1,853 (5.0%) | 1,503 (5.1%) | 350 (4.5%) | |||
|
| ||||||
| Other | 2,289 (6.1%) | 1,954 (6.6%) | 335 (4.3%) | |||
|
| ||||||
| Ethnicity | Hispanic | 919 (2.5%) | 853 (2.9%) | 66 (0.8%) | 0.000 | |
|
| ||||||
| Non-Hispanic | 36,342 (97.5%) | 28,596 (97.1%) | 7,746 (99.2%) | |||
|
| ||||||
| Sex | Female | 12,101 (32.5%) | 9,503 (32.3%) | 2,598 (33.3%) | 0.098 | |
|
| ||||||
| Male | 25,160 (67.5%) | 19,946 (67.7%) | 5,214 (66.7%) | |||
|
| ||||||
| Admission source | Transfer | 4,337 (11.6%) | 3,778 (12.8%) | 559 (7.2%) | 0.000 | |
|
| ||||||
| Non-transfer | 32,924 (88.4%) | 25,671 (87.2%) | 7,253 (92.8%) | |||
|
| ||||||
| Insurance type (Primary)** | Medicare | 21,749 (58.4%) | 17,149 (58.2%) | 4,600 (58.9%) | 0.000 | |
|
| ||||||
| Medicaid | 2,402 (6.5%) | 1,939 (6.6%) | 463 (5.9%) | |||
|
| ||||||
| Commercial | 11,956 (32.1%) | 9,714 (33.0%) | 2,242 (28.7%) | |||
|
| ||||||
| Other | 876 (2.4%) | 444 (1.5%) | 432 (5.5%) | |||
|
| ||||||
| Uninsured | 278 (0.7%) | 203 (0.7%) | 75 (1.0%) | |||
|
| ||||||
| Charlson Comorbidity Index, median (IQR) | 1 (1–2) | 1 (1–2) | 1 (1–2) | 0.071 | ||
|
| ||||||
| Surgery type | CABG only | 22,191 (59.6%) | 17,321 (58.8%) | 4,870 (62.3%) | 0.000 | |
|
| ||||||
| Valve repair or replacement only | 9,626 (25.8%) | 7,854 (26.7%) | 1,772 (22.7%) | |||
|
| ||||||
| CABG and valve | 5.444 (14.6%) | 4,274 (14.5%) | 1,170 (15.0%) | |||
|
| ||||||
| Patient outcomes | ||||||
|
| ||||||
| Length of stay (LOS), days*** | ICU LOS | 0.000 | ||||
| Median (IQR) | 6 (3–10) | 6 (3–10) | 7 (4–11) | |||
| Mean ± SD | 8.15 ± 8.7 | 7.9 ± 8.9 | 9.0 ± 7.8 | |||
|
| ||||||
| Hospital LOS | 0.001 | |||||
| Median (IQR) | 8 (6–12) | 8 (6–12) | 8 (6–12) | |||
| Mean ± SD | 12.1 23.5 | 14.0 ± 26.1 | 10.1 ± 6.8 | |||
|
| ||||||
| Mortality | Death in 7 days from surgery | 544 (1.45%) | 431 (1.46%) | 113 (1.45%) | 0.911 | |
|
| ||||||
| Death in 30 days from surgery | 1,110 (2.98%) | 901 (3.06%) | 209 (2.68%) | 0.076 | ||
|
| ||||||
| In-hospital mortality | 925 (2.48%) | 738 (2.51%) | 187 (2.39%) | 0.571 | ||
CABG: coronary artery bypass grafting; SD: standard deviation; ICU: intensive care unit; IQR: interquartile rangePercentages do not all sum to 100% due to rounding error.
Hospital Safety Score is a quality performance grade conferred by the Leapfrog Group.
Magnet® status is an indicator of nursing excellence granted by the American Nurses Credentialing Center.
44 hospitals responded to our facility survey, but one was unable to be linked to PHC4 data with a unique identifier (it shared a facility code with another hospital). This hospital and its corresponding discharges were therefore excluded from analysis.
For discharges with more than one insurance type, a primary payer is designated in the Pennsylvania Health Care Cost Containment Council dataset.
Excludes patients who died during their hospitalization.
Table 2.
ICU-level characteristics of Pennsylvania cardiac surgery ICUs responding to survey instrument (n=43).
| Attributes | ICUs with attribute, n (%; 95% CI) |
|---|---|
| Structural Attributes | |
| ICU dedicated to cardiac surgery | 16 (37.2%; 23.0–53.3%) |
| NDNQI participation | 40 (93.0%; 80.9–98.5%) |
| Presence of protocols for: | |
| Low tidal volume ventilation for acute lung injury* (n=42) | 18 (42.9%; 27.7–59.0%) |
| Liberation from mechanical ventilation | 36 (83.7%; 69.3–93.2%) |
| Sedation management | 33 (76.7%; 61.4–88.2%) |
| Therapeutic hypothermia after cardiac arrest | 37 (86.0%; 72.1–94.7%) |
| Checklist for central line insertion* (n=42) | 41 (97.6%; 87.4–99.9%) |
| Respiratory therapists participate in daily rounds | 26 (60.5%; 44.4–75.0%) |
| Pharmacists participate in daily rounds | 23 (53.5%; 37.7–68.8%) |
| Presence of nurse practitioners or physician assistants | 37 (86.0%; 72.1–94.7%) |
| Telemedicine access (n=41) | 12 (29.3%; 16.1–45.5%) |
| Nursing Attributes | |
| >2/3 weekday nurses with 2+ years of experience* (n=41) | 25 (61.0%; 44.5–75.8%) |
| Nurses allowed to work 16-hour shift* (n=42) | 29 (69.0%; 52.9–82.4%) |
| >2/3 weekday nurses with BSN degree* (n=41) | 11 (26.8%; 14.2–42.9%) |
| Physician Attributes | |
| Presence of daytime intensivists** (n=39) | 21 (53.8%; 37.2–69.9%) |
| Presence of attending at night* (n=42) | 25 (59.5%; 43.3–74.4%) |
| If night attending present, presence of nighttime intensivist** (n=25) | 8 (18.6%; 8.4–33.4%) |
| Hospital has teaching affiliation | 27 (62.8%; 46.7–77.0%) |
| Fellows present in cardiac ICU | 7 (16.3%, 6.8–30.7%) |
| Interns or residents present in cardiac ICU | 8 (18.6%, 8.4–33.4%) |
ICU: intensive care unit; NDNQI: National Database of Nursing Quality Indicators
n<43 for these attributes due to missing data
Presence defined as some or all of attending physicians having critical care training.
None of the respondents reported significant changes in physician or nurse staffing schemes between 2009 and 2012. Slightly fewer than half the ICUs (48.8%, 21/43) had daytime attending intensivists. 60.5% of the ICUs (26/43) had attending physicians present in the hospital at night, but just 8 of these (18.6% of the total) had nighttime intensivists. In 20/43 ICUs (46.5%), attending intensivists did not staff ICUs during day or night.
Nurse BSN preparation was common: 11/42 (26.2%) reported that >2/3 of their nurses working weekday shifts had a BSN degree and 27/42 (64.3%) reported that between 1/3 and 2/3 of their ICU nurses working weekday shifts had a BSN degree. A small number of ICUs reported differences in nurse experience and education on nights and weekends; 6/42 ICUs (14.3%) had less experienced nurses on nights/weekends and 4/42 ICUs (9.5%) had a higher proportion of RNs with a BSN degree on nights/weekends. Nursing shift length was more uniform, with 41/43 (95.4%) ICUs reporting 12 hours as a standard shift length. In 29/43 ICUs (67.4%), however, nurses were allowed to work 16 hour shifts. Full survey response data are provided in Supplemental Digital Content 3.
38,673 hospital discharges involved CABG, valve, or combined CABG/valve surgeries from 2009 to 2011, all of which represent unique patients. Overall, 29,449 (76.1%) of these patients received care in hospitals responding to our facility survey. There were statistically significant differences in the patients cared for in responding versus non-responding hospitals (Table 1); patients in responding hospitals were more ethnically diverse, had a higher proportion of valvular surgeries, and had a higher proportion of commercial or other non-federal insurance type. However, there were no statistically significant differences in unadjusted outcomes for patients in responding versus non-responding hospitals.
Patients in the dataset combining facility and discharge information (n=29,449) had a median age of 68 years, were mostly white, and had mostly Medicare or commercial insurance (Table 1). Bivariate analyses revealed statistically significant associations between our primary outcome and multiple ICU-level variables; these included telemedicine access, nurse experience, and presence of residents or fellows (Table 3). However, these findings did not persist after adjustment for patient characteristics (Table 3). We repeated all reported analyses using both Elixhauser comorbidities and MediQual risk adjustment (for the subset of patients, n=12,907, with available MediQual scores); although precise odds ratios were different, the associations observed were similar.
Table 3.
Association between facility-level characteristics and odds of death in 30 days after cardiac surgery in bivariate and multivariable logistic regression models (n=29,449).
| Exposure Variable | Unadjusted OR (95% CI) | P-value | Adjusted OR (95% CI) | P-value |
|---|---|---|---|---|
| Structural attributes | ||||
| ICU dedicated to cardiac surgery | 1.05 (0.92–1.20) | 0.484 | 1.09 (0.84–1.42) | 0.502 |
| NDNQI participation | 0.82 (0.61–1.09) | 0.167 | 0.94 (0.71–1.23) | 0.644 |
| Protocols*: | ||||
| Low tidal volume ventilation** | 0.91 (0.79–1.04) | 0.153 | 0.92 (0.72–1.17) | 0.503 |
| Sedation management | 1.08 (0.93–1.26) | 0.290 | 1.29 (0.98–1.69) | 0.067 |
| Therapeutic hypothermia after cardiac arrest | 1.30 (1.03–1.63) | 0.025 | 1.19 (0.73–1.95) | 0.477 |
| Liberation from mechanical ventilation | 0.98 (0.79–1.21) | 0.840 | 0.89 (0.70–1.13) | 0.345 |
| Respiratory therapists participate in daily rounds | 0.89 (0.78–1.02) | 0.105 | 0.92 (0.70–1.22) | 0.571 |
| Pharmacists participate in daily rounds | 0.84 (0.73–0.96) | 0.012 | 0.89 (0.70–1.12) | 0.317 |
| Presence of nurse practitioners or physician assistants | 1.05 (0.82–1.34) | 0.715 | 1.00 (0.76–1.32) | 0.999 |
| Telemedicine access | 0.81 (0.70–0.95) | 0.007 | 0.87 (0.67–1.13) | 0.295 |
| Nursing attributes | ||||
| Proportion of nurses with <2 years ICU experience***: | ||||
| <1/3 (more experienced) | Referent | Referent | ||
| >1/3 (less experienced) | 1.18 (1.04–1.33) | 0.008 | 1.20 (0.97–1.47) | 0.090 |
| Proportion of nurses with BSN degree | ||||
| <1/3 (more experienced) | Referent | Referent | ||
| >1/3 (less experienced) | 1.13 (0.83–1.54) | 0.424 | 0.94 (0.76–1.17) | 0.593 |
| Physician attributes | ||||
| Presence of daytime intensivist | 1.21 (1.06–1.38) | 0.005 | 1.12 (0.89–1.40) | 0.351 |
| Nighttime attending staffing: | ||||
| No nighttime attending | Referent | Referent | ||
| Non-intensivist nighttime attending | 1.09 (0.94–1.26) | 0.255 | 0.91 (0.71–1.16) | 0.439 |
| Intensivist nighttime attending | 0.90 (0.74–1.09) | 0.268 | 0.85 (0.65–1.12) | 0.259 |
| Presence of interns or residents | 1.75 (1.51–2.04) | <0.001 | 1.34 (0.98–1.82) | 0.066 |
| Presence of fellows | 1.61 (1.39–1.87) | <0.001 | 1.25 (0.89–1.76) | 0.196 |
CI: confidence interval; OR: odds ratio. Multivariable models accounted for patient clustering within ICUs and controlled for patient age, sex, race, Charlson comorbidity score, insurance type, admission source, and surgery type. Odds ratios less than 1 indicate a lower risk of death in the 30 days after surgery.
Use of a protocol for central line insertion was excluded from multivariable analysis due to low numbers of ICUs not reporting use of this protocol type.
ICU uses a protocol for low tidal volumes in mechanically ventilated patients with acute respiratory distress syndrome.
Refers to nurses working during weekday shifts.
As part of an exploratory analysis to test whether acuity influenced the association between facility-level characteristics and short-term mortality, we separately analyzed patients admitted electively (n=16,214) and urgently or emergently (n=13,235) (Supplemental Digital Content 4). In the subgroup of patients admitted electively, adjusted models indicated statistically significantly lower odds of 30-day mortality associated with presence of nighttime intensivists (OR 0.70, 95% CI 0.49–1.00, p=0.047), and presence of a protocol for liberation from mechanical ventilation (OR 0.73, 95% CI 0.55–0.97, p=0.030), but higher odds of mortality associated with presence of interns and residents in the ICU (OR 1.59, 95% CI 1.06–2.40, p=0.026). In the subgroup of patients admitted for emergent procedures, 30-day mortality was associated with less experienced nurses (OR 1.25, 95% CI 1.01–1.54, p=0.037) (Supplemental Digital Content 5).
Of note, the transcatheter approach to valve replacement was introduced during the study period, although hospital coding for the procedure may not have reflected distinctions in surgical approach. Data on transcatheter valve replacement use were unavailable in the PHC4 dataset used for this project. To test whether the observed associations held true for non-transcatheter surgeries, we repeated analyses excluding valve-only procedures (combined CABG-valve surgeries would not have been performed with a transcatheter approach). Our findings were similar: while there were bivariate associations between facility-level variables and 30-day mortality, none of these associations persisted after adjustment (Supplemental Digital Content 6).
Discussion
In this study, we found variable organizational practices to be highly variable across Pennsylvania cardiac surgery intensive care units. We did not identify specific practices that were associated with 30-day mortality after risk adjustment in the full patient cohort. However, in patients admitted electively for CABG and/or valve surgery, one ICU-level variable (presence of nighttime intensivist) was associated with decreased mortality and two variables (presence of a nighttime non-intensivist physician dedicated to the ICU and presence of interns or residents) were associated with increased odds of mortality. In patients admitted urgently or emergently, less nurse experience was associated with increased odds of mortality. Finding associations between staffing and mortality in electively admitted patients may seem counterintuitive. We posit that mortality in emergently or urgently admitted patients may be driven more by acuity than by ICU staffing variables, which would explain finding associations only in electively admitted patients. This finding, based on exploratory analyses, will need to be addressed in future studies.
The introduction of transcatheter approaches from 2009–2012 posed a challenge to this analysis. According to a 2015 study published in the Journal of the American College of Cardiology, between 2011 and 2013, there were 417 centers performing transcatheter aortic valve replacement (TAVR) on Medicare beneficiaries in the United States.(13) The median procedures per center was 17 (range 2–46) over the three-year period, which is after the procedures in our database. Given that there were over 9,600 valve procedures in our dataset, it is likely that the TAVR procedures represent an extremely small component of these. We do recognize that the TAVR patients may have different mortality rates, though the current literature is conflicting (13, 14). Still, the volume of TAVR procedures in the years of study were likely small enough to not have significantly skewed our calculated mortality rates. To address this issue fully, as stated in the results, we still performed an additional analysis excluding valve only procedures, finding no statistically significant associations between facility-level variables and mortality.
Our findings demonstrate that cardiac ICUs in Pennsylvania have devised myriad strategies to meet the challenge of caring for patients recovering from cardiac surgery. For example, many of these ICUs have nurse practitioners and/or physician assistants, but some also have residents and fellows. These clinicians have overlapping scope of practice in many institutions, and further research is needed to understand the roles that they play in any given setting. The presence of other clinicians, including attending physicians, pharmacists, and respiratory therapists, was similarly variable. Although the effects that these staffing decisions may have on patient outcomes remains unclear, these decisions certainly have different cost profiles. Moving forward, studies of cost-effectiveness would be useful to inform efficient choices about staffing and resource use.
This work adds to the growing literature about associations between ICU staffing practices and patient outcomes. Recent data suggest that ICU staffing decisions may have some effect on patient outcomes.(1, 2, 4, 15) At the same time, the mounting number of studies finding no association(16–18) or an inconsistent association(3) suggest that there are other factors at play modulating the effect that ICU staffing may have on patient outcomes. Alternative study designs, such as qualitative or mixed methods approaches, could be used to contextualize the numeric associations observed in our and other studies. The findings reported here may inform future research by aiding in the generation of testable hypotheses about organizational practices and patient outcomes. Especially intriguing is the idea that patients admitted electively may be differently impacted by organizational practices than those admitted urgently or emergently; this finding has implications for care networks and efforts to regionalize specialty care.
This study had several important limitations. First, our study sample was drawn from a single state, which potentially limits generalizability. Second, facility staffing surveys and clinical outcome data were recorded at slightly different time points, creating the potential for misclassification. However, we asked nurse managers whether ICU practices changed in the 2009–2011 period, and all respondents denied significant disruptions or changes in organizational practices. Third, as we were unable to obtain data from all Pennsylvania cardiac surgery units, our findings could be influenced by non-response bias; however, we obtained a high response rate (75.4%) and observed no significant differences between responders and non-responders across a range of hospital characteristics. Fourth, although we administered a detailed survey, we do not have complete information about availability of physicians who were not “in-house”. We did ask about nighttime non-ICU in-house physician availability as well the use of telemedicine (Supplemental Digital Content 1), which were not associated with 30-day mortality. Fifth, we chose to survey nurse managers because we believed they would most accurately describe nursing attributes, and because all ICUs in our sample did not have physician medical directors. Even though we pilot tested our instrument, there may be remaining measurement error related to individual respondents’ knowledge and interpretation of our survey questions. Sixth, although there were no statistically significant differences in responding versus non-responding hospitals, we did note that there was a higher proportion of Magnet hospitals in the responding group. The importance of this is unclear, but there may be unmeasured structural differences between our responding and non-responding hospitals that may attenuate our ability to detect associations between the variables we studied. Additionally, there were differences between responders and non-responders with respect to patient-level characteristics (e.g. race, ethnicity, admission source, length of stay). These differences raise the concern that non-response bias may affect the validity of our analysis. However, our response rate (75.4%), reflecting 79.0% of cardiac surgery admissions, combined with broad representation of hospital types and geographic areas, increases our confidence that we have been able to provide a reasonable depiction of post-cardiac surgery ICU care. Additionally, there were no statistically significant differences in mortality between responding and non-responding hospitals, which increases confidence that the patient cohorts, while statistically significantly different in other respects, may have similar risk of death after cardiac surgery. Finally, our use of administrative data limited our ability to risk adjust beyond Elixhauser comorbidities. Although PHC4 does collect granular clinical data about cardiac surgery patients, these data are not available to researchers. Subgroup analyses restricted to the group of patients with MediQual predicted risk of death scores revealed similar findings as the overall analysis. Nevertheless, there is the possibility of residual confounding attributable to patient illness or other characteristics. As such, these results should not be interpreted as implying causality.
Despite these limitations, our study has several strengths. We collected detailed ICU-level data from most of the ICUs in Pennsylvania that provide care to cardiac surgical patients. The bivariate associations between ICU-level characteristics and patient outcomes, while not maintained in a multivariable model, are nonetheless provocative and may enable generation of hypotheses about the impact that policies and procedures may have on patient outcomes. Additionally, we linked this ICU-level data to more than 29,000 patient discharges, allowing us to generate a comprehensive picture of routine cardiac surgical care in Pennsylvania.
In conclusion, Pennsylvania cardiac surgery ICUs have variable structures, care practices, and clinician staffing, but these do not appear to be associated with 30-day mortality after cardiac surgery. When patients are stratified by urgency of admission, several ICU-level characteristics were associated with outcomes, suggesting that acuity may influence the impact that ICU organizational characteristics has on patients’ outcomes. Future research is needed to understand the relationship between cardiac ICU staffing and patient outcomes.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge the contributions of the following individuals in the design and execution of the work described: Deelan Ayhan (data collection), Jill Gehman, RN, BSN, CCRN (study design), George Iyoob, BSN, MHA (study design), John McConnell, MD (study design), Victoria Rich, PhD, RN, FAAN (study design), Kelly Wiltse Nicely, PhD, CRNA (study design).
Financial support: The work reported herein was funded by the National Heart, Lung, and Blood Institute of the National Institutes of Health (Grant number T32 HL098054-03, PI: David Asch), which supported Meghan Lane-Fall. Meghan Lane-Fall currently receives research funding from the following: University of Pennsylvania Provost’s Office and the Robert Wood Johnson Foundation. Mark Neuman receives financial support from the National Institutes of Health (National Institute of Aging) and the Patient-Centered Outcomes Research Institute.
Dr. Lane-Fall’s institution received funding from the National Institutes of Health (NIH), National Heart, Lung, and Blood Institute (NHLBI), Robert Wood Johnson Foundation Harold Amos Medical Faculty Development Program, Anesthesia Patient Safety Foundation, National Institute on Minority Health and Health Disparities Loan Repayment Program; she disclosed receiving honoraria for serving as a visiting professor at the following institutions: Massachusetts General Hospital (2014), Stanford University (2014), Cornell University (2014), University of Alabama at Birmingham (2014), Vanderbilt University (2016); and she received support for article research from the NIH. Dr. Fleisher’s institution received funding from NHLBI T32 grant to first author, and he received support for article research from the NIH. Dr. Neuman received support for article research from the NIH.
Footnotes
Location where work performed: Perelman School of Medicine, University of Pennsylvania
Copyright form disclosure: The remaining authors have disclosed that they do not have any potential conflicts of interest.
Contributor Information
Meghan B. Lane-Fall, Department of Anesthesiology and Critical Care, Perelman School of Medicine, University of Pennsylvania; Penn Center for Perioperative Outcomes Research and Transformation; Penn Center for Healthcare Improvement and Patient Safety; Leonard Davis Institute of Health Economics, University of Pennsylvania; Christiana Care Health System Value Institute; Robert Wood Johnson Foundation Harold Amos Medical Faculty Development Program, Postal address: 309 Blockley Hall, 423 Guardian Drive, Philadelphia, PA 19104 USA, Meghan.Lane-Fall@uphs.upenn.edu, Telephone: +1-215-573-7399, Facsimile: +1-215-662-7106.
Tara S. Ramaswamy, Perelman School of Medicine, University of Pennsylvania; Philadelphia, PA, USA, TRamaswamy34@gmail.com.
Sydney E. S. Brown, Department of Anesthesiology and Critical Care, Perelman School of Medicine, University of Pennsylvania; Philadelphia, PA, USA, Sydney.Brown@uphs.upenn.edu.
Xu He, Case Western Reserve University School of Medicine; Cleveland, OH, USA, HeXu927@gmail.com.
Jacob T. Gutsche, Department of Anesthesiology and Critical Care, Perelman School of Medicine, University of Pennsylvania; Philadelphia, PA, USA, Jacob.Gutsche@uphs.upenn.edu.
Lee A. Fleisher, Department of Anesthesiology and Critical Care, Perelman School of Medicine, University of Pennsylvania; Penn Center for Perioperative Outcomes Research and Transformation; Leonard Davis Institute of Health Economics; National Quality Forum; Philadelphia, PA, USA, Lee.Fleisher@uphs.upenn.edu.
Mark D. Neuman, Department of Anesthesiology and Critical Care, Perelman School of Medicine, University of Pennsylvania; Penn Center for Perioperative Outcomes Research and Transformation; Leonard Davis Institute of Health Economics; Philadelphia, PA, USA, Mark.Neuman@uphs.upenn.edu.
References
- 1.Pronovost PJ, Jenckes MW, Dorman T, et al. Organizational characteristics of intensive care units related to outcomes of abdominal aortic surgery. J Am Med Assoc. 1999;281(14):1310–1317. doi: 10.1001/jama.281.14.1310. [DOI] [PubMed] [Google Scholar]
- 2.Kahn JM, Brake H, Steinberg KP. Intensivist physician staffing and the process of care in academic medical centres. Qual Saf Health Care. 2007;16(5):329–333. doi: 10.1136/qshc.2007.022376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wallace DJ, Angus DC, Barnato AE, et al. Nighttime intensivist staffing and mortality among critically ill patients. N Engl J Med. 2012;366(22):2093–2101. doi: 10.1056/NEJMsa1201918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pronovost PJ, Angus DC, Dorman T, et al. Physician staffing patterns and clinical outcomes in critically ill patients: A systematic review. J Am Med Assoc. 2002;288(17):2151–2162. doi: 10.1001/jama.288.17.2151. [DOI] [PubMed] [Google Scholar]
- 5.Burnham EL, Moss M, Geraci MW. The case for 24/7 in-house intensivist coverage. Am J Respir Crit Care Med. 2010;181(11):1159–1160. doi: 10.1164/rccm.201004-0651ED. [DOI] [PubMed] [Google Scholar]
- 6.Garland A, Gershengorn HB. Staffing in ICUs: Physicians and alternative staffing models. Chest. 2013;143(1):214–221. doi: 10.1378/chest.12-1531. [DOI] [PubMed] [Google Scholar]
- 7.Kahn JM, Matthews FA, Angus DC, et al. Barriers to implementing the Leapfrog Group recommendations for intensivist physician staffing: A survey of intensive care unit directors. J Crit Care. 2007;22(2):97–103. doi: 10.1016/j.jcrc.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 8.Pronovost P, Thompson DA, Holzmueller CG, et al. Impact of the Leapfrog Group's intensive care unit physician staffing standard. J Crit Care. 2007;22(2):89–96.e24. doi: 10.1016/j.jcrc.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 9.Engelman RM, Rousou JA, Flack JE, Iii, et al. Fast-track recovery of the coronary bypass patient. The Annals of Thoracic Surgery. 1994;58(6):1742–1746. doi: 10.1016/0003-4975(94)91674-8. [DOI] [PubMed] [Google Scholar]
- 10. [cited 2013 5/22/2013];AHA Healthcare DataViewer. Available from: http://www.ahadataviewer.com/
- 11.Charlson ME, Pompei P, Ales KA, et al. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 12.White H. A Heteroskedasticity-Consistent Covariance Matrix Estimator and a Direct Test for Heteroskedasticity. Econometrica. 1980;48(4):817–838. [Google Scholar]
- 13.Murugiah K, Wang Y, Desai NR, et al. Hospital Variation in Outcomes for Transcatheter Aortic Valve Replacement Among Medicare Beneficiaries, 2011 to 2013. Journal of the American College of Cardiology. 2015;66(23):2678–2679. doi: 10.1016/j.jacc.2015.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hermiller JB, Jr, Yakubov SJ, Reardon MJ, et al. Predicting Early and Late Mortality After Transcatheter Aortic Valve Replacement. J Am Coll Cardiol. 2016;68(4):343–352. doi: 10.1016/j.jacc.2016.04.057. [DOI] [PubMed] [Google Scholar]
- 15.Pronovost PJ, Dang D, Dorman T, et al. Intensive care unit nurse staffing and the risk for complications after abdominal aortic surgery. Effective clinical practice : ECP. 2001;4(5):199–206. [PubMed] [Google Scholar]
- 16.Kerlin MP, Small DS, Cooney E, et al. A randomized trial of nighttime physician staffing in an intensive care unit. N Engl J Med. 2013;368(23):2201–2209. doi: 10.1056/NEJMoa1302854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wilcox ME, Harrison DA, Short A, et al. Comparing mortality among adult, general intensive care units in England with varying intensivist cover patterns: a retrospective cohort study. Crit Care. 2014;18(4):1–12. doi: 10.1186/s13054-014-0491-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Levy MM, Rapoport J, Lemeshow S, et al. Association between Critical Care Physician Management and Patient Mortality in the Intensive Care Unit. Ann Intern Med. 2008;148(11):801–809. doi: 10.7326/0003-4819-148-11-200806030-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.