Abstract
Objective
Clinical Assessment Interview for Negative Symptoms (CAINS) has recently been developed to improve measurement of negative symptoms in schizophrenia. We performed a multi-center study to validate the Korean version of the CAINS (CAINS-K) and explore potential cultural variation.
Methods
One hundred eighty schizophrenia patients diverse in demographic and illness profile were recruited from four centers in Korea. Along with the CAINS-K, the Scale for the Assessment of Negative Symptoms (SANS), Brief Psychiatric Rating Scale (BPRS), Calgary Depression Scale for Schizophrenia (CDSS), a self-report measure of behavioral inhibition and activation (BIS/BAS) and neurocognitive tasks were administered to verify external validities.
Results
The CAINS-K showed high internal-consistency (0.92) and inter-rater reliability (0.77). Exploratory Factor Analysis replicated a two-factor structure of the original scale including motivation/pleasure and expression deficits dimensions. Korean patients tended to report lower pleasure compared to American patients in the prior study. The CAINS-K showed an adequate convergent validity with the SANS, negative symptoms of the BPRS, and BAS. A divergent validity was supported as the CAINS-K showed zero or only weak correlations with other symptoms of the BPRS, depression from the CDSS, and neurocognitive tasks.
Conclusion
The CAINS-K demonstrated high internal consistency and adequate external validities, and is expected to promote studies on negative symptoms in Korean patients with schizophrenia.
Keywords: Clinical Assessment Interview for Negative Symptoms, Negative symptoms, schizophrenia, Validity, Measurement
INTRODUCTION
Negative symptoms are a fundamental feature of schizophrenia considered independent from positive and disorganized symptoms.1 Current understanding of this symptom cluster acknowledges that it consists of multiple domains including blunted affect, alogia, anhedonia, amotivation, and asociality.2 They are observed from prodromal to chronic stage and increasingly recognized as a major contributor to functional impairments of people with schizophrenia over the past decades.3 Nevertheless, negative symptoms are known to be resistant to available treatment options; a recent meta-analysis concluded that effectiveness of most treatments on negative symptoms did not achieve clinically significant improvements.4 Therefore, growing efforts are made to advance knowledge about this symptomatology as well as develop better treatment.
One of these efforts is to improve measurement of negative symptoms.2 First-generation measurements of negative symptoms such as the Scale for the Assessment of Negative Symptoms (SANS) and Positive and Negative Syndrome Scale (PANSS) have been acknowledged with several problems.2,5 First, it has been pointed out that SANS and PANSS have several items which are thought to be irrelevant with current understandings of negative symptoms construct. For example, cognitive items such as difficulty with abstract thinking and stereotyped thinking are included in PANSS, and inappropriate affect and attentional disturbances in SANS.2 Second, SANS and PANSS do not cover all domains of negative symptoms currently recognized; PANSS lacks a measure of anhedonia while SANS contains it but does not distinguish consummatory and anticipatory aspects of pleasure, the latter of which has been shown to be more relevant to schizophrenia.6 Last, the rating of negative symptoms typically relies on outward behaviors rather than probing internal experience of motivation and pleasure, leading to a measurement of functioning rather than negative symptoms themselves.5
Second-generation assessments of negative symptoms including Clinical Assessment Interview for Negative Symptoms (CAINS) and Brief Negative Symptoms Scale (BNSS) were developed in response to the necessity for new measurements of this symptom, addressing above-mentioned problems of existing measures. They were developed to cover a wide range of facets of negative symptoms from anhedonia, avolition, asociality, which are often grouped as a motivation deficits dimension, to alogia and blunted affect, an expression deficits dimension. They also distinguish between consummatory and anticipatory aspects of pleasures and include a direct assessment of internal experiences of pleasure and motivation. These newer measurements were developed through iterative and empirical processes and demonstrated high external validity, internal consistency, test-retest reliability, and inter-rater reliability.7,8,9 Factor analyses have supported the two-factor structure of these assessments, i.e., motivation and expression dimensions,8,9,10,11 with one notable exception reporting three components underlying BNSS.12
The aim of the current study was to examine the psychometric properties of the Korean version of the CAINS (CAINS-K) in a large outpatient sample with schizophrenia. Currently, the CAINS has not been translated into Korean, preventing its wide use in this population. We expect that the CAINS-K would exhibit high internal consistency as well as good convergent and divergent validities. As the two-factor structure of the CAINS has been supported in several non-English speaking populations including Spain, Germany, and China,10,11,13 we hypothesized that two-factor structure would be replicated in a Korean sample. Finally, we were also interested in whether cultural variations found in a preliminary Chinese version of the CAINS also exists in the CAINS-K.
METHODS
Participants
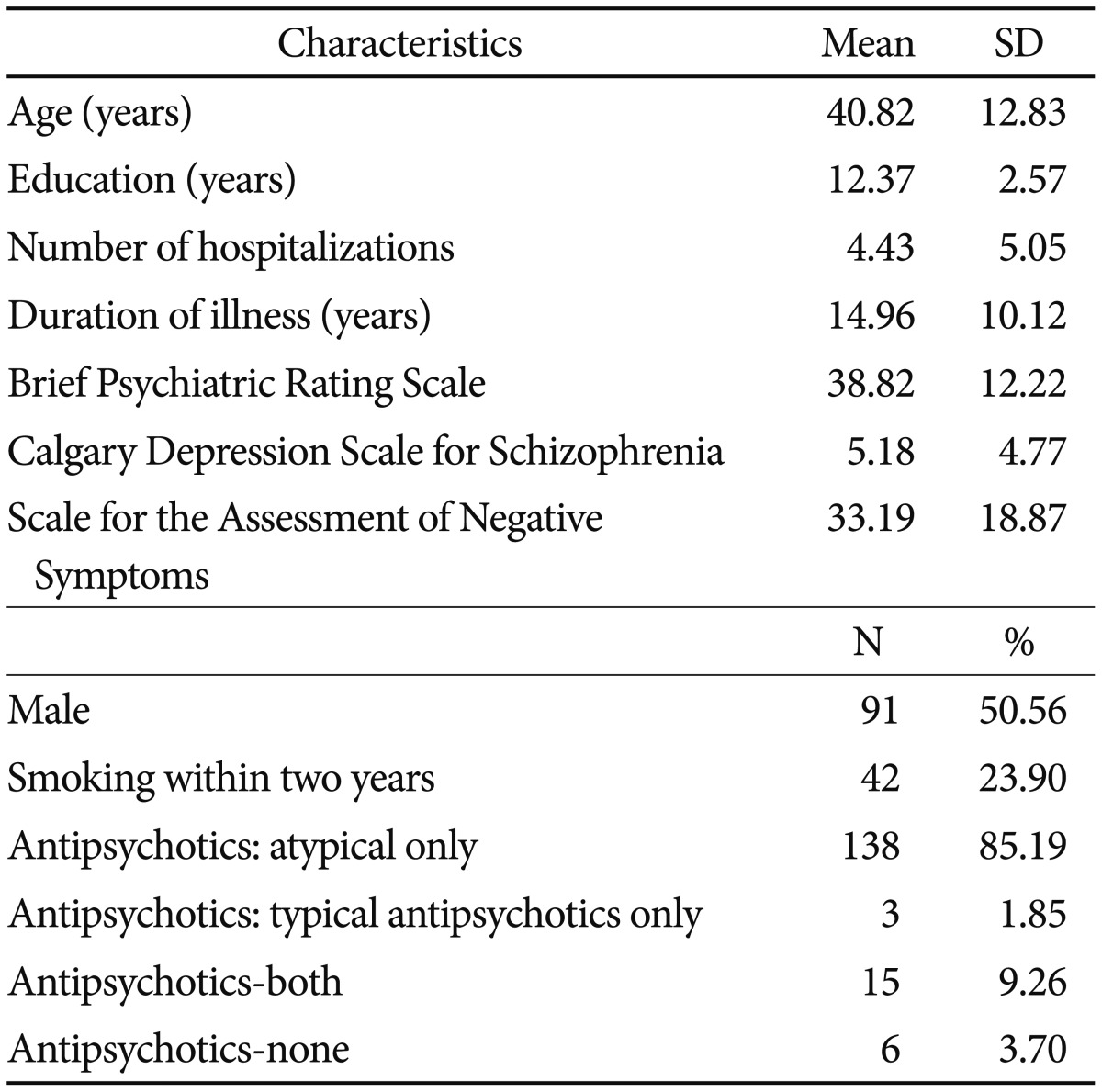
The total sample included 180 patients with schizophrenia recruited from outpatient clinics at four sites (Inje University Ilsan Paik hospital, Yong In mental hospital, Hallym University Kangnam Sacred Heart Hospital, and Korea University). Diagnoses were made by psychiatrists using the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID; First, Spitzer, Gibbon Williams14). Exclusion criteria included: 1) history of head injury or electro-convulsive treatment, 2) comorbid substance dependence or abuse in past three months, 3) serious medical conditions, and 4) low intelligence without the ability to understand instructions presented in the study. Demographic characteristics of participants are presented in Table 1. All participants gave written informed consent. The study was approved by ethics committees of the Institutional Review Board at all four sites (Inje University Ilsan Paik Hospital, Yong In Mental Hospital, Hallym University Kangnam Sacred Heart Hospital, Korea University).
Table 1. Demographic and clinical characteristics of the sample (N=180).
Measures
Clinical Assessment Interview for Negative Symptoms
The Clinical Assessment Interview for Negative Symptoms (CAINS) is a 13-item standardized interview that assesses the presence and severity of negative symptoms.8 It provides comprehensive and descriptive interview probes and anchor points. All items are rated on a five-point scale from 0 (no impairment) to 4 (severe deficit). The CAINS consists of two subscales which measure motivation and pleasure (MAP) and expression (EXP) deficits, respectively. The CAINS-MAP assesses current and anticipatory motivation and pleasure for social, vocational, and recreational activities, while the CAINS-EXP measures facial, vocal, and bodily expressions of emotion.
Other symptoms measure
Brief Psychiatric Rating Scale (BPRS15) was administered to assess positive, negative, mood, and agitation symptoms of schizophrenia. Negative symptoms were also assessed with the Scale for the Assessment of Negative Symptoms (SANS1) which provides a wide array of negative symptoms and thus is suitable to establish external validity of the CAINS. Calgary Depression Scale for Schizophrenia (CDSS16) was included to measure depressive symptoms of schizophrenia. Negative symptoms and depression often share some phenomenological features such as anhedonia and amotivation,16 therefore it is important to accurately measure negative symptoms construct distinct from depression. Cronbach's alphas of the BPRS and SANS were found to be 0.85 and 0.95, respectively, in the current study.
Cognitive tests
To examine a potential relationship between negative symptoms and neuro-cognitions, three tests measuring cognitive functions known to be largely impaired in people with schizophrenia were administered: Coding, Trail-Making Test-B (TMT-B), and verbal fluency task. The Coding test measures processing speed, short-term visual memory, and visual-motor coordination in schizophrenia,17 whereas the performance of TMT-B has been related to executive functions such as set-shifting ability.18 Verbal fluency task has been related to disorganized semantic system, altered psychomotor speed, and fronto-striatal dysfunction.19,20
Behavioral Inhibition/Behavioral Activation Scales
Consistent with the original CAINS study, Behavioral inhibition and activation (BIS/BAS) scale was included to explore potential relationships between negative symptoms and neural motivation systems in schizophrenia.21 BIS/BAS includes 20 items with a 4-point Likert-type scale to assess sensitivity of approach and avoidance motivation. It has four subscales: behavioral inhibition, reward responsiveness, drive, and fun-seeking. We used an aggregated score of three BAS subscales (reward responsiveness, drive, and fun-seeking). Cronbach's alphas of the BIS and BAS were 0.85 and 0.71, respectively, in the current study.
Procedure
The CAINS was translated into Korean by two researchers fluent in English and Korean (LSH and LJS) with prior agreement from developers of the original scale. A final consensus version was discussed in a panel with clinically experienced colleagues and was then back-translated into English by one translator (LJH). The translation was compared with the original English version, and no further changes were deemed necessary. The CAINS manual was also translated into Korean (Supplementary Material 1 in the online-only Data Supplement).
Five psychiatrists and five clinical psychologists rated psychiatric symptoms of participants using the CAINS, BPRS and SANS, and also administered CDSS, cognitive tests, and BIS/BAS. With regard to symptoms assessments, they attended a training workshop (1 day, approximately 8 hours) to learn about the administration and scoring of the CAINS, BPRS, and SANS. This workshop included a review of the CAINS, joint assessment of six video-recorded patient interviews, and evaluation of agreements with gold standard ratings of video-taped materials.
Statistical analysis
We first calculated Cronbach's alpha of 13 items along with item-total correlations to ensure items are internally consistent. Inter-rater agreement was also calculated. Then, a factor structure of the CAINS-K was identified through Exploratory Factor Analysis (EFA) with principal factoring and promax rotation as two factors are not assumed to be orthogonal.8 Last, two-tailed Pearson correlations between the CAINS-K and external variables were computed to examine convergent and divergent validity. All statistical analyses were conducted using IBM SPSS 23.0.
RESULTS
Descriptive statistics
The mean total score of the CAINS-K was 23.70 with standard deviation (SD) 10.65. The means and SDs of the CAINS-K motivation and expression subscales were 18.51 (7.99) and 5.06 (3.58), respectively.
Internal consistency
Internal consistencies of the CAINS-K subscales (MAP and EXP) and total score were 0.91, 0.89, and 0.92, respectively. All items showed acceptable item-total correlations from 0.55 to 0.73 (Supplementary Material 2 in the online-only Data Supplement). Deletion of no items yielded higher Cronbach's alphas.
Inter-rater agreement
Inter-rater reliability was obtained by calculating intraclass correlation coefficient (single measure) using the PASW 18.0 and found to be 0.77.
Factor structure
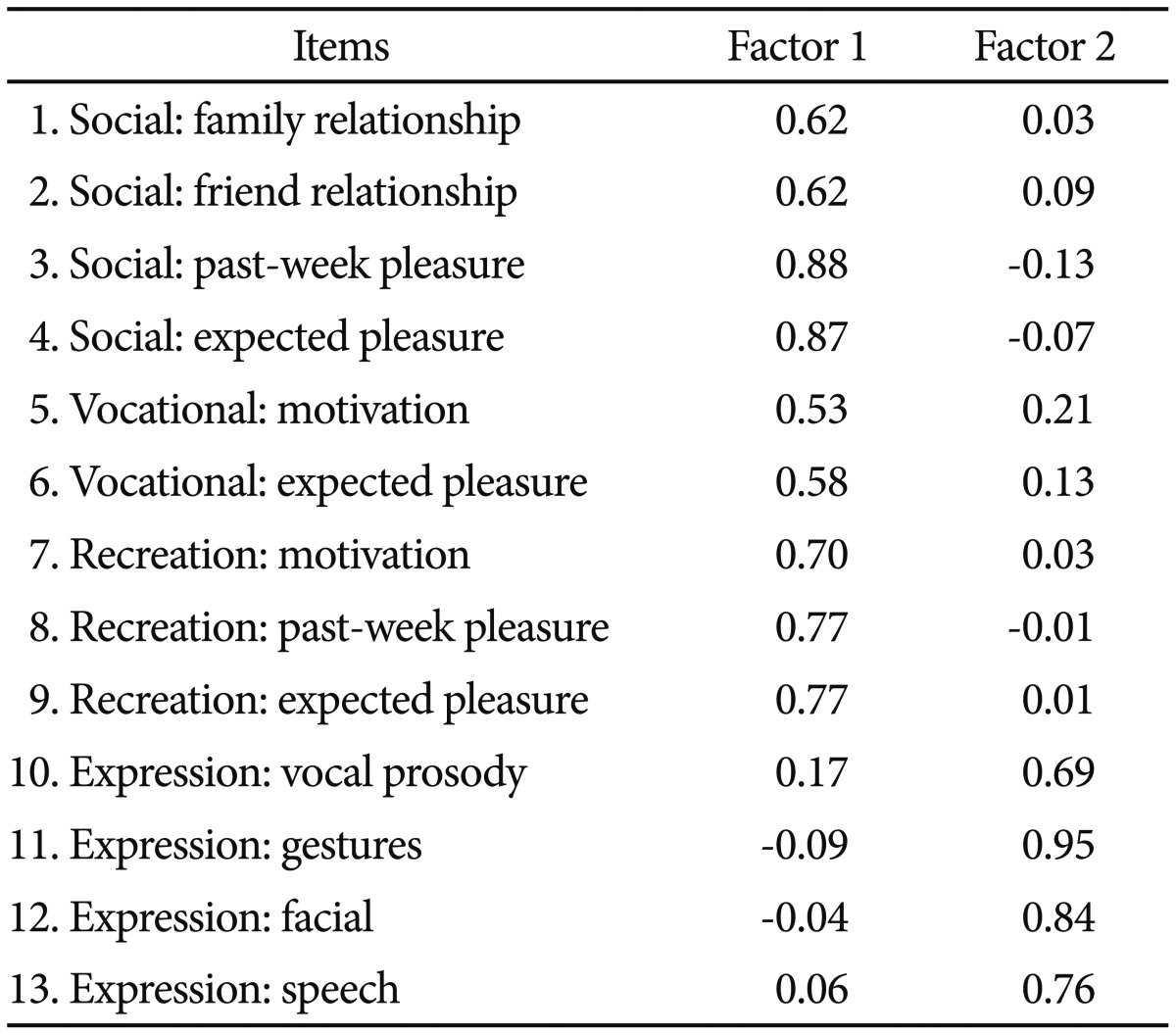
We examined the factor structure of the CAINS-K by using an EFA.8,10,11,13 Kaiser-Meyer-Olkin was 0.88, χ2=1567.23, df=78, p<0.001, indicating our data was suitable for the EFA. All items showed communalities higher than 0.40, therefore, all items were retained. Visual inspection of a scree plot indicated a two-factor structure with the same item composition with that from other studies,8,10,11 explaining 63.64% of the total variance. The first factor was motivation and pleasure deficits dimension and the second factor was expression deficits dimension, each of which explained 49.92% and 13.72% of the total variance, respectively (Table 2).
Table 2. Two-factor structure of the CAINS items.
Pattern matrix was reported. CAINS: Clinical Assessment Interview for Negative Symptoms
Effects of gender
We tested whether there were gender differences in the CAINS-K total and subscale scores. Independent samples t-tests indicated no gender differences in MAP, EXP, and total score of the CAINS-K (p>0.05).
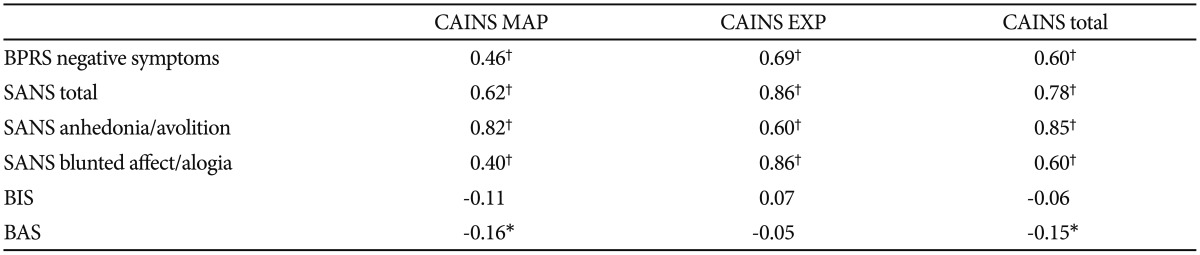
Convergent validity
To examine convergent validity, correlations of CAINS-K total and subscale scores with SANS total and subscale scores, BPRS negative symptoms, BIS and BAS scores were computed (Table 3). CAINS-K total score was significantly and positively correlated with total scores of SANS (r=0.78, p<0.001) and negative symptoms scores of BPRS (r=0.60, p<0.001). It also showed a small but significant negative correlation with the BAS (r=-0.15, p<0.05).
Table 3. Convergent validity of the CAINS (N=180).
*p<0.001, †p<0.05. BPRS: Brief Psychiatric Rating Scale, SANS: Scale for the Assessment of Negative Symptoms, CAINS MAP: Motivation and pleasure factor in the CAINS, CAINS EXP-Expression factor in the CAINS. CAINS: Clinical Assessment Interview for Negative Symptoms, BIS: Behavioral Inhibition System, BAS: Behavioral Activation System
For CAINS-K subscales, the MAP score was significantly and positively correlated with BPRS negative symptoms (r=0.46, p<0.001), SANS anhedonia/avolition (r=0.82, p<0.001), SANS blunted affect/alogia (r=-0.40, p<0.001), and negatively with the BAS (r=0.16, p<0.05). The correlation between MAP and SANS anhedonia/avolition was significantly greater than that between MAP and SANS blunted affect/alogia(z=8.45, p<0.001). The EXP was significantly and positively correlated with BPRS negative symptoms (r=0.69, p<0.001), SANS anhedonia/avolition (r=0.60, p<0.001), and SANS blunted affect/alogia (r=0.86, p<0.001). The correlation between the EXP and SANS blunted affect/alogia was significantly greater than that with the EXP and SANS anhedonia/avolition (z=-6.42, p<0.001).22
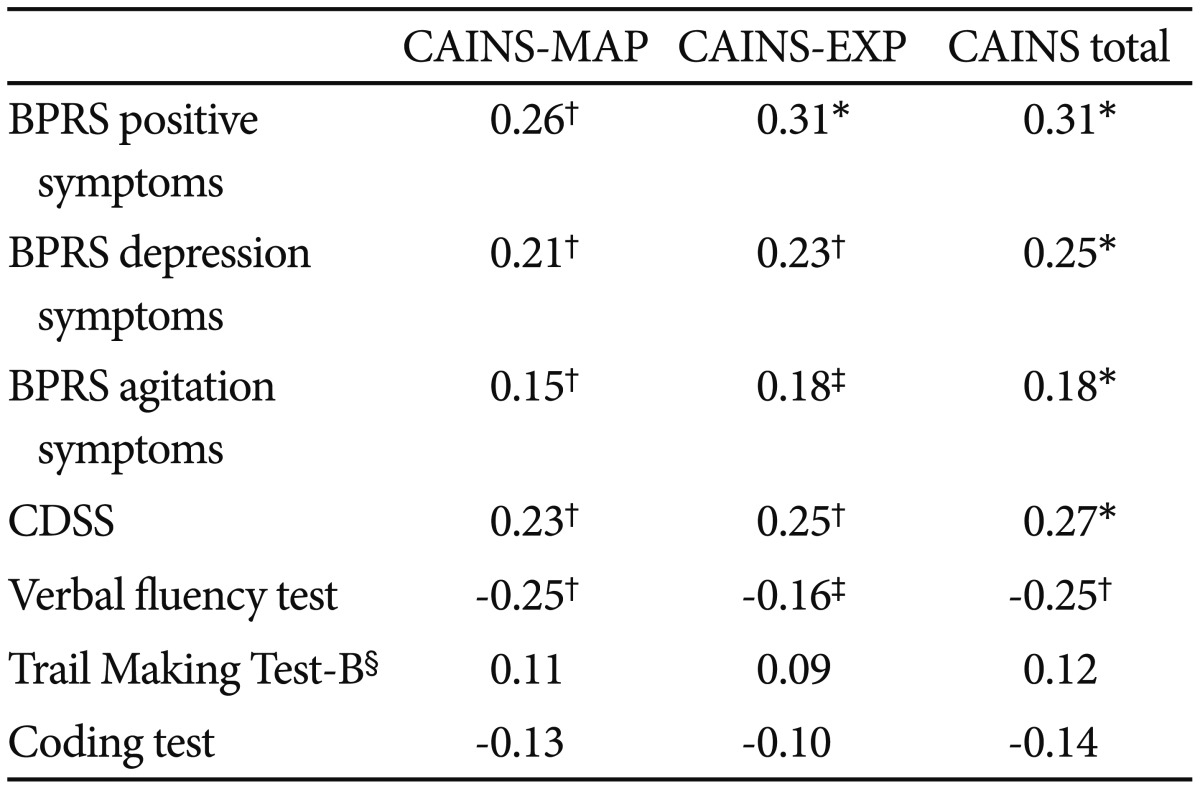
Discriminant validity
Discriminant validity was examined by calculating correlations of the CAINS-K with positive, depression, and agitation symptoms of BPRS, CDSS total score, and performances of cognitive tasks (Table 4). Only small sized correlations were found between the CAINS-K and BPRS positive, depression, agitation symptoms, and CDSS (0.15 to 0.31). Among neurocognitive tasks, only the performance of verbal fluency task was negatively correlated with CAINS-K total and subscales scores with small magnitude (-0.16 to -0.25).
Table 4. Discriminant validity of the CAINS (N=180).
*p<0.001, †p<0.01, ‡p<0.05, §n=169 and 177 for Trail Making Test-B and Coding Test, respectively. CAINS MAP: motivation and pleasure factor in the CAINS, CAINS EXP: expression factor in the CAINS. BPRS: Brief Psychiatric Rating Scale, CDSS: Calgary Depression Scale for Schizophrenia, CAINS: Clinical Assessment for Negative Symptoms, BIS: Behavioral Inhibition System, BAS: Behavioral Activation System
DISCUSSION
The goal of the present study was to validate a Korean version of the CAINS with a large sample from Korean population with schizophrenia and to promote its use in international trials of treatment and mechanism studies of negative symptoms. In the current study, the CAINS-K showed an excellent internal consistency, inter-rater reliability, and adequate convergent and discriminant validities as in the original scale and several non-English versions of the CAINS.8,10,11,13
Our sample consisted of outpatients diverse in age, symptoms, and illness onset and duration. Most of them were symptomatically stable and taking antipsychotic medications, mostly atypical ones. Their age, education level, and the severity of psychiatric symptoms were comparable to those in the original studies.7,8 However, our samples included an almost equal number of both sexes unlike the original study8 which included more male than female participants. Participants of the current study also reported a fewer number of hospitalizations during life time than those in the original study.
We replicated the two-factor structure, i.e., MAP and EXP, respectively, with the same composition of items for each factor as the original study.8 Unlike previous studies of non-English versions of the CAINS in which some items in one factor were also loaded on the other factor,11,13 current results showed a relatively clear-cut two-factor structure. Our results were also divergent from the study on the Chinese version of theCAINS which reported some cultural variations in item compositions of the two-factor structure such that motivation for family relationship (item 1) and vocational activities (item 5) were loaded on the EXP factor instead of being loaded on the MAP factor. However, it was a preliminary result and most of other studies examining a validity of non-English versions of the CAINS reported these two items loaded onto the MAP factor.
Our study showed that an average score of MAP items was slightly higher than those reported in an American sample of the original study, while an average score of EXP items was similar across both studies.8 One possibility to this difference on MAP scores between two countries may be related to the higher percentage of female participants in current than the original study. However, we could not find any gender differences in total and subdomain scores of the CAINS-K. Another possibility may be related to cultural variations on emotional experiences or reports of emotional experiences. To illustrate, relatively higher MAP score compared to that on the American sample was also found in the German sample.10 Authors of this study explained this may reflect cultural differences in emotional experience and appraisal, based on previous literature suggesting Americans tend to report positive emotions more frequently than negative ones,23 as well as appraise emotional lives as more pleasant than Asians.24 It is also argued that individuals from East Asia and Western culture may have different set of norms regarding emotional experiences, which in turn influences the actual experience of emotion.25 That is, whereas maximizing positive and minimizing negative emotional experiences is valued in Western context, the balance between positive and negative emotions is pursued in East Asian context. Higher MAP scores in our study may reflect these cultural differences. However, due to speculative nature of this account, further studies need to directly test potential cultural differences on reports of pleasure experiences in people with schizophrenia.
Regarding reliability, the CAINS-K exhibited a high internal consistency (MAP=0.91, EXP=0.90, total score=0.92) and inter-rater reliability (0.77). No item deletion was required considering adequate communalities among items and total-item correlations ranging from 0.55 to 0.73. Together, this corroborates a high internal consistency of the CAINS-K in line with other studies in which internal consistencies were reported to be 0.74,8 0.87,10 0.93,11 and 0.91.13
With regards to the external validity, the CAINS-K was closely related with other instruments for negative symptoms such as BPRS and SANS with correlations ranging from 0.59 to 0.85, indicating a strong convergent validity. Importantly, the MAP score was more closely related to anhedonia and avolition subscales than blunted affect and alogia subscales of the SANS. Conversely, the EXP score was more closely related to blunted affect and alogia subscales of the SANS than its anhedonia and avolition subscales, supporting external validities at a subscale level of the CAINS-K.
The CAINS-K total and subscale scores were only weakly related to CDSS and positive, depression, and agitation symptoms of the BPRS in the current study. Previous studies reported null relationships between the CAINS and other symptoms, e.g., positive and depressive symptoms,10,13 In this regard, the discriminant validity of the CAINS-K might be weaker than these CAINS versions (German and Chinese ones). However, some other studies reported small but significant correlations between CAINS subscales and positive and agitation symptoms8 and also depressive symptoms.11 One possibility for these significant correlations is that overall severity of illness may have confounded the observed relations between the CAINS negative symptoms and other symptoms. In line with this idea, correlations with positive and depressive symptoms became decreased or insignificant after the general severity of illness was controlled for in Spanish version of the CAINS.11 When we controlled BPRS total score and obtained partial correlations between the CAINS total score and other clinical measures (BPRS, SANS, and CDSS) in additional analysis, we also observed significant correlations with depression and agitation symptoms of the BPRS and CDSS became non-significant or reduced, while correlations with SANS still remained significant and strong.
With respect to cognition, the CAINS-K exhibited no correlation with TMT-B and Coding test, indicating negative symptoms measured by the CAINS-K may not be closely related to these neurocognitive functions, supporting discriminant validity. It is interesting to note that total and subscale scores of the CAINS-K exhibited a small but significant correlation with the verbal fluency test. This may be consistent with the account that negative symptoms are closely related to fronto-striatal dysfunction which has been thought to underlie impaired verbal fluency in schizophrenia as well.19
Last, we found only the MAP but not EXP score was positively correlated with self-reported behavior activation with a small magnitude (r=0.164). Previous studies reported conflicting results regarding the relationship between them. One study found high BAS score was related to low negative symptoms measured by PANSS,26 whereas the other study reported only BIS but not BAS score was positively correlated with expression deficits dimension of the CAINS.27 The discrepancy may be partly attributed to differences in sample characteristics such as a shorter illness duration in the current study compared to the previous one.27 Additionally, it is recently suggested that negative symptoms of schizophrenia may involve at least two distinct motivational profiles including high BIS and moderate BAS, and low BIS and BAS, rather than a single motivational dimension solely implicated in these symptoms.27 According to this account, a categorical approach rather than considering BIS and BAS as continuous and orthogonal variables may better elucidate motivation systems involved in manifestations of negative symptoms. Therefore, it is possible that understanding of the relationship between the CAINS-K and latent motivation systems may be better aided by considering different combinations of BIS and BAS, which should be investigated in future studies.
Several limitations of the present study should be acknowledged. First, the current sample consisted of chronic outpatients with overall mild symptoms. Therefore, the results may not be generalized to Korean patients in the acute phase or in their first episodes. Second, previous studies indicated that negative symptoms measured by the CAINS, mainly motivational and pleasure deficits, were related to functional outcomes.8,10 However, we were not able to replicate this finding as we did not include functioning measures. Furthermore, the current study was not able to examine the test-retest reliability of the scale. Future studies need to further examine the functional significance and test-retest reliability of the CAINS-K. Next, two subscales (MAP and EXP) of the CAINS-K were related with each other (r=0.50), which was also found in other studies.8,11 More studies are necessary to determine the nature of this correlation between two facets of negative symptoms. Last, clinical ratings, i.e., CAINS, PANSS, and SANS, were completed by same raters for each patient. Although raters were trained for evaluating symptoms following specific criteria and anchors of each scale, the shared rater variance may have affected observed correlations among clinical measures.
Overall, the present study revealed that the CAINS-K is a valid measurement of negative symptoms in the Korean population. It has strengths in that it was validated with the largest sample since the original study, which was recruited from multi-centers, and also extends the validity of the CAINS to an Asian population. We expect that the CAINS-K promotes international trials of treatment and mechanism of negative symptoms in schizophrenia.
Acknowledgments
This research was supported by Jisan Cultural Psychiatry Research Fund (2014). The authors wish to thank JC for helping us with all the processes.
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.4306/pi.2017.14.4.413.
Descriptive statistics for 13 CAINS items
References
- 1.Andreasen NC. Scale for the Assessment of Negative Symptoms (SANS) Br J Psychiatry. 1989;155(Suppl 7):53–58. [PubMed] [Google Scholar]
- 2.Kirkpatrick B, Fenton WS, Carpenter WT, Jr, Marder SR. The NIMH-MATRICS consensus statement on negative symptoms. Schizophr Bull. 2006;32:214–219. doi: 10.1093/schbul/sbj053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Piskulic D, Addington J, Cadenhead KS, Cannon TD, Cornblatt BA, Heinssen R, et al. Negative symptoms in individuals at clinical high risk of psychosis. Psychiatry Res. 2012;196:220–224. doi: 10.1016/j.psychres.2012.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fusar-Poli P, Papanastasiou E, Stahl D, Rocchetti M, Carpenter W, Shergill S, et al. Treatments of negative symptoms in schizophrenia: meta-analysis of 168 randomized placebo-controlled trials. Schizophr Bull. 2014;41:892–899. doi: 10.1093/schbul/sbu170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garcia-Portilla MP, Garcia-Alvarez L, Saiz PA, Al-Halabi S, Bobes-Bascaran MT, Bascaran MT, et al. Psychometric evaluation of the negative syndrome of schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2015;265:559–566. doi: 10.1007/s00406-015-0595-z. [DOI] [PubMed] [Google Scholar]
- 6.Gard DE, Kring AM, Gard MG, Horan WP, Green MF. Anhedonia in schizophrenia: distinctions between anticipatory and consummatory pleasure. Schizophr Res. 2007;93:253–260. doi: 10.1016/j.schres.2007.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Horan WP, Kring AM, Gur RE, Reise SP, Blanchard JJ. Development and psychometric validation of the Clinical Assessment Interview for Negative Symptoms (CAINS) Schizophr Res. 2011;132:140–145. doi: 10.1016/j.schres.2011.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kring AM, Gur RE, Blanchard JJ, Horan WP, Reise SP. The Clinical Assessment Interview for Negative Symptoms (CAINS): final development and validation. Am J Psychiatry. 2013;170:165–172. doi: 10.1176/appi.ajp.2012.12010109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Strauss GP, Keller WR, Buchanan RW, Gold JM, Fischer BA, McMahon RP, et al. Next-generation negative symptom assessment for clinical trials: validation of the Brief Negative Symptom Scale. Schizophr Res. 2012;142:88–92. doi: 10.1016/j.schres.2012.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Engel M, Fritzsche A, Lincoln TM. Validation of the German version of the Clinical Assessment Interview for Negative Symptoms (CAINS) Psychiatry Res. 2014;220:659–663. doi: 10.1016/j.psychres.2014.07.070. [DOI] [PubMed] [Google Scholar]
- 11.Valiente-Gómez A, Mezquida G, Romaguera A, Vilardebò I, Andrés H, Granados B, et al. Validation of the Spanish version of the Clinical Assessment for Negative Symptoms (CAINS) Schizophr Res. 2015;166:104–109. doi: 10.1016/j.schres.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 12.Garcia-Portilla MP, Garcia-Alvarez L, Mane A, Garcia-Rizo C, Sugranyes G, Berge D, et al. The negative syndrome of schizophrenia: three -underlying components are better than two. Schizophr Res. 2015;166:115–118. doi: 10.1016/j.schres.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 13.Chan RC, Shi C, Lui SS, Ho KK, Hung KS, Lam JW, et al. Validation of the Chinese version of the Clinical Assessment Interview for Negative Symptoms (CAINS): a preliminary report. Front Psychol. 2015;6:7. doi: 10.3389/fpsyg.2015.00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV Axis I Disorders: Patient Edition (February 1996 Final), SCID-I/P. New York: Biometrics Research; 1998. [Google Scholar]
- 15.Overall JE, Gorham DR. The brief psychiatric rating scale. Psychol Rep. 1962;10:799–812. [Google Scholar]
- 16.Addington D, Addington J, Maticka-Tyndale E. Assessing depression in schizophrenia: the Calgary Depression Scale. Br J Psychiatry Suppl. 1993;(22):39–44. [PubMed] [Google Scholar]
- 17.Wechsler D. Wechsler Adult Intelligence Scale-Fourth Edition (WAIS-IV) San Antonio, TX: NCS Pearson; 2008. [Google Scholar]
- 18.Reitan RM. Validity of the Trail Making Test as an indicator of organic brain damage. Percept Mot Skills. 1958;8:271–276. [Google Scholar]
- 19.Joyce E, Collinson S, Crichton P. Verbal fluency in schizophrenia: relationship with executive function, semantic memory and clinical alogia. Psychol Med. 1996;26:39–49. doi: 10.1017/s0033291700033705. [DOI] [PubMed] [Google Scholar]
- 20.Bowie CR, Harvey PD, Moriarty PJ, Parrella M, White L, Davis KL. A comprehensive analysis of verbal fluency deficit in geriatric schizophrenia. Arch Clin Neuropsychol. 2004;19:289–303. doi: 10.1016/S0887-6177(03)00041-6. [DOI] [PubMed] [Google Scholar]
- 21.Carver CS, White TL. Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: the BIS/BAS scales. J Pers Soc Psychol. 1994;67:319–333. [Google Scholar]
- 22.Steiger JH. Tests for comparing elements of a correlation matrix. Psychol Bull. 1980;87:245–251. [Google Scholar]
- 23.Kitayama S, Markus HR, Kurokawa M. Culture, emotion, and well-being: good feelings in Japan and the United States. Cogn Emot. 2000;14:93–124. [Google Scholar]
- 24.Mesquita B, Karasawa M. Different emotional lives. Cogn Emot. 2002;16:127–141. [Google Scholar]
- 25.Sims T, Tsai JL, Jiang D, Wang Y, Fung HH, Zhang X. Wanting to maximize the positive and minimize the negative: implications for mixed affective experience in American and Chinese contexts. J Pers Soc Psychol. 2015;109:292–315. doi: 10.1037/a0039276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Scholten MR, van Honk J, Aleman A, Kahn RS. Behavioral inhibition system (BIS), behavioral activation system (BAS) and schizophrenia: relationship with psychopathology and physiology. J Psychiatr Res. 2006;40:638–645. doi: 10.1016/j.jpsychires.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 27.Felice Reddy L, Green MF, Rizzo S, Sugar CA, Blanchard JJ, Gur RE, et al. Behavioral approach and avoidance in schizophrenia: an evaluation of motivational profiles. Schizophr Res. 2014;159:164–170. doi: 10.1016/j.schres.2014.07.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Descriptive statistics for 13 CAINS items