Abstract
Objective
The purpose of this study was to investigate the characteristics of psychological factors that are related to irritable bowel syndrome (IBS) and their effects on the quality of life (QOL) of firefighters in South Korea.
Methods
This study examined data collected from 1217 firefighters in South Korea. After identifying firefighters with IBS according to the Rome III diagnostic criteria for functional gastrointestinal disorders (FGIDs), we collected demographic data and psychological variables through self-administered questionnaires. In order to observe the distribution of the high-risk group in the Korean occupational stress scale (KOSS) subcategories, we conducted logistic multiple linear regression. The correlations between psychological factors and QOL were analyzed and we performed a stepwise regression analysis.
Results
The groups (firefighters with and without IBS) showed differences by sex, working period, task, working pattern, Patient Health Questionnaire-9, Generalized Anxiety Disorder Questionnaire-7, Korean Occupational Stress Scale, Rosenberg's Self-Esteem Scale, and the World Health Organization Quality of Life-BREF. IBS risk was higher in the following KOSS subcategories: job demand (OR 1.79, 95% CI: 1.11–2.89), interpersonal conflict (OR 2.21, 95% CI: 1.25–4.33), organizational system (OR 1.87, 95% CI: 0.58–3.30), and lack of reward (OR 2.39, 95% CI: 1.08–5.26). The final regression model explained 42.6% of the variance in overall quality of life.
Conclusion
The findings of this study indicate that a number of psychological factors increase the likelihood of irritable bowel syndrome (IBS) and affect QOL. Therefore, when diagnosing IBS in the future, mental health aspects should be considered in addition to physical health.
Keywords: Irritable bowel syndrome, Occupational stress, Quality of life, Depression, Firefighters
INTRODUCTION
In South Korea, firefighters are civil servants, whose duties involve emergency rescue, fire prevention, monitoring fire risk, and extinguishing fires. The functional aspects of firefighting duties can be classified into fire safety and volunteer functions. Moreover, firefighting duties have special characteristics in terms of risks, 24-hour shifts, and working environments, compared with the duties of other civil servants.1 In addition, firefighters require robust physical fitness to manage the health-related risks, emergencies, and unusual environments in which they work. Although there may be differences in the types and characteristics of activities, fire-fighting involves life-threatening risks, such as exposure to toxic gases (including carbon monoxide and phosgene), death or injury, and accidents caused by unforeseen explosions. Moreover, firefighters are required to act immediately, whether firefighting or conducting rescue and first aid activities, in order to reduce risks to survivors. As such, firefighters are exposed to a range of serious risks in the course of their duties, and the likelihood of emotional stress and other work-related diseases is high.2
Nevertheless, there are very few studies of firefighters' exposure to risk or biological monitoring of firefighters; studies of the effect of firefighters' duties on their health are limited to an examination of occupational stress, posttraumatic stress disorder (PTSD), and physical diseases, including pulmonary dysfunction, respiratory symptoms, noise-induced deafness, musculoskeletal diseases, and cancer.3,4,5,6 However, a recent study reported a high prevalence of functional gastrointestinal disorders (FGIDs) in firefighters.7 In particular, irritable bowel syndrome (IBS), caused by the irregular working environment and work structure involving high stress, appears to impose a serious burden on firefighters' health.
Irritable bowel syndrome (IBS) is a common functional gastrointestinal disorder characterized by chronic, relapsing abdominal pain or discomfort and disordered defecation.8 The prevalence of IBS in the general population is estimated to range from 3% to 20% based on the Rome III criteria.9,10,11,12 Although the symptoms of IBS often impair the patient's quality of life (QOL), many individuals with IBS ignore their symptoms and tend not to seek medical care.13
Psychological factors such as stress play an important role in the onset of IBS.14,15 Several community studies comparing the psychological profiles of consulters, non-consulters, and controls free of symptoms from the same population have demonstrated that consulters with IBS had significantly higher anxiety and depression scores than either the non-consulters or the controls.16,17 The quality of life (QOL) of patients with irritable bowel syndrome (IBS) is closely related to disability, health care resource utilization, and clinical response to treatment.18,19 Therefore, it is crucial to understand the factors that affect the quality of life of IBS patients; these factors include extra-intestinal symptoms, psychiatric symptoms, disease severity, and sex.20 The health-relatedquality of life of IBS patients is similar to that of patients with diabetes mellitus, cancer, and end stage renal disease, and is lower than that of general population.21,22
Although the prevalence of IBS is high in firefighters and psychological factors are strongly associated with IBS manifestation and its aggravation, there are very few studies of the relationship between IBS and particular psychological factors. Therefore, this study investigated the characteristics of the psychological factors that are related to IBS and their effects on the quality of life of firefighters in South Korea.
METHODS
Subjects
Planning for the study began in July 2014 and data analysis was completed in March 2015. The fieldwork was conducted between September and October 2014. A total of 1,355 firefighters participated in the study. The exclusion criteria were as follows: 1) esophageal or gastric malignancy, 2) prior gastric surgery, 3) peptic ulcer disease, 4) chronic use of antacid medication, such as proton pump inhibitors or H2-receptor antagonists, for more than two months prior to survey, and 5) pregnancy. This resulted in 1,217 eligible firefighters for analysis (an eligibility rate of 89.81%).
We followed the Rome III diagnostic criteria to identify patients with FGIDS. The Rome III diagnostic criteria operate as a system to classify the functional gastrointestinal disorders of the digestive system (FGIDS) in which symptoms cannot be explained by the presence of structural or tissue abnormality, based on clinical symptoms.23 Examples of FGIDs include irritable bowel syndrome, functional dyspepsia, functional constipation, and functional heartburn. The diagnosis of IBS is confirmed if symptoms persist for at least six months and the patient had recurring abdominal pain and discomfort that lasted at least three days per month for the past three months. IBS is also diagnosed if a patient satisfies any two of the following three criteria: 1) relief from abdominal pain or discomfort on defecation; 2) change in frequency of defecation frequency; and 3) change in the state/shape of the stool.
We obtained each participant's demographic data and psychological variables through six questionnaires in total. After the researchers explained the purpose of this study, all participants provided written informed consent. This study was approved bythe Wonkwang University Hospital Institutional Review Board (IRB).
Measures
Patient Health Questionnaire-9
The Patient Health Questionnaire-9 (PHQ-9) is composed of nine items to identify depression.24 The severity of depression in the previous two weeks is scored, with each item awarded 0–3 points. A final score of 5–9 points is defined as mild depression, 10–14 points as moderate depression, and 15 points or more as severe depression. The validity and reliability of the Korean version has been verified by Han et al.25
Generalized Anxiety Disorder Questionnaire-7
The Generalized Anxiety Disorder Questionnaire-7 (GAD-7) is composed of seven items to identify anxiety. Each item is awarded 0–3 points and the maximum score is 21.26 A cut-off score of 10 points is optimal for detecting anxiety, and sensitivity and specificity are highest when the cut-off score is eight points.27
Korean Occupational Stress Scale
The Korean Occupational Stress Scale (KOSS) was developed to assess occupational stress. It is composed of eight domains: physical environment, job demand, insufficient job control, interpersonal conflict, job insecurity, organizational system, lack of reward, and occupational climate.28 We used the Korea Occupational Safety & Health Agency (KOSHA) Guide H-67-2012 to obtain occupational stress scores. We converted the scores in each subcategory to 100, and the high-scoring group (above the median score of Korean workers) was defined as the “high-risk stress group,” and the low-scoring group (below the median score of Korean workers) was defined as the “ low-risk stress group.”29
Ways of Coping Checklist
The Ways of Coping Checklist (WCCL) consists of four domains: problem-focused, seeking social support, emotion-focused, and wishful thinking.30 The domains are further divided into an active coping style, which combines problem-focused and seeking social support, and a passive coping style, which combines emotion-focused and wishful thinking.
Rosenberg's Self-Esteem Scale
The scale consists of ten items, five of which are worded positively and five negatively. The items are scored on a four-point scale ranging from 1 (strongly disagree) to 4 (strongly agree), with higher scores indicating higher self-esteem. Possible scores on the Rosenberg's Self-Esteem Scale (RSES) range from 10 to 40.31 The validity and reliability of the Korean version has been verified by Lee et al.32
World Health Organization Quality of Life-BREF
The World Health Organization Quality of Life-BREF (WH-OQOL-BREF) is a quality of life scale developed by the WH-OQOL Group. Itcomprises 26 items, which measure the following broad domains: physical health, psychological health, social relationships, and environment. Each item is awarded a score of 0–5 points, and higher scores signify higher quality of life.33 The validity and reliability of the Korean version has been verified by Min et al.34
Statistical analysis
We calculated the mean and standard deviation of continuous variables and the frequency and percentage of categorical variables. We employed chi-square tests to analyze the differences in the demographic data of participants with and without IBS (IBS-positive and IBS-negative, respectively). Independent t-tests were used to analyze the total scores of PHQ-9, GAD-7, KOSS, WCCL, RSES, and WHOQOL-BREF as continuous variables. We assessedthe IBS risk for each of the KOSS sub-categories by conducting a logistic regression analysis after controlling for sex, age, and education.We explored predictive variables that influenced quality of life through stepwise multiple regression analysis. The statistical analyses were performed using SPSS software (SPSS, Version 21; Chicago, IL, USA).
RESULTS
Difference between IBS-positive group and IBS-negative group
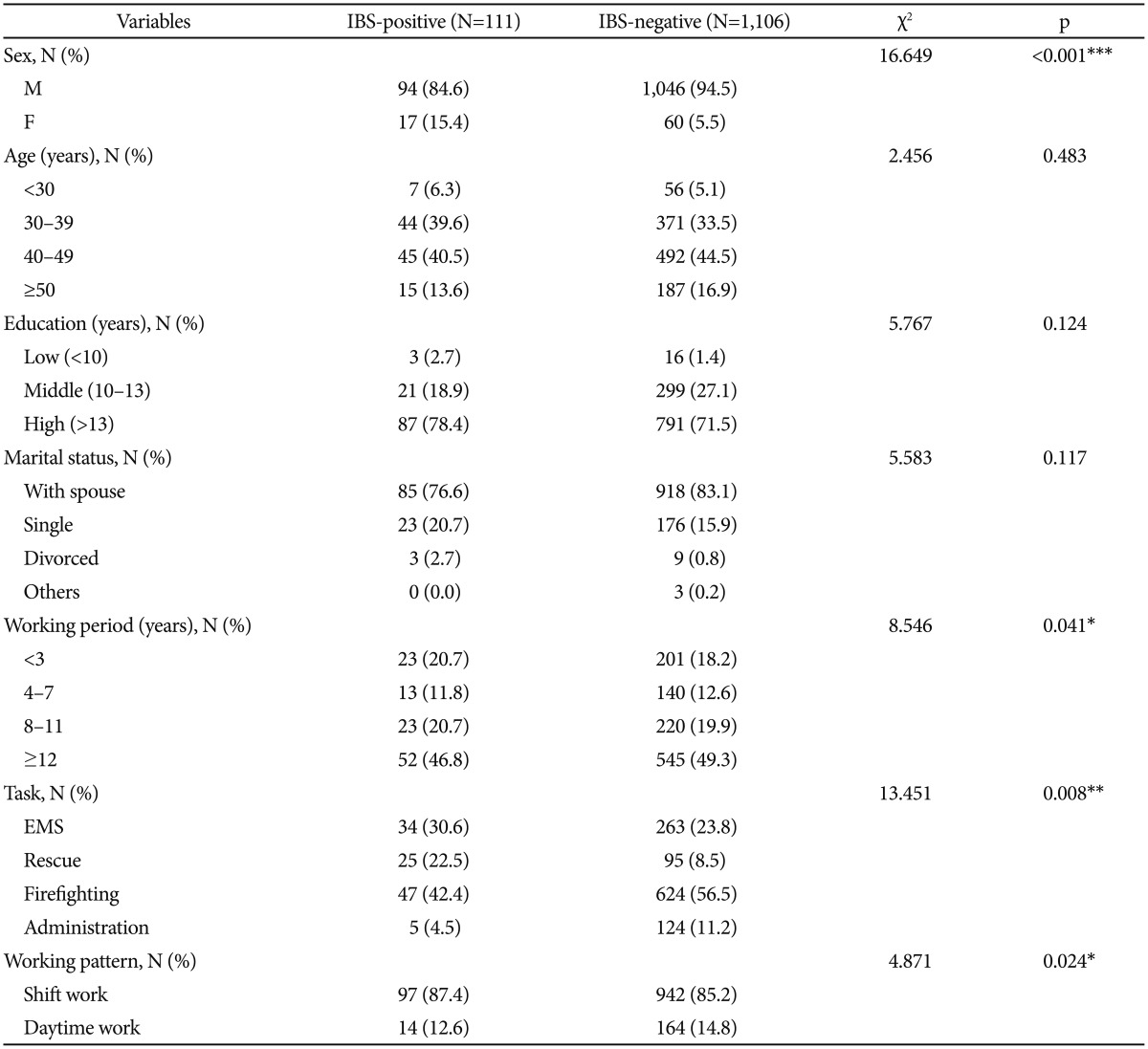
The chi-square tests of the demographic data revealed differences between the two groups by sex (χ2=16.649, df=1, p< 0.001), working period (χ2=8.546, df=3, p=0.041), task (χ2= 13.451, df=3, p=0.008), and working pattern (χ2=4.871, df=1, p=0.024). However, no differences by age, education, or marital status were observed (Table 1).
Table 1. Demographic characteristics of subjects.
*p<0.05, **p<0.01, ***p<0.001. IBS: irritable bowel syndrome, N: number, M: male, F: female, EMS: emergency medical service
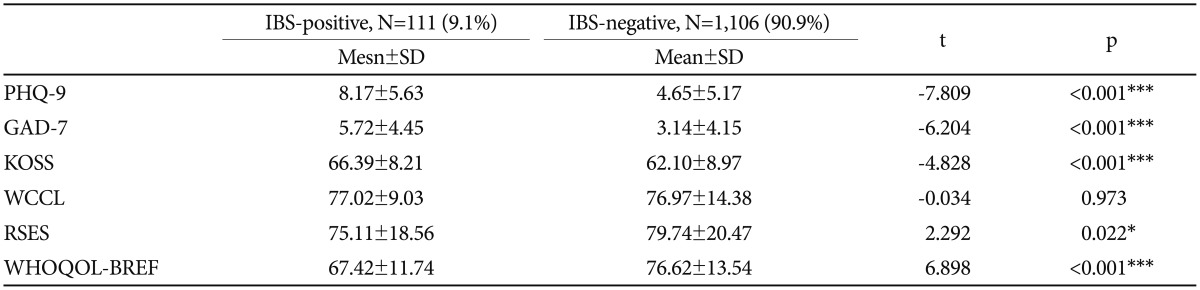
In the independent t-tests conducted to identify differences between the IBS-positive and IBS-negative groups by psychological variables, significant differences were observed in PHQ-9 (t=-7.809, p<0.001), GAD-7 (t=-6.204, p<0.001), KOSS (t=-4.828, p<0.001), RSES (t=2.292, p=0.022), and WHOQOL-BREF (t=6.898, p<0.001). However, no significant difference between the two groups was observed for WCCL (Table 2).
Table 2. Comparison of psychological variables between IBS-positive and IBS-negative group.
*p<0.05, ***p<0.001. IBS: irritable bowel syndrome, N: number, SD: standard deviation, PHQ-9: patient health questionnaire-9, GAD-7: generalized anxiety disorder-7, KOSS: Korean Occupational Stress Scale, WCCL: Ways of Coping Checklist, RSES: Rosenberg's Self-Esteem Scale, WHOQOL-BREF: World Health Organization Quality of life-BREF
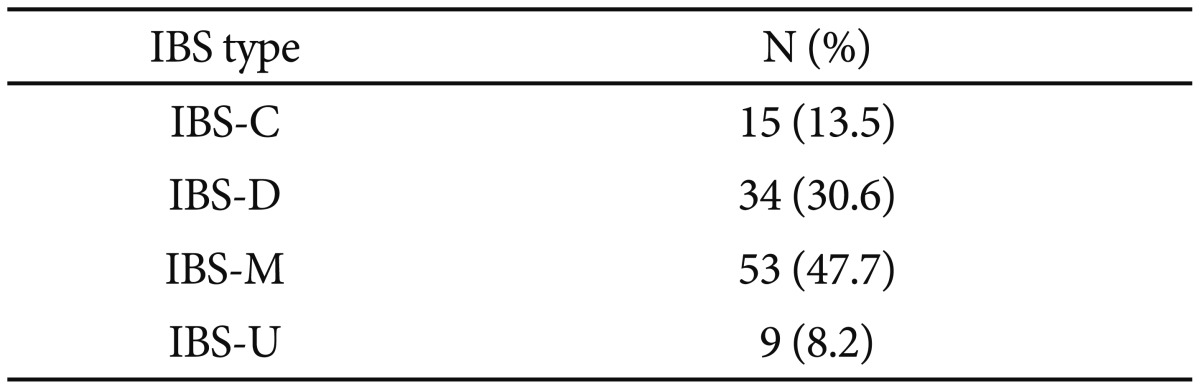
IBS subtypes among the subjects
The major overlap among subjects with IBS was IBS-M: IBS-mixed type (47.7%) (Table 3).
Table 3. IBS subtypes among the subjects (N=111).
N: number, IBC: irritable bowel syndrome, IBS-C: IBS-constipation, IBS-D: IBS-diarrhea, IBS-M: IBS-mixed type, IBS-U: IBS-unspecified
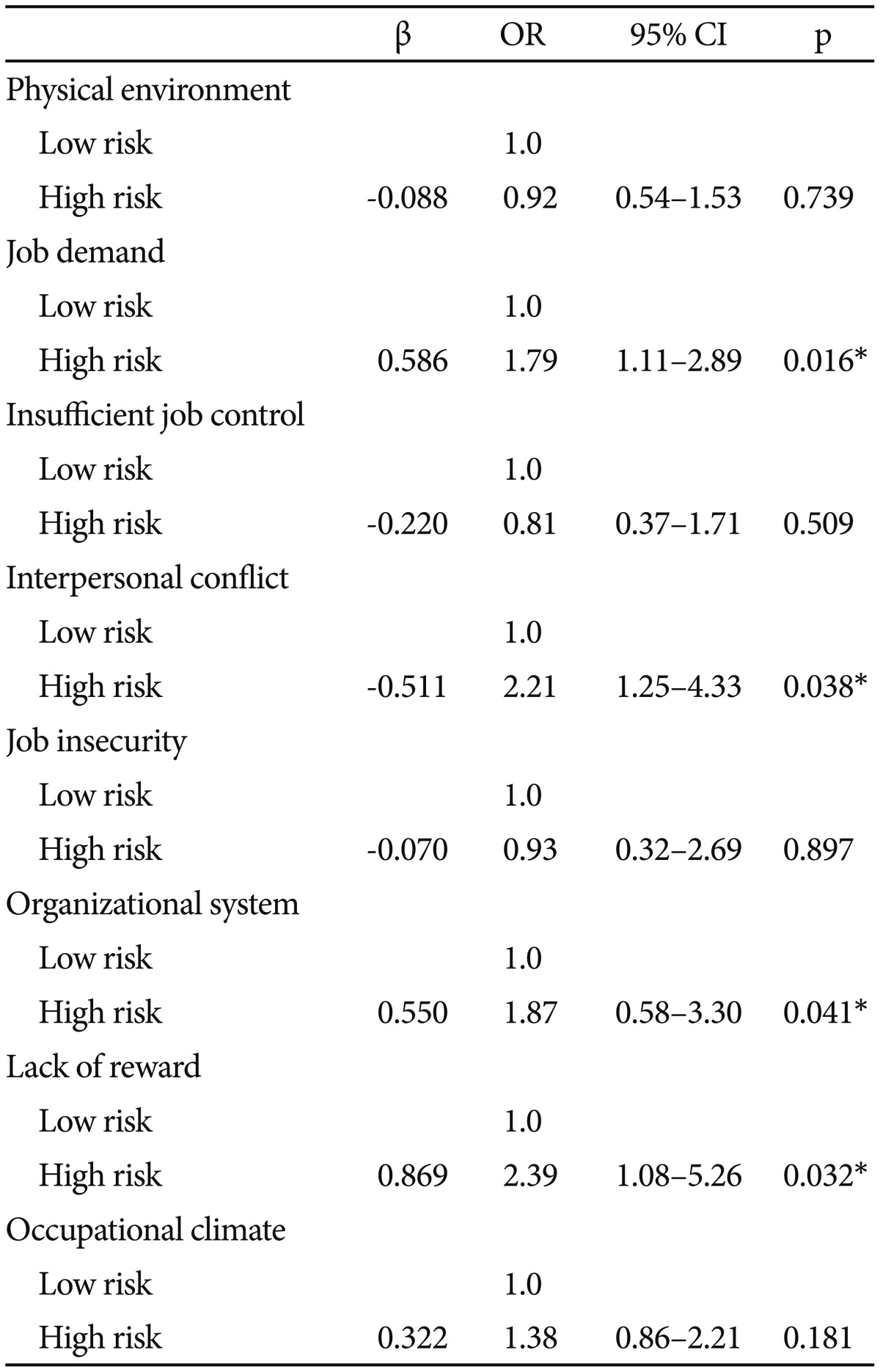
Age-adjusted odds ratios for IBS with psychological variables
We adjusted for age and conducted logistic multiple linear regression in order to minimize the likelihood of misinterpretation of the results. In the high-risk group, the risk of IBS was higher in the following KOSS subcategories: job demand (OR 1.79, 95% CI: 1.11–2.89), interpersonal conflict (OR 2.21, 95% CI: 1.25–4.33), organizational system (OR 1.87, 95% CI: 0.58–3.30) and lack of reward (OR 2.39, 95% CI: 1.08–5.26). Statistically significant correlations were not observed in the other subcategories (Table 4).
Table 4. Adjusted odds ratio of IBS according to occupational stress.
*p<0.05. IBS: irritable bowel syndrome
Factors influencing quality of life in IBS group
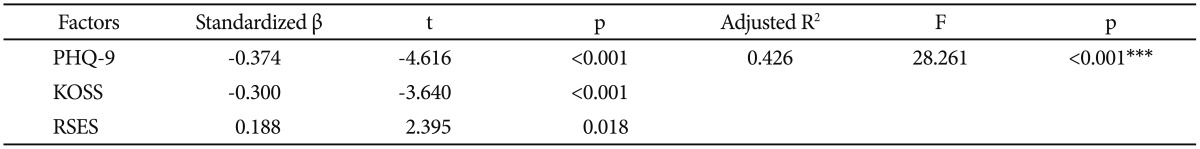
A stepwise multiple regression analysis was conducted to identify models that may predict quality of life in IBS-positive firefighters. We included in the multiple regression model variables that had significant correlations with QOL in the earlier bivariate analysis (age, working period, PHQ-9, GAD-7, KOSS, WCCL, and RSES). We also included task, which was a demographic variable that was expected to exert a significant influences on QOL. In the final regression model, PHQ-9 (β=-0.374, p<0.001), KOSS (β=-0.300, p<0.001), and RSES (β=0.188, p=0.018), which explained 42.6% of the variance in the total QOL, were included (Table 5).
Table 5. Factors influencing quality of life in IBS.
***p<0.001. IBS: irritable bowel syndrome, PHQ-9: patient health questionnaire-9, KOSS: Korean Occupational Stress Scale, RSES: Rosenberg's Self-Esteem Scale
DISCUSSION
Various psychosocial factors put firefighters at a high risk of experiencing psychological and physical diseases. Psychosocial factors are very closely related to FGIDs, including IBS.35 Although some studies have reported the prevalence of overlap syndrome in FGIDs, research into the role of psychological factors in affecting quality of life is very rare.36 Therefore, we aimed in this study to identify differences in demographic and psychosocial factors in firefighters with IBS and those without IBS, and to assess the effects of these factors on quality of life.
The incidence of IBS in this study was 9.1% (111 individuals). The prevalence of IBS reported in previous studies of the general population ranged between 4.4% and 19.4%. Despite the target population having a higher level of work-related stress in this study, the prevalence for IBS was relatively low. Previous studies have reported a substantially higher prevalence of IBS in females than in males. The relatively low prevalence of IBS in this study may be the consequence of the pre-ponderance (94%) of male participants.37,38,39,40 The subtype “IBS-mixed type” was the most common type (47.7%) of IBS among the participants, and this finding is in line with that of previous studies.41,42,43
Significant differences were observed between the IBS-positive and IBS-negative groups for the psychosocial factors of depression, anxiety, occupational stress, self-esteem, and quality of life. In a previous study by Fond et al.,44 patients with IBS had significantly higher anxiety and depression levels than controls. Lee et al.45 reported in their community-based study that depression and chronic stress can cause IBS. In addition, Stanculete et al.46 identified the role of irrational cognition and coping mechanisms in patients with IBS. The relationship between psychosocial factors and IBS has been explained by two major theories. First, the concept of a dysregulated gut-brain axis has been adopted as a suitable model for IBS.47 Second, the gut microbiome may play an important role in the onset and exacerbation of symptoms of the disorder.48
The findings of this study agree with previous studies in terms of context; moreover, by investigating differences in occupational stress, self-esteem, and stress coping styles that have not been investigated previously, the present study has broadened the scope of understanding of psychosocial factors in IBS.
The high-risk group in the subdomains of occupational stress including job demand, interpersonal conflict, organizational system, and lack of reward had a higher probability of IBS. Previous studies also reported that IBS has a very close association with stress. In a study by Koh et al.,49 the prevalence of psychosocial stress among nurses who work rotating shifts is associated with the development of functional gastrointestinal disorders. Eriksen et al.50 reported that occupational stressors such as patient care, team conflicts, role ambiguity, and lack of autonomy were some of the contributing factors to IBS. Qin et al.51 reported that psychological stressors have a marked impact on intestinal sensitivity, motility, secretion, and permeability. In this study, stress due to interpersonal conflict and occupational climate, in addition to occupational characteristics, exerted a substantial influence on IBS, possibly influenced by the hierarchical organization and a public service system focused on command and discipline. These create Korean occupational environments that are very different from Western occupational environments.
PHQ-9, KOSS, and RSES, which account for 42.6% of the variance in the total QOL, are factors that influence the quality of life of the IBS group. When Park et al.52 evaluated health-related quality of life using SF-36 questionnaires, IBS patients had lower QOL scores in all areas, in comparison to the control group. Moreover, Amouretti et al.'s study,53 suggested that continuous pressure was a factor that reduces the quality of life in IBS patients. Although quality of life differs depending on the presence or absence of IBS in previous studies, the studies did not report which psychosocial factor was important in this aspect; therefore, the findings of the present study are significant.
The limitations of our study include that fact that, first, it was a cross-sectional study, so we could not assess effects over time. Second, we used self-reported data to evaluate psychological variables; therefore, there was the possibility of researchers' subjective bias, and there was no study of the severity of IBS symptoms. Third, since it was a population-based study, our study did not include endoscopy data. Finally, because we investigated firefighters, a specific occupational group, it is difficult to generalize the results to the characteristics of all IBS patients. Fifth, since the proportion of male subjects was extremely high (94%), we could not confirm differences by sex.
Nonetheless, this study was conducted with a large number of participants with IBS; the study also is advantageous in examining the influences of occupational stress, stress coping styles, and self-esteem, which have not been investigated previously. In addition, the study is significant, as it has suggested a new approach to the physical and psychological health of firefighters, which recently has become a social issue.
Future research into the influence of various psychosocial factors on IBS would expand present knowledge about the illness. Simultaneous physical and mental health approaches should be undertaken in the treatment of IBS. Moreover, more interest and research into the mental health of those employed in disaster control jobs, including firefighters, is necessary.
Acknowledgments
This research was supported by the National Research Foundation of Korea (NRF) Grant funded by the Ministry of Science, ICT & Future Planning for convergent research in Development program for convergence R&D over Science and Technology Liberal Arts (NRF-2016M3C1B6929822).
References
- 1.Ha J, Kim DI, Seo BS, Kim WS, Yoo SH, Kim SK. Job stress and psychosocial stress among firefighters. Korean J Occup Environ Med. 2008;20:104–111. [Google Scholar]
- 2.Kim KS. Health hazards in firefighters. Hanyang Med Rev. 2010;30:296–304. [Google Scholar]
- 3.Kim SH, Kim JW, Kim JE, Son BC, Kim JH, Lee CH, et al. Pulmonary function and respiratory symptoms of municipal fire officers in Busan. Korean J Occup Environ Med. 2006;18:103–111. [Google Scholar]
- 4.Kim KH, Kim JW, Kim SH. Influences of job stressors on psychosocial well-being, fatigue and sleep sufficiency among firefighters. Korean J Occup Environ Med. 2006;18:232–245. [Google Scholar]
- 5.Kim DS, Moon MK, Kim KS. A survey of musculoskeletal symptoms and risk factors for the 119 emergency medical service (EMS) activities. J Ergon Soc Korea. 2010;29:211–216. [Google Scholar]
- 6.Lovejoy S, Gillespie GL, Christianson J. Exploring physical health in a sample of firefighters. Workplace Health Saf. 2015;63:253–258. doi: 10.1177/2165079915576922. [DOI] [PubMed] [Google Scholar]
- 7.Roh SG, Kim JH. Work related diseases in Korean fire fighters. J Dis Pol Manage. 2013;11:571–576. [Google Scholar]
- 8.El-Salhy M, Hatlebakk JG, Gilja OH, Hausken T. Irritable bowel syndrome: recent development in diagnosis, pathophysiology, and treatment. Expert Rev Gastroenterol Hepatol. 2014;8:435–443. doi: 10.1586/17474124.2014.888952. [DOI] [PubMed] [Google Scholar]
- 9.Mykletun A, Jacka F, Williams L, Pasco J, Henry M, Nicholson GC, et al. Prevalence of mood and anxiety disorder in self-reported irritable bowel syndrome (IBS). An epidemiological population based study of women. BMC Gastroenterol. 2010;10:88. doi: 10.1186/1471-230X-10-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guo Y, Niu K, Momma H, Kobayashi Y, Chujo M, Otomo A, et al. Irritable bowel syndrome is positively related to metabolic syndrome: a population-based cross sectional study. PLoS One. 2014;9:e112289. doi: 10.1371/journal.pone.0112289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grundmann O, Yoon SL. Irritable bowel syndrome: epidemiology, diagnosis and treatment: an update for health care practitioners. J Gastroenterol Hepatol. 2010;25:691–699. doi: 10.1111/j.1440-1746.2009.06120.x. [DOI] [PubMed] [Google Scholar]
- 12.Miwa H. Prevalence of irritable bowel syndrome in Japan: Internet survey using Rome III criteria. Patient Prefer Adherence. 2008;2:143–147. [PMC free article] [PubMed] [Google Scholar]
- 13.Mönnikes H. Quality of life in patients with irritable bowel syndrome. J Clin Gastroenterol. 2011;45(Suppl):S98–S101. doi: 10.1097/MCG.0b013e31821fbf44. [DOI] [PubMed] [Google Scholar]
- 14.Lydiard RB. Irritable bowel syndrome, anxiety, and depression: what are the links? J Clin Psychiatry. 2001;62(Suppl 8):38–45. [PubMed] [Google Scholar]
- 15.Mayer EA, Naliboff BD, Chang L, Coutinho SV. V. Stress and irritable bowel syndrome. Am J Physiol Gastrointest Liver Physiol. 2001;280:G519–G524. doi: 10.1152/ajpgi.2001.280.4.G519. [DOI] [PubMed] [Google Scholar]
- 16.Thijssen AY, Jonkers DM, Leue C, van der Veek PP, Vidakovic-Vukic M, van Rood YR, et al. Dysfunctional cognitions, anxiety and depression in irritable bowel syndrome. J Clin Gastroenterol. 2010;44:e236–e241. doi: 10.1097/MCG.0b013e3181eed5d8. [DOI] [PubMed] [Google Scholar]
- 17.Whitehead WE, Bosmajian L, Zonderman AB, Costa PT, Jr, Schuster MM. Symptoms of psychological distress associated with irritable bowel syndrome. Gastroenterology. 1988;95:709–714. doi: 10.1016/s0016-5085(88)80018-0. [DOI] [PubMed] [Google Scholar]
- 18.Hahn BA, Yan S, Strassels S. Impact of irritable bowel syndrome on quality of life and resource use in the United States and United Kingdom. Digestion. 1999;60:77–81. doi: 10.1159/000007593. [DOI] [PubMed] [Google Scholar]
- 19.Wang YT, Lim HY, Tai D, Krishnamoorthy TL, Tan T, Barbier S, et al. The impact of irritable bowel syndrome on health-related quality of life: a Singapore perspective. BMC Gastroenterol. 2012;12:104. doi: 10.1186/1471-230X-12-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh P, Agnihotri A, Pathak MK, Shirazi A, Tiwari RP, Sreenivas V, et al. Psychiatric, somatic and other functional gastrointestinal disorders in patients with irritable bowel syndrome at a tertiary care center. J Neurogastroenterol Motil. 2012;18:324–331. doi: 10.5056/jnm.2012.18.3.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.El-Serag HB, Olden K, Bjorkman D. Health-related quality of life among persons with irritable bowel syndrome: a systematic review. Aliment Pharmacol Ther. 2002;16:1171–1185. doi: 10.1046/j.1365-2036.2002.01290.x. [DOI] [PubMed] [Google Scholar]
- 22.Gralnek IM, Hays RD, Kilbourne A, Naliboff B, Mayer EA. The impact of irritable bowel syndrome on health-related quality of life. Gastroenterology. 2000;119:654–660. doi: 10.1053/gast.2000.16484. [DOI] [PubMed] [Google Scholar]
- 23.Drossman DA. Rome III: The Functional Gastrointestinal Disorders. 3rd Ed. MacLean, VA: Degnon Association Inc; 2006. [Google Scholar]
- 24.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Han C, Jo SA, Kwak JH, Pae CU, Steffens D, Jo I, et al. Validation of the Patient Health Questionnaire-9 Korean version in the elderly population: the Ansan Geriatric study. Compr Psychiatry. 2008;49:218–223. doi: 10.1016/j.comppsych.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 26.Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 27.Kroenke K, Spitzer RL, Williams JB, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146:317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- 28.Chang SJ, Koh SB, Kang D, Kim SA, Kang MG, Lee CG, et al. Developing an occupational stress scale for Korean employees. Korean J Occup Environ Med. 2005;17:297–317. [Google Scholar]
- 29.KOSHA. KOSHA GUIDE H-67-1012. Seoul: Korea Occupational Safety & Health Agency; 2012. [Google Scholar]
- 30.Folkman S, Lazarus RS. If it changes it must be a process: study of emotion and coping during three stages of a college examination. J Pers Soc Psychol. 1985;48:150–170. doi: 10.1037//0022-3514.48.1.150. [DOI] [PubMed] [Google Scholar]
- 31.Rosenberg HS. Society and Adolescent Self-image. Princeton: Princeton University Press; 1965. [Google Scholar]
- 32.Lee JY, Nam SK, Lee MK, Lee JH, Lee SM. Rosenberg's self-esteem scale: analysis of item-level validity. Korean J Couns Psychother. 2009;21:173–189. [Google Scholar]
- 33.WHOQOL Group. Development of the World Health Organization WHOQOL-BREF Quality of life assessment. Psychol Med. 1998;28:551–558. doi: 10.1017/s0033291798006667. [DOI] [PubMed] [Google Scholar]
- 34.Min SK, Lee CI, Kim KI, Suh SY, Kim DK. Development of Korean version of WHO quality of life scale abbreviated version (WHOQOL-BREF) J Korean Neuropsychiatr Assoc. 2000;39:571–579. [Google Scholar]
- 35.Levy RL, Olden KW, Naliboff BD, Bradley LA, Francisconi C, Drossman DA, et al. Psychosocial aspects of the functional gastrointestinal disorders. Gastroenterology. 2006;130:1447–1458. doi: 10.1053/j.gastro.2005.11.057. [DOI] [PubMed] [Google Scholar]
- 36.Jones MP, Crowell MD, Olden KW, Creed F. Functional gastrointestinal disorders: an update for the psychiatrist. Psychosomatics. 2007;48:93–102. doi: 10.1176/appi.psy.48.2.93. [DOI] [PubMed] [Google Scholar]
- 37.Chang FY, Chen PH, Wu TC, Pan WH, Chang HY, Wu SJ, et al. Prevalence of functional gastrointestinal disorders in Taiwan: questionnaire-based survey for adults based on the Rome III criteria. Asia Pac J Clin Nutr. 2012;21:594–600. [PubMed] [Google Scholar]
- 38.Choung RS, Locke GR, 3rd, Schleck CD, Zinsmeister AR, Talley NJ. Overlap of dyspepsia and gastroesophageal reflux in the general population: one disease or distinct entities? Neurogastroenterol Motil. 2012;24:229–234. doi: 10.1111/j.1365-2982.2011.01845.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rasmussen S, Jensen TH, Henriksen SL, Haastrup PF, Larsen PV, Søndergaard J, et al. Overlap of symptoms of gastroesophageal reflux disease, dyspepsia and irritable bowel syndrome in the general population. Scand J Gastroenterol. 2015;50:162–169. doi: 10.3109/00365521.2014.983157. [DOI] [PubMed] [Google Scholar]
- 40.Kaji M, Fujiwara Y, Shiba M, Kohata Y, Yamagami H, Tanigawa T, et al. Prevalence of overlaps between GERD, FD and IBS and impact on health-related quality of life. J Gastroenterol Hepatol. 2010;25:1151–1156. doi: 10.1111/j.1440-1746.2010.06249.x. [DOI] [PubMed] [Google Scholar]
- 41.Shinozaki M, Fukudo S, Hongo M, Shimosegawa T, Sasaki D, Matsueda K, et al. High prevalence of irritable bowel syndrome in medical outpatients in Japan. J Clin Gastroenterol. 2008;42:1010–1016. doi: 10.1097/MCG.0b013e318150d006. [DOI] [PubMed] [Google Scholar]
- 42.Makharia GK, Verma AK, Amarchand R, Goswami A, Singh P, Agnihotri A, et al. Prevalence of irritable bowel syndrome: a community based study from Northern India. J Neurogastroenterol Motil. 2011;17:82–87. doi: 10.5056/jnm.2011.17.1.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Krogsgaard LR, Engsbro AL, Bytzer P. The epidemiology of irritable bowel syndrome in Denmark. A population-based survey in adults ≤50 years of age. Scand J Gastroenterol. 2013;48:523–529. doi: 10.3109/00365521.2013.775328. [DOI] [PubMed] [Google Scholar]
- 44.Fond G, Loundou A, Hamdani N, Boukouaci W, Dargel A, Oliveira J, et al. Anxiety and depression comorbidities in irritable bowel syndrome (IBS): a systematic review and meta-analysis. Eur Arch Psychiatry Clin Neurosci. 2014;264:651–660. doi: 10.1007/s00406-014-0502-z. [DOI] [PubMed] [Google Scholar]
- 45.Lee SP, Sung IK, Kim JH, Lee SY, Park HS, Shim CS. The effect of emotional stress and depression on the prevalence of digestive diseases. J Neurogastoenterol Motil. 2015;21:273–282. doi: 10.5056/jnm14116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stanculete MF, Matu S, Pojoga C, Dumitrascu DL. Coping strategies and irrational beliefs as mediators of the health-related quality of life impairments in irritable bowel syndrome. J Gastrointestin Liver Dis. 2015;24:159–164. doi: 10.15403/jgld.2014.1121.242.strt. [DOI] [PubMed] [Google Scholar]
- 47.Fukudo S, Kanazawa M. Gene, environment, and brain-gut interactions in irritable bowel syndrome. J Gastroenterol Hepatol. 2011;26(Suppl 3):110–115. doi: 10.1111/j.1440-1746.2011.06631.x. [DOI] [PubMed] [Google Scholar]
- 48.Mayer EA, Savidge T, Shulman RJ. Brain-gut microbiome interactions and functional bowel disorders. Gastroenterology. 2014;146:1500–1512. doi: 10.1053/j.gastro.2014.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Koh SJ, Kim M, Oh da Y, Kim BG, Lee KL, Kim JW. Psychosocial stress in nurses with shift work schedule is associated with functional gastrointestinal disorders. Neurogastroenterol Motil. 2014;20:516–522. doi: 10.5056/jnm14034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Eriksen W, Tambs K, Knardahl S. Work factors and psychological distress in nurses' aides: a prospective cohort study. BMC Public Health. 2006;6:290. doi: 10.1186/1471-2458-6-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Qin HY, Cheng CW, Tang XD, Bian ZX. Impact of psychological stress on irritable bowel syndrome. World J Gastroenterol. 2014;20:14126–14131. doi: 10.3748/wjg.v20.i39.14126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Park JM, Choi MG, Kim YS, Choi CH, Choi SC, Hong SJ, et al. Quality of life of patients with irritable bowel syndrome in Korea. Qual Life Res. 2009;18:435–446. doi: 10.1007/s11136-009-9461-7. [DOI] [PubMed] [Google Scholar]
- 53.Amouretti M, Le Pen C, Gaudin AF, Bommelaer G, Frexinos J, Ruszniewski P, et al. Impact of irritable bowel syndrome (IBS) on health-related quality of life (HRQOL) Gastroenterol Clin Biol. 2006;30:241–246. doi: 10.1016/s0399-8320(06)73160-8. [DOI] [PubMed] [Google Scholar]