Summary
TERT promoter mutations (TERT-mut) have been detected in 60% to 80% of urothelial carcinomas. A molecular urine-based screening assay for the detection of TERT-mut is currently being pursued by our group and others. A small but significant number of bladder carcinomas are adenocarcinoma. The current study assesses the incidence of TERT-mut in primary adenocarcinomas of urinary bladder. A retrospective search of our institutional pathology records identified 23 cystectomy specimens with a diagnosis of adenocarcinoma (2000–2014). All slides were reviewed by a senior urologic pathologist to confirm tumor type and select a representative formalin-fixed, paraffin-embedded block for mutational analysis. Adequate material for DNA testing was available in 14 cases (7 enteric type and 7 not otherwise specified). TERT-mut sequencing analysis was performed using previously described SafeSeq technique. Overall, 28.5% of primary adenocarcinoma harbored TERT-mut. Interestingly, 57% of nonenteric adenocarcinomas were mutation positive, whereas none of the enteric-type tumors harbored mutations. Similar to urothelial carcinoma, we found a relatively higher rate of TERT-mut among nonenteric-type adenocarcinomas further supporting the potential utility of TERT-mut urine-based screening assay for bladder cancer.
Keywords: Adenocarcinoma, Telomerase reverse transcriptase, TERT, Mutation, Bladder carcinoma, Telomerase
1. Introduction
Telomeres must be maintained to assure cell survival and continued replication [1]. One mechanism by which proliferating cells maintain telomeres is through the action of a complex that includes the product of the telomerase reverse transcriptase (TERT) gene adding telomeric repeats to the end of chromosomes [1]. High rates of activating mutations in the upstream promoter of the TERT gene have been reported in numerous human cancers [2–5]. Mutations tend to occur in certain “hot spots,” most notably g.1295228C>T and g.1295250C>T. These mutations generate a CCGGAA/T or GGAA/T motif thereby altering the binding site for Ets transcription factor, subsequently leading to increased TERT promoter activity [2,6,7].
Our group and others have demonstrated TERT promoter mutations (TERT-mut) in a large subset (60%–80%) of urothelial carcinomas and some of their histologic variants [8–14]. These mutations have been found in both noninvasive and invasive urothelial carcinomas and have been detected in urine specimens from patients with urothelial carcinoma, making them attractive candidates for early detection and disease surveillance [8,12,15]. In the current study, we sought to determine the rate of TERT-mut in primary adenocarcinoma of the urinary bladder.
2. Materials and methods
A retrospective search of our institutional archives was conducted for all cases of adenocarcinoma primary to the urinary bladder between the years 2000 and 2014. Focal glandular differentiation can be encountered in association with urothelial carcinomas and other variants. Therefore, to ensure the inclusion of only “pure” adenocarcinoma cases that would satisfy the World Health Organization/International Society of Urologic Pathology 2004 [16] definition of the entity, we limited our study to cystectomy and cystoprostatectomy specimens. Cases with clinical evidence to indicate a secondary involvement of the bladder by an extravesical primary (eg, colorectal) were also excluded. All histologic slides were reviewed to confirm the diagnosis and select a representative tumor section for mutation analysis. A total of 14 cases were included in the study based on the availability of formalin-fixed, paraffin-embedded (FFPE) tissue blocks with sufficient tumor for sampling. The tumor areas were cored with a sterile 16-gauge needle, and the fraction of neoplastic cells was estimated from adjacent sections. The cores were placed in 1.5-mL sterile tubes for DNA purification.
Two sets of negative control samples were also analyzed. Ninety-four peripheral blood samples from healthy population were tested for TERT-mut as negative polymerase chain reaction (PCR) procedure controls. Eight FFPE benign transurethral bladder biopsy samples were also used as negative tissue controls.
After DNA purification, samples were analyzed with Safe-SeqS, a sequencing error reduction technology described previously [17], which better discriminates genuine TERT-mut from artefactual sequencing variants introduced during the sequencing process. Safe-SeqS amplification primers were designed to amplify segments containing the region of the TERT promoter previously shown to harbor mutations in melanomas and other tumors [12] (Fig. 1). The forward and reverse amplification primers contained the TERT-specific sequences at their 3′ ends and a universal priming site at their 5′ end. The reverse primer additionally contained a 14-base unique identifier composed of 14 degenerate N bases (equal likelihood of being an A, C, T, or G) between the universal priming site and gene-specific sequences. The sequences of the forward and reverse primers were either 5′-CACACAG-GAAACAGCTATGACCATGGGCCGCGGAAAGGAAG and 5′-CGACGTAAAACGACGGCCAGTNNNNNNNNN NNNNNCGTCCTGCCCCTTCACC or 5′-CACACAGGAA ACAGCTATGACCATGGCGGAAAGGAAAGGGAG and 5′-CGACGTAAAACGACGGCCAGTNNNNNNNNNNNN NNCCGTCCCGACCCCTC. PCR products were purified with AMPure and sequenced on a MiSeq instrument. Data were analyzed as previously described [17]. Tumor samples were considered positive if the fraction of mutations exceeded 1% of alleles, which was a frequency at least 5 × higher than found in control DNA templates. All sequencing assays scored as positive were confirmed in at least 1 additional, independent PCR and sequencing experiment.
Fig. 1.
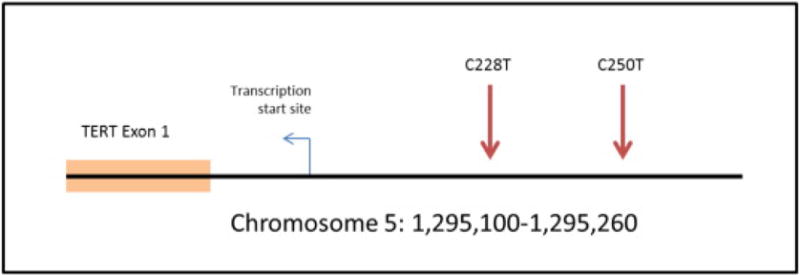
Two mutational “hotspots” are repeatedly seen in the TERT promoter, at position 250 and position 228. Both of the mutations are a C >T base substitution mutation.
3. Results
3.1. Patient demographics and tumor morphology
The patient demographics, including age, sex, race, TNM stage at time of diagnosis, and outcomes, are reported in Table 1. The mean age of the analyzed patients was 58.3 years (range, 28–74 years). The tumors were primarily located either in the bladder wall or dome (Table 1). Of the 14 patients, 4 (28.5%) died of disease (mean survival from time of surgery, 297.5 days). An additional 5 patients are known to have died; information about the cause of death was not available for these patients.
Table 1.
Patient demographics, outcome, tumor subtype, and pathologic findings in 14 primary urinary bladder adenocarcinomas included in the study
| Case | TERT-mut | Adenocarcinoma subtype | Age | Sex | Location | Race | pTNM stage | Recurrence | Progression | Survival outcome | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Y | NOS | 68 | M | Wall | W | T3 | NX | N | N | UNK |
| 2 | N | NOS | 48 | F | Trigone, urethra | B | T4 | NX | Y | Y | DOD |
| 3 | Y | NOS | 64 | M | Wall | W | T4 | N0 | N | N | UNK |
| 4 | N | Enteric | 46 | M | Wall | B | T2 | N0 | N | Y | AWD |
| 5 | Y | NOS | 67 | M | Wall | W | T3b | N2 | N | N | UNK |
| 6 | N | Enteric | 28 | M | Urachus | W | T3 | NX | Y | Y | DOD |
| 7 | N | NOS | 71 | M | Wall | W | T3 | N0 | N | N | UNK |
| 8 | N | Enteric | 53 | M | Urachus | W | T3a | N0 | N | N | NED |
| 9 | N | NOS | 52 | M | Trigone, ureter | B | T2b | NX | Y | Y | UNK |
| 10 | N | Enteric | 69 | M | Trigone, urethra | B | T4 | N2 | N | N | DOD |
| 11 | N | Enteric | 55 | M | Urachus | W | T3 | N1 | Y | Y | DOD |
| 12 | Y | NOS | 74 | M | Wall | W | T2a | N0 | N | N | NED |
| 13 | N | Enteric | 51 | M | Urachus | W | T4b | N2 | N | Y | AWD |
| 14 | N | Enteric | 70 | M | Trigone, urethra | W | T4 | N0 | N | N | NED |
NOTE. Patient age reported at time of surgery. Tumor stage reported at diagnosis.
Abbreviations: Y, yes; N, no; M, male; F, female; W, white; B, black; DOD, died of disease; DWD, died with disease; AWD, alive with disease; NED, no evidence of disease; UNK, unknown cause of death.
After morphologic review, 7 of the 14 cases of adenocarcinoma had histologic features of enteric differentiation. These tumors were composed of glands lined by columnar cells with tall eosinophilic cytoplasm and elongated, hyperchromatic nuclei. Typical areas of central (“dirty”) necrosis were identifiable. Variable degree of mucin production was found [18,19]. Four of these tumors with enteric morphology were located in the bladder dome and were consistent with urachal origin. Two of the remaining 3 enteric-type adenocarcinomas involved the trigone region and urethra. The remaining case was centered in the bladder wall. The second subset of cases (7/14) was characterized as nonenteric. This designation encompasses tumors with variable histology, including signet ring, mucinous, and not otherwise specified (NOS). Of the 7 nonenteric cases, 3 had at least a focal poorly differentiated component with intracytoplasmic mucin thereby acquiring signet ring features, and an additional 3 had areas of extracellular mucinous pools. The final case had nonspecific glandular features and was categorized as NOS (Fig. 2).
Fig. 2.
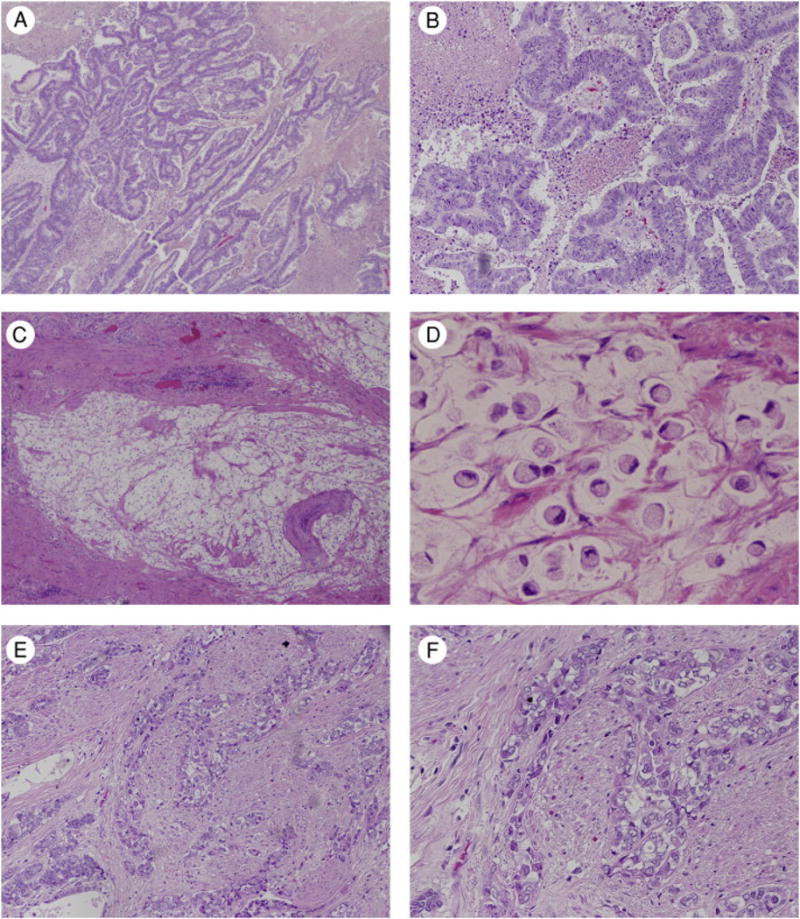
Representative images of the histologic subtypes. A and B, Tumors with enteric differentiation are indistinguishable morphologically from colon adenocarcinoma. Tumors with nonenteric histology include signet ring cell adenocarcinoma (C and D) and adenocarcinoma NOS (E and F). Hematoxylin and eosin, original magnification, × 100 (A, C, and E) and × 200 (B, D, and F).
3.2. TERT-mut detection
Overall, TERT-mut were identified in 4 (28.5%) of 14 cases of primary bladder adenocarcinoma with all showing an identical mutation type (g.1295228C>T) (Table 2). In the 2 morphologic subsets (enteric versus NOS), TERT-mut were only present in the tumors with nonenteric morphology (4/7, 57%) and not found in any of the 7 tumors with enteric differentiation, including those of urachal origin.
Table 2.
TERT-mut status and mutation type by histologic type of adenocarcinoma
| Adenocarcinoma histologic type | TERT-mut detected | Mutation type
|
|
|---|---|---|---|
| 228 T>C | 250 C>T | ||
| Enteric (n = 7) | 0/7 (0%)* | – | – |
| NOS (n = 7) | 4/7 (57%)* | 4/4 (100%) | 0/4 (0%) |
| All (n = 14) | 4/14 (28.5%) | 4/4 (100%) | 0 (0%) |
P = .06 (Fisher exact test) for difference in TERT-mut rates in enteric versus NOS subtypes.
All of the blood and FFPE samples used as negative controls tested negative for TERT-mut.
4. Discussion
Bladder carcinoma is the most common malignancy of the urinary tract and the fourth most common carcinoma in men in the Western world. Among bladder cancers, urothelial carcinoma is by far the most prevalent histologic type, with squamous cell carcinoma and adenocarcinoma making up less than 5% of cases [20]. Per patient, the cost of bladder cancer management is the highest among all tumors, due to the need for long-term monitoring with regular cystoscopy, imaging, and urine cytology [21–23].
TERT-mut were first reported in melanoma [2]. Subsequently, our group and others demonstrated the presence of similar mutations in a wide spectrum of solid cancers, including urothelial carcinoma, gliomas, and hepatocellular carcinoma, among others [3–5]. High rates of TERT-mut have been conspicuously absent in colorectal and lung carcinomas [3,24].
In the urinary bladder, TERT-mut has also been detected at a high rate in small cell carcinoma, urothelial carcinomas with focal squamous differentiation, and nested variants of urothelial carcinoma [13,24,25]. However, to our knowledge, this study is the first to describe TERT-mut in primary bladder adenocarcinoma. Furthermore, the cases evaluated here are intentionally devoid of histologic features of urothelial differentiation (“pure” adenocarcinoma). Here, we demonstrate, for the first time, the presence of TERT-mut in a significant subset (57%) of primary adenocarcinomas of the urinary bladder with nonenteric morphology. All of the adenocarcinomas with TERT-mut had the same C to T mutation (g.1295228C>T). Evaluation of prognostic significance of TERT-mut was not feasible in this limited study.
Bladder adenocarcinomas may be thought of as morphologically dichotomous, appearing as either enteric-type tumors or adenocarcinoma NOS [18]. The latter encompasses multiple types, including the signet ring and mucinous types. Enteric-type adenocarcinomas of the bladder are morphologically indistinguishable from secondary involvement from colorectal carcinoma; clinical correlation is usually required to establish the diagnosis [26]. A difference in TERT promoter mutation rates emerged between enteric adenocarcinoma and adenocarcinoma NOS (0% versus 57%), although the numbers of cases were small and the difference not statistically significant. Intriguingly, TERT-mut have not been detected in colorectal adenocarcinoma [3]. If confirmed, the shared similarities between enteric-type bladder adenocarcinoma and colorectal cancers appear to include the absence of TERT-mut in addition to morphologic and immunophenotypic features.
A subset of tumors with enteric-type morphology arise in the dome of the bladder from embryologic remnants of the urachus and are referred to as urachal adenocarcinomas [27,28]. Four of our enteric-type adenocarcinomas were located in the dome of the bladder and were consistent with urachal adenocarcinomas. Interestingly, none of the urachal tumors harbored TERT-mut in agreement with their phenotypic enteric differentiation.
Surprisingly, when all cases are taken into account, TERT-mut was detected in only 4 (26.7%) of 14 of bladder adenocarcinomas in this study. This figure appears relatively low, considering previous reports have shown that nearly 80% of urothelial carcinomas harbor TERT-mut, and it might be expected that all bladder carcinomas would harbor TERT-mut at some similar rate [3,8,11,12,15]. This low rate of TERT-mut in this study may be in part due to the fact that TERT-mut and the presence of enteric differentiation (including urachal adenocarcinomas) appear so far mutually exclusive.
A recent study by Vail et al [14] addressed the potential diagnostic utility of TERT-mut in differentiating benign from malignant glandular lesions of the bladder including primary adenocarcinoma of bladder. The study failed to detect TERT-mut in 10 cases of primary adenocarcinoma [14]. However, the authors did not further classify the type (enteric versus NOS) of adenocarcinoma analyzed, making it difficult to compare their findings to the current study.
In summary, the present study illustrates the presence of TERT-mut in a significant proportion of primary bladder adenocarcinomas of nonenteric morphology, albeit at a slightly lower rate compared to that reported for urothelial carcinoma. In contrast, the enteric-type adenocarcinomas, including urachal carcinomas, lack TERT-mut. Our group has previously demonstrated the potential role of urine-based assay for TERT-mut as a molecular screening method for the detection of urothelial carcinoma [8,12,15]. Briefly, TERT-mut were consistently detected in the urine of 74% of patients with non-invasive urothelial carcinomas and, on follow-up, were predictive of disease recurrence [17]. These results suggest TERT-mut as a potential biomarker for development of screening and/or diagnostic tests based on analysis of tumor DNA in urine. One potential limitation of such a molecular urine screening assay for bladder cancer would be the ability to detect other bladder carcinomas beyond urothelial carcinoma, such as adenocarcinoma. The present findings of a high rate of TERT-mut (57%) in nonenteric-type adenocarcinoma demonstrate that these tumors may harbor the same biomarker and thus further broaden the clinical utility of a potential assay. Future studies will be needed to address the ability to detect adenocarcinoma in urine samples from patients and determine performance characteristics of such an assay.
Footnotes
Competing interests: K. W. K., N. P., and B. V. are founders of Personal Genome Diagnostics and PapGene and advise Sysmex-Inostics. These companies and others have licensed technologies from Johns Hopkins, of which B. V., K. W. K., and N. P. are inventors and receive royalties from these licenses. The terms of these arrangements are being managed by the university in accordance with its conflict of interest policies.
Funding/Support: This study is supported in part by a grant from The Johns Hopkins Greenberg Bladder Cancer Institute, Baltimore, MD.
References
- 1.Lu W, Zhang Y, Liu D, Songyang Z, Wan M. Telomeres—structure, function, and regulation. Exp Cell Res. 2013;319:133–41. doi: 10.1016/j.yexcr.2012.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang FW, Hodis E, Xu MJ, Kryukov GV, Chin L, Garraway LA. Highly recurrent TERT promoter mutations in human melanoma. Science. 2013;339:957–9. doi: 10.1126/science.1229259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Killela PJ, Reitman ZJ, Jiao Y, et al. TERT promoter mutations occur frequently in gliomas and a subset of tumors derived from cells with low rates of self-renewal. Proc Natl Acad Sci U S A. 2013;110:6021–6. doi: 10.1073/pnas.1303607110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scott GA, Laughlin TS, Rothberg PG. Mutations of the TERT promoter are common in basal cell carcinoma and squamous cell carcinoma. Mod Pathol. 2014;27:516–23. doi: 10.1038/modpathol.2013.167. [DOI] [PubMed] [Google Scholar]
- 5.Qu Y, Shi L, Wang D, et al. Low frequency of TERT promoter mutations in a large cohort of gallbladder and gastric cancers. Int J Cancer. 2014;134:2993–4. doi: 10.1002/ijc.28633. [DOI] [PubMed] [Google Scholar]
- 6.Horn S, Figl A, Rachakonda PS, et al. TERT promoter mutations in familial and sporadic melanoma. Science. 2013;339:959–61. doi: 10.1126/science.1230062. [DOI] [PubMed] [Google Scholar]
- 7.Huang D-S, Wang Z, He X-J, et al. Recurrent TERT promoter mutations identified in a large-scale study of multiple tumour types are associated with increased TERT expression and telomerase activation. Eur J Cancer. 2015:969–76. doi: 10.1016/j.ejca.2015.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Allory Y, Beukers W, Sagrera A, et al. Telomerase reverse transcriptase promoter mutations in bladder cancer: high frequency across stages, detection in urine, and lack of association with outcome. Eur Urol. 2014;65:360–6. doi: 10.1016/j.eururo.2013.08.052. [DOI] [PubMed] [Google Scholar]
- 9.Wu S, Huang P, Li C, et al. Telomerase reverse transcriptase gene promoter mutations help discern the origin of urogenital tumors: a genomic and molecular study. Eur Urol. 2014;65:274–7. doi: 10.1016/j.eururo.2013.10.038. [DOI] [PubMed] [Google Scholar]
- 10.Rachakonda PS, Hosen I, de Verdier PJ, et al. TERT promoter mutations in bladder cancer affect patient survival and disease recurrence through modification by a common polymorphism. Proc Natl Acad Sci U S A. 2013;110:17426–31. doi: 10.1073/pnas.1310522110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Borah S, Xi L, Zaug AJ, et al. TERT promoter mutations and telomerase reactivation in urothelial cancer. Science. 2015;347:1006–10. doi: 10.1126/science.1260200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kinde I, Munari E, Faraj SF, et al. TERT promoter mutations occur early in urothelial neoplasia and are biomarkers of early disease and disease recurrence in urine. Cancer Res. 2013;73:7162–7. doi: 10.1158/0008-5472.CAN-13-2498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhong M, Tian W, Zhuge J, et al. Distinguishing nested variants of urothelial carcinoma from benign mimickers by TERT promoter mutation. Am J Surg Pathol. 2015;39:127–31. doi: 10.1097/PAS.0000000000000305. [DOI] [PubMed] [Google Scholar]
- 14.Vail E, Zheng X, Zhou M, et al. Annals of diagnostic pathology telomerase reverse transcriptase promoter mutations in glandular lesions of the urinary bladder. Ann Diagn Pathol. 2015;19:301–5. doi: 10.1016/j.anndiagpath.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 15.Hurst CD, Platt FM, Knowles MA. Comprehensive mutation analysis of the TERT promoter in bladder cancer and detection of mutations in voided urine. Eur Urol. 2014;65:367–9. doi: 10.1016/j.eururo.2013.08.057. [DOI] [PubMed] [Google Scholar]
- 16.Eble JN, Sauter G, Epstein JI, Sesterhenn I. Pathology and Genetics of Tumours of the Urinary System and Male Genital Organs. Lyon, France: IARC Press; 2004. World Health Organization Classification of Tumours. [Google Scholar]
- 17.Kinde I, Wu J, Papadopoulos N, Kinzler KW, Vogelstein B. Detection and quantification of rare mutations with massively parallel sequencing. Proc Natl Acad Sci U S A. 2011;108:9530–5. doi: 10.1073/pnas.1105422108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roy S, Parwani AV. Adenocarcinoma of the urinary bladder. Arch Pathol Lab Med. 2011;135:1601–5. doi: 10.5858/arpa.2009-0713-RS. [DOI] [PubMed] [Google Scholar]
- 19.Zhong M, Gersbach E, Rohan SM, Yang XJ. Primary adenocarcinoma of the urinary bladder: differential diagnosis and clinical relevance. Arch Pathol Lab Med. 2013;137:371–81. doi: 10.5858/arpa.2012-0076-RA. [DOI] [PubMed] [Google Scholar]
- 20.Cohen SM, Shirai T, Steineck G. Epidemiology and etiology of premalignant and malignant urothelial changes. Scand J Urol Nephrol Suppl. 2000:105–15. doi: 10.1080/00365590050509869. [DOI] [PubMed] [Google Scholar]
- 21.Anastasiadis A, Cordeiro E, Bus MT, Alivizatos G, de la Rosette JJ, de Reijke TM. Follow-up procedures for non-muscle-invasive bladder cancer: an update. Expert Rev Anticancer Ther. 2012;12:1229–41. doi: 10.1586/era.12.98. [DOI] [PubMed] [Google Scholar]
- 22.Anastasiadis A, de Reijke TM. Best practice in the treatment of nonmuscle invasive bladder cancer. Ther Adv Urol. 2012;4:13–32. doi: 10.1177/1756287211431976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Avritscher EBC, Cooksley CD, Grossman HB, et al. Clinical model of lifetime cost of treating bladder cancer and associated complications. Urology. 2006;68:549–53. doi: 10.1016/j.urology.2006.03.062. [DOI] [PubMed] [Google Scholar]
- 24.Cheng KA, Kurtis B, Babayeva S, et al. Heterogeneity of TERT promoter mutations status in squamous cell carcinomas of different anatomical sites. Ann Diagn Pathol. 2015;19:146–8. doi: 10.1016/j.anndiagpath.2015.03.005. [DOI] [PubMed] [Google Scholar]
- 25.Zheng X, Zhuge J, Bezerra SM, et al. High frequency of TERT promoter mutation in small cell carcinoma of bladder, but not in small cell carcinoma of other origins. J Hematol Oncol. 2014;7:47. doi: 10.1186/s13045-014-0047-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang HL, Lu DW, Yerian LM, et al. Immunohistochemical distinction between primary adenocarcinoma of the bladder and secondary colorectal adenocarcinoma. Am J Surg Pathol. 2001;25:1380–7. doi: 10.1097/00000478-200111000-00005. [DOI] [PubMed] [Google Scholar]
- 27.Grignon DJ, Ro JY, Ayala AG, Johnson DE, Ordóñez NG. Primary adenocarcinoma of the urinary bladder. A clinicopathologic analysis of 72 cases Cancer. 1991;67:2165–72. doi: 10.1002/1097-0142(19910415)67:8<2165::aid-cncr2820670827>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 28.Gopalan A, Sharp DS, Fine SW, et al. Urachal carcinoma. Am J Surg Pathol. 2009;33:659–68. doi: 10.1097/PAS.0b013e31819aa4ae. [DOI] [PMC free article] [PubMed] [Google Scholar]


