Abstract
Background: Papillary thyroid cancer is often described as the “good cancer” because of its treatability and relatively favorable survival rates. This study sought to characterize the thoughts of papillary thyroid cancer patients as they relate to having the “good cancer.”
Methods: This qualitative study included 31 papillary thyroid cancer patients enrolled in an ongoing randomized trial. Semi-structured interviews were conducted with participants at the preoperative visit and two weeks, six weeks, six months, and one year after thyroidectomy. Grounded theory was used, inductively coding the first 113 interview transcripts with NVivo 11.
Results: The concept of thyroid cancer as “good cancer” emerged unprompted from 94% (n = 29) of participants, mostly concentrated around the time of diagnosis. Patients encountered this perception from healthcare providers, Internet research, friends, and preconceived ideas about other cancers. While patients generally appreciated optimism, this perspective also generated negative feelings. It eased the diagnosis of cancer but created confusion when individual experiences varied from expectations. Despite initially feeling reassured, participants described feeling the “good cancer” characterization invalidated their fears of having cancer. Thyroid cancer patients expressed that they did not want to hear that it's “only thyroid cancer” and that it's “no big deal,” because “cancer is cancer,” and it is significant.
Conclusions: Patients with papillary thyroid cancer commonly confront the perception that their malignancy is “good,” but the favorable prognosis and treatability of the disease do not comprehensively represent their cancer fight. The “good cancer” perception is at the root of many mixed and confusing emotions. Clinicians emphasize optimistic outcomes, hoping to comfort, but they might inadvertently invalidate the impact thyroid cancer has on patients' lives.
Keywords: : papillary thyroid cancer, good cancer, patient perspectives, thyroidectomy, qualitative research
Introduction
The incidence of papillary thyroid cancer is increasing, and approximately 64,300 new cases of thyroid cancer were diagnosed in the United States in 2016 (1,2). Largely due to its treatability and excellent survival rates, the idea that papillary thyroid cancer is relatively “good” permeates the medical culture.
Unfortunately, relatively favorable survival rates do not comprehensively represent the impact of a cancer diagnosis. In this regard, the “good cancer” characterization may not accurately describe papillary thyroid cancer patients' fight against their disease. In fact, many patients with well-differentiated thyroid cancer suffer a persistent and severe decrease in quality of life, are unsatisfied with the support they receive, live with fear of recurrences and additional treatments, and commonly experience feelings of isolation (3–13). Besides physical and psychosocial struggles, financial difficulties are more common with thyroid cancer than with other malignancies (14).
Despite the documented negative impact of papillary thyroid cancer on patients' lives, the “good cancer” characterization persists. However, much of the focus on thyroid cancer patients' perceptions of having the “good cancer” is based on lay press (15,16). One qualitative study does address patient perceptions of having the “good cancer,” but patients were recruited one to five years following their cancer treatment and were interviewed only once (5). Another qualitative study included participants in three focus groups at an average of five years following their diagnosis, but was able to document the dismissive impact the “good cancer” has on thyroid cancer survivors (13). Therefore, the present study aimed to characterize how patients with papillary thyroid cancer encounter this perspective at diagnosis and how these patients relate to having the “good cancer” throughout their treatment course.
Methods
Patients with papillary thyroid cancer were interviewed during their participation in an ongoing randomized clinical trial (NCT02138214). Both male and female patients aged 21–73 years were eligible. Inclusion was limited to those with a preoperative diagnosis or suspicion of papillary thyroid cancer, based on ultrasound and fine-needle biopsy, without evidence of cervical lymph node involvement or distant metastases. Patients with cancer <1 cm in diameter or T4 disease were excluded. Additional exclusion criteria included prior thyroid surgery, pre-existing vocal cord paralysis or laryngeal pathology, neurologic conditions that affect speech or swallowing, pregnancy, and concurrent malignancy. Participants were interviewed at five time periods (preoperative clinic visit [TP1], two weeks post surgery [TP2], six weeks post surgery [TP3], six months post surgery [TP4], and one year post surgery [TP5]). The University of Wisconsin–Madison Health Sciences Institutional Review Board approved this study. Participants provided written informed consent at the time of recruitment into the clinical trial, and additional verbal consent was obtained before each interview was conducted. Participants were free to decline to answer any question and to end each interview at any time with no justification required.
Trained interviewers (n = 10), who were not members of the clinical staff, performed the interviews and encouraged respondents to speak freely about their experiences. Semi-structured interviews were conducted using an interview guide developed in consultation with clinical staff and piloted with eight respondents at various stages of recovery from thyroidectomy. The interview guide included prompted and unprompted open-ended questions and was revised based on responses to the pilot interviews. Pilot interviews were not included in the results of this study. The final interview guide explored daily life before and after surgery, the experience of diagnosis and treatment, and participants' experiences of and reflections on any postsurgical complications and fear of recurrence. Interviews averaged one hour in length (range 45–120 minutes). All interviews were transcribed verbatim, and any identifiers were removed from transcripts prior to analysis.
Four team members (R.S., N.C., C.M., and J.O.) analyzed a representative subset of interview transcripts line by line (n = 8) for emergent themes and developed a coding structure using a grounded theory approach (17). Themes and coding structures were compared among researchers, and discrepancies were resolved by consensus. After the open coding process, a catalogue of focused codes was developed, and a group of trained coders applied the confirmed coding structure to the entire data set using NVivo 11 (QSR International) software. Emerging themes were continuously integrated into the codebook using a constant comparative method. “Good cancer” was a theme that emerged unprompted from the interviews at multiple time points.
Although discussions of the meaning and impact of “good cancer” emerged throughout all interviews at multiple time points, questions that elicited this theme included, “Can you walk me through the process of learning your diagnosis?” (TP1), “What advice would you give to someone else receiving this diagnosis?” (TP1–5), and “What advice would you give to a surgeon treating someone with your diagnosis?” (TP1–5).
As the study progressed, more transcripts became available for analysis, and memo writing continued until data saturation was achieved. Toward the conclusion of memo writing for this research question, we presented preliminary results to the Madison Thyroid Cancer Survivors Support Group and encouraged feedback as member validation. The themes elicited at this meeting had already been identified within the transcripts, further confirming data saturation.
Results
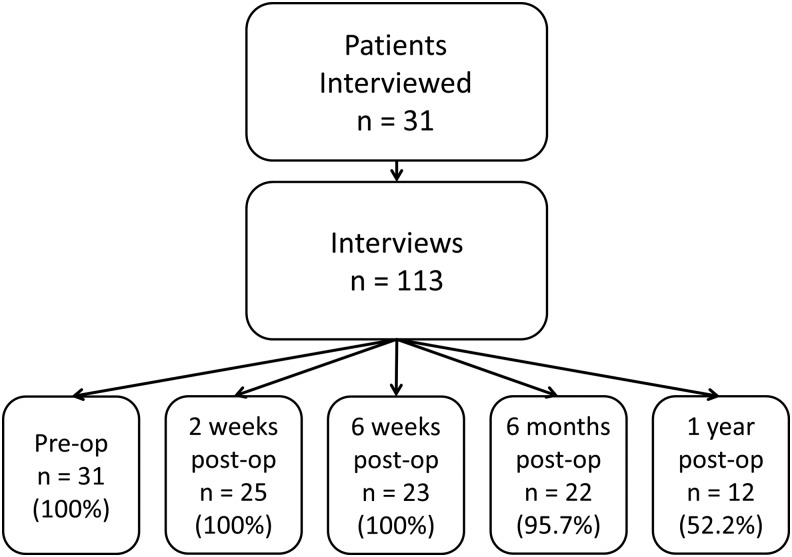
A total of 31 participants with thyroid cancer undergoing 113 interviews were included in the analysis before data saturation was achieved (Fig. 1). Six participants had initial interviews but dropped out before TP2. Another two participants dropped out between TP2 and TP3. Participant ages ranged from 22 to 67 years, and most participants were female, married, and college graduates (Table 1). Median tumor size was 1.5 cm (range 0.6–4.8 cm). The concept of papillary thyroid cancer being the “good cancer” emerged unprompted from 29 (94%) participants and during 52 (46%) interviews. Most discussion (50%) regarding “good cancer” was concentrated at the initial interview, post diagnosis but pre surgery.
FIG. 1.
Diagram of participants and interviews included in the data analysis. At the time of data saturation, 31 patients were interviewed 113 times total at five time periods throughout their thyroid cancer treatment. This figure depicts the number (and percent of participants represented) of transcribed and coded interviews available for analysis at each time point prior to reaching data saturation.
Table 1.
Demographic Data and Disease Characteristics
| Characteristic | n = 31 |
|---|---|
| Age (years), median (range) | 47 (22–67) |
| Sex, n (%) | |
| Male | 7 (22.6) |
| Female | 24 (77.4) |
| Race, n (%) | |
| Caucasian | 30 (96.8) |
| Asian | 1 (0.3) |
| Education, n (%) | |
| High school diploma or equivalent | 9 (29.0) |
| College degree | 9 (29.0) |
| Postgraduate degree | 13 (41.9) |
| Marital status, n (%), n = 29 | |
| Single | 5 (17.2) |
| Married | 21 (72.4) |
| Divorced | 2 (6.9) |
| Widowed | 1 (3.4) |
| Children living at home, n (%), n = 30 | 13 (43.3) |
| Personal history of cancer, n (%), n = 29 | 5 (17.2) |
| Family history of cancer, n (%), n = 29 | 22 (75.9) |
| Tumor size (cm), median (range) | 1.5 (0.6–4.8) |
| Multifocal, n (%) | 11 (35.5) |
| Extrathyroidal extension, n (%) | 4 (12.9) |
| Vascular invasion, n (%) | 2 (6.5) |
Encountering the “good cancer” perspective
Participants encountered the perception that papillary thyroid cancer was the “good cancer” from multiple sources, including healthcare providers, Internet research, and loved ones. Some arrived at the “good cancer” characterization based on their own interpretation of their disease and planned treatment. In recounting conversations with healthcare providers who disclosed the diagnosis, participants indicated that they were told papillary thyroid cancer was “one of the easiest cancers to fix” or that it “is treatable and curable.” In one instance, participant 4 (TP1) remembered being told “…it's no big deal because this is very easy to cure.” Providers frequently situated thyroid cancer in the context of other cancers often quoted as saying, “If you have to have a cancer, this is the best one to have.”
The Internet provided the “good cancer” characterization by comparing papillary thyroid cancer to other forms of cancer: “…with the Internet, we do a lot of reading about … what could this be, what would be the worst case scenario, so I felt informed enough to know that at least it's different from some forms of cancer where it's less treatable” (participant 6, TP1). Participant 7 (TP1) reiterated this theme, saying, “…look it up online, type in ‘best cancer,’ and thyroid will come up.”
The “good cancer” theme was also echoed from participants' loved ones with prior knowledge of thyroid cancer: “So, of course, I talked to my sister who had thyroid cancer … and she said basically what the surgeon told me … if you have to have a cancer, this is the one to have” (participant 3, TP1). Besides discussing aspects of thyroid cancer that allow patients to contextualize the disease for themselves, sometimes friends and family communicated a more blatant message that thyroid cancer is “no big deal.” Participants quoted others as saying, “Oh, well it's only thyroid cancer” or “Oh, well, I've never known anybody to die of that.”
Lastly, participants seemed to contextualize their own cancer as being relatively good based on their personal perceptions of cancer. For example, participant 30 (TP1) said, “If it had been breast cancer, that'd be different, I'd be worried. My sister passed away from that, but I understand that thyroid cancer is very treatable, it's the ‘good cancer,’ if you're gonna have a cancer.” Others thought that the need for chemotherapy is what defines cancer as being bad: “It's just another procedure … and I wouldn't feel like this if the doctor had said … ‘you have to have all these chemotherapy treatments.’ Then I'd be worried” (participant 4, TP1).
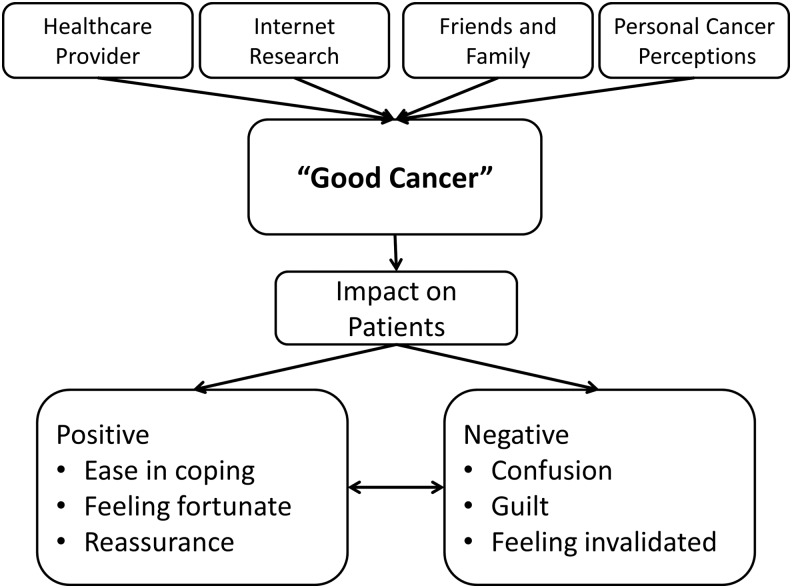
Impact of the “good cancer”
The impact of the “good cancer” perspective varied from patient to patient (Fig. 2). For many, thoughts of their cancer being relatively good were quite positive, eliciting feelings of comfort, gratitude, and reassurance. For others, the “good cancer” perspective, apart from the diagnosis itself, negatively affected their experience with thyroid cancer and resulted in guilt, confusion, and invalidation. Often, both positive and negative emotions occurred simultaneously in participants trying to contextualize their disease.
FIG. 2.
Diagram depicting the source of the “good cancer” perception and effects on patients with papillary thyroid cancer. The characterization of papillary thyroid cancer being “good” arises from multiple, common sources. The impact of such a characterization is often positive but can also be negative, and many people shift between positive and negative responses throughout their treatment.
Positive impact
The “good cancer” theme often helped to ease the diagnosis of papillary thyroid cancer. For example, participant 16 (TP1) said her doctor “put [her] at ease, somewhat, as much as you can with cancer” by informing her that papillary thyroid cancer is the one to have if faced with a cancer diagnosis. Besides easing the diagnosis, many participants felt reassured when encountering the “good cancer” framing of their disease. When asked how hearing, “If you gotta have a cancer, this is probably the best cancer to have”, participant 35 replied, “I was relieved.” Other participants similarly expressed the reassurance that followed hearing that thyroid cancer is the “best one to have.”
Gratitude also emerged as participants considered the behavior of their “good cancer.” Reflecting on being told this cancer was the cancer to have, participant 3 (TP4) explained, “I totally agree with that. So no, I felt good, upbeat, happy in many ways … in my family, there's been a lot of cancer, and to have this discovered purely by accident so early on, I really feel fortunate.” Participant 5 (TP2) put it, “I mean, how much luckier can I get? If I had a cancer for a year and a half, and it never left that spot, pretty lucky.” Other participants expressed feelings of luck while comparing their disease to people with more aggressive cancers. For example, “I don't want to say lucky to have thyroid cancer, but lucky that I didn't have anything worse than thyroid cancer” (participant 21, TP4).
Negative impact
Yet, the idea of a cancer being good also cultivated negative responses in some participants, including guilt and confusion. Participant 19 (TP1) reported it being “kind of a weird sensation, because people will say, ‘Oh you got the good cancer.’” Confusion resulted from unanticipated symptoms or treatment side-effects when participants primed with a “good cancer” mentality expected to have an “easy” cancer. In these instances, the “good cancer” framing of the disease led patients who experienced post-surgical symptoms or other adverse treatment effects to question whether their response to treatment was normal or if their disease was somehow more progressed than expected. Some even felt betrayed by the initial description of their cancer. Probably the most pervasive negative impact of “good cancer” themes was its tendency to invalidate and diminish the struggles of thyroid cancer patients. Participant 16 (TP1) articulated, “…but then it makes it feel a little more inconsequential, but I don't think [the doctor] did that on purpose.” She later elaborated in the same interview, “I feel bad sometimes that people think it's a lesser cancer … that people don't take it as seriously … which just negates it, and it negates me personally.”
Trends over time
Of the 25 participants interviewed at multiple time points, 14 (48%) discussed “good cancer” themes during more than one interview (Table 2). Trending the impact of “good cancer” across time points for the individuals revealed that impressions were largely positive and stayed positive. The “good cancer” perspective started and remained positive in seven (50%) participants, but the other half experienced negative feelings at some point during their treatment. The impact of “good cancer” started mixed or negative and trended toward positive in two (14%) participants, started and remained negative for one (7%) participant, and trended toward negative despite being initially positive in four (29%) participants. Of these four who trended toward negative after initially describing positive feelings about “good cancer,” three had voice abnormalities persisting six weeks after surgery, and the fourth had an abnormal lymph node requiring biopsy one year after surgery. While the “good cancer” characterization softened the initial blow of the diagnosis, it seemed to facilitate an underestimation of treatment challenges, post-treatment symptoms, and fears of recurrence. Yet, two of these three participants with voice complaints whose perceptions trended from positive to negative described the shift in perception after their voice concerns had resolved, possibly indicating these events were not directly related.
Table 2.
Trends in the Perception of the “Good Cancer” Characterization of Papillary Thyroid Cancer Over Time
| Participant no. | TP 1 (preop) | TP 2 (2 weeks) | TP 3 (6 weeks) | TP 4 (6 months) | TP 5 (1 year) | Perceived trend |
|---|---|---|---|---|---|---|
| 2 | Both | Positive | Positive | NM | Neutral | To positive |
| 3 | Positive | NM | Positive | Positive | NM | All positive |
| 4 | Positive | NM | Negative | NM | NM | To negative |
| 5 | Positive | Positive | NM | NM | Negative | To negative |
| 7 | Both | Negative | NM | NM | Negative | To negative |
| 9 | Positive | NM | NM | NM | Positive | All positive |
| 12 | Positive | Positive | NM | NM | Positive | All positive |
| 16 | Both | Both | Both | NM | Negative | To negative |
| 18 | Negative | Both | Negative | All negative | ||
| 20 | Neutral | NM | Positive | NM | NM | All positive |
| 21 | Negative | NM | NM | Positive | NM | To positive |
| 22 | Positive | Neutral | NM | NM | All positive | |
| 28 | Neutral | NM | Positive | NM | All positive | |
| 32 | Neutral | Positive | Positive | NM | All positive |
Fourteen participants discussed “good cancer” themes during multiple interviews during the study period. Their perceptions regarding the “good cancer” characterization were classified as positive, negative, both, or neutral. The perceived trend is indicated in the right-most column.
TP, time point; NM, no mention of “good cancer” themes; blank, interview not available.
Encouragement and advice
When participants were asked about advice they would give to other patients going through a similar experience or to clinicians breaking the news of a new thyroid cancer diagnosis, many participants echoed “good cancer” themes. Some encouragement was positive, reflecting the participant's own experience. Participant 12 (TP2) encouraged others not to fear, saying, “It's 100% treatable … no need to worry.” Others advised providers to guard their optimism: “It is a very treatable cancer, but it is still a cancer. And so I just would be really cautious about sharing the optimism … let the person who's going through it put the value on what the experience is going to be” (participant 18, TP2). Some were quite direct about avoiding a description of thyroid cancer as good: “Oh, my God, don't say, ‘You've got the good cancer’” (participant 19, TP1). Similarly, participant 7 (TP1) reiterated, “Probably don't tell them that it's the best cancer cause it diminishes whatever they're feeling about having it.” Participant 16 (TP1) encouraged a hypothetical patient by directly speaking against the invalidating effects of “good cancer” themes: “Your cancer is valid. Your fear is valid, despite what other people might say or think or act.” At a later interview (TP3), the same participant reiterated, “Cancer is cancer, no matter what form it takes, even if it's a very treatable cancer.”
Discussion
Papillary thyroid cancer is often labeled the “good cancer” because of its favorable prognosis, and patients newly diagnosed with thyroid cancer frequently encounter this perspective. This study investigated how the concept of thyroid cancer as the “good cancer” affected the experience of patients with this disease. Although this perspective often evoked feelings of reassurance, many patients experienced negative feelings such as invalidation and confusion, especially when their experiences varied from expectations.
Most of the literature investigating the psychosocial and support needs of patients with papillary thyroid cancer is limited to survey studies (3,4,6–9,11,12). Presently, qualitative research is needed to define better how patients with thyroid cancer navigate their disease and treatment (12). Importantly, Easley et al. (5), in a prior qualitative study, identified strong feelings of isolation associated with the “good cancer” characterization. While their findings highlighted another negative aspect likely to arise when describing thyroid cancer as “good,” their method of enrolling patients several years following their treatment is likely biased toward those with worse experiences or perhaps those who continue to struggle with their disease (5). Similarly, Sawka et al. (13) identified that well-differentiated thyroid cancer survivors perceive “good cancer” terminology as dismissive of the importance of their disease, but up to one third of these had already battled recurrence (13). In contrast, the participants in the current study were enrolled prior to their treatment and are more likely to be a representative sample of patients presenting with papillary thyroid cancer. This method also allowed some positive aspects of the “good cancer” characterization to be identified and patient perspectives to be followed over time.
Patients diagnosed with thyroid cancer frequently encounter the “good cancer” perspective because the sources of this concept are ubiquitous. Clinicians likely compare thyroid cancer to “worse” cancers to reassure patients, and the present results show that the goal of comforting patients is often achieved. Patients tend to perceive more compassion from providers when an optimistic message is delivered (18). Unfortunately, these good intentions are not always met with positive responses. Such framing may come across as cavalier and prime patients for disappointment, confusion, or even a sense of betrayal when they suffer complications or experience recurrences that do not make their cancer seem “easy” or “good.”
While we cannot deny the positive impact that the “good cancer” theme had on many patients, for others it was largely negative. Lay press discussing the negative implications of the “good cancer” terminology suggests that reasons for the disconnect between patient experiences and the “good cancer” perspective include lifelong troubles regulating thyroid hormone replacement, recurrence and fear of recurrence, and living with permanent complications from treatment (15,16). In the current study, which included only patients with clinically node-negative disease during the first year of their treatment, these factors were not driving forces behind the negative impact of the “good cancer” perspective. Additionally, the participants whose perceptions shifted from initially being positive to being entirely negative experienced that shift after transient voice alterations had resolved. Therefore, the “good cancer” characterization can be bad for any patient, not just for those with a prolonged treatment course, extensive disease, and poor outcomes. This finding is important because most patients with papillary thyroid cancer present with local disease, suggesting the results are generalizable to the majority of patients (19).
The current findings have major implications for physicians who diagnose and treat thyroid cancer. Even participants who were initially reassured by having “good cancer” recommended avoiding terminology that assigns a value to their cancer. Instead, providers are encouraged to discuss the facts and expected outcomes and allow patients the freedom to assign their own meaning to the cancer diagnosis. While physicians rarely initiate discussion about psychosocial issues for cancer patients (20), doing so may help patients navigate their feelings when they do encounter the “good cancer” perspective outside of the medical environment. Propagating the “good cancer” theme seems to reduce the disease to “no big deal” and often leaves a chasm between those experiencing it and those treating it.
This study has limitations that should be considered when generalizing the findings to other patients with thyroid cancer. As a criterion for enrollment in the clinical trial, patients were only included when they had no clinically apparent nodal disease. As such, the opinions expressed may not reflect those presenting with extensive disease, prolonged treatment courses, and iterative operations. However, the study cohort is representative of patients with the most common presentation of papillary thyroid cancer, and likely reflects the perspectives of the majority of patients. In addition, the analysis only included information for up to one year following surgery for any given participant. It is possible that opinions of having the “good cancer” may change after years of follow-up or possible recurrences. Lastly, 10 interviewers performed the 113 interviews included, which averages to 11 interviews per interviewer. This relatively small number of interviews performed per interviewer may have introduced some heterogeneity in the interviews, although all interviewers were trained in qualitative interviews and adhered to a semi-structured guide to help reduce variability.
Conclusion
Patients with papillary thyroid cancer commonly encounter the “good cancer” perspective from multiple sources shortly after their diagnosis. For many, this perspective has a positive connotation, but for others, conceptualizing cancer as “good” is confusing and invalidating. Patients advise avoiding “good cancer” terminology and similar language that diminishes their cancer diagnosis. Instead, healthcare providers should reassure patients with facts about effective treatments, low recurrence rates, and high survival rates in order to provide patients with the freedom to assign their own individual value to their cancer experience.
Acknowledgments
Support for this research included the University of Wisconsin Carbone Cancer Center Support Grant P30 CA014520 and the National Cancer Institute of the National Institutes of Health award number R01CA176911. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This study was presented at the 25th Annual Meeting of the American Association of Clinical Endocrinologists in Orlando, Florida May, 2016.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Cramer JD, Fu P, Harth KC, Margevicius S, Wilhelm SM. 2010. Analysis of the rising incidence of thyroid cancer using the Surveillance, Epidemiology and End Results national cancer data registry. Surgery 148:1147–1152 [DOI] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KD, Jemal A. 2016. Cancer statistics, 2016. CA Cancer J Clin 66:7–30 [DOI] [PubMed] [Google Scholar]
- 3.Applewhite MK, James BC, Kaplan SP, Angelos P, Kaplan EL, Grogan RH, Aschebook-Kilfoy B. 2016. Quality of life in thyroid cancer is similar to that of other cancers with worse survival. World J Surg 40:551–561 [DOI] [PubMed] [Google Scholar]
- 4.Aschebrook-Kilfoy B, James B, Nagar S, Kaplan S, Seng V, Ahsan H, Angelos P, Kaplan EL, Guerro MA, Kuo JH, Lee JA, Mitmaker EJ, Moalem J, Ruan DT, Shen WT, Grogan RH. 2015. Risk factors for decreased quality of life in thyroid cancer survivors: initial findings from the North American Thyroid Cancer Survivorship Study. Thyroid 25:1313–1321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Easley J, Miedema B, Robinson L. 2013. It's the “good” cancer, so who cares? Perceived lack of support among young thyroid cancer survivors. Oncol Nurs Forum 40:596–600 [DOI] [PubMed] [Google Scholar]
- 6.Gamper EM, Wintner LM, Rodrigues M, Buxbaum S, Nilica B, Singer S, Giesinger JM, Holzner B, Virgolini I. 2015. Persistent quality of life impairments in differentiated thyroid cancer patients: results from a monitoring programme. Eur J Nucl Med Mol Imaging 42:1179–1188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roberts KJ, Lepore SJ, Urken ML. 2008. Quality of life after thyroid cancer: an assessment of patient needs and preferences for information and support. J Cancer Educ 23:186–191 [DOI] [PubMed] [Google Scholar]
- 8.Singer S, Husson O, Tomaszewska IM, Locati L, Kiyota N, Scheidemann-Wesp U, Hofmeister D, Winterbotham M, Brannan C, Araujo C, Gamper E, Kulis D, Rimmele H, Andry G, Licitra L. 2016. Quality of life priorities in patients with thyroid cancer—a multi-national EORTC phase I study. Thyroid 26:1605–1613 [DOI] [PubMed] [Google Scholar]
- 9.Dow KH, Ferrell BR, Anello C. 1997. Balancing demands of cancer surveillance among survivors of thyroid cancer. Cancer Pract 5:289–295 [PubMed] [Google Scholar]
- 10.Hyun YG, Alhashemi A, Fazelzad R, Goldberg AS, Goldstein DP, Sawka AM. 2016. A systematic review of unmet information and psychosocial support needs of adults diagnosed with thyroid cancer. Thyroid 26:1239–1250 [DOI] [PubMed] [Google Scholar]
- 11.Goldfarb M, Casillas J. 2016. Thyroid cancer-specific quality of life and health-related quality of life in young adult thyroid cancer survivors. Thyroid 26:923–932 [DOI] [PubMed] [Google Scholar]
- 12.Morley S, Goldfarb M. 2015. Support needs and survivorship concerns of thyroid cancer patients. Thyroid 25:649–656 [DOI] [PubMed] [Google Scholar]
- 13.Sawka AM, Goldstein DP, Brierley JD, Tsang RW, Rotstein L, Ezzat S, Straus S, George SR, Abbey S, Rodin G, O'Brien MA, Gafni A, Thabane L, Goguen J, Naeem A, Magalhaes L. 2009. The impact of thyroid cancer and post-surgical radioactive iodine treatment on the lives of thyroid cancer survivors: a qualitative study. PloS One 4:e4191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ramsey S, Blough D, Kirchhoff A, Kreizenbeck K, Fedorenko C, Snell K, Newcomb P, Hollingworth W, Overstreet K. 2013. Washington State cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Aff 32:1143–1152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Almendrala A. 2015. Why you should stop calling thyroid cancer “good cancer.” The Huffington Post, February 6
- 16.Mullin E. 2015. Is thyroid cancer the “good” cancer? It doesn't feel that way when you get it. The Washington Post, September 7
- 17.Charmaz K. 2014. Constructing Grounded Theory. Second edition. Sage, Thousand Oaks, CA, pp 162–195 [Google Scholar]
- 18.Tanco K, Rhondali W, Perez-Cruz P, Tanzi S, Chisholm GB, Baile W, Frisbee-Hume S, Williams J, Masino C, Cantu H, Sisson A, Arthur J, Bruera E. 2015. Patient perception of physician compassion after a more optimistic vs a less optimistic message: a randomized clinical trial. JAMA Oncol 1:176–183 [DOI] [PubMed] [Google Scholar]
- 19.Aschebrook-Kilfoy B, Ward MH, Sabra MM, Devesa SS. 2011. Thyroid cancer incidence patterns in the United States by histologic type, 1992–2006. Thyroid 21:125–134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Detmar SB, Aaronson NK, Wever LD, Muller M, Schornagel JH. 2000. How are you feeling? Who wants to know? Patients' and oncologists' preferences for discussing health-related quality-of-life issues. J Clin Oncol 18:3295–3301 [DOI] [PubMed] [Google Scholar]