Abstract
Objective
Accurate and complete long-term post-operative outcome data is critical to improving value in healthcare delivery. The Society for Vascular Surgery – Vascular Quality Initiative (VQI) is an important tool to achieve this goal in vascular surgery. To improve on the capture of long term outcomes after vascular surgery procedures for patients in the VQI, we sought to match VQI data to Medicare Claims for comprehensive capture of major clinical outcomes in the first several years following vascular procedures.
Methods
Patient and procedure characteristics for abdominal aortic aneurysm procedures captured in the SVS-VQI between January 1, 2002, and December 31, 2013 were matched to Medicare claims data using an indirect identifier methodology. Late outcomes captured in the VQI and in Medicare claims were compared.
Results
Matching procedures yielded 9,895 endovascular aneurysm repair (EVAR) patients (82.4% of eligible VQI patients) and 3,405 open aneurysm repair (OAR) patients (74.4% of eligible). Comparison of patients that did and did-not match to a Medicare claim demonstrated similar patient and procedure characteristics. Evaluation of late outcomes revealed good patient-level agreement on mortality for both EVAR (kappa 0.64) and OAR (kappa 0.82). Post-operative reintervention rates demonstrated lower agreement for both EVAR (kappa 0.26) and OAR (kappa 0.16).
Conclusions
This work demonstrates the feasibility of an algorithm using indirect identifiers to match VQI patients and procedures to Medicare claims data. The refinement of this strategy will focus on establishing and improving algorithms related to identifying and categorizing late events after EVAR, and may serve as a mechanism to ensure the best quality follow-up information is achieved within the Vascular Quality Initiative.
BACKGROUND
The Society for Vascular Surgery Vascular Quality Initiative (SVS-VQI) is a national quality improvement network organized a patient safety organization. It is an Agency for Healthcare Research and Quality (AHRQ) Patient Safety Organization (PSO) with restrictions and protections on the use of patient, procedure and outcome information for the express use of quality improvement and research.1 Data is prospectively collected by participating centers within the PSO and composed in a secure setting allowing de-identified outcome comparisons between participating provider groups. VQI data is collected for the perioperative period and at 1-year in follow-up giving the ability to evaluate perioperative and late outcomes.2
The emphasis on outcomes beyond the perioperative period represents a unique element of the VQI and reflects the chronic nature of vascular disease. However, comprehensive collection of long term outcome data is time consuming and problematic. For example, prior research has shown considerable variation in follow-up at one year within the VQI, for patient, provider, and center-specific reasons3. While the explicit goal is to provide at least 80% follow-up for all procedures entered in the VQI, recent review of data entered suggests that the rate of 1-year follow-up is substantially below this threshold.4
Vascular disease affects older Americans, many of whom are 65 years and older and are enrolled in Medicare. The comprehensive data available in Medicare claims affords an opportunity to track outcomes for patients undergoing procedures tracked by VQI regardless of location and time of follow-up. The strategy of matching specific patient data to Medicare claims has been used by institutions5–7 and by registries such as the Surveillance Epidemiology and End Result Program (SEER),8–11 National Cardiovascular Data Registry (NCDR)12, 13 and the National Surgical Quality Improvement Program (NSQIP)14 using various strategies. In particular, many have utilized an indirect identifier strategy where patient information available in both registry data and Medicare claims are the data fields for linkage including date and location of procedure, and birthdate and gender of patient.7, 12, 13
Here we describe our efforts to evaluate the feasibility and potential of using indirect identifiers to match VQI data with Medicare claims data. While matching efforts have been performed for nearly all procedures entered in the VQI dataset, as a descriptive model herein we describe the treatment of infrarenal abdominal aortic aneurysm either by Endovascular aortic Aneurysm Repair (EVAR) or Open aortic Aneurysm Repair (OAR).
METHODS
Data Source
Procedure and perioperative data for patients undergoing EVAR and OAR is entered by each participating center into the VQI registry using a web-based system maintained by M2S, Inc (Lebanon, NH). At the time of 1-year follow-up (defined as 9 to 21 months post procedure) additional outcome data is collected and similarly maintained and protected. Patient-specific, peri-operative VQI data contains pre-surgical, surgical and in-hospital post-operative information. Follow-up data includes death, reinterventions and procedure specific outcomes. Data collection in the VQI began in 2003.
The Medicare inpatient claims dataset contains reimbursed inpatient hospital claims for Medicare beneficiaries. Hospitals, providers and beneficiaries were identifiable with unique identification numbers that allowed linking across annual datasets. Until December 31, 2005, a random 20% of claims were available and afterward 100% of claims were available. Longitudinal data was not available on Medicare Beneficiaries that are enrolled in non fee-for-service, health maintenance organization programs such as Medicare Part C or Medicare Advantage plan. Patients that left Medicare fee-for-service and entered any of these alternate programs were censored at the time of their switch. The Medicare Denominator file was used to identify death dates. To reduce computational burden of matching with VQI data, the Medicare dataset was restricted to patients with a hospital admission containing International Classification of Diseases Ninth Revision (ICD-9) procedure codes for open or endovascular aortic aneurysm repair.
Data protection
Data collected within the VQI is compiled on servers secured and maintained by M2S, Inc. As a provision of the PSO designation of the SVS-VQI, all unique identifiers of patient, provider and center are prohibited from dissemination. Mortality data derived from center reporting and is supplemented by linkage to the Social Security Death Index (SSDI) database.
Medicare inpatients claims data is secured and maintained within The Dartmouth Institute - Data Analytic Core (TDI-DAC). Matching of VQI and Medicare claims data is performed within the TDI-DAC with VQI data provided from M2S, Inc. via secure crosswalk that maintains data integrity and confidentiality as outlined in the SVS-PSO charter. (Figure 1) The data security, data use and analytic plan were all evaluated by the SVS-VQI and TDI-DAC and this work was approved by the Dartmouth College Institutional Review Board.
Figure 1.
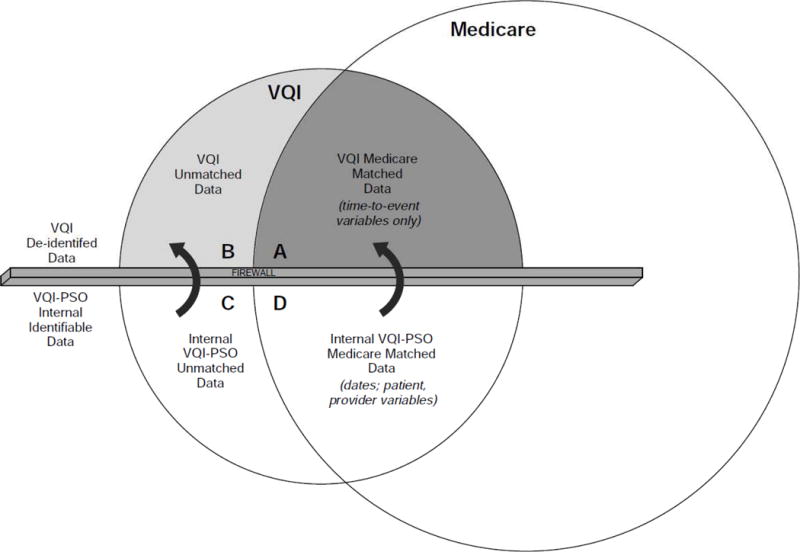
Graphical representation of data security and matching process. All patient and physician identifiers are securely maintained within the VQI and TDI (Group C and Group D). Only de-identified matched (Group A) and unmatched (Group B) data leave the secure environment for review including quality improvement and research work.
Matching
Because of direct patient and provider identifiers were not legally permissible by AHRQ PSO rules to exchange between the VQI and Medicare, matching was performed using an indirect identifier methodology similar to that described previously.2, 7, 13 We maximized our matching efficiency through three rounds of a two-step matching process. (Figure 2). This two-step process was developed after pilot-testing several one-step processes to determine which combinations would yield the highest number of direct matches, without the occurrence of duplicative matching (i.e., matching more than one patient to the same Medicare claim record).
Figure 2.
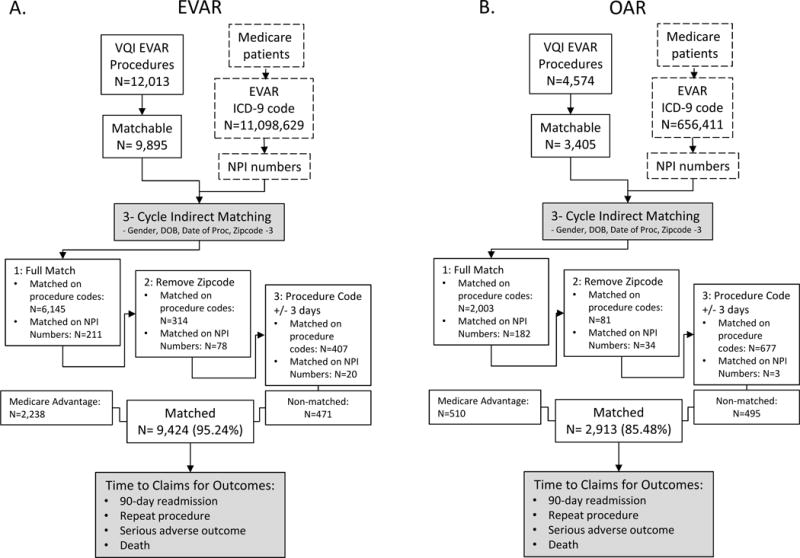
Flow diagram for matching procedures for patients that have undergone EVAR (A) and OAR (B).
In the first step, matching was performed by matching ICD-9 procedure code (see Appendix I for complete listing of codes used), date of surgery, and patient date of birth, gender, and three-digit zip code prefix of residence on the date of surgery. Exact correlation of all five criteria constitutes a positive match. The second step substituted the National Provider Identifier (NPI) number of the surgeon/interventionalist for the ICD-9 applied the same strategy to the remaining unmatched patients. These two steps were repeated for two additional rounds of matching. In the second round of matching, zip code was eliminated from the matching process. In the third round, the procedure date was broadened to plus or minus three-days. This strategy of successively less-restrictive matching criteria on a progressively smaller cohort of patients was performed to maximize matching efficiency. Sensitivity analyses revealed that this hierarchical approaches among unmatched patients garners additional matches without resulting in duplicative matching.
This matching strategy was applied to a cohort of VQI patients 65-years and older that underwent EVAR or OAR between January 2003 (the earliest VQI data) and December 31, 2013 (the latest Medicare data available). Follow-up rates for patients in the Vascular Quality Improvement registry were between 70–75% during the time intervals considered in this study.
Outcomes
Once we had matched cases between the VQI data and the Medicare data, we measured outcomes across all available years (2003 to 2013) of Medicare inpatient claims data. Outcomes were measured starting on the date of discharge following the hospital admission for the index procedure. Outcomes that occurred during the index hospital admission were not recorded, since those are captured in detail in the VQI dataset. Late outcomes were defined as within two years post-procedure because the 1-year VQI follow-up window between 2003 and 2013 was defined as 9–21 months post-procedure.
We identified four outcomes in the Medicare data: death, aortic aneurysm rupture, repeat aortic aneurysm repair procedures, and 90-day hospital readmissions. Death was identified in the Medicare denominator file. Cause of death is not available in this dataset. Aortic aneurysm rupture was recorded as an outcome when inpatient hospital claims indicated primary diagnosis on a subsequent admission was aortic rupture. However, if someone came to the emergency room and with a ruptured aorta and died before admission, that was recorded as a death.
VQI data is linked to mortality data from the Social Security Death Index on a bi-annual basis. Repeat procedures were any secondary AAA repair or intervention for aneurysm-related complications following the index procedure. Ninety day hospital readmissions were measured for 90 days following discharge from the index hospitalization. Using the array of diagnostic codes that accompany each admission, we categorized the reasons for readmission as being related to the surgery (e.g. vascular complication, post-operative infection, cardiac complications, etc.; complete list in Appendix I).
As a provision of the SVS-VQI PSO designation, sharing of potential patient or provider identifying data is prohibited. Therefore, post-operative events were converted to time to event variables. For each outcome, we calculated days to the outcome following the discharge from the index admission. Also for each event, we provided the ICD-9 codes for the outcome.
Validation
Raw match rate was calculated for EVAR and OAR by dividing matched patient numbers by the total VQI cohort with potential to match in fee-for-service Medicare based on patient age (65-years and older), US citizenship, and procedure within the available range of our Medicare denominator file. Patients determined to be in a non-fee-for-service program (Medicare Advantage, etc.) were included in the match rate calculation, but did not have data available for determination of outcomes. Patient characteristics were compared between those that matched to Medicare claims data and those that did not using chi-square for categorical variables and two-way unpaired t-test for continuous variables. Fidelity of outcome measurement was evaluated in matched subjects by comparing post-operative reintervention that were captured by both VQI and Medicare. (See Appendix I for complete list of events and corresponding ICD-9 codes.) Similarly, mortality in matched subjects was compared between VQI and Medicare data. These analyses were limited only to the successfully matched patients.
Outcome agreement for reintervention and mortality between VQI and Medicare data was determined using Cohen’s Kappa. The Kappa for rare events was adjusted using the correction of Ciccetti and Feinstein.15, 16 Additional time-to-event comparisons were performed with Kaplan-Meier estimates. We obtained IRB approval from the Center for the Protection of Human Subjects at Dartmouth for this work, and no individual patient informed consent was deemed necessary.
RESULTS
Between 1/1/2003 and 12/31/2013, 12,031 EVAR procedures and 4,574 OAR procedures have been captured in the VQI. Our study cohort of patients aged 65-years and older undergoing procedures in this timeframe included 9,895 EVAR patients and 3,405 OAR patients. Of these there were 9,424 (95.2%) matched EVAR patients and 2,913 (85.5%) matched OAR patients. (Figure 2)
Patient Characteristics
Medicare-matched and unmatched patients 65-years and older were compared for both EVAR and OAR. Demographics and patient characteristics were similar for patients undergoing both EVAR and OAR. Differences between matched and unmatched cohorts included a slightly higher likelihood of male sex, white race, preoperative living at home and non-urgent/emergent procedure in the Medicare-matched cohort. In addition, unmatched patients that underwent EVAR were slightly more likely to be unfit for open surgical repair. Prior work has suggested that this subjective assessment of patient functional status is associated with long-term outcomes17. There were no significant differences between cohorts in comorbidities, smoking status, or prior vascular procedures. (Table 1)
Table 1.
Characteristics of VQI patients 65 years and older that were matched and un-matched to Medicare claims for EVAR (left columns) and OAR (right columns).
| EVAR | OAR | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Patient Characteristic, n/N* (%) | VQI-Medicare Matched (N=7,159) |
VQI Unmatched (N=3,035) |
p-valueˆ | VQI-Medicare Matched (N=2,399) |
VQI Unmatched (N=1,095) |
p-valueˆ |
| Age (Median, IQR) | 76,10 | 75,11 | 0.001 | 74,9 | 72,10 | 0.001 |
| Male Sex | 5646/7159 (78.9) | 2444/3033(80.6) | 0.050 | 1676/2395 (70.0) | 808/1095 (73.8) | 0.014 |
| White Race | 6748/7158 (94.3) | 2714/3029 (89.6) | <0.001 | 2291/2394 (95.7) | 979/1091 (89.7) | <0.001 |
| Smoking | 0.001 | 0.005 | ||||
| Prior smoking | 4092/7131 (57.4) | 1613/2999 (53.8) | 1205/2363 (51.0) | 485/1077 (45.0) | ||
| Current Smoking | 1894/7131 (26.6) | 897/2999(29.9) | 872/2363 (36.9) | 442/1077 (41.0) | ||
| HTN | 6019/7133 (84.4) | 2521/3009 (83.8) | 0.449 | 1974/2380 (82.9) | 928/1086 (85.5) | 0.063 |
| Diabetes | 1424/7132 (20.0) | 591/3006 (19.7) | 0.725 | 377/2377 (15.9) | 154/1083 (14.2) | 0.214 |
| CAD | 2185/7129 (30.7) | 925/3003 (30.8) | 0.879 | 713/2369 (30.1) | 284/1083 (26.2) | 0.020 |
| COPD | 2342/7127 (32.9) | 994/3006 (33.1) | 0.840 | 855/2375 (36.0) | 368/1085 (33.9) | 0.234 |
| CHF | 867/7131 (12.2) | 334/3008 (11.1) | 0.133 | 194/2370 (8.2) | 89/1084 (8.2) | 0.980 |
| Dialysis | 85/7145 (1.2) | 26/3009 (0.9) | 0.150 | 15/2387 (0.6) | 6/1086 (0.6) | 0.789 |
| Prior CABG or PCI | 1378/3741 (36.8) | 672/1900 (35.4) | 0.279 | 714/2365 (30.2) | 305/1080 (28.2) | 0.245 |
| Positive Preoperative Stress Test | 766/7106 (10.8) | 323/2996 (10.8) | 0.998 | 298/2377 (12.5) | 108/1083 (10.0) | 0.030 |
| Living at Home | 7019/7129 (98.5) | 2959/3005 (98.5) | 0.964 | 2360/2387 (98.9) | 1079/1084 (99.5) | 0.056 |
| Prior Aortic Surgery (any) | 307/7122 (4.3) | 148/3002 (4.9) | 0.169 | 204/2377 (8.6) | 81/1084 (7.5) | 0.271 |
| Urgency | <0.001 | 0.001 | ||||
| Symptomatic | 563/7130 (7.9) | 253/3011 (8.4) | 236/2393 (9.9) | 126/1088 (11.6) | ||
| Ruptured | 330/7130 (4.6) | 199/3011 (6.6) | 433/2393 (18.1) | 247/1088 (22.7) | ||
| Unfit for Open Repair | 1461/7124 (20.5) | 657/3001 (21.9) | 0.118 | N/A | N/A | N/A |
| Unfit for General Anesthesia | 218/7124 (3.1) | 90/3002 (3.0) | 0.868 | N/A | N/A | N/A |
observations with missing values tor each variable were not included in the analysis, percentage refers to column percentage
p-value for categorical/dichotomous variables from chi-square test, Student’s t-test for continuous variables
Mortality
In Medicare-matched subjects that underwent EVAR, we compared mortality rates between the VQI data and Medicare claims data. The positive percent agreement between VQI and Medicare data for death was 63% and negative percent agreement was 92%. This resulted in a Cohen’s Kappa of 0.55 for all post procedure time-points. Because the VQI specifically tracks 1-year outcomes, we also determined a 70% positive percent agreement and 94% negative percent agreement for death for patients with late follow-up in VQI and a two-year time window after discharge in Medicare, resulting in Kappa=0.64. The Kaplan-Meier estimates for survival after EVAR comparing VQI and Medicare claims data demonstrated statistically significant divergence of mortality rates between the two datasets with a higher mortality rate for Medicare claims data compared to the SSDI-linked VQI data (p<0.001, Figure 3a)
Figure 3.
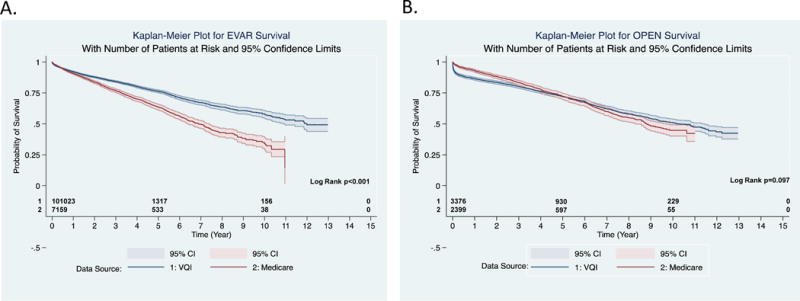
Kaplan-Meier estimate for survival after EVAR (A) and OAR (B) as collected in the VQI (blue) and in Medicare claims data (red).
Mortality rates between the VQI data and Medicare claims data for patients that underwent OAR also had moderate agreement. The positive percent agreement between VQI and Medicare data for death was 64% and negative percent agreement was 86% in the VQI data. This resulted in a Cohen’s Kappa of 0.51 for all post procedure time-points. The 1-year mortality after OAR demonstrated a 86% positive percent agreement and 96% negative percent agreement for the VQI data to detect death for patients with late follow-up in VQI and a two-year time window after post-procedure discharge in Medicare, resulting in Kappa=0.82. The Kaplan-Meier estimates for survival after OAR comparing VQI and Medicare claims data demonstrated statistically significant divergence of mortality rates between the two datasets with a higher mortality rate for Medicare claims data compared to the SSDI-linked VQI data at one year following the procedure (p<0.001, figure 3b), but these differences had disappeared by five year following the procedure among the matched VQI-Medicare patients.
Reintervention
Comparison of reintervention rates after EVAR between VQI and Medicare claims data demonstrated a positive percent agreement of 29% and negative percent agreement of 92% with a kappa of 0.23. Pearson’s r=0.20 for the correlation between counts of reinterventions in Medicare and VQI at all time-points. Reintervention rates in the patients with late follow-up in VQI and a two-year time window after discharge in Medicare demonstrated a positive percent agreement of 33% and negative percent agreement of 91% for a kappa of 0.26. Pearson’s r=0.20 for the correlation between counts of reinterventions among VQI patients with late follow-up and Medicare claims two years post-procedure. The low kappa is driven by reinterventions present in one data source, but not present in the other. For example, 524 of 647 reinterventions (81%) captured in Medicare claims data were not captured in VQI while 82 of 205 reinterventions (40%) captured in VQI did not have an associated Medicare claim. The Kaplan-Meier estimates for reintervention after EVAR comparing VQI and Medicare claims data demonstrate clear difference at early time points that disappear at late time points as the number at risk in the VQI data drops. (p<0.001, Figure 4a)
Figure 4.
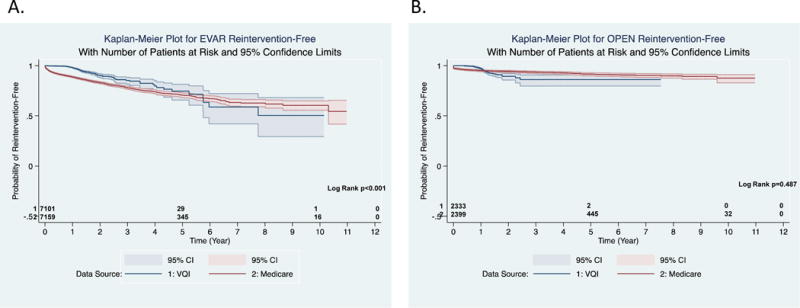
Kaplan-Meier estimate for freedom from reintervention after EVAR (A) and OAR (B) as collected in the VQI (blue) and in Medicare claims data (red).
Similar results were obtained after OAR with reintervention rate comparison between VQI and Medicare yielding a positive percent agreement of 12% and negative percent agreement of 96% for a Kappa of 0.07 at all time-points. Pearson’s r=0.06 for the correlation between counts of reinterventions in Medicare and VQI. The reintervention rates in patients with late follow-up in VQI and a two-year time window after discharge in Medicare demonstrated a positive percent agreement of 21% and negative percent agreement of 95% with a Kappa of 0.16. Pearson’s r=0.13 for the correlation between counts of reinterventions among VQI patients with long-term follow-up and Medicare claims two years post-procedure. Like the EVAR data, there were 70 out of 79 reinterventions (89%) captured in Medicare claims data were not captured in VQI and 68 of 77 (88%) captured in VQI did not have an associated Medicare claim. However, the Kaplan-Meier estimates for reintervention after OAR comparing VQI and Medicare claims data demonstrate no difference in of intervention capture at late time points in VQI. (p=0.497, Figure 4b).
DISCUSSION
For patients facing vascular treatments, understanding surgical outcomes beyond the peri-operative period is essential for measuring the value of our interventions. To this end, we have developed, and described herein a methodology for determining post-operative events in Medicare beneficiaries treated with procedural interventions such as aortic surgery. Our match rate was 95.2% for EVAR and 85.5% for OAR. These rate are similar to those described by others using indirect identifier methodology. Specifically, two studies used patient gender, patient date of birth, hospital admission date and hospital ID to match Medicare claims to the NCDR with match rates of 75.2% for PCI12 and 56% for ICD implantation.13 In surgery, the addition of CPT and ICD-9 coding to the matching algorithm resulted in an 80.5% match rate in the NSQIP database to Medicare claims.7
Other studies have achieved higher rates of matching by use of a direct identifier match based on Social Security Number1, 9, 10, 12 with match rates between 91% and 98%. However, because VQI collects data within an AHRQ PSO, data sharing is strictly regulated and, at this time, precludes use of direct patient identifiers. Efforts to develop the pathways necessary to preserve patient anonymity, yet still allow direct Medicare matching “within the PSO” are underway, and will be used for future renditions of this work. Other large cardiovascular registries, such as the American College of Cardiology and the Society for Thoracic Surgery, have reported similar success rates using a variety of matching strategies18, 19. Similarly, national registries for transplantation have been successfully linked to Medicare for evaluation of long-term outcomes20.
We achieved a moderate degree of accuracy in detection of late mortality in our matched patients with a Cohen’s Kappa of 0.64 for EVAR and 0.82 for OAR. However, agreement decreased when all time-points were evaluated. This is further demonstrated by Kaplan-Meier analysis for survival which demonstrated a statistically significant divergence in mortality curves based on the source dataset. Interestingly, the rate of mortality was higher in the Medicare dataset compared to VQI even though the VQI data was linked to SSDI prior to being matched to Medicare.
In contrast, in our evaluation, detection of reintervention was less effective when considering potentially disparate data sources of VQI and Medicare claims. We noted that 81% of reinterventions after EVAR and 89% of reinterventions after OAR had a Medicare claim but were not captured in VQI. Similarly, 40% of EVAR reinterventions and 89% of OAR reinterventions captured in VQI lacked an associated Medicare claim. Many of these differences, we hypothesize, are likely are due to differences between the Medicare events we used to define re-intervention – generally ICD-9 procedure codes indicative of an inpatient stay – and much broader VQI-based definitions, which may be indicative of outpatient procedures such as an endoleak embolization. Improvement and harmonization of our coding algorithms, especially outpatient procedures, will be the focus of our future work in an effort to improve the ability of our linked datasets to successfully describe the long-term outcomes of aortic aneurysm repair using linked clinical-claims datasets. Further, additional work needs to be done to determine if these reflect true missed events, or simply an error in the correlation of late events between Medicare and VQI.
A number of limitations are present within our analysis, largely due to the de-identified nature of our data. We are unable to directly identify patients and therefore sensitivity analysis is limited to specific outcomes captured in both datasets. Further, because of the potential for errors within either dataset, no gold-standard is easily determined, and future validation efforts will necessitate chart-level validation of both registry and claims datasets. Prior analyses examining the weaknesses of claims-based datasets have shown that different coding algorithms can affect the absolute rates of important outcomes, such as stroke following carotid revascularization21. Further, characterization of patient-level events using administrative claims can result in differences that may not accurately reflect true patient risk strata22.
Our future work will focus on: (1) revising and optimizing our matching algorithm without sacrificing fidelity, (2) ensuring complete and reliable capture of late events in the Medicare claims data across datasets including, but not limited to EVAR. Improving out matching algorithm will entail development of a multi-step matching algorithm balancing maximum matching efficiency with accurate capture. Continuing to develop the ICD-9 code selection for reintervention and readmission will improve the quality of our capture of late events. Subsequent to algorithm optimization, we intend to apply these strategies to all procedures captured by the VQI. Eventually, as regulatory mechanisms allow transmission of patient identifiers between a PSO and Medicare claims, we look forward to the opportunity to perform direct, non-probabilistic matching between patients in VQI and their respective Medicare claims.
CONCLUSIONS
Matching of patient-level VQI and Medicare claims data has the potential to be a powerful tool for the evaluation of long-term post-operative outcomes for patients undergoing vascular procedures. Our initial work has demonstrated feasibility of matching procedures and future work will focus on refinement and broad application of this methodology to provide comprehensive outcome data with the ultimate goal of improving care for all patients undergoing vascular procedures.
Acknowledgments
Disclosure: Drs. Goodney and Sedrakyan were supported by U01 FD005478 (Sedrakyan, PI), from the US Food and Drug Administration (FDA), for creation of The Vascular Implant Surveillance and Interventional Outcomes Network (VISION)
Appendix 1: List of clinical events and the corresponding administrative data codes used in our analysis
ICD-9 Diagnostic and Procedure Codes used for matching and identification of outcomes An X in the code indicates that any number 0–9 could go in that place.
Matching: Open Abdominal aortic aneurysm Repair (OAR)
38.34, 38.44, 38.64, 39.52, 39.7X, 44.22
Matching: Endovascular Abdominal aortic aneurysm Repair (EVAR)
38.04, 38.06, 38.08, 38.14, 38.16, 38.18, 38.34, 38.36, 38.38, 38.44, 38.46, 38.48, 38.64, 38.66, 38.68, 38.84, 38.86, 38.88, 38.91, 38.93, 39.25, 39.26, 39.29, 39.30, 39.31, 39.50, 39.51, 39.52, 39.54, 39.56, 39.57, 39.58, 39.59, 39.71, 39.72, 39.73, 39.74, 39.75, 39.76, 39.77, 39.78, 39.79, 39.90
Outcome: aortic rupture diagnostic codes
441.3X
Outcome: open abdominal aortic aneurysm reintervention
38.34, 38.44, 38.64, 39.52, 39.7X, 44.22 (procedures)
996.1, 996.59, 996.6, 441.3, 441.5, 440.0, 995.7, 444.2x, 444.8x (diagnosis of postsurgical complications)
Outcome: categories for 90-day Readmissions (ICD-9 Diagnostic codes anywhere in the admission code string)
Vascular complications: 997.71, 997.72, 997.79
Postoperative Infection: 998.5x, 998.51, and 998.59
Postoperative stroke: 997.02
Cardiac complications: 997.1x, 428.0x, 428.1x, 428.2x, 428.3x, 428.4x, 428.9x, 427.0x, 427.3x, 427.4x, 427.5x, 427.8x, 427.9x
Urinary/renal complications: 997.5x, 593.3x, 593.9x
GI Complications: 997.4x, 560.9x, 557.0x, 557.9x
Respiratory complications: 997.3x, 518.4x, 518.5x
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.AHRQ. Patient safety rule. 2009 [Google Scholar]
- 2.Cronenwett JL, Kraiss LW, Cambria RP. The society for vascular surgery vascular quality initiative. Journal of vascular surgery. 2012;55:1529–1537. doi: 10.1016/j.jvs.2012.03.016. [DOI] [PubMed] [Google Scholar]
- 3.J DR, Simons JP, Flahive JM, Patel VI, Nolan BW, Bachman M, Healey CT, Schanzer A. Determinants of follow-up failure in patients enrolled in the vascular study group of new england (vsgne) Journal of vascular surgery. 2015;61:154–155. [Google Scholar]
- 4.Vascular study group of new england semi-annual meeting. 2015 [Google Scholar]
- 5.Weiner M, Stump TE, Callahan CM, Lewis JN, McDonald CJ. A practical method of linking data from medicare claims and a comprehensive electronic medical records system. International journal of medical informatics. 2003;71:57–69. doi: 10.1016/s1386-5056(03)00089-3. [DOI] [PubMed] [Google Scholar]
- 6.Hammill BG, Hernandez AF, Peterson ED, Fonarow GC, Schulman KA, Curtis LH. Linking inpatient clinical registry data to medicare claims data using indirect identifiers. American heart journal. 2009;157:995–1000. doi: 10.1016/j.ahj.2009.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mark TL, Lawrence W, Coffey RM, Kenney T, Chu BC, Mohler ER, 3rd, Steiner C. The value of linking hospital discharge and mortality data for comparative effectiveness research. Journal of comparative effectiveness research. 2013;2:175–184. doi: 10.2217/cer.13.4. [DOI] [PubMed] [Google Scholar]
- 8.Potosky AL, Riley GF, Lubitz JD, Mentnech RM, Kessler LG. Potential for cancer related health services research using a linked medicare-tumor registry database. Medical care. 1993;31:732–748. [PubMed] [Google Scholar]
- 9.Bradley CJ, Given CW, Luo Z, Roberts C, Copeland G, Virnig BA. Medicaid, medicare, and the michigan tumor registry: A linkage strategy. Medical decision making: an international journal of the Society for Medical Decision Making. 2007;27:352–363. doi: 10.1177/0272989X07302129. [DOI] [PubMed] [Google Scholar]
- 10.Nadpara PA, Madhavan SS. Linking medicare, medicaid, and cancer registry data to study the burden of cancers in west virginia. Medicare & medicaid research review. 2012;2 doi: 10.5600/mmrr.002.04.a01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Setiawan VW, Virnig BA, Porcel J, Henderson BE, Le Marchand L, Wilkens LR, Monroe KR. Linking data from the multiethnic cohort study to medicare data: Linkage results and application to chronic disease research. American journal of epidemiology. 2015;181:917–919. doi: 10.1093/aje/kwv055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brennan JM, Peterson ED, Messenger JC, Rumsfeld JS, Weintraub WS, Anstrom KJ, Eisenstein EL, Milford-Beland S, Grau-Sepulveda MV, Booth ME, Dokholyan RS, Douglas PS. Linking the national cardiovascular data registry cathpci registry with medicare claims data: Validation of a longitudinal cohort of elderly patients undergoing cardiac catheterization. Circulation Cardiovascular quality and outcomes. 2012;5:134–140. doi: 10.1161/CIRCOUTCOMES.111.963280. [DOI] [PubMed] [Google Scholar]
- 13.Setoguchi S, Zhu Y, Jalbert JJ, Williams LA, Chen CY. Validity of deterministic record linkage using multiple indirect personal identifiers: Linking a large registry to claims data. Circulation Cardiovascular quality and outcomes. 2014;7:475–480. doi: 10.1161/CIRCOUTCOMES.113.000294. [DOI] [PubMed] [Google Scholar]
- 14.Lawson EH, Ko CY, Louie R, Han L, Rapp M, Zingmond DS. Linkage of a clinical surgical registry with medicare inpatient claims data using indirect identifiers. Surgery. 2013;153:423–430. doi: 10.1016/j.surg.2012.08.065. [DOI] [PubMed] [Google Scholar]
- 15.Feinstein AR, Cicchetti DV. High agreement but low kappa: I. The problems of two paradoxes. Journal of clinical epidemiology. 1990;43:543–549. doi: 10.1016/0895-4356(90)90158-l. [DOI] [PubMed] [Google Scholar]
- 16.Cicchetti DV, Feinstein AR. High agreement but low kappa: Ii. Resolving the paradoxes. Journal of clinical epidemiology. 1990;43:551–558. doi: 10.1016/0895-4356(90)90159-m. [DOI] [PubMed] [Google Scholar]
- 17.De Martino RR, Brooke BS, Robinson W, Schanzer A, Indes JE, Wallaert JB, Nolan BW, Cronenwett JL, Goodney PP. Designation as “unfit for open repair” is associated with poor outcomes after endovascular aortic aneurysm repair. Circulation Cardiovascular quality and outcomes. 2013;6:575–581. doi: 10.1161/CIRCOUTCOMES.113.000095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brennan JM, Peterson ED, Messenger JC, Rumsfeld JS, Weintraub WS, Anstrom KJ, Eisenstein EL, Milford-Beland S, Grau-Sepulveda MV, Booth ME, Dokholyan RS, Douglas PS, Duke Clinical Research Institute DT Linking the national cardiovascular data registry cathpci registry with medicare claims data: Validation of a longitudinal cohort of elderly patients undergoing cardiac catheterization. Circulation Cardiovascular quality and outcomes. 2012;5:134–140. doi: 10.1161/CIRCOUTCOMES.111.963280. [DOI] [PubMed] [Google Scholar]
- 19.Jacobs JP, Edwards FH, Shahian DM, Haan CK, Puskas JD, Morales DL, Gammie JS, Sanchez JA, Brennan JM, O’Brien SM, Dokholyan RS, Hammill BG, Curtis LH, Peterson ED, Badhwar V, George KM, Mayer JE, Jr, Chitwood WR, Jr, Murray GF, Grover FL. Successful linking of the society of thoracic surgeons adult cardiac surgery database to centers for medicare and medicaid services medicare data. The Annals of thoracic surgery. 2010;90:1150–1156. doi: 10.1016/j.athoracsur.2010.05.042. discussion 1156–1157. [DOI] [PubMed] [Google Scholar]
- 20.Massie AB, Kucirka LM, Segev DL. Big data in organ transplantation: Registries and administrative claims. American journal of transplantation: official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2014;14:1723–1730. doi: 10.1111/ajt.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fokkema M, Hurks R, Curran T, Bensley RP, Hamdan AD, Wyers MC, Moll FL, Schermerhorn ML. The impact of the present on admission indicator on the accuracy of administrative data for carotid endarterectomy and stenting. Journal of vascular surgery. 2014;59:32–38 e31. doi: 10.1016/j.jvs.2013.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Finlayson EV, Birkmeyer JD, Stukel TA, Siewers AE, Lucas FL, Wennberg DE. Adjusting surgical mortality rates for patient comorbidities: More harm than good? Surgery. 2002;132:787–794. doi: 10.1067/msy.2002.126509. [DOI] [PubMed] [Google Scholar]


