Abstract
Background
Liver resections have classically been distinguished as “minor” or “major” based on number of segments removed. This is flawed since the number of segments resected alone does not convey the complexity of a resection. We recently developed a three-tiered classification for the complexity of liver resections based on utility weighting by experts. This study aims to complete the prior classification and to illustrate its application.
Study Design
Two surveys were administered to expert liver surgeons. Experts were asked to rate the difficulty of various open liver resections on a scale of 1–10. Statistical methods were then used to develop a complexity score for each procedure.
Results
66 of 135 (48.9%) surgeons responded to the prior survey, and 66 of 122 (54.1%) responded to the current survey. In all, 19 procedures were rated. The lowest mean score of 1.36—indicating least difficulty—was given to peripheral wedge resection. Right hepatectomy with IVC reconstruction was deemed most difficult with a score of 9.35. Complexity scores were similar for nine procedures present in both surveys. Caudate resection, hepaticojejunostomy, and vascular reconstruction all significantly increased the complexity of standard resections.
Conclusions
These data permit quantitative assessment of the difficulty of a variety of liver resections. The complexity scores generated allow for separation of liver resections into three categories of complexity (Low Complexity, Medium Complexity, and High Complexity) on a quantitative basis. This allows more accurate representation of the complexity of procedures in comparative studies.
Introduction
In 1956 Claude Couinaud introduced a classification that divided liver resections into “minor” types, (2 segments or less) and “major” types, (3 segments or more) (1). At that time, most resections of 2 segments or fewer were subsegmental resections or left lateral sectionectomies, and most resections of 3 or more segments were right or left hepatectomies. The “minor” procedures not only resected less liver but they were technically less complex. Thus the terms “minor” and “major” fit the procedures well both in terms of the amount of liver resected and the complexity of doing so. With time more kinds of liver resections were introduced, and it became evident that complexity of liver resection is not solely related to the amount of liver resected. For instance, several types of two-segment resections vary widely in complexity. Left lateral sectionectomy is a much less difficult procedure than right anterior sectionectomy though both are two-segment resections. Isolated resection of the caudate lobe is anatomically complex and the complexity of this “minor” procedure seems to be at least equal to that of some “major” resections. It is clear that the major/minor classification can lead to inappropriate comparison of outcomes since within these categories there is a wide range of complexity of procedures. Thus an improved method of classification which lessened this problem is desirable. This method would allow expression of variables in addition to size of as a determinant of complexity.
This is the second of two papers devoted to creating a new classification for the complexity of liver resections using utility grading, a powerful tool that allows weighting of multidimensional states. Experts may integrate many factors such as the number of segments resected, anatomic accessibility, proximity to major vascular structures, size of transection plane, and other variables to estimate complexity quantitatively.
In both studies, experts rated the complexity of liver resections on a scale from 1 to 10. The study was done in two parts to avoid taxing respondents with over 20 questions in one survey and compromising validity. Doing the study in two parts allowed repetition of questions in order to determine consistency of results. The first study, included 12 different liver resections (2). The results were used to complete a three-tier classification of complexity. This preliminary classification has been validated by Muangkaew, et al recently in a study of 150 liver resections for hepatocellular carcinoma (3). In the current study, nine resection types were reassessed to test for reproducibility. Also the effect of addition of vascular reconstruction, biliary reconstruction, and concomitant caudate lobe resection were assessed. All of these additions to standard resections are now performed with increasing frequency (4–7). In all, 19 different liver resections have been rated. Adjusted complexity scores were developed for each resection, and a new complexity classification was generated. Additionally, an example is provided in tabular form demonstrating how quantitative weighting of liver resection complexity can be used to compare two large groups of liver resections in order to determine whether they differ in complexity significantly.
Methods
Study Design
A five-question survey was administered by email to 122 expert liver surgeons in 13 countries from April 2015 through May 2015. The survey was anonymous and was created using a widely available internet tool (http://www.surveymonkey.com). The surgeons were identified primarily by contributions to the literature on hepatic surgery. The selection of experts was shifted somewhat from our prior study to include predominantly countries in North America and Europe in which English is a national language. This change was instituted because of a low response rate in the first survey from other countries (2).
The first four questions related to the country in which the surgeon was practicing, experience in liver surgery, and type of practice. The fifth question asked the experts to rate the complexity of various liver resections on a scale of 1–10. Level 1 was labeled as “easier,” and level 10 was labeled as “more difficult or complex.” The survey specified that all resections were to be considered open rather than laparoscopic procedures, and all resections other than peripheral wedge resection were to be considered anatomic in nature. The same survey was sent to all 122 surgeons. See the supplemental material for the actual survey questions.
Data Analysis
To increase the precision of measurement and statistical power, we pooled the data from the current survey (survey #2) with the first survey (survey #1) (2). A total of 19 procedures (3 procedures specific to survey #1, 7 procedures specific to survey #2, and 9 procedures common to both) were scored in the pooled data. As noted previously, the purpose of repeating 9 procedures in the second survey was to estimate consistency of results between the two surveys. Also, as the newly-added procedures involving caudate resections, vascular resections, and biliary-enteric anastomoses were expected to be rated as more complex, there was the possibility that this would systematically drive the scores of other procedures toward the “easier” end. To account for this possibility, a regression model using generalized estimating equation (GEE) was first fitted to estimate and compare the average scores for the 9 procedures common to both surveys after adjusting for surgeons’ characteristics including country (US vs. non-US) and the number of resections performed. GEE also allowed us to account for the correlation among scores from the same surgeon and provided an efficient way to handle repeated measurement data without requiring multivariate normal distribution (8). The results indicated only a slight shift (~4%) in the average scores, and the scores from the current survey were then aligned by multiplying 104% to each procedure. Next, similar GEE regression models were used to compare the average scores and rank the relative complexity among all procedures, as well as to assess the association between perceived complexity and other characteristics such as surgeon’s experience or practice patterns. The resultant p-values were corrected for multiple comparisons using false discovery rate (FDR) adjustment (9). All tests were two-sided and an adjusted p-value of 0.05 or less was taken to indicate statistical significance. The statistical analysis was performed using SAS 9.4 (SAS Institutes, Cary, NC). The Cochran–Armitage Test was used to evaluate the ranking of procedures in the hypothetical comparison of procedures given in the Discussion.
Results
Participant Demographics
122 surveys were administered. 110 of these were sent to North America and Europe. 66 of 122 (54.1%) surgeons responded to the survey. This was slightly higher than our previous response rate of 48.9% (2). 30 of 61 (49.2%) respondents that identified their location practiced in the United States, and 37 practiced in North America (60.7%). 17 (27.9%) surgeons practiced in Europe, and 3 (4.9%) practiced in Asia and South America. 5 surgeons did not list their location. Characteristics of the respondents are summarized in Table 1. Respondents from our prior study and this survey are compared.
Table 1.
Demographic Characteristics of Expert Surgeons
| Survey 1 | Survey 2 | |
|---|---|---|
| Country/ continent | ||
| USA | 34 | 30 |
| Canada | 5 | 7 |
| Europe | 12 | 17 |
| Asia | 12 | 3 |
| South America | 1 | 3 |
| Other | 0 | 1 |
| Unknown | 2 | 5 |
| No. of resections performed in career | ||
| 0–250 | 14 | 12 |
| 250–500 | 16 | 17 |
| 500–1000 | 18 | 23 |
| >1000 | 18 | 14 |
| No. of resections performed per year | ||
| 0 – 25 | 11 | 9 |
| 25 – 50 | 19 | 22 |
| 50 – 75 | 8 | 11 |
| 75 – 100 | 11 | 11 |
| >100 | 17 | 11 |
| Unknown | 1 | 2 |
| Practice type | ||
| HPB | 34 | |
| Liver surgery including transplantation | 15 | |
| Liver surgery without transplantation | 13 | |
| Surgical oncology | 3 | |
| Gastrointestinal surgery | 1 |
Participants were also asked their annual and career volume of liver resections as well as how they characterize their current practice. 37/66 surgeons (56.1%) have performed more than 500 resections in their career, while 29/66 (43.9%) have performed fewer than 500. 33 surgeons currently perform at least 50 liver resections per year. 34 of the 66 respondents characterized their practice as hepato-pancreato-biliary surgery (>50% pancreatobiliary surgery) (Table 1). 13 characterized their practice as primarily liver surgery but not transplantation. 15 surgeons’ practices included transplantation. 4 surgeons were primarily gastrointestinal surgeons or surgical oncologists (>50% non-HPB surgery).
Complexity Scores for 9 procedures common to both surveys
The mean scores of the nine procedures which were present in both surveys are shown in Table 2. In both cases the scores are adjusted for surgeon characteristics including country and the number of resections performed. The results were strikingly similar. The rank order in which the procedures were rated was identical in both studies. The absolute values were very similar but slightly lower in the second survey than in the first. This tendency was greater for procedures that were rated as more complex. In both surveys, peripheral wedge resection was rated least complex and left trisectionectomy with caudate resection was rated as the most complex of these 9 procedures.
Table 2.
Adjusted Complexity Scores for the 9 Procedures Scored in both Survey 1 and Survey 2
| Procedure | Survey 1 score (n, 95% CI) | Survey 2 score (n, 95% CI) |
|---|---|---|
| Peripheral wedge resection, < 3 cm | 1.365 (66, 1.018–1.712) | 1.328 (65, 1.148–1.508) |
| Left lateral sectionectomy | 2.011 (66, 1.687–2.335) | 1.917 (66, 1.704–2.131) |
| Left hepatectomy without caudate resection | 4.240 (33, 3.751–4.729) | 4.220 (65, 3.861–4.579) |
| Right hepatectomy | 4.919 (66, 4.584–5.254) | 4.629 (66, 4.287–4.972) |
| Left hepatectomy with caudate resection | 5.525 (33, 5.028–6.023) | 5.372 (66, 5.034–5.710) |
| Isolated caudate resection | 5.904 (66, 5.433–6.374) | 5.705 (66, 5.220–6.190) |
| Right trisectionectomy | 6.242 (66, 5.849–6.635) | 5.982 (65, 5.559–6.405) |
| Right anterior sectionectomy | 6.680 (65, 6.245–7.114) | 6.205 (66, 5.810–6.600) |
| Left trisectionectomy with caudate resection | 8.283 (32, 7.843–8.723) | 7.845 (64, 7.441–8.249) |
Adjusted Complexity Scores
Generalized Estimating Equations methods were used to adjust for the differences between surveys (see Methods). This allowed us to generate an adjusted complexity score for all queried procedures (Table 3). The scores derived from the current survey encompassed almost the entire possible range of complexity from 1 to 10. Peripheral wedge resection was rated as the easiest procedure with a score of 1.36. Left lateral sectionectomy was the second least complex procedure. There was a significant difference in the difficulty of wedge resection and left lateral sectionectomy versus all other resections. Thus, peripheral wedge resection and left lateral sectionectomy make up a group that is easily distinguished from all other procedures.
Table 3.
Adjusted Complexity Scores for All Surveyed Procedures
| Procedure | Adjusted complexity score (Mean +/− SE) | 95% Confidence interval |
|---|---|---|
| Peripheral wedge resection, < 3 cm | 1.361 +/− 0.594 | 1.244 – 1.477 |
| Left lateral sectionectomy | 1.994 +/− 0.776 | 1.840 – 2.148 |
| Left hepatectomy without caudate resection | 4.392 +/− 0.140 | 4.118 – 4.665 |
| Right hepatectomy | 4.866 +/− 0.124 | 4.622 – 5.110 |
| Right posterior sectionectomy | 5.479 +/− 0.223 | 5.042 – 5.917 |
| Left hepatectomy with caudate resection | 5.505 +/− 0.145 | 5.222 – 5.789 |
| Isolated caudate resection | 5.895 +/− 0.176 | 5.551 – 6.239 |
| Right trisectionectomy | 6.206 +/− 0.151 | 5.909 – 6.502 |
| Right anterior sectionectomy | 6.583 +/− 0.155 | 6.280 – 6.886 |
| Right hepatectomy with caudate resection | 6.767 +/− 0.171 | 6.432 – 7.101 |
| Right hepatectomy with hepaticojejunostomy | 6.850 +/− 0.186 | 6.486 – 7.215 |
| Anatomic middle hepatectomy | 7.205 +/− 0.205 | 6.804 – 7.607 |
| Right trisectionectomy with caudate resection | 7.239 +/− 0.181 | 6.885 – 7.594 |
| Left trisectionectomy without caudate resection | 7.378 +/− 0.330 | 6.732 – 8.024 |
| Right trisectionectomy with hepaticojejunostomy | 7.522 +/− 0.175 | 7.180 – 7.865 |
| Left trisectionectomy with caudate resection | 8.257 +/− 0.149 | 7.965 – 8.548 |
| Right hepatectomy with portal vein reconstruction, main to left | 8.754 +/− 0.167 | 8.427 – 9.082 |
| Right trisectionectomy with portal vein reconstruction, main to left | 8.988 +/− 0.178 | 8.640 – 9.337 |
| Right hepatectomy with IVC reconstruction | 9.351 +/− 0.174 | 9.010 – 9.692 |
The relative complexity of the procedures is best understood from Figure 1 which shows the mean scores and 95% confidence limits for these procedures. Left hepatectomy without caudate resection was deemed next easiest procedure with a score of 4.39. The five procedures with the highest scores were right trisectionectomy with hepaticojejunostomy, left trisectionectomy with caudate resection, and three right sided resections associated with a vascular resection and reconstruction.
Figure 1.
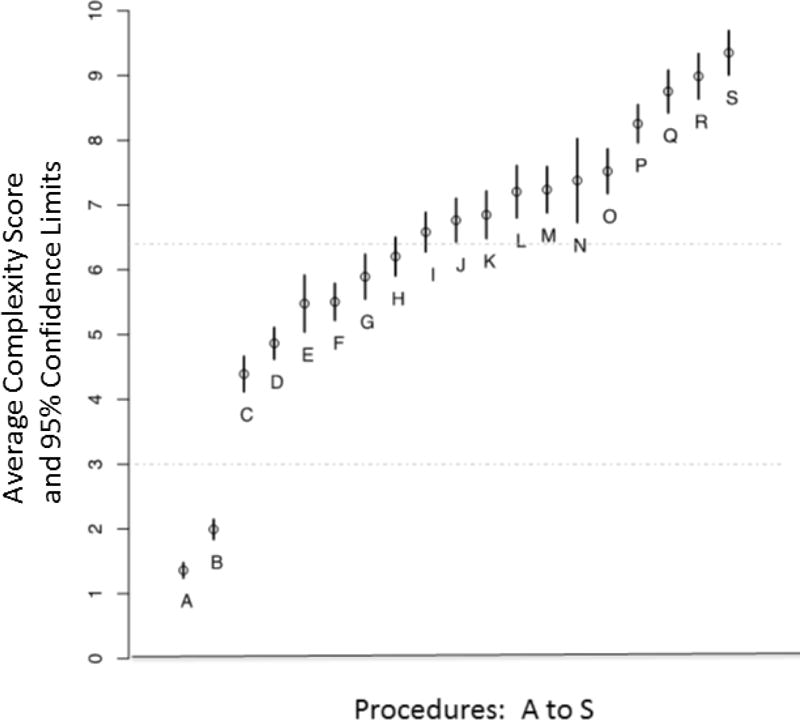
The adjusted mean complexity score and 95% confidence interval for each type of liver resection included in the survey. (A) Peripheral wedge resection; (B) left lateral sectionectomy; (C) left hepatectomy without caudate resection; (D) right hepatectomy; (E) right posterior sectionectomy; (F) left hepatectomy with caudate resection; (G) isolated caudate resection; (H) right trisectionectomy; (I) right anterior sectionectomy; (J) right hepatectomy with caudate resection; (K) right hepatectomy with hepaticojejunostomy; (L) anatomic middle hepatectomy; (M) right trisectionectomy with caudate resection; (N) left trisectionectomy without caudate resection; (O) right trisectionectomy with hepaticojejunostomy; (P) left trisectionectomy with caudate resection; (Q) right hepatectomy with portal vein reconstruction [main to left]); (R) right trisectionectomy with portal vein reconstruction [main to left]; (S) right hepatectomy with IVC reconstruction.
Effect of Addition of Caudate Resection
Figure 2 demonstrates the shift in the frequency curve of complexity scores as well as the shift in the mean scores when caudate resection is added to four standard liver resections. The addition of caudate resection resulted in a statistically significant increase in complexity scores in all four cases. This was particularly evident for right hepatectomy, for which addition of caudate resection increased difficulty from a score of 4.86 to 6.77. Interestingly, left hepatectomy with caudate resection had a lower score (5.51) than isolated caudate resection (5.90), although this difference was not statistically significant.
Figure 2.
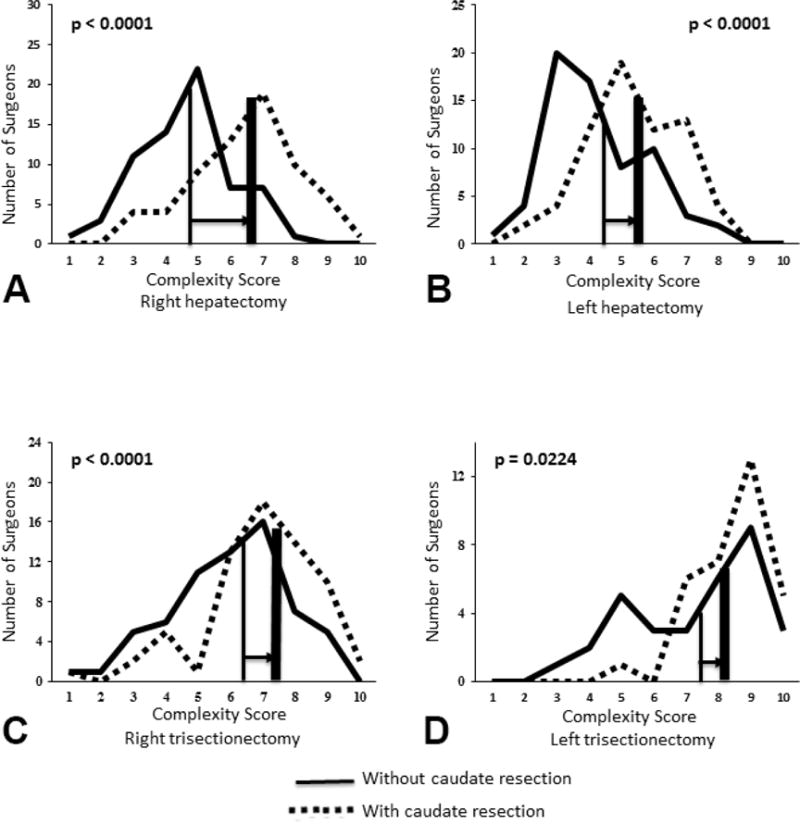
Effect on complexity score of addition of caudate resection to: (A) Right hepatectomy; (B) left hepatectomy; (C) right trisectionectomy; (D) left trisectionectomy. In each case the solid curve indicates the results for a procedure without caudate resection and the dotted curve the results for the same procedure with caudate resection added. The horizontal axis is the complexity score and the vertical axis is the number of surgeons who selected a particular score. The thin solid vertical line where it intersects the horizontal axis indicates the mean score for each procedure without caudate resection. The thick vertical line where it intersects the horizontal axis is the mean score for each procedure with caudate resection. The horizontal arrow depicts the shift in the mean score when caudate resection was added to each procedure. The p value indicates the significance of this difference.
Effect of Addition of Hepaticojejunostomy
Figure 3 demonstrates the shift in the frequency curve of complexity scores as well as the shift in the mean scores when hepaticojejunostomy is added to right hepatectomy and right trisectionectomy. The addition of hepaticojejunostomy resulted in a statistically significant increase in complexity scores in both cases (Figure 3).
Figure 3.
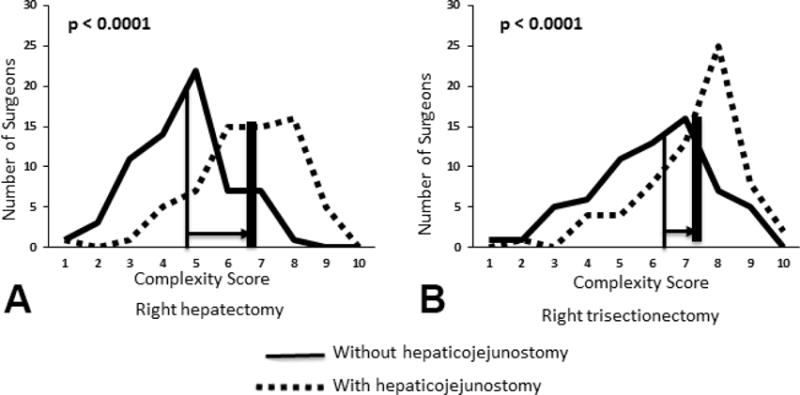
Effect on complexity score of addition of hepaticojejunostomy to: (A) Right hepatectomy; (B) right trisectionectomy. Axes and lines as for Figure 2
Effect of Addition of Vascular Resection
Figure 4 demonstrates the shift in the frequency curve of complexity scores as well as the shift in the mean scores when vascular resections were added to standard liver procedures. We evaluated the addition of portal vein resection to right hepatectomy and right trisectionectomy and the addition of inferior vena cava resection to right hepatectomy. The addition of vascular resection resulted in a statistically significant increase in complexity scores in all cases (Figure 4). These were the largest shifts in mean scores that were seen in this study. Addition of inferior vena cava resection to right hepatectomy resulted in the largest shift in complexity score from 4.87 to 9.35. The latter was the highest score recorded for any procedure. Resection and reconstruction of the vena cava was rated as more difficult than portal vein resection, as a right hepatectomy with IVC reconstruction was deemed significantly more difficult than either right hepatectomy or right trisectionectomy with portal vein reconstruction (p = 0.0003 and p = 0.011, respectively). For all resections, hepatectomy with venous reconstruction was rated as significantly more difficult than hepatectomy with hepaticojejunostomy (p < 0.0001 for all resections).
Figure 4.
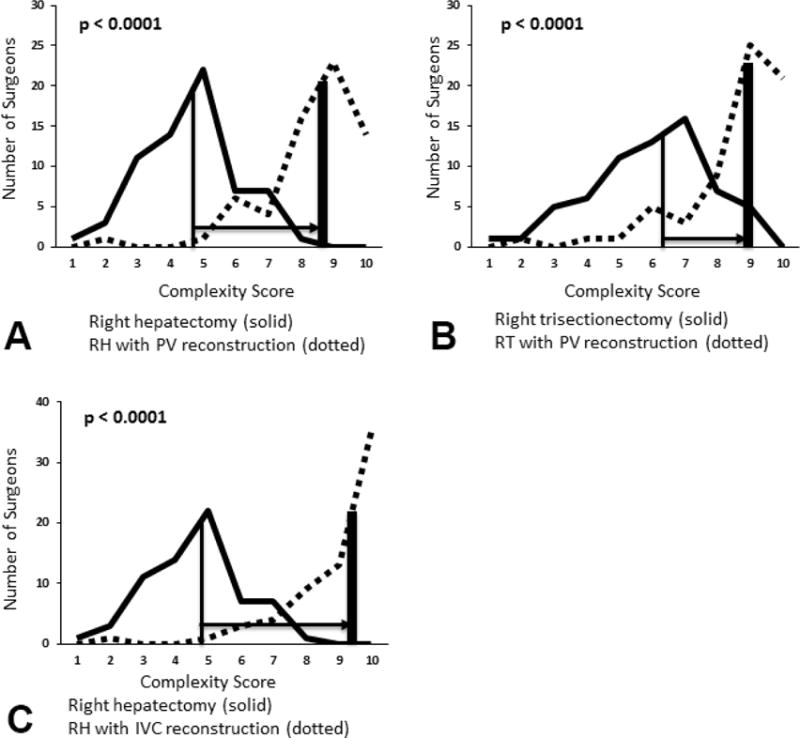
(A) Effect on complexity score of addition of portal vein resection and reconstruction to right hepatectomy; (B) effect of addition of portal vein resection and reconstruction to right trisectionectomy; (C) effect of addition resection and reconstruction of the inferior vena cava to right hepatectomy. Axes and lines as for Figure 2.
The effects of experience and practice patterns on complexity scoring
Table 4 breaks down the complexity scores by the level of experience. Our prior results suggested that more experienced surgeons are likely to rate the same procedure as easier than less experienced surgeons (2). To formally evaluate this trend, we divided the respondents into surgeons who had performed 0–500 liver resections in their career and surgeons that had performed over 500. The differences between individual procedures were not statistically significant in any case. However, 18 of the 19 resections in the study were rated less difficult by more experienced surgeons (Table 4). After adjusting multiple comparisons, the more experienced surgeons had a lower overall score (p=0.022) (Table 4). The procedures that showed the greatest differences in scoring were right trisectionectomy, left trisectionectomy with caudate resection, anatomic middle hepatectomy, and the three resections with vascular reconstruction. Notably, three of the five procedures with the smallest discrepancy were wedge resection, left lateral sectionectomy, and right hepatectomy. These likely represent the three most commonly performed liver resections.
Table 4.
Effect of Experience on Complexity Scoring
| Procedure | Group 1 score, <500resections | Group 2 score, >500resections | p Value |
|---|---|---|---|
| Peripheral wedge resection, < 3 cm | 1.401 | 1.288 | 0.464 |
| Left lateral sectionectomy | 2.020 | 1.929 | 0.656 |
| Left hepatectomy without caudate resection | 4.633 | 4.152 | 0.245 |
| Right hepatectomy | 4.871 | 4.820 | 0.838 |
| Right posterior sectionectomy | 5.800 | 5.167 | 0.362 |
| Left hepatectomy with caudate resection | 5.818 | 5.228 | 0.184 |
| Isolated caudate resection | 6.136 | 5.658 | 0.361 |
| Right trisectionectomy | 6.521 | 5.909 | 0.176 |
| Right anterior sectionectomy | 6.837 | 6.333 | 0.245 |
| Right hepatectomy with caudate resection | 7.029 | 6.521 | 0.362 |
| Right hepatectomy with hepaticojejunostomy | 6.778 | 6.876 | 0.838 |
| Anatomic middle hepatectomy | 7.733 | 6.714 | 0.176 |
| Right trisectionectomy with caudate resection | 7.495 | 6.999 | 0.386 |
| Left trisectionectomy without caudate resection | 7.546 | 7.191 | 0.690 |
| Right trisectionectomy with hepaticojejunostomy | 7.639 | 7.396 | 0.656 |
| Left trisectionectomy with caudate resection | 8.6 | 7.922 | 0.176 |
| Right hepatectomy with portal vein reconstruction, main to left | 9.145 | 8.407 | 0.176 |
| Right trisectionectomy with portal vein reconstruction, main to left | 9.396 | 8.629 | 0.176 |
| Right hepatectomy with IVC reconstruction | 9.826 | 8.938 | 0.176 |
There were no statistically-significant differences in the complexity scores given by HPB surgeons, non-transplant liver surgeons, and transplant surgeons for any individual resection (data not shown). There was also no difference in the overall score (p=0.951). No clearly discernible trends were noted between these groups.
Discussion
Historically, liver resections have been classified as “minor” or “major” depending on the number of segments resected (1). As a classification of complexity, this division is clearly flawed. The number of segments resected is important in predicting postoperative liver failure, and the minor/major division should be retained for that purpose. However, the number of segments resected is at best modestly correlated with the complexity of the resection. We previously surveyed expert liver surgeons to develop the first quantitative assessment of the complexity of liver resections (2). This formed the basis for a three-tiered complexity classification. However, the initial classification did not account for variants such as the addition of caudate resection, hepaticojejunostomy or vascular resection.
Our prior report essentially served as a precursor to this more detailed study. The methodology was similar, but this study is more complete due to the larger number of resections and the ability to evaluate concomitant procedures. As explained, it is difficult to accomplish this with one study, as evaluating 20 resections at once can generate responder fatigue. This may compromise both the response rate and the validity of the data. An alternative would have been to send different surveys to different surgeons and to merge the results. However, this strategy may not have generated enough responses for each procedure to allow conclusions. Instead, we first developed a survey with a smaller number of core procedures and then sent this more robust survey to a similar cohort of surgeons many of whom were familiar with the prior survey. This was in our opinion a better way to obtain valid data for a large group of resections.
Comparing this study and our prior report, we found that the assessment of complexity for the nine in-common procedures was similar. The rank order of complexity for the nine resections was completely identical in the two surveys, and the actual complexity scores were quite similar as well. This was especially true for lower complexity procedures. As would be expected, the addition of several highly complex procedures in this report resulted in lower scores for procedures previously deemed most difficult. The similarity in rank order and actual scores occurred despite the fact that the surgeon responders presumably differ to some degree. In this way, the current study validates the findings of the prior report and lends credence to the results of both studies.
We also found that caudate resection and biliary reconstruction were perceived fairly similarly in terms of added complexity. Both significantly increased the complexity of a resection and did so to a similar degree. A concomitant vascular resection added significantly more complexity than caudate resection or biliary reconstruction. The experts rated the addition of a caudate resection to a right hepatectomy as more complex than the addition of a caudate resection to a left hepatectomy as would be expected. Likewise experts considered the addition of inferior vena caval resection as more challenging than the addition of a portal vein resection.
Amending the complexity classification based on the present study
We previously used complexity scores to divide procedures into three categories —Low Complexity, Medium Complexity, and High Complexity (2). All seven of the procedures newly evaluated in this study fit best in the high complexity range as shown by the bolded entries in Table 5. The classification is otherwise unchanged. The classification is unbalanced if judged by the number of procedures in each category but is quite justified and practical. As noted in the prior study and shown in Figure 1, the two entries in the Low Complexity group had scores that were statistically significantly different from all other procedures. This justifies a cutpoint at the interface between these and higher complexity procedures. In the prior study, the High Complexity procedures were separated from the procedures of Medium Complexity at a cutpoint around 6.5 which is two-thirds of the way up the scale. The High Complexity procedures included all four procedures in which the right intersectional plane is traversed. The newly evaluated procedures all fit in the range above 6.5 and have been placed in the High Complexity group for that reason. Although there are 6 entries in the Medium Complexity group and 11 in the High Complexity group, the Medium Complexity group consists of more commonly performed procedures. The groups should therefore equalize in terms of the numbers of procedures performed, which is an important factor in comparative studies. This concept also illustrates the problem with adding another group—dividing the high complexity procedures into two groups would decrease their numbers and make comparative studies more difficult.
Table 5.
A New Classification for the Complexity of Liver Resections
| Complexity group, procedure | Complexity score |
|---|---|
| Low complexity | |
| Peripheral wedge resection, < 3 cm | 1.361 |
| Left lateral sectionectomy | 1.994 |
| Medium complexity | |
| Left hepatectomy without caudate resection | 4.392 |
| Right hepatectomy without caudate resection | 4.866 |
| Right posterior sectionectomy | 5.479 |
| Left hepatectomy with caudate resection | 5.505 |
| Isolated caudate resection | 5.895 |
| Right trisectionectomy | 6.206 |
| High complexity | |
| Right anterior sectionectomy | 6.583 |
| Right hepatectomy with caudate resection | 6.767 |
| Right hepatectomy with hepaticojejunostomy | 6.850 |
| Anatomic middle hepatectomy | 7.205 |
| Right trisectionectomy with caudate resection | 7.239 |
| Left trisectionectomy without caudate resection | 7.378 |
| Right trisectionectomy with hepaticojejunostomy | 7.522 |
| Left trisectionectomy with caudate resection | 8.257 |
| Right hepatectomy with portal vein reconstruction (main to left) | 8.754 |
| Right trisectionectomy with portal vein reconstruction (main to left) | 8.988 |
| Right hepatectomy with IVC reconstruction | 9.351 |
Use of Complexity Scores to compare procedural complexity of two hypothetical groups of patients
One use of procedural complexity scores will be to compare quantitatively the relative complexity of liver resections between groups of patients in outcomes studies. In Table 6 two hypothetical groups of patients are compared. In this example, there are 100 patients in each group and each group has an identical number of “minor” and “major” procedures. However the mean complexity score in group 2 (4.69 +/−1.94SD) is significantly higher than that in group 1 (3.94 +/−1.84 SD)(p = 0.006). This type of complexity analysis should be useful in future comparisons of among groups of patients in studies of methods and devices used in liver resection. Complexity score might also be helpful in cost studies especially as it seems to relate well to morbidity, in studies on prediction of complications, and to evaluate training in liver surgery. It could also be used as a variable in propensity scoring. Notably, it is absolutely essential to use large groups of patients i.e., at least as large as this example in these types of comparisons. Otherwise there may be an error of the second kind in which it is concluded that there is no difference between groups when what is lacking is group size.
Table 6.
Comparison of Procedural Complexity in 2 Hypothetical Groups of Patients
| Group 1 | Group 2 | |||||
|---|---|---|---|---|---|---|
| Procedure | n | Unit complexity score | Mean complexity score | n | Unit complexity score | Mean complexity score |
| Peripheral wedge resection | 12 | 1.36 | 16.32 | 8 | 1.36 | 10.88 |
| Left lateral sectionectomy | 26 | 1.99 | 51.74 | 18 | 1.99 | 35.82 |
| Right posterior sectionectomy | 10 | 5.48 | 54.80 | 14 | 5.48 | 76.72 |
| Right anterior sectionectomy | 2 | 6.58 | 13.16 | 10 | 6.58 | 65.80 |
| Left hepatectomy | 14 | 4.39 | 61.46 | 8 | 4.39 | 35.12 |
| Right hepatectomy | 24 | 4.87 | 116.88 | 20 | 4.87 | 97.40 |
| Right trisectionectomy | 10 | 6.21 | 62.10 | 18 | 6.21 | 111.78 |
| Right hepatectomy with PV reconstruction | 2 | 8.75 | 17.50 | 4 | 8.75 | 35.00 |
Group 1 mean complexity score = 3.94 (1.84 SD); group 2 mean complexity score = 4.69 (1.94SD); p = 0.006.
Surgeon perceptions on complexity
The study also provides insight into how expert surgeons determine complexity. The four procedures rated as easiest in this survey were peripheral wedge resection, left lateral sectionectomy, left hepatectomy, and right hepatectomy. These procedures differ significantly in terms of the number of segments resected, the mobilization of the liver, and the anatomic considerations. What they share is that they are common and are thus familiar to any surgeon with extensive training in liver surgery. By contrast, the four most complex procedures are performed infrequently by most liver surgeons. It is clear that the “complexity” of a procedure is based at least in part on its familiarity. This likely explains why more experienced surgeons essentially always rated a procedure as less complex than similarly-trained but less experienced liver surgeons. It may also explain why resections involving the right intersectional plane were viewed as the most difficult liver resections in both studies and much more complex than resections through the midplane or the umbilical fissure.
Vascular resection and reconstruction was felt to be much more difficult than biliary reconstruction. Anatomically, identifying and dissecting a bile duct is not much easier than doing the same for a portal vein. The caliber of bile ducts is usually much smaller than that of a portal vein branch, and a biliary anastomosis does require creation of a Roux limb. Why, then, is portal venous reconstruction so much more complex than biliary reconstruction? One reason is that biliary-enteric anastomosis is done more frequently including some procedures in which liver resection is not done. Secondly, venous reconstruction is more hazardous than biliary reconstruction. The potential for major blood loss and life-threatening complications is higher. In these ways, the perceived difference between a vascular and biliary reconstruction suggests that familiarity, hazard, and morbidity are also central components of perceived complexity.
Limitations of the Study
There are several limitations to the current survey. First, it is clear that not all resections are created equal. A right hepatectomy may be straightforward or very difficult depending on patient and tumor factors such as body mass index, tumor size, tumor location, and anatomic anomalies. We cannot account for this in our survey which asks responders only to rate “right hepatectomy.” It is likely that responders are rating these procedures assuming that they are straightforward or “typical.”
The response rate in our survey (54.1%) is slightly higher than our last response rate but remains less than ideal. This study is dominated by respondents from North America and Europe and largely excludes Asia. This was based on very low response rates from Asia in our last study. Because we wanted a similar number of respondents, the two surveys from the prior and current survey were sent to a somewhat different cohort of surgeons. This did require some adjustment in deriving our complexity scores. However, it was advantageous in one respect. We found that the order of difficulty and the complexity scores for the in-common procedures was quite similar. This served as a validation for the results of the prior study as two non-identical surgeon groups viewed the procedures similarly.
The variety of possible liver resections is great and not all types and variations could be included in these studies. For instance large non-anatomical resection (i.e. over 3 cm in maximum diameter) has not been included because it is difficult to define. Individual anatomic segment resections other than caudate resection are not included since there were just too many to encompass in these two studies. Living donor hepatectomies are important variations of standard procedures due to the requirements for recognizing, identifying, and preserving the arterial, venous, and biliary structures. Variations of standard procedures such as this were not included. The number of resections evaluated here does allow for the relative complexity of some non-surveyed procedure to be inferred. For instance, a left trisectionectomy with portal vein reconstruction would certainly be a high complexity procedure and would likely be the highest or second-highest procedure scored were it surveyed. This is based on the fact that left trisectionectomy was deemed the most difficult pure liver resection, and procedures that included venous resections were consistently rated most difficult.
Lastly, this study is designed to assess only technical difficulty and not morbidity. Alternative models have defined minor and major hepatectomy based on morbidity alone, but the types of resections were limited (10). While morbidity relates to more than simply the technical difficulty of a procedure, there is evidence that these complexity scores correlate with morbidity. Muangkaew, et al. recently reviewed 150 resections done for hepatocellular carcinoma (3). They found that estimated blood loss, transfusion, operative time, overall complications, and major complications were associated with the complexity group. On multivariable analysis, complexity classification was predictive of major postoperative complications. This study demonstrates how the complexity classification can be used to stratify procedures and that morbidity correlated with complexity.
Précis.
Utility weighting was used to develop complexity scores for a variety of liver resections including several that involved caudate resection, hepaticojejunostomy, and vascular reconstructions. The scores promote more accurate separation of liver resections into 3 categories of complexity on a quantitative basis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Couinaud C. [Contribution of anatomical research to liver surgery] Fr Med. 1956;19:5–12. [PubMed] [Google Scholar]
- 2.Lee MKt, Gao F, Strasberg SM. Perceived complexity of various liver resections: results of a survey of experts with development of a complexity score and classification. J Am Coll Surg. 2015;220:64–69. doi: 10.1016/j.jamcollsurg.2014.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Muangkaew P, Cho JY, Han HS, et al. Defining surgical difficulty according to the perceived complexity of liver resection: validation of a complexity classification in patients with hepatocellular carcinoma. Ann Surg Oncol. 2016 doi: 10.1245/s10434-015-5058-2. in press. [DOI] [PubMed] [Google Scholar]
- 4.de Jong MC, Marques H, Clary BM, et al. The impact of portal vein resection on outcomes for hilar cholangiocarcinoma: a multi-institutional analysis of 305 cases. Cancer. 2012;118:4737–4747. doi: 10.1002/cncr.27492. [DOI] [PubMed] [Google Scholar]
- 5.Abbas S, Sandroussi C. Systematic review and meta-analysis of the role of vascular resection in the treatment of hilar cholangiocarcinoma. HPB (Oxford) 2013;15:492–503. doi: 10.1111/j.1477-2574.2012.00616.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Azoulay D, Pascal G, Salloum C, et al. Vascular reconstruction combined with liver resection for malignant tumours. Br J Surg. 2013;100:1764–1775. doi: 10.1002/bjs.9295. [DOI] [PubMed] [Google Scholar]
- 7.Chen W, Ke K, Chen YL. Combined portal vein resection in the treatment of hilar cholangiocarcinoma: a systematic review and meta-analysis. Eur J Surg Oncol. 2014;40:489–495. doi: 10.1016/j.ejso.2014.02.231. [DOI] [PubMed] [Google Scholar]
- 8.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–130. [PubMed] [Google Scholar]
- 9.Benjamini YaH Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Royal Stat Soc Series B. 1995;57:289–300. [Google Scholar]
- 10.Shubert CR, Habermann EB, Truty MJ, et al. Defining perioperative risk after hepatectomy based on diagnosis and extent of resection. J Gastrointest Surg. 2014;18:1917–1928. doi: 10.1007/s11605-014-2634-x. [DOI] [PubMed] [Google Scholar]


